Abstract
The link between depression and sexual risk-taking has received mixed findings in the literature. The current study analyzed the links between depression and recent condomless anal sex (CAS) with casual partners among 1033 HIV-negative, non-PrEP-using, gay and bisexual men. When CAS was dichotomized as either none or some, depression was not associated with the odds of CAS (with receptive and insertive combined) or insertive CAS only, but was positively associated with the odds of receptive CAS. When CAS was tallied as a count variable of events, depression was positively associated with total CAS, receptive CAS, and insertive CAS. With the addition of a quadratic term for depression, a positive quadratic effect was only found for total CAS and receptive CAS, but not for insertive CAS. These findings highlight the utility of using count data for CAS events and treating CAS separately with regard to receptive and insertive positioning when considering the role of depression among gay and bisexual men.
Keywords: Condom use, Sexual minority, Men who have sex with men (MSM), Casual sex, Positioning
Abstract
El enlace entre la depresión y el riesgo sexual ha recibido resultados mixtos en la literatura. El presente estudio analizó los vínculos entre la depresión y el sexo anal sin condón reciente (CAS, siglas en Inglés) con parejas ocasionales en 1033 hombres gay y bisexuales VIH-negativo que no utilizaban PrEP. Cuando dicotomizada a algún o ningún episodio de CAS, la depresión no estuvo asociada con la probabilidad de CAS (con receptivo e insertivo combinados) o CAS insertivo solamente, pero sí estuvo asociada positivamente con la probabilidad de CAS receptivo. Cuando el CAS se contabilizó como una variable de recuento de los acontecimientos, la depresión se asoció positivamente con el número total de CAS, con el CAS receptivo, y el CAS insertivo. Con la adición de un término cuadrático para la depresión, un efecto cuadrático positivo sólo se encontró para el CAS total y CAS receptivo, pero no para el CAS insertivo. Estos resultados resaltan la utilidad de usar los datos de recuento de acontecimientos del CAS y de tratar el CAS por separado con respecto a la posición receptiva e insertiva al considerar el rol de la depresión entre hombres gays y bisexuales.
Introduction
Gay and bisexual men continue to experience disproportionately high rates both of HIV infection [1] and depression relative to heterosexuals [2–4], and a number of studies have shown that these two disparities are interconnected [5–7]. However, an earlier meta-analysis by Crepaz and Marks [8] of 27 studies dating from 1990 to 1999 is often cited as evidence of a very weak effect size for depressive symptoms on sexual risk-taking behavior among women and men (overall ES = .04). It should be noted however, that only 16 of the 34 samples included in that meta-analysis focused on men who have sex with men (MSM), and only five of those featured analyses specific to HIV-negative MSM—generating effect sizes of .46 [9], .28 [10], −.03 [11], −.12 [12], and −.17 [13].
The importance of considering the impact of depression on sexual risk-taking behavior specifically in relation to gay and bisexual men is highlighted by research on the dual control model of sexual response [14] which makes a distinction between sexual excitatory processes (e.g., arousal, interest) and sexual inhibitory processes (e.g., suppression, regulation). Although negative mood (including depressive symptomatology) is generally expected to dampen sexual excitation, the model makes room for the possibility that it might also simultaneously impair one’s capacity and/or motivation to inhibit sexual response. Furthermore, research indicates that these two potential effects of negative mood vary according to gender and sexual orientation—negative mood more reliably predicts lowered sexual excitation in women than in men, while it better predicts increased problems with inhibiting sexual excitation in men than in women [15]. Further, depression was associated with greater rates of condomless sex amongst gay men while there was no such association for heterosexual men, and the effects of depression on tallies of sex partners and one-night-stands were stronger for gay men than for heterosexual men [16]. In other words, it is less clear that depression lowers sexual excitation in men, but it is more likely that depression heightens men’s problems with inhibition, and perhaps increases risk-taking even more so among gay and bisexual men. Indeed, a 2014 study of highly sexually-active gay and bisexual men found that a composite score of depression and anxiety was actually associated with increased sexual excitation, as well as with minimized self-efficacy regarding inhibiting sexual thoughts and urges, and stronger beliefs in the perceived necessity of having sex [17]. These distinctions may help explain the null effect of depression on sexual risk-taking found in Crepaz and Marks’ [8] meta-analysis which combined studies across gender and sexual orientation.
In more recent studies focusing solely on gay and bisexual men, depression has been positively associated with the odds of having recent sexual risk in a number of diverse samples, including: Black MSM [18], samples of mostly HIV-negative gay and bisexual men [6, 19], HIV-negative MSM in Belgium [20], HIV-positive MSM [5, 21, 22], and young MSM [23]. It should be noted that, in each of these studies, sexual risk-taking behavior was dichotomized into either having none or having any condomless anal sex (CAS) in a specified period of time, as was also done in Stall et al.’s [7] original application of syndemics theory to sexual risk-taking among MSM.
One possible explanation for variability in findings across studies is the variety of ways in which sexual risk has been operationalized and measured, whether as a dichotomized variable indicating no risk versus any risk, or as a continuous variable in which the count of risk events is summed or used to calculate a proportion score. A count of CAS events was used in Houston, Sandfort, Dolezal, and Carballo-Diéguez’ study [24], and its association with depression was found among HIV-negative MSM, but not among HIV-positive MSM. The number of CAS events as a proportion of one’s total sex events was utilized in Safren et al.’s [25] study of HIV-positive MSM, and was positively linked with greater depression. A more elaborate rating of sexual risk-taking was used in Mustanski’s [26] daily diary study which explored state-level mood or affect among a sample of mostly HIV-negative gay and bisexual men. Day-level behavioral risk was measured as the sum of various sexual behaviors, with each behavior weighted according to riskiness, applicable for each sex event on a given day. Analyses found that, while state-level negative affect did not predict increased sexual risk-taking on a given day, a lack of positive affect (which also characterizes depression) did. In sum, counts of the number or frequency of CAS events may be more informative than a dichotomized variable when considering the role of depression, as it is possible that depression is not as strongly involved for an individual reporting a single CAS event as it might be for an individual reporting multiple or regular CAS events.
There is also evidence to suggest that the strength of the association with depression may differ depending on sexual positioning in the CAS event—whether the individual is the receptive (‘bottom’) or insertive (‘top’) partner. While the majority of studies do not analyze receptive and insertive CAS separately, it is generally acknowledged that receptive CAS represents a greater risk for HIV transmission compared to insertive CAS [27]. When predicting CAS without distinguishing receptive from insertive positioning, Hanson et al. [28] did not detect an effect for depression among HIV-negative MSM—however, when positioning was factored in, they found that depression did predict greater likelihood of receptive CAS but not insertive CAS, highlighting the importance of analyzing these behaviors separately. Focusing on sexual positioning as an identity rather than on counts of behavioral events, Starks et al. [29] found that identifying as a ‘bottom’ was directly associated with heightened internalized homonegativity and anticipated stigma, and was indirectly associated with greater depression. Although Fendrich et al. [19] found links between depression and both receptive and insertive CAS, Poppen et al. [30] found that depression was only associated with insertive CAS, not receptive CAS. While the literature is mixed, the consideration of CAS in terms of whether it is receptive or insertive, as advocated by Jin et al. [31], may be informative in understanding associations with depression.
An additional factor which may contribute to variability in the literature is that some component of the association between depression and sexual risk behavior may be indirect and/or non-linear—for example, Alvy et al. [32] provided evidence of psychosocial mediators such as self-efficacy and cognitive closure. Klein [33] found that depression, while not related to actual sexual risk behaviors among gay and bisexual men, was associated with condom use beliefs which were, in turn, related to sexual risk behavior. Perdue et al. [34] found that depression was linked with increased number of partners among MSM but not with increased sexual risk-taking with those partners. Further, a number of studies have found evidence of a quadratic effect for depression on sex risk among HIV-negative MSM [35], among HIV-positive MSM [36], and among a sample of mostly HIV-negative MSM in Taiwan [37]. In each of these studies, the quadratic effect was negative, such that likelihood of sex risk (dichotomized) was lower at the lowest and highest levels of depression, and higher at moderate levels of depression. Similarly, risk was found to be highest among MSM with moderate depression (i.e., dysthymic disorder without major depression) compared to those with no depression or major depression [38]. That sex risk might decline at severely high levels of depression was also found in a study of young MSM, among whom major depressive disorder was associated with reduced sexual risk-taking [39].
The purpose of the current study was to illustrate how variability in the operationalization of sexual risk behavior and the incorporation of quadratic effects into regression models may influence conclusions about the depression-CAS link. Accordingly, the current study aimed to clarify the link between depression and CAS by focusing on CAS: (i) with casual partners only; (ii) treated separately as total CAS, receptive CAS, and insertive CAS; (iii) among HIV-negative gay and bisexual men only, and; (iv) with the inclusion of a quadratic term for depression. The study analyzed the three CAS outcomes separately as both dichotomized variables (i.e., none vs. some CAS with casual partners in the past 90 days) and as count variables (i.e., the sum of events with casual partners in the past 90 days). The study also considered whether depression was associated with total number of casual male partners in the past 90 days. It was hypothesized that a positive linear association would be found between depression and all three CAS outcomes both when dichotomized and treated as count variables. In line with previous studies, it was also hypothesized that a significant and negative quadratic association would be found with depression. No hypotheses were advanced for whether depression would be associated with number of recent casual male partners.
Methods
Participants
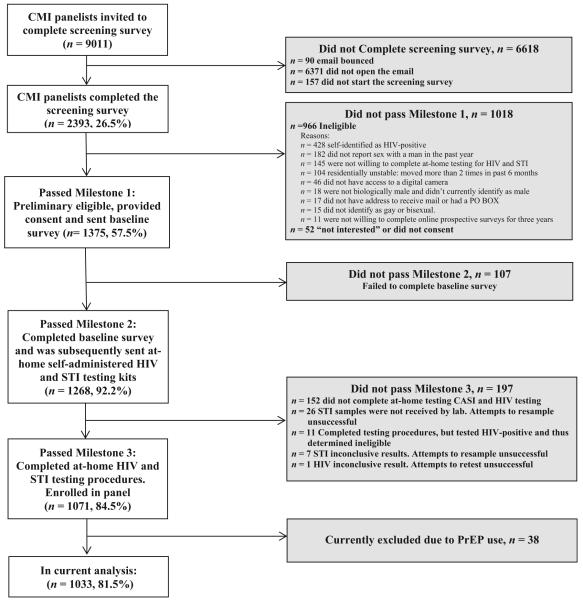
Cross-sectional data were drawn from the first wave of the One Thousand Strong panel—a longitudinal study following a national U.S. sample of gay and bisexual men over 3 years. Potential participants were identified via Community Marketing and Insight’s (CMI) panel of over 22,000 gay and bisexual men throughout the U.S. To reflect population densities across regions, 9011 men were invited to complete a 2-min screening survey and were deemed eligible if they: were at least 18 years of age; were biologically male and currently identified as male and as gay or bisexual; self-reported an HIV-negative status; and were able to complete online surveys in English and at-home self-administered testing for HIV, chlamydia, and gonorrhea. Participants also needed to report having sex with a man within the past 5 years, to have an address to receive mail that was not a P.O. Box, and to have not moved more than twice in the past 6 months (i.e., residential stability). Of the 2393 (26.5 %) who completed the screening survey, 1375 men (57.5 %) met study eligibility criteria and provided consent, were asked to complete additional items, and were compensated with a $10 Amazon gift card. Figure 1 displays these enrollment details, which are described elsewhere [40].
Fig. 1.
Enrollment of the One Thousand Strong panel
In total, 1071 men (84.5 %) were included in the final cohort and completed the first full online survey (via a unique link to a Qualtrics survey), receiving one $25 Amazon gift card for survey completion and another for completion of HIV/STI testing. For the present study however, 38 men who reported having been prescribed pre-exposure prophylaxis (PrEP) were excluded from analyses, resulting in a final analytic sample of 1033 HIV-negative gay and bisexual men who were not on PrEP. All study protocols were approved by CUNY IRB.
Measures
Demographics
Participants reported their date of birth, race/ethnicity, zip code, annual income, level of education, sexual orientation (whether gay or bisexual), and relationship status (whether partnered or single).
Depression
The Center for Epidemiological Studies Depression Scale (CESD) [41] consists of 20 items asking participants to rate how often they have experienced symptoms of depression (such as “I did not feel like eating,” “I felt that everything I did was an effort,” and “My sleep was restless”). Response options range from 0 (rarely or none of the time) to 3 (most or all of the time). Typically, individuals are asked about the presence of symptoms within the past week, and studies have specified a cutoff of 16 or greater as being indicative of clinically meaningful depression [42]. However, to align with the period of sexual activity reported in the current study (i.e., past 90 days), the CESD was adapted to ask participants: “How often have you felt this way in the last 3 months?”, with response options omitting the specification of how many days. Accordingly, comparisons with established clinical cut-offs could not be conducted in the current study, in which the scale showed strong internal consistency, α = .93.
Recent Casual Sexual Activity
Participants reported the number of male casual sex partners during the past 90 days, and the total number of anal sex events (whether receptive or insertive, and whether or not condoms were used) with casual partners in the past 90 days. Total CAS, receptive CAS, and insertive CAS with casual partners in the past 90 days were each analyzed both as a dichotomized ‘none versus some’ variable (with 0 = no CAS events, and 1 = one or more CAS events), and as a count variable.
Analytic Plan
Demographic comparisons of depression scores were conducted using ANOVAs (for race/ethnicity, income, education, and region), independent t tests (for relationship status and sexual orientation), and Pearson’s bivariate correlation (for age). Inclusion of education, but not income, as a covariate in the following analyses was decided due to redundancy in the models. Subsequently, the three CAS outcomes—total CAS, receptive CAS, and insertive CAS—were each analyzed separately as: (i) dichotomized variables in binary logistic regressions (reported in Table 2), and (ii) count variables in negative binomial regressions with maximum likelihood estimation of the dispersion parameter (reported in Table 3). Both depression and the quadratic term for depression were entered alongside the relevant control variables: age, race/ethnicity (reference group = White), education (reference group = graduate school), and relationship status (reference group = partnered). Additionally, a negative binomial regression, also controlling for the covariates listed above, tested whether depression (and quadratic depression) was associated with total number of casual male partners in the past 90 days (whether with or without condoms). All analyses utilized IBM SPSS Version 22.
Table 2.
Regression results for CAS (dichotomized) with casual partners
| Without quadratic term |
With quadratic term |
|||||||
|---|---|---|---|---|---|---|---|---|
| b | Exp(β) | p | 95 % CI for Exp(β) | b | Exp(β) | p | 95 % CI for Exp(β) | |
| Any CAS | ||||||||
| Constant | −.78 | .46 | <.001 | −.93 | .40 | <.001 | ||
| Age | .00 | 1.00 | .81 | .99, 1.01 | .00 | 1.00 | .77 | .99, 1.01 |
| Race/ethnicity (ref. White) | .08 | 1.08 | .63 | .79, 1.47 | .07 | 1.07 | .67 | .78, 1.46 |
| Education (ref. Grad school) | .05 | 1.05 | .77 | .76, 1.44 | .04 | 1.04 | .80 | .76, 1.43 |
| Relationship (ref. partnered) | 1.21 | 3.35 | <.001 | 2.52, 4.45 | 1.22 | 3.38 | <.001 | 2.54, 4.49 |
| Depression | .19 | 1.21 | .11 | .96, 1.54 | −.14 | .87 | .73 | .40, 1.90 |
| Depression quadratic | .16 | 1.17 | .38 | .83, 1.66 | ||||
| Any receptive CAS | ||||||||
| Constant | −1.47 | .23 | <.001 | −1.51 | .22 | <.001 | ||
| Age | −.01 | .99 | .28 | .98, 1.01 | −.01 | .99 | .28 | .98, 1.01 |
| Race/ethnicity (ref. White) | −.19 | .83 | .33 | .57, 1.21 | −.19 | .83 | .32 | .56, 1.21 |
| Education (ref. Grad school) | .02 | 1.02 | .93 | .69, 1.51 | .02 | 1.02 | .94 | .69, 1.51 |
| Relationship (ref. partnered) | 1.33 | 3.76 | <.001 | 2.60, 5.45 | 1.33 | 3.77 | <.001 | 2.60, 5.46 |
| Depression | .36 | 1.43 | <.01 | 1.08, 1.90 | .28 | 1.32 | .57 | .51, 3.45 |
| Depression quadratic | .04 | 1.04 | .87 | .69, 1.57 | ||||
| Any insertive CAS | ||||||||
| Constant | −1.29 | .28 | <.001 | −1.45 | .23 | <.001 | ||
| Age | .00 | 1.00 | .69 | .99, 1.01 | .00 | 1.00 | .74 | .99, 1.01 |
| Race/ethnicity (ref. White) | .27 | 1.31 | .11 | .94, 1.82 | .26 | 1.30 | .12 | .93, 1.80 |
| Education (ref. Grad school) | .08 | 1.09 | .64 | .77, 1.52 | .08 | 1.08 | .67 | .77, 1.52 |
| Relationship (ref. partnered) | .98 | 2.66 | <.001 | 1.95, 3.61 | .99 | 2.68 | <.001 | 1.97, 3.64 |
| Depression | .16 | 1.17 | .24 | .90, 1.51 | −.21 | .81 | .62 | .35, 1.86 |
| Depression quadratic | .17 | 1.19 | .36 | .82, 1.71 | ||||
Table 3.
Regression results for CAS events (count) with casual partners
| Without quadratic term |
With quadratic term |
|||||||
|---|---|---|---|---|---|---|---|---|
| b | Exp(β) | p | 95 % CI for Exp(β) | b | Exp(β) | p | 95 % CI for Exp(β) | |
| Total CAS events | ||||||||
| Constant | .37 | 1.44 | .03 | .11 | 1.12 | .55 | ||
| Age | .00 | 1.00 | .58 | .99, 1.00 | .00 | 1.00 | .38 | .99, 1.00 |
| Race/ethnicity (ref. White) | −.14 | .87 | .13 | .73, 1.04 | −.14 | .87 | .11 | .73, 1.03 |
| Education (ref. Grad school) | −.27 | .77 | <.01 | .64, .92 | −.26 | .77 | <.01 | .64, .92 |
| Relationship (ref. partnered) | .87 | 2.38 | <.001 | 2.03, 2.79 | .87 | 2.40 | <.001 | 2.04, 2.81 |
| Depression | 34 | 1.40 | <.001 | 1.23, 1.60 | −.25 | .78 | .28 | .49, 1.22 |
| Depression quadratic | .28 | 1.32 | <.01 | 1.08, 1.63 | ||||
| Receptive CAS events | ||||||||
| Constant | −.30 | .75 | .17 | −.69 | .50 | <.01 | ||
| Age | −.02 | .98 | <.001 | .98, .99 | −.02 | .98 | <.001 | .97, .99 |
| Race/ethnicity (ref. White) | −.60 | .56 | <.001 | .43, .70 | −.65 | .53 | <.001 | .41, .68 |
| Education (ref. Grad school) | −.01 | .99 | .95 | .77, 1.27 | .01 | 1.01 | .96 | .78, 1.29 |
| Relationship (ref. partnered) | .89 | 2.43 | <.001 | 1.96, 3.02 | .90 | 2.46 | <.001 | 1.98, 3.06 |
| Depression | .68 | 1.97 | <.001 | 1.67, 2.32 | −.42 | .66 | .18 | .36, 1.22 |
| Depression quadratic | .49 | 1.63 | <.001 | 1.25, 2.12 | ||||
| Insertive CAS events | ||||||||
| Constant | −.34 | .71 | .06 | −.42 | .66 | .05 | ||
| Age | .01 | 1.01 | .08 | 1.00, 1.01 | .01 | 1.01 | .09 | 1.00, 1.01 |
| Race/ethnicity (ref. White) | .05 | 1.05 | .61 | .87, 1.27 | .05 | 1.05 | .63 | .87, 1.27 |
| Education (ref. Grad school) | −.44 | .65 | <.001 | .54, .78 | −.43 | .65 | <.001 | .54, .78 |
| Relationship (ref. partnered) | .88 | 2.41 | <.001 | 2.02, 2.87 | .88 | 2.41 | <.001 | 2.02, 2.88 |
| Depression | .17 | 1.19 | .02 | 1.02, 1.38 | −.01 | .99 | .98 | .61, 1.61 |
| Depression quadratic | .09 | 1.09 | .44 | .87, 1.36 | ||||
Results
The final sample of 1033 men was mostly White (71.7 %), and self-identified as gay (94.8 %). Over 55 % had at least a Bachelor degree, and 45.9 % earned $50,000 or more annually. Ages ranged from 18 to 79 years, with a mean of 40.5 years (SD = 13.9). Further demographic details are displayed in Table 1, along with comparisons of depression scores. The average score on the CESD was 16.3 (SD = 11.5) and, on average, depression was significantly higher among younger men, those with less than graduate school-level education and lower income, and those who reported being single. Of the 1,033 men, 331 reported at least one CAS event with a casual male partner in the past 90 days (range 1–60). Some CAS was reported by 44.7 % of the 526 single men and by 18.9 % of the 507 partnered men.
Table 1.
Demographics and depression comparisons
| Total N = 1033 |
Depression CESD |
Test statistic |
||||
|---|---|---|---|---|---|---|
| n | % | M | SD | p | ||
| Race/ethnicity | ||||||
| Black | 78 | 7.6 | 16.2 | 12.2 | F (3, 1029) = 1.91 | .13 |
| Latino | 129 | 12.5 | 17.0 | 12.5 | ||
| White | 741 | 71.7 | 15.9 | 11.1 | ||
| Multiracial/other | 85 | 8.2 | 18.9 | 12.6 | ||
| Education | ||||||
| High School or less | 77 | 7.5 | 19.1a | 11.2 | F (3, 1029) = 7.73 | <.001 |
| Some College | 381 | 36.9 | 17.5a | 12.4 | ||
| Bachelor Degree | 302 | 29.2 | 16.5a | 10.6 | ||
| Graduate School | 273 | 26.4 | 13.7b | 10.9 | ||
| Income | ||||||
| <20 K | 203 | 19.7 | 21.2a | 12.2 | F (2, 1030) = 40.77 | <.001 |
| 20–49 K | 356 | 34.5 | 17.7b | 12.1 | ||
| 50 K or more | 474 | 45.9 | 13.2c | 9.8 | ||
| Sexual orientation | ||||||
| Gay | 979 | 94.8 | 16.4 | 11.7 | t (1031) = .35 | 73 |
| Bisexual | 54 | 5.2 | 15.8 | 9.2 | ||
| Relationship status | ||||||
| Single | 197 | 19.1 | 18.0 | 11.7 | t (1031) = 4.65 | <.001 |
| Partnered | 188 | 18.2 | 14.6 | 11.1 | ||
| Current region in the U.S. | ||||||
| Northeast | 197 | 19.1 | 15.5 | 10.4 | F (3, 1029) = .47 | .76 |
| Midwest | 188 | 18.2 | 15.9 | 11.1 | ||
| South | 366 | 35.4 | 16.7 | 12.1 | ||
| West | 281 | 27.2 | 16.7 | 11.8 | ||
|
| ||||||
| M | SD | r | p | |||
|
| ||||||
| Age (years) | 40.5 | 13.9 | −.17 | <.001 | ||
Superscripts denote significant differences in post hoc comparisons, p <.05
CAS with Casual Partners as a Dichotomous Variable
As displayed in Table 2, logistic regression analyses found that, controlling for age, race/ethnicity, education, and relationship status, depression was not associated with the likelihood of having had CAS with casual partners in the past 90 days, when treated as any CAS (whether receptive or insertive). However, when treated as separate outcomes, depression was positively associated with increased likelihood of having had receptive CAS—b = .36, AOR = 1.43, p < .01, 95 % CI 1.08, 1.90—but not insertive CAS. The addition of the quadratic term for depression showed no significant findings with respect to any of the three dichotomized CAS outcomes.
CAS with Casual Partners as a Count Variable
As displayed in Table 3, negative binomial regression analyses found that, controlling for age, race/ethnicity, education, and relationship status, depression was positively associated with the number of CAS events with casual partners in the past 90 days, when treated as a count variable with receptive or insertive CAS combined—b = .34, Exp(B) = 1.40, p < .001, 95 % CI 1.23, 1.60. When treated as separate outcomes, depression was positively associated with both the number of receptive CAS events—b = .68, Exp(B) = 1.97, p < .001, 95 % CI 1.67, 2.32—and number of insertive CAS events—b = .17, Exp(B) = 1.19, p = .02, 95 % CI 1.02, 1.38.
The addition of the quadratic term for depression showed a positive quadratic association with total CAS events and receptive CAS events—b = .28, Exp(B) = 1.32, p < .01, 95 % CI 1.08, 1.63, and b = .49, Exp(B) = 1.63, p < .001, 95 % CI 1.25, 2.12, respectively—but not with insertive CAS events. In other words, the strength of the association between depression and number of events increased with depression scores.
Finally, there was no linear or quadratic effect for depression on participants’ number of recent casual male partners, b = .01, Exp(B) = 1.01, p = .84, 95 % CI .89, 1.15, and b = .00, Exp(B) = 1.00, p = .99, 95 % CI .83, 1.21, respectively. This indicates that depression is not associated with a greater number of casual male partners overall.
Discussion
The various findings of the current study highlight the importance of considering how the outcome of CAS with casual partners among HIV-negative gay and bisexual men is operationalized when investigating associations with depression. These considerations include: (1) whether to treat CAS as a dichotomous (none vs. some) variable or as a count variable; (2) whether to combine all CAS together or treat separately with regard to receptive versus insertive positioning, and; (3) whether to look for a linear or quadratic effect of depression. When dichotomized as having none versus any CAS, depression was not associated with increased odds of having any CAS—but, when treated as a count variable that tallied the number of CAS events, depression was found to be positively associated with a greater number of events, and furthermore there was a positive quadratic effect for depression. Importantly, depression was not associated with total number of recent casual partners (whether involving condoms or not)—in other words, depression was not associated with having a greater or lesser number of recent casual partners, but was associated with the frequency of CAS with those casual partners.
When dichotomized CAS was operationalized without regard for positioning, no effect for depression was detected—however, when CAS was separated, depression was found to predict the odds of receptive CAS, but not insertive CAS. When CAS events were tallied without regard for positioning, depression was positively associated with total number of events—however, subsequent analyses showed that the strength of this association was greater for receptive CAS events than for insertive CAS events, the latter of which became non-significant with the addition of a quadratic term for depression.
Taken together, these findings suggest that important information is obscured and goes undetected when CAS is dichotomized instead of tallied as a count variable, and/or when receptive and insertive CAS is combined into a single CAS variable. This may in part explain why some previous studies have not found effects for depression on CAS. The finding that depression appears more strongly involved in the prediction of receptive CAS is of great importance given the increased risk of HIV transmission posed by being the receptive partner in CAS [27].
These findings contradict the null finding in Crepaz and Marks’ [8] meta-analysis of 27 studies dating from 1990 to 1999, which included studies of both men and women of a range of sexual orientations. In these studies, sexual risk-taking may have included both vaginal and anal sex, and in the five studies that focused specifically on HIV-negative gay and bisexual men, CAS was treated as a dichotomous (none vs. some) variable. The current findings are, however, in line with numerous studies published since 2001 which, focusing on gay and bisexual men, have shown a positive association between depression and CAS [5, 6, 19, 20].
The findings also accord with research on the dual control model [14, 43], which found that depression did not reduce sexual excitation in gay and bisexual men as had been observed in other populations, but may simultaneously impair the capacity to inhibit sexual response. In qualitative interviews [44] with a sample of mostly HIV-negative gay and bisexual men, depression was associated with increased sexual interest, often prompting the seeking of sexual contact as a source of mood repair and validation. Some men also reported increased risk-taking in sexual situations when depressed due to a reduced concern about adverse consequences. In a study of highly sexually-active gay and bisexual men, depression was associated with increased sexual excitation, minimized self-efficacy in resisting sexual thoughts and urges, and a strengthened belief in the necessity of having sex [17]. Further, greater depression is consistently observed among sexually compulsive gay and bisexual men, among whom the sense of feeling out-of-control and powerless in the face of sexual fantasies, urges, and behaviors is commonly reported [45–48].
The finding of a positive quadratic association between depression and total number of casual CAS events, indicates that CAS increased more steeply at higher levels of depression in the current sample. This finding appears counter to previous studies’ findings of an inverted U-shape effect such that the likelihood of risk was highest at moderate levels of depression, while decreasing at severe levels of depression [35–37]. This may be due to differences in how CAS was defined across studies. While our sex risk outcome was CAS with casual partners, O’Cleirigh et al.’s [36] study included only CAS with serodiscordant main or casual partners, and both Koblin at el. [35] and Shiu et al. [37] included any CAS whether with main or casual partners. Differences in sample characteristics and study purpose may also be involved—although ours was a national sample of HIV-negative gay and bisexual men participating in an online survey, the Koblin et al. [35] study excluded men who were in monogamous relationships, the O’Cleirigh et al. [36] study focused on HIV-positive gay and bisexual men in a risk-reduction intervention program, and the Shui et al. [37] study recruited men in-person who were visiting a community health center. It is possible that our sample did not contain enough people at severely high levels of depression to detect the reduction in risk that has been observed elsewhere. It may also be that our study’s modification of the CESD’s timeframe from the past 7 days to cover the past 3 months may have obscured patterns among those experiencing high levels of recent or current depression. A further possibility is that the link between depression and CAS operates differently in gay and bisexual men depending on their HIV status because CAS generally represents a greater health risk for HIV-negative men than for HIV-positive men, and may thus hold a range of different meanings. Further, a HIV-positive man struggling with depressive symptoms may experience sex with casual partners as a reminder of his HIV status [22], and this may dissuade him from engaging in casual sex with the same frequency as a depressed HIV-negative man. These numerous possibilities should be explored in future research.
The current findings suggest that, while depression may not be a reliable predictor of the mere presence or absence of recent sexual risk (which in many cases may be referring to a single CAS event), it can be more reliably expected to predict higher tallies of risk events, indicating repeated or regular risk-taking, both among single and partnered gay and bisexual men. It is noteworthy that depression did not have an impact on participants’ numbers of recent casual partners—in other words, depression was not associated with greater or lesser numbers of casual partners, but was associated with decreased condom use with those partners.
Although the current study provided evidence of a strong link between depression and CAS in gay and bisexual men, future research should seek to explore specific mechanisms by which depression may be impacting an individual’s likelihood of sexual risk-taking. Depression is often linked with a variety of factors or features which may be involved in impaired self-regulation such as emotion dysregulation, impulsivity, and reduced self-efficacy [17], external locus of control [49], and as mentioned above, sexual compulsivity [45, 47, 48]. Accordingly, it may be that depression, in part, impels people to seek out sources of positive affect and distraction [46], while also depleting their capacity for self-regulation in the face of sexual risk. It may also be that the experience of depression involves dramatic fluctuations in self-esteem, and that this self-esteem instability predicts increased sexual risk-taking among gay and bisexual men [50]. Longitudinal research should also consider whether an individual’s previous experiences of CAS may be contributing to the low self-regard that is common in the experience of depression.
The strengths of our study should be considered in light of the following limitations. Data for our study were cross-sectional, thus causality cannot be inferred. In terms of our sample’s representativeness of the wider gay and bisexual male population, due to the eligibility criteria for the study, ours consisted solely of HIV-negative, non-PrEP-using gay and bisexual men. Recruitment parameters were set based on U.S. Census estimates of the distribution of same-sex couples across the country. The Census does not however collect data on sexual identity—thus there are no estimates available as to the distribution of single/divorced/widowed gay and bisexual men across the U.S. The participants were all voluntarily participating in regular online survey research, had at-home Internet access, and were residentially stable, and the relatively high levels of income and education in the current sample may further limit generalizability. Further, the current study focused on sexual risk-taking with casual partners—future research should also consider the impact of depression on sexual risk-taking among HIV-positive men and between main partners, as well as other forms of sexual risk-taking and risk reduction practices (e.g., seropositioning, PrEP use).
Conclusions
In closing, the current study contributes to a growing body of recent studies showing evidence of a link between depression and increased sexual risk-taking among gay and bisexual men, and does so by focusing on HIV-negative men and CAS with casual partners. The findings provide support for the utility of measuring CAS as a count variable in which number of risk events are summed, rather than as a dichotomized variable indicating any CAS versus no CAS, and for delineating between receptive and insertive CAS. The study’s findings of a positive quadratic association, such that CAS risk was highest at higher levels of depression, highlight the need for HIV prevention efforts to address depressive symptomatology, with the aim of improving mental health and sexual health among gay and bisexual men.
Acknowledgments
The authors would like to acknowledge the contributions of the other members of the One Thousand Strong Study Team (Dr. Ana Ventuneac, Dr. Jonathan Rendina, Demetria Cain, Mark Pawson, Michael Castro, Ruben Jimenez, Chloe Mirzayi, Raymond Moody, Thomas Whitfield, and Jonathan Lassiter) and other staff from the Center for HIV/AIDS Educational Studies and Training (Chris Hietikko, Andrew Cortopassi, Brian Salfas, Doug Keeler, Chris Murphy, and Carlos Ponton). We would also like to thank the staff at Community Marketing and Insights Inc (David Paisley, Heather Torch, and Thomas Roth) as well as Patrick Sullivan, Jessica Ingersoll, Deborah Abdul-Ali, and Doris Igwe at the Emory Center for AIDS Research (P30 AI050409). Finally, we thank Jeffrey Schulden at NIDA and all of our participants in the One Thousand Strong study.
Funding The One Thousand Strong study was funded by a research grant from the National Institute on Drug Abuse (R01 DA036466: Jeffrey T. Parsons & Christian Grov, MPIs). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
Informed Consent Informed consent was obtained from all individual participants included in the study.
Compliance with Ethical Standards
Research Involving Human and Animal Rights All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.CDC [Accessed 1 Nov 2015];HIV Surveillance Report. 2013 25 http://www.cdc.gov/hiv/library/reports/surveillance/ [Google Scholar]
- 2.King M, Semlyen J, Tai SS, et al. A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry. 2008;8(1):70–86. doi: 10.1186/1471-244X-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewis NM. Mental health in sexual minorities: Recent indicators, trends, and their relationships to place in North America and Europe. Health Place. 2009;15(4):1029–45. doi: 10.1016/j.healthplace.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 4.Marshal MP, Dietz LJ, Friedman MS, et al. Suicidality and depression disparities between sexual minority and heterosexual youth: a meta-analytic review. J Adolescent Health. 2011;49(2):115–23. doi: 10.1016/j.jadohealth.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parsons JT, Halkitis PN, Wolitski RJ, Gomez CA. Correlates of sexual risk behaviors among HIV-positive men who have sex with men. AIDS Educ Prev. 2003;15:383–400. doi: 10.1521/aeap.15.6.383.24043. [DOI] [PubMed] [Google Scholar]
- 6.Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occuring psychological health problems, and HIV risk among gay and bisexual men: further evidence of a syndemic. Am J Public Health. 2012;102(1):156–62. doi: 10.2105/AJPH.2011.300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stall R, Mills TC, Williamson J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93(6):939–42. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychol. 2001;20(4):291–9. doi: 10.1037//0278-6133.20.4.291. [DOI] [PubMed] [Google Scholar]
- 9.Perkins DO, Leserman J, Murphy C, Evans DL. Psychosocial predictors of high-risk sexual behavior among HIV-negative homosexual men. AIDS Educ Prev. 1993;5(2):141–52. [PubMed] [Google Scholar]
- 10.Strathdee SA, Hogg RS, et al. Determinants of sexual risk-taking among young HIV-negative gay and bisexual men. JAIDS. 1998;19(1):61–6. doi: 10.1097/00042560-199809010-00010. [DOI] [PubMed] [Google Scholar]
- 11.Dilley JW, McFarland W, Sullivan P, Discepola M. Psychosocial correlates of unprotected anal sex in a cohort or gay men attending an HIV-negative support group. AIDS Educ Prev. 1998;10(4):317–26. [PubMed] [Google Scholar]
- 12.de Vroome EM, de Wit JB, Stroebe W, Sandfort TG, van Griensven GJ. Sexual behavior and depression among HIV-positive gay men. AIDS Behav. 1998;2(2):137–49. [Google Scholar]
- 13.Mayne TJ, Acree M, Chesney MA, Folkman S. HIV sexual risk behavior following bereavement in gay men. Health Psychol. 1998;17(5):403–11. doi: 10.1037//0278-6133.17.5.403. [DOI] [PubMed] [Google Scholar]
- 14.Bancroft J, Janssen E. The dual control model of male sexual response: a theoretical approach to centrally mediated erectile dysfunction. Neurosci Biobehav R. 2000;24(5):571–9. doi: 10.1016/s0149-7634(00)00024-5. [DOI] [PubMed] [Google Scholar]
- 15.Lykins AD, Janssen E, Graham CA. The relationship between negative mood and sexuality in heterosexual college women and men. J Sex Res. 2006;43(2):136–43. doi: 10.1080/00224490609552308. [DOI] [PubMed] [Google Scholar]
- 16.Bancroft J, Janssen E, Carnes L, Goodrich D, Strong D, Long JS. Sexual activity and risk taking in young heterosexual men: the relevance of sexual arousability, mood, and sensation seeking. J Sex Res. 2004;41(2):181–92. doi: 10.1080/00224490409552226. [DOI] [PubMed] [Google Scholar]
- 17.Pachankis JE, Rendina HJ, Ventuneac A, Grov C, Parsons JT. The role of maladaptive cognitions in hypersexuality among highly sexually active gay and bisexual men. Arch Sex Behav. 2014;43(4):669–83. doi: 10.1007/s10508-014-0261-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reisner SL, Mimiaga MJ, Skeer M, et al. Clinically significant depressive symptoms as a risk factor for HIV infection among Black MSM in Massachusetts. AIDS Behav. 2009;13(4):798–810. doi: 10.1007/s10461-009-9571-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fendrich M, Avci O, Johnson TP, Mackesy-Amiti ME. Depression, substance use and HIV risk in a probability sample of men who have sex with men. Addict Behav. 2013;38(3):1715–8. doi: 10.1016/j.addbeh.2012.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wim VB, Christiana N, Marie L. Syndemic and other risk factors for unprotected anal intercourse among an online sample of Belgian HIV-negative men who have sex with men. AIDS Behav. 2014;18(1):50–8. doi: 10.1007/s10461-013-0516-y. [DOI] [PubMed] [Google Scholar]
- 21.Cook SH, Valera P, Wilson PA. Interventions ATNfHA. HIV status disclosure, depressive symptoms, and sexual risk behavior among HIV-positive young men who have sex with men. J Behav Med. 2015;38(3):507–17. doi: 10.1007/s10865-015-9624-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson PA, Stadler G, Boone MR, Bolger N. Fluctuations in depression and well-being are associated with sexual risk episodes among HIV-positive men. Health Psychol. 2014;33(7):681–6. doi: 10.1037/a0035405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mustanski B, Garofalo R, Herrick A, Donenberg G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Ann Behav Med. 2007;34(1):37–45. doi: 10.1080/08836610701495268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Houston E, Sandfort T, Dolezal C, Carballo-Diéguez A. Depressive symptoms among MSM who engage in bareback sex: does mood matter? AIDS Behav. 2012;16(8):2209–15. doi: 10.1007/s10461-012-0156-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Safren SA, Traeger L, Skeer MR, et al. Testing a social-cognitive model of HIV transmission risk behaviors in HIV-infected MSM with and without depression. Health Psychol. 2010;29(2):215–21. doi: 10.1037/a0017859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mustanski BS. The influence of state and trait affect on HIV risk behaviors: a daily diary study of MSM. Health Psychol. 2007;26(5):618–26. doi: 10.1037/0278-6133.26.5.618. [DOI] [PubMed] [Google Scholar]
- 27.CDC [Accessed 1 May 2016];HIV transmission risk. 2012 http://www.cdc.gov/hiv/law/pdf/Hivtranmsmision.pdf.
- 28.Hanson KE, Mansergh G, Koblin BA, Flores SA, Hudson SM, Myers L, Colfax GN. Depressive symptoms by HIV serostatus are differentially associated with unprotected receptive and insertive anal sex among substance-using men who have sex with men in the United States. JAIDS. 2015;68(1):e13–6. doi: 10.1097/QAI.0000000000000396. [DOI] [PubMed] [Google Scholar]
- 29.Starks TJ, Rendina HJ, Breslow AS, Parsons JT, Golub SA. The psychological cost of anticipating HIV stigma for HIV-negative gay and bisexual men. AIDS Behav. 2013;17(8):2732–41. doi: 10.1007/s10461-013-0425-0. [DOI] [PubMed] [Google Scholar]
- 30.Poppen PJ, Reisen CA, Zea MC, Bianchi FT, Echeverry JJ. Predictors of unprotected anal intercourse among HIV-positive Latino gay and bisexual men. AIDS Behav. 2004;8(4):379–89. doi: 10.1007/s10461-004-7322-5. [DOI] [PubMed] [Google Scholar]
- 31.Jin F, Prestage GP, Mao L, Poynten IM, Templeton DJ, Grulich AE, Zablotska I. “Any condomless anal intercourse” is no longer an accurate measure of HIV sexual risk behavior in gay and other men who have sex with men. Front Immunol. 2015;6:1–7. doi: 10.3389/fimmu.2015.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Alvy LM, McKirnan DJ, Mansergh G, et al. Depression is associated with sexual risk among men who have sex with men, but is mediated by cognitive escape and self-efficacy. AIDS Behav. 2011;15(6):1171–9. doi: 10.1007/s10461-010-9678-z. [DOI] [PubMed] [Google Scholar]
- 33.Klein H. Depression and HIV risk-taking among men who have sex with other men and who use the internet to find partners for unprotected sex. J Gay Lesbian Ment Health. 2014;18(2):164–89. doi: 10.1080/19359705.2013.834858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Perdue T, Hagan H, Thiede H, Valleroy L. Depression and HIV risk behavior among Seattle-area injection drug users and young men who have sex with men. AIDS Educ Prev. 2003;15(1):81–92. doi: 10.1521/aeap.15.1.81.23842. [DOI] [PubMed] [Google Scholar]
- 35.Koblin BA, Husnik MA, Colfax G, et al. Risk factors for HIV infection among sex who have sex with men. AIDS Behav. 2006;20(5):731–9. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- 36.O’Cleirigh C, Newcomb ME, Mayer KH, Skeer M, Traeger L, Safren SA. Moderate levels of depression predict sexual transmission risk in HIV-infected MSM: a longitudinal analysis of data from six sites involved in a “prevention for positives” study. AIDS Behav. 2013;17(5):1764–9. doi: 10.1007/s10461-013-0462-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shiu CS, Chen YC, Tseng PC, et al. Curvilinear relationship between depression and unprotected sexual behaviors among men who have sex with men. J Sex Med. 2014;11(10):2466–73. doi: 10.1111/jsm.12638. [DOI] [PubMed] [Google Scholar]
- 38.Rogers G, Curry M, Oddy J, Pratt N, Beilby J, Wilkinson D. Depressive disorders and unprotected casual anal sex among Australian homosexually active men in primary care. HIV Med. 2003;4(3):271–5. doi: 10.1046/j.1468-1293.2003.00155.x. [DOI] [PubMed] [Google Scholar]
- 39.Beidas RS, Birkett M, Newcomb ME, Mustanski B. Do psychiatric disorders moderate the relationship between psychological distress and sexual risk-taking behaviors in young men who have sex with men? A longitudinal perspective. AIDS Patient Care STDs. 2012;26(6):366–74. doi: 10.1089/apc.2011.0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grov C, Cain D, Whitfield TH, Rendina HJ, Pawson M, Ventuneac A, Parsons JT. Recruiting a US National sample of HIV-negative gay and bisexual men to complete at-home self-administered HIV/STI testing and surveys: challenges and opportunities. Sex Res Social Policy. 2016;13(1):1–21. doi: 10.1007/s13178-015-0212-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Radloff LS. The CES-D scale: a self report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 42.Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. 1997;12(2):277–87. doi: 10.1037//0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- 43.Bancroft J, Janssen E, Strong D, Carnes L, Vukadinovic Z, Long JS. Sexual risk-taking in gay men: the relevance of sexual arousability, mood, and sensation seeking. Arch Sex Behav. 2003;32(6):555–72. doi: 10.1023/a:1026041628364. [DOI] [PubMed] [Google Scholar]
- 44.Bancroft J, Janssen E, Strong D, Vukadinovic Z. The relation between mood and sexuality in gay men. Arch Sex Behav. 2003;32(3):231–42. doi: 10.1023/a:1023461500810. [DOI] [PubMed] [Google Scholar]
- 45.Kalichman SC, Rompa D. Sexual sensation seeking and sexual compulsivity scales: reliability, validity, and predicting HIV risk behavior. J Pers Assess. 1995;65(3):586–601. doi: 10.1207/s15327752jpa6503_16. [DOI] [PubMed] [Google Scholar]
- 46.Parsons JT, Kelly BC, Bimbi DS, DiMaria L, Wainberg ML, Morgenstern J. Explanations for the origins of sexual compulsivity among gay and bisexual men. Arch Sex Behav. 2008;37(5):817–26. doi: 10.1007/s10508-007-9218-8. [DOI] [PubMed] [Google Scholar]
- 47.Morgenstern J, Muench F, O’Leary A, Wainberg ML, Parsons JT, Hollander E. Assessing non-paraphilic compulsive sexual behavior and psychiatric co-morbidities in a community sample of gay and bisexual men. J Sex Res. 2011;18(3):114–34. doi: 10.1080/10720162.2011.593420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, Parsons JT. LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: a randomized controlled trial of a transdiagnostic minority stress approach. J Consult Clin Psychol. 2015;83(5):875–89. doi: 10.1037/ccp0000037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Carter LW, II, Mollen D, Smith NG. Locus of control, minority stress, and psychological distress among lesbian, gay, and bisexual individuals. J Couns Psychol. 2014;61(1):169–76. doi: 10.1037/a0034593. [DOI] [PubMed] [Google Scholar]
- 50.Martin JI, Knox J. Self-esteem instability and its implications for HIV prevention among gay men. Health Soc Work. 1997;22(4):264–75. doi: 10.1093/hsw/22.4.264. [DOI] [PubMed] [Google Scholar]