Abstract
Objective
The purpose of this study was to examine how emotion dysregulation (ED) might help explain the relationship between posttraumatic stress disorder (PTSD) and alcohol dependence (AD) symptoms in females.
Method
Participants included 260 women from primary, diabetes, and gynecological clinics of an urban public hospital. This is a primarily African American sample (96.9%), including individuals reporting exposure to at least 1 traumatic event. We examined the associations and predictability patterns between severity of PTSD symptoms, ED, and AD symptoms.
Results
Using linear regression analyses, PTSD avoidance and numbing symptoms and ED were significant predictors of AD symptoms. When looking at specific dimensions of ED, one's inability to engage in goal‐directed behavior under strong emotional influences showed a full indirect effect on the relationship between PTSD avoidance and numbing symptoms and AD symptoms.
Conclusion
Our findings suggest that having poor emotion regulation skills may help explain why females with PTSD become dependent on alcohol.
Keywords: emotion dysregulation, PTSD, alcohol dependence, traumatized population, women
In the general population, approximately 6%–8% of individuals suffer from posttraumatic stress disorder (PTSD; Kessler, Berglund, et al., 2005). In urban, low socioeconomic populations, that rate is significantly higher, with lifetime prevalence estimates of PTSD closer to 40%–50% (Alim et al., 2006; Gillespie et al., 2009; Schwartz, Bradley, Sexton, Sherry, & Ressler, 2005). Rates of PTSD are also higher in females than in males, so traumatized women may be a particularly important group to study with regard to negative outcomes (Alim et al., 2006; Breslau, David, Andreski, & Peterson, 1997; Gillespie et al., 2009; McLean, Asnaani, Litz, & Hofmann, 2011). Using the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition Text Revision (DSM‐IV‐TR; American Psychological Association, 2000) diagnostic criteria, there are three symptom clusters of PTSD, including reexperiencing (Criterion B), avoidance and numbing (Criterion C), and hyperarousal (Criterion D) symptoms. There is significant diversity in symptom presentation and the number of combinations of symptoms that might occur for individuals with PTSD. Different symptoms may relate to distinct functional problems or other psychiatric conditions.
One major problem to consider is the high rates of comorbid alcohol use disorders (i.e., alcohol abuse and dependence) among individuals with PTSD. The positive association between alcohol use disorder and PTSD and the prevalence of comorbidity are well established in the literature (e.g., Kessler, Chiu, Demler, & Walters, 2005; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; McFarlane, 1998; Stewart, Pihl, Conrod, & Dongier, 1998). The association with alcohol dependence (AD) may be particularly strong for avoidance and numbing and hyperarousal PTSD symptom clusters (see Debell et al., 2014, for a review). Some evidence suggests that PTSD is more likely to precede the onset of AD in women (Sonne, Back, Zuniga, Randall, & Brady, 2003). Moreover, there have been a number of longitudinal studies suggesting direct and temporal relationships between trauma exposure, the onset of PTSD symptoms, and the later development of alcohol use disorders (see Khantzian, 1997 and Stewart et al., 1998, for review; Cheng & Mallinckrodt, 2015; Haller & Chassin, 2014; Kline et al., 2014; Nickerson et al., 2014).
There is strong evidence for an emotional component underlying the relationship between PTSD and AD. For instance, when compared to individuals without PTSD, those with PTSD are more likely to use alcohol when confronted with negative situations and emotions (Khantzian, 1997; Waldrop, Back, Verduin, & Brady, 2007). Turning to alcohol in these highly emotional contexts may be an avoidance mechanism (Brady, Back, & Coffey, 2004). Therefore, one construct through which the link between PTSD and AD may be understood is emotion dysregulation (ED). ED–the inability to properly regulate one's emotions–is a complex construct that represents how individuals might experience and have difficulty managing strong emotions.
ED is associated with many negative mental health outcomes, including both PTSD and AD (Bonn‐Miller, Vujanovic, & Zvolensky, 2008; Bradley et al., 2011; Dvorak et al., 2014; Lilly & Lim, 2013; Tull, Barrett, McMillan, & Roemer, 2007; Weiss, Tull, Davis, et al., 2012). Studies have shown that ED is related to both the development and the severity of posttraumatic stress symptoms, across all three symptom clusters (Bradley et al., 2011; Lilly & Lim, 2013; Tull et al., 2007; Weiss, Tull, Davis, et al., 2012; Weiss, Tull, Viana, Anestis, & Gratz, 2012). Some studies have examined associations between specific dimensions of ED and PTSD symptom clusters, finding that all PTSD symptom clusters are significantly positively correlated with most ED dimensions (with exceptions involving difficulties with awareness and clarity of emotions; Tull et al., 2007; Weiss, Tull, Davis, et al., 2012). The literature also sheds light on the role of ED in alcohol use behaviors and consequences, especially in traumatized or PTSD populations (Bradley et al., 2011; Weiss, Tull, Anestis, & Gratz, 2013; Weiss, Tull, Viana et al., 2012).
While the avoidance and numbing symptom cluster of PTSD is defined in part by the avoidance of trauma triggers, individuals with greater Criterion C symptom severity may have more generalized underlying avoidance problems. Avoiding negative emotions is a maladaptive emotion regulation strategy, as these behaviors seek to discard negative emotions rather than processing and modulating them. In fact, individuals with PTSD often describe alcohol as a common avoidance strategy used to control emotions (Hayes, Wilson, Gifford, Follette, & Strosahl, 1996; Khantzian, 1997).
Although several studies have shown associations between PTSD, AD, and ED, we are unaware of any that examine whether ED helps to explain the relationship between PTSD and AD symptoms in a nonclinical, civilian sample of highly traumatized women. Furthermore, many studies did not examine differential associations across ED and the three PTSD symptom clusters in relation to AD, and there remains a great deal to be understood about these specific associations. Therefore, differences across PTSD symptom clusters and ED dimensions in relation to AD symptoms will be examined. The goal of the present study is to fill this gap in the literature by examining the associations between PTSD symptoms, ED dimensions, and AD symptoms. We will focus on an urban civilian population of females in which rates of trauma exposure and PTSD symptoms are high (Gillespie et al., 2009). We hypothesize that ED will have an indirect effect on the relationship between PTSD symptoms and AD symptoms.
Method
Procedure
Participants were drawn from a National Institute of Mental Health‐funded study of risk factors for the development of PTSD in a low socioeconomic, primarily African American urban population. Participants were recruited from waiting rooms in the diabetes, gynecology, and primary care medical (nonpsychiatric) clinics at Grady Memorial Hospital, a publicly funded hospital in Atlanta, Georgia. Interviewers approached participants waiting for appointments. To be eligible for participation, subjects had to be at least 18 years old and able to give informed consent. The investigation was carried out in accordance with the latest version of the Declaration of Helsinki and informed consent of the participants was obtained after the nature of the procedures had been fully explained.
After signing the informed consent approved by the Emory Institutional Review Board, an initial interview was administered with questionnaires regarding trauma history and psychological variables. Trained research assistants administered this interview by reading each question aloud to participants; interviews took 45–75 minutes to complete (duration largely dependent on the participant's trauma history and symptoms). A more detailed and comprehensive assessment of psychological functioning was conducted in an associated study, which included a subset of participants who completed the initial assessment (see Gillespie et al., 2009, for full details regarding study procedures).
Participants
The current study includes 260 females with a mean age of 39.76 years (standard deviation [SD] = 11.73 years) who completed both the initial and secondary assessments. The majority of the participants self‐identified as African American (96.9%, n = 252). The remaining ethnicities represented included Caucasian (1.1%, n = 3) and Mixed or Other (2.0%, n = 5). This was a highly traumatized sample, with all participants reporting the experience of at least one type of trauma in their lifetime (mean [M] = 4.97, SD = 2.96).
Measures
Difficulties in Emotion Regulation Scale (DERS)
The DERS (Gratz & Roemer, 2004) is a psychometrically validated, self‐report, 36‐item measure of emotion regulation difficulties. It measures several aspects of emotion regulation, including awareness and understanding of one's emotions, acceptance of negative emotions, the ability to successfully engage in goal‐directed behavior and control impulsive behavior when experiencing negative emotions, and the ability to use situationally appropriate emotion regulation strategies. For the present study, the overall scale and six subscales of emotion regulation were examined. The internal consistency of the DERS total scale was high (α = 0.92).
Clinician‐Administered PTSD Scale
(CAPS). The CAPS is an interviewer‐administered, psychometrically validated diagnostic instrument measuring PTSD (Blake et al., 1990, 1995). It includes items that rate social and occupational functioning, global PTSD symptom severity, and the validity of a participant's responses. The CAPS assesses current PTSD and yields a continuous measure of the severity of overall PTSD and the three DSM‐IV‐TR symptom clusters (i.e., reexperiencing, avoidance and numbing, and arousal, or Criterion B, C, and D, respectively). The frequency and intensity scores for each of the 17 diagnostic criteria are summed to arrive at a total severity score, and each criterion also has a total severity score based on the individual items for the respective criterion (five for Criterion B, seven for Criterion C, and five for Criterion D).
MINI International Neuropsychiatric Interview
The MINI (Sheehan et al., 1998) is a structured diagnostic interview that assesses mood, anxiety, substance use, and psychotic disorders based on DSM‐IV‐TR criteria. The MINI has shown good reliability and validity across different samples (Lecrubier et al., 1997; Sheehan et al., 1997). For the present study, only the current AD section was used. Within our sample, 24.2% (n = 63) affirmed to drinking three or more alcoholic drinks in a 6‐hour period on three or more occasions within the past year, and 6.9% met full DSM‐IV criteria for AD. For all analyses, we created a continuous variable to measure AD in an effort to capture overall severity of AD symptoms.
Traumatic Events Inventory (TEI)
The TEI (Gillespie et al., 2009; Schwartz et al., 2005) is a 14‐item screening instrument for lifetime history of traumatic events witnessed or experienced. The TEI was used in this investigation to assess total number of types of traumas exposed to in one's lifetime; therefore, the types of traumatic events either witnessed or experienced were summed to obtain an overall trauma load score.
Statistical Analysis
The overall analytic approach was to examine the predictive utility of current PTSD symptoms and ED on reported AD symptoms. We first examined the distributions of all key predictor variables. The PTSD, trauma exposure, and ED variables were positively skewed. However, the level of skewness (range: 0.42–1.66) as well as the level of kurtosis (range: −0.63–1.43) in this sample fell within acceptable parameters for the sample size on all variables (Tabachnick & Fidell, 2000). Descriptive statistics of the sample and all variables of interest were computed and are presented in Table 1. Bivariate correlations among variables of interest are described in Table 2.
Table 1.
Descriptive Characteristics of Sample
| Mean (SD, range) | |
|---|---|
| Age | 39.76 (11.73, 18–64) |
| TEI Total | 4.97 (2.96, 1–14) |
| Alcohol dependence symptoms total (MINI) | 0.43 (1.18, 0–7) |
| DERS Total | 70.31 (23.03, 36–165) |
| Nonacceptance | 11.12 (5.22, 6–30) |
| Goals | 11.48 (4.71, 5–25) |
| Impulse | 10.88 (4.72, 6–30) |
| Awareness | 12.86 (4.82, 6–27) |
| Strategies | 14.53 (6.03, 8‐37) |
| Clarity | 9.46 (4.00, 5–23) |
| CAPS Total | 21.05 (24.44, 0–99) |
| Reexperiencing | 4.62 (7.13, 0–33) |
| Avoidance/numbing | 8.18 (10.55, 0–42) |
| Hyperarousal | 8.72 (9.49, 0–33) |
| N | 260 |
Note. SD = standard deviation; TEI = Traumatic Events Inventory; MINI = MINI International Neuropsychiatric Interview; DERS = Difficulties in Emotion Regulation Scale; CAPS = Clinician‐Administered PTSD Scale.
Table 2.
Bivariate Correlations Between Variables of Interest
| Current alcohol dependence | CAPS | CAPS | CAPS | ||
|---|---|---|---|---|---|
| symptom severity | Total | Criterion B | Criterion C | Criterion D | |
| CAPS total | 0.09 | — | — | — | — |
| Reexperiencing | 0.07 | — | — | — | — |
| Avoidance and numbing | 0.16* | — | — | — | — |
| Hyperarousal | 0.06 | — | — | — | — |
| DERS total | 0.37** | 0.39** | 0.25** | 0.45** | 0.33** |
| Nonacceptance | 0.23** | 0.41** | 0.27** | 0.43** | 0.38** |
| Goals | 0.34** | 0.25** | 0.16* | 0.30** | 0.21** |
| Impulse | 0.34** | 0.27** | 0.19** | 0.32** | 0.22** |
| Awareness | 0.23** | 0.18* | 0.08 | 0.24** | 0.15* |
| Strategies | 0.28** | 0.37** | 0.26** | 0.41** | 0.33** |
| Clarity | 0.34** | 0.31** | 0.20** | 0.39** | 0.25** |
Note. DERS = Difficulties in Emotion Regulation Scale; CAPS = Clinician‐Administered PTSD Scale.
*p ≤ 0.01. **p ≤ 0.001.
Then, based on the results of the correlational analyses, two hierarchical linear regression models were used to examine the unique predictive value of PTSD symptoms and ED (total and separated by the individual dimensions of ED) on AD symptoms. Both because it will provide a more nuanced understanding of associations between variables and because results have differed by PTSD symptom cluster in previous research (Debell et al., 2014; Saladin, Brady, Dansky, & Kilpatrick, 1995), we analyzed the three symptom clusters of PTSD separately. Because research has shown that rates of AD vary by age and trauma exposure (Kessler, Berglund, et al., 2005; Turner & Lloyd, 1995), these variables were included as covariates in analyses.
Finally, mediation analyses were performed with INDIRECT (Preacher & Hayes, 2008) for SPSS to test whether ED had an indirect effect on the relationship between current avoidance and numbing PTSD symptoms and AD symptoms. Bootstrapping with 95% confidence intervals (CIs) was used to determine significance of mediation effects. Bootstrapping is a particularly useful method for interpreting mediation analyses because it does not assume that sampling distributions of the indirect effects are normally distributed (Preacher & Hayes, 2008). Again, age and lifetime trauma were included as covariates in the INDIRECT analysis. Reexperiencing and hyperarousal symptoms were also controlled for in an effort to determine the specific association between avoidance and numbing and AD symptoms.
Results
To determine the extent of association between our predictor variables and current AD symptoms, we first calculated Pearson correlation coefficients. As shown in Table 2, of the current PTSD variables measured, only PTSD symptom cluster C (avoidance and numbing) was significantly positively correlated with current AD symptoms (p < 0.01). Total ED and all six dimensions of ED measured by the DERS also were significantly positively correlated with current AD symptoms (p ≤ 0.001). Furthermore, overall ED and all six dimensions of ED were significantly correlated with each PTSD symptom cluster (p < 0.01), except for a nonsignificant association between lack of emotional awareness and PTSD symptom cluster B.
A hierarchical linear regression model was first run to test the differential associations of PTSD symptoms and ED with current AD symptoms. Age and overall trauma load were entered in the first step of each regression as covariates. As shown in Table 3, when the three PTSD symptom clusters were entered into the second step of the regression model, they were significantly predictive of AD symptoms (p < 0.05). Of the three symptom clusters included in the model, only avoidance and numbing symptoms were predictive (p < 0.01) of AD symptoms above and beyond the effects of age and trauma load. When overall ED was included in the model in step 3, the effect of avoidance and numbing symptoms was no longer significant. Overall, ED was significantly predictive of AD symptoms (p < 0.001), suggesting that ED may mediate the relationship between avoidance and numbing symptoms of PTSD and current AD symptoms. Age and trauma exposure were not significantly predictive of AD symptoms at any step.
Table 3.
Linear Regression Model Predicting Current Alcohol Dependence Symptom Severity From Current PTSD Symptoms and Overall ED
| β | t | p | R | R2 change | F change | p change | |
|---|---|---|---|---|---|---|---|
| Step 1 | 0.11 | 0.01 | 1.59 | 0.21 | |||
| Age | −0.003 | −0.44 | 0.66 | ||||
| TEI | 0.04 | 1.75 | 0.08 | ||||
| Step 2 | 0.22 | 0.03 | 3.01 | 0.03* | |||
| Age | −0.002 | −0.24 | 0.81 | ||||
| TEI | 0.03 | 1.22 | 0.22 | ||||
| Reexperiencing | −0.01 | −0.52 | 0.60 | ||||
| Avoidance and numbing | 0.04 | 2.90 | 0.004** | ||||
| Hyperarousal | −0.02 | −1.62 | 0.11 | ||||
| Step 3 | 0.39 | 0.11 | 31.21 | <0.001*** | |||
| Age | −0.001 | −0.16 | 0.88 | ||||
| TEI | 0.02 | 0.74 | 0.46 | ||||
| Reexperiencing | 0.001 | 0.06 | 0.95 | ||||
| Avoidance and numbing | 0.01 | 1.08 | 0.28 | ||||
| Hyperarousal | −0.02 | −1.66 | 0.10 | ||||
| DERS total | 0.02 | 5.59 | <0.001*** |
Note. PTSD = posttraumatic stress disorder; ED = emotion dysregulation; TEI = Traumatic Events Inventory; DERS = Difficulties in Emotion Regulation Scale.
* p ≤ 0.05. ** p ≤ 0.01. *** p ≤ 0.001.
We also examined the effects of the six dimensions of ED independently to determine if there were differential effects (see Table 4). Each dimension was included in the regression model together. Similar results emerged in step 2 of this model; more specifically, only avoidance and numbing symptoms were significantly predictive of AD symptoms (p < 0.01). In step 3, ED dimensions were significantly predictive of current AD symptoms, accounting for 14% of additional variance in explaining alcohol symptoms independent of age, trauma exposure, and current PTSD symptoms. As shown in Table 4, the only ED dimension significant at step 3 was difficulty with goal directed behavior in the presence of strong emotions after controlling for the effects of age, trauma exposure, PTSD symptoms, and the other dimensions of ED. Again, avoidance and numbing PTSD symptoms were no longer significant when ED dimensions were included in the model, suggesting a potential mediation effect.
Table 4.
Linear Regression Model Predicting Current Alcohol Dependence Symptom Severity From Current PTSD Symptoms and the Six Dimensions of ED
| β | t | p | R | R2 change | F change | p change | |
|---|---|---|---|---|---|---|---|
| Step 1 | 0.11 | 0.01 | 1.59 | 0.21 | |||
| Age | −0.003 | −0.44 | 0.66 | ||||
| TEI | 0.04 | 1.75 | 0.08 | ||||
| Step 2 | 0.22 | 0.03 | 3.01 | 0.03* | |||
| Age | −0.002 | −0.24 | 0.81 | ||||
| TEI | 0.03 | 1.22 | 0.22 | ||||
| Reexperiencing | −0.01 | −0.52 | 0.60 | ||||
| Avoidance and numbing | 0.04 | 2.90 | 0.004*** | ||||
| Hyperarousal | −0.02 | −1.62 | 0.11 | ||||
| Step 3 | 0.42 | 0.13 | 6.50 | <0.001*** | |||
| Age | −0.001 | −0.10 | 0.92 | ||||
| TEI | 0.02 | 0.61 | 0.54 | ||||
| Reexperiencing | 0.001 | 0.10 | 0.92 | ||||
| Avoidance and numbing | 0.01 | 0.94 | 0.35 | ||||
| Hyperarousal | −0.02 | −1.26 | 0.21 | ||||
| Nonacceptance | 0.001 | 0.05 | 0.97 | ||||
| Goals | 0.05 | 2.29 | 0.02* | ||||
| Impulse | 0.04 | 1.52 | 0.13 | ||||
| Awareness | 0.02 | 0.91 | 0.36 | ||||
| Strategies | −0.02 | −0.88 | 0.38 | ||||
| Clarity | 0.05 | 1.92 | 0.06 |
Note. PTSD = posttraumatic stress disorder; ED = emotion dysregulation; TEI = Traumatic Events Inventory; DERS = Difficulties in Emotion Regulation Scale.
* p ≤ 0.05. ** p ≤ 0.01. *** p ≤ 0.001.
We used Preacher and Hayes’ (2008) INDIRECT to formally test the mediation model suggested by the linear regression analyses. Age, trauma load, and CAPS subscales for reexperiencing symptoms (Criterion B) and hyperarousal symptoms (Criterion D) were entered in the model as covariates. As shown in Figure 1, overall ED showed a full indirect effect on the relationship between avoidance and numbing PTSD symptoms and current AD symptoms (overall model: R2 = 0.15, F = 7.49, p < 0.001; bias corrected 95% CI [0.01, 0.04]). A similar full indirect effect was found when running the mediation model using the difficulty with goal‐directed behavior dimension of the DERS (overall model: R2 = 0.13, F = 6.42, p < 0.001; bias corrected 95% CI [0.01, 0.03]). Again, age, trauma load, and CAPS subscales for reexperiencing symptoms (Criterion B) and hyperarousal symptoms (Criterion D) were entered in the model as covariates and none of the covariates were significant.
Figure 1.
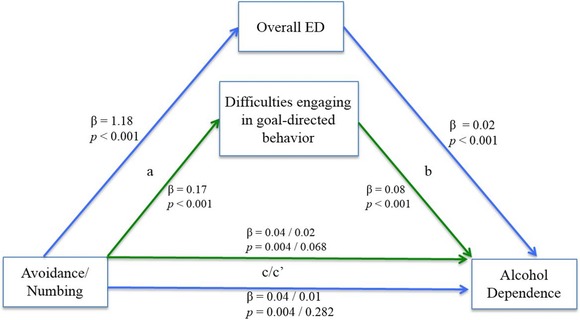
The full indirect effects of overall emotion dysregulation and difficulties engaging in goal‐directed behavior on the relation between current avoidance and numbing PTSD symptoms and current alcohol dependence symptoms in females.Note. Age, trauma exposure, reexperiencing, and hyperarousal PTSD symptoms were controlled.
Discussion
In support of previous research (e.g., Brady et al., 2004; Kessler et al., 1995; Kessler, Chiu, et al., 2005; McFarlane, 1998; Stewart et al., 1998; Swendsen et al., 2010), we found a significant association between PTSD symptoms and AD symptoms in this sample of urban, minority females. When examining the specific PTSD symptom clusters, only avoidance and numbing PTSD symptoms were significantly correlated to AD symptoms. Lifetime trauma load was not significantly related to AD, suggesting that within this sample it was not the number of traumatic events experienced but the presence of anxiety symptoms attributable to PTSD that contributed to AD. This adds to research suggesting that alcohol is used as an avoidance strategy in PTSD patients (Brady et al., 2004; Hayes et al., 1996) and highlights that trauma load itself may not increase risk for dependence, although it may increase risk for the development of PTSD which might then increase risk for alcohol use problems.
Our results also showed that all dimensions of ED were positively significantly correlated with AD, supporting previous findings that ED and AD are associated (Bonn‐Miller et al., 2008; Dvorak et al., 2014). Expanding previous research, we also found that ED had a full indirect effect on the relationship between current PTSD avoidance and numbing symptoms and current AD symptoms among traumatized females. Moreover, difficulties engaging in goal‐directed behaviors had an indirect effect on this relationship above and beyond the other dimensions of ED in this sample. These findings suggest that poor emotion regulation in general, and an inability to stay focused on goal‐directed behaviors when faced with strong emotions in particular, may help explain why women with PTSD are driven to AD. Individuals with PTSD may experience greater negative emotions, and if they do not have adequate emotion regulation capabilities, then they might use alcohol to avoid those negative emotions (Cooper, Russell, Skinner, Frone, & Mudar, 1992; Hayes et al., 1996; Khantzian, 1997; Stewart, Zvolensky, & Eifert, 2002; Tull et al., 2007). The specific use of alcohol as an avoidance strategy may help explain why there was only a significant association between AD symptoms and the avoidance and numbing symptom cluster, although that cannot be determined from the current study based on its cross‐sectional nature.
It is unclear why having difficulties with goal‐directed behaviors in the presence of strong emotions in particular was related to AD in these women. One possibility is that if negative emotions repeatedly resurface while attempting to focus and engage in goal‐directed behavior, then women with a tendency to try to control rather than modulate emotions may choose alcohol as a way to numb themselves from the negative situation. This behavior pattern would be analogous to the self‐medication theory, whereby individuals suffering from PTSD turn to alcohol abuse as a way to avoid fearful memories and to dampen negative emotions brought on by those memories (Brady et al., 2004; Khoury, Tang, Bradley, Cubells, & Ressler, 2010; Leeies, Pagura, Sareen, & Bolton, 2010; Quitkin, Rifkin, Kaplan, & Klein, 1972; Read, Merrill, Griffin, Bachrach, & Khan, 2014).
Self‐medicating with alcohol among women with PTSD may involve ED processes. Lehavot, Stappenbeck, Luterek, Kaysen, and Simpson (2014) found that coping motives (i.e., drinking to avoid negative affect) were associated with amount of alcohol use in women. Additional research is needed to determine how in fact ED does relate to the self‐medication theory in traumatized females with PTSD. Future studies of urban females suffering from PTSD would benefit from including direct measures of self‐medication and drinking motives in addition to ED dimensions to further delineate how these constructs are interrelated with each other and with alcohol problems.
The results of this study provide further support for targeting emotion regulation skills in therapy for traumatized individuals. Interventions for individuals suffering from PTSD and AD symptoms should be broad enough to support the needs of comorbidities and underlying areas of dysfunction (e.g., ED). The most common and effective therapy for PTSD treatment is prolonged exposure therapy (see Mørkved et al., 2014, for review). While early studies warned against antagonistic effects of exposure therapy in people with comorbid addiction disorders (e.g., Becker, Zayfert, & Anderson, 2004; Pitman et al., 1991), studies that are more recent have shown successful treatment in populations with comorbid PTSD and AD using various types of exposure therapy (e.g., Berenz, Rowe, Schumacher, Stasiewicz, & Coffey, 2012; Nosen, Littlefield, Schumacher, Stasiewicz, & Coffey, 2014). It is possible that targeting emotion regulation skills in addition to trauma‐focused treatment would be beneficial for traumatized females.
Theoretically, improving emotion regulation abilities in women suffering from PTSD and AD may lessen AD symptoms, allowing for a more successful intervention of PTSD symptoms later in treatment. This has been shown in other populations, such as those with exposure to childhood sexual abuse (Cloitre, Koenen, Cohen, & Han, 2002; Cloitre, Stovall‐McClough, Miranda, & Chemtob, 2004), and researchers should continue to examine how best to incorporate emotion regulation training into treatment protocols.
Limitations
There are several noteworthy limitations of this study. First is the cross‐sectional design of our study. We cannot say for certain that the onset of PTSD and ED symptoms preceded the onset of AD symptoms in every participant, and therefore we cannot determine directional causality. Prospective, longitudinal studies are required to examine the temporal onset of ED, PTSD, and AD symptoms. Also, although the DERS is a validated measure of ED, it is inherently biased by its self‐report nature. Finally, our sample was largely low‐income African American females, which limits the generalizability of our findings to other populations. However, this weakness is balanced by the public health importance of studying these variables in an often underresearched and underserved population with such high rates of trauma exposure as well as mental health problems.
Conclusion
This study contributes to the research on PTSD and AD comorbidity by identifying a potential underlying factor that may help explain this well‐established relationship. In a highly traumatized, low socioeconomic, urban sample of women, we found that ED had a full indirect effect on the association between avoidance and numbing PTSD symptoms and AD symptoms; therefore, ED may be an important component of what drives this relationship. The current findings provide support for growing literature suggesting the addition of therapeutic interventions for emotion regulation difficulties in traumatized patient populations, especially those with comorbid PTSD and AD.
Kerry J. Ressler is now at the Division of Depression and Anxiety at Harvard University.
This work was primarily supported by the National Institute of Mental Health (MH071537; MH102890) and the National Institute of Child Health and Human Development (HD071982). Support also included Emory and Grady Memorial Hospital General Clinical Research Center, NIH National Centers for Research Resources (M01 RR00039).
References
- Alim, T. N. , Graves, E. , Mellman, T. A. , Aigbogun, N. , Gray, E. , Lawson, W. , & Charney, D. S. (2006). Trauma exposure, posttraumatic stress disorder and depression in an African‐American primary care population. Journal of the National Medical Association, 98(10), 1630–1636. [PMC free article] [PubMed] [Google Scholar]
- Association American Psychological. (2000). Diagnostic and statistical manual of mental disorders‐IV‐TR. Washington, DC: American Psychological Association. [Google Scholar]
- Becker, C. B. , Zayfert, C. , Anderson, E. , (2004). A survey of psychologists‧ attitudes towards and utilization of exposure therapy for PTSD. Behaviour Research and Therapy, 42(3), 277–292. doi:10.1016/S0005-7967(03)00138‐4 [DOI] [PubMed] [Google Scholar]
- Berenz, E. C. , Rowe, L. , Schumacher, J. A. , Stasiewicz, P. R. , & Coffey, S. F. (2012). Prolonged exposure therapy for posttraumatic stress disorder among individuals in a residential substance use treatment program: A case series. Professional Psychology: Research and Practice, 43(2), 154–161. doi:10.1037/a0026138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake, D. D. , Weathers, F. W. , Nagy, L. M. , Kaloupek, D. G. , Klauminzer, G. , Charney, D. S. (1990). A clinician rating scale for assessing current lifetime PTSD: The CAPS‐1. Behavior Therapy, 13, 187–188. [Google Scholar]
- Blake, D. D. , Weathers, F. W. , Nagy, L. M. , Kaloupek, D. G. , Gusman, F. D. , Charney, D. S. , & Keane, T. M. (1995). The development of a clinician administered PTSD scale. Journal of Traumatic Stress, 8, 75–90. [DOI] [PubMed] [Google Scholar]
- Bonn‐Miller, M. O. , Vujanovic, A. A. , & Zvolensky, M. J. (2008). Emotional dysregulation: Association with coping‐oriented marijuana use motives among current marijuana users. Substance Use & Misuse, 43(11), 1653–1665. doi:10.1080/10826080802241292 [DOI] [PubMed] [Google Scholar]
- Bradley, B. , DeFife, J. A. , Guarnaccia, C. , Phifer, J. , Fani, N. , Ressler, K. J. , & Westen, D. (2011). Emotion dysregulation and negative affect: Association with psychiatric symptoms. Journal of Clinical Psychiatry, 72(5), 685–691. doi:10.4088/JCP.10m06409blu [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady, K. T. , Back, S. E. , & Coffey, S. F. (2004). Substance abuse and posttraumatic stress disorder. Current Directions In Psychological Science, 13(5), 206–209. doi:10.1111/j.0963-7214.2004.00309.x [Google Scholar]
- Breslau, N. , David, G. C. , Andreski, P. , & Peterson, E. L. (1997). Sex differences in posttraumatic stress disorder. Archives of General Psychiatry, 54, 1044–1048. [DOI] [PubMed] [Google Scholar]
- Cheng, H. , & Mallinckrodt, B. (2015). Racial/ethnic discrimination, posttraumatic stress symptoms, and alcohol problems in a longitudinal study of Hispanic/Latino college students. Journal of Counseling Psychology, 62(1), 38–49. doi:10.1037/cou0000052 [DOI] [PubMed] [Google Scholar]
- Cloitre, M. , Koenen, K. C. , Cohen, L. R. , & Han, H. (2002). Skills training in affective and interpersonal regulation followed by exposure: A phase‐based treatment for PTSD related to childhood abuse. Journal of Consulting and Clinical Psychology, 70(5), 1067–1074. doi:10.1037/0022-006X.70.5.1067 [DOI] [PubMed] [Google Scholar]
- Cloitre, M. , Stovall‐McClough, K. C. , Miranda, R. , & Chemtob, C. M. (2004). Therapeutic alliance, negative mood regulation, and treatment outcome in child abuse‐related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 72(3), 411–416. doi:10.1037/0022-006X.72.3.411 [DOI] [PubMed] [Google Scholar]
- Cooper, M. L. , Russell, M. , Skinner, J. B. , Frone, M. R. , & Mudar, P. (1992). Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. Journal Of Abnormal Psychology, 101(1), 139–152. doi:10.1037/0021-843X.101.1.139 [DOI] [PubMed] [Google Scholar]
- Debell, F. , Fear, N. T. , Head, M. , Batt‐Rawden, S. , Greenberg, N. , Wessely, S. , & Goodwin, L. (2014). A systematic review of the comorbidity between PTSD and alcohol misuse. Social psychiatry and psychiatric epidemiology, 49(9), 1401–1425. [DOI] [PubMed] [Google Scholar]
- Dvorak, R. D. , Sargent, E. M. , Kilwein, T. M. , Stevenson, B. L. , Kuvaas, N. J. , & Williams, T. J. (2014). Alcohol use and alcohol‐related consequences: Associations with emotion regulation difficulties. The American Journal of Drug and Alcohol Abuse, 40(2), 125–130. doi:10.3109/00952990.2013.877920 [DOI] [PubMed] [Google Scholar]
- Gillespie, C. F. , Bradley, B. , Mercer, K. , Smith, A. K. , Conneely, K. , Gapen, M. , &... Ressler, K. J. (2009). Trauma exposure and stress‐related disorders in inner city primary care patients. General Hospital Psychiatry, 31(6), 505–514. doi:10.1016/j.genhosppsych.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz, K. L. , & Roemer, L. (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. doi:10.1023/B:JOBA.0000007455.08539.94 [Google Scholar]
- Haller, M. , & Chassin, L. (2014). Risk pathways among traumatic stress, posttraumatic stress disorder symptoms, and alcohol and drug problems: A test of four hypotheses. Psychology of Addictive Behaviors, 28(3), 841–851. doi:10.1037/a0035878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, S. C. , Wilson, K. G. , Gifford, E. V. , Follette, V. M. , & Strosahl, K. (1996). Experiential avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64(6), 1152–1168. doi:10.1037/0022-006X.64.6.1152 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. , Berglund, P. , Demler, O. , Jin, R. , Merikangas, K. R. , & Walters, E. E. (2005). Lifetime prevalence and age‐of‐onset distributions of DSM‐IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. doi:10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- Kessler, R. C. , Chiu, W. T. , Demler, O. , & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12‐month DSM‐IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627. doi:10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C. , Sonnega, A. , Bromet, E. , Hughes, M. , & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048–1060. doi:10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- Khantzian, E. J. (1997). The self‐medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry, 4(5), 231–244. doi:10.3109/10673229709030550 [DOI] [PubMed] [Google Scholar]
- Khoury, L. , Tang, Y. L. , Bradley, B. , Cubells, J. F. , & Ressler, K. J. (2010). Substance use, childhood traumatic experience, and posttraumatic stress disorder in an urban civilian population. Depression and Anxiety, 27(12), 1077–1086. doi:10.1002/da.20751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline, A. , Weiner, M. D. , Ciccone, D. S. , Interian, A. , St. Hill, L. , & Losonczy, M. (2014). Increased risk of alcohol dependency in a cohort of National Guard troops with PTSD: A longitudinal study. Journal of Psychiatric Research, 50, 18–25. [DOI] [PubMed] [Google Scholar]
- Lecrubier Y, Sheehan D, Weiller, E ., Amorim, P. , Bonora, I. , Sheehan, K. H. , … Dunbar G. (1997). The Mini International Neuropsychiatric Interview (MINI): A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry, 12(5), 224–231. [Google Scholar]
- Leeies, M. , Pagura, J. , Sareen, J. , & Bolton, J. M. (2010). The use of alcohol and drugs to self‐medicate symptoms of posttraumatic stress disorder. Depression and Anxiety, 27(8), 731–736. [DOI] [PubMed] [Google Scholar]
- Lehavot, K. , Stappenbeck, C. A. , Luterek, J. A. , Kaysen, D. , & Simpson, T. L. (2014). Gender differences in relationships among PTSD severity, drinking motives, and alcohol use in a comorbid alcohol dependence and PTSD sample. Psychology of Addictive Behaviors, 28(1), 42–52. doi:10.1037/a0032266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lilly, M. M. , & Lim, B. (2013). Shared pathogeneses of posttrauma pathologies: Attachment, emotion regulation, and cognitions. Journal of Clinical Psychology, 69(7), 737–748. doi:10.1002/jclp.21934 [DOI] [PubMed] [Google Scholar]
- McFarlane, A. C. (1998). Epidemiological evidence about the relationship between PTSD and alcohol abuse: The nature of the association. Addictive Behaviors, 23(6), 813–826. doi:10.1016/S0306-4603(98)00098-7 [DOI] [PubMed] [Google Scholar]
- McLean, C. P. , Asnaani, A. , Litz, B. T. , & Hofmann, S. G. (2011). Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research, 45(8), 1027–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mørkved, N. , Hartmann, K. , Aarsheim, L. , Holen, D. , Milde, A. , Bomyea, J. , & Thorp, S. (2014). A comparison of narrative exposure therapy and prolonged exposure therapy for PTSD. Clinical Psychology Review, 34(6), 453–467. doi:10.1016/j.cpr.2014.06.005 [DOI] [PubMed] [Google Scholar]
- Nosen, E. , Littlefield, A. K. , Schumacher, J. A. , Stasiewicz, P. R. , & Coffey, S. F. (2014). Treatment of co‐occurring PTSD‐AUD: Effects of exposure‐based and non‐trauma focused psychotherapy on alcohol and trauma cue‐reactivity. Behaviour Research and Therapy, 61, 35–42. doi:10.1016/j.brat.2014.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickerson, A. , Barnes, J. B. , Creamer, M. , Forbes, D. , McFarlane, A. C. , O'Donnell, M. , &... Bryant, R. A. , (2014). The temporal relationship between posttraumatic stress disorder and problem alcohol use following traumatic injury. Journal of Abnormal Psychology, 123(4), 821–834. doi:10.1037/a0037920 [DOI] [PubMed] [Google Scholar]
- Pitman R.K., Altman,B. , Greenwald, E. , Longpre, R.E. , Macklin, M.L. , Poire, R.E. , & Steketee, G.S. , (1991). Psychiatric complications during flooding therapy for posttraumatic stress disorder. Journal of Clinical Psychiatry, 52(1), 17–20. [PubMed] [Google Scholar]
- Preacher, K. J. , & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. doi:10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Quitkin, F. M. , Rifkin, A. , Kaplan, J. , & Klein, D. F. (1972). Phobic anxiety syndrome complicated by drug dependence and addiction: A treatable form of drug abuse. Archives of General Psychiatry, 27(2), 159–162. [DOI] [PubMed] [Google Scholar]
- Read, J. P. , Merrill, J. E. , Griffin, M. J. , Bachrach, R. L. , & Khan, S. N. (2014). Posttraumatic stress symptoms and alcohol problems: Self‐medication or trait vulnerability? The American Journal on Addictions, 23(2), 108–116. doi:10.1111/j.1521-0391.2013.12075.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saladin, M. E. , Brady, K. T. , Dansky, B. S. , & Kilpatrick, D. G. (1995). Understanding comorbidity between PTSD and substance use disorders: Two preliminary investigations. Addictive behaviors, 20(5), 643–655. [DOI] [PubMed] [Google Scholar]
- Schwartz, A. C. , Bradley, R. L. , Sexton, M. , Sherry, A. , & Ressler, K. J. (2005). Posttraumatic stress disorder among African Americans in an inner city mental health clinic. Psychiatric Services, 56, 212–215 [DOI] [PubMed] [Google Scholar]
- Sheehan, D. V. , Lecrubier, V. , Sheehan, K. H. , Amorim, P. , Janavs, J. , Weiller, E. , … Dunbar, G. C. (1998). The Mini‐International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM–IV and ICD‐10. Journal of Clinical Psychiatry, 59, 22–33. [PubMed] [Google Scholar]
- Sheehan, D. V. , Lecrubier, V. , Sheehan, K. H. , Janavs, J. , Weiller, E. , Keskiner, A , … Dunbar, G. C. (1997). The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID‐P and its reliability. European Psychiatry, 12, 232–241. [Google Scholar]
- Sonne, S. C. , Back, S. E. , Zuniga, C. D. , Randall, C. L. , & Brady, K. T. (2003). Gender Differences in Individuals with comorbid alcohol dependence and post‐traumatic stress disorder. The American Journal on Addictions, 12, 412–423. [PubMed] [Google Scholar]
- Stewart, S. H. , Pihl, R. O. , Conrod, P. J. , & Dongier, M. (1998). Functional associations among trauma, PTSD and substance‐related disorders. Addictive Behaviors, 23(6), 797–812. doi:10.1016/S0306-4603(98)00070-7 [DOI] [PubMed] [Google Scholar]
- Stewart, S. H. , Zvolensky, M. J. , & Eifert, G. H. (2002). The relations of anxiety sensitivity, experiential avoidance, and alexithymic coping to young adults‧ motivations for drinking. Behavior Modification, 26(2), 274–296. doi:10.1177/0145445502026002007 [DOI] [PubMed] [Google Scholar]
- Swendsen, J. , Conway, K. P. , Degenhardt, L. , Glantz, M. , Jin, R. , Merikangas, K. R. , … & Kessler, R. C. (2010). Mental disorders as risk factors for substance use, abuse and dependence: Results from the 10‐year follow‐up of the National Comorbidity Survey. Addiction, 105, 1117–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick, B. G. & Fidell, L. S. (2000). Using multivariate statistics (4th ed.). Boston, MA: Allyn and Bacon. [Google Scholar]
- Tull, M. T. , Barrett, H. M. , McMillan, E. S. , & Roemer, L. (2007). A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy, 38(3), 303–313. doi:10.1016/j.beth.2006.10.001 [DOI] [PubMed] [Google Scholar]
- Turner, R. , & Lloyd D. A.. (1995). Lifetime traumas and mental health: The significance of cumulative adversity. Journal of Health and Social Behavior, 36(4), 360–376. doi:10.2307/2137325. [PubMed] [Google Scholar]
- Waldrop, A. E. , Back, S. E. , Verduin, M. L. , & Brady, K. T. (2007). Triggers for cocaine and alcohol use in the presence and absence of posttraumatic stress disorder. Addictive Behaviors, 32(3), 634–639. doi:10.1016/j.addbeh.2006.06.001 [DOI] [PubMed] [Google Scholar]
- Weiss, N. H. , Tull, M. T. , Anestis, M. D. , & Gratz, K. L. (2013). The relative and unique contributions of emotion dysregulation and impulsivity to posttraumatic stress disorder among substance dependent inpatients. Drug and Alcohol Dependence, 128(1‐2), 45–51. doi:10.1016/j.drugalcdep.2012.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss, N. H. , Tull, M. T. , Davis, L. T. , Dehon, E. E. , Fulton, J. J. , & Gratz, K. J. (2012). Examining the association between emotion regulation difficulties and probable posttraumatic stress disorder within a sample of African Americans. Cognitive Behaviour Therapy, 41(1), 5–14. doi:10.1080/16506073.2011.621970 [DOI] [PubMed] [Google Scholar]
- Weiss, N. H. , Tull, M. T. , Viana, A. G. , Anestis, M. D. , & Gratz, K. L. (2012). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26(3), 453–458. doi:10.1016/j.janxdis.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


