Abstract
Objective:
Modified Limb Lead (MLL) ECG system may be used during rest or exercise ECG, or atrial activity enhancement. Because of modification in the limb electrode placement, changes are likely to happen in ECG wave amplitudes and frontal plane axis, which may alter the clinical limits of normality and ECG diagnostic criteria. The present study investigated the effects of the modified limb electrode position on the electrocardiographic waveforms, ST segment amplitudes (STa) and frontal plane axis.
Methods:
The observational study included sixty sinus rhythm subjects of mean age 38.85±8.76 (SD) in the range 25 to 58 years. In addition to 12-lead ECG, MLL ECG was recorded with, the RA electrode placed in the 3rd right intercostal space to the right of the parasternal line, the LA electrode placed in the 5th right intercostal space to the right of the mid-clavicular line and the LL electrode placed in the 5th right intercostal space on the mid-clavicular line.
Results:
The modification produced profound changes in ECG wave amplitudes and STa amplitudes in frontal plane leads. The QRS and T wave axis shifted on the average by –17° and 41°, respectively, with considerable individual variation, which altered the diagnostic criteria.
Conclusion:
The ECG amplitudes and STa changes produced by the MLL system showed that all remains within the clinical limits, except the R wave amplitude in the modified lead I. It is evident that the MLL system produced deviations in frontal plane QRS axis which altered the diagnostic interpretation.
Keywords: electrocardiogram, modified limb lead, standard 12-lead, STa, QRS axis
Introduction
The standard positioning of the limb lead electrodes for electrocardiogram was first devised by Willem Einthoven (1). Consequently the study and standardization on the precordial leads for electrocardiogram were performed by Barnes et al. (2). Motion artifact is a major concern on the limb lead electrodes, as it has a great influence on the ECG waveform amplitudes (3). During exercise stress testing, motion of the limbs can disrupt the ECG recordings and in conditions where limbs become clinically inaccessible, the modified limb electrode position on the torso addresses the above problem (4). Mason et al. (5) proposed alternative limb electrodes for the use in exercise stress testing. A variety of modified limb electrode configurations placed on the torso of healthy subjects is discussed (6–9).
The modified limb electrode placed on the torso had an effect on the wave amplitudes in the frontal plane ECG and false-positive ECG changes have been reported previously (10–15). Significant R, S, and T wave amplitude changes because of modi- fied limb electrode placement have been reported previously (16–18). It has been reported that with the modified limb electrode placement, no significant changes were observed in the ECG waveform in the transverse plane, as the precordial leads are unchanged (19). In addition to the modified limb electrode placement, which affects the waveform amplitudes and frontal plane axis, several other alternative lead systems, placed on the human torso exist for recording and studying the electrical activity of the atria (20).
The authors of this study recently proposed a Modified Limb Lead (MLL) system for unmasking the atrial repolarization (Ta wave) in sinus rhythm subjects and in AV block patients (21–23). Further, in their subsequent study, they reported on the normal limits of the proposed MLL system and documented the changes happened in P wave amplitudes and frontal plane P wave axis (24). In that study it was found that P wave amplitude increased in all the modified leads compared with that in the standard leads, and according to the results of that study, it was found that the MLL system was optimal in studying the electrical activi- ty of the atrial ECG components.
In this study, the purpose of the investigation was to examine the magnitude of the ECG wave amplitudes and ST segment amplitudes (STa) differences between the standard limb lead (SLL) and the MLL ECG system. In addition, it was also exami- ned whether the modification led to any deviations in the frontal plane axis beyond the clinical limits of normality.
Methods
Study design
This was an observational study which includes 60 male subjects in sinus rhythm of mean age 38.85±8.76 (SD) in the range of 25 to 58 years with normal body composition. All volunteers were recruited into the study from the outpatient department of the Rajiv Gandhi Government General Hospital, Chennai and all were medically examined to exclude any form of cardiovascular disease. Non-hypertensive subjects were included in the study. Smokers and patients with congestive heart failure, valvular di- sease, atrial fibrillation, and other cardiopulmonary diseases that may alter the ECG morphology were excluded from this study, which was approved by the Institutional Ethics Committee. Before data recording, all subjects gave informed consent to their participation in this study.
Modified limb electrode placement
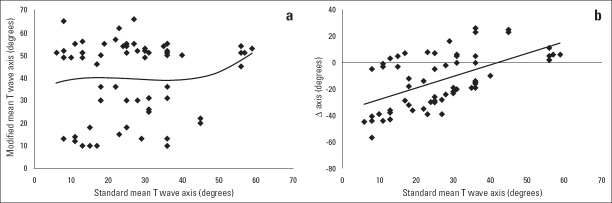
The modified limb electrode placement (21, 22) of the MLL system is briefly described as follows (Fig. 1). The right arm electrode is placed on the subject’s third right intercostal space, slightly to the left of the mid-clavicular line. The left arm electrode is placed in the 5th right intercostal space, slightly to the right of the mid-clavicular line, and the left leg electrode is placed in the 5th right intercostal space, on the mid-clavicular line. The right leg electrode is placed on the subject’s right ankle. The polarity of the right arm electrode is negative, and the polari- ty of the left arm and left leg electrode is positive. The usual terminology applies-e.g., the potential difference between the right arm electrode (RA) and left arm electrode (LA) is still denoted as lead I, etc. The standard precordial electrode positions V1–V6 are unchanged in this study during the MLL recordings, but they have no role to play in this study.
Figure 1.
(a) Placement of modified limb electrodes on the torso. The precordial leads V1_V6 are unchanged. (b) Modified Limb Lead system.
ECG acquisition
A digital ECG recorder (EDAN SE-1010 PC ECG system, EDAN Instruments, Inc., China) operating at 1000 samples per second with a frequency response of 0.05 Hz to 150 Hz was used to acquire ECG data.
ECGs could be printed at a variable gain from 2.5 mm/mV to 100 mm/mV and a variable paper speed of 5 mm/s to 200 mm/s. All ECGs were recorded in the supine position using surface Ag–AgCl electrodes. All the ECGs were recorded, first using the standard 12-lead electrode positions and subsequently by the MLL system by repositioning the right arm, left arm and left leg electrodes as indicated in Figure 1. All the ECGs were recorded at standard ECG paper speed of 25 mm/s and 10 mm/mV.
Data analysis
All the ECG data were analyzed automatically by an automa- tic analysis smart ECG measurement and interpretation programs of EDAN ECG machine in offline. The ECG values such as frontal plane axis (P, QRS, and T), amplitudes of each waveform (R, S, and T) and STa were all recorded and stored for further analysis. The STa is measured from the J point to 80 ms after the onset of the J point (J+80 ms) in this study. The STa deviations are analyzed for each 20 ms after the onset of the J point to validate whether the MLL system has any effect on the ST segments. All the ECG data were plotted digitally and analyzed separately for comparison purpose.
Statistical analysis
The data presented are expressed as mean±standard deviation (SD), mean±standard error (SE). The Student’s t-test was used to determine statistical significance of all measurement differences. The Shapiro-Wilk W test was used for testing the normality and all the data were normally distributed (p=“0.78”). Linear and curvilinear regression analysis was performed on the data for the mean distribution of QRS and T wave axis. Linear regression analysis was used on the data between the standard and modified mean QRS and T wave axis changes. All tests were two-sided and value p<0.05 was considered statistically significant. The collected data were statistically evaluated using Win STAT in Excel for Windows.
Results
The 12-lead ECG recorded on male subjects in sinus rhythm revealed no trace of cardiac disorders and was reported as being within normal limits. All ECG data were normally distri- buted. The standard 12-lead ECG and MLL ECG (21, 22) recor- ded at standard ECG paper speed in supine position for healthy male subjects is shown in Figure 2. It is noted that very large amplitude changes take place with the MLL system. The MLL ECG showed significant R wave amplitude changes (23). As the left arm electrode and left leg electrode are beside each other in the MLL system, the modified lead III ECG is essentially seen as flat trace in all the recordings. But still, small R wave amplitude was noticeable in the modified lead III with no distinct P and T wave. Since the amplitude, axis changes of the P wave and the importance of the MLL system in detecting the atrial ECG components have been previously reported as a separate paper (24) this study emphasis on other wave amplitudes (R, S, and T), STa and deviations in frontal plane axis caused by the MLL system.
Figure 2.
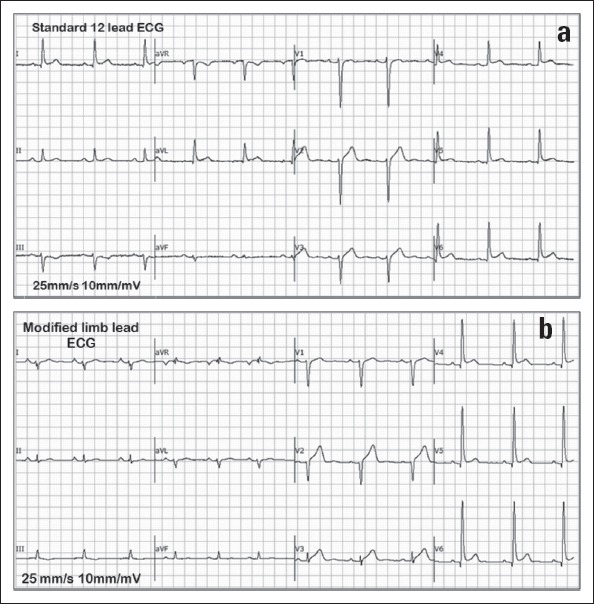
(a) Standard 12-lead ECG of a male subject in sinus rhythm. The R wave has maximum amplitude in all the leads. (b) MLL ECG of the same male subject in sinus rhythm used in the standard 12 lead ECG. The MLL ECG shows the presence of large P wave amplitudes and reduced R wave amplitudes in the limb leads
Changes in QRS and T wave axis
Compared with the standard 12-lead ECG, MLL placement resulted in the frontal plane axis shift in P, QRS, and T waves. The axis measurements were generally more affected by the chan- ges in the modified limb electrode placement. The distribution of the QRS and T wave axis changes between the standard and the modified position is shown in Figure 3, 4. The difference in the frontal plane axis (QRS and T) values between the MLL ECG and SLL ECG is shown in Table 1. The frontal plane mean QRS axis had significant changes in the MLL system, with an average axis shift of –17±91° when the electrodes were moved from the limb to the torso of the subjects. The mean difference between the modified and standard lead (M-S) of the QRS axis is found to be –61°. There are considerable individual variations in the degree of this shift. The least square cubic fit for the modified axis (am) calculated from the standard axis (as) from Figure 3a is given as
Figure 3.
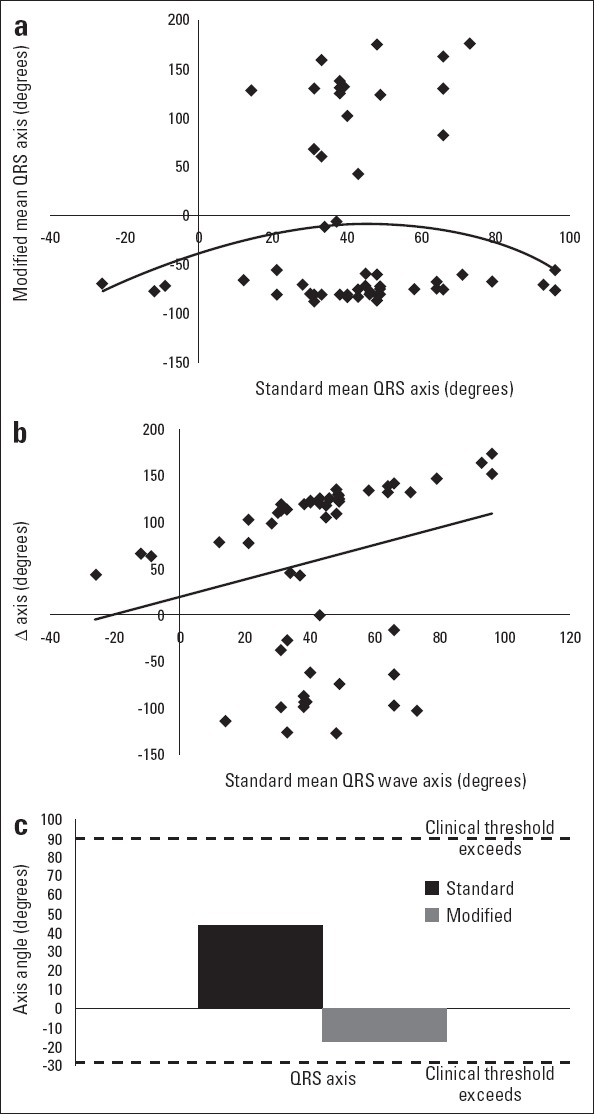
(a) Distribution of mean QRS wave axis in standard and modi-fied position and curvilinear regression calculated from the axis values (b) Distribution of mean QRS wave axis in standard position (x-axis) ver-sus the change in the measurement when the electrodes are moved to the torso and linear regression calculated from the axis values (c) Mean electrical axes of the QRS complex in standard and modified position showing the thresholds for clinical abnormality
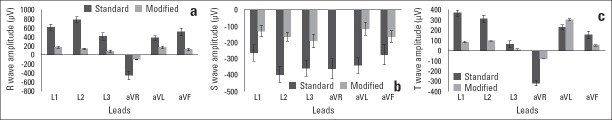
Figure 4.
(a) Distribution of mean T wave axis in standard and modified position and curvilinear regression calculated from the axis values (b) Distribution of mean T wave axis in standard position (X-axis) versus the change in the measurement when the electrodes are moved to the torso and linear regression calculated from the axis values
Table 1.
Changes in the frontal plane axis with the standard and modified positions
| Electrocardiographic axis in degrees for sinus rhythm subjects ECG | ||||||||
|---|---|---|---|---|---|---|---|---|
| Standard position (SLL) | Modified position (MLL) | Difference | ||||||
| Mean | SD | Range | Mean | SD | Range | M-S | P* | |
| QRS axis | 44.11 | 22.79 | -26 to 96 | -16.93 | 91.05 | -88 to 176 | -61.04 | <0.05 |
| T axis | 26.65 | 13.46 | 06 to 59 | 40.23 | 17.06 | 10 to 66 | 13.58 | <0.05 |
MLL - modified limb lead; SD - standard deviation; SLL - standard limb lead;
Paired sample t-test
αm=–0.00004αs3 –0.010αs2+1.225αs –39.32 (1)
The equation of the linear regression line from Figure 3b is given as
ΔQRS axis (°)=20.14+0.927 x QRS (2)
where QRS is the QRS wave axis.
The T wave axis measurements were also affected likewise in the P and QRS axis. The distribution of the T wave axis in the SLL and MLL system is shown in Figure 4. The frontal plane mean T wave axis had an average shift of 40±17° in the MLL system, when the electrodes are moved from the limb to the torso of the subjects. The mean difference between the modified and standard (M-S) of the T wave axis is found to be 13°. The least square cubic fit for the modified axis (am) calculated from the standard axis (as) from Figure 4a is given as
αm=0.000αs3 –0.036αs2+0.881s2+33.51 (3)
The equation of the linear regression line from Figure 4b is given as
ΔT axis (°)=–36.77+0.870 x T (4)
where T is the T wave axis.
QRS axis deviations
Surawicz et al. (25) defined the clinical limits of mean frontal plane axis of QRS normality and abnormality (i.e., < > –30° to +90°). The range of deviations in QRS axis in the MLL system was –88° to 176°, whereas in the SLL system it was –26° to 96°. Although the modification produced individual variations in degree of the axis shift, the mean frontal QRS axis of the MLL system was –17° as seen in Figure 3c. Out of total 60 sinus rhythm subjects, the MLL system in sinus rhythm subjects produced normal QRS axis shift [–30° to +90°, (n=6)], marked left axis deviation [–45° to –90°, (n=41)], moderate right axis deviation [90° to 120°, (n=1)] and marked right axis deviation [120° to 180°, (n=12)]. No sinus rhythm subjects produced any moderate left axis deviation (–30° to –45°). It is clear evident that the modified limb electrode placement in the torso produced deviations in the frontal plane mean QRS axis and this may have an effect on the clinical specificity.
Changes in ECG amplitudes and waveforms
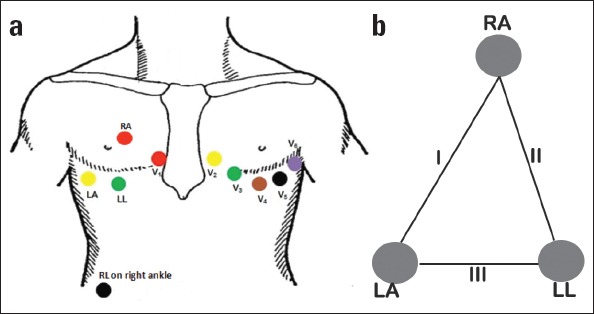
Consequent to the changes in the frontal plane axis shift resulted by the modification in the position of the limb electrodes, it is noted that very large amplitude differences takes place in the frontal plane leads. As with the axis changes the largest vol- tage changes are found when the electrodes are moved from the limb to the torso. As expected, no significant changes are seen in the ECG amplitudes of the transverse plane leads (V1–V6) as they are unchanged during the recording of the modified positioning of the limb electrodes. The MLL system produced significant R wave amplitude changes when compared with the other frontal plane leads and produced false ECG changes in the modified lead I of the R wave amplitude. The mean R wave amplitude of modified lead I is 0.17 mV, which is <0.2 mV defined as the clinical threshold of abnormality (26). The plot of mean±SE of R wave amplitudes in MLL and SLL recordings is shown in Figure 5a. In frontal plane leads the R wave amplitude decreased in the modified leads I-aVF.
Figure 5.
Plot of mean±SE of R, S, and T wave amplitudes of the frontal plane leads in the standard and the modified electrode positions
Similarly, the modified limb electrode placement produced amplitude changes in S and T waves respectively as shown in Figures 5b–c. The S wave amplitude decreased in all the frontal plane leads of the MLL system. The T wave amplitude decreased in all the modified leads except the modified lead aVL. The R, S, and T wave amplitude values of the MLL system are shown in Table 2. Mean values are listed for the difference between the modified and standard lead (M-S) in which positive value indicates an increase and a negative value indicates a decrease caused by modification of the electrode positioning.
Table 2.
ECG waves with the standard and modification of the limb electrode positions. Mean values are listed for the difference (M-S) in which positive values indicate an increase in amplitude and negative values indicate a decrease caused by modification. Percentage gains in mean amplitudes are also provided. Amplitudes are in microvolts. N/A=not applicable
| Measurement | Leads | Standard position (SLL) | Modified position (MLL) | Modified–Standard position (% change) | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | % | ||
| R amplitude | I | 611 | 283 | 170 | 98 | -441 | -72 |
| II | 774 | 274 | 130 | 96 | -644 | -83 | |
| III | 412 | 348 | 79 | 108 | -333 | -81 | |
| aVR | -447 | 387 | -100 | 39 | -347 | -78 | |
| aVL | 373 | 223 | 163 | 120 | -210 | -56 | |
| aVF | 508 | 343 | 119 | 119 | -389 | -76 | |
| S amplitude | I | 264 | 209 | 129 | 98 | -135 | -51 |
| II | 396 | 198 | 163 | 96 | -233 | -59 | |
| III | 357 | 201 | 190 | 108 | -167 | -47 | |
| aVR | 361 | 244 | 0 | 39 | -361 | N/A | |
| aVL | 341 | 195 | 116 | 120 | -225 | -66 | |
| aVF | 275 | 244 | 163 | 119 | -112 | -41 | |
| T amplitude | I | 363 | 119 | 79 | 34 | -284 | -78 |
| II | 309 | 137 | 91 | 20 | -218 | -70 | |
| III | 58 | 143 | 7 | 50 | - 51 | -88 | |
| aVR | 323 | 106 | 82 | 16 | -217 | -67 | |
| aVL | 226 | 96 | 29 | 44 | -197 | -87 | |
| aVF | 150 | 148 | 49 | 38 | -101 | -67 | |
MLL - modified limb lead; SD - standard deviation; SLL - standard limb lead; values are in microvolts
Changes in ST segment amplitudes (STa) level
Consequent to the changes in the ECG amplitudes, the modification of the limb electrode produced changes in the STa in the frontal plane leads. The STa is measured from the J point to 80 ms after the onset of the J point (J+80 ms) in this study. The STa deviations are analyzed for each 20 ms after the onset of the J point to validate whether the MLL system has any effect on the ST segments. In general the ST segment elevation greater than 100 µV is defined as the clinical threshold level in the frontal plane. Compared with the SLL system, the MLL system had an influence in the STa, as the values of STa reduced in all the modified leads (I-aVF) for (J+0 ms) and (J+80 ms) which are found to be well within the clinical limits. Increased values of STa in modified lead aVF for J+20 ms, J+40 ms, J+60 ms were found and all are within the normal clinical limits. The plot of mean±SE of ST (J) wave amplitudes in MLL and SLL recordings are shown in Figure 6. The ST segment amplitude between the values of the modified and standard position is shown in Table 3 and the mean values are listed for the difference between the modified and standard lead (M-S) in which positive value indicates an increase and a negative value indicates a decrease caused by the modification.
Figure 6.
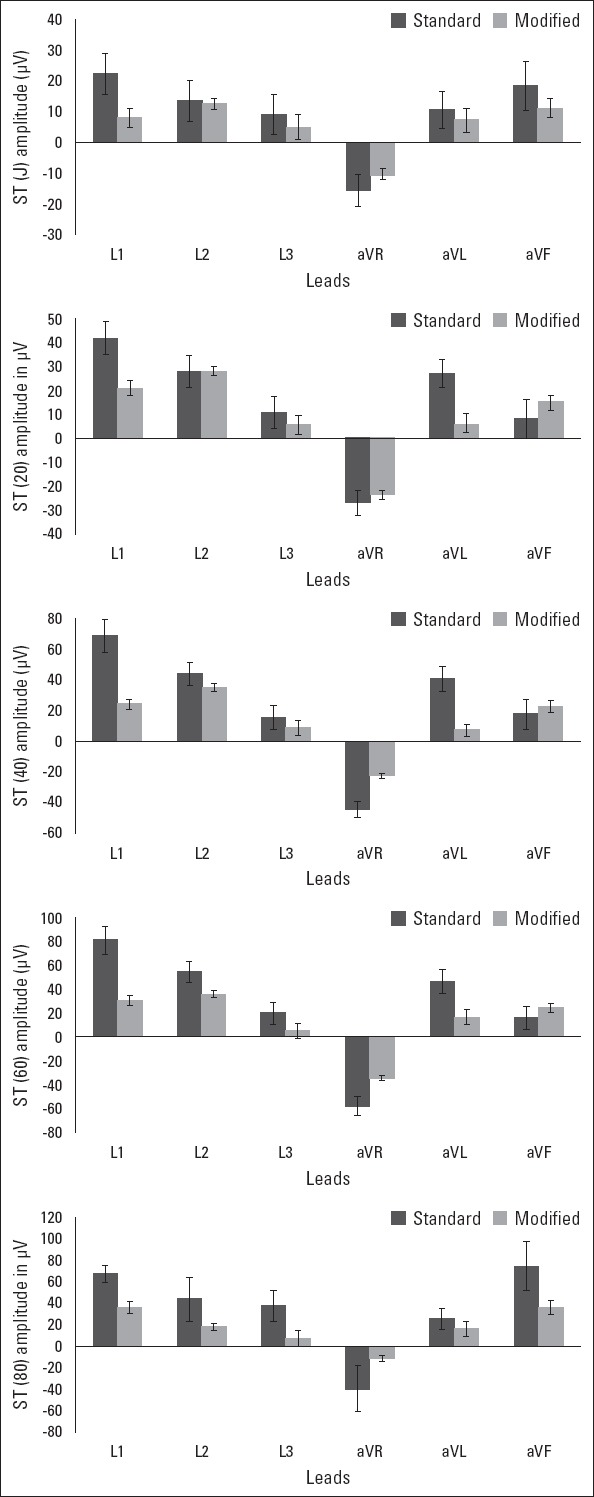
Plot of mean±SE of STa [J + ST (80)] of the frontal plane leads in the standard and the modified electrode positions
Table 3.
STa with the standard and modification of the limb electrode positions. Mean values are listed for the difference (M-S) in which positive values indicate an increase in amplitude and negative values indicate a decrease caused by modification. Percentage gains in mean amplitudes are also provided. Amplitudes are in microvolts
| Measurement | Leads | Standard position (SLL) | Modified position (MLL) | Modified–Standard position (% change) | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | % | ||
| ST(J) amplitude | I | 22 | 12 | 8 | 5 | -14 | -64 |
| II | 13 | 8 | 11 | 7 | -2 | -15 | |
| III | 9 | 5 | 5 | 2 | -4 | -44 | |
| aVR | -16 | 11 | -11 | 9 | -5 | -31 | |
| aVL | 11 | 5 | 7 | 4 | -4 | -36 | |
| aVF | 18 | 10 | 11 | 7 | -8 | -44 | |
| ST (J+20) amplitude | I | 42 | 27 | 21 | 10 | -21 | -50 |
| II | 28 | 14 | 25 | 12 | -3 | -11 | |
| III | 11 | 6 | 6 | 3 | -5 | -45 | |
| aVR | -27 | 10 | -23 | 12 | -4 | -15 | |
| aVL | 27 | 13 | 7 | 5 | -20 | -74 | |
| aVF | 8 | 3 | 15 | 9 | 7 | 87 | |
| ST (J+40) amplitude | I | 69 | 44 | 24 | 14 | -45 | -65 |
| II | 44 | 30 | 35 | 10 | -9 | -20 | |
| III | 15 | 8 | 9 | 5 | -6 | -40 | |
| aVR | -45 | 22 | -23 | 7 | -22 | -49 | |
| aVL | 41 | 27 | 7 | 3 | -34 | -83 | |
| aVF | 18 | 9 | 23 | 11 | 5 | 28 | |
| ST (J+60) amplitude | I | 81 | 49 | 31 | 17 | -50 | -62 |
| II | 55 | 35 | 36 | 11 | -19 | -34 | |
| III | 20 | 11 | 5 | 2 | -15 | -75 | |
| aVR | -58 | 33 | -34 | 9 | -24 | -41 | |
| aVL | 47 | 32 | 17 | 10 | -30 | -64 | |
| aVF | 16 | 9 | 25 | 11 | 9 | 56 | |
| ST (J+80) amplitude | I | 67 | 34 | 36 | 22 | -31 | -46 |
| II | 43 | 21 | 17 | 9 | -16 | -37 | |
| III | 37 | 19 | 7 | 4 | -30 | -81 | |
| aVR | -40 | 23 | -12 | 5 | -28 | -70 | |
| aVL | 25 | 13 | 16 | 11 | -9 | -36 | |
| aVF | 74 | 37 | 36 | 20 | -38 | -51 | |
MLL - modified limb lead; SD - standard deviation; SLL - standard limb lead; values are in microvolts
Temporal changes in PR interval, QRS complex, and QT interval
As expected the MLL system has no effect on the temporal aspects of the ECG waveform as shown in Table 4.
Table 4.
Modification produced no measurable temporal changes in the ECG waveform in all frontal planes
| ECG intervals | Standard limb lead (SLL) ECG | Modified limb lead (MLL) ECG | P* | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | Range | Mean | SD | Range | ||
| PR Interval | 160.16 | 9.76 | 140 to 176 | 161.16 | 8.76 | 144 to 177 | >0.05 |
| QRS wave | 94.38 | 8.71 | 78 to 109 | 92.98 | 9.23 | 78 to 106 | >0.05 |
| QT Interval | 341.23 | 21.36 | 302 to 380 | 344.57 | 19.98 | 302 to 388 | >0.05 |
SD - standard deviation; values are in miliseconds;
Paired sample t-test
Discussion
In this present study, the authors sought to investigate the changes in ECG wave amplitudes and deviations in the frontal plane axis for the MLL system which was originally designed to facilitate the study of atrial P and Ta waves in healthy male subjects and with a view to study the dynamics of Ta wave in patients with AV block. During this investigation, the authors found that the MLL system placed on the torso of the sinus rhythm subjects produced profound changes in the ECG wave amplitudes, STa and deviations in the frontal plane axis. The waveform changes are associated with modified limb electrode with a more vertical, rightward, and leftward shift of the QRS frontal plane axis. The deviation in the frontal plane axis had the R wave, S wave, and T wave amplitude decrease in all the frontal plane leads. As the limb electrodes are moved over the chest, the ECG wave amplitudes, STa and deviations in the frontal plane axis changes were seen predominantly.
Rautaharju et al. (27) showed that limb electrodes, placed over the chest, even produced changes in the transverse plane leads that are statistically significant but this is not evident in this study. Sheppard et al. (19) studied that the Takuma electrode modification did produce ECG wave amplitude and frontal plane axis changes, which are statistically significant but not clinically significant by comparing with the guidelines of the clinical thresholds for normality (25, 26, 28). The present study is in agreement with Sheppard et al. (19) with few exceptions, in the frontal plane QRS axis deviations and R wave amplitude changes which are clinically significant and above the clinical threshold for normality.
The ST segment is used as a key indicator of myocardial ischemia during exercise stress testing and emergency monitoring. In this study, it was found that the MLL system did not alter the STa values in any of the modified leads which were analyzed. The STa deviations were analyzed for each 20 ms after the onset of the J point to (J+80 ms) and all the values are found to be within the normal clinical limits.
In the present study, the deviations in frontal plane axis is investigated in 60 sinus rhythm subjects and found that only 6 subjects exhibited normal QRS axis shift. Marked left axis deviation were seen in 41 subjects, marked right axis deviation in 12 subjects, and moderate right axis deviation in 1 subject, which is in the range of clinical threshold of abnormality. This result is in contrast to all the previous study done on the modification. In this study, the deviations in the QRS axis produced false-positive ECG changes in frontal plane axis, which would lead to false interpretation of heart diseases.
In previous studies it has been asserted that variations in ECGs obtained with modified limb electrode do not affect diagnostic interpretation (4–6). This is not true in the present study, as the frontal plane QRS axis shift in 54 sinus rhythm subjects and R wave amplitude changes in modified Lead I of all the 60 sinus rhythm subjects would lead to false interpretation of heart disease and it would develop “heart disease of electrocardiographic origin” termed by Prinzmetal et al. (29). Such abnormalities may generate unnecessary investigations.
Study limitations
The results of the present study are valid only for resting, supine sinus rhythm male subjects. No female subjects were included in this study. We have not yet studied the patients with known and unknown abnormalities to test whether the modification in the electrode placement alters the clinical sensitivity.
Conclusion
Finally, we show that the MLL system, used in this study, produces profound changes in ECG wave amplitudes, STa, and deviations in QRS and T wave axis in the frontal plane leads. We have quantified that the changes in ECG wave amplitudes, STa and deviations in QRS and T wave axis, produced by the MLL system shows that many remains within the clinical limits with few exceptions. In this study, the modification does alter the clini- cal specificity of the standard ECG to some extent in the frontal plane QRS axis and R wave amplitude in modified lead I thus producing false-positive ECG changes in sinus rhythm subjects.
Acknowledgements:
One of the authors would like to thank the fund from the DST-FIST, Govt of India, vide Ref.: SR/FST/College-189/2013, Dated: 6th August 2014.
Footnotes
Conflict of interest: None declared.
Peer-review: Externally peer-reviewed.
Authorship contributions: Concept – S.J.; Design – S.J.; Supervision – V.S., R.P., R.M.S.; Fundings – S.J., V.S., R.P.; Materials – S.J., V.S., J.J., R.M.S.; Data collection &/or processing – S.J., V.S., R.M.S., J.J.; Analysis &/or interpretation – S.J., R.M.S., J.J.; Literature search – S.J., V.S., R.P., J.J.; Writing – S.J., V.S., J.J.; Critical review – S.J., V.S., R.P., R.M.S., J.J.; Other – S.J.

From Handan Yörükçü’s collections
References
- 1.Einthoven W. The different forms of the human electrocardiogram and their signification. Lancet. 1912;1:853–61. [Google Scholar]
- 2.Barnes AR, Pardee HEB, White PD, Wilson FN, Wolferth CC. Standardization of precordial leads - Supplementary report. Am Heart J. 1938;15:235–9. [Google Scholar]
- 3.Webster JG. Reducing motion artifacts and interference in biopotential recording. IEEE Trans Biomed Eng. 1984;31:823–6. doi: 10.1109/TBME.1984.325244. [DOI] [PubMed] [Google Scholar]
- 4.Diamond D, Griffith DH, Greenberg ML, Carleton RA. Torso mounted electrocardiographic electrodes for routine clinical electrocardiography. J Electrocardiol. 1979;12:403–6. doi: 10.1016/s0022-0736(79)80010-2. [DOI] [PubMed] [Google Scholar]
- 5.Mason RE, Likar I. A new system of multiple-lead exercise electrocardiography. Am Heart J. 1966;71:196–205. doi: 10.1016/0002-8703(66)90182-7. [DOI] [PubMed] [Google Scholar]
- 6.Edenbrandt L, Pahlm O, Sornmo L. An accurate exercise lead system for bicycle ergometer tests. Eur Heart J. 1989;10:268–72. doi: 10.1093/oxfordjournals.eurheartj.a059475. [DOI] [PubMed] [Google Scholar]
- 7.Sevilla DC, Dohrmann ML, Somelofski CA, Wawrzynski RP, Wagner NB, Wagner GS. Invalidation of the resting electrocardiogram obtained via exercise electrode sites as a standard 12-lead recording. Am J Cardiol. 1989;63:35–9. doi: 10.1016/0002-9149(89)91072-2. [DOI] [PubMed] [Google Scholar]
- 8.Krucoff MW, Loeffler KA, Haisty WK, Jr, Pope JE, Sawchak ST, Wagner GS, et al. Simultaneous ST-segment measurements using standard and monitoring-compatible torso limb lead placements at rest and during coronary occlusion. Am J Cardiol. 1994;74:997–1001. doi: 10.1016/0002-9149(94)90847-8. [DOI] [PubMed] [Google Scholar]
- 9.Takuma K, Hori S, Sasaki J, Shinozawa Y, Yoshikawa T, Handa S, et al. An alternative limb lead system for electrocardiographs in emergency patients. Am J Emerg Med. 1995;13:514–7. doi: 10.1016/0735-6757(95)90160-4. [DOI] [PubMed] [Google Scholar]
- 10.Gamble P, McManus H, Jensen D, Froelicher V. A comparison of the standard 12-lead electrocardiogram to exercise electrode placements. Chest. 1984;85:616–22. doi: 10.1378/chest.85.5.616. [DOI] [PubMed] [Google Scholar]
- 11.Jowett NI, Turner AM, Cole A, Jones PA. Modified electrode placement must be recorded when performing 12-lead electrocardiograms. Postgrad Med J. 2005;81:122–5. doi: 10.1136/pgmj.2004.021204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kleiner JP, Nelson WP, Boland MJ. 12-lead electrocardiogram in exercise testing. A misleading baseline? Arch Intern Med. 1978;138:1572–3. [PubMed] [Google Scholar]
- 13.Pahlm O, Haisty WK, Jr, Edenbrandt L, Wagner NB, Sevilla DC, Selvester RH, et al. Evaluation of changes in standard electrocardiographic QRS waveforms recorded from activity-compatible proximal limb lead positions. Am J Cardiol. 1992;69:253–7. doi: 10.1016/0002-9149(92)91315-u. [DOI] [PubMed] [Google Scholar]
- 14.Papouchado M, Walker PR, James MA, Clarke LM. Fundamental differences between the standard 12-lead electrocardiograph and the modified (Mason- Likar) exercise lead system. Eur Heart J. 1987;8:725–33. doi: 10.1093/eurheartj/8.7.725. [DOI] [PubMed] [Google Scholar]
- 15.Wiens RD, Chaitman BR. An alternate limb lead system for electrocardiograms in emergency patients. Am J Emerg Med. 1997;15:94–5. doi: 10.1016/s0735-6757(97)90060-7. [DOI] [PubMed] [Google Scholar]
- 16.Harrigan RA, Chan TC, Brady WJ. Electrocardiographic electrode misplacement, misconnection, and artifact. J Emerg Med. 2012;43:1038–44. doi: 10.1016/j.jemermed.2012.02.024. [DOI] [PubMed] [Google Scholar]
- 17.Anter E, Frankel DS, Marchlinski FE, Dixit S. Effect of electrocardiographic lead placement on localization of outflow tract tachycardias. Heart Rhythm. 2012;9:697–703. doi: 10.1016/j.hrthm.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 18.Tragardh-Johansson E, Welinder A, Pahlm O. Similarity of ST and T waveforms of 12-lead electrocardiogram acquired from different monitoring electrode positions. J Electrocardiol. 2011;44:109–14. doi: 10.1016/j.jelectrocard.2010.11.012. [DOI] [PubMed] [Google Scholar]
- 19.Sheppard JP, Barker TA, Ranasinghe AM, Clutton-Brock TH, Frenneaux MP, Parkes MJ. Does modifying electrode placement of the 12 lead ECG matter in healthy subjects? Int J Cardiol. 2011;152:184–91. doi: 10.1016/j.ijcard.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 20.Szekely P. Chest leads for the demonstration of auricular activity. Br Heart J. 1944;6:238–46. doi: 10.1136/hrt.6.4.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sivaraman J, Uma G, Venkatesan S, Umapathy M, Dhandapani VE. A novel approach to determine atrial repolarization in electrocardiograms. J Electrocardiol. 2013;46:e1. [Google Scholar]
- 22.Sivaraman J, Uma G, Venkatesan S, Umapathy M, Ravi MS. Unmasking of atrial repolarization waves using a simple modified limb lead system. Anatol J Cardiol. 2015;15:605–10. doi: 10.5152/akd.2014.5695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sivaraman J, Uma G. Umapathy M. A. modified chest leads for minimization of ventricular activity in electrocardiograms. Proceedings of the International Conference on Biomedical Engineering. Vol. 2002. Penang, Malaysia: 2002. Feb 27-28, pp. 79–82. [Google Scholar]
- 24.Sivaraman J, Uma G, Venkatesan S, Umapathy M, Dhandapani VE. Normal limits of ECG measurements related to atrial activity using a modified limb lead system. Anatol J Cardiol. 2015;15:2–6. doi: 10.5152/akd.2014.5155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Surawicz B, Childers R, Deal BJ, Gettes LS, Bailey JJ, Gorgels A, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram part III:intraventricular conduction disturbances:a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology;the American College of Cardiology Foundation;and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009;53:976–81. doi: 10.1016/j.jacc.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 26.Rautaharju PM, Surawicz B, Gettes LS. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram part IV:the ST segment, T and U waves, and the QT interval. J Am Coll Cardiol. 2009;53:982–91. doi: 10.1016/j.jacc.2008.12.014. [DOI] [PubMed] [Google Scholar]
- 27.Rautaharju PM, Prineas RJ, Crow RS, Seale D, Furberg C. The effect of modified limb electrode positions on electrocardiographic wave amplitudes. J Electrocardiol. 1980;13:109–13. doi: 10.1016/s0022-0736(80)80040-9. [DOI] [PubMed] [Google Scholar]
- 28.Wagner GS, Macfarlane P, Wellens H, Josephson M, Gorgels A, Mirvis DM, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram part VI:acute ischemia/infarction. J Am Coll Cardiol. 2009;53:1003–11. doi: 10.1016/j.jacc.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 29.Prinzmetal M, Goldman A, Massumi RA, Rakita L, Schwartz L, Kennamer R, et al. Clinical implications of errors in electrocardiograp-hic interpretation:heart disease of electrocardiographic origin. J Am Med Assoc. 1956;161:138–43. doi: 10.1001/jama.1956.02970020018005. [DOI] [PubMed] [Google Scholar]