Abstract
Background:
Despite the large increase in total hip arthroplasties and total knee arthroplasties, the incidence and prevalence of additional contralateral or ipsilateral joint arthroplasty are poorly understood. The purpose of this study was to determine the rate of additional joint arthroplasty after a primary total hip arthroplasty or total knee arthroplasty.
Methods:
This historical cohort study identified population-based cohorts of patients who underwent primary total hip arthroplasty (n = 1,933) or total knee arthroplasty (n = 2,139) between 1969 and 2008. Patients underwent passive follow-up through their medical records beginning with the primary total hip arthroplasty or total knee arthroplasty. We assessed the likelihood of undergoing a subsequent total joint arthroplasty, including simultaneous and staged bilateral procedures. Age, sex, and calendar year were evaluated as potential predictors of subsequent arthroplasty.
Results:
During a mean follow-up of 12 years after an initial total hip arthroplasty, we observed 422 contralateral total hip arthroplasties (29% at 20 years), 76 contralateral total knee arthroplasties (6% at 10 years), and 32 ipsilateral total knee arthroplasties (2% at 20 years). Younger age was a significant predictor of contralateral total hip arthroplasty (p < 0.0001), but not a predictor of the subsequent risk of total knee arthroplasty. During a mean follow-up of 11 years after an initial total knee arthroplasty, we observed 809 contralateral total knee arthroplasties (45% at 20 years), 31 contralateral total hip arthroplasties (3% at 20 years), and 29 ipsilateral total hip arthroplasties (2% at 20 years). Older age was a significant predictor of ipsilateral or contralateral total hip arthroplasty (p < 0.001).
Conclusions:
Patients undergoing total hip arthroplasty or total knee arthroplasty can be informed of a 30% to 45% chance of a surgical procedure in a contralateral cognate joint and about a 5% chance of a surgical procedure in noncognate joints within 20 years of initial arthroplasty. Increased risk of contralateral total knee arthroplasty following an initial total hip arthroplasty may be due to gait changes prior to and/or following total hip arthroplasty. The higher prevalence of bilateral total hip arthroplasty in younger patients may result from bilateral disease processes that selectively affect the young hip, such as osteonecrosis, or structural hip problems, such as acetabular dysplasia or femoroacetabular impingement.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Total joint arthroplasty is a reliable and successful solution to the functional impact of osteoarthritis of the hip and knee. It has been estimated that around 7 million people living in the United States have undergone a total joint arthroplasty1 and that the need for total hip arthroplasty and total knee arthroplasty will increase in the next 15 years2.
Several studies have estimated the rate of contralateral joint replacement following primary total hip arthroplasty or total knee arthroplasty. For example, two retrospective case series reported a 30% to 35% rate of contralateral total hip arthroplasty at 10 to 15 years following primary hip replacement3,4. Similarly, other studies have estimated the rate of contralateral total knee arthroplasty at 37% to 46% at 10 to 15 years after primary knee replacement3,5,6. Likewise, additional studies have evaluated the rate of knee replacement following primary total hip arthroplasty. Most studies have concluded that primary total hip arthroplasty is associated with a higher rate of subsequent total knee arthroplasty in the contralateral knee4,7,8. Using nationwide data from Australia and Norway, Gillam et al. reported that, at 5 years following primary total hip arthroplasty, the risk of knee replacement was 1.7 times greater in the contralateral knee than in the ipsilateral knee8. In contrast, in a Canadian cohort of about 5,000 patients, Shao et al. reported that the ipsilateral knee was twice as likely to undergo total knee arthroplasty at a mean time of 17.8 years following primary hip replacement3.
Although these studies help to describe the natural history of subsequent arthritis following primary total hip arthroplasty or total knee arthroplasty, many were limited by small referral cohorts and short follow-up time, or they evaluated only total knee arthroplasty or total hip arthroplasty as outcomes. To our knowledge, except from Australia and Norway, population-based studies have been lacking, and similarly, few studies have evaluated risk factors for subsequent joint replacement following primary total knee arthroplasty or total hip arthroplasty. Therefore, the goals of this study were to determine the rate of an additional total joint replacement after a primary total hip arthroplasty or total knee arthroplasty and to evaluate factors associated with additional lower-extremity joint replacement following primary joint arthroplasty. This information could be used to help to educate patients on the need for subsequent joint replacement and to help to manage expectations after primary total hip arthroplasty and total knee arthroplasty.
Materials and Methods
This was a historical cohort study conducted in Olmsted County, Minnesota, which had a population of 144,260 according to the 2010 census. The resources of the Rochester Epidemiology Project (REP) were used to define population-based cohorts of patients who had primary total hip arthroplasty or total knee arthroplasty from 1969 to 20089-12. Briefly, the REP is a large records linkage system containing the complete medical records for all residents of Olmsted County, Minnesota, regardless of the facility in which the care was administered. It allows access to the original medical records for validation of diagnosis, treatments, and outcomes. This population-based infrastructure provides nearly complete ascertainment and follow-up of all patients who underwent primary total hip arthroplasty or total knee arthroplasty in a geographically defined community.
During the study period, we identified 4,072 residents of Olmsted County, Minnesota, who underwent primary total hip arthroplasty or total knee arthroplasty. All patients underwent passive follow-up through their medical records to determine if they underwent a subsequent total hip arthroplasty in the contralateral hip or a primary total knee arthroplasty on either the ipsilateral or contralateral knee. The medical records were reviewed manually to identify subsequent procedures that had been performed elsewhere. The estimates included patients who underwent simultaneous arthroplasties. Revision total hip arthroplasty or total knee arthroplasty of the primary joint replacement was not considered as an outcome. Follow-up of individuals who moved out of the county and were lost to follow-up was censored. As shown in previous studies, >90% of the elderly population (>65 years of age) in this community have complete follow-up11. The cumulative incidence of subsequent total hip arthroplasty or total knee arthroplasty (including simultaneous or staged bilateral procedures) was calculated using the Kaplan-Meier method. Multivariable Cox proportional hazards regression analysis was performed to examine age, sex, and calendar year as potential predictors of subsequent arthroplasty from the time of the original surgical procedure. Cumulative probabilities of subsequent arthroplasty and hazards ratios are reported with 95% confidence intervals (CIs).
Results
The final study cohort comprised 1,933 patients who underwent primary total hip arthroplasty and 2,139 patients who underwent primary total knee arthroplasty during the study period. The mean age at the time of the primary total hip arthroplasty was 66.3 years, and 1,129 patients (58%) were female. Similarly, the mean age at the time of primary total knee arthroplasty was 68.8 years, and 1,339 patients (63%) were female.
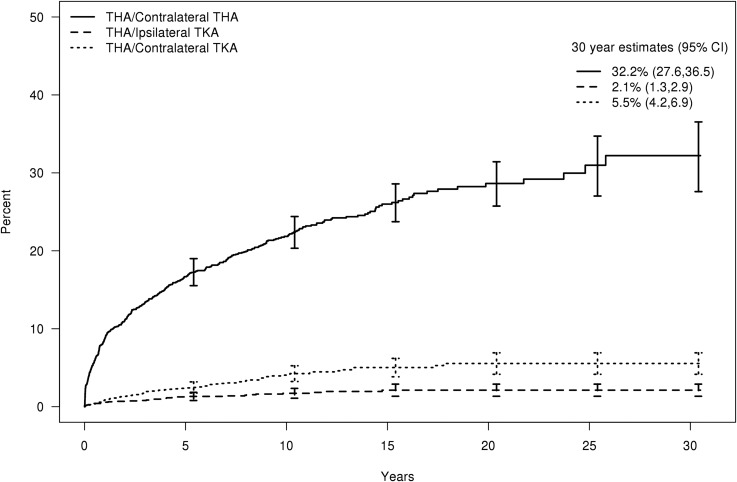
During a mean follow-up (and standard deviation) of 12 ± 7.5 years of the 1,933 patients who underwent a primary total hip arthroplasty, 422 patients underwent a contralateral total hip arthroplasty, corresponding to a cumulative incidence of 21.8% (95% CI, 19.8% to 23.8%) at 10 years and 28.6% (95% CI, 25.7% to 31.4%) at 20 years (Fig. 1). Of the 422 contralateral total hip arthroplasties, 165 were performed within 12 months of the index total hip arthroplasty (1-year cumulative incidence, 9%). Similarly, a total of 32 patients underwent an ipsilateral total knee arthroplasty, with a cumulative incidence of 2.1% (95% CI, 1.3% to 2.9%) at 20 years and 76 patients underwent a contralateral total knee arthroplasty, with a cumulative incidence of 5.5% (95% CI, 4.2% to 6.9%) at 20 years; these cumulative incidences corresponded to a 2.6-fold higher risk of contralateral total knee arthroplasty than ipsilateral total knee arthroplasty (p < 0.001). Younger age at the time of index total hip arthroplasty was a significant predictor of contralateral total hip arthroplasty (p < 0.0001), but not for the subsequent risk of total knee arthroplasty (Table I). Neither sex nor calendar year was significantly associated with a higher risk of subsequent total knee arthroplasty, and the likelihood of contralateral total hip arthroplasty declined over time (p = 0.001).
Fig. 1.
Cumulative incidence of subsequent arthroplasty following primary total hip arthroplasty (THA). The error bars indicate the 95% CI. TKA = total knee arthroplasty.
TABLE I.
Predictors of Subsequent Arthroplasty Among 1,933 Patients Following Primary Total Hip Arthroplasty
| Hazard Ratio* | P Value | |
| Contralateral total hip arthroplasty | ||
| Age | 0.98 (0.98 to 0.99) | <0.0001 |
| Male sex | 1.00 (0.85 to 1.26) | 0.70 |
| Calendar year | 0.99 (0.98 to 0.99) | 0.006 |
| Ipsilateral total knee arthroplasty | ||
| Age | 0.99 (0.96 to 1.02) | 0.41 |
| Male sex | 0.55 (0.25 to 1.20) | 0.13 |
| Calendar year | 0.98 (0.95 to 1.01) | 0.23 |
| Contralateral total knee arthroplasty | ||
| Age | 1.00 (0.98 to 1.02) | 0.99 |
| Male sex | 0.79 (0.49 to 1.27) | 0.32 |
| Calendar year | 0.99 (0.97 to 1.01) | 0.43 |
The values are given as the hazard ratio, with the 95% CI in parentheses.
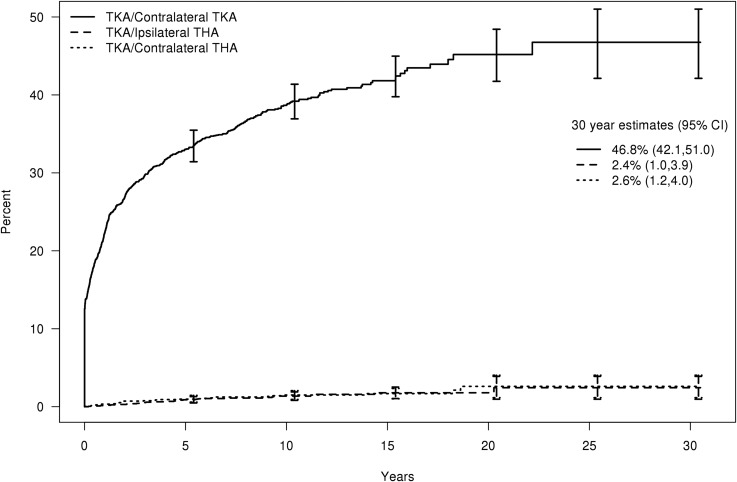
During a mean follow-up of 11 ± 5.5 years of the 2,139 patients who underwent a primary total knee arthroplasty, we observed 809 contralateral total knee arthroplasties, corresponding to a cumulative incidence of 38.7% (95% CI, 36.4% to 40.8%) at 10 years and 45.2% (95% CI, 41.7% to 48.4%) at 20 years (Fig. 2). Of the 809 contralateral total knee arthroplasties, 269 were simultaneous total knee arthroplasties, and 207 additional contralateral total knee arthroplasties were performed within 12 months of the index total knee arthroplasty (1-year cumulative incidence, 22%). During the same time period, a total of 29 patients underwent an ipsilateral total hip arthroplasty, corresponding to a cumulative incidence of 1.8% (95% CI, 1.0% to 2.5%) at 20 years, and 31 patients underwent a contralateral total hip arthroplasty, corresponding to a cumulative incidence of 2.6% (95% CI, 1.2% to 4.0%) at 20 years. Older age at the time of the index total knee arthroplasty was a significant predictor of both ipsilateral and contralateral total hip arthroplasty (p < 0.001 for both) (Table II). Sex was not significantly associated with an increased risk of subsequent arthroplasty following total knee arthroplasty. The likelihood of contralateral total knee arthroplasty and ipsilateral total hip arthroplasty declined significantly (p < 0.001) over time (Table II).
Fig. 2.
Cumulative incidence of subsequent arthroplasty following primary total knee arthroplasty (TKA). The error bars indicate the 95% CI. THA = total hip arthroplasty.
TABLE II.
Predictors of Subsequent Arthroplasty Among 2,139 Patients Following Primary Total Knee Arthroplasty
| Hazard Ratio* | P Value | |
| Contralateral total knee arthroplasty | ||
| Age | 0.99 (0.98 to 1.00) | 0.07 |
| Male sex | 1.14 (0.99 to 1.31) | 0.07 |
| Calendar year | 0.96 (0.96 to 0.97) | <0.0001 |
| Ipsilateral total hip arthroplasty | ||
| Age | 1.11 (1.06 to 1.17) | <0.0001 |
| Male sex | 1.59 (0.75 to 3.38) | 0.23 |
| Calendar year | 0.95 (0.91 to 0.98) | 0.005 |
| Contralateral total hip arthroplasty | ||
| Age | 1.09 (1.04 to 1.14) | 0.0003 |
| Male sex | 1.23 (0.59 to 2.54) | 0.58 |
| Calendar year | 0.99 (0.95 to 1.03) | 0.52 |
The values are given as the hazard ratio, with the 95% CI in parentheses.
Discussion
Despite the extensive volume of research on total joint arthroplasty in the United States, relatively little is known about the long-term need for additional joint replacement following primary total hip arthroplasty and total knee arthroplasty. To our knowledge, there have been no population-based studies in the United States evaluating the rate of additional arthroplasty after index joint replacement. Therefore, the goals of this study were to identify a geographically defined cohort of patients who underwent primary total hip arthroplasty or total knee arthroplasty and to evaluate both the rate and predictive factors of additional joint arthroplasty.
By 10 years following primary total hip arthroplasty, 22% of patients in the cohort had been treated with contralateral total hip arthroplasty, and by 20 years, 29% had undergone a contralateral total hip arthroplasty. This is slightly lower than previously reported rates of 30% to 35% by 10 to 15 years after primary total hip arthroplasty3,4. The lower rate of subsequent total hip arthroplasty in this cohort is possibly related to the population-based design of this study rather than results based on selected cohorts at orthopaedic referral centers. Our results also indicate that after primary total hip arthroplasty, patients undergo contralateral total knee arthroplasty twice as often as ipsilateral total knee arthroplasty. This finding is consistent with most previous reports showing more frequent total knee arthroplasty in the contralateral knee following hip replacement7,8. In particular, Gillam et al.8 reported similar findings from the Australian registry (n = 78,634) and the Norwegian registry (n = 19,786). After the first total hip arthroplasty, the hazard of undergoing a total knee arthroplasty on the contralateral side was higher than the hazard of undergoing a total knee arthroplasty on the ipsilateral side, with a hazard ratio of 1.83 in Australia and 2.97 in Norway. Similarly, Jungman et al. recently reported that the contralateral knee had lower functional scores and more frequent cartilage injury than the ipsilateral knee both at baseline and 4 years following total hip arthroplasty7. Although the reasons for this association are not completely understood, it is possible that gait changes in patients with hip arthritis place increased stress on the contralateral knee prior to and/or after total hip arthroplasty, leading to accelerated degenerative changes and symptom exacerbation in the contralateral knee7,13.
Following total hip arthroplasty, young age was predictive of patients undergoing a contralateral total hip arthroplasty. The higher prevalence of bilateral total hip arthroplasty in younger patients may result from bilateral disease processes that selectively affect younger hips, such as osteonecrosis, or structural hip problems, such as acetabular dysplasia and femoroacetabular impingement. In this cohort, 65 patients who were <50 years of age underwent bilateral total hip arthroplasties. Among these patients, 15% were diagnosed with osteonecrosis prior to total hip arthroplasty. Similarly, in this same group, 21% were diagnosed with either femoroacetabular impingement or hip dysplasia prior to the surgical procedure.
Of the patients who had been treated with a contralateral total knee arthroplasty following primary total knee arthroplasty, 39% had been treated by 10 years, and 45% had been treated by 20 years. These findings are again consistent with but slightly lower than previously reported rates of 37% to 46% at a 10 to 15-year follow-up3,5,6. After total knee arthroplasty, patients have a high likelihood of undergoing a contralateral total knee arthroplasty and a low likelihood of a subsequent total hip arthroplasty (2%), which is equal between both hips. A possible explanation for this is that the biologic and mechanical factors leading to arthritis often affect both knees. Furthermore, some biomechanical studies have shown adduction moment abnormalities and continued reliance on the contralateral knee after total knee arthroplasty, resulting in dynamic loading asymmetries between the knees14-16.
Despite the population-based design, our findings should be interpreted in light of potential limitations. The population of Olmsted County, Minnesota, is primarily Caucasian, and Olmsted County residents are served by a robust health-care infrastructure. Therefore, the generalizability of our estimates to populations with more racial or socioeconomic diversity or differences in health-care utilization is unknown. The regional and national variation in rates of arthroplasty also limits the generalizability of our findings. This study focused only on subsequent primary joint replacement and did not capture any revision surgical procedure of the index joint replacement. Despite the long and complete follow-up, the sample size was too small to examine some issues related to laterality. In addition, we did not account for any baseline diagnosis of arthritis in other joints at the time of index joint replacement, which likely influences the likelihood of subsequent arthroplasty. We also did not account for other factors, such as insurance status and comorbidities, that may influence subsequent arthroplasty. However, despite these limitations, the unique ability to identify a population-based cohort of patients who underwent primary joint arthroplasty and the long and complete follow-up over time allowed us to describe the true rate of subsequent joint replacement.
In conclusion, patients undergoing total hip arthroplasty or total knee arthroplasty can be informed of a 30% to 45% chance of a surgical procedure in the contralateral cognate joint and a 5% chance of a surgical procedure in noncognate joints within 20 years of the first arthroplasty. Increased risk of contralateral total knee arthroplasty following an initial total hip arthroplasty may be due to gait changes following and/or prior to total hip arthroplasty. The higher prevalence of bilateral total hip arthroplasty in younger patients may result from bilateral disease processes that selectively affect the young hip, such as osteonecrosis, or structural hip problems, such as acetabular dysplasia or femoral acetabular impingement.
Footnotes
Investigation performed at the Departments of Orthopedic Surgery and Health Sciences Research, Mayo Clinic, Rochester, Minnesota
Disclosure: This study relied on the Rochester Epidemiology Project infrastructure, which is supported by the National Institute on Aging of the National Institutes of Health under award number R01AG034676. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work and “yes” to indicate that the author had a patent and/or copyright, planned, pending, or issued, broadly relevant to this work (http://links.lww.com/JBJS/A24).
Disclaimer: The findings and conclusions of this report are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
References
- 1.Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, Jiranek WA, Berry DJ. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015. September 2;97(17):1386-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007. April;89(4):780-5. [DOI] [PubMed] [Google Scholar]
- 3.Shao Y, Zhang C, Charron KD, Macdonald SJ, McCalden RW, Bourne RB. The fate of the remaining knee(s) or hip(s) in osteoarthritic patients undergoing a primary TKA or THA. J Arthroplasty. 2013. December;28(10):1842-5. [DOI] [PubMed] [Google Scholar]
- 4.Sayeed SA, Trousdale RT, Barnes SA, Kaufman KR, Pagnano MW. Joint arthroplasty within 10 years after primary Charnley total hip arthroplasty. Am J Orthop (Belle Mead NJ). 2009. August;38(8):E141-3. [PubMed] [Google Scholar]
- 5.Ritter MA, Carr KD, Keating EM, Faris PM. Long-term outcomes of contralateral knees after unilateral total knee arthroplasty for osteoarthritis. J Arthroplasty. 1994. August;9(4):347-9. [DOI] [PubMed] [Google Scholar]
- 6.McMahon M, Block JA. The risk of contralateral total knee arthroplasty after knee replacement for osteoarthritis. J Rheumatol. 2003. August;30(8):1822-4. [PubMed] [Google Scholar]
- 7.Jungman P, Nevitt M, Baum T, Liebl H, Nardo L, Liu F, Lane N, McCulloch C, Link T. Relationship of unilateral total hip arthroplasty (THA) to contralateral and ipsilateral knee joint degeneration – a longitudinal 3T MRI study from the Osteoarthritis Initiative (OAI). Osteoarthritis Cartilage. 2015. July;23(7):1144-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gillam MH, Lie SA, Salter A, Furnes O, Graves SE, Havelin LI, Ryan P. The progression of end-stage osteoarthritis: analysis of data from the Australian and Norwegian joint replacement registries using a multi-state model. Osteoarthritis Cartilage. 2013. March;21(3):405-12. Epub 2012 Dec 26. [DOI] [PubMed] [Google Scholar]
- 9.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ 3rd. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012. December;87(12):1202-13. Epub 2012 Nov 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012. February;87(2):151-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, Pankratz JJ, Brue SM, Rocca WA. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012. December;41(6):1614-24. Epub 2012 Nov 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester Epidemiology Project. Am J Epidemiol. 2011. May 1;173(9):1059-68. Epub 2011 Mar 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shakoor N, Foucher KC, Wimmer MA, Mikolaitis-Preuss RA, Fogg LF, Block JA. Asymmetries and relationships between dynamic loading, muscle strength, and proprioceptive acuity at the knees in symptomatic unilateral hip osteoarthritis. Arthritis Res Ther. 2014. December 14;16(6):455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alnahdi AH, Zeni JA, Snyder-Mackler L. Gait after unilateral total knee arthroplasty: frontal plane analysis. J Orthop Res. 2011. May;29(5):647-52. Epub 2010 Dec 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Milner CE, O’Bryan ME. Bilateral frontal plane mechanics after unilateral total knee arthroplasty. Arch Phys Med Rehabil. 2008. October;89(10):1965-9. [DOI] [PubMed] [Google Scholar]
- 16.Worsley P, Stokes M, Barrett D, Taylor M. Joint loading asymmetries in knee replacement patients observed both pre- and six months post-operation. Clin Biomech (Bristol, Avon). 2013. October;28(8):892-7. Epub 2013 Aug 7. [DOI] [PubMed] [Google Scholar]