Abstract
Objective:
The authors evaluate the significance of atlantoaxial instability in the management of idiopathic syringomyelia.
Background:
We recently observed that atlantoaxial dislocation can be present even when the atlantodental interval was within normal range. Atlantoaxial instability can be identified on the basis of facetal mal-alignment or even by direct observation of status of joint during surgery. Our observations are discussed in nine patients where we identified and treated atlantoaxial instability in cases that would otherwise be considered as having “idiopathic” syrinx.
Materials and Methods:
The authors report experience with nine cases that were diagnosed to have “idiopathic” syrinx. The main bulk of the syrinx was located in the cervico-dorsal spinal region in all cases. One patient had been treated earlier by syringo-subarachnoid shunt surgery and one patient had undergone foramen magnum decompression.
Results:
On radiological evaluation, eight patients had posterior atlantoaxial facetal (Type B) dislocation. In one patient there was no facetal mal-alignment and was labeled to have axial or central (Type C) facetal instability. All patients were treated by atlantoaxial fixation. All patients improved symptomatically in the immediate postoperative period and the improvement was progressive and sustained on follow-up. In one case, the size of syrinx reduced in the immediate postoperative imaging. In the period of follow-up (range 6–42 months - average 19 months), reduction in the size of syrinx was demonstrated on imaging in three cases.
Conclusions:
The positive clinical outcome suggests that atlantoaxial instability may be the defining phenomenon in development of previously considered “idiopathic” syringomyelia.
Key words: Atlantoaxial dislocation, basilar invagination, Chiari 1 malformation, syringomyelia
Introduction
Syringomyelia is a relentlessly and progressively growing intramedullary phenomenon that is related to chronic or longstanding pathological alterations in and around the spinal cord.[1,2] Factors like trauma, infections, tumors and craniovertebral junctional abnormalities have been incriminated to be causative. However, there is a significant subgroup where no cause is identified and syringomyelia in such patients is labeled to be “idiopathic.”[3,4,5,6,7] In general, in the later group of patients no clear direction regarding pathogenesis or treatment has yet been specified in the literature. We evaluated nine patients, who were earlier diagnosed on the basis of standard discussed parameters to have “idiopathic” syringomyelia. On radiological re-evaluation Type B or posterior atlantoaxial facetal dislocation was identified in eight cases.[8,9] In the case where no radiological facetal mal-alignment was identified, the patient was considered to have Type C (central or axial) atlantoaxial facetal dislocation.[9] All patients underwent atlantoaxial fixation. No foramen magnum bone or dural decompression was done. The results of surgical treatment are evaluated. On the basis of our experience, an alternative hypothesis of pathogenesis of the previously labeled “idiopathic” subgroup of syringomyelia is presented.
Materials and Methods
During the period August 2012–July 2015, we identified and surgically treated nine consecutive cases where there was syringomyelia and wherein no pathogenetic cause could be identified on conventional imaging parameters. The main bulk of syrinx was located in the cervico-dorsal region of the spine in all cases. None of the patients had associated spinal tumors, definite evidence or clinical history suggestive of infection, trauma, and craniovertebral junction bone anomalies or associated Chiari malformation. There was no atlantoaxial dislocation when assessed by conventional parameters that relate to alterations in atlantodental interval or by evidence of direct neural compression at the level of craniocervical cord. The ages of the patients ranged from 30 to 60 years (average 41 years). There were four males and five females. The presenting clinical symptoms are elaborated in Table 1. The duration of symptoms ranged from 36 to 252 months. All patients underwent dynamic plain radiography, computed tomography (CT) scanning and magnetic resonance imaging (MRI). There was atlantoaxial instability that was manifested as Type B (posterior) atlantoaxial facetal dislocation in eight cases. In one case the facets were in alignment and instability was labeled as Type C (central or axial) atlantoaxial facetal dislocation [Table 1]. All patients underwent segmental atlantoaxial fixation with the technique described by us in 1994.[10,11,12,13] The patients were placed prone for surgery and the head end of the operating table was elevated. Intraoperative Gardner Wells traction was applied essentially to keep the head stable during surgery. Traction assisted in placing the head in a near floating position and the face and eyes were not in direct contact with the headrest and avoided any subsequent pressure injury. Lateral mass fixation was done with titanium plates and screws. C2 ganglion was sectioned in two cases to facilitate joint exposure. In rest of the cases, C2 ganglion was elevated superiorly for joint exposure. The articular cartilage was denuded in all cases and the joint cavity was stuffed with bone chips. Plate and screw fixation was then carried out. Bone graft was additionally placed in the midline over the arch of atlas and lamina of C2 after appropriately preparing the host bone. Bone graft was harvested from the iliac crest.
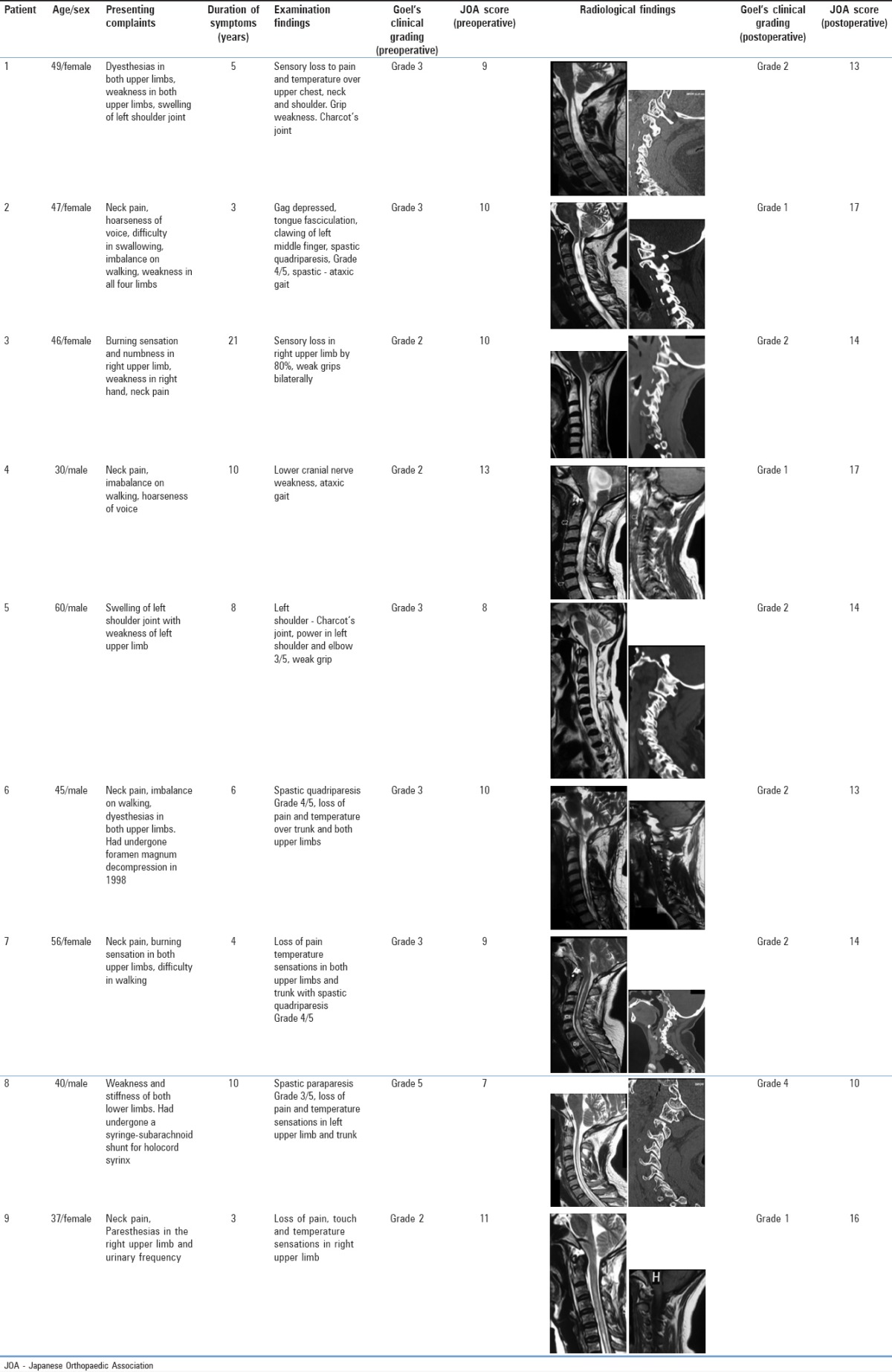
Table 1.
The pre- and post-operative clinical and radiological findings
Results
All patients had “significant” and varying degree of clinical improvement in the immediate postoperative phase and the improvement was progressive and sustained at follow-up. No patient worsened in symptoms after the surgery or after an initial improvement. The clinical recovery as observed at the last follow-up is detailed in the Table 1. Postoperative imaging included CT scan and MRI in the immediate postoperative phase, after 3 months and at the time of last follow-up [Figures 1 and 2]. The syrinx cavity reduced in dimensions in the immediate postoperative imaging in one patient. At 6 months interval, reduction in the size of syrinx was observed in three patients. In rest of the five patients, there was no definite reduction in syrinx size.
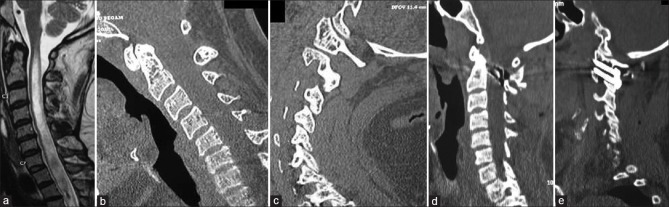
Figure 1.
Images of a 49-year-old female patient. (a) T2-weighted magnetic resonance imaging showing extensive syringomyelia. There is no craniovertebral bone or soft tissue abnormality. (b) Sagittal image of computed tomography scan, with the head in flexion position, showing no evidence of atlantoaxial instability when assessed by parameter of atlantodental interval abnormality. (c) Sagittal computed tomography with the cut passing through the facets showing Type B facetal instability. (d) Postoperative computed tomography scan after atlantoaxial fixation. (e) Postoperative computed tomography scan with the cut through the facets showing the implant
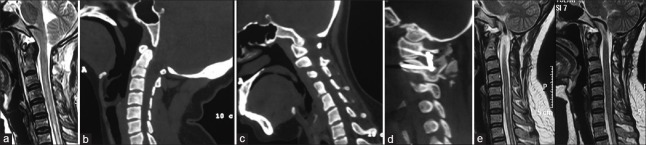
Figure 2.
Images of a 37-year-old female patient. (a) T2-weighted magnetic resonance imaging shows normal bone and neural architecture in the region of foramen magnum and craniovetebral junction. Syringomyelia can be noted. (b) Computed tomography scan shows no evidence of instability as measured by atlantodental interval alteration. (c) Computed tomography scan of the head in flexed position showing Type B facetal dislocation. (d) Postoperative computed tomography scan showing the implant and fixation. (e) Delayed postoperative T2-weighted magnetic resonance imaging showing reduction in the size of the syrinx
Discussion
The subject of syringomyelia is under evaluation for over a century. A number of speculations and hypotheses have been suggested that evaluate the pathogenesis and treatment of this vexed clinical problem.[3,4,5,6,7] In the year 2000, we classified syringomyelia into three groups depending on the identified etiological factor.[12] Group 1 cases included those where no definite cause could be identified. This formed a relatively small but a distinct subgroup of patients. There are several articles in the literature that discuss “idiopathic” syrinx. Alteration in the cerebrospinal fluid flow dynamics in the region of craniovertebral junction related to chronic inflammation is the most frequently speculated cause of such syringomyelia. As no definite cause is identified, the treatment recommended is usually shunt surgery that involves drainage of the syrinx cavity. There have been reports where opening of the foramen magnum and lysing the arachnoidal adhesions have been recommended. However, no universally accepted treatment protocol is yet available.
We recently evaluated atlantoaxial instability in chronically “unstable” clinical situations like basilar invagination, wherein there is a longstanding alteration in the physical musculoskeletal and neural structural form.[14] We analyzed the role of atlantoaxial instability in pathogenesis of cases having Chiari malformation with or without the association of syringomyelia and with or without the association of bone abnormality in the craniovertebral junction.[15,16] On the basis of our observation it was concluded that Chiari malformation may have “air-bag” type of naturally protective effect on the spinal cord and may have a role in preventing pinching of critical neural structures between bones.[17] We also speculated that syringomyelia may be a natural self-neural destruction that ultimately works in the best interest of the patient.[1]
The commonly recognized radiological parameter of identification of atlantoaxial instability is to observe abnormal alterations in atlantodental interval and to identify indentation of the odontoid process into the cervico-medullary cord. We observed that atlantoaxial instability can be identified by focusing the attention on the facets. We discussed three types of atlantoaxial facetal dislocation.[8,9] Type A atlantoaxial facetal dislocation is the more common form of dislocation wherein the facet of atlas is dislocated anterior to the facet of axis. We identified such a form of dislocation as atlantoaxial facetal listhesis and related it to more frequently identified and recognized entity of lumbo-sacral spondylolisthesis.[10,18] In this form of instability, the atlantodental interval increases and the odontoid process indents into the neural structures. Such dislocation is associated with relatively acute clinical presentation. Type B atlantoaxial facetal dislocation is when the facet of atlas is dislocated posterior to the facet of axis. Type C atlantoaxial facetal instability is when the facets are in alignment but the atlantoaxial joint is unstable. Such instability is also called axial or central instability. Instability in Types B and C is identified during direct observation and manipulations of the facets during surgery that involves fixation of the lateral masses.[19] As in both Types B and C, the odontoid process is not displaced posteriorly and there is no direct indention of the neural structures, they are associated with more chronic form of musculoskeletal and neural alterations.
In the present series, we identified that eight cases had Type B and one patient had Type C atlantoaxial facetal dislocation. There was no or only “insignificant” evidence of cord compression at the level of foramen magnum. Our experience of manual handling the facets of atlas and axis and the atlantoaxial joint for over 27 years and surgically treating over 1400 cases having instability of the region, we identified that the joint in these cases was clearly unstable. Moreover, fixation of the joint resulted in an immediate postoperative relief from symptoms. Remarkable reduction in the size of the syrinx cavity in one case in the immediate postoperative imaging and in three cases on imaging after 3 months without any dural violation or syrinx cavity manipulation does suggest the validity of the observation.
Essentially, the observation leads to the suggestion that atlantoaxial instability can be a possible cause in cases having “idiopathic” syringomyelia. The reason as to why Chiari malformation is not associated is unclear. Our observations suggest that investigations should focus the attention on the status of alignment of facets of atlas and axis. Whilst some degree of facetal mal-alignment can be within the range of normalcy, its presence in association with syringomyelia can have clinical and therapeutic significance. In the presence of even subtle evidence of bone abnormalities in the craniovertebral junction, like bone fusions or malformations, even normal facetal alignment can signify instability. We labeled such form of facetal instability as axial or central instability (Type C instability).
Remarkable clinical improvement following atlantoaxial fixation suggests the validity of the observation. However, a larger experience on the subject is mandatory before any conclusions can be drawn.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Goel A. Is syringomyelia pathology or a natural protective phenomenon? J Postgrad Med. 2001;47:87–8. [PubMed] [Google Scholar]
- 2.Goel A, Desai K. Surgery for syringomyelia: An analysis based on 163 surgical cases. Acta Neurochir (Wien) 2000;142:293–301. doi: 10.1007/s007010050038. [DOI] [PubMed] [Google Scholar]
- 3.Logue V, Edwards MR. Syringomyelia and its surgical treatment – An analysis of 75 patients. J Neurol Neurosurg Psychiatry. 1981;44:273–84. doi: 10.1136/jnnp.44.4.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Padovani R, Cavallo M, Gaist G. Surgical treatment of syringomyelia: Favorable results with syringosubarachnoid shunting. Surg Neurol. 1989;32:173–80. doi: 10.1016/0090-3019(89)90175-4. [DOI] [PubMed] [Google Scholar]
- 5.Nakamura M, Ishii K, Watanabe K, Tsuji T, Matsumoto M, Toyama Y, et al. Clinical significance and prognosis of idiopathic syringomyelia. J Spinal Disord Tech. 2009;22:372–5. doi: 10.1097/BSD.0b013e3181761543. [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez A, Kuhn EN, Somasundaram A, Couture DE. Management of idiopathic pediatric syringohydromyelia. J Neurosurg Pediatr. 2015;16:452–7. doi: 10.3171/2015.3.PEDS14433. [DOI] [PubMed] [Google Scholar]
- 7.Roy AK, Slimack NP, Ganju A. Idiopathic syringomyelia: Retrospective case series, comprehensive review, and update on management. Neurosurg Focus. 2011;31:E15. doi: 10.3171/2011.9.FOCUS11198. [DOI] [PubMed] [Google Scholar]
- 8.Goel A. Goel's classification of atlantoaxial “facetal” dislocation. J Craniovertebr Junction Spine. 2014;5:3–8. doi: 10.4103/0974-8237.135206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goel A. Facetal alignment: Basis of an alternative Goel's classification of basilar invagination. J Craniovertebr Junction Spine. 2014;5:59–64. doi: 10.4103/0974-8237.139199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goel A. Treatment of basilar invagination by atlantoaxial joint distraction and direct lateral mass fixation. J Neurosurg Spine. 2004;1:281–6. doi: 10.3171/spi.2004.1.3.0281. [DOI] [PubMed] [Google Scholar]
- 11.Goel A, Bhatjiwale M, Desai K. Basilar invagination: A study based on 190 surgically treated patients. J Neurosurg. 1998;88:962–8. doi: 10.3171/jns.1998.88.6.0962. [DOI] [PubMed] [Google Scholar]
- 12.Goel A, Desai KI, Muzumdar DP. Atlantoaxial fixation using plate and screw method: A report of 160 treated patients. Neurosurgery. 2002;51:1351–6. [PubMed] [Google Scholar]
- 13.Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien) 1994;129:47–53. doi: 10.1007/BF01400872. [DOI] [PubMed] [Google Scholar]
- 14.Goel A, Shah A. Reversal of longstanding musculoskeletal changes in basilar invagination after surgical decompression and stabilization. J Neurosurg Spine. 2009;10:220–7. doi: 10.3171/2008.12.SPINE08499. [DOI] [PubMed] [Google Scholar]
- 15.Goel A. Is atlantoaxial instability the cause of Chiari malformation? Outcome analysis of 65 patients treated by atlantoaxial fixation. J Neurosurg Spine. 2015;22:116–27. doi: 10.3171/2014.10.SPINE14176. [DOI] [PubMed] [Google Scholar]
- 16.Goel A, Achawal S. The surgical treatment of Chiari malformation association with atlantoaxial dislocation. Br J Neurosurg. 1995;9:67–72. [PubMed] [Google Scholar]
- 17.Goel A. Is Chiari malformation nature's protective “air-bag”? Is its presence diagnostic of atlantoaxial instability? J Craniovertebr Junction Spine. 2014;5:107–9. doi: 10.4103/0974-8237.142302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kothari M, Goel A. Transatlantic odonto-occipital listhesis: The so-called basilar invagination. Neurol India. 2007;55:6–7. doi: 10.4103/0028-3886.30416. [DOI] [PubMed] [Google Scholar]
- 19.Goel A. Instability and basilar invagination. J Craniovertebr Junction Spine. 2012;3:1–2. doi: 10.4103/0974-8237.110115. [DOI] [PMC free article] [PubMed] [Google Scholar]