Abstract
Background:
Many patients suffer from radiculopathy and low back pain due to lumbar disc hernia. Transforaminal percutaneous endoscopic discectomy (TPED) is a minimally invasive method that accesses the disc pathology through the intervertebral foramen. Health-related quality of life (HRQoL) has been previously assessed for this method. However, a possible effect of the level of operation on the postoperative progress of HRQoL remains undefined.
Purpose:
The purpose of this study was to evaluate the impact of the level of operation on HRQoL, following TPED.
Patients and Methods:
A total of 76 patients diagnosed with lumbar disc hernia were enrolled in the study. According to the level of operation, they were divided into three groups: Group A (21 patients) for L3–L4, Group B (40 patients) for L4–L5, and Group C (15 patients) for L5–S1 intervertebral level. All patients underwent TPED. Their HRQoL was evaluated by the short-form-36 (SF-36) health survey questionnaire before the operation and at 6 weeks, 3, 6, and 12 months postsurgery. The progress of SF-36 was analyzed in relation to the operated level.
Results:
All aspects of SF-36 showed statistical significant improvement, at every given time interval (P ≤ 0.05) in the total of patients and in each group separately. Group A had a significantly higher increase in physical functioning (PF) score at 3 and 12 months postsurgery (P = 0.046 and P = 0.056, respectively). On the other hand, Group B had a significant lower increase in mental health (MH) score at 6 months (P = 0.009) postoperatively.
Conclusion:
Our study concludes that the level of operation in patients who undergo TPED for lumbar disc herniation affects the HRQoL 1 year after surgery, with Group A having a significantly greater improvement of PF in comparison with Groups B and C.
Key words: Health-related quality of life, low back pain, lumbar disc herniation, short-form-36 health survey, transforaminal percutaneous endoscopic discectomy
Introduction
Low back pain (LBP) is one of the most common complaints affecting 80% of the general population and it has a significant impact on the sectors of health and socioeconomics.[1,2,3] Radiculopathy refers to a set of conditions in which one or more nerves are affected and do not work properly. The location of the injury is at the level of the nerve root. Disc herniation, also called intervertebral disc displacement, is a type of spinal disease with characteristic symptoms of local pain, and in some cases, radiculopathy syndromes and sciatica due to mechanical compression and autoimmune mechanisms upon the corresponding nerve roots.[4] It is more frequent in men, but the prevalence is quite high in both genders.[5] The pathophysiology of disc herniation is mainly attributed to intervertebral disc degeneration.[6]
A high percentage of patients with LBP who remain without treatment suffer for a long time, experience relapses of pain, and present high frequency of work absence.[7] Therapeutic management of lumbar disc herniation has been well described in literature. Surgical intervention is considered in cases nonresponsive to conservative treatment. Surgical techniques include open discectomy, microdiscectomy, and transforaminal percutaneous endoscopic discectomy (TPED).[8,9] Discectomy is the most frequently performed spinal surgery, and the traditional open approach has been replaced by microdiscectomy, which is now the gold standard method.[10,11,12] However, endoscopy is used more and more in the past decades in spinal surgery.[13] TPED allows surgeons to approach the epidural space through the intervertebral foramen, and it is associated with reduced traumatization, hospital stay, and postsurgical morbidity. Nevertheless, it offers direct visualization of the intervertebral space and preservation of the dorsal musculature, the vertebrae, and the ligamentous structures.[14,15,16]
Lumbar disc herniation is more common at the lower levels of lumbar spine, causing sciatica, and less common at the upper levels of the lumbar spine, causing femoralgia. Health-related quality of life (HRQoL) following TPED has been previously reported in the literature. However, the potential impact of the level of operation on the postoperative progress of HRQoL has not been previously studied.[17]
Patients and Methods
Patients and their baseline demographics
All patients agreed to participate in the study and signed a fully informed written consent. The study was approved by the medical council of the hospital and the local Ethics Committee. All the patients enrolled in our study were diagnosed with lumbar hernia and fulfilled all the indications for discectomy.
Inclusion criteria were: (i) radiculopathy (ii) positive nerve root tension sign (iii) sensory or motor neurologic lesion on clinical examination (iv) hernia confirmed by magnetic resonance imaging (MRI) of the lumbar spine, in compliance with clinical findings (v) failure of 12-week conservative treatment.
Exclusion criteria were: (i) noncontaminated disc hernia exceeding the one-third of the spinal canal on the sagittal MRI scans (ii) sequestration of the disc (iii) central or lateral recess spinal stenosis (iv) recurrent herniated disc or previous surgery at the affected level (iii) segmental instability or spondylolisthesis (iv) spinal tumor or infection (v) vertebral fracture.
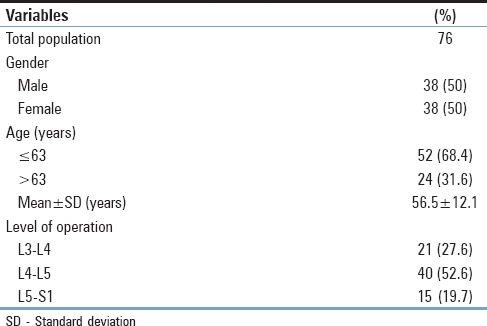
A total of 76 patients were divided into three groups according to the level of operation. Group A consisted of 21 (27.6%) patients, Group B consisted of 40 (52.6%) patients, and Group C consisted of 15 (19.7%) patients, who had been diagnosed with lumbar herniated disc at the levels L3–L4, L4–L5, and L5–S1, respectively. Out of the total 76 patients, 38 (50%) were male and 38 (50%) were female. Moreover, 52 (68.4%) patients were ≤63 years old, while the rest 24 (31.4%) were >63 years old (mean ± standard deviation [SD] = 56.5 ± 12.1 years).
Methods
All patients were scheduled to undergo TPED in the same center by one experienced surgeon. A rehabilitation program including swimming in supine position had been followed by all patients for 4 weeks. Their HRQoL was evaluated by using the short-form-36 (SF-36) health survey questionnaire. Patients were asked to complete the scores right before the surgery. The same procedure was repeated at the following intervals after surgery: 6 weeks, 3 months, 6 months, and 1 year. Our primary hypothesis was that the level of operation could affect the postoperative progress of HRQoL, measured by SF-36 1 year after TPED.
Surgical technique
The surgical technique was TPED. The procedure was performed under local anesthesia and mild sedation. All patients were monitored in terms of blood pressure, pulse rate, oxygen saturation, and electrocardiographic signals. Patients were positioned at the lateral decubitus position, lying down on the opposite site to make the lesion face upward [Figure 1].[13] After the disinfection of the surgical field, local anesthesia was initially performed at the needle entry site. The needle was placed through the Kambin's triangle 11 cm of the midline, under fluoroscopic technique [Figure 2].[13,18] After verification of the level, mild sedation and analgesia were provided with fentanyl (fentanyl ampule) because the enlargement of the neural foramen is painful. The compliance of the patients was affected during the sequential passage of three different size reamers (5.5, 6.5, and 7.5 mm). The cannula and the endoscope were, then, placed and the nerve root was secured. Subsequently, the discectomy was performed with graspers. The patients were monitored for the following hour in the wards and then mobilized. The patients were discharged 1 day after the surgery. Complications were not observed.
Figure 1.
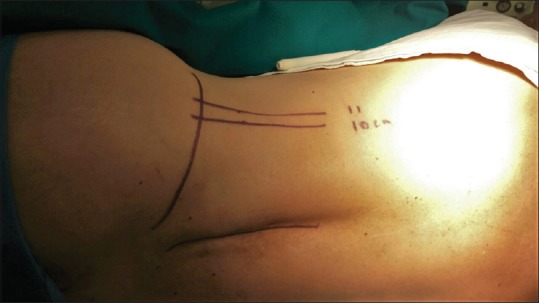
Patients in transforaminal percutaneous endoscopic discectomy procedure are positioned at the lateral decubitus position, while they are lying down on the opposite site to make the lesion face upward. The iliac crest, the spinous processes, and the spot from where the needle is placed through the Kambin's triangle, 11 cm of the midline, are marked
Figure 2.
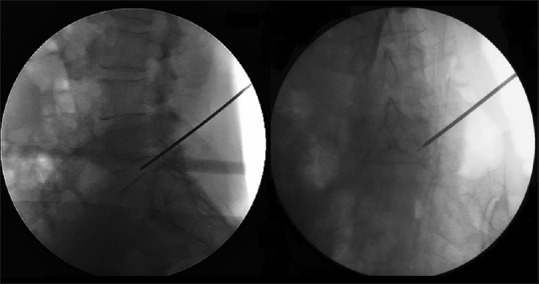
Anteroposterior (right) and lateral (left) intraoperative fluoroscopic images of the guidewire placed at the level where the disc herniation is present
Short-form-36 scoring scale
The scale has 36 items and assesses eight dimensions: physiological function (physical functioning [PF]), physical function (role-physical [RP]), bodily pain (bodily pain [BP]), general health (general health [GH]), energy (vitality [VT]), social function (social functioning [SF]), emotional function (role-emotional [RE]), and mental health (mental health [MH]). The higher the total score of all these eight dimensions is, the better the quality of life of the participants. If respondents answer less than half of the number of entries, their questionnaires are deemed invalid.[19]
Statistical analysis
Continuous variables (age, SF-36 score) are expressed as mean ± SD and categorical variables (gender, level of operation) as percentages [Table 1].
Table 1.
Statistical analysis of continuous (age) and categorical variables (gender, level of operation)
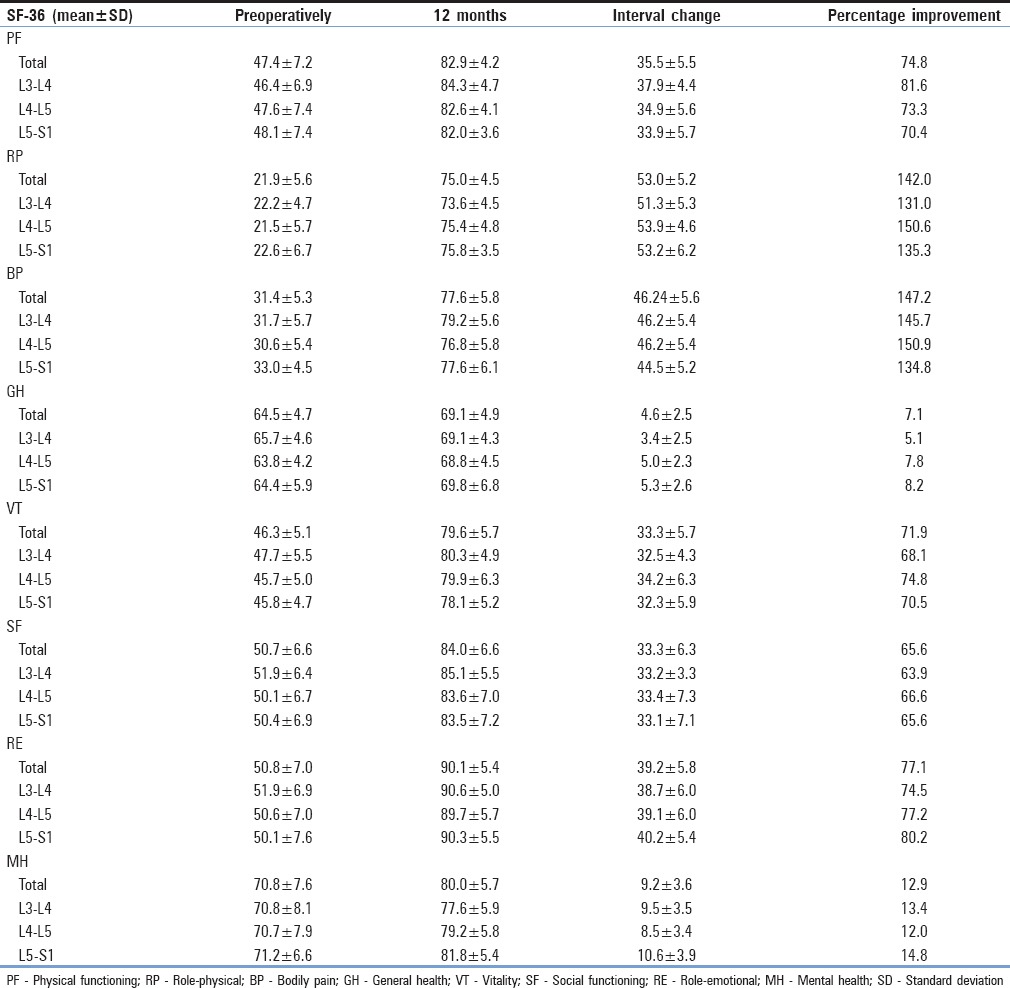
Student's t-test was used for quantitative-continuous variables and Wilcoxon signed-rank test for repeated measurements on a single sample (total number of patients, Group A, Group B, and Group C) to assess whether their mean ranks differ in each one of the eight aspects of SF-36 [Table 2].
Table 2.
Physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health values preoperatively and 1 year postsurgery, interval change and improvement percentage in the total of patients, in Groups A, B, and C
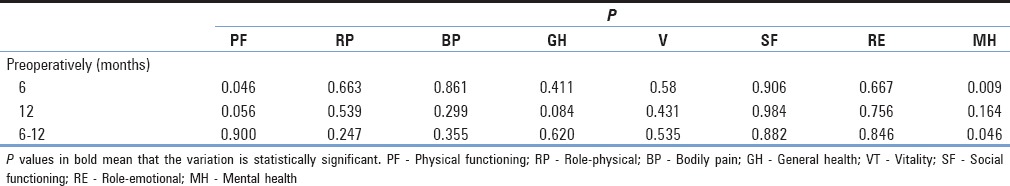
Kruskal–Wallis test or one-way ANOVA was used for the evaluation of the variation of the eight scores between two chronological phases depending on the level of operation (between the three groups-independent samples) [Table 3].
Table 3.
P values of the comparison of the variation of all social functioning-36 parameters preoperatively-6 months, preoperatively-12 months, and 6-12-month intervals, between Groups A, B, and C
SF-36 measures were assessed preoperatively and at 6 weeks, 3 months, 6 months, and 1 year postsurgery. We searched for any statistical important difference at the eight scores of SF-36 between two chronological phases in the total number of patients, in each group and between groups.
Results
The increase in all the eight scores of SF-36 after 1-year follow-up was statistically significantly important (P ≤ 0.05) in the total number of patients and in each group separately [Table 2].
Physical function (PF), bodily pain (BP), vitality (VT), social function (SF), and emotional function (RE) scores were higher in every visit for all the three groups, but the variation between groups was not significant (P > 0.05) [Table 3].
Group A (L3–L4) had a significant higher increase of physical function (PF) score in 3 months (P = 0.046) and 12 months (P = 0.056) postsurgery and in the interval 6 weeks–12 months (P = 0.041) compared with the other two groups [Table 3 and Figure 3].
Figure 3.
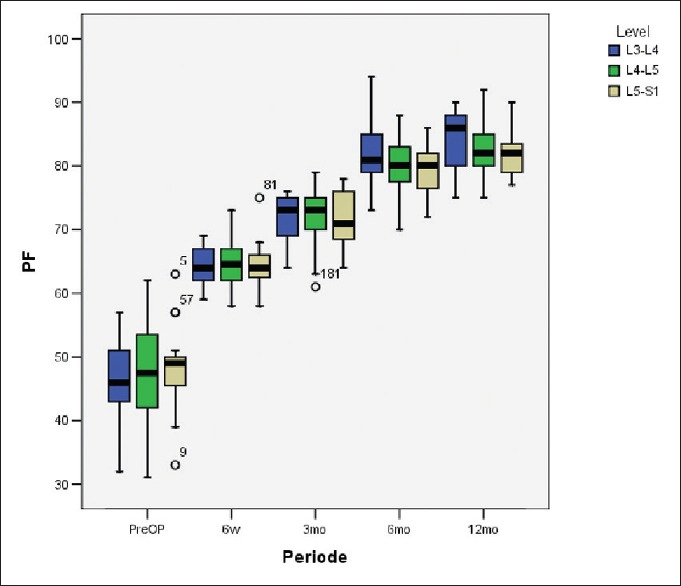
Box plot with physical functioning values of Groups A, B, and C preoperatively, in 6 weeks and in 3, 6, and 12 months postsurgery. Pre-op: Preoperatively, PF: Physical functioning
Group B (L4–L5) had a statistical significant increase of general health (GH) score in the interval 3–12 months (P = 0.006) compared with the other two groups.
Group B (L4–L5) had a significant lower increase of mental health (MH) score in 6 months (P = 0.009) and in the interval 6 weeks–6 months in comparison with the other two groups, and Group A (L3–L4) had a significant lower increase of MH score in the interval 6–12 months (P = 0.046) [Table 3].
At the end of the follow-up, PF, RP, BP, GH, VT, SF, RE, and MH scores in the total number of patients were improved by 74.8%, 142.0%, 147.2%, 7.1%, 71.9%, 65.6%, 77.1%, and 12.9%, respectively [Table 2].
Discussion
Lumbar disc herniation is a very common condition that leads to the compression of the corresponding nerve roots, local pain, and in some cases sciatica.[4] The pathophysiology of the disease is connected to the intervertebral disc degeneration. The exact pathophysiologic mechanism remains unknown and multifactorial. Factors such as the migration of the herniated nucleus pulposus tissue, the complex interactions among the nucleus pulposus, the dural sac and the nerve roots, the changes of microcirculation and the inflammation of the herniated nucleus pulposus tissue, the hyperosteogeny at the corresponding segment of the lumbar vertebrae, and the posture changes seem to play a significant role.[6,20]
TPED is a minimally invasive spinal surgical technique that can be operated under local anesthesia and mild sedation and has numerous advantages compared to other types of spinal surgeries, including direct visualization of the intervertebral space, preservation of the bony structures, ligaments and dorsal muscles, less paravertebral muscle damage, reduced recovery time and hospital stay.[14,15,16,21] The technique was first introduced by Hijikata with the name percutaneous nucleotomy.[22] Kambin[23], who was also a pioneer of this method, Schreiber, and Leu improved the method by using an endoscope or arthroscope in the transforaminal approach. After decades of application, nowadays, TPED is a spinal surgery technique with multiple advantages, especially in single-level herniations.[23,24,25]
Despite the existence of studies on TPED for lumbar herniated disc and HRQoL, none of them has commented on specific factors, related to the technique itself (such as the level of operation) that could independently affect the progress of HRQoL after the procedure.[26] Taking into consideration, that TPED preserves the biomechanics of the lumbar spine, including the soft tissues and the bony structures, and offers stability to the operated and adjacent levels due to the smaller traumatization of the supportive paraspinal tissues, TPED is theoretically associated with many advantages despite the operated level. However, it is critical to understand if the anatomy of the disc pathology and its relation to adjacent structures, as defined by the level of operation, has an independent effect on the success of the procedure and HRQoL 1 year postoperatively.[27]
Knowledge of the anatomy of the operated level could explain some of the results of our study and support the idea that HRQoL could differ among patients subjected to TPED for lumbar disc herniation at different intervertebral levels. Limitations of the spinal anatomy constitute that the transforaminal approach is very useful at levels higher than L4–L5, because at higher lumbar levels, the foramen is larger. On the other hand, at the L5–S1 lumbar segment, the transforaminal approach is not the preferable type of spinal surgery. Anatomical obstacles, such as the iliac wings, frequently block the approach and necessitate a steeper and endoscope insertion under vertical angulation. Nevertheless, the transverse processes are larger at the L5 vertebral level, and consequently, the foraminal space is too narrowed for the insertion of the endoscope into the safety zone.[26] As stated above, the anatomy of the lower lumbar levels makes it difficult and dangerous to manipulate the endoscope in the intervertebral disc space and through the transforaminal route. Hence, the endoscopic interlaminar approach is more frequently used effectively in L5–S1 disc herniation rather than the transforaminal approach.[26] All these data give an explanation on why patients from Group A have a significant higher increase in the PF score 1 year after surgery, compared to the other two groups.
Assessing HRQoL is a complex procedure and it should not only include the assessment of PF as the disability of those patients influences their social and mental health, and other domains of their daily routine. The SF-36 health survey questionnaire is a questionnaire which assesses eight domains of health-related functions, which reflect the conception of the GH symptoms or damage, restrictions on activities and participation.[28] In other words, SF-36 facilitates the global evaluation of our patients' health and this is the reason we have chosen this type of questionnaire.
The independent effect of the operated level on HRQoL following TPED is a rational way to export conclusions on the anatomic limitations and particularities of the endoscopic technique. Our results add to our limited knowledge on the anatomical burdens of TPED and enlighten specific considerations of the technique, posed by the local anatomy. More studies are expected to further investigate the clinical significance of our statistical analysis and more strictly define the indications–contradictions of TPED, to assist clinical practice for spinal surgeons.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Nikoobakht M, Yekanineajd MS, Pakpour AH, Gerszten PC, Kasch R. Plasma disc decompression compared to physiotherapy for symptomatic contained lumbar disc herniation: A prospective randomized controlled trial. Neurol Neurochir Pol. 2016;50:24–30. doi: 10.1016/j.pjnns.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 2.Shaikh M, Östör AJ. Evaluating the patient with low back pain. Practitioner. 2015;259:21. [PubMed] [Google Scholar]
- 3.Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354:581–5. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 4.Wang HQ, Samartzis D. Clarifying the nomenclature of intervertebral disc degeneration and displacement: From bench to bedside. Int J Clin Exp Pathol. 2014;7:1293–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Picavet HS, Hazes JM. Prevalence of self reported musculoskeletal diseases is high. Ann Rheum Dis. 2003;62:644–50. doi: 10.1136/ard.62.7.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu XX, Liu LM. Progress on the cause and mechanism of a separation of clinical symptoms and signs and imaging features in lumbar disk herniation. Zhongguo Gu Shang. 2015;28:970–5. [PubMed] [Google Scholar]
- 7.Hestbaek L, Leboeuf-Yde C, Manniche C. Low back pain: What is the long-term course? A review of studies of general patient populations. Eur Spine J. 2003;12:149–65. doi: 10.1007/s00586-002-0508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manchikanti L, Falco FJ, Pampati V, Cash KA, Benyamin RM, Hirsch JA. Cost utility analysis of caudal epidural injections in the treatment of lumbar disc herniation, axial or discogenic low back pain, central spinal stenosis, and post lumbar surgery syndrome. Pain Physician. 2013;16:E129–43. [PubMed] [Google Scholar]
- 9.Gregory DS, Seto CK, Wortley GC, Shugart CM. Acute lumbar disk pain: Navigating evaluation and treatment choices. Am Fam Physician. 2008;78:835–42. [PubMed] [Google Scholar]
- 10.Weinstein JN, Lurie JD, Tosteson TD, Skinner JS, Hanscom B, Tosteson AN, et al. Surgical vs. nonoperative treatment for lumbar disk herniation: The Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296:2451–9. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mixter W, Barr J. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med. 1934;211:210–5. [Google Scholar]
- 12.Postacchini F, Postacchini R. Operative management of lumbar disc herniation: The evolution of knowledge and surgical techniques in the last century. Acta Neurochir Suppl. 2011;108:17–21. doi: 10.1007/978-3-211-99370-5_4. [DOI] [PubMed] [Google Scholar]
- 13.Brayda-Bruno M, Cinnella P. Posterior endoscopic discectomy (and other procedures) Eur Spine J. 2000;9(Suppl 1):S24–9. doi: 10.1007/PL00010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mayer HM, Brock M. Percutaneous endoscopic lumbar discectomy (PELD) Neurosurg Rev. 1993;16:115–20. doi: 10.1007/BF00258242. [DOI] [PubMed] [Google Scholar]
- 15.Mathews HH. Transforaminal endoscopic microdiscectomy. Neurosurg Clin N Am. 1996;7:59–63. [PubMed] [Google Scholar]
- 16.Yeung AT, Yeung CA. Minimally invasive techniques for the management of lumbar disc herniation. Orthop Clin North Am. 2007;38:363–72. doi: 10.1016/j.ocl.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 17.Schoenfeld AJ, Weiner BK. Treatment of lumbar disc herniation: Evidence-based practice. Int J Gen Med. 2010;3:209–14. doi: 10.2147/ijgm.s12270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kambin P, Gellman H. Percutaneous lateral discectomy of the lumbar spine A preliminary report. Clin Orthop. 1983;174:127–32. [Google Scholar]
- 19.Wang S, Fan W, Yu W, Li J, Xu D, Cao H, et al. Analysis on reliability and validity of SF-36 scale in urban residents. Zhonghua Liu Xing Bing Xue Za Zhi. 2016;37:344–7. doi: 10.3760/cma.j.issn.0254-6450.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Petit A, Roquelaure Y. Low back pain, intervertebral disc and occupational diseases. Int J Occup Saf Ergon. 2015;21:15–9. doi: 10.1080/10803548.2015.1017940. [DOI] [PubMed] [Google Scholar]
- 21.Yamashita K, Higashino K, Sakai T, Takata Y, Abe M, Morimoto M, et al. Revision percutaneous endoscopic lumbar discectomy under the local anesthesia for the recurrent lumbar herniated nucleus pulposus in a high class athlete: A case report. J Med Invest. 2016;63:135–9. doi: 10.2152/jmi.63.135. [DOI] [PubMed] [Google Scholar]
- 22.Hijikata S. Percutaneous nucleotomy. A new concept technique and 12 years' experience. Clin Orthop Relat Res. 1989;238:9–23. [PubMed] [Google Scholar]
- 23.Kambin P. Arthroscopic microdiscectomy. Arthroscopy. 1992;8:287–95. doi: 10.1016/0749-8063(92)90058-j. [DOI] [PubMed] [Google Scholar]
- 24.Schreiber A, Leu H. Percutaneous nucleotomy: Technique with discoscopy. Orthopedics. 1991;14:439–44. doi: 10.3928/0147-7447-19910401-07. [DOI] [PubMed] [Google Scholar]
- 25.Türk CÇ, Kara NN, Biliciler B, Karasoy M. Clinical outcomes and efficacy of transforaminal lumbar endoscopic discectomy. J Neurosci Rural Pract. 2015;6:344–8. doi: 10.4103/0976-3147.154575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim HS, Ju CI, Kim SW, Kim JG, Lee SM, Kim BW. Minimally invasive percutaneous endoscopic 2 levels adjacent lumbar discectomy through 1 portal skin incision: Preliminary study. Asian J Neurosurg. 2015;10:95–101. doi: 10.4103/1793-5482.154977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsou PM, Yeung AT. Transforaminal endoscopic decompression for radiculopathy secondary to intracanal noncontained lumbar disc herniations: Outcome and technique. Spine J. 2002;2:41–8. doi: 10.1016/s1529-9430(01)00153-x. [DOI] [PubMed] [Google Scholar]
- 28.Chwastiak LA, Von Korff M. Disability in depression and back pain: Evaluation of the World Health Organization Disability Assessment Schedule (WHO DAS II) in a primary care setting. J Clin Epidemiol. 2003;56:507–14. doi: 10.1016/s0895-4356(03)00051-9. [DOI] [PubMed] [Google Scholar]


