Abstract
Objectives
To evaluate the effects of a workplace-based intervention on actigraphic and self-reported sleep outcomes in an extended care setting.
Design
Cluster randomized trial.
Setting
Extended-care (nursing) facilities.
Participants
US employees and managers at nursing homes. Nursing homes were randomly selected to intervention or control settings.
Intervention
The Work, Family and Health Study developed an intervention aimed at reducing work-family conflict within a 4-month work-family organizational change process. Employees participated in interactive sessions with facilitated discussions, role-playing, and games designed to increase control over work processes and work time. Managers completed training in family-supportive supervision.
Measurements
Primary actigraphic outcomes included: total sleep duration, wake after sleep onset, nighttime sleep, variation in nighttime sleep, nap duration, and number of naps. Secondary survey outcomes included work-to-family conflict, sleep insufficiency, insomnia symptoms and sleep quality. Measures were obtained at baseline, 6-months and 12-months post-intervention.
Results
A total of 1,522 employees and 184 managers provided survey data at baseline. Managers and employees in the intervention arm showed no significant difference in sleep outcomes over time compared to control participants. Sleep outcomes were not moderated by work-to-family conflict or presence of children in the household for managers or employees. Age significantly moderated an intervention effect on nighttime sleep among employees (p=0.040), where younger employees benefited more from the intervention.
Conclusion
In the context of an extended-care nursing home workplace, the intervention did not significantly alter sleep outcomes in either managers or employees. Moderating effects of age were identified where younger employees’ sleep outcomes benefited more from the intervention.
INTRODUCTION
Sleep critically affects physical and mental health.1 This line of inquiry is important given the rise of 24-7 economies that push more workers into long and nonstandard work hours that can interfere with sleep quantity and quality. Indeed, 30% of U.S. workers today have insufficient sleep – less than 6 hours per night2 – which may be linked to poor general health and increased disease risk relative to obtaining 7-8 hours of sleep.3 Moreover, the trend of sleep insufficiency is likely to vary markedly across workforce age cohorts and occupational categories.4
Cross-sectional studies show that longer work hours are consistently related to poorer sleep quality and reduced sleep quantity.5, 6 There are also longitudinal links between work time and sleep, such that having less control over work time increases the risk of sleep disturbances (symptoms 5-7 nights/week) among employees.6 Sleep typically occurs at home, making it important to understand how work and family interactions shape employee sleep. Because time is a limited resource, sleep time often competes with time allocated to work and family demands. For example, employees are more likely to have shorter sleep duration when they spend longer hours at work, and even more so when they also are committed to spending time with family.7 Thus, a growing body of evidence is suggesting that incompatible work to family role demands, or work-family conflict (WFC)8 may spillover to employees’ personal life and influence their sleep. Specifically, work role expectations and stressors can carry over to the family domain to interfere with family/personal activities. Work-family conflict is an important psychological stressor for employees that increases need for recovery from work and fatigue.9 Prior studies have shown that WFC is negatively associated with employees’ sleep quantity and quality.10, 11 Most of these studies are cross-sectional and lacking the capacity to determine the causal direction between WFC and sleep. However, a few promising studies have also provided longitudinal evidence that WFC increases sleep problems.12, 13 Moreover, the causal link has been found in a number of countries, including the UK, Finland, and Japan.12 These studies suggest that WFC, mostly time-based conflicts between work and family roles, are detrimental to employee sleep, across times and settings.
Workplace interventions may reduce tensions between work and family life and thereby improve employee sleep. In our prior study with Information Technology (IT) workers, we found that employees whose managers were less supportive of work and family issues slept less.14-16 Thus far, our prior study has demonstrated a positive effect of a workplace intervention for reducing WFC17 on objective sleep outcomes within a randomized controlled trial. In a randomized experiment in an IT firm, the workplace intervention that addressed reducing WFC through an organizational change process significantly increased employees’ actigraphically-assessed total sleep duration and perceived sleep sufficiency.18 This research points to the possible benefits of interventions aimed at increasing workplace and manager support as well as increasing employee's control over work time to improve employee sleep, and the need to investigate intervention effects in other settings such as health care. Limited research on workplace intervention effects on sleep has focused on individual-level employees’ coping behaviors, such as mindfulness practices,17, 19 rather than organizational changes in work practices. A few studies, however, have suggested that it is critical to reduce WFC at the workplace level to enhance employee well-being, including sleep.20-22 To extend these findings, we test whether a workplace intervention previously proven effective can improve sleep quantity and quality when implemented in a markedly different industry with lower-wage hourly workers in extended-care (nursing) facilities. Examining workers in the extended-care setting was of our interest, because their work context may be associated with high job strain, less control over work time, and high work-family conflict, which may have implications for poor sleep.23
This study therefore evaluated the effects of a randomized workplace intervention designed to increase family-supportive supervision and employee control over work time24 on objectively-measured actigraphic and self-reported measures of sleep in employees in the extended-care setting. Our primary hypotheses were that the intervention would improve sleep outcomes in both managers and employees in an extended care setting at the 12-month time point relative to the usual practice condition. We tested secondary hypotheses that the effect of the intervention on sleep outcomes would be moderated by life-course factors, such as age, baseline work-to-family conflict, or presence of children in the household. Age-related vulnerabilities in sleep physiology25 and age-related differences in work conditions could modify intervention effects. The baseline level of work-to-family conflict could also interact with intervention effects, such that workers who had higher work-to-family conflict at baseline may benefit more from the intervention than those with lower work-to-family conflict.21 In a similar vein, the intervention could bring more benefits to parents than non-parents because the former is in greater need for workplace support/flexibility.21
PARTICIPANT AND METHODS
Study participants
This study is part of the Work, Family, and Health Network (WFHN) Study.24 Study participants were recruited from an extended care (nursing home) industry partner.26 The study cohort consisted of a low-wage, primarily hourly workforce from 30 distinct worksites located in the northeastern US. Eligible employees were involved in direct patient care, typically worked at least 22 hours/week, and did not do regular nightwork. Overall, of the 1,783 eligible employees with direct patient care responsibilities, 1,524 were recruited (85% participation rate) and among the 211 eligible managers, 184 were recruited (87% participation rate). Study worksites were then adaptively randomized to either receive the intervention or continue with usual practice, as previously described.26 Both actigraphic and self-reported measurements were collected at baseline (prior to the intervention), 6-months, and 12-months post baseline. Figure 1 depicts study enrollment and follow-up. Appropriate Institutional review boards approved the study. All procedures were conducted in accordance with the Declaration of Helsinki.
Figure 1.
Flow diagram of study recruitment and retention.
Primary Outcomes: Actigraphic Sleep Measures
Primary actigraphic sleep measures were collected via a wrist-worn sleep monitor (Actiwatch Spectrum; Philips-Respironics, Murrysville, PA) they were instructed to wear for one week. Employees received up to $60 for completing all worksite data collection components at each time point. Actigraphy data were analyzed for subjects with at least three days of valid recordings and scored using the Actiware Sleep Scoring Program (Version 5.71, Philips-Respironics, 2012). A recently validated standard algorithm was used by at least two members of the scoring team to determine the validity of each day of recording, and then manually inserted visually-identified periods (main sleep intervals and naps). Scorers identified decreased activity levels within the context of the overall activity profile for the subject. Sudden, decreased light levels were confirmatory but not required. Actigraphy scorers determined a recording to be invalid if there was either constant false activity (i.e., device battery failure signal) on the recording, if the data were unable to be retrieved, or participant non-compliance (i.e., >4 hour of off-wrist time in a day, or an off-wrist period of more than 60 min within 10 min of the determined beginning or end of the main sleep period for that day). Each scored record was checked on an interval-by-interval basis for inter-rater agreement ensuring no differences in measures below exceeded a 15 min difference between raters. Actigraphic outcome measures were calculated as previously described18:
Mean Total Sleep Time
Mean total sleep (naps and main sleep) per day (minutes).
Nighttime sleep duration
The longest sleep period of the day was defined as the main, nighttime sleep. All other sleep periods of the day were defined as naps. Mean nighttime sleep duration was computed across all valid days (in minutes).
Wake After Sleep Onset (WASO)
WASO was computed as the average amount of time spent “awake” after sleep onset and before sleep offset during nighttime sleep, in minutes, as previously validated versus polysomnography (PSG).27
Nighttime sleep duration standard deviation
Standard deviation of all valid nighttime sleep period durations.
Number of Naps
Nap number was calculated as the average number of nap episodes (where nap episode=1) per day, regardless of length.
Nap duration
Mean nap duration (for those who had any naps) was computed in minutes per day.
Secondary Outcomes: Self-Reported Sleep and WFC Measures
Secondary self-reported sleep outcomes, demographic and working characteristics were collected using trained field interviewers who administered face-to-face Computer-Assisted Personal Interviews (CAPI) lasting 60 minutes. Final self-reported sleep outcome measures were calculated as described below.
Sleep Insufficiency was measured using a single item: ‘How often during the past 4 weeks did you get enough sleep to feel rested upon waking up?’ with answers selected from a 1-5 scale (ranging from ‘never’, to ‘very often’). Lower scores indicate higher levels of sleep insufficiency. This item has been used in prior research and is similar to current Centers for Disease Control and Prevention (CDC) surveillance for state-level sleep sufficiency.28
Insomnia Symptoms were measured using a single item, taken from the Pittsburgh Sleep Quality Index (PSQI)29: ‘During the past 4 weeks, how often did you wake up in the middle of the night or early morning?’, with answers selected from a 1-4 scale (ranging from ‘1, never’ to ‘ 4, three or more times a week’). High scores indicated higher levels of insomnia symptoms.
Sleep Quality was measured using a single item taken from the PSQI: ‘Over the past 4 weeks, how would you rate your sleep quality overall?’ with answers selected from a 1-4 scale (ranging from ‘1, very good’ to ‘4, very bad’. High scores indicated worse sleep quality.
Work-to-family conflict (WFC) was measured using the five-item subscale developed by Netemeyer and colleagues.30 This subscale consists of items rated on a scale from 1 (strongly disagree) to 5 (strongly agree) with higher scores indicating higher WFC and has a high reliability estimate of Cronbach's α=0.89.
Intervention
The WFH workplace intervention, named STAR (Support. Transform, Achieve. Results), was designed to increase employees’ control over their work and work time and increase family supportive supervisor behavior within a 4-month organizational change process. The intervention was previously evaluated in an information technology firm for safety and performance outcomes31, employee well-being32 and sleep outcomes18 and employees’ child sleep outcomes33. This workplace intervention was customized and implemented in the extended care industry34 to consist of facilitator-led sessions and activities for both employees and managers to help transition them from a time-base to a result-based work culture. Managers also received supplemental training and activities focused on increasing family-supportive supervision. The intervention was also branded START as unrelated program named STAR was already in place.
In the extended care setting the intervention included four facilitator-led sessions for all employees and managers together, and three facilitator-led sessions for managers and supervisors only. During sessions, employees discussed how to increase support for coworkers, such as moving to a more results-oriented work culture as well as eliminating negative judgments about how coworkers appeared to be spending their time at work.35 To support transfer of training, following this session employees participated in a collective self-monitoring of their experiences and how often they applied specific tactics learned in training, such as positively redirecting negative interactions. The additional training for managers and supervisors was delivered through computer-based training on family-supportive supervisory behaviors and their importance for employee health and workplace productivity. To support transfer, facilitators then provided managers with handheld devices with an application that helped them select particular supportive behaviors they wanted to focus on and set goals for the total supportive behaviors they would like to provide during the next two weeks. An example category of supportive behavior is Creative Work-Life Management that is one of the supportive behaviors identified in previous validation work,36 and an example behavior in this category was “Asking for input about how work can be organized to benefit both company and family or personal priorities.” Managers were then given feedback on goal progress each time they used the application, with collective, norm-referenced feedback at the end of the two-week period. This supportive behavior self-monitoring activity for managers was repeated once again toward the end of the intervention process; for more discussion of the intervention components, see Kossek et al.35
Statistical Methods
To analyze the potentially heterogeneous effects of the STAR intervention on outcomes among employees and managers, we stratified all analyses based on employee or manager status. Differences in individual demographic and working characteristics across intervention and usual practice groups were assessed using chi squared and Fisher's exact tests. These baseline comparisons were performed separately for different outcomes as different sample sizes were available for self-reported and actigraphic measures (Figure 1). Demographic characteristics that differed significantly across groups at baseline were included as covariates in final regression models.
To examine the relationship between intervention and sleep measures across time we used a generalized linear mixed modeling approach with restricted maximum-likelihood estimation.37 This allowed us to model the hierarchical structure of the data with measurements at each time point nested within individuals, and then further nested within worksites. The effect of the intervention was represented by a model parameter reflecting the interaction between an indicator for measurement time point and an indicator for being in the intervention group. This parameter represents the difference in relative average difference in outcomes between intervention individuals relative to usual practice individuals across time. Model diagnostic checks identified the appropriateness of a generalized linear mixed model with identity link for the following outcome measures: total sleep time, nighttime sleep time, wake after sleep onset (WASO), nighttime sleep duration standard deviation, sleep insufficiency, insomnia symptoms, sleep quality and work-to-family conflict (WFC). A Poisson mixed-effects model was used for number of naps per valid actigraphy day per subject. Zero-inflated Poisson mixed modeling38 was used for nap duration as the distribution included many zeroes due to non-napping subjects.
To test the hypotheses that the effect of the intervention on sleep outcomes would be moderated by participant characteristics, we adapted the generalized linear mixed models to include a three-way interaction for the moderating variable of interest: baseline work-to-family conflict (WFC), baseline categorical age (‘17-34 years’, ‘35-49 years’ and ‘50-75 years’), and presence of children in the house (dichotomous: yes/no). The three-way interaction parameter represents the moderating effect of the specified variable on the difference in relative average difference in outcomes between intervention individuals relative to usual practice individuals across time after controlling for potential confounders. All statistical tests were two-sided and statistical significance was defined as p-value less than 0.05. Statistical analyses were performed in SAS 9.3.
RESULTS
Overall, 1,967 participants were eligible and 1,708 were enrolled (enrollment rate of 86.8%). Of those enrolled, 1,524 were health care employees and 184 were managers across thirty worksites in one company (Figure 1). Of these, 1,522 (99.9%) employees and 184 (100%) managers provided self-reported sleep measures at baseline. For actigraphic measures, 1,220 (80.1%) employees provided at least 3 days of valid actigraphy data (a quality metric for reliable sleep estimates) at baseline. Only 81 of the 184 managers were offered actigraphy at baseline and among those, 65 managers (80.2%) provided at least 3 days of valid actigraphy data. At 12 months, 1,083 (71.1%) employees and 145 (78.8%) managers provided self-reported sleep measures. Among subjects with valid actigraphic baseline data, 733 (60.1%) employees and 49 (75.4%) managers provided valid actigraphy data at 12 months.
Subject characteristics for employees and managers with complete self-reported sleep measures at baseline are presented in Table 1. Because a lower percentage of study participants contributed baseline actigraphic data, the same subject characteristics among the sub-sample of participants with actigraphy are presented in Appendix Table 1. Overall, employees were typically female (91.8%), non-Hispanic White (66.6%), married (62.9%), and averaged 38.5 years of age with about one child. Similar subject characteristics were observed for managers, though this sample averaged 45.5 years of age. From Table 1, we observe that total hours worked per week differed significantly between intervention (mean 40.5±11.0 hours per week) and usual practice (mean 39.3±10.1 hours per week) conditions for employees. We observed a similar difference among employees providing actigraphy at baseline (Total hours worked per week: intervention 40.7±10.9, usual practice 39.2±9.4). Among managers in Table 1, levels of education differed at baseline between intervention and usual practice conditions with a higher percentage of college graduates in the usual practice arm. No statistically significant differences between study arms were observed among managers with valid baseline actigraphic measurements and both arms had similar dropout rates.
Table 1.
Patient characteristics at baseline by intervention condition stratified by Employee/Manager status (Percentage or mean ± SD reported)
| Employees | Managers | |||||
|---|---|---|---|---|---|---|
| Usual Practice (n = 799) | Intervention (n = 723) | P-value | Usual Practice (n = 96) | Intervention (n = 88) | P-value | |
| Female | 90.7% | 93.1% | 0.09 | 92.7% | 84.1% | 0.07 |
| Age (years) | 39.0±12.3 | 38.0±12.7 | 0.09 | 47.0±10.5 | 43.9±11.7 | 0.06 |
| Race | 0.11 | 0.80* | ||||
| White non-Hispanic | 65.7% | 67.6% | 90.6% | 87.5% | ||
| Black | 12.8% | 15.2% | 1.0% | 3.4% | ||
| Hispanic | 14.5% | 10.9% | 1.0% | 1.1% | ||
| Other | 7.0% | 6.2% | 7.3% | 8.0% | ||
| Married or living with partner | 64.8% | 60.7% | 0.10 | 71.9% | 68.2% | 0.58 |
| No of Children | 1.1±1.2 | 1.0±1.2 | 0.18 | 0.8±1.0 | 1.0±1.1 | 0.21 |
| Elder Care role | 27.9% | 32.4% | 0.06 | 28.1% | 28.4% | 0.97 |
| Education | 0.31 | 0.03* | ||||
| Less than High School Graduate | 5.8% | 5.8% | 0.0% | 0.0% | ||
| High School Graduate | 31.0% | 34.2% | 0.0% | 6.8% | ||
| Some College or technical school | 49.9% | 49.4% | 53.1% | 51.1% | ||
| College graduate | 13.4% | 10.7% | 46.9% | 42.1% | ||
| Total hours worked per week | 40.5±11.0 | 39.3±10.1 | 0.03 | 48.8±8.9 | 50.7±12.4 | 0.23 |
| Shift | 0.60 | 0.72* | ||||
| Variable | 4.4% | 4.6% | 24.0% | 22.7% | ||
| Regular daytime | 49.8% | 51.0% | 61.5% | 67.1% | ||
| Regular evening | 34.2% | 33.6% | 7.3% | 6.8% | ||
| Regular night | 2.0% | 1.1% | 0.0% | 0.0% | ||
| Rotating | 5.9% | 5.8% | 3.1% | 0.0% | ||
| Split | 2.5% | 1.8% | 2.1% | 1.1% | ||
| Other | 1.3% | 2.1% | 2.1% | 2.3% | ||
Fisher's exact test used as one or more expected cell counts <5
Note: Descriptive statistics shown for all subjects included in self-reported sleep outcome analysis. For the following patient characteristics, we observed some missing data on the survey items: EMPLOYEES: age (1 missing from intervention group and 1 missing from usual practice), no. of children (1 missing from usual practice), total hours worked per week (2 missing from intervention group and 2 missing from control group), education (1 missing from usual practice). MANAGERS: total hours (1 missing from usual practice).
The baseline burden of sleep deficiency for employees and managers, as estimated using actigraphic and self-reported sleep measures, is presented in Figure 2. At baseline, 67% of employees exhibited at least one component of sleep deficiency, with the highest category being sleep disrupted with 44% of employees having WASO ≥45 minutes per day. Only 14% of employees exhibited short sleep duration (<6.5 hours per day) at baseline. Similar observations were identified for managers.
Figure 2. Venn Diagram of the sleep deficiency in the study population at baseline for employees and managers.
Sleep deficiency at baseline (inadequate sleep quality and/or insufficient sleep duration) was defined as having ≥ 1 of the following components: Wake after Sleep Onset (WASO) > 45 minutes per main sleep period (measured using wrist actigraphy and suggestive of insomnia), self-reported sleep insufficiency (never or rarely feeling rested upon waking) and/or mean actigraphically-measured total sleep time < 6.5 hours per 24 hours.
Intervention effects on actigraphic sleep outcomes
The model predicted means based on generalized linear mixed models of actigraphic outcome measures over time by manager and employee strata are shown in Tables 2. Raw unadjusted means and standard deviations for actigraphic sleep outcomes by condition over time are presented in Appendix Table 2. We observed no statistically significant intervention effects for our primary actigraphic sleep outcomes for either employees or managers. Among employees, adjusted mean total sleep time change from 0 months to 12 months in the intervention condition was −4.1 minutes (95% CI −10.1, 1.9), and in the usual practice condition, the observed change was −1.2 minutes (95% CI −6.6, 1.9). Among managers, adjusted mean total sleep time change from 0 months to 12 months was −7.0 minutes (95% CI −30.1, 16.1) with usual practice increasing mean total sleep time by 16.6 minutes (95% CI −6.9, 40.1) from baseline to 12 months. For employees in the intervention group, from baseline to 12-month follow-up, we observed an increase in mean WASO (+2.0 min) and a decrease in mean nighttime sleep duration (−3.6 minutes) while employees in the usual practice saw an increase in mean WASO of 0.4 minutes and increased mean nighttime sleep of 1.2 minutes. Among managers, the change in mean WASO from baseline to 12-months was +1.0 minutes for the intervention group and +4.6 for the control group (p=0.726). An average change in mean nighttime sleep between baseline and 12-months of −6.0 minutes was observed in managers in the intervention arm and +18.2 in the usual practice arm (p=0.226). The intervention group showed a smaller change in nighttime sleep variability from baseline to follow-up relative to usual practice for both employees and managers; however, these differences were not statistically significant. Within-group rate ratios denoting change from baseline to 12-months for number of naps and nap duration are presented in Table 2. No significant difference from baseline to 12-months was observed within or between groups.
Table 2.
Adjusted mean actigraphic outcomes by intervention condition among employees and managers. Confidence intervals presented in parentheses. Change is defined as 12-month outcome minus baseline outcome. Reported p-values denote statistical test of parallel lines (i.e. intervention group by time interaction).
| Employees | Managers | |||
|---|---|---|---|---|
| Outcome Measure | Intervention (baseline n=568) | Usual Practice (baseline n=652) | Intervention (baseline n=33) | Usual Practice (baseline n=32) |
| Total Sleep (minutes) | p=0.179 | p=0.321 | ||
| Baseline | 458.6 (451.6, 465.6) | 450.2 (443.6, 456.9) | 466.6 (442.6, 490.6) | 456.0 (427.6, 484.3) |
| 6 months | 456.0 (448.5, 463.6) | 454.7 (447.7, 461.7) | 462.3 (435.0, 489.6) | 455.9 (425.4, 486.4) |
| 12 months | 454.5 (446.7, 462.3) | 449.0 (441.8, 456.3) | 459.6 (433, 486.3) | 472.6 (442.4, 502.8) |
| Change | −4.1 (−10.1, 1.9) | −1.2 (−6.6, 4.2) | −7.0 (−30.1, 16.1) | +16.6 (−6.9, 40.1) |
| Wake After Sleep Onset (minutes) | p=0.265 | p=0.726 | ||
| Baseline | 44.3 (42.5, 46.0) | 45.2 (43.6, 46.8) | 45.2 (36.5, 53.9) | 49.8 (39.6, 60.1) |
| 6 months | 48.0 (46.1, 49.9) | 48.8 (47.0, 50.5) | 48.8 (39.2, 58.4) | 54.0 (43.2, 64.8) |
| 12 months | 46.4 (44.4, 48.4) | 45.6 (43.8, 47.4) | 46.2 (36.8, 55.6) | 54.4 (43.7, 65.2) |
| Change | +2.1 (0.4, 3.8) | +0.4 (−1.2, 1.9) | +1.0 (−5.9, 7.9) | +4.6 (−2.4, 11.7) |
| Nighttime Sleep Duration (minutes) | p=0.067 | p=0.226 | ||
| Baseline | 433.7 (425.7, 441.8) | 426.5 (418.8, 434.1) | 451.4 (427.1, 475.7) | 438.0 (409.1, 466.9) |
| 6 months | 432.5 (424.0, 441.1) | 434.5 (426.5, 442.5) | 453.0 (426.0, 480.0) | 444.4 (413.8, 475.1) |
| 12 months | 430.1 (421.3, 438.9) | 427.6 (419.4, 435.9) | 445.3 (418.8, 471.9) | 456.2 (425.8, 486.6) |
| Change | −3.6 (−9.8, 2.5) | +1.2 (−4.4, 6.7) | −6.0 (−26.6, 14.5) | +18.2 (−2.7, 39.2) |
| Nighttime Sleep Duration SD (minutes) | p=0.152 | p=0.526 | ||
| Baseline | 88.5 (84.5, 92.6) | 85.2 (81.4, 89.1) | 70.7 (55.6, 85.8) | 61.2 (43.6, 78.8) |
| 6 months | 88.9 (84.2, 93.5) | 90.5 (86.3, 94.7) | 69.1 (51.3, 87.0) | 56.4 (37.1, 75.7) |
| 12 months | 88.3 (83.4, 93.2) | 83.4 (79.0, 87.9) | 74.9 (57.7, 92.1) | 76.3 (57.2, 95.4) |
| Change | −0.2 (−5.2, 4.8) | −1.8 (−6.3, 2.7) | +4.2 (−13.4, 21.9) | +15.1 (−2.9, 33.1) |
| Number of Naps per subject per week (n) | p=0.498 | p=0.967 | ||
| Baseline | 1.5 (1.3, 1.6) | 1.4 (1.3, 1.5) | 1.1 (0.7, 1.8) | 1.2 (0.7, 2.1) |
| 6 months | 1.4 (1.2, 1.5) | 1.2 (1.1, 1.3) | 0.8 (0.4, 1.5) | 1.0 (0.5, 1.8) |
| 12 months | 1.4 (1.3, 1.6) | 1.3 (1.2, 1.4) | 1.2 (0.7, 2.0) | 1.3 (0.7, 2.3) |
| Change (Rate Ratio) | 0.99 (0.89,1.11) | 0.94 (0.85, 1.04) | 1.07 (0.66, 1.73) | 1.05 (0.67, 1.63) |
| Nap Duration per nap (minutes) | p=0.553 | p=0.083 | ||
| Baseline | 34.4 (31.7, 37.4) | 36.1 (33.2, 39.3) | 29.0 (21.3, 39.4) | 24.2 (16.3, 35.9) |
| 6 months | 34.3 (31.1, 37.8) | 34.4 (31.1, 38.0) | 16.4 (8.9, 30.0) | 26.0 (18.5, 36.7) |
| 12 months | 34.5 (30.9, 38.6) | 32.9 (29.7, 36.4) | 22.4 (16.4, 30.7) | 35.4 (23.7, 52.9) |
| Change (Rate Ratio) | 1.00 (0.88, 1.13) | 0.91 (0.81, 1.02) | 0.78 (0.52, 1.16) | 1.46 (0.89, 2.42) |
Note: Adjusted means were estimated using linear mixed model with identity link for the following outcome measures: total sleep time, wake after sleep onset, nighttime sleep duration and nighttime sleep duration standard deviation. A Poisson mixed-effects model was used for number of naps per valid day of actigraphy per subject. Zero-inflated Poisson mixed modeling was used for nap duration as the distribution included many zeroes due to non-napping subjects. For count outcomes, change from baseline to 12-months is reported as a rate ratio. For employee analyses, all models adjusted for total hours worked per week. For manager analyses, all models adjusted for education level. Bolded statistics denote statistically significant change from baseline to 12-month within groups.
Intervention effects on self-reported sleep outcomes
Table 3 displays the model predicted means of self-reported outcomes measures by managers and employees designation over time. We observed no statistically significant intervention effects for our secondary self-reported sleep outcomes. For employees and managers, the baseline mean of self-reported insomnia symptoms and sleep insufficiency is around three and this does not change over the study period for either intervention or usual practice groups. Mean WFC at baseline for all subjects was about 3.0 out of 5.0, and this did not significantly change over time for employees or managers in either intervention or usual practice groups.
Table 3.
Adjusted model mean self-reported outcome measures by intervention condition among employees and managers. Confidence intervals presented in parentheses. Change is defined as 12-month outcome minus baseline outcome. Reported p-values denote statistical test of parallel lines (i.e. intervention group by time interaction).
| Employees | Managers | |||
|---|---|---|---|---|
| Intervention (baseline n=723) | Usual Practice (baseline n=799) | Intervention (baseline n=88) | Usual Practice (baseline n=96) | |
| WFC (1-5)a | p=0.541 | p=0.385 | ||
| Baseline | 2.9 (2.8, 2.9) | 2.8 (2.7, 2.8) | 3.0 (2.7, 3.3) | 2.5 (2.2, 2.9) |
| 6 months | 2.9 (2.8, 2.9) | 2.7 (2.6, 2.8) | 2.9 (2.6, 3.2) | 2.6 (2.2, 2.9) |
| 12 months | 2.8 (2.7, 2.9) | 2.7 (2.6, 2.7) | 2.8 (2.5, 3.1) | 2.5 (2.1, 2.8) |
| Change | +0.0 (−0.1, 0.0) | −0.1 (−0.2, 0.0) | −0.2 (−0.4, 0.0) | −0.1 (−0.2, 0.1) |
| Sleep Insufficiency (1-5)b | p=0.906 | p=0.636 | ||
| Baseline | 3.0 (2.9, 3.0) | 3.0 (2.9, 3.0) | 3.3 (3.0, 3.5) | 3.4 (3.1, 3.7) |
| 6 months | 3.0 (2.9, 3.1) | 3.0 (2.9, 3.1) | 3.4 (3.1, 3.7) | 3.5 (3.2, 3.8) |
| 12 months | 3.0 (2.9, 3.1) | 3.0 (3.0, 3.1) | 3.3 (3.0, 3.6) | 3.5 (3.2, 3.8) |
| Change | +0.1 (0.0, 0.1) | +0.1 (0.0, 0.2) | +0.0 (−0.2, 0.2) | +0.0 (−0.2, 0.2) |
| Insomnia Symptoms (1-4)c | p=0.569 | p=0.362 | ||
| Baseline | 3.2 (3.1, 3.3) | 3.3 (3.2, 3.3) | 3.4 (3.1, 3.6) | 3.5 (3.2, 3.8) |
| 6 months | 3.1 (3.0, 3.2) | 3.2 (3.1, 3.3) | 3.2 (3.0, 3.5) | 3.4 (3.1, 3.7) |
| 12 months | 3.2 (3.1, 3.3) | 3.2 (3.1, 3.3) | 3.4 (3.1, 3.6) | 3.4 (3.1, 3.7) |
| Change | +0.0 (−0.1, 0.1) | −0.1 (−0.1, 0.0) | +0.0 (−0.2, 0.2) | −0.2 (−0.3, 0.0) |
| Sleep Quality (1-4)d | p=0.644 | p=0.343 | ||
| Baseline | 2.3 (2.3, 2.4) | 2.4 (2.3, 2.4) | 2.2 (2.0, 2.4) | 2.2 (1.9, 2.4) |
| 6 months | 2.2 (2.2, 2.3) | 2.2 (2.2, 2.3) | 2.0 (1.8, 2.3) | 2.1 (1.9, 2.3) |
| 12 months | 2.2 (2.1, 2.3) | 2.2 (2.2, 2.3) | 2.2 (2.0, 2.4) | 2.1 (1.9, 2.3) |
| Change | −0.1 (−0.2, 0.1) | −0.1 (−0.2, −0.1) | 0.0 (−0.1, 0.2) | 0.0 (−0.2, 0.1) |
Note: Adjusted means were estimated using linear mixed model for all outcome measures. For count outcomes, change from baseline to 12-months is reported as a rate ratio. For employee analyses, all models adjusted for total hours worked per week. For manager analyses, all models adjusted for education level. Bolded statistics denote statistically significant change from baseline to 12-month within groups.
For WFC usual practice baseline n = 797; WFC is uses a five-item subscale rated on a scale from 1 (strongly disagree) to 5 (strongly agree) with higher scores indicating higher WFC.
Sleep insufficiency is the single item ‘How often during the past 4 weeks did you get enough sleep to feel rested upon waking up?’ and is rated from 1 (never) to 5 (very often) with lower scores indicating higher levels of sleep insufficiency.
Insomnia symptoms is the single item ‘During the past 4 weeks, how often did you wake up in the middle of the night or early morning?’ with answers ranging from 1 (never) to 4 (three or more times a week) with higher scores indicating higher levels of insomnia symptoms.
Sleep quality is the single item ‘Over the past 4 weeks, how would you rate your sleep quality overall?’ with answers ranging from 1 (very good) to 4 (very bad) with higher scores indicating worse sleep quality.
Moderator Analysis of Intervention effects on actigraphic and self-reported sleep outcomes
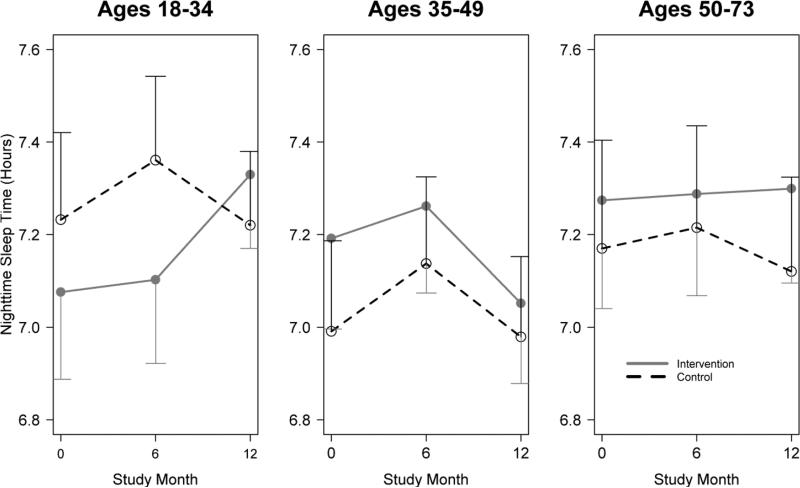
Three-way interactions of time, intervention condition and potential moderators modeled whether heterogeneous intervention effects were observed among subgroups of participants. We observed no significant moderation of the intervention effect by baseline WFC or presence of children in the household. Among employees, a significant age moderation of the intervention effect was observed for nighttime sleep such that nighttime sleep increased as age decreased (p=0.04). Figure 3 plots the adjusted model nighttime sleep profiles across age groups, with points representing the mean and bars representing 95% confidence intervals. Graphically it can be seen that in the 18-34 year old group the intervention results in an increase in nighttime sleep duration in intervention employees by 12 months whereas a decrease in seen in usual practice employees.
Figure 3. Adjusted model nighttime sleep profiles across age groups for employees.
Points represent the mean and bars represent 95% confidence intervals. Test of moderation by age (p=0.040).
Note: Test for moderation was performed using adaptations of the generalized linear mixed models testing intervention effects by including a three-way interaction of age with time and intervention condition. P-value reflects the global test of the three-way interaction regression coefficients.
DISCUSSION
There is a paucity of rigorous research examining linkages between work-family conflict, sleep and work family interventions in extended health care settings with a large group of low income workers. This study employed a randomized controlled design to evaluate effects of a workplace intervention on directly measured sleep outcomes 12 months after baseline in an extended care setting. We also evaluated potential participant-level moderators of intervention effects. Relative to usual practice participants, we observed no statistically significant improvements in actigraphic or self-reported sleep outcomes over the 12-month follow-up. Perhaps, some differences between the STAR intervention and usual practice employees might have hidden the treatment effect. One possible reason may be that the randomization to treatment occurred at the larger facility level, neither at the employee level nor at the employees’ family context level,26 and thus employees in the two conditions might have experienced different nightly sleep contexts that the present study could not capture However, the intervention did exhibit heterogeneous effects on nighttime sleep among employees of particular age categories. Specifically, we found younger employees, those ages 18 to 34, randomized to the intervention arm exhibited increased sleep duration compared to those in the control arm. This suggests that the STAR intervention was especially important for younger participants working in the extended-care setting. This is an important and novel finding as previous research on the family supportive supervisory component of the intervention with low income workers in grocery store settings39 found that work-family demands moderated the effects of the intervention, yet here we are seeing a millennial generation cohort effect that other studies have not documented for other similar work family interventions. There are two more straightforward explanations for the observed null overall effects but stronger effects among younger men and women. First is that low-wage workers must deal with the chronic stress of insufficient earnings and the corollary stressors it spawns, including poor health, effectively suppressing any potentially salutary intervention effects. Second is that the intervention, though effective in white-collar knowledge workforce contexts,18 may be ill-suited for some health-related outcomes in hourly workers in the highly-regulated health care industry. We have demonstrated in this industry a positive effect of this intervention on safety compliance and organizational citizenship.20 These are hands-on jobs, requiring workers’ physical presence, so the workplace intervention aimed to increase work time flexibility may not have been able to help if work time and timing is mostly driven by patients’ needs (not by workers’ discretion). It is difficult to modify time-based encroachments on family obligations or sleep time except for episodic flexibility in switching full shifts or obtaining time off. This stands in contrast with the potential degrees of freedom among knowledge workers who may literally work from almost anywhere at any time with a laptop and cell phone. The intervention may need to be further customized to this very different type of work than ‘desk and computer’ work that can more easily vary by time and place. In the meantime, the finding that the intervention effect was more apparent among younger workers than older workers may suggest that younger workers in the extended-care setting are a more vulnerable group who suffers from sleep deficit, potentially associated with less control over work or more or different demands outside work. Indeed, they exhibited shorter nighttime sleep duration than other age groups at baseline (Figure 3), which might have contributed to their increases in nighttime sleep duration in response to the workplace support. Finally, our test of intervention effects is extremely rigorous in that it follows an intent-to-treat model, was randomized at the nursing home level instead of the participant-level and aims to demonstrate sleep benefits of a workplace-based initiative that did not overtly address sleep outcomes.40 A more effective intervention could have considered an individual-level sleep behavior change to increase sleep duration to healthy levels. Doing so would target short sleepers showing signs of sleep insufficiency, and then offer specific tailored sleep-related behavior change support to enhance effectiveness. Through inspection of the sleep deficiency diagram, it is clear that this day-working population had very low levels of short sleeping compared to other industries or our prior studies.18, 41 If we sought to improve insomnia-like sleep patterns for individual-level yet different cognitive-behavioral type therapy to improve insomnia symptoms. Figure 2 shows that insomnia-like symptoms of WASO are relatively high in this midlife and primarily female sample, and might have been an appropriate intervention target. In contrast, we did not specifically target or provoke individual-level behavior change in this study.
Study Limitations and Future Research
The current study has several limitations. First, regular night workers, those with the greatest work-related reductions in sleep duration and quality, were excluded due to difficulties with facilitators delivering the intervention during night hours, given more limited workplace (and intervention) staffing. Moreover, the distinctive nature of nighttime care work presents a very different context in which to assess the intervention's effectiveness relative to day shift demands in the same facilities. Our previous studies have shown that nursing home workers who regularly work night shifts have significantly reduced sleep duration and significantly increased health risks associated with night shift work.42 Among day shift workers in the current study, only 14% exhibited short sleep duration, thus the potential for improving sleep was likely substantially constrained by the decision to focus exclusively on day shift workers.
Although we incorporated objective markers of sleep using week-long actigraphy data or each wave, WFC and perceived sleep were measured by self-reports, which poses a potential risk for a common-method bias.43 For example, employees who reported higher WFC might have responded negatively to the self-reported sleep questions. Moreover, the global assessments of WFC and self-reported sleep limit our ability to capture how daily fluctuations in these variables are affected by the STAR intervention, and more importantly, how daily WFC moderates the effects of intervention on nightly sleep measured via actigraphy. Second, the sample of this study was purposively selected from an extended-care setting, and thus the findings may not be generalized to shift workers in other work contexts. Future research may need to test whether a workplace intervention can improve sleep in younger age employees (18-34 years) who work in extended care facilities and other industry samples. Third, we tested whether the STAR intervention changed employee sleep at post-intervention follow-ups approximately 12-months after the baseline assessment. Although our general logic model was that the intervention improves employee health through several months of changed workplace practices,24 it may be that sleep is a more proximal outcome and we missed immediate post-intervention effects. For example, employees might have been able to sleep better on nights following intervention sessions where they were working to implement new work practices, but such positive effects may have disappeared several months after the active phase of the intervention. Fourth, we were not able to capture whether actigraphy recordings were during work days or days off which may introduce confounding effects. We know that subjects were at work the day of sleep watch distribution and collection, and generally were at work (i.e., not vacation) but do not have further information on a daily level. Future studies using daily diary and other designs should capture this information. Additionally, future research could assess daily actigraphic sleep data during the process of an intervention to examine day-to-day linkages between intervention participation, daily work-related practices and stressors, and nightly sleep. This study implemented a pure organizational intervention that not discuss sleep or individual health or health behaviors explicitly. Next generation studies might explicitly integrate health messages into the intervention and potentially increase the timing/number of sessions, including individually-directed behavior change strategies, to be more effective.
Despite these limitations, this study advances the literature examining the link between work and sleep. The null main effect of the STAR intervention, which was effective in another context, may indicate inherent challenges in reducing work-family conflict and protecting employee sleep in hourly shift work environments. However, the moderating effect of age, where intervention employees aged 18-34 significantly improved their nighttime sleep as compared to control employees, suggests that future intervention studies may need to take into account employee-level characteristics, to examine for whom and under what circumstances the intervention would be effective to improve sleep. Given that sleep is important not only for employee health but also for organizational outcomes44, 45 workplaces should continue to make efforts to reorganize the structure of work to reduce stress and protect their employees’ sleep, which, in turn, may increase workplace productivity.
CONCLUSION
This study employed a randomized controlled design to evaluate effects of a workplace intervention, intended to improve family-supportive supervision and employee control over work time, on directly measured sleep outcomes 12 months after baseline in an extended care setting. Relative to usual practice participants, we observed no statistically significant improvements in actigraphic or self-reported sleep outcomes over the 12-month follow-up. We did observe significant moderation effects for age suggesting the intervention was more effective in younger employees, which suggests that future interventions should consider age in the context of workplace health interventions in extended care settings.
ACKNOWLEDGEMENTS
The authors wish to thank Jamie Porter, Deirdre McLaren, Chloe Beverly, and Rick Lilienthal for scoring of actigraphy data and Jessica Minnier for her statistical expertise.
SUPPORT
This research was conducted as part of the Work Family Health Network (www.WorkFamilyHealthNetwork.org), which is funded by a cooperative agreement through the National Institute of Health and the Centers for Disease Control and Prevention: Eunice Kennedy Shriver National Institute of Child Health and Human Development (U01HD051217, U01HD051218, U01HD051256, and U01HD051276); National Institute on Aging (U01AG027669); Office of Behavioral and Social Sciences Research and National Institute for Occupational Safety and Health (U01OH008788 and U01HD059773). Grants from the National Heart, Lung and Blood Institute (R01HL107240), William T. Grant Foundation, Alfred P Sloan Foundation, and the Administration for Children and Families have provided additional funding. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of these institutes and offices.
APPENDICES
Appendix Table 1.
Percentage or mean ± SD for demographic characteristics by condition for managers/employees with valid baseline actigraphy data
| Employees (n=1,220) | Managers (n=65) | |||||
|---|---|---|---|---|---|---|
| Usual Practice (n = 568) | Intervention (n = 652) | P-value | Usual Practice (n = 32) | Intervention (n = 33) | P-value | |
| Female | 91.7% | 93.7% | 0.20 | 90.6% | 93.9% | 0.67* |
| Age | 38.9±12.3 | 37.8±12.7 | 0.13 | 45.9±11.9 | 43.2±9.2 | 0.31 |
| Race | 0.11 | 0.67* | ||||
| White | 66.4% | 70.8% | 90.6% | 93.9% | ||
| Black | 12.3% | 13.2% | 0.0% | 0.0% | ||
| Hispanic | 14.6% | 10.2% | 0.0% | 0.0% | ||
| Other | 6.8% | 5.8% | 9.4% | 6.1% | ||
| Married or living with partner | 64.1% | 64.1% | 0.99 | 71.9% | 72.7% | 0.94 |
| No of Children | 1.1±1.2 | 1.0±1.2 | 0.39 | 0.9±1.0 | 1.0±1.1 | 0.73 |
| Elder Care | 28.4% | 31.2% | 0.29 | 21.9% | 33.3% | 0.30 |
| Education | 0.25 | 0.13* | ||||
| Less than High School Graduate | 6.3% | 6.2% | 0.0% | 0.0% | ||
| High School Graduate | 30.5% | 35.6% | 0.0.% | 12.1% | ||
| Some College or technical school | 50.0% | 47.4% | 50.0% | 51.5% | ||
| College graduate | 13.2% | 10.9% | 50.0% | 36.4% | ||
| Hours worked per week | 40.7±10.9 | 39.2±9.4 | 0.01 | 47.2±6.8 | 52.0±13.2 | 0.07 |
| Shift | 0.30 | 0.34* | ||||
| Variable | 4.0% | 4.4% | 15.6% | 21.2% | ||
| Regular daytime | 51.4% | 50.9% | 68.8% | 75.8% | ||
| Regular evening | 33.0% | 34.0% | 9.4% | 0.0% | ||
| Regular night | 2.2% | 0.9% | 0.0% | 0.0% | ||
| Rotating | 6.0% | 5.5% | 0.0% | 0.0% | ||
| Split | 2.5% | 1.9% | 3.1% | 0.0% | ||
| Other | 1.1% | 2.5% | 3.1% | 3.0% | ||
Fisher's exact test used as one or more expected cell counts <5
Note: Descriptives shown for all subjects included in self-reported sleep outcome analysis. For the following patient characteristics, we observed some missing data on the survey items: EMPLOYEES: age (1 missing from intervention group and 1 missing from usual practice), no. of children (1 missing from usual practice), total hours worked per week (2 missing from intervention group and 2 missing from control group). MANAGERS: none missing
Appendix Table 2.
Raw unadjusted means and standard deviations for primary actigraphic outcome measures by intervention condition among employees and managers. Standard deviations presented in parentheses. Change is defined as 12-month outcome minus baseline outcome.
| Employees | Managers | |||
|---|---|---|---|---|
| Outcome Measure | Intervention (baseline n=568) | Usual Practice (baseline n=652) | Intervention (baseline n=33) | Usual Practice (baseline n=32) |
| Total Sleep (mins) | ||||
| Baseline | 459.1 (59.1) | 448.7 (61.0) | 469.1 (58.9) | 461.0 (48.2) |
| 6 months | 457.3 (56.4) | 452.3 (65.3) | 467.9 (56.8) | 457.7 (53.8) |
| 12 months | 455.9 (58.9) | 447.9 (61.8) | 463.8 (63.2) | 476.1 (66.3) |
| Change | −5.9 (60.4) | −1.7 (55.1) | −9.8 (62.5) | 17.5 (60.1) |
| WASO (mins) | ||||
| Baseline | 44.3 (15.9) | 45.2 (17.2) | 43.4 (25.2) | 46.3 (17.5) |
| 6 months | 47.7 (17.5) | 49.0 (20.0) | 47.4 (22.5) | 49.9 (18.4) |
| 12 months | 45.6 (16.1) | 45.3 (16.8) | 45.7 (18.7) | 50.3 (16.8) |
| Change | 2.1 (14.2) | 0.4 (16.4) | −0.2 (18.9) | 5.3 (18.5) |
| Nighttime Sleep (mins) | ||||
| Baseline | 434.4 (61.4) | 424.2 (64.3) | 453.3 (54.2) | 441.6 (49.7) |
| 6 months | 434.5 (59.9) | 431.2 (65.4) | 458.0 (60.7) | 441.4 (48.6) |
| 12 months | 432.0 (61.0) | 426.3 (61.6) | 449.0 (64.0) | 455.1 (71.7) |
| Change | −5.4 (60.1) | 0.9 (58.9) | −8.1 (48.3) | 20.6 (58.7) |
| Nap Time (mins) | ||||
| Baseline | 24.7 (29.0) | 24.5 (31.8) | 15.9 (23.4) | 19.4 (23.1) |
| 6 months | 22.8 (27.7) | 21.1 (29.8) | 9.9 (18.3) | 16.3 (18.9) |
| 12 months | 23.8 (28.7) | 21.6 (27.2) | 14.8 (15.9) | 21.1 (28.4) |
| Change | −0.5 (32.5) | −2.6 (32.6) | −1.6 (22.4) | −3.1 (31.1) |
| Nighttime Sleep SD (mins) | ||||
| Baseline | 88.1 (38.6) | 85.3 (39.3) | 74.6 (31.2) | 66.8 (32.1) |
| 6 months | 88.2 (41.8) | 90.6 (44.0) | 74.6 (38.2) | 62.2 (39.9) |
| 12 months | 86.9 (41.2) | 82.7 (43.9) | 79.4 (40.9) | 81.5 (40.7) |
| Change | 0.2 (47.1) | −0.7 (50.2) | 6.4 (36.8) | 16.6 (46.1) |
| Number of Naps (n) | ||||
| Baseline | 1.9 (2.0) | 1.8 (2.0) | 1.2 (1.7) | 1.5 (1.5) |
| 6 months | 1.7 (1.9) | 1.5 (2.0) | 0.8 (1.0) | 1.3 (1.5) |
| 12 months | 1.8 (1.9) | 1.6 (1.8) | 1.3 (1.4) | 1.6 (2.0) |
| Change | −0.1 (2.1) | −0.2 (2.0) | 0.1 (1.9) | −0.2 (1.5) |
Appendix Table 3.
Raw unadjusted means and standard deviations for secondary self-reported outcome measures by intervention condition among employees and managers. Standard deviations presented in parentheses.
| Employees | Managers | |||
|---|---|---|---|---|
| Intervention (baseline n=723) | Usual Practice (baseline n=799) | Intervention (baseline n=88) | Usual Practice (baseline n=96) | |
| WFC (1-5)* | ||||
| Baseline | 2.8 (0.9) | 2.8 (0.9) | 3.3 (1.0) | 2.8 (0.9) |
| 6 months | 2.8 (0.9) | 2.7 (0.9) | 3.1 (1.1) | 2.8 (0.9) |
| 12 months | 2.7 (0.9) | 2.6 (0.9) | 2.9 (1.0) | 2.7 (0.9) |
| Change | 0.0 (0.8) | −0.1 (0.8) | −0.2 (0.7) | 0.0 (1.0) |
| Sleep Insufficiency (1-5) | ||||
| Baseline | 2.9 (0.9) | 3.0 (1.0) | 3.0 (1.0) | 3.1 (0.9) |
| 6 months | 3.0 (0.9) | 3.0 (1.0) | 3.2 (0.9) | 3.2 (0.9) |
| 12 months | 3.0 (0.9) | 3.0 (1.0) | 3.1 (0.9) | 3.2 (1.0) |
| Change | 0.1 (1.0) | 0.1 (1.0) | 0.0 (1.0) | 0.0 (0.9) |
| Insomnia Symptoms (1-4) | ||||
| Baseline | 3.2 (1.0) | 3.2 (1.0) | 3.4 (0.9) | 3.6 (0.8) |
| 6 months | 3.1 (1.0) | 3.2 (1.0) | 3.3 (1.0) | 3.4 (0.8) |
| 12 months | 3.2 (1.0) | 3.2 (1.0) | 3.4 (1.0) | 3.4 (0.9) |
| Change | 0.0 (1.0) | −0.1 (1.0) | 0.0 (0.7) | −0.1 (0.9) |
| Sleep Quality (1-4) | ||||
| Baseline | 2.3 (0.8) | 2.4 (0.8) | 2.3 (0.7) | 2.3 (0.7) |
| 6 months | 2.2 (0.8) | 2.2 (0.8) | 2.1 (0.7) | 2.2 (0.7) |
| 12 months | 2.2 (0.8) | 2.2 (0.8) | 2.3 (0.7) | 2.2 (0.6) |
| Change | −0.1 (0.8) | −0.1 (0.8) | 0.0 (0.7) | 0.0 (0.7) |
Number of usual practice Employees for WFC at baseline was 797
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURES
Buxton discloses consulting (speaking) at Chevron outside of the present work. All other authors have no conflict of interest or disclosures to report. Oregon Health & Science University has a significant financial interest in NwETA, a company that may have a commercial interest in the results of the research and technology used in the intervention.
REFERENCES
- 1.Luyster FS, Strollo PJ, Jr., Zee PC, Walsh JK. Sleep: a health imperative. Sleep. 2012;35(6):727–34. doi: 10.5665/sleep.1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Short sleep duration among workers -- United States, 2010. Morbidity and Mortality Weekly Report (MMWR) 2012;61(16):281–5. [PubMed] [Google Scholar]
- 3.Watson NF, Badr MS, Belenky G, et al. Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society on the Recommended Amount of Sleep for a Healthy Adult: Methodology and Discussion. Sleep. 2015 doi: 10.5665/sleep.4886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Czeisler CA. Perspective: Casting light on sleep deficiency. Nature. 2013;497(7450):S13. doi: 10.1038/497S13a. [DOI] [PubMed] [Google Scholar]
- 5.Basner M, Fomberstein KM, Razavi FM, et al. American time use survey: Sleep time and its relationship to waking activities. Sleep. 2007;30(9):1085–95. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salo P, Ala-Mursula L, Rod NH, et al. Work time control and sleep disturbances: prospective cohort study of Finnish public sector employees. Sleep. 2014;37(7):1217–25. doi: 10.5665/sleep.3842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnes CM, Wagner DT, Ghumman S. Borrowing from Sleep to Pay Work and Family: Expanding Time-Based Conflict to the Broader Non-Work Domain. Personnel Psychology. 2012 [Google Scholar]
- 8.Greenhaus JH, Beutell NJ. Sources of conflict between work and family roles. Academy of Management Review. 1985;10(1):76–88. [Google Scholar]
- 9.Jansen NW, Kant I, Kristensen TS, Nijhuis FJ. Antecedents and consequences of work-family conflict: a prospective cohort study. Journal of Occupational and Environmental Medicine. 2003;45(5):479–91. doi: 10.1097/01.jom.0000063626.37065.e8. [DOI] [PubMed] [Google Scholar]
- 10.Berkman LF, Liu SY, Hammer L, et al. Work-Family Conflict, Cardiometabolic Risk, and Sleep Duration in Nursing Employees. Journal of Occupational Health Psychology. 2015;20(4):420–33. doi: 10.1037/a0039143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buxton OM, Lee S, Beverly C, et al. Work-family conflict and employee sleep: Evidence from IT workers in the Work, Family and Health Study. Sleep. 2016 doi: 10.5665/sleep.6172. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lallukka T, Ferrie JE, Kivimaki M, et al. Conflicts between work and family life and subsequent sleep problems among employees from Finland, Britain, and Japan. Int. J. Behav. Med. 2014;21(2):310–8. doi: 10.1007/s12529-013-9301-6. [DOI] [PubMed] [Google Scholar]
- 13.Lallukka T, Arber S, Laaksonen M, Lahelma E, Partonen T, Rahkonen O. Work-family conflicts and subsequent sleep medication among women and men: a longitudinal registry linkage study. Soc. Sci. Med. 2013;79:66–75. doi: 10.1016/j.socscimed.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 14.Moen P, Kelly EL, Tranby E, Huang Q. Changing work, changing health: can real work-time flexibility promote health behaviors and well-being? Journal of Health and Social Behavior. 2011;52(4):404–29. doi: 10.1177/0022146511418979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berkman LF, Buxton OM, Ertel K, Okechukwu C. Manager's practices related to work-family balance predict employee cardiovascular risk and sleep duration in extended care settings. Journal of Occupational Health Psychology. 2010;115(3):316–29. doi: 10.1037/a0019721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sorensen G, Stoddard AM, Stoffel S, et al. The role of the work context in multiple wellness outcomes for hospital patient care workers. Journal of Occupational and Environmental Medicine. 2011;53(8):899–910. doi: 10.1097/JOM.0b013e318226a74a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Crain TL, Schonert-Reichl KA, Roeser RW. Cultivating Teacher Mindfulness: Effects of a Randomized Controlled Trial on Work, Home, and Sleep Outcomes. Journal of Occupational Health Psychology. 2016 doi: 10.1037/ocp0000043. [DOI] [PubMed] [Google Scholar]
- 18.Olson R, Crain TL, Bodner TE, et al. A workplace intervention improves sleep: results from the randomized controlled Work, Family, and Health Study. Sleep Health. 2015;1(1):55–65. doi: 10.1016/j.sleh.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brand S, Holsboer-Trachsler E, Naranjo JR, Schmidt S. Influence of mindfulness practice on cortisol and sleep in long-term and short-term meditators. Neuropsychobiology. 2012;65(3):109–18. doi: 10.1159/000330362. [DOI] [PubMed] [Google Scholar]
- 20.Hammer LB, Kossek EE, Anger WK, Bodner T, Zimmerman KL. Clarifying work-family intervention processes: The roles of work-family conflict and family-supportive supervisor behaviors. Journal of Applied Psychology. 2010;96(1):134–50. doi: 10.1037/a0020927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelly EL, Moen P, Oakes M, Fan W. Changing work and work-family conflict in an information technology workplace: evidence from a group-randomized trial. American Sociological Review. 2014;70:485–516. doi: 10.1177/0003122414531435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kelly EL, Moen P, Tranby E. Changing workplaces to reduce work-family conflict: schedule control in a white-collar organization. American Sociological Review. 2011;76(2):265–90. doi: 10.1177/0003122411400056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Karhula K, Harma M, Sallinen M, et al. Job strain, sleep and alertness in shift working health care professionals -- a field study. Industrial Health. 2013;51(4):406–16. doi: 10.2486/indhealth.2013-0015. [DOI] [PubMed] [Google Scholar]
- 24.King RB, Karuntzos GT, Casper LM, et al. Work-family Balance Issues and Work-Leave Policies. In: Gatchel RJ, Schultz IZ, editors. Handbook of Occpational Health and Wellness. Springer; New York: 2013. pp. 323–40. [Google Scholar]
- 25.Ohayon MM, Zulley J, Guilleminault C, Smirne S, Priest RG. How age and daytime activities are related to insomnia in the general population: consequences for older people. Journal of the American Geriatric Society. 2001;49(4):360–6. doi: 10.1046/j.1532-5415.2001.49077.x. [DOI] [PubMed] [Google Scholar]
- 26.Bray JW, Kelly E, Hammer LB, et al. An integrative, multilevel, and transdisciplinary research approach to challenges of work, family, and health. Research Triangle Park, NC: 2013. [Google Scholar]
- 27.Marino MM, Li Y, Rueschman MN, et al. Measuring sleep: Accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013;36(11):1747–55. doi: 10.5665/sleep.3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System Survey Questionnaire. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2013. [Google Scholar]
- 29.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 30.Netemeyer RG, Boles JS, McMurrian R. Development and validation of work-family conflict and family-work conflict scales. Journal of Applied Psychology. 1996;81(4):400–10. [Google Scholar]
- 31.Hammer LB, Johnson RC, Crain TL, et al. Intervention Effects on Safety Compliance and Citizenship Behaviors: Evidence From the Work, Family, and Health Study. Journal of Applied Psychology. 2015;101(2):190–208. doi: 10.1037/apl0000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moen P, Kelly EL, Fan W, et al. Does a Flexibility/Support Organizational Initiative Improve High-Tech Employees’ Well-Being? Evidence from the Work, Family, and Health Network. American Sociological Review. 2016;81(1):134–64. [Google Scholar]
- 33.McHale SM, Lawson KM, Davis KD, Casper L, Kelly EL, Buxton O. Effects of a Workplace Intervention on Sleep in Employees’ Children. Journal of Adolescent Health. 2015;56(6):672–7. doi: 10.1016/j.jadohealth.2015.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kossek EE, Hammer LB, Kelly E, Moen P. Designing work, family & health organizational change initiatives. Organizational Dynamics. 2014;43:53–63. doi: 10.1016/j.orgdyn.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kossek E, Wipfli B, Thompson R, Brockwood K. The Work, Family & Health Network intervention: Core elements and customization for diverse occupational health contexts. Occupational Health and Disparities among Racial and Ethnic Minorities: Formulating Research Needs and Directions. In press. [Google Scholar]
- 36.Hammer LB, Kossek EE, Yrgaui NL, Bodner TE, Hanson GC. Development and validation of a multidimensional measure of family supportive supervisor behaviors (FSSB). Journal of Management. 2009;35(4):837–56. doi: 10.1177/0149206308328510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McCulloch CE, Neuhaus JM. Generalized Linear Mixed Models. Encyclopedia of Biostatistics. 2005 [Google Scholar]
- 38.Lee AH, Wang K, Scott JA, Yau KK, McLachlan GJ. Multi-level zero-inflated Poisson regression modelling of correlated count data with excess zeros. Stat. Methods Med. Res. 2006;15(1):47–61. doi: 10.1191/0962280206sm429oa. [DOI] [PubMed] [Google Scholar]
- 39.Hammer LB, Kossek EE, Anger WK, Bodner T, Zimmerman K. Clarifying work-family intervention process: the roles of work-family conflict and family supportive supervisor behaviors. Journal of Applied Psychology. 2011;96(1):134–50. doi: 10.1037/a0020927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Burg MM, King RB, Stoney CM, Troxel WM. Insights from the OppNet initiatives on psychosocial stress and sleep: themes for multidisciplinary team science research. Sleep Health. 2016;2(1):8–11. doi: 10.1016/j.sleh.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 41.Jackson CL, Redline S, Kawachi I, Williams MA, Hu FB. Racial Disparities in Short Sleep Duration by Occupation and Industry. Am.J Epidemiol. 2013 doi: 10.1093/aje/kwt159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ertel KA, Berkman LF, Buxton OM. Socioeconomic status, occupational characteristics, and sleep duration in African/Caribbean immigrants and US white health care workers. Sleep. 2011;34(4):509–18. doi: 10.1093/sleep/34.4.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. Journal of Applied Psychology. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- 44.Barnes CM, Ghumman S, Scott BA. Sleep and Organizational Citizenship Behavior: The Mediating Role of Job Satisfaction. Journal of Occupational Health Psychology. 2012 doi: 10.1037/a0030349. [DOI] [PubMed] [Google Scholar]
- 45.Buxton OM, Hopcia K, Sembajwe G, et al. Relationship of sleep deficiency to perceived pain and functional limitations in hospital patient care workers. Journal of Occupational and Environmental Medicine. 2012;54(7):851–8. doi: 10.1097/JOM.0b013e31824e6913. [DOI] [PMC free article] [PubMed] [Google Scholar]