Abstract
Marital quality and social support satisfaction were tested as moderators of the association between maternal depressive symptoms and parenting during early childhood (18-36 months) among two large, divergent, longitudinal samples (n = 526; n = 570). Unexpectedly, in both samples the association between maternal depressive symptoms and reduced parenting quality was strongest in the context of high marital quality and high social support, and largely non-significant in the context of low marital quality and low social support. Possible explanations for these surprising findings are discussed. Results point to the importance of accounting for factors in the broader family context in predicting the association between depressive symptoms and maternal parenting.
Keywords: maternal depressive symptoms, parenting, marital quality, social support, family context
Maternal Depressive Symptoms and Parenting in Early Childhood: Contextual Influence of Marital Quality and Social Support in Two Samples
Maternal depressive symptoms have been consistently related to parenting. Mothers who are depressed tend to engage in higher levels of harsh, negative parenting and lower levels of positive, sensitive parenting compared to mothers who are not experiencing depressive symptoms (Lovejoy, Graczyk, O'Hare, & Neuman, 2000). ‘Positive parenting’ is an umbrella term used to refer to dimensions of parenting such as warmth, sensitivity, limit setting, appropriate scaffolding, and contingency-based reinforcement (Waller et al., 2015). ‘Negative parenting’, in turn, refers to parenting behaviors that are inconsistent, over-reactive, controlling, and, especially, harsh (Lovejoy et al., 2000). Parenting low in positivity and high in negativity has been linked to a variety of negative child outcomes, including lower levels of social competence, academic achievement, and emotion regulation abilities, and elevated levels of internalizing and externalizing behavior problems (Belsky & Fearon, 2002; Leerkes, Blankson, & O'Brien, 2009; Dishion et al., 2008). Advancing our understanding of the nature of the association between maternal depressive symptoms and parenting in early childhood is especially important because their associations with child outcomes tend to be stronger during this period compared to later in development (Goodman et al., 2011; Lovejoy et al., 2000).
In considering the impact of depression on parenting, however, it is important to take into account the broader context in which the parent-child relationship is embedded (e.g., Bronfenbrenner & Morris, 2007). Mothers’ relationships with significant others—whether these be friends, extended family, or a spouse—may influence the extent to which depressive symptoms negatively interfere with parenting. Additionally, the role of significant-other support may differ based on other familial contextual factors, such as socioeconomic status and single-parenthood (McLoyd, 2011; Mistry, Vandewater, Huston, & McLoyd, 2002). The current study explored the potential moderating role of marital quality and social support on the association between depressive symptoms and parenting among two divergent samples, both in terms of risk status and marital status.
Maternal Depression and Parenting Behavior
Maternal depression occurring in infancy and early childhood has an established association with a host of adverse child outcomes, including higher levels of general psychopathology, negative affect, and internalizing and externalizing behavior problems (Bagner, Pettit, Lewinsohn, & Seeley, 2010; Campbell et al., 2009; Goodman et al., 2011; Zahn-Waxler, Denham, Iannotti, & Cummings, 1992). As noted above, maternal depression has also been linked to maternal caregiving and parenting—the focus of the present study—and has been found to mediate associations between maternal depression and later child outcomes (e.g., NICHD ECCRN 1999), although maternal depression and parenting likely share a reciprocal relationship (Lagacé-Séguin & d'Entremont, 2006). As both clinical depression and elevated levels of depressive symptoms have been similarly linked to both child and parenting outcomes (e.g. Goodman, 2007; Lovejoy et al., 2000), the term ‘maternal depression’ will be used to refer either to clinical or subsyndromal depression.
Although maternal depression is consistently associated with less positive and more negative parenting, the strength of the association has been found to vary by child's age and the parenting dimension studied (Lovejoy et al., 2000). Additionally, effect sizes for the association of depression with parenting were stronger for mothers of infants compared to mothers of older children (d = .47 for infants vs. .19 for later childhood). Theoretically, maternal depression might have a greater effect on parenting and subsequent child behavior during early childhood relative to later developmental periods because of the greater physical and psychological demands of rearing infants and toddlers versus school-age children (Shaw & Bell, 1993). Therefore, advancing our understanding of what conditions might moderate the magnitude of the association between maternal depression and parenting in early childhood is important because of consistent associations between maternal depression and parenting and between parenting and child outcomes during early childhood, and because understanding the predictors of parenting during this time may also increase our ability to intervene with families. As significant variability exists in the relation between maternal depression and parenting across variations in children's developmental status, it is likely that other child and contextual factors moderate the strength of this association. The present study explored as moderators two related factors that have established direct associations with both depression and parenting: marital quality and social support satisfaction.
Maternal Depression and Parenting: Moderation by Marital Quality
As with all variables discussed in this study, marital quality and parenting likely share reciprocal relations (Kwok, Cheng, Chow, & Ling, 2015; Lavee, Sharlin, & Katz, 1996). As with maternal depression, impairments in marital quality are associated with adverse child outcomes, including internalizing and externalizing behavior problems and poor interpersonal relationships (Cummings & Davies, 1994; Katz & Woodin 2002). Most pertinent to this study, marital quality has also been found to be associated with both positive (Planalp, Braungrat-Rieker, Lickenbrock & Zentall, 2013) and negative (Rhoades et al., 2011) dimensions of parenting, often explained by the ‘spillover hypothesis’ (Easterbrooks, Cummings, & Emde, 1994). Although recent research has deepened our understanding of the spillover hypothesis by considering the impact of factors such as genetics, maternal personality, and child evocative effects (Ganiban et al., 2009; Harold et al., 2013), the basic premise is that the quality of parents’ romantic relationship impacts the way that they interact with and parent their children. The spillover hypotheses is supported by a meta-analysis of 68 studies, which found a moderate effect (d = .46) of marital quality on parent-child relationship quality (Erel & Burman, 1995). A variation of the spillover hypothesis may also apply to the effect of marital quality on mothers’ psychological functioning, as poor marital quality has been found to be subsequently associated with higher levels of maternal depression (Mamun et al., 2009).
Beyond establishing direct associations of marital quality on parenting and maternal depression, theory and empirical evidence also support the possibility that marital relationship quality may moderate the association between maternal depression and parenting. According to Belsky's (1984) process model, parenting is influenced by parent and infant characteristics, as well as the broader context in which the parent-child relationship is embedded. Consistent with Belsky's model, it is possible that mothers who have warm, supportive partners who are available to help maintain routine and regularity in the household, and perhaps serve as a model for positive parenting, may more likely prevent their depressive symptoms from spilling-over and adversely affecting their parenting behavior compared to mothers who feel less satisfied with their partner.
A small number of studies have examined interactive associations between parental depressive symptoms and marital functioning on both parenting and child outcomes among school-aged children (Davies, Sturge-Apple, & Cummings, 2004; Kouros, Papp, Goeke-Morey, & Cummings, 2014; Papp, Goeke-Morey, & Cummings, 2004). These studies examined depressive symptoms as moderators of the association between marital functioning and either parenting or child outcomes, with most—but not all—finding depressive symptoms to strengthen links from lower levels of marital quality to reduced parenting quality, parent-child relationship quality, and child adjustment. Still, this body of work is not conclusive, and more research is needed to understand the subtleties of the interactive relation between marital quality and parental depressive symptoms. The present study will examine relations among these variables in two independent samples during early childhood.
Maternal Depression and Parenting: Moderation by Social Support
In addition to support that mothers may receive from their spouses, mothers also receive other sources of support. Social support is generally thought to have three main components: emotional (e.g., encouragement, nurturance), informational (e.g., advice, useful information), and instrumental (e.g., financial assistance; Barnett, de Baca, Jordan, Tilley, & Ellis, 2015), and has been linked to both depressive symptoms and parenting. Mothers’ report of higher levels of social support is associated with lower levels of maternal depressive symptoms (Bost et al., 2002; Cairney et al., 2003), and this also has been found among low-income mothers (Jackson, 2000). Additionally, mothers’ perceptions of high social support have been associated with higher levels of parenting efficacy (Suzuki et al., 2009) and parenting quality (Ceballo & McLoyd, 2002). As with marital quality, little research has moved beyond exploring direct associations among these variables to testing whether perceptions of social support may interact with depressive symptoms in predicting parenting behavior.
Although research and theory suggest that low or high marital quality may moderate associations between depressive symptoms and parenting, many mothers do not have a spouse or long-term partner. This is especially the case in low-income families where rates of stable-partnering are relatively low (Trail & Karney, 2012). Because rates of depressive symptoms also tend to be higher among low-income families (Lorant et al., 2003) and single mothers (Cairney et al., 2003), we sought to extend our exploration of potential moderators of the association between depression and parenting quality in a manner consistent with the ecological context of many low-income families. Hence, we thought a broad-factor of social support would provide an ecologically-valid way of examining how qualities of support among important adults in low-income, single parents’ lives might moderate associations between maternal depression and parenting.
From a theoretical perspective and consistent with Belsky's (1984) model, it seems plausible that for mothers without a long-term partner, high levels of support from other sources (e.g., friends, neighbors, church group) may serve to buffer the impact that depressive symptoms have on parenting. Conversely, for mothers whose social support system is lacking, it may be more difficult to maintain positive parenting practices in the context of depressive symptoms, as these mothers may not only have fewer people available to provide assistance with childcare and household tasks, but also may not have adequate encouragement and support from close others. Further, it may be the case that social support serves a greater moderating influence among single compared to partnered mothers, as these women are not receiving support from a spouse. This is consistent with past research demonstrating that social support from friends and extended family may partially compensate for father absence in single-mother families (Hrdy, 2009; Jones et al., 2007; Jackson, 2000).
Present Study
As strong relations exist among maternal depressive symptoms, parenting, and child outcomes, especially during early childhood, exploration of the conditions under which maternal depressive symptoms are associated with more significant disruptions in parenting may increase our ability to reduce and prevent child emotional and behavioral problems. Although many established theories highlight the importance of context in terms of understanding parenting and child development (e.g., Belsky, 1984; Bronfenbrenner, 1986), little research has explored specific contextual factors that may moderate the association between depressive symptoms and parenting. Further, it remains unclear whether these moderating variables may operate differently among low- versus high-SES families.
Using data from two large, divergent, and longitudinal samples, the present study sought to examine whether marital quality and social support moderated the association between maternal depressive symptoms and both positive and negative parenting, and further, whether the patterns of interactions among these variables differed between a stable, relatively low-risk sample and a high-risk, low-income sample. Both data sets utilized similar (at times identical) measures of depressive symptoms, marital quality, social support, and parenting when children were between the ages of 18 and 48 months.
Based on theory and existing literature, we hypothesized: a) that among mothers who were married or in a committed relationship, marital quality would moderate the association between maternal depressive symptoms and parenting (higher negativity, lower positivity), such that high marital quality was expected to attenuate the magnitude of associations between depressive symptoms and both positive and negative parenting; b) that among mothers who were not married or in a live-in partnership, high levels of social support would—in line with marital quality—attenuate the magnitude of associations between depressive symptoms and both positive and negative parenting; and, c) that social support would more strongly moderate the association between depressive symptoms and parenting among single compared to partnered mothers.
Method
Participants and Procedures
Sample 1. Early Growth and Development Study (EGDS)
Participants were a subsample (n = 526; 94% of original 561; two-father families not included) of adoptive families recruited as part of two cohorts of the Early Growth and Development Study (EGDS), an ongoing, multisite, longitudinal sample of adopted children, adoptive parents, and birth parents (Leve et al., 2007). Recruitment of this sample took place from 2003 to 2010, through rolling enrollment at adoption agencies in the Mid-Atlantic, West/Southwest, and Pacific Northwest (N = 45 agencies in 15 states). Adoptive families in this sample were well-resourced. The majority of adoptive mothers were Caucasian (91.8%), with a mean age of 37.4 years (SD = 5.6 years) at the time of the child's birth. The median household income for adoptive parents was >$100,000 per year, and mothers were well-educated (78.8% college degree; 37% graduate degree). The majority of adoptive parents were married (91.1%) at the time of the child's birth. Just over half of adoptive children participating in the study were male (57.2 %). The majority of children were Caucasian (55.6%; Multi-racial =19.3%; African American = 13%; Latino = 10.9%). The median age of placement for adopted children was 2 days (M = 6.2, SD = 12.45; range = 0-91 days). Home assessments of adoptive parents and children occurred when children were 9, 18, and 27 months old, with data from the 18 and 27 month assessments utilized for the current study. During assessments, parents returned completed survey materials that had been mailed to them, participated in computer-assisted interviews, and engaged in a variety of interactions and standardized tasks with their infants. Assessments lasted from 2 to 4 hours, and were videotaped for later coding. See Leve at al., 2013 for additional details regarding study participants and methods.
Sample 2. Early Steps Multisite Study
Participants were drawn from the Early Steps Multisite Study (Dishion et al., 2008), a randomized controlled intervention trial of 731 families recruited from Women Infant and Children's Nutritional Supplement centers in and around Pittsburgh, PA (37% of families), Eugene, OR (37%), and Charlottesville, VA (26%). Children and their primary caregivers were recruited based on sociodemographic, family, and child risk factors between 2002 and 2003 when children were approximately 24 months old. Mothers and children in this sample were racially and ethnically diverse, with children belonging to the following racial groups: 27.9% African American, 50.1% Caucasian, 13.0% Biracial, and 8.9% other races (e.g., American Indian, Native Hawaiian), and more than two-thirds of the sample had an annual income of less than $20,000 at recruitment. Thirty-seven percent of mothers lived with their child's biological father; twenty-one percent reported they were single parents. Roughly half (49%) of children in this sample were female, and were a mean age of 29.9 months (SD = 3.2) at the time of the first assessment.
When children were between 24-35 months old (referred to as 30 months below for brevity) and again between 36-47 months (referred to as 42 months below for brevity), mothers, children, and alternate caregivers (when available) participated in a 2.5-hour home assessment. Alternate caregivers were adults identified by mothers as someone who regularly cared for the child. During assessments, caregivers completed questionnaires and participated in interactive tasks with their child. Families in this study were randomly assigned to participate in the Family Check-Up (FCU) intervention at the end of the 30-month assessment. As the intervention was not a focus of the present study, intervention status was included as a covariate in all analyses. See Dishion et al., 2008 for additional details regarding study participants and methods.
Measures
Depressive symptoms
Adoptive mothers in the EGDS sample completed the Beck Depression Inventory (BDI; Beck & Steer, 1993) during the 18-month assessment. Mothers rated the intensity with which they had experienced 20 depressive symptoms on a scale from 0-3 (internal consistency: α = .79 at 18 months). Adoptive mothers had a mean score or 3.81 (SD = 3.83) on the BDI at 18 months. As this is well below the cutoff score of 10 indicative of mild depression (Beck & Beamesderfer, 1974), adoptive mothers in this sample generally reported low levels of depressive symptoms.
At the 30-month assessment, mothers in the ES study completed the Center for Epidemiological Studies on Depression Scale (CES-D), a well-established measure of depressive symptoms (Radloff, 1977). Mothers used a 0-3 Likert scale to report on frequency of 20 depressive symptoms over the past week. Items were summed to create an overall depressive symptoms score (α = .76). The cutoff score for clinical depression based on the CES-D is 16, while the mean for mothers in this sample was 16.75 (SD = 10.66), indicating that this sample was experiencing moderate to severe depressive symptoms.
Relationship status
As all mothers in the EGDS study were in a relationship at the time of the child's birth, we did not need to determine relationship status in this sample. Among mothers in the ES sample, relationship status was assessed and computed based on mothers’ report of relationship status on the Locke-Wallace Marital Adjustment Test (LWMAT; described below) at ages 30 and 42 months, and on a demographic questionnaire administered at 30 months. To better facilitate comparisons between this sample and the EGDS sample (stably married mothers), mothers in this sample met the serious relationship criterion if they reported on the LWMAT that they were married or had a live-in partner at both the 30-month and 42-month assessments. Sixty-two percent of these mothers were married when their children were 30 months old. Because a subset of mothers in the study who reported they were single did not fill out the LWMAT, the 30-month demographic questionnaire was also used to assess relationship status. Mothers were classified as not in a serious relationship if they were not married and were not cohabitating when their child was 30 months old.
Marital quality
Mothers in the EGDS sample completed the Behavior Affective Rating Scale (Melby, Conger, Ge, & Warner, 1995) at 18 months to assess both marital hostility and marital warmth. Using a 7-point likert scale, both parents were asked to report how often in the last year their partner expressed certain emotions or behaviors. The hostility scale included items such as: ‘Get angry at you; Criticize you or your ideas; Insult or swear at you; Boss you around a lot.’ The warmth/support scale included items such as: ‘Listen carefully to your point of view; Help you do something that was important to you; Act loving and affectionate toward you.’ Each scale included 13 items (Mother Warmth α = .91, Mother Hostility α = .89; Father Warmth α = .92 Father Hostility α = .91). Adoptive mother and adoptive father scores were significantly correlated (Warmth/Support, r = .69, p < .01; Hostility, r = .66, p < .001). As scores on the warmth and hostility scales were significantly and negatively correlated (Mother, r = −.62, p <.001; Father, r = −.60, p <.001), warmth and hostility scores were aggregated with higher scores representing higher levels of warmth relative to hostility. Scores were then averaged by dyad to create a composite.
Mothers in the ES sample who were in a serious relationship (spouse or live-in partner) completed the short form of the LWMAT (Locke & Wallace, 1959) during the 42-month assessment as a measure of romantic relationship quality. For simplicity's sake, this measure will be referred to as marital quality, even though some mothers in this sample were not legally married. Mothers were asked to complete this measure regarding their relationship satisfaction with their partner over the previous year. The LWMAT uses Likert scales to assess marital happiness, disagreements, conflict resolution, engagement in shared interests, ability to confide in one's partner, and thoughts about ending the relationship. Consistent with extensive prior research using this measure (McEachern et al., 2013), items were standardized and then averaged such that higher scores indicated greater satisfaction with one's significant other during the past year (α = .87).
Social support satisfaction
Mothers in both studies completed the General Life Satisfaction Questionnaire (GLS; Crnic et al., 1984) to assess their satisfaction with perceived social support in three broad areas: intimate relationships, friendships, and neighborhood/community. Mothers used a 4-point scale to report on the frequency of support and participation in pleasant activities, and their level of satisfaction with each. This study used the “general life satisfaction” subscale, which averaged 8 items that asked about satisfaction with support in relationships, friendships, and the community. Mothers in the EGDS (α = .81) and ES (α = .74) samples completed the measure at 27 months and at 30 months, respectively.
Warm and harsh parenting
EGDS (parent report)
During the 27-month assessment, mothers and their partners filled out a questionnaire to measure mothers’ warmth and hostility toward her child (Iowa Youth and Families scales; Melby & Conger, 2001). Adoptive parents each completed the 9-item questionnaire by rating aspects of warmth (e.g., act loving and affectionate toward [child]; 4 items) and hostility (e.g., shout or yell at [child] because you were mad at him/her; 5 items) displayed toward the target child within the past month. Parents used a 7-point scale to respond to each question. Mothers and fathers both reported on mothers’ parenting (i.e., our measure of mothers’ parenting was comprised of both self-report and partner-report), and because they were significantly correlated (warmth, r = .90; hostility, r = .74), they were averaged to generate a composite (warmth, α = .93; hostility, α = .89).
ES (observed parenting)
A composite measure of positive parenting, maternal positive behavior support (PBS), at 42 months was created as a latent variable comprised of three different observational strategies (Dishion, Shaw et al, 2008). First, home visitors completed a modified version the infant/toddler home observation for measurement of the environment (IT-HOME; Bradley & Caldwell, 1984). This measure included ratings of maternal responsivity, acceptance, child involvement, social skills, and ratings of the home environment. Thirteen items were summed to create a directly observed positive behavior support subscale, which demonstrated satisfactory reliability (α = .76). Second, a team of undergraduates, blind to child and family data, coded videotaped family tasks using the relationship affect coding system (RACS; Peterson, Winter, Jabson, & Dishion, 2008), a micro-social coding system that captures the topography (verbal and physical behaviors) and affect (anger/disgust, validation, distress, positive affect, and ignore) within relationship behaviors. For the current study, the durations of positive and neutral engagement between mother and child were used to create a summary score that reflected positive behavior support. Reliability coefficients for RACS coding were in the “good” to “excellent” range with an overall kappa score of .93. Third, following micro-social (RACS) coding, coders completed a macro-social rating scale on the same videotaped interactions, using the coder impressions (COIMP) inventory (Dishion, Hogansen, Winter, & Jabson, 2004). This measure tapped items such as proactive parenting, structuring of the child's environment, parental warmth, positive parental reinforcement through praise, and displays of affection. Eleven items reflecting positive behavior support were summed to form a composite, showing good reliability (α = .84). A detailed description of the PBS construct can be found in Waller et al., 2015.
Observed maternal harsh parenting was derived from videotaped parent-child interactions at the 42-month home assessment. A composite index of harsh parenting was created using five items from the COIMP and three duration proportions from the Relationship Process Code (RPC; Jabson, Dishion, Gardner, & Burton, 2004). The COIMP items came from videotape coders’ ratings of mothers’ provision of developmentally-inappropriate reasons for children's behavior change, displays of anger or annoyance with the child, criticizing or blaming the child for family problems, use of physical discipline, ignoring/rejecting the child, and messages about the child's worthlessness (Moilanen et al., 2010). RPC codes included duration proportions of parental negative verbal, directive, and physical behavior. These individual items were standardized and summed to create the harsh parenting composite (α = .75).
Demographics
Basic demographic information collected from EGDS mothers at the initial 9-month assessment included child sex, parent age, openness of adoption, and obstetric complications, which were used as covariates in all analyses.
Demographic information collected from ES mothers at the 30-month assessment included child sex, child race and ethnicity, maternal educational attainment, and family income. As assessment site (Pittsburgh, Eugene, Charlotte) and race/ethnicity were confounded in this sample, we chose to covary by race and ethnicity as we felt this was a better approximation of family culture than was geographic location. Child gender, child minority status, child ethnicity (Hispanic v. non-Hispanic), and FCU intervention group status were included as dummy-coded covariates in all analyses, whereas family income and maternal educational attainment were included as continuous covariates. Income was rated on a scale from 1-13, with higher numbers representing higher annual household income (e.g., 1 = < $5,000; 4 = $15,000 to $19,999).
Data analytic plan
Analyses were conducted in Mplus Version 7.3 (Muthèn & Muthèn, 2011). Warm and harsh parenting were moderately correlated in both samples (EGDS, r = −.37; ES, r = −.30), and were examined as separate but correlated outcomes in all models. Thus, for each model, harsh and warm parenting at Time 2 were regressed on maternal depressive symptoms at Time 1, as was the given moderator variable (marital quality or social support) and the given interaction term (e.g., depressive symptoms * marital quality). Covariates were also regressed onto all model paths, resulting in fully-saturated models. Independent variables were centered in all analyses. In models testing the moderating effect of marital quality, we controlled for maternal social support to explore whether marital quality mattered above and beyond general support; similarly, in models testing the moderating effect of social support among partnered women, we controlled for marital quality. Significant interaction terms were probed by assessing the beta values of the interaction terms, and then plotting the interactions (without covariates) at the mean and one standard deviation above and below the mean, and examining the values of the simple slopes, as described in Cohen, Cohen, West & Aiken (2003).
Among mothers in the ES sample, separate models were run based on maternal relationship status, with moderation by marital quality tested only among mothers who were classified as being in a serious relationship (n = 275). Moderation by social support was tested separately both among this subsample and among mothers classified as not in a serious relationship (n = 295). To test the hypothesis that social support satisfaction would be a stronger moderator of the association between depressive symptoms and parenting for single compared to partnered women (hypothesis c), we collapsed all ES mothers into the same dataset, and created a dichotomous partnership term (single versus partnered). We first computed a model that included a social support*partnership status interaction term and the depression*social support interaction term previously described. We then added the three-way depression*partnership*social support interaction to test whether the interaction of social support and partnership was a significant moderator of the association between depressive symptoms and parenting.
Results
Descriptive Statistics
Descriptive statistics and bivariate correlations among EGDS and ES study variables are reported in Tables 1 and 2. Correlations among study variables were modest, in directions consistent with expectations based on prior literature (Ceballo & McLoyd, 2002; Lovejoy et al., 2000; Planalp et al., 2013; Rhodes et al., 2011). In the EGDS sample, maternal depressive symptoms, marital quality, and social support satisfaction were all correlated with both harsh and warm parenting at 27 months, in expected directions. In the ES sample, maternal depressive symptoms were negatively correlated with positive behavior support (PBS) as expected, but were not correlated with the harsh parenting measure. Marital quality was positively correlated with PBS, but not with harsh parenting. Finally, social support was negatively correlated with harsh parenting, but not with PBS.
Table 1.
Descriptive Statistics of Study Variables
| Measure | Time (months) | Range | Mean | SD |
|---|---|---|---|---|
| EGDS | ||||
| Adoptive mother BDI | 18 | 0-25 | 3.81 | 3.83 |
| Marital quality | 18 | −40.5-48.5 | 22.31 | 13.92 |
| Social support | 27 | 1.25-4 | 3.34 | .51 |
| Warm parenting | 27 | 16-28 | 25.55 | 2.42 |
| Harsh parenting | 27 | 5-19.5 | 8.68 | 2.47 |
| Maternal age | Birth | 23.73-55.08 | 37.43 | 5.60 |
| Obstetric complications | Birth | 0-6 | 2.22 | 1.31 |
| Adoption openness | Birth | −2.23-1.86 | .04 | .93 |
| Early Steps | ||||
| CES-D | 30 | 0-55 | 16.75 | 10.66 |
| Marital quality | 42 | 27-74 | 58.10 | 9.27 |
| Social support | 30 | 16-55 | 39.97 | 7.15 |
| Positive Behavior Support | 42 | −2.37-2.03 | .00 | .76 |
| Harsh parenting | 42 | −4.25-35.3 | .00 | 5.13 |
| Income | 30 | 1-9 | 3.59 | 1.77 |
| n | % of sample | ||
|---|---|---|---|
| Intervention status | Control Group = 0 | 293 | 49.9 |
| Intervention Group = 1 | 294 | 50.1 | |
| Parent education | Less than high school = 0 | 132 | 22.5 |
| High school or more = 1 | 455 | 77.5 | |
| Child race | Caucasian/Other = 0 | 362 | 61.7 |
| Black/biracial = 1 | 224 | 38.2 | |
| Child ethnicity | Non-Hispanic = 0 | 499 | 85 |
| Hispanic/Latino = 1 | 82 | 14 |
Note. BDI: Beck Depression Inventory; CES-D: Center for Epidemiologic Studies Depression Scale
Table 2.
Variable Correlations
| EGDS | Time (months) | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|---|
| 1. BDI | 18 | - | - | - | - | - | - | - | - |
| 2. Marital Quality | 18 | −.29** | - | - | - | - | - | - | - |
| 3. Social Support | 27 | −.26** | .31** | - | - | - | - | - | - |
| 4. Warm Parenting | 27 | −.14** | .19** | .21** | - | - | - | - | - |
| 5. Harsh Parenting | 27 | .23** | −.14** | −.15** | −.36** | - | - | - | - |
| 6. Child Gender | Birth | −.06 | .01 | .02 | .07 | −.05 | - | - | - |
| 7. Maternal Age | Birth | .05 | −.18** | −.16** | −.05 | −.06 | .01 | - | - |
| 8. Obstetric Complications | Birth | −.05 | −.10* | −.01 | .05 | −.07 | −.02 | .05 | - |
| 9. Adoption Openness | Birth | .10* | .00 | .07 | −.04 | −.12* | −.06 | .02 | .02 |
| ES | |||||||||
| 1. CES-D | 30 | - | - | - | - | ||||
| 2. Social Support | 30 | −.34** | - | - | - | ||||
| 3. Marital Quality | 30 | −.14** | .30** | - | - | ||||
| 4. PBS | 42 | −.12** | .08 | .12* | - | ||||
| 5. Harsh Parenting | 42 | .05 | −.09* | −.01 | −.31** | ||||
Note.
p < .05
p < .01
BDI: Beck Depression Inventory; CES-D: Center for Epidemiologic Studies Depression Scale; PBS: Positive Behavior Support.
Moderation by Marital Quality
Among EGDS mothers
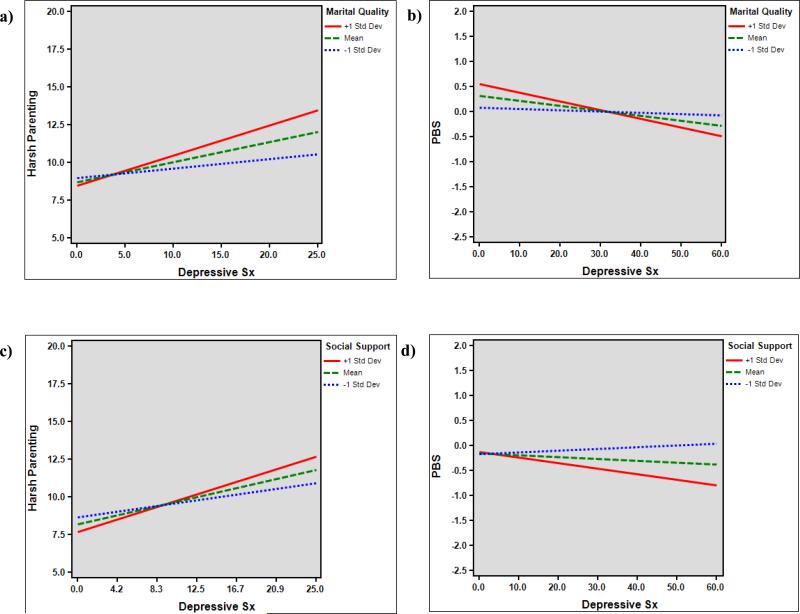
Coefficients for Model 1, testing the hypothesis that higher levels of marital quality would decrease the strength of the association between depressive symptoms and parenting among mothers in the EGDS sample, are presented in Table 3. Marital quality was not a significant moderator of the association between depressive symptoms and warm parenting from 18 to 27 months. It was, however, a significant moderator of the association between depressive symptoms and harsh parenting. Surprisingly, the direction of this moderation differed from our hypothesis—the association between maternal depressive symptoms and harsh parenting was strongest for mothers with higher levels of marital quality (B =.20, SE = .05 p < .001). For mothers with lower levels of marital quality, the association between depressive symptoms and harsh parenting was not significant (B = .06, SE = .04, p = .14; see Figure 1a).
Table 3.
Model 1, EGDS: Depressive symptoms (18 mo.) predicting warm parenting (27 mo.) and harsh parenting (27 mo.), moderated by marital quality (18 mo.).
| Warm Parenting | Harsh Parenting | |||
|---|---|---|---|---|
| B(SE) | β | B(SE) | β | |
| Child Sex | .29(.24) | .06 | −.27(.24) | −.06 |
| Obstetric | .13(.09) | .07 | −.12(.09) | −.06 |
| Mother Age | .00(.02) | .01 | −.06(.02)* | −.12 |
| Openness | −.07(.13) | −.03 | −.34(.13)* | −.12 |
| Social Support | .80(.26)** | .16 | −.77(.27)** | −.15 |
| BDI | −.02(.04) | −.03 | .11(.04)** | .16 |
| Marital Quality | .03(.01)** | .14 | −.02(.01)+ | −.10 |
| Interaction | .00(.00) | .01 | .01(.00)* | .12 |
| R-Squared | .08(.03)** | .12(.03)** | ||
Note.
p < .10
p < .05
p < .01
Obstetric: adoptive child obstetric complications; Interaction: BDI*Marital Quality.
Figure 1.
a) Depression (18 mo.) predicting harsh parenting (27 mo.) moderated by marital quality (18 mo.) among adoptive mothers (EGDS); b) depression (30 mo.) predicting Positive Behavior Support (42 mo.), moderated by marital quality (42 mo.) among low-income mothers in a serious relationship; c) depression (18 months) predicting harsh parenting (27 months) moderated (marginal) by social support satisfaction (27 months) among adoptive mothers (EGDS); (ES); d) depression (30 mo.) predicting Positive Behavior Support (42 mo.), moderated by social support satisfaction (30 mo.), among low-income mothers not in a serious relationship (ES).
Among ES mothers
When this model (Model 2) was tested among mothers in the ES sample who were in a serious relationship, marital quality was a significant moderator of the association between maternal depressive symptoms and PBS from 30 to 42 months (Table 4). Again, the direction of moderation differed from our original hypothesis—the association between maternal depressive symptoms and decreased PBS was strongest for mothers with higher levels of marital quality (B = −.02, SE = .0, p = .01), and was also significant for mothers at mean levels of marital quality (B = −.01, SE = .00, p < .05). For mothers with lower levels of marital quality, the association between depressive symptoms and PBS was not significant (B = .00, SE = .01, p = .82; see Figure 1b). Marital quality was not a significant moderator of the association between depressive symptoms and harsh parenting among mothers in the ES sample.
Table 4.
Model 2, Early Steps: Depressive symptoms (30 mo.) predicting Positive Behavior Support (42 mo.) and harsh parenting (42 mo.), moderated by marital quality (42 mo.).
| PBS | Harsh Parenting | |||
|---|---|---|---|---|
| B(SE) | β | B(SE) | β | |
| Intervention | .17(.08)* | .13 | .00(.56) | .00 |
| Child Sex | .06(.08) | .04 | .68(.56) | .08 |
| Education | .09(.04)* | .16 | −.30(.28) | −.09 |
| Income | .01(.03) | .03 | −.20(.17) | −.08 |
| Race | −.24(.11)* | −.15 | 2.31(.70)** | .22 |
| Ethnicity | .14(.11) | .09 | −.31(.92) | −.03 |
| Social Support | .00(.01) | .04 | −.02(.05) | −.03 |
| CES-D | −.01(.01)+ | −.13 | .05(.03) | .12 |
| Marital Quality | .01(.01)* | .15 | −.06(.04) | −.13 |
| Interaction | −.00(.00)* | −.14 | .00(.00) | .04 |
| R-Squared | .13(.04)** | .11(.04)** | ||
Note.
p < .10
p < .05
p < .01
Interaction: CES-D*Marital Quality.
Moderation by Social Support Satisfaction
Among EGDS mothers
Model 3 tested the hypothesis that higher levels of perceived social support would decrease the strength of the association between maternal depressive symptoms and parenting. Social support was not a significant moderator of the association between depressive symptoms and warm parenting from 18 to 27 months, but it was a marginally significant moderator of the association between depressive symptoms and harsh parenting (Table 5). Again, the direction of moderation differed from our hypothesis—the association between maternal depressive symptoms and harsh parenting was strongest for mothers with higher levels of social support satisfaction (B = .20, SE = .04, p < .001), and weakest for mothers with lower levels of social support satisfaction (B = .09, SE = .04, p < .05; see Figure 1c).
Table 5.
Model 3, EGDS: Depressive symptoms (18 mo.) predicting warm parenting (27 mo.) and harsh parenting (27 mo.), moderated by social support satisfaction (27 mo.).
| Warm Parenting | Harsh Parenting | |||
|---|---|---|---|---|
| B(SE) | β | B(SE) | β | |
| Child Sex | .29(.24) | .06 | −.14(.24) | −.05 |
| Obstetric | .13(.09) | .07 | −.11(.09) | −.06 |
| Mother Age | .00(.02) | .01 | −.05(.02)* | −.12 |
| Openness | −.08(.13) | −.03 | −.36(.13)** | −.13 |
| Marital Quality | .03(.01)** | .14 | −.02(.01)+ | −.10 |
| BDI | −.03(.04) | −.04 | .10(.04)** | .15 |
| Social Support | .85(.26)** | .17 | −.78(.27)** | −.16 |
| Intervention | −.04(.06) | −.04 | .09(.06)+ | .09 |
| R-Squared | .08(.03)** | .11(.03)** | ||
Note.
p < .10
p < .05
p < .01
Interaction: BDI*Support.
Among ES mothers
Among mothers in the ES sample who were in a serious relationship, social support satisfaction did not moderate associations between depressive symptoms and either warm or harsh parenting from 30 to 42 months (Model 4; Table 6). Among mothers in the ES sample who were not in a serious relationship, however, social support was a significant moderator of the association between depressive symptoms and PBS (Model 4; Table 7). The direction of moderation followed the same pattern as in previous analyses, with the strongest association between depressive symptoms and reduced PBS being found for mothers with higher reported levels of social support satisfaction (B = −.01, SE = .01, p = .09), and the weakest association between depressive symptoms and reduced PBS found for mothers with lower levels of social support satisfaction (B = .00, SE = .01, p = .53; see Figure 1d). Social support was not a significant moderator of the association between depressive symptoms and harsh parenting for this group of mothers.
Table 6.
Model 4, Early Steps: Depressive symptoms (30 mo.) predicting Positive Behavior Support (42 mo.) and harsh parenting (42 mo.), moderated by social support (42 mo.), among mothers in a serious relationship.
| PBS | Harsh Parenting | |||
|---|---|---|---|---|
| B(SE) | β | B(SE) | β | |
| Intervention | .16(.09)+ | .12 | −.12(.58) | −.02 |
| Child Sex | .06(.09) | .04 | .71(.56) | .09 |
| Education | .10(.04)* | .17 | −.29(.27) | −.09 |
| Income | .00(.03) | .01 | −.19(.17) | −.08 |
| Race | −.25(.11)* | −.15 | 2.32(.70)** | .22 |
| Ethnicity | .16(.11) | .10 | −.31(.91) | −.03 |
| Marital Quality | .01(.01)* | .14 | −.06(.04) | −.13 |
| CES-D | −.01(.01) | −.10 | .04(.03) | .11 |
| Social Support | .00(.01) | .03 | −.01(.05) | −.01 |
| Interaction | .00(.00) | .01 | −.00(.00) | −.07 |
| R-Squared | .11(.04)** | .12(.04)** | ||
Note.
p < .10
p < .05
p < .01
Interaction: CES-D*Support.
Table 7.
Model 5, Early Steps: Depressive symptoms (30 mo.) predicting Positive Behavior Support (42 mo.) and harsh parenting (42 mo.), moderated by social support (42 mo.), among mothers not in a serious relationship.
| PBS | Harsh Parenting | |||
|---|---|---|---|---|
| B(SE) | β | B(SE) | β | |
| Intervention | .04(.09) | .02 | 1.02(.65) | .10 |
| Child Sex | −.09(.09) | −.06 | 1.11(.64)+ | .11 |
| Education | .17(.04)** | .24 | −.24(.31) | −.05 |
| Income | .01(.03) | .02 | −.37(.22)+ | −.11 |
| Race | −.48(.10)** | −.31 | −.35(.68) | −.03 |
| Ethnicity | .01(.19) | .00 | −1.25(1.44) | −.06 |
| CES-D | −.00(.00) | −.03 | .00(.03) | .00 |
| Social Support | .01(.01) | .04 | .03(.05) | .05 |
| Interaction | −.00(.00)* | −.14 | .00(.00) | .02 |
| R-squared | .17(.04)** | .04(.02)+ | ||
Note.
p <.10
p < .05
p < .01
Interaction: CES-D*Support.
Prior to computing the three-way interaction model testing whether the moderating role of social support on the association between depressive symptoms and parenting differed as a function of partnership status, we examined the effects of the two two-way terms. The social support*depression term was not significant for either PBS (β = −.03; SE = .03, p > .10) or harsh parenting (β = −.01; SE = .04, p > .10), indicating that social support was not a significant moderator of the association between depression and parenting among the full sample. The social support*partnership term was not significant when PBS was the outcome (β = .04; SE = .05; p > .10). However, this interaction was significant when harsh parenting was the outcome (β = −.14; SE = .06, p < .05), indicating that social support was more strongly associated with harsh parenting among single—compared to partnered—women in this sample. These results were unchanged by the removal of the other two-way interaction term. The three-way (depression*partnership*social support*) interaction was not significant for either of the parenting variables, indicating that the moderating role of social support on the association between depression and parenting did not differ significantly as a function of partnership status (Table 8). Thus, although in prior analyses, social support emerged as a significant moderator among single, but not partnered, women in the ES sample, the null three-way interaction term indicated that these two effects were not significantly different from one another.
Table 8.
Three-way interaction results, Early Steps: moderating role of social support (42 mo.) on associations between depressive symptoms (30 mo.) and both Positive Behavior Support (42 mo.) and harsh parenting (42 months) among full sample.
| PBS | Harsh Parenting | |||
|---|---|---|---|---|
| B(SE) | β | B(SE) | β | |
| Intervention | .14(.06)* | .09 | .74(.42)+ | .07 |
| Child Sex | .02(.06) | .01 | 1.30(.42)** | .13 |
| Education | .15(.03)** | .22 | −.61(.21)** | −.13 |
| Income | .01(.02) | .02 | −.10(.13) | −.04 |
| Race | −.35(.07)** | −.22 | .17(.46) | .02 |
| Ethnicity | .21(.09)* | .09 | −1.51(.81)+ | −.10 |
| CES-D | −.00(.00) | −.03 | .00(.02) | .00 |
| Social Support | .00(.01) | .04 | .01(.05) | .02 |
| Partnership | .24(.07)** | .15 | −.75(.50) | −.07 |
| CES-D*SS | −.00(.00) | −.08 | −.00(.00) | −.01 |
| SS*Partnership | .00(.01) | .03 | −.15(.06)* | −.14 |
| Three-way | .00(.00) | .07 | .00(.01) | .00 |
| R-squared | .18(.03)** | .08(.02)** | ||
Note.
p <.10
p < .05
p < .01
SS: adoptive mother social support satisfaction; Partnership: single versus stably partnered; Three-way: CES-D*social support*partnership.
Discussion
This project is one of the first to test the potential moderating role of marital quality and social support on the association between depressive symptoms and parenting behavior in early childhood. Although maternal depression is relatively common among mothers of young children (Kessler, 2006; Shaw, Bell, & Gilliom, 2000) and has consistently been linked to impaired parenting (Lovejoy et al., 2000) and negative child outcomes (Goodman et al., 2011), surprisingly few studies have explored possible moderating factors of this relation (as exceptions, see Davies, Sturge-Apple, & Cummings, 2004; Engle & McElwain, 2013; Kouros, Papp, Goeke-Morey, & Cummings, 2014). In line with established theories that highlight the importance of contextual influences on parenting behaviors (e.g., Belsky, 1984; Bronfenbrenner, 1986), the present study sought to expand our understanding of the relation between maternal depressive symptoms and both positive and negative parenting. We predicted that among two divergent samples, maternal depressive symptoms would be less strongly associated with reductions in parenting quality in the context of high marital quality and in the context of high levels of social support satisfaction. Further, we predicted that social support satisfaction would play a more salient moderating role among mothers who were not in a serious relationship, and thus could not rely on a partner as a primary source of support.
Findings indicate that among mothers in the EGDS sample, marital quality was a significant moderator of the association between depressive symptoms and harsh parenting, while social support was a marginally significant moderator of this association. Among ES mothers who were married or cohabitating, marital quality was a significant moderator of the association between depressive symptoms and PBS, while the moderating effect of social support satisfaction differed based on the partnership status of mothers in this sample. Social support satisfaction was a significant moderator of the association between depressive symptoms and reduced PBS only among mothers who were not married or cohabitating. When the interactions were probed, however, the pattern of results was unexpected, yet largely consistent across both samples.
Moderation by Marital Quality
Among both a well-resourced sample of married, adoptive mothers, and a high-risk sample of mothers married or in a serious relationship, marital quality was a significant moderator of the association between depressive symptoms and parenting, such that in the context of high levels of marital quality, the association between depressive symptoms and reduced parenting quality was strongest. However, in the context of low levels of marital quality the association between depressive symptoms and reduced parenting quality was not significant. Specifically, in the lower-risk adoption sample, the association between depressive symptoms at 18 months and reported harsh parenting at 27 months was strongest for mothers with higher reported levels of marital quality. In the higher-risk ES sample, the association between depressive symptoms at 30 months and lower levels of observed positive parenting at 42 months was again strongest for mothers with higher reported levels of marital quality.
This pattern of results was unexpected, as marital quality has been found to have a positive association with parenting in prior literature (Planalp et al., 2013; Rhoades et al., 2011), and bivariate correlations in this study were also consistent with prior research, with marital quality being a significant negative predictor of harsh parenting and a significant positive predictor of warm parenting (Proulx, Helms, & Buehler, 2007). Interestingly, among the small body of literature that has explored interactive effects among depressive symptoms, marital quality, and parenting, Engle and McElwain (2013) also demonstrated results consistent with the present study, finding that maternal depressive symptoms when children were 4.5 years old were associated with less optimal parenting at age 6.5 only for mothers whose reported marital intimacy was moderate to high. For mothers who reported low levels of marital intimacy, the association between depressive symptoms and parenting was not significant. Thus, results from both Engle and McElwain and the present study suggest that the moderating effect of marital quality on the relation between maternal depressive symptoms and parenting is more complex than the direct paths from either marital quality or maternal depression to parenting. One possibility for this surprising finding is that when mothers in high-quality marital relationships experience depressive symptoms, they are willing and able to rely on their spouses to take over the majority of parenting responsibilities. Although this may benefit the child, these mothers are then less experienced at parenting when down and depressed, and may be less skillful at doing so, compared to depressed mothers who do not feel they can rely on their spouse, and must “push through” the depressive symptoms and parent their child anyway.
As an alternative explanation for this study's findings, it is possible that when fewer risk factors are present—as in the case of a mother in a high quality marriage—the impact of maternal depressive symptoms on parenting becomes more salient. When mothers are experiencing multiple risk factors, including depressive symptoms, poor marital quality, or financial strain, among others, the impact of an individual risk factor, such as depression, on parenting may be attenuated by other stressors in the mother's life. While outside the scope of the current project, models exploring moderation while accounting for risk factors at multiple levels may be necessary to test this hypothesis.
Moderation by Social Support
Many mothers of young children do not have a spouse, and this is especially the case among low-income families (Trail & Karney, 2012). As we wanted to extend our exploration of moderators of the association between depressive symptoms and parenting to be consistent with the ecological context of many low-income families, we re-computed our moderation analyses using a broad factor of social support quality. Our findings generally paralleled those reported for marital quality, again with a consistent, albeit unexpected, pattern of results.
Among low-income mothers who were not in a serious relationship, social support satisfaction moderated the association between maternal depressive symptoms at 24 months and positive parenting at 36 months, such that the strongest association between depressive symptoms and decreased positive parenting was evidenced for mothers reporting higher levels of social support, and the weakest association between depressive symptoms and decreased positive parenting was found for mothers with lower reported levels of social support. It is essential to note that formal statistical testing via a three-way interaction demonstrated that the moderating effect of social support among single women in this sample was not significantly different from the moderating role of social support among stably partnered mothers. Because of the scarcity of research on this topic and also because the pattern of moderation for social support among single women was consistent with other unexpected findings in our study, we believe it is worth mentioning, and will briefly theorize on this finding below. However, on the basis of the current study, it is not appropriate to conclude that social support is an especially important moderator of the association between depression and parenting for women who are not in committed relationships. Future research is necessary to understand this relation.
Theory and research indicate that social support among single-parent families, and especially among African-American families, often takes the form of friends and extended family members stepping in to provide direct care and support for children when no spouse is present to assist with childrearing (Murry et al., 2001). Therefore, it is possible that among these families, social support functions in a similar manner to marital quality, in that mothers who feel strongly supported by friends and family pass day-to-day parenting responsibilities to trusted others when they are feeling depressed, thus lessening their opportunities for learning to maintain high levels of parenting quality in the context of depressive symptoms. In line with this theory and the findings of the present study, Jackson (1998) found a moderating role of instrumental support on the association between depressive symptoms and maternal use of physical punishment among a sample of low-income, African American families. For mothers in this sample who were high on depression, greater instrumental support was associated with more frequent use of physical punishment, possibly because these mothers lacked practice resisting harsh parenting when they were experiencing depressive symptoms.
Among mothers in both samples who were married or in a serious relationship, social support satisfaction played a weak or non-significant role. For married mothers in the lower-risk adoptive sample (EGDS), while controlling for marital quality, social support was a marginally significant moderator of the association between depressive symptoms at 18 months and harsh parenting at 27 months, such that the association between depressive symptoms and harsh parenting was strongest for mothers with higher reported levels of social support satisfaction and weakest for mothers with lower reported levels of social support satisfaction. Especially based on the large number of participants in this sample, this marginal interaction should be interpreted with caution. However, as the pattern of results is consistent with our other significant moderation findings, we believe it is still worth noting. For mothers who were married or had a live-in partner in our high-risk sample (ES), social support satisfaction was not found to moderate the association between depressive symptoms and either positive or negative parenting. Again, it is important to recognize that formal statistical testing did not indicate differences in the strength of the moderating role of social support as a function of partnership. Still, it is possible that spouses provide a primary source of both emotional (e.g., encouragement, affection) and instrumental (e.g., childcare, household tasks) support for their partners, potentially reducing the salience of other forms of support.
Limitations and Future Directions
This study has a number of important strengths, such as testing a novel, theory-based hypothesis, utilizing two large, longitudinal samples; testing our research question among two distinctly different populations, thus increasing the generalizability of our findings; utilizing both observational and report measures of parenting; and taking a family systems perspective by considering child, adoptive mother, and birth mother characteristics as well as contextual influences. Still, there are limitations that should be considered.
First, although we were able to utilize both observational and report measures of our parenting outcome variable, we did not have both types of measures available for each sample. This makes differences in results between the two samples more difficult to interpret. Although the significant interactions that emerged were consistent across samples, increasing our confidence in their replicability, we found moderation of the association between depressive symptoms and higher negative parenting (but not lower positive parenting) in the EGDS sample, and moderation of the association between depressive symptoms and lower positive parenting (but not higher negative parenting) in the ES sample. This may be because of differences in the way that parenting was measured within each sample, or because of differences in normative parenting between the two samples. Among the well-resourced adoptive sample, where we would expect high levels of warm, positive parenting overall, we found a significant interaction for the less-normative parenting behavior, harsh parenting. Similarly, we may expect harsh, negative parenting to be more normative among our high-risk, low-income sample (Lansford, 2004), for which we found significant interactions for positive parenting. A related issue exists regarding our marital quality findings, as the measurement of marital quality was based on partner-report in the EGDS sample and self-report in the ES sample. Future research utilizing both observational and report measures of parenting across samples in early childhood would be helpful for parsing method from sample variance.
Second, the assessment timing of our constructs of interest was not equivalent across the two samples. Although maternal depressive symptoms at Time 1 (T1) always predicted parenting at Time 2 (T2), marital quality was measured at T1 in the EGDS sample and T2 in the ES sample; similarly, social support satisfaction was measured at T2 in the EGDS sample and T1 in the ES sample. Once again, this limitation impedes our ability to parse method from sample variance as it is possible that differences in moderation results between the two samples are because of differences in timing rather than differences in sample characteristics, such as risk-status. As an attempt to ameliorate this issue, we computed a post-hoc analysis testing whether marital quality at T1 would likewise moderate associations between depressive symptoms and parenting among partnered mothers in the ES sample. However, this interaction was not significant. Thus, the relationship between measurement timing and sample characteristics seems to be complex, and should be further explored in future research.
Third, the differences in timing among our moderator variables combined with the relative stability of maternal depressive symptoms and our inability to control for prior parenting limit our ability to make claims about temporal order. Thus, although in this manuscript depressive symptoms (T1) are the predictor variable and positive and harsh parenting (T2) are the outcome variables, methodological limitations necessitate that we focus on associations among our study variables, rather than directionality of effects. Future research utilizing transactional models of depressive symptoms and parenting behavior will be essential for establishing the directionality of the relation between these two variables across developmental time.
Fourth, in keeping with the majority of past literature, this study focused on depressive symptoms and parenting of mothers (Belsky & Barends, 2002). Past work has focused on mothers because women are more often primary caregivers, and also because of the higher rates of depression in women compared to men (Shaw et al, 2009). In line with Belsky (1984) and Bronfenbrenner (1986), this study sought to capture the larger context in which parenting takes place. However, fathers are clearly an important part of this context, and should not be ignored (Parke, 2000). Research has demonstrated significant associations between paternal depression and paternal parenting behavior (Wilson & Durbin, 2010), and recent research with the EGDS sample has found that even after controlling for the effects of maternal depressive symptoms, paternal depressive symptoms at 9 months were linked to higher levels of paternal harsh parenting at 18 months and higher levels of child externalizing symptoms at 27 months (Taraban et al., 2016). Future research, therefore, would greatly benefit from the inclusion of fathers, and as both samples used in this project have adequate data on fathers it presents a promising area for further exploration.
Finally, it is worth considering that although the adoption sample is low-risk in terms of typical markers, like income and educational and minority status, there are likely things about this sample that are unique to adoptive parents. These include factors like older parental age, higher levels of paternal investment in childrearing, and participation in the highly effortful adoption process, all of which may impact the way that parental and contextual influences interact with parenting. Thus, some differences in results between the two samples may not be due to differences in “risk status,” but due to differences in adoptive versus biological mothers and their perceptions of and interactions with their children.
Conclusions
Much research has been devoted to understanding relations between depressive symptoms and parenting behavior, but studies examining this relation in a larger ecological context have been relatively limited. The findings of the current study introduce the possibility that marital quality and social support, while being understood as protective factors for both depressive symptoms and parenting, may have a more complex and less clearly positive role when examined as moderators of the association between depressive symptoms and parenting. Among two very different samples and utilizing both observational and report measures, results of this study consistently indicated that high levels of both marital quality and social support are associated with the strongest relations between depressive symptoms and reduced parenting quality; low levels of marital quality and social support are associated with weak and non-significant relations between depressive symptoms and parenting. Results of this study point to the importance of accounting for larger family context in identifying mothers whose parenting is most likely to be negatively impacted by depressive symptoms. Further, these mothers may benefit from continued engagement in day-to-day parenting of their children, even when they have the option of relying on others to take over parenting responsibilities. Future work is necessary to understand this unexpected pattern of results and their impact on informing intervention with depressed mothers.
Acknowledgments
This project was supported by grant R01 HD042608 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development and the National Institute on Drug Abuse, NIH, U.S. PHS (PI Years 1–5: David Reiss, MD; PI Years 6–10: Leslie Leve, PhD). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health & Human Development or the National Institutes of Health. In addition, this project was supported by grant R01 DA020585 from the National Institute on Drug Abuse, the National Institute of Mental Health and OBSSR, NIH, U.S. PHS (PI: Jenae Neiderhiser, Ph.D.) and by grant R01 MH092118 from the National Institute of Mental Health, NIH, U.S. PHS (PIs: Jenae Neiderhiser, Ph.D. and Leslie Leve, Ph.D.).
Dr. Thomas J. Dishion is the developer of the Family Check-up intervention, but receives no monetary reimbursement for its use. We thank Dr. Aidan G.C. Wright for generously providing statistical consultation for this manuscript.
References
- Bagner DM, Pettit JW, Lewinsohn PM, Seeley JR. Effect of maternal depression on child behavior: A sensitive period? Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(7):699–707. doi: 10.1016/j.jaac.2010.03.012. doi: http://dx.doi.org/10.1097/00004583-201007000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett MA, de Baca TC, Jordan A, Tilley E, Ellis BJ. Associations among child perceptions of parenting support, maternal parenting efficacy and maternal depressive symptoms. Child & Youth Care Forum. 2015;44(1):17–32. doi:10.1007/s10567-008-0034-z. [Google Scholar]
- Beck AT, Beamesderfer A. Psychological measurements in psychopharmacology. S. Karger; Oxford: 1974. Assessment of depression: The depression inventory; p. 267. [Google Scholar]
- Beck AT, Steer RA, Beck JS, Newman CF. Hopelessness, depression, suicidal ideation, and clinical diagnosis of depression. Suicide and Life-Threatening Behavior. 1993;23(2):139–145. [PubMed] [Google Scholar]
- Belsky J. The Determinants of Parenting: A Process Model. Child Development. 1984;55(1):83–96. doi: 10.1111/j.1467-8624.1984.tb00275.x. doi:10.2307/1129836. [DOI] [PubMed] [Google Scholar]
- Belsky J, Barends N. Personality and parenting. Handbook of parenting: Vol. 3: Being and becoming a parent (2nd ed.) Lawrence Erlbaum Associates Publishers; Mahwah, NJ: 2002. pp. 415–438. [Google Scholar]
- Belsky J, Fearon RMP. Early attachment security, subsequent maternal sensitivity, and later child development: Does continuity in development depend upon continuity of caregiving? Attachment & Human Development. 2002;4(3):361–387. doi: 10.1080/14616730210167267. doi: http://dx.doi.org/10.1080/14616730210167267. [DOI] [PubMed] [Google Scholar]
- Bost KK, Cox MJ, Burchinal MR, Payne C. Structural and supporting changes in couples' family and friendship networks across the transition to parenthood. Journal of Marriage and Family. 2002;64(2):517–531. [Google Scholar]
- Bradley RH, Caldwell BM. The HOME Inventory and family demographics. Developmental Psychology. 1984;20(2):315–320. doi: http://dx.doi.org/10.1037/0012-1649.20.2.315. [Google Scholar]
- Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22(6):723–742. doi: http://dx.doi.org/10.1037/0012-1649.22.6.723. [Google Scholar]
- Bronfenbrenner U, Morris PA. The Bioecological Model of Human Development. Handbook of Child Psychology. John Wiley & Sons, Inc.; 2007. [Google Scholar]
- Cairney J, Boyle M, Offord DR, Racine Y. Stress, social support and depression in single and married mothers. Social Psychiatry and Psychiatric Epidemiology. 2003;38(8):442–449. doi: 10.1007/s00127-003-0661-0. doi: http://dx.doi.org/10.1007/s00127-003-0661-0. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Morgan-Lopez AA, Cox MJ, McLoyd VC. A latent class analysis of maternal depressive symptoms over 12 years and offspring adjustment in adolescence. Journal of Abnormal Psychology. 2009;118(3):479–493. doi: 10.1037/a0015923. doi: http://dx.doi.org/10.1037/a0015923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceballo R, McLoyd VC. Social support and parenting in poor, dangerous neighborhoods. Child Development. 2002;73(4):1310–1321. doi: 10.1111/1467-8624.00473. doi: http://dx.doi.org/10.1111/1467-8624.00473. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Lawrence Erlbaum Associates Publishers; Mahwah, NJ: 2003. [Google Scholar]
- Crnic KA, Greenberg MT, Robinson NM, Ragozin AS. Maternal stress and social support: Effects on the mother-infant relationship from birth to eighteen months. American Journal of Orthopsychiatry. 1984;54(2):224–235. doi: 10.1111/j.1939-0025.1984.tb01490.x. doi: http://dx.doi.org/10.1111/j.1939-0025.1984.tb01490.x. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Maternal depression and child development. Child Psychology & Psychiatry & Allied Disciplines. 1994;35(1):73–112. doi: 10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Davies PT, Sturge-Apple ML, Cummings EM. Interdependencies among interparental discord and parenting practices: The role of adult vulnerability and relationship perturbations. Development and Psychopathology. 2004;16(3):773–797. doi: http://dx.doi.org/10.1017/S0954579404004778. [PubMed] [Google Scholar]
- Dishion T, Hogansen J, Winter C, Jabson J. The coder impressions inventory. Child and Family Center; Eugene, OR: 2004. Unpublished manual. [Google Scholar]
- Dishion TJ, Shaw D, Connell A, Gardner F, Weaver C, Wilson M. The Family Check-Up with high-risk indigent families: Preventing problem behavior by increasing parents' positive behavior support in early childhood. Child Development. 2008;79(5):1395–1414. doi: 10.1111/j.1467-8624.2008.01195.x. doi: http://dx.doi.org/10.1111/j.1467-8624.2008.01195.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Easterbrooks MA, Cummings EM, Emde RN. Young children's responses to constructive marital disputes. Journal of Family Psychology. 1994;8(2):160–169. doi: http://dx.doi.org/10.1037/0893-3200.8.2.160. [Google Scholar]
- Engle JM, McElwain NL. Parental depressive symptoms and marital intimacy at 4.5 years: Joint contributions to mother–child and father–child interaction at 6.5 years. Developmental Psychology. 2013;49(12):2225–2235. doi: 10.1037/a0032450. doi:10.10170S0954579404004778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erel O, Burman B. Interrelatedness of marital relations and parent-child relations: A meta-analytic review. Psychological Bulletin. 1995;118(1):108–132. doi: 10.1037/0033-2909.118.1.108. doi: http://dx.doi.org/10.1037/0033-2909.118.1.108. [DOI] [PubMed] [Google Scholar]
- Ganiban JM, Ulbricht JA, Spotts EL, Lichtenstein P, Reiss D, Hansson K, Neiderhiser JM. Understanding the role of personality in explaining associations between marital quality and parenting. Journal of Family Psychology. 2009;23(5):646–660. doi: 10.1037/a0016091. doi: http://dx.doi.org/10.1037/a0016091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman SH. Depression in mothers. Annual Review of Clinical Psychology. 2007;3:107–135. doi: 10.1146/annurev.clinpsy.3.022806.091401. doi: http://dx.doi.org/10.1146/annurev.clinpsy.3.022806.091401. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review. 2011;14(1):1–27. doi: 10.1007/s10567-010-0080-1. doi: http://dx.doi.org/10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- Harold GT, Leve LD, Elam KK, Thapar A, Neiderhiser JM, Natsuaki MN, Reiss D. The nature of nurture: Disentangling passive genotype–environment correlation from family relationship influences on children's externalizing problems. Journal of Family Psychology. 2013;27(1):12–21. doi: 10.1037/a0031190. doi: http://dx.doi.org/10.1037/a0031190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hrdy SB. Mothers and others: The evolutionary origins of mutual understanding. Harvard University Press; Cambridge, MA: 2009. [Google Scholar]
- Jabson J, Dishion T, Gardner F, Burton J. Relationship Process Code v-2.0. training manual: A system for coding relationship interactions. Child and Family Center. 2004;160 [Google Scholar]
- Jackson AP. The role of social support in parenting for low-income, single, black mothers. The Social Service Review. 1998;72(3):365–378. [Google Scholar]
- Jackson AP, Brooks-Gunn J, Huang C-C, Glassman M. Single mothers in low-wage jobs: Financial strain, parenting, and preschoolers' outcomes. Child Development. 2000;71(5):1409–1423. doi: 10.1111/1467-8624.00236. doi: http://dx.doi.org/10.1111/1467-8624.00236. [DOI] [PubMed] [Google Scholar]
- Jones DJ, Zalot AA, Foster SE, Sterrett E, Chester C. A Review of Childrearing in African American Single Mother Families: The Relevance of a Coparenting Framework. Journal of Child and Family Studies. 2007;16(5):671–683. doi: http://dx.doi.org/10.1007/s10826-006-9115-0. [Google Scholar]
- Katz LF, Woodin EM. Hostility, hostile detachment, and conflict engagement in marriages: Effects on child and family functioning. Child Development. 2002;73(2):636–651. doi: 10.1111/1467-8624.00428. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The Epidemiology of Depression among Women. Cambridge University Press; New York, NY: 2006. [Google Scholar]
- Kouros CD, Papp LM, Goeke-Morey MC, Cummings EM. Spillover between marital quality and parent–child relationship quality: Parental depressive symptoms as moderators. Journal of Family Psychology. 2014;28(3):315–325. doi: 10.1037/a0036804. doi: http://dx.doi.org/10.1037/a0036804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwok SYCL, Cheng L, Chow BWY, Ling CCY. The spillover effect of parenting on marital satisfaction among Chinese mothers. Journal of Child and Family Studies. 2015;24(3):772–783. doi:10.1007/s1082601296661 . [Google Scholar]
- Lagacé-Séguin DG, d'Entremont M-RL. Less than optimal parenting strategies predict maternal low-level depression beyond that of child transgressions. Early Child Development and Care. 2006;176(3-4):343–355. doi: http://dx.doi.org/10.1080/03004430500040000. [Google Scholar]
- Lansford JE, Deater-Deckard K, Dodge KA, Bates JE, Pettit GS. Ethnic differences in the link between physical discipline and later adolescent externalizing behaviors. Journal of Child Psychology and Psychiatry. 2004;45(4):801–812. doi: 10.1111/j.1469-7610.2004.00273.x. doi: http://dx.doi.org/10.1111/j.1469-7610.2004.00273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavee Y, Sharlin S, Katz R. The effect of parenting stress on marital quality: An integrated mother–father model. Journal of Family Issues. 1996;17(1):114–135. doi: http://dx.doi.org/10.1177/019251396017001007. [Google Scholar]
- Leerkes EM, Blankson AN, O'Brien M. Differential effects of maternal sensitivity to infant distress and nondistress on social-emotional functioning. Child Development. 2009;80(3):762–775. doi: 10.1111/j.1467-8624.2009.01296.x. doi: http://dx.doi.org/10.1111/j.1467-8624.2009.01296.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Neiderhiser JM, Ge X, Scaramella LV, Conger RD, Reid JB, Reiss D. The Early Growth and Development Study: A prospective adoption design. Twin Research and Human Genetics. 2007;10(1):84–95. doi: 10.1375/twin.10.1.84. doi: http://dx.doi.org/10.1375/twin.10.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Neiderhiser JM, Shaw DS, Ganiban J, Natsuaki MN, Reiss D. The Early Growth and Development Study: A prospective adoption study from birth through middle childhood. Twin Research and Human Genetics. 2013;16(1):412–423. doi: 10.1017/thg.2012.126. doi:10.1111/j.1467-8624.2012.01859.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke HJ, Wallace KM. Short Marital-Adjustment and Prediction Tests: Their Reliability and Validity. Marriage and Family Living. 1959;21(3):251–255. doi:10.2307/348022. [Google Scholar]
- Lorant V, Kampfl D, Seghers A, Deliège D, Closon MC, Ansseau M. Socioeconomic differences in psychiatric in-patient care. Acta Psychiatrica Scandinavica. 2003;107(3):170–177. doi: 10.1034/j.1600-0447.2003.00071.x. doi: http://dx.doi.org/10.1034/j.1600-0447.2003.00071.x. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20(5):561–592. doi: 10.1016/s0272-7358(98)00100-7. doi: http://dx.doi.org/10.1016/S0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Mamun AA, Clavarino AM, Najman JM, Williams GM, O'Callaghan MJ, Bor W. Maternal depression and the quality of marital relationship: A 14-year prospective study. Journal of Women's Health. 2009;18(12):2023–2031. doi: 10.1089/jwh.2008.1050. doi: http://dx.doi.org/10.1089/jwh.2008.1050. [DOI] [PubMed] [Google Scholar]
- McEachern AD, Fosco GM, Dishion TJ, Shaw DS, Wilson MN, Gardner F. Collateral benefits of the family check-up in early childhood: Primary caregivers' social support and relationship satisfaction. Journal of Family Psychology. 2013;27(2):271–281. doi: 10.1037/a0031485. doi: http://dx.doi.org/10.1037/a0031485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLoyd V. How Money Matters for Children's Socioemotional Adjustment: Family Processes and Parental Investment. In: Carlo G, Crockett LJ, Carranza MA, editors. Health Disparities in Youth and Families. Vol. 57. Springer; New York: 2011. pp. 33–72. [DOI] [PubMed] [Google Scholar]
- Melby JN, Conger RD. The Iowa Family Interaction Rating Scales: Instrument summary. Lawrence Erlbaum Associates Publishers; Mahwah, NJ: 2001. pp. 33–58. [Google Scholar]
- Melby JN, Conger RD, Ge X, Warner TD. The use of structural equation modeling in assessing the quality of marital observations. Journal of Family Psychology. 1995;9(3):280–293. doi: http://dx.doi.org/10.1037/0893-3200.9.3.280. [Google Scholar]
- Mistry RS, Vandewater EA, Huston AC, McLoyd VC. Economic well-being and children's social adjustment: The role of family process in an ethnically diverse low-income sample. Child Development. 2002;73(3):935–951. doi: 10.1111/1467-8624.00448. doi: http://dx.doi.org/10.1111/1467-8624.00448. [DOI] [PubMed] [Google Scholar]
- Moilanen KL, Shaw DS, Dishion TJ, Gardner F, Wilson M. Predictors of longitudinal growth in inhibitory control in early childhood. Social Development. 2010;19(2):326–347. doi: 10.1111/j.1467-9507.2009.00536.x. doi: http://dx.doi.org/10.1111/j.1467-9507.2009.00536.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murry VM, Bynum MS, Brody GH, Willert A, Stephens D. African American Single Mothers and Children in Context: A Review of Studies on Risk and Resilience. Clinical Child and Family Psychology Review. 2001;4(2):133–155. doi: 10.1023/a:1011381114782. doi: http://dx.doi.org/10.1023/A:1011381114782. [DOI] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus user's guide. 2010. Vol. 6. Muthén & Muthén; Los Angeles, CA: 2011. [Google Scholar]
- Network NECR. Chronicity of maternal depressive symptoms, maternal sensitivity, and child functioning at 36 months. Developmental Psychology. 1999;35(5):1297–1310. doi: 10.1037//0012-1649.35.5.1297. doi: http://dx.doi.org/10.1037/0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- Papp LM, Goeke-Morey MC, Cummings EM. Mothers' and fathers' psychological symptoms and marital functioning: Examination of direct and interactive links with child adjustment. Journal of Child and Family Studies. 2004;13(4):469–482. doi: http://dx.doi.org/10.1023/B:JCFS.0000044728.34058.c0. [Google Scholar]
- Parke R. Father involvement. Marriage and Family Review. 2000;29(2):43–58. [Google Scholar]
- Peterson J, Winter C, Jabson J, Dishion T. University of Oregon, Child and Family Center; Eugene: 2008. Relationship affect coding system. Unpublished coding manual. [Google Scholar]
- Planalp EM, Braungart-Rieker JM, Lickenbrock DM, Zentall SR. Trajectories of parenting during infancy: The role of infant temperament and marital adjustment for mothers and fathers. Infancy. 2013;18(Suppl 1):E16–E45. doi: http://dx.doi.org/10.1111/infa.12021. [Google Scholar]
- Proulx CM, Helms HM, Buehler C. Marital quality and personal well-being: A meta-analysis. Journal of Marriage and Family. 2007;69(3):576–593. doi: http://dx.doi.org/10.1111/j.1741-3737.2007.00393.x. [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi: http://dx.doi.org/10.1177/014662167700100306. [Google Scholar]
- Rhoades KA, Leve LD, Harold GT, Neiderhiser JM, Shaw DS, Reiss D. Longitudinal pathways from marital hostility to child anger during toddlerhood: Genetic susceptibility and indirect effects via harsh parenting. Journal of Family Psychology. 2011;25(2):282–291. doi: 10.1037/a0022886. doi: http://dx.doi.org/10.1037/a0022886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw DS, Bell RQ. Developmental theories of parental contributors to antisocial behavior. Journal of Abnormal Child Psychology. 1993;21(5):493–518. doi: 10.1007/BF00916316. doi: http://dx.doi.org/10.1007/BF00916316. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Bell RQ, Gilliom M. A truly early starter model of antisocial behavior revisited. Clinical Child and Family Psychology Review. 2000;3(3):155–172. doi: 10.1023/a:1009599208790. doi: http://dx.doi.org/10.1023/A:1009599208790. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Connell A, Dishion TJ, Wilson MN, Gardner F. Improvements in maternal depression as a mediator of intervention effects on early childhood problem behavior. Development and Psychopathology. 2009;21(2):417–439. doi: 10.1017/S0954579409000236. doi: http://dx.doi.org/10.1017/S0954579409000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki S, Holloway SD, Yamamoto Y, Mindnich JD. Parenting self-efficacy and social support in Japan and the United States. Journal of Family Issues. 2009;30(11):1505–1526. doi: http://dx.doi.org/10.1177/0192513X09336830. [Google Scholar]
- Trail TE, Karney BR. What's (Not) Wrong With Low-Income Marriages. Journal of Marriage and Family. 2012;74(3):413–427. [Google Scholar]
- Waller R, Gardner F, Dishion T, Sitnick SL, Shaw DS, Winter CE, Wilson M. Early Parental Positive Behavior Support and Childhood Adjustment: Addressing Enduring Questions with New Methods. Social Development. 2015;24(2):304–322. doi: 10.1111/sode.12103. doi:10.1111/sode.12103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson S, Durbin CE. Effects of paternal depression on fathers' parenting behaviors: A meta-analytic review. Clinical Psychology Review. 2010;30(2):167–180. doi: 10.1016/j.cpr.2009.10.007. doi:10.1016/0272-7358(94)90047-7. [DOI] [PubMed] [Google Scholar]
- Zahn-Waxler C, Radke-Yarrow M, Wagner E, Chapman M. Development of concern for others. Developmental Psychology. 1992;28(1):126–136. doi: http://dx.doi.org/10.1037/0012-1649.28.1.126. [Google Scholar]