Abstract
Background:
Utilization of total knee and hip arthroplasty has greatly increased in the past decade in the United States; these are among the most expensive procedures in patients with Medicare. Advances in surgical techniques, anesthesia, and care pathways decrease hospital length of stay. We examined how trends in hospital cost were altered by decreases in length of stay.
Methods:
Procedure, demographic, and economic data were collected on 6.4 million admissions for total knee arthroplasty and 2.8 million admissions for total hip arthroplasty from 2002 to 2013 using the National (Nationwide) Inpatient Sample, a component of the Healthcare Cost and Utilization Project. Trends in mean hospital costs and their association with length of stay were estimated using inflation-adjusted, survey-weighted generalized linear regression models, controlling for patient demographic characteristics and comorbidity.
Results:
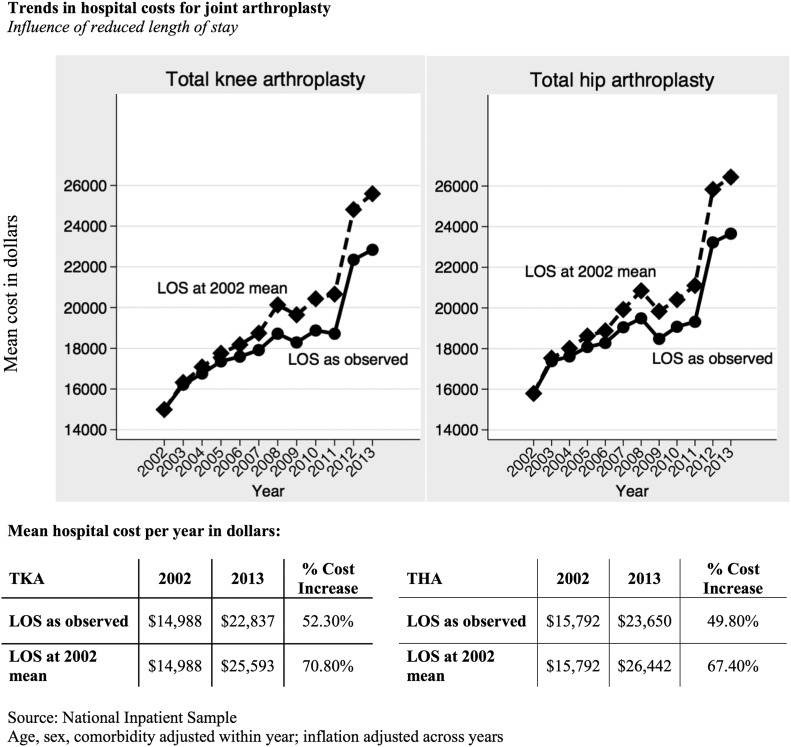
From 2002 to 2013, the length of stay decreased from a mean time of 4.06 to 2.97 days for total knee arthroplasty and from 4.06 to 2.75 days for total hip arthroplasty. During the same time period, the mean hospital cost for total knee arthroplasty increased from $14,988 (95% confidence interval [CI], $14,927 to $15,049) in 2002 to $22,837 (95% CI, $22,765 to $22,910) in 2013 (an overall increase of $7,849 or 52.4%). The mean hospital cost for total hip arthroplasty increased from $15,792 (95% CI, $15,706 to $15,878) in 2002 to $23,650 (95% CI, $23,544 to $23,755) in 2013 (an increase of $7,858 or 49.8%). If length of stay were set at the 2002 mean, the growth in cost for total knee arthroplasty would have been 70.8% instead of 52.4% as observed, and the growth in cost for total hip arthroplasty would have been 67.4% instead of 49.8% as observed.
Conclusions:
Hospital costs for joint replacement increased from 2002 to 2013, but were attenuated by reducing inpatient length of stay. With demographic characteristics showing an upward trend in the utilization of joint arthroplasty, including a shift toward younger population groups, reduction in length of stay remains an important target for procedure-level cost containment under emerging payment models.
Total knee arthroplasty and total hip arthroplasty are two of the most common surgical procedures performed in the United States and among the greatest surgical expenditures in patients with Medicare1. The utilization of total knee arthroplasty and total hip arthroplasty has increased with >700,000 annual cases of total knee arthroplasty and >300,000 annual cases of total hip arthroplasty2. An aging population, the growing obesity epidemic, and expanded indications have contributed to the increase3,4. As costs associated with the operative procedure, inpatient care, rehabilitation, and postoperative care have increased, physician reimbursement has decreased5. With reimbursement rates unlikely to rise, the financial feasibility of total knee arthroplasty and total hip arthroplasty has focused on cost containment by ensuring efficiency and minimizing complications.
Reducing length of stay is a common focus for hospitals seeking to contain costs. The mean length of stay for total knee arthroplasty and total hip arthroplasty has decreased over the past 2 decades as pain management protocols, implants, anesthesia procedures, and surgical techniques have improved6-9. In 1987, the mean length of stay for total knee arthroplasty and total hip arthroplasty was 3 weeks10, dropping to 5 days by the 2000s9. We sought to examine trends in mean hospital costs for total knee arthroplasty and total hip arthroplasty from 2002 to 2013. We hypothesized that the reduced length of stay attenuated mean hospital cost trends, suggesting that this was a beneficial strategy to slow the pace of increase in costs for these two common procedures.
Materials and Methods
Data Sources
We examined the Agency for Healthcare Research and Quality (AHRQ) National (Nationwide) Inpatient Sample (NIS), a component of the Healthcare Cost and Utilization Project (HCUP). The NIS is a discharge database providing uniformly coded patient demographic characteristics; diagnosis and procedure codes from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM); discharge disposition; and hospital charges. Hospitals included in the NIS derive from a sample of the American Hospital Association’s Annual Survey11. Design and weighting variables, included with the NIS, ensure that the sample is nationally representative of discharges from U.S. community hospitals.
We examined trends in procedure rates, length of stay, and hospital costs for inpatient total knee and hip replacements from 2002 through 2013. The starting year of 2002 was selected because it was the first year that the NIS included variables to identify elective admissions, which was our primary focus.
Supplemental data used for our analyses include HCUP’s year and hospital-specific Cost-to-Charge Ratio (CCR) files to estimate hospital costs and the U.S. Bureau of Economic Analysis GDP (Gross Domestic Product) Implicit Price Deflator to adjust for inflation. An Implicit Price Deflator is a price index used to estimate the inflation and deflation of cost with respect to a specific base year, making prices less distorted over time.
Study Population
We identified adults (≥20 years of age) undergoing elective total knee or hip replacement for osteoarthritis from 2002 to 2013. We included only patients who had both a diagnosis code for osteoarthritis and a procedure code for total knee or hip replacement. Patients were identified using relevant ICD-9-CM diagnosis and procedure codes12,13.
We excluded admissions that included codes for total knee revision or removal (which implied previous total knee arthroplasty), repair of fracture, arthroscopy, excision of a joint structure, or arthrodesis (see Appendix). Patients who underwent total knee arthroplasty and had co-listed diagnoses of arthralgia, arthropathy, structural knee problems (e.g., meniscal tears), rheumatoid arthritis or polyarthropathies, osteonecrosis, and/or a septic joint were retained in the analysis. We were unable to identify patients undergoing bilateral procedures during the same admission from the NIS; staged bilateral replacements would have been included as two separate procedures.
Exclusions for the total hip arthroplasty cohort were diagnoses of osteoporosis, osteonecrosis, deformity, congenital or traumatic dislocation and fractures, and procedures of joint revision or removal, resurfacing, fracture repair, reduction of total hip arthroplasty, tenotomy, and partial hip replacement. From both cohorts, we also excluded patients with diagnosis codes for cancer or immunodeficiency diseases.
Calculating Costs
The NIS includes hospital charges to Medicare, Medicaid, commercial insurance, and self-paid sources, excluding professional and non-covered services. Admissions with hospital charges that were excessively high or low were recoded as missing (the NIS retains those between $25 and $1.0 million, inclusive, from 2002 to 2006, and between $100 and $1.5 million, inclusive, beginning in 2007). The NIS database is limited to total hospital charges, which reflect the amount billed to the payer for each admission. Hospital costs are distinct from hospital charges or reimbursements and are intended to reflect the actual dollars for providing a service. Hospital costs were estimated by multiplying the charges by HCUP’s Group Average All-Payer Inpatient Cost-to-Charge (GAPICC) ratio, the inpatient costs incurred by the hospital divided by the inpatient charges for all payers as reported on Medicare cost reports. When the all-payer costs and charges are not known for a specific hospital, the GAPICC ratio calculates the mean CCR for a hospital based on similar hospitals within the same state or urban or rural location, and on the bed count for which the cost and charge values are reported14.
Descriptive Variables
Changes in patient characteristics and length of stay may explain some of the utilization and cost trends over time. HCUP includes variables for age, sex, race, income quartile, and primary payer. We recoded race and ethnicity variables into white, black, or other (which grouped Hispanic, Asian, Pacific Islander, Native American, and other ethnicities together, because of small numbers in some categories). Because some hospitals do not report patient race or ethnicity to the NIS, this variable was missing for a large proportion of cases and was not used in our regression analyses. The median income for the zip code where the patient lives was used as a proxy for socioeconomic status and was grouped into quartiles by HCUP. Income thresholds for this variable change in absolute values annually, and we reported this variable as it was coded by HCUP beginning in 2003. The patient’s primary payer was grouped into Medicare, Medicaid, commercial insurance, and other. The latter category included self-pay and charity service as well as cases in which information on the payer was unavailable from the source hospital. We estimated comorbidity using the Quan version of the Charlson Comorbidity Index15. This index was entered into our analysis as a categorical variable grouped as 0, 1, or ≥2.
Statistical Analysis
We compared patient characteristics between 2002 and 2013 using chi-square comparisons for differences in proportions or t tests for the continuous age variable. The mean hospital costs were initially calculated using survey-weighted generalized linear regression models (gamma distribution, log-link function) including categorical variables for year, sex, and comorbidity, and continuous variables for age (centered at the mean) and length of stay. The model is robust in that it prevents skewed distributions and extreme outliers from being overly influential in estimating means. We Winsorized the length of stay at 7 days (equivalent to the 95th percentile) to prevent a small number of patients with extremely long lengths of stay from driving the mean results. Winsorizing is a statistical transformation to account for extreme values by setting values above the 95th percentile to the 95th percentile. A polynomial term for age was considered, but was not necessary in the final model. The insurance variable was excluded from the final model because it was collinear with age (people who are >65 years of age are primarily insured through Medicare). To estimate the effect of reduced length of stay on cost trends, we examined changes in the annual marginal costs between a model with a length of stay fixed at the 2002 mean and a model with length of stay as observed.
A waiver from human subjects review was obtained from the Committee for the Protection of Human Subjects at Dartmouth College, which designates the NIS as public data. All analyses were performed using Stata-MP, version 13.1 (StataCorp), with hypothesis testing at an alpha level set at 0.05.
Results
Cohorts
From 2002 to 2013, there were approximately 6.4 million admissions for total knee arthroplasty and 2.8 million admissions for total hip arthroplasty combined with a diagnosis code for osteoarthritis. In 2013, the most recent year of data, there were 663,945 total knee arthroplasty admissions and 313,460 total hip arthroplasty admissions combined with a diagnosis code for osteoarthritis. Focusing on elective total knee arthroplasty and total hip arthroplasty admissions, we excluded 1,274,942 admissions for total knee arthroplasty and 605,858 admissions for total hip arthroplasty (see Appendix). Patient demographic characteristics (Table I) show that patients who are white, those who are female, and those who are ≥65 years of age and have Medicare encompass the majority of total knee arthroplasty and total hip arthroplasty admissions. However, the proportion of all total knee arthroplasties that were performed among younger patients (20 to 64 years of age) increased from 37% to 43% from 2002 to 2013 (p < 0.001), with a similar increase from 39% to 46% for total hip arthroplasty during the same time period (p < 0.001). Although the white population encompassed 84% to 89% of the inpatient sample, depending on the year, black groups increased by ∼0.6% to 1.5% in both total knee arthroplasty and total hip arthroplasty. We found a substantial decrease in the length of stay. From 2002 to 2013, the mean hospital stay decreased from 4.06 to 2.97 days for total knee arthroplasty and from 4.06 to 2.75 days for total hip arthroplasty (see Appendix). Hospital stays of ≥5 days for total knee arthroplasty reduced from 24.7% in 2002 to 6.1% in 2013, and those for total hip arthroplasty reduced from 24.5% in 2002 to 4.9% in 2013 (Table I).
TABLE I.
Patient Characteristics
| Total Knee Arthroplasty* |
Total Hip Arthroplasty* |
|||||
| 2002 | 2013 | All Years | 2002 | 2013 | All Years | |
| Age | ||||||
| Mean age (yr) | 67.3 | 66.0 | 66.4 | 66.6 | 65.4 | 65.8 |
| Age group† | ||||||
| 20 to 64years | 36.8 | 42.8 | 41.9 | 39.1 | 45.9 | 44.2 |
| ≥65 years | 63.2 | 57.2 | 58.1 | 60.9 | 54.1 | 55.8 |
| Sex† | ||||||
| Male | 35.8 | 38.1 | 36.8 | 43.8 | 45.6 | 45.4 |
| Female | 64.2 | 61.9 | 63.2 | 56.2 | 54.4 | 54.6 |
| Race† | ||||||
| White | 84.3 | 82.9 | 84.0 | 89.3 | 87.0 | 88.1 |
| Black | 6.9 | 7.5 | 7.0 | 5.5 | 6.9 | 6.2 |
| Asian | 6.0 | 5.5 | 5.1 | 3.0 | 3.1 | 2.8 |
| Other or multiple | 2.8 | 4.2 | 3.8 | 2.2 | 3.0 | 2.9 |
| No. of comorbidities† | ||||||
| 0 | 66.8 | 58.9 | 61.1 | 72.7 | 66.1 | 67.7 |
| 1 | 26.7 | 28.1 | 28.5 | 22.3 | 23.7 | 23.9 |
| ≥2 | 6.5 | 13.0 | 10.3 | 5.0 | 10.2 | 8.3 |
| Income quartile†‡ | ||||||
| 1 (low income) | NA | 21.8 | 21.6 | NA | 18.0 | 17.7 |
| 2 | NA | 27.5 | 26.9 | NA | 24.7 | 24.7 |
| 3 | NA | 26.9 | 26.7 | NA | 27.6 | 27.2 |
| 4 (high income) | NA | 23.7 | 24.7 | NA | 29.8 | 30.4 |
| Insurance† | ||||||
| Medicare | 59.9 | 55.3 | 55.8 | 57.0 | 52.0 | 53.1 |
| Medicaid | 2.2 | 2.9 | 2.6 | 1.8 | 2.7 | 2.4 |
| Commercial | 34.4 | 37.9 | 37.8 | 39.0 | 42.0 | 41.6 |
| Other or uninsured | 3.5 | 3.9 | 3.7 | 2.1 | 3.3 | 2.9 |
| Length of stay† | ||||||
| 1 day | 0.8 | 4.4 | 2.3 | 0.6 | 8.9 | 3.3 |
| 2 days | 5.7 | 25.7 | 13.4 | 5.2 | 32.1 | 16.5 |
| 3 days | 36.0 | 53.3 | 51.2 | 35.9 | 45.5 | 48.7 |
| 4 days | 32.7 | 10.5 | 20.2 | 33.8 | 8.6 | 19.4 |
| ≥5 days | 24.7 | 6.1 | 13.0 | 24.5 | 4.9 | 12.1 |
| Diagnosis† | ||||||
| Osteoarthritis† | 94.9 | 92.3 | 93.6 | 95.2 | 93.5 | 94.2 |
| Rheumatoid arthritis† | 5.1 | 7.7 | 6.4 | 4.8 | 6.5 | 5.8 |
| Pulmonary embolism or deep venous thrombosis† | ||||||
| No | 98.8 | 99.3 | 99.1 | 99.5 | 99.8 | 99.6 |
| Yes | 1.2 | 0.7 | 0.9 | 0.5 | 0.2 | 0.4 |
The differences among groups in each category were significant at p < 0.001.
The values are given as the percentage of patients; these values were determined on the basis of the survey-weighted sample.
Income quartile was not available (NA) in 2002.
Hospital Costs
Using 2002 as a reference year, we calculated the additional mean hospital costs for each year up to 2013 (i.e., the marginal effect for each year), holding all other variables in the model at their respective annual means. As shown in Figure 1, the mean hospital cost of total knee arthroplasty increased from $14,988 (95% confidence interval [CI], $14,928 to $15,049) in 2002 to $22,837 (95% CI, $22,765 to $22,910) in 2013 (an overall increase of $7,849 or 52.4%). Similarly, observed hospital costs for total hip arthroplasty increased from $15,792 (95% CI, $15,706 to $15,878) in 2002 to $23,650 (95% CI, $23,544 to $23,755) in 2013 (an increase of $7,858 or 49.8%). The rate of cost increases slowed between 2009 and 2011, before increasing again in 2012.
Fig. 1.
Mean hospital cost for total knee arthroplasty (TKA) and total hip arthroplasty (THA) from 2002 to 2013, based on NIS data. Total knee arthroplasty and total hip arthroplasty showed a steady increase from 2002 to 2012, with a slowed rate of cost increase between 2009 and 2011. A reduced length of stay (LOS) decreases mean hospital costs. Inflation was adjusted on the basis of the GDP Implicit Price Deflator from the U.S. Bureau of Economic Analysis.
Hospital cost increases were attenuated by the reduction in length of stay over time. When we control for length of stay (that is, removed the effect of length of stay reductions on costs by holding it constant), the marginal costs for the year indicator variables increase, as shown by the differences between the model with length of stay as observed and the model with no length of stay reduction. If the length of stay was set at the 2002 mean (4.06 days) and was not reduced, we estimated that the mean hospital cost for total knee arthroplasty would have increased from $14,988 (95% CI, $14,928 to $15,049) in 2002 to $25,593 (95% CI, $25,466 to $25,720) in 2013 (an increase of $10,605 or 70.8%) (Fig. 1). Similarly, the cost of total hip arthroplasty would have increased from $15,792 (95% CI, $15,706 to $15,878) in 2002 to $26,442 (95% CI, $26,178 to $26,707) in 2013 (an overall increase of $10,650 or 67.4%) (Fig. 1).
These findings suggest that the health-care costs for both total knee arthroplasty and total hip arthroplasty would be increasing at a greater pace in the absence of reduced length of stay. Taking into account demographic factors such as age, race, and insurance as variables did not substantially impact the increased cost trends compared with changes in the length of stay.
Discussion
From 2002 to 2013, the mean hospital cost of total knee arthroplasty and total hip arthroplasty in the United States increased by $7,849 or 52.4% for total knee arthroplasty and $7,858 or 49.8% for total hip arthroplasty. The total hospital cost for joint replacement for osteoarthritis nearly tripled during this 12-year period, amounting to $12.0 billion for total knee arthroplasty and $6.0 billion for total hip arthroplasty in 2013. Reducing the length of stay appeared to be one successful approach to slowing the pace of increase in mean hospital costs for joint arthroplasty. In the absence of a reduced length of stay, the 2013 mean inpatient hospital costs would have increased by 18.5% for total knee arthroplasty and 17.6% for total hip arthroplasty, which is considerable given the large volume and progressive use of joint arthroplasty. Interestingly, increasing trends in mean hospital costs stabilized from 2009 to 2011, with a relatively sharper increase in cost in 2012 (Fig. 1), which may have been partly influenced by a methodological change in the NIS sampling strategy14.
The growth in hospital cost can be attributed to many causes, including rising total joint arthroplasty utilization due to expanding indications, an aging population, increased patient obesity, and elevated prices of orthopaedic implants. The list prices for implants, the recommended retail prices that are distinct from wholesale costs, have increased 4.8% to 5.5% annually for primary uncomplicated hip and knee devices. The mean implant price is comparable with total Medicare reimbursement for service rendered ($12,000 for primary uncomplicated total knee arthroplasty and $14,000 for primary uncomplicated total hip arthroplasty)5. Although not directly derived from our data, the 4.8% to 5.5% annual increase in implant list price could theoretically account for a 48% to 55% increase in the hospital charges over the course of a decade, which is similar to the mean hospital cost increase that we saw for total joint arthroplasty from 2002 to 2013.
Much of the hospital cost for total knee arthroplasty and total hip arthroplasty comprised the length of stay, which declined from a mean of 3 weeks10 to 3 to 5 days8,9 in the past 2 decades. This decrease in length of stay was reflected in our data and was consistent with the February 2015 Centers for Disease Control and Prevention (CDC) National Center for Health Statistics (NCHS) report16. Shorter hospital stays and lower costs have been associated with the greater adoption of clinical pathways that seek to align patient treatment goals with optimal care6,17. Similarly, preoperative patient education programs that encourage patients to take an active role in treatment and rehabilitation and aggressive postoperative mobilization goals significantly reduce the mean length of stay7. Advancing techniques for pain control and anesthesia, such as increased use of peripheral nerve or surgical site blocks, have led to improved postoperative pain control, decreased mental status alteration, and lower rates of nausea and vomiting8,9. These improvements result in earlier mobilization of patients, which decreases the time to safe discharge by meeting rehabilitation and safety goals at an expedited pace.
The reported effects of reduced length of stay on outcomes have been mixed. Although several studies have shown no difference in the rate of complications after a short stay after total knee arthroplasty compared with those after a longer stay after the procedure18,19, others found decreased pain and stiffness in early discharge groups, along with a higher risk of revisions from increased dislocations, infections, and implant loosening20. To determine whether reducing length of stay is safe, it is necessary to examine complications, readmissions, and quality metrics during post-acute care and to consider each hospital admission as a part of an episode of care. The NIS data do not enable us to examine postoperative care or readmissions.
Most recently, the Centers for Medicare & Medicaid Services (CMS) have implemented the Comprehensive Care for Joint Replacement Program (CJR), which involves bundled payments and quality measures. Annually, CMS will compare the actual total cost of care for all episodes provided at a hospital with a predetermined episode target price. The target price is a combination of the hospital’s regional and historical episodic spending discounted by 2% to 3%. Hospitals above the target price will be required to pay the difference21. The CJR may lead hospitals to change how they deliver joint replacement services and to possibly alter the costs of joint arthroplasty.
There were several limitations to this study. We reported only hospital cost trends during an initial inpatient admission; we did not show 90-day episode-of-care costs, which include post-acute services, professional fees, complications, and readmissions. We did not explore the regional variability of cost. Additionally, we inferred that length of stay was shortening because of the higher quality of the procedure, decreased risk of complications, improved clinical efficiency, adjusted patient expectations, and improved anesthesia, but we could not account for those specific factors in our data. This study also utilized ICD-9-CM coding to identify total joint arthroplasties and their associated costs, which may misclassify procedures such as unicompartmental knee arthroplasty compared with total knee arthroplasty. Although, to our knowledge, there have been only a few studies examining the validity of ICD-9-CM codes for accurately identifying joint replacement22-24, the general consensus is that administrative codes accurately identify knee and hip arthroplasty. Finally, the analysis of databases containing large samples can increase the possibility of a type-I error, falsely concluding that there is an important association where none exists. A statistical test with a large sample is likely to produce a lower p value, showing significance but not necessarily clinical importance.
Although we included same-day joint replacement procedures performed within the hospital setting, we did not include joint replacements performed in an outpatient or ambulatory setting because our data derived from an inpatient database. Other research has shown that same-day surgical procedures for total knee arthroplasty and total hip arthroplasty may result in safe and cost-effective care for appropriately selected patients, such as those undergoing primary uncomplicated total knee arthroplasty or total hip arthroplasty with limited comorbidities. In one study of patients with short-stay total knee arthroplasty, outpatient groups had costs that were $8,527 lower than those of the 3 to 4-day stay group20. Same-day joint replacements may show a decrease in costs and complications in appropriate patients under a clinical pathway program.
Joint arthroplasty is a major cost driver in U.S. health care, leading policymakers to pursue aggressive cost containment. Our study suggests that hospital cost trends for joint replacement from 2002 to 2013 increased, but were attenuated by concurrent trends in reduced hospital length of stay. It might be troublesome to see cost trends continuing to increase despite the substantial reduction in length of stay from 2002 to 2013, particularly because additional reductions in length of stay may have diminishing returns. Continued efforts to reduce episode-of-care costs, particularly in the context of bundled payment reimbursements, might be sought through implant standardization, utilization of outpatient arthroplasties, improved risk identification, and coordination with post-acute care facilities.
Appendix
A figure showing trends in inpatient length of stay following total knee arthroplasty or total hip arthroplasty from 2002 to 2013, based on NIS data, and tables showing the inclusion and exclusions for hip and knee joint cohorts and multivariable models for annual cost trends in total knee arthroplasty and total hip arthroplasty are available with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/A26).
Footnotes
Investigation performed at the Department of Orthopaedics, Dartmouth Hitchcock Medical Center, and the Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire
Disclosure: One author of this study (B.I.M.) received grants for this project from the Agency for Healthcare Research and Quality (grant HS021695) and the National Institute of Arthritis and Musculoskeletal and Skin Diseases (grant P60AR062799). On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJS/A25).
References
- 1.Cutler DM, Ghosh K. The potential for cost savings through bundled episode payments. N Engl J Med. 2012. March 22;366(12):1075-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention/National Center for Health Statistics. National Hospital Discharge Survey. 2015 Sep 2. http://www.cdc.gov/nchs/nhds/. Accessed 2016 Sep 8.
- 3.Kim SH. Morbid obesity and excessive hospital resource consumption for unilateral primary hip and knee arthroplasty. J Arthroplasty. 2010. December;25(8):1258-66. Epub 2009 Oct 30. [DOI] [PubMed] [Google Scholar]
- 4.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012. February 1;94(3):201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Belatti DA, Pugely AJ, Phisitkul P, Amendola A, Callaghan JJ. Total joint arthroplasty: trends in Medicare reimbursement and implant prices. J Arthroplasty. 2014. August;29(8):1539-44. Epub 2014 Mar 22. [DOI] [PubMed] [Google Scholar]
- 6.Barbieri A, Vanhaecht K, Van Herck P, Sermeus W, Faggiano F, Marchisio S, Panella M. Effects of clinical pathways in the joint replacement: a meta-analysis. BMC Med. 2009. July 1;7:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mertes SC, Raut S, Khanduja V. Integrated care pathways in lower-limb arthroplasty: are they effective in reducing length of hospital stay? Int Orthop. 2013. June;37(6):1157-63. Epub 2013 Mar 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hebl JR, Dilger JA, Byer DE, Kopp SL, Stevens SR, Pagnano MW, Hanssen AD, Horlocker TT. A pre-emptive multimodal pathway featuring peripheral nerve block improves perioperative outcomes after major orthopedic surgery. Reg Anesth Pain Med. 2008. Nov-Dec;33(6):510-7. [PubMed] [Google Scholar]
- 9.Anastase DM, Florescu SC, Munteanu AM, Stoica I, Antonescu D. The influence of the analgesic model on postoperative pain in major knee surgery. Chirurgia (Bucur). 2013. Nov-Dec;108(6):764-9. [PubMed] [Google Scholar]
- 10.Epstein AM, Read JL, Hoefer M. The relation of body weight to length of stay and charges for hospital services for patients undergoing elective surgery: a study of two procedures. Am J Public Health. 1987. August;77(8):993-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Hospital Association. AHA Annual Survey Database. https://www.ahadataviewer.com/book-cd-products/AHA-Survey/. Accessed 2016 Sep 8.
- 12.Martin B. Coding algorithm for classifying knee-related and hip-related medical encounters for selection, exclusion and classification of safety outcomes. http://www.researchgate.net/profile/Brook_Martin. Accessed 2016 Aug 16.
- 13.Martin B. Coding algorithm for classifying knee-related and hip-related medical encounters for selection, exclusion and classification of safety outcomes. http://www.researchgate.net/profile/Brook_Martin. Accessed 2016 Aug 16.
- 14.Healthcare Cost and Utilization Project. Cost-to-Charge Ratio files. 2015. http://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed 2016 Aug 16.
- 15.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005. November;43(11):1130-9. [DOI] [PubMed] [Google Scholar]
- 16.Wolford ML, Palso K, Bercovitz A. Hospitalization for total hip replacement among inpatients aged 45 and over: United States, 2000-2010. NCHS Data Brief. 2015. February;186:1-8. [PubMed] [Google Scholar]
- 17.Kim S, Losina E, Solomon DH, Wright J, Katz JN. Effectiveness of clinical pathways for total knee and total hip arthroplasty: literature review. J Arthroplasty. 2003. January;18(1):69-74. [DOI] [PubMed] [Google Scholar]
- 18.Teeny SM, York SC, Benson C, Perdue ST. Does shortened length of hospital stay affect total knee arthroplasty rehabilitation outcomes? J Arthroplasty. 2005. October;20(7)(Suppl 3):39-45. [DOI] [PubMed] [Google Scholar]
- 19.Calliess T. [Comparison of outpatient vs inpatient total knee arthroplasty]. Z Orthop Unfall. 2009. Jul-Aug;147(4):410 Epub 2009 Aug 19. German. [DOI] [PubMed] [Google Scholar]
- 20.Lovald ST, Ong KL, Malkani AL, Lau EC, Schmier JK, Kurtz SM, Manley MT. Complications, mortality, and costs for outpatient and short-stay total knee arthroplasty patients in comparison to standard-stay patients. J Arthroplasty. 2014. March;29(3):510-5. Epub 2013 Aug 21. [DOI] [PubMed] [Google Scholar]
- 21.Department of Health and Human Services. CMS proposes major initiative for hip and knee replacements. 2015. http://www.hhs.gov/news/press/2015pres/07/20150709.html. Accessed 2016 Aug 16.
- 22.Daneshvar P, Forster AJ, Dervin GF. Accuracy of administrative coding in identifying hip and knee primary replacements and revisions. J Eval Clin Pract. 2012. June;18(3):555-9. Epub 2011 Jan 11. [DOI] [PubMed] [Google Scholar]
- 23.Bozic KJ, Chiu VW, Takemoto SK, Greenbaum JN, Smith TM, Jerabek SA, Berry DJ. The validity of using administrative claims data in total joint arthroplasty outcomes research. J Arthroplasty. 2010. September;25(6)(Suppl):58-61. Epub 2010 Jun 8. [DOI] [PubMed] [Google Scholar]
- 24.Singh JA, Kundukulam JA, Bhandari M. A systematic review of validated methods for identifying orthopedic implant removal and revision using administrative data. Pharmacoepidemiol Drug Saf. 2012. January;21(Suppl 1):265-73. [DOI] [PubMed] [Google Scholar]