Abstract
Rates of cardiovascular mortality and morbidity in Russia have been among the highest in Europe. A comprehensive health system improvement program targeting better diagnosis and control of hypertension was undertaken in the Yaroslavl Region of Russia. This initiative was a joint program between clinicians, the Department of Health and Pharmacy of the Yaroslavl Region, and Novartis Pharma LLC. From 2011 to 2014, the blood pressure control rate improved substantially (94% relative improvement), the percentage of patients with a systolic blood pressure ≥180 mm Hg decreased (from 10% to 5%), and there was a reduction in stroke incidence rate from 4.6 to 3.7 per 1000 population. During this same period, significant changes were made to the way hypertension was diagnosed and treated across all regional government polyclinics, and the use of antihypertensive therapies increased.
Historically, rates of cardiovascular (CV) mortality and morbidity in Russia have been among the highest in Europe.1 Hypertension prevalence is also high (~40% in adults) and is considered the most significant risk factor for total and CV mortality; thus, reducing the incidence and improving the control of hypertension in Russia is imperative. To this end, a comprehensive health system improvement program targeting better diagnosis and control of hypertension was undertaken in the Yaroslavl Region of Russia. This initiative was a joint program between clinicians, the Department of Health and Pharmacy of the Yaroslavl Region, and Novartis Pharma LLC, under the framework of the Memorandum of Understanding between the government of the Yaroslavl Region and Novartis Pharma LLC, Russia. One year after initiation of this program, a significant improvement in blood pressure (BP) control rates and a significant reduction in mean BP level were reported.2 This paper provides the details of the continued improvement 4 years after program implementation (2011–2014).
Assessment of the Problem
Prior to developing and implementing specific improvement initiatives, a cross‐sectional survey was conducted in 39 outpatient institutions of the Yaroslavl Region in 2011, with 154 general practitioners and 26 cardiologists participating.3 Physicians prospectively completed anonymous observational diaries on 10 consecutive adult patients whose visits were related to hypertension. No additional examinations, tests, interventions, or specific procedures were performed during data collection.
Demographic and baseline characteristics of patients from this initial survey (Table 1) have been previously reported.3 In summary, almost all diagnosed patients (97%) had already been prescribed antihypertensive therapy, with the most frequently used agents being β‐blockers (50% of all patients), angiotensin‐converting enzyme (ACE) inhibitors (49%), and diuretics (40%). Calcium channel blockers were reportedly used in only 26% and angiotensin receptor blockers (ARBs) in 16% of all patients. Mean BP was 151/90 mm Hg. Most patients (44%) had a systolic BP (SBP) range of 140 to 159 mm Hg, although 26% had grade 2 (SBP 160 to 179 mm Hg) and 10% had grade 3 (SBP ≥180 mm Hg) hypertension. Controlled BP (<140/90 mm Hg) was achieved in 17% of all patients.
Table 1.
Demographics, Hypertension History, Patient Risk Factors, End Organ Disease, and Associated Clinical Conditions
| Characteristic | Year of Survey (Number of Patients Surveyed) | |
|---|---|---|
| 20113 (N=1794) | 2014 (N=3015) | |
| Men/women/not specified, % | 37/60/3 | 37/63/1 |
| Mean age, y | 60 | 60 |
| Patient distribution by age group, y, % | ||
| Younger than 50 | 19 | 16 |
| 50–59 | 34 | 29 |
| 60–69 | 25 | 32 |
| 70 and older | 23 | 23 |
| Patient population of working agea | 50 | 43 |
| Patient distribution by duration of hypertension, % | ||
| ≤1 y | 18 | 4 |
| 2–9 y | 40 | 52 |
| ≥10 y | 42 | 43 |
| Patient distribution by risk factors, end organ disease, and associated clinical conditions, % | ||
| Left ventricular hypertrophy | 72 | 72 |
| Abdominal obesity | 54 | 51 |
| Dyslipidemia | 48 | 46 |
| Regular alcohol consumption | 37 | 26 |
| Family history of premature CVD | 33 | 29 |
| Current or past smoker | 24 | 22 |
| Diabetes type 2 | 21 | 18 |
| Carotid artery changes | 17 | 18 |
| Peripheral artery disease | 6 | 2 |
| Diabetic nephropathy | 3 | 3 |
| Microalbuminuria | 3 | 5 |
| Heart diseases | 48 | 39 |
| Chronic heart failure | 38 | 28 |
| Angina pectoris | 29 | 20 |
| Myocardial infarction | 11 | 10 |
| Hypertensive retinopathy | 20 | 15 |
| Cerebrovascular diseases | 15 | 15 |
| Stroke | 6 | 7 |
| TIA | 6 | 6 |
Abbreviations: CVD, cardiovascular diseases; TIA, transient ischemic attack.
In Russia, “working age” is defined as younger than 60 years for men and younger than 55 years for women.
Strategy for Change
Subsequent to this cross‐sectional survey, a novel private–government partnership was developed.2 The diagnostic phase evaluated the causes of poor hypertension control and then designed and prioritized potential interventions aimed at improving clinical operations, such as how people were diagnosed and treated for hypertension and how they were monitored and called back for clinic visits to review their BP level—especially if their BP or overall CV risk profile was high. Interventions were also put in place to improve performance management of the health system dealing with hypertensive patients, as well as enhancing the skills, mindsets, and behaviors of key players in the system, eg, patients, nurses, physicians, and clinic administrators. This was followed by the implementation phase that included ongoing continuous improvement of hypertension diagnosis and treatment to goal, along with regular reporting and performance management techniques at the clinic and prescriber level.
The initial interventions implemented during the first year of the program were largely described in 2013 by Mozheyko and colleagues.2 In brief, they included: (1) physician education (including a series of small‐group, targeted, case‐based discussions led by local clinical experts to address barriers to care and to provide information on evidence‐based guidelines and individualized treatment selection); (2) increased community awareness through a public education campaign (outdoor advertisements, patients’ schools, and short video advertisements in local public transportation) to improve patient engagement, adherence, and persistence with therapy; (3) development of a patient registry to identify and track patients with hypertension; and (4) establishment of three “improvement” pilot sites to implement a more detailed treatment protocol based on national guidelines, use a manual tracking and call‐back system for patients with hypertension, and measure and report clinic‐level BP control rates on a quarterly basis.
Additional strategies subsequently implemented after 2012 included: (1) mandatory collection and quarterly information–technology–enabled reporting of BP measurements for all patients seen at all government clinics across the Yaroslavl Region; (2) overall and clinic‐specific performance review of hypertension control rate performance to assess overall progress and identify specific clinics for targeted, increased awareness and physician training; (3) scaling up of small‐group, case‐based physician training for the majority of government‐clinic–based physicians (508 in 36 clinics through the end of 2014) in hypertension management, patient adherence, and engagement in self‐measurement and management of their hypertension; (4) clinic‐level follow‐up and monthly call‐back of patients (targeting those with high BP/poor control); (5) referrals of “difficult to control” patients to the regional hypertension center at a central hospital in Yaroslavl City; (6) nurses’ awareness and best‐practice case sharing; (7) symbolic rewards system to best‐performing and most‐improved clinics across the Yaroslavl Region; and (8) modeling of the potential impact of better hypertension and other CV risk factor management improvement, with communication to policy makers to reinforce the importance of hypertension management and to keep it a public health priority.4
Effects of Change (2011 and 2014)
Demographics
A total of 3015 patient surveys were completed in 2014 (Table 1). Patient characteristics of the population surveyed in 2014 were similar to the population surveyed in 2011. Most patients in 2014 had been prescribed antihypertensive therapy (92%), with 77% prescribed more than one drug; 2014 data were generally consistent with 2011 data (97% and 83%, respectively).3
BP Control Rates/Hypertension Stages
In 2014, mean BP decreased to 145/86 mm Hg compared with 151/90 mm Hg in 2011. Controlled BP (<140/90 mm Hg) was achieved in 33% of patients, demonstrating a 94% relative improvement from 20113 when only 17% of all patients had SBP <140 mm Hg (Figure 1). Distribution of patients’ SBP changed from 20% (2011)3 to 36% (2014) controlled (<140 mm Hg), 44% to 39% SBP 140 to 159 mm Hg, 26% to 21% SBP 160 to 179 mm Hg, and 10% to 5% SBP ≥180 mm Hg (Figure 2).
Figure 1.
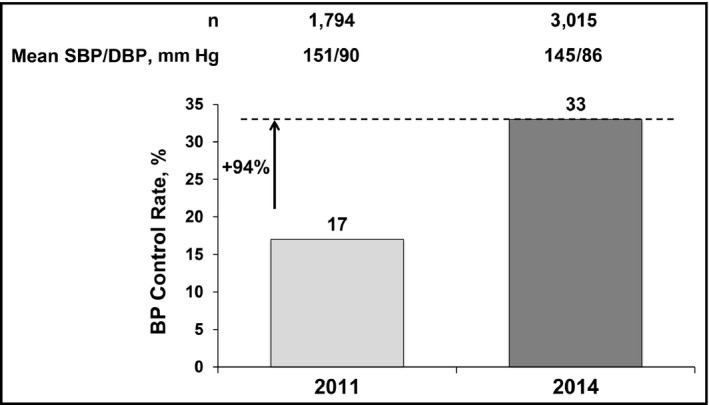
Blood pressure (BP) control rates (<140/90 mm Hg). SBP indicates systolic blood pressure; DBP, diastolic blood pressure.
Figure 2.
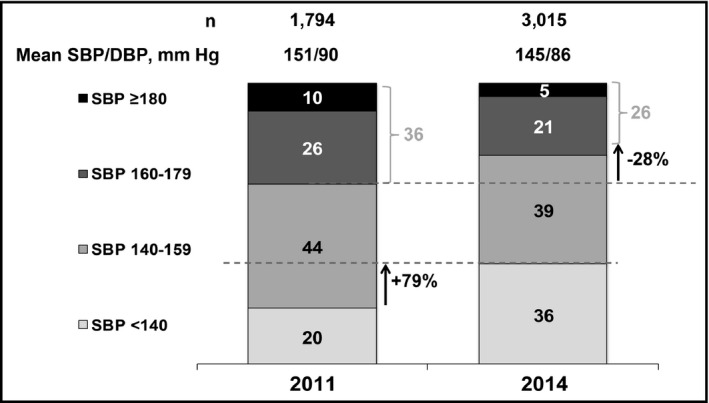
Patient distribution according to systolic blood pressure (SBP) level. DBP indicates diastolic blood pressure.
Stroke Incidence
During the course of this study, the number of registered strokes (International Classification of Disease, 10th Revision code I60–I64) fell in the Yaroslavl Region from 4933 in 2011 to 3872 in 2014 (−21.5%), corresponding to a reduction in stroke incidence rate from 4.6 to 3.7 per 1000 population (Figure 3A).5 With regard to the different types of strokes, the largest reduction—in terms of absolute numbers—was observed in cerebral infarction (ischemic stroke), which constituted the majority of stroke incidence reported; however, proportionally, the largest decrease was observed in the relative rates of subarachnoid hemorrhage (Figure 3A).
Figure 3.
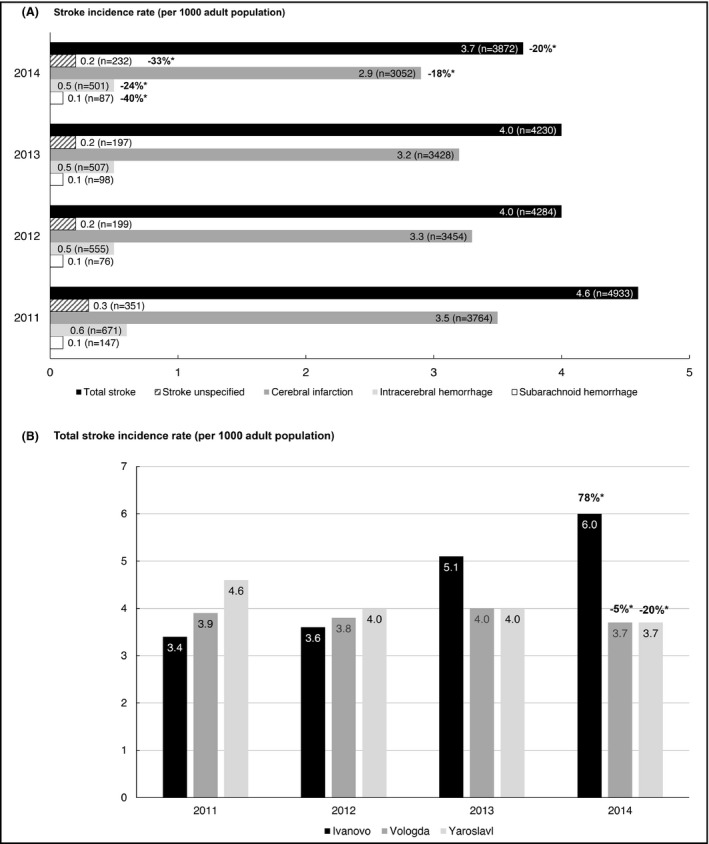
Incidence of stroke in Yaroslavl (A) and other regions (B) from 2011 to 2014.5, 6 *Indicates the change in relative rate from 2011 to 2014. n=xx denotes the absolute number of patients with reported stroke incidence.
In comparison, in two similar neighboring regions without comprehensive health system interventions, over the same period, the incidence of total stroke increased from 3.4 (in 2011) to 6.0 (in 2014) per 1000 population (78%) in Ivanovo; and there was a minor decrease in the total stroke incidence in the Vologda Region from 3.9 (in 2011) to 3.7 (in 2014) per 1000 population (−5%; Figure 3B).5, 6
Medications
In 2014, the most frequently used antihypertensive agents in the Yaroslavl Region were β‐blockers (reported in 41% [1220 of 3000] of physician‐completed observation diaries), ACE inhibitors (36% [1071 of 3000]), and diuretics (27% [802 of 3000]), consistent with the most frequently used medications in 2011. Compared with 2011, 2014 saw a significant (P=.05) decrease in the use of ACE inhibitors (49% 2011 vs 36% 2014), β‐blockers (50% vs 41%), and diuretics (40% vs 27%), and a significant (P=.05) increase in the use of ARBs (16% vs 20%). However, there was no major difference in the use of calcium channel blockers from 2011 (26%) to 2014 (24%).
The number of units of antihypertensive therapies dispensed increased from approximately 3,700,000 packs in 2011 to approximately 4,400,000 packs in 2014. Evaluating packs per person per year, there was a 16% increase in hypertensive drug consumption in the Yaroslavl Region in 2014 compared with 2011. This increase correlates with the implementation of a health system improvement program targeting better diagnosis and control of hypertension and seems to be specific for the Yaroslavl Region. In comparison, in Vologda, the volume of antihypertensive therapies increased 10% from 2011 to 2014, while in Ivanovo, the volume of antihypertensive therapies decreased 15% (Figure 4). (Unpublished data sourced from an IMS database subscription accessible to the authors from [www.imshealth.com]; Federal Statistic Service Demographic Yearbook.)
Figure 4.
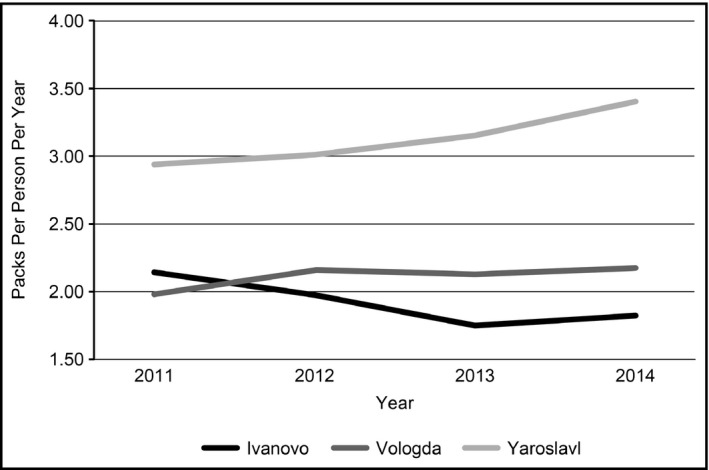
Volume of antihypertensive therapies dispensed (retail channel); Yaroslavl Region 2011 to 2014 packs per person per year. (Unpublished data sourced from an IMS database subscription accessible to the authors [www.imshealth.com]).22
Discussion
The initiation of a novel private–government partnership to address the high rate of hypertension and CV‐related events, such as strokes, in the Yaroslavl Region of Russia has resulted in many benefits. From 2011 to 2014, the BP control rate improved substantially, the percentage of patients with an SBP ≥180 mm Hg decreased, and there was a decrease in the absolute number of strokes across the region. During this same period, significant changes were made to the way hypertension was diagnosed and treated across all regional government polyclinics, and the use of antihypertensive therapies increased. Alternative data collection from a large number of people with an established hypertension diagnosis visiting the Government Health Clinics in the Yaroslavl Region confirms broad improvement in BP control rates across the region over the same period (ie, 36% in 2013 and 53% in 2014). (Data on file: Medication Information Analytical Center of Yaroslavl Region.) Of note, this program is becoming a model for other communities across Russia and has been mentioned in a recent paper on the topic of global prevention and control of hypertension, receiving a recognition award from the World Hypertension League.7
The Yaroslavl Program is just one of several large‐scale, regional hypertension programs that have been implemented and evaluated, including those in North America (eg, Canada,8, 9 California,10 Minnesota11), Europe (eg, England,12 Finland,13), and Asia (eg, China14), as well as others in Russia.15, 16
In Canada, the Canadian Hypertension Education Program (CHEP) began in 1999.8 CHEP includes three task forces: the Clinical Recommendations Task Force (which develops and updates hypertension recommendations), the Implementation Task Force (which summarizes the recommendations and creates partnerships to develop and disseminate materials to specific audiences), and the Outcomes Research Task Force (which evaluates the success of the recommendations and identifies areas for further improvement).17 Of note, BP control (<140/90 mm Hg) improved after its initiation (from 13.2% of patients in 1992 [n=22,314]18 to 68.1% in 2013 [n=5785]).19 There were decreases in rates of stroke, heart failure, and myocardial deaths and increased antihypertensive prescriptions that have been associated with the start of CHEP17 Although these findings occurred with the introduction of CHEP, causal effect cannot be confirmed. Senior professionals from CHEP engaged with key clinicians and administrators from the Yaroslavl Region to share lessons learned from their program as well as materials for physicians, nursing staff, patients, and their families regarding diagnosis and treatment of hypertension.
Potential barriers to healthcare change may still include lack of leadership support, resistance or skepticism from staff, hesitancy to invest time and money, shortage of internal resources to lead change initiative, waning commitment, and uncertain roles and/or lack of accountability.20 Success of the Yaroslavl Program is due, in part, to overcoming these barriers with an approach consistent with many of the steps associated with successful, large, healthcare system transformation and change management initiatives. However, as with almost any healthcare program, the Yaroslavl Program has its limitations, particularly with collecting and interpreting the data. There have been challenges with obtaining baseline measurements, especially for the pilot sites. In addition, data are collected only for patients “in the system” visiting outpatient clinics, although many others in the community may be at risk. Although all patients in the Yaroslavl Region are included in the morbidity and mortality data for main events, the BP control data and the impact of the educational program are limited to those patients who came to the polyclinics. Of note, although there may be potential bias in our data (as BP rates are self‐reported by patients’ own doctors and patients are chosen by the participating physician), data collected in parallel and in much greater quantities from the Yaroslavl Department of Health confirms the program data. Limitations include difficulty in linking treatment prescribed to patient outcomes, lack of data on patients’ adherence with therapy, inability to adjust for comorbidities, and the lack of a control group. We have addressed this last element by comparing results observed in Yaroslavl Region to other nationwide figures, as well as metrics from similar neighboring regions (ie, Ivanovo and Vologda). While it is difficult to provide a comprehensive stroke incidence geographic analysis, as data from regional hypertension programs in Russia and their influence on stroke are scarce, we have tried to explore this by analyzing data from comparable regions. Unlike Yaroslavl, in these other regions, there are no known hypertension programs, and the number of antihypertensive medications sold to the population may be the proxy of hypertension control changes in those regions. In Ivanovo, there was a 15% decrease in the volume of antihypertensive pills sold from 2011 to 2014 and a 78% increase in the total stroke incidence; whereas, in the Vologda Region there was a 10% increase in the volume of antihypertensive pills sold from 2011 to 2014, with a minor decrease in total stroke incidence (−5%) (Unpublished data sourced from an IMS database subscription accessible to the authors from [www.imshealth.com];5, 6 Federal Statistic Service Demographic Yearbook). Although these data are not a part of a comprehensive causality analysis, they do confirm an expected pattern of correlation between the volume of antihypertensive medication sales and stroke incidence, as observed in the Yaroslavl Program.
Conclusions
As implementation of the Yaroslavl Program has not been without its challenges, we hope that countries interested in developing similar programs will benefit from our “lessons learned” (Table 2). Importantly, the Yaroslavl Program is strengthening. The program continues to enhance education among physicians, nurses, and patients to keep the focus on BP as a key predictor of CV event outcomes. Currently, the Yaroslavl Program is being utilized as a model to urge other Regional Ministries of Health in Russia to consider similar healthcare system improvement projects. In the future, we hope that hospitalization and mortality information will be linked through electronic records to outpatient data in polyclinics to allow more direct evaluation of the intervention to patient outcomes at a clinic and healthcare provider level. Consideration should be given to expanding educational/awareness programs to include other early predictors of CV outcomes, such as smoking, lipid control, and glycemic control; and for improving medication availability in the system to improve program outcome and sustained BP control. With a higher prevalence of hypertension and lower control rates than other global regions, the importance of hypertension control programs in Russia cannot be underestimated—particularly following the results of the Systolic Blood Pressure Intervention Trial (SPRINT),21 which recently demonstrated that more stringent BP control (systolic BP <120 mm Hg) significantly lowers the rate of major CV events and all‐cause mortality compared with standard BP control.
Table 2.
Lessons Learned
| • Engage the administration from the top |
| • Invest in understanding the situation through data and focus on understanding the root causes behind suboptimal performance |
| • Invest in sustained, targeted educational activities |
| • Be aware of knowledge gaps among some medical professionals |
| • Closing the knowledge gap may not be enough; changes in behaviors and practices may be needed |
| • Invest in an information technology infrastructure, with key metrics reported and discussed in an appropriate forum and feedback to clinicians and clinic administrators: |
| • These data can be used to track progress and also to identify clinics/locations or issues that require additional intervention |
Statements of Financial Disclosure
Maria Mozheyko has received lecturer's honoraria and travel support and participated in research conducted by Novartis Pharma LLC, Russia. Sergey Eregin has received lecturer's honoraria and travel support from Novartis Pharma LLC Russia. Natalia Danilenko is Deputy Director of Yaroslavl Department of Health and received travel support from Novartis Pharma LLC. Alexey Vigdorchik is a former employee of Novartis Pharma LLC, Russia. Sheldon Tobe has received lecturer's honoraria and travel support from Novartis Pharma LLC, Russia. Norman Campbell received travel support for a site visit from Novartis Pharma LLC, Russia, in 2012. Donna McLean has no conflicts of interest to declare. Zhanna Baskakova, Ilnaz Klimovskaia, and Krishnan Ramanathan are employees of Novartis Pharma LLC, Russia. David Hughes is an employee of Novartis Pharma AG, Switzerland. These surveys were initiated by the Department of Health and Pharmacy of the Yaroslavl Region, designed and reviewed by all authors, conducted by the International Institute for Market Research GFK Rus, and funded by Novartis International AG, Basel, Switzerland. Editorial assistance was provided by Oxford PharmaGenesis, Newtown, PA, USA. Editorial assistance was funded by Novartis International AG, Basel, Switzerland.
Author Contributions
All authors had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. The draft manuscript was prepared by David Hughes and Alexey Vigdorchik with input from Maria Mozheyko, Sergey Eregin, Natalia Danilenko, Sheldon Tobe, Norman Campbell, Donna McLean, Zhanna Baskakova, Ilnaz Klimovskaia, and Krishnan Ramanathan.
Acknowledgments
The authors would like to thank Olga Chernichenko, Andrey Karasev, Ekaterina Germanova, and Anna Skvortsova of International Institute for Market Research GFK Rus for assistance in planning, conducting, and preliminary analysis of these surveys. The medical interventions are consistent with Russia National Guidelines and accepted medical practice, and approved by the Department of Health and Pharmacy of the Yaroslavl Region. The project and interventions were approved by the Department of Health and Pharmacy of the Yaroslavl Region and the ethics review board of the Yaroslavl Regional Clinical Hospital of War Veterans, Yaroslavl, Russia.
J Clin Hypertens (Greenwich). 2017;19:198–204. DOI: 10.1111/jch.12885. © 2016 The Authors. The Journal of Clinical Hypertension Published by Wiley Periodicals, Inc.
References
- 1. Nichols M, Townsend N, Luengo‐Fernandez R, et al. European cardiovascular disease statistics 2012. European Heart Network, Brussels, European Society of Cardiology, Sophia Antipolis; 2012. https://www.escardio.org/static_file/Escardio/Press-media/press-releases/2013/EU-cardiovascular-disease-statistics-2012.pdf. Accessed February 11, 2016.
- 2. Mozheyko M, Eregin S, Vigdorchik A, et al. Changes in hypertension treatment in the Yaroslavl region of Russia: improvements observed between 2 cross‐sectional surveys. J Clin Hypertens (Greenwich). 2013;15:918–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mozheyko M, Eregin S, Vigdorchik A, Hughes D. A cross‐sectional survey of hypertension diagnosis and treatment practices among physicians in Yaroslavl Region, Russia. Adv Ther. 2012;29:1016–1025. [DOI] [PubMed] [Google Scholar]
- 4. Shum K, Alperin P, Shalnova S, et al. Simulating the impact of improved cardiovascular risk interventions on clinical and economic outcomes in Russia. PLoS One. 2014;9:e103280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Central Scientific Research Institute of Healthcare Informatization and Organization of the Ministry of Healthcare of Russia . Disease incidence of adult population in Russia in year 2014: Statistical materials, Part III. Moscow, 2015.
- 6. Central Scientific Research Institute of Healthcare Informatization and Organization of the Ministry of Healthcare of Russia . Data for 2011 and 2012: Disease incidence of adult population in Russia in year 2012: Statistical materials, Part III. Moscow, 2013.
- 7. Campbell NR, Niebylski ML, World Hypertension League Executive . Prevention and control of hypertension: developing a global agenda. Curr Opin Cardiol. 2014;29:324–330. [DOI] [PubMed] [Google Scholar]
- 8. Campbell NR, Tu K, Brant R, et al; Canadian Hypertension Education Program Outcomes Research Task Force . The impact of the Canadian Hypertension Education Program on antihypertensive prescribing trends. Hypertension. 2006;47:22–28. [DOI] [PubMed] [Google Scholar]
- 9. Tu JV, Nardi L, Fang J, et al. National trends in rates of death and hospital admissions related to acute myocardial infarction, heart failure and stroke, 1994‐2004. CMAJ. 2009;180:E118–E125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jaffe MG, Lee GA, Young JD, et al. Improved blood pressure control associated with a large‐scale hypertension program. JAMA. 2013;310:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sillah A, Sidebottom AC, Boucher JL, et al. Program participation and blood pressure improvement in the Heart of New Ulm Project, Minnesota, 2009‐2011. Prev Chronic Dis. 2014;11:E48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Falaschetti E, Chaudhury M, Mindell J, Poulter N. Continued improvement in hypertension management in England: results from the Health Survey for England 2006. Hypertension. 2009;53:480–486. [DOI] [PubMed] [Google Scholar]
- 13. Nissinen A, Kastarinen M, Tuomilehto J. Community control of hypertension—experiences from Finland. J Hum Hypertens. 2004;18:553–556. [DOI] [PubMed] [Google Scholar]
- 14. Chen XJ, Gao XL, You GY, et al. Higher blood pressure control rate in a real life management program provided by the community health service center in China. BMC Public Health. 2014;14:801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Oschepkova EV. On the implementation of federal targeted program: Prevention and the Treatment of Hypertension in Russian Federation. http://federalbook.ru/files/FSZ/soderghanie/Tom%206/XIII/Oschepkova.pdf. Accessed February 11, 2016.
- 16. Russian Federation . Government Decree No. 280. On the Federal Targeted Program Prevention and Control of Social Diseases (2007‐2012). http://pravo.gov.ru/proxy/ips/?docbody=&nd=102114055&rdk%20=&backlink=1. Accessed February 11, 2016.
- 17. Campbell NR, Brant R, Johansen H, et al. Increases in antihypertensive prescriptions and reductions in cardiovascular events in Canada. Hypertension. 2009;53:128–134. [DOI] [PubMed] [Google Scholar]
- 18. McAlister F, Wilkins K, Joffres M, et al. Changes in the rates of awareness, treatment and control of hypertension in Canada over the past two decades. CMAJ. 2011;183:1007–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Padwal RS, Bienek A, McAlister FA, Campbell NR, Outcomes Research Task Force of the Canadian Hypertension Education Program . Epidemiology of hypertension in Canada: an update. Can J Cardiol. 2016;32:687–694. [DOI] [PubMed] [Google Scholar]
- 20. Trusko B, Pexton C, Harrington J, Gupta PK. Improving Healthcare Quality and Cost with Six Sigma. Upper Saddle River, NJ: FT Press; 2007. [Google Scholar]
- 21. SPRINT Research Group ; Wright JT, Jr , Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood‐pressure control. N Engl J Med. 2015;373:2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Federal State Statistics Service . Demographic yearbook of Russia. http://www.gks.ru/wps/wcm/connect/rosstat_main/rosstat/ru/statistics/publications/catalog/doc_1137674209312. Accessed February 11, 2016.


