Abstract
Background
AIDS, caused by HIV, is a multisystem disease that affects hematopoiesis. The aim of this study was to assess cytopenias among HIV-infected children who had a follow-up at Felege Hiwot Referral Hospital, Bahir Dar, northwest Ethiopia.
Methods
An institution-based cross-sectional study was conducted between April and May 2013. Systematic random sampling method was used to select the study participants. Descriptive statistics, independent t-test as well as chi-square and logistic regression were used for analysis. A p-value <0.05 was considered as statistically significant.
Results
A total of 224 children (112 highly active antiretroviral therapy [HAART]-naïve and 112 HAART-experienced) participated in the study. The magnitude of anemia, thrombocytopenia, neutropenia, leukopenia and pancytopenia among HAART-naïve HIV-infected children were 30.4%, 9.8%, 8%, 4.5% and 1.8%, respectively. The overall prevalence of anemia, neutropenia, thrombocytopenia, leukopenia and pancytopenia were 29.5%, 8.9%, 8%, 4.5% and 1.4%, respectively. Cluster of differentiation-4 percentage and mean corpuscular volume were significantly different between HAART-experienced and HAART-naïve children. Being of younger age and severely immunosuppressed were risk factors of anemia.
Conclusion
Anemia was the most common cytopenia, followed by neutropenia. Severe immunosuppression and younger age were significantly associated with anemia. Therefore, emphasis should be given for investigation and management of cytopenias in HIV-infected children, particularly for those who are immunosuppressed and of younger age.
Keywords: anemia, children, cytopenia, HAART, HIV, leukopenia, neutropenia, pancytopenia, thrombocytopenia
Background
AIDS is caused by HIV and is characterized by progressive damage to the body’s immune system, which results in a number of OIs, immunological and hematological complications.1,2 Immunological complication due to CD4+ T-lymphocyte depletion is a hallmark of HIV infection.3 Hematological manifestations are among the most common clinicopathological manifestations of HIV infection, and they have been documented as the second most common cause of morbidity and mortality in HIV patients.4–6 These complications are generally marked with cytopenias and dysplasias of all major blood cell lines, leading to anemia, leukopenia, thrombocytopenia and neoplasms.7–9
Despite the attempts made to clearly understand the hematopoiesis impairment mechanism(s), it remained an intractable problem because of the paucity of studies using a suitable experimental animal model that closely replicates human hematopoiesis during an ongoing HIV infection in vivo.10 It has been evidenced that HIV-associated cytopenias seem to be dependent on the level of viral replication, OIs, liver cirrhosis, malignancies and the effects of the HAART used.11,12 Involvement of the hematopoietic system tends to be more severe in advanced stages of the disease.7,13 The incidence and severity of cytopenias are generally correlated to the stage of the disease. In addition, cytopenias can adversely affect ART outcomes and result in higher mortality.12,14–16 In HIV-infected children, cytopenias are the common problems.3,17–21 The pathophysiology of HIV-related cytopenias in childhood is not well understood, which may be due to the complicated and dynamic changes associated with normal hematological development in early life.18 The frequency and severity of cytopenias vary, while the disease progresses from the asymptomatic carrier state to advanced symptomatic stages. The frequencies of anemia, leukopenia and thrombocytopenia in asymptomatic HIV-infected children were 20%, 10% and 15%, respectively, while in HIV-infected children at the AIDS stage, their proportions were 70%, 65% and 40%, respectively.22
Even though the use of HAART reduces the rate of mortality, therapy-related potential adverse events are becoming the major concern in the era of HAART, particularly in resource-limited counties where undernutrition is common.23–26 Both HIV/AIDS and undernutrition affect immune function; HIV/AIDS, together with lack of essential micronutrients, leads to severe immune dysfunction. Furthermore, compromised immune status increases susceptibility to infectious diseases and profoundly complicates cytopenias and their management.27,28 A number of studies have been conducted on cytopenias among adult HIV-infected patients before and after the initiation of HAART. However, in HIV-infected children, limited data are available, and these are not much well elucidated, especially in developing countries. Moreover, there are controversial reports regarding the efficacy and impact of HAART in resolving immunological and hematological complication in HIV patients.29–31 Thus, this study was aimed to assess the cytopenias among HAART-naïve and HAART-experienced HIV-infected children.
Patients and methods
Study setting, population, sample size and sampling procedure
A cross-sectional study was conducted at Bahir Dar Felege Hiwot Referral Hospital, northwest Ethiopia, between April and May 2013. Felege Hiwot Referral Hospital is found in Bahir Dar, which is located 565 km away from Addis Ababa. Geographically, the city is located between 9°20′ and 14°20′ north latitudes and between 30°20′ and 40°20′ east longitudes and is at an altitude of 1,830 m above sea level. The hospital serves >5 million people and provides comprehensive health care services, including ART treatment and monitoring for both pediatric and adult people living with HIV/AIDS.
The study population comprised HIV-infected children who had been followed up at the Pediatric ART Clinic of Felege Hiwot Referral Hospital during the study period. HIV-infected children who were HAART-naïve and HAART-experienced for at least 6 months were eligible to be included in the study. Children who had been previously confirmed as having chronic renal failure and liver disease prior to HIV infection, as well as those who underwent radiation therapy and/or immunosuppressive chemotherapy in the previous 45 days, were excluded from the study due to the fact that these may unambiguously affect the hematological values.
For sample size determination, double population proportional formula was used by considering the following assumptions: 2-sided confidence level at 95%, power of 80% and 1:1 ratio of HAART-experienced:HAART-naïve children. We used a 21.9% prevalence rate of anemia for HAART-experienced children, as per a study conducted in Jimma, Ethiopia,32 and 40% for HAART-naïve children (a default value of OpenEpi) to get the maximum sample size. Then, a total of 224 HIV-infected children (112 HAART-naïve and 112 HAART-experienced for at least 6 months) were included in the study.
A systematic random sampling technique was used. On a daily basis, an average of 9 HAART-naïve and 12 HAART-experienced children were getting health care service in the Pediatric ART Clinic of Felege Hiwot Referral Hospital. A total of 840 HIV-infected children (360 HAART-naïve and 480 HAART-experienced) visited the ART clinic during the study period. Every third HAART-naïve HIV-infected child from the sequence of ART visitors was included in the study. Similarly, every fourth HAART-experienced HIV-infected child was included.
Data collection and laboratory analysis
Sociodemographic and socioeconomic characteristic of children and their caregivers were collected using a structured questionnaire via a face-to-face interview technique. Clinical data were collected by reviewing the medical records of HIV-infected children. The aforementioned data were collected by trained clinical nurses working in the Pediatric ART Clinic. Weight and height were measured, and the weight-for-age status and height-for-age status were scored from the child’s growth monitoring chart.
Venous blood (4 mL) was collected from each study participant using test tubes containing ethylenediaminetetraacetic acid following aseptic procedures. Part of the blood sample was analyzed using Cell DYN 1800 (Abbott Laboratories, Abbott Park, IL, USA) for the determination of hematological parameters, which include RBC parameters (RBC count, Hg level, MCH, MCHC, MCV and RDW%); WBC parameters (total WBC count, ANC, neutrophil percentage, lymphocyte count, lymphocyte percentage, mid count that encompasses eosinophil, basophil and monocyte and mid cell percentage) and platelet parameter (platelet count and MPV). The remaining blood sample was analyzed for the determination of CD4+ T-cell value using fluorescence-activated cell sorter counter (BD, San Jose, CA, USA). While doing all laboratory analyses, the standard operating procedure, daily maintenance, weekly maintenance and internal quality control procedure were strictly followed throughout the research process.
Assessment of cytopenias and immunological status
HIV-associated immunodeficiency was defined using the World Health Organization (WHO) age-related CD4 value stratification for HIV-infected infants and children.33 Mild immunodeficiency was defined as CD4% of 30% to <35% for infants <11 months, CD4% of 25% to <30% for children of age 12–35 months, CD4% of 20% to <25% for children aged 36–59 months and CD4 count of 350–499 cells/mm3 for children aged >5 years. Advanced immunodeficiency was defined as follows: CD4% of 25% to <30% for infants <11 months, CD4% of 20% to <25% for children aged 12–35 months, CD4% of 15% to <20% for children aged 36–59 months and CD4 count of 200–349 cells/mm3 for children aged >5 years. Severe immunodeficiency was also defined as follows: CD4% <25% for infants <11 months, 15% to <20% for children aged 12−35 months and <15% for children aged >3 years.33
Anemia was defined based on the WHO criteria after Hg has been adjusted for altitude and was stratified based on age (Hg <11.0 g/dL for children aged 6–59 months, Hg <11.5 g/dL for children aged 5–11 years and Hg <12.0 g/dL for children aged ≥12 years). Mild anemia was defined as follows: Hg 10.0–10.9 g/dL for children aged 5–59 months, 11.0–11.4 g/dL for children aged 5–11 years and 11.0–11.9 g/dL for children aged 12–14 years. Moderate anemia was defined as Hg 7.0–9.9 g/dL for children aged 5–59 months and 8–10.9 g/dL for children aged 5–14 years. Severe anemia was also defined as Hg <7.0 g/dL for children aged 6–59 months and <8.0 g/dL for those aged 5–14 years.34
Leukopenia was defined as a total WBC count <3,000 cells/mm3.9 Thrombocytopenia and thrombocytosis were defined as a platelet count <150,000/mm3 and platelet count >450 × 103 cells/mm3, respectively.32 Neutropenia was also defined as absolute neutrophil count of <1,000/mm3, and the severity has also been classified as mild, moderate and severe.32
Statistical analysis
Data were cleaned, sorted, categorized, coded and entered into Epi Info version 3.5.1. The data were transferred to SPSS version 20 for analysis. Descriptive statistics were obtained and the results are presented in Tables 1–6 and Figure 1. Normality of data was checked; and chi-square and independent t-tests were used to compare the mean hematological values between the HAART-naïve and HAART-experienced HIV-infected children. Bivariate logistic regression analyses were carried out for the cytopenias, and variables having p-value <0.2 in bivariate logistic analysis were included in the multivariable logistic analysis model to assess the association between cytopenias and explanatory variables. Odds ratios (ORs) with 95% CIs were used to measure the strength of the statistical associations. A p-value <0.05 was considered statistically significant.
Table 1.
Sociodemographic characteristics of caregivers/guardians and HIV-infected children at the Pediatric ART Clinic, Felege Hiwot Referral Hospital, Bahir Dar, northwest Ethiopia, 2013
| Characteristics | HAART-naïve | HAART-experienced | Total |
|---|---|---|---|
|
| |||
| n (%) | n (%) | N (%) | |
| Age of child, years | |||
| ≤5 | 32 (28.6) | 24 (21.4) | 56 (25) |
| 6–10 | 53 (47.3) | 53 (47.3) | 106 (47.3) |
| 11–14 | 27 (24.1) | 35 (31.2) | 62 (27.7) |
| Sex of child | |||
| Male | 67 (59.8) | 59 (52.7) | 126 (56.3) |
| Female | 45 (40.2) | 53 (47.3) | 98 (43.7) |
| Residence of child | |||
| Urban | 89 (79.5) | 91 (81.25) | 180 (80.4) |
| Rural | 23 (20.5) | 21 (18.75) | 44 (19.6) |
| Educational status of children | |||
| Nursery | 15 (13.4) | 9 (8) | 24 (10.7) |
| Kindergarten | 32 (28.6) | 26 (23.2) | 58 (25.9) |
| Primary school (1–4) | 51 (45.5) | 45 (40.2) | 96 (42.9) |
| Elementary (5–8) | 14 (12.5) | 32 (28.6) | 46 (20.5) |
| Whom the child lives with | |||
| Parents | 72 (64.3) | 71 (63.4) | 143 (63.8) |
| Father only | 7 (6.2) | 15 (13.4) | 22 (9.8) |
| Mother only | 23 (20.5) | 18 (16) | 41 (18.3) |
| Grandparents | 2 (1.8) | 2 (1.8) | 4 (1.8) |
| Guardian | 1 (0.9) | 1 (0.9) | 2 (0.9) |
| Relative | 5 (4.5) | 3 (2.7) | 8 (3.6) |
| Caregiver | 2 (1.8) | 2 (1.8) | 4 (1.8) |
| Parental status | |||
| Both alive | 73 (65.2) | 77 (68.7) | 150 (67) |
| Father dead | 18 (16.1) | 10 (8.9) | 28 (12.5) |
| Mother dead | 6 (5.3) | 16 (14.3) | 22 (9.8) |
| Separated | 8 (7.1) | 6 (5.4) | 14 (6.2) |
| Both mother and father dead | 7 (6.3) | 3 (2.7) | 10 (4.5) |
| Family size, n | |||
| ≤3 | 52 (46.4)) | 46 (41.1) | 98 (43.8) |
| 4–5 | 54 (48.2) | 54 (48.2) | 108 (48.2) |
| >5 | 6 (5.4) | 12 (10.7) | 18 (8) |
| Monthly family income, ETB | |||
| Lowest | 75 (67) | 82 (73.2) | 157 (70.1) |
| Middle | 36 (32.1) | 27 (24.1) | 63 (28.1) |
| High | 1 (0.9) | 3 (2.7) | 4 (1.8) |
| Caregiver’s educational status | |||
| Unable to read and write | 19 (17) | 42 (37.5) | 61 (27.2) |
| Able to read and write only | 22 (19.6) | 14 (12.5) | 36 (16.1) |
| Primary school | 18 (16.1) | 16 (14.3) | 34 (15.2) |
| High school | 23 (20.5) | 17 (15.2) | 40 (17.9) |
| Tertiary education | 30 (26.8) | 23 (20.5) | 53 (23.7) |
| Caregiver occupational status | |||
| Privately employed | 43 (38.4) | 44 (39.3) | 87 (38.8) |
| Government employed | 23 (20.5) | 35 (31.2) | 58 (25.9) |
| Merchant | 26 (23.2) | 16 (14.3) | 42 (18.8) |
| Farmer | 20 (17.9) | 17 (15.2) | 37 (16.5) |
Abbreviations: ART, antiretroviral treatment; ETB, Ethiopian Birr; HAART, highly active antiretroviral therapy; HIV, human immunodeficiency virus.
Table 2.
Medical characteristics of HIV-infected children at the Pediatric ART Clinic, Felege Hiwot Referral Hospital, Bahir Dar, northwest Ethiopia, 2013 (N=224)
| Clinical characteristic | HAART-naïve | HAART-experienced | Total |
|---|---|---|---|
|
| |||
| n (%) | n (%) | N (%) | |
| WHO staging | |||
| I | 64 (57.2) | 47 (41.9) | 111 (49.6) |
| II | 36 (32.1) | 32 (28.6) | 68 (30.3) |
| III | 12 (10.7) | 30 (26.8) | 42 (18.8) |
| IV | 0 | 3 (2.7) | 3 (1.3) |
| Immune status | |||
| Severe immunosuppression | 17 (15.2) | 23 (20.5) | 40 (17.9) |
| Advanced immunosuppression | 12 (10.7) | 17 (15.2) | 29 (12.9) |
| Mild immunosuppression | 40 (35.7) | 32 (28.6) | 72 (32.1) |
| Normal immune status | 43 (38.4) | 40 (37.7) | 83 (37.1) |
| Weight-for-age status | |||
| Underweight | 30 (26.8) | 44 (39.3) | 74 (33) |
| Normal | 82 (73.2) | 68 (60.7.) | 150 (67) |
| Height-for-age status | |||
| Stunted | 39 (34.8) | 31 (27.7) | 70 (31.3) |
| Normal | 73 (65.2) | 81 (72.3) | 154 (68.7) |
| OIs | |||
| Yes | 15 (13.4) | 10 (9) | 25 (11.2) |
| No | 97 (86.6) | 102 (91) | 212 (88.8) |
| Gastroenteritis | |||
| Yes | 6 (5.4) | 9 (8) | 15 (6.7) |
| No | 106 (94.6) | 103 (92) | 209 (93.3) |
| Pneumonia | |||
| Yes | 14 (12.5) | 10 (9) | 24 (10.7) |
| No | 98 (87.5) | 102 (91) | 200 (89.3) |
| Oral thrush | |||
| Yes | 9 (8) | 5 (4.5) | 14 (6.2) |
| No | 103 (92) | 107 (95.5) | 210 (93.8) |
| Skin rash | |||
| Yes | 16 (14.3) | 14 (12.5) | 30 (13.4) |
| No | 96 (85.7) | 98 (87.5) | 194 (86.4) |
| Fever | |||
| Yes | 19 (17) | 13 (11.6) | 32 (14.3) |
| No | 93 (83) | 99 (88.4) | 192 (85.7) |
| Presence of diarrhea | |||
| Yes | 15 (13.4) | 8 (7.1) | 23 (10.3) |
| No | 97 (86.6) | 104 (92.9) | 201 (89.7) |
| Kind of diarrhea | |||
| Acute | 8 (53.3) | 7 (87.5) | 15 (65.2) |
| Chronic | 7 (46.7) | 1 (12.5) | 8 (34. 8) |
Abbreviations: ART, antiretroviral treatment; HAART, highly active antiretroviral therapy; HIV, human immunodeficiency virus; OIs, opportunistic infections; WHO, World Health Organization.
Table 3.
Comparison of hematological profiles between HAART-naïve and HAART-experienced HIV-infected children at Pediatric ART Clinic of Felege Hiwot Referral Hospital in Bahir Dar, northwest Ethiopia, 2013 (N=224)
| Hematological values
| ||||
|---|---|---|---|---|
| Variables | HAART-naïve | HAART-experienced | Total | p-value |
|
| ||||
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Hg, g/dL | 13.25±3.03 | 13.21±1.60 | 13.23±2.41 | 0.936 |
| RBC, ×106/µL | 4.48±0.58 | 4.94±4.75 | 4.71±3.39 | 0.319 |
| HCT, % | 38.21±4.85 | 38.43±4.00 | 38.32±4.44 | 0.708 |
| MCV, fL | 86.67±13.17 | 90.10±11.6 | 87.88±12.59 | 0.008** |
| MCH, pg | 29.88±5.46 | 31.11±4.07 | 30.50±4.85 | 0.057 |
| MCHC, g/dL | 33.92±1.96 | 34.09±3.74 | 34.01±2.9 | 0.671 |
| RDW, % | 15.11±2.57 | 14.76±2.18 | 14.94±2.39 | 0.264 |
| WBC, ×103/µL | 8.18±3.32 | 8.01±3.26 | 8.09±3.29 | 0.708 |
| ANC, ×103/µL | 3.94±2.26 | 3.74±2.05 | 3.84±2.16 | 0.499 |
| Lymphocyte count, ×103/µL | 3.46±2.2 | 3.74±5.17 | 3.6±3.97 | 0.603 |
| Mid (absolute), ×103/µL | 1.34±1.7 | 2.21±8.10 | 1.76±5.77 | 0.247 |
| Neutrophil, % | 45.22±11.98 | 45.24±14 | 45.23±13.01 | 0.992 |
| Lymphocyte, % | 41.31±11.67 | 41.67±12.67 | 41.49±12.21 | 0.827 |
| Mid, % | 13.41±5.17 | 12.51±4.81 | 12.96±5 | 0.178 |
| PLT, ×103cells/µL | 297.91±107.67 | 300.99±105.10 | 299.45±06.16 | 0.829 |
| MPV, % | 9.72±1.92 | 9.82±7.96 | 9.77±5.77 | 0.899 |
| CD4, cells/µL | 873.16±466.53 | 767.86±486.60 | 820.51±78.52 | 0.100 |
| CD4, % | 28.73±14.22 | 24.78±10.69 | 26.73±12.71 | 0.018* |
Note:
Significant at p<0.05;
significant at p<0.01 by independent t-test analysis.
Abbreviations: ANC, absolute neutrophil count; ART, antiretroviral treatment; CD4, cluster of differentiation-4; HAART, highly active antiretroviral therapy; HCT, hematocrit; HIV, human immunodeficiency virus; Hg, hemoglobin; MCH, mean corpuscular hemoglobin; MCHC, mean corpuscular hemoglobin concentration; MCV, mean corpuscular volume; mid, mixed cell; MPV, mean platelet volume; PLT, platelets; RBC, red blood cell; RDW, red cell distribution width; SD, standard deviation; WBC, white blood cell.
Table 4.
Cytopenias with regard to immune status of HIV-infected children at Pediatric ART Clinic, Felege Hiwot Referral Hospital, Bahir Dar, northwest Ethiopia, 2013 (N=224)
| Cytopenic status | Immunosuppression
|
|||
|---|---|---|---|---|
| No (%) | Mild (%) | Advanced (%) | Severe (%) | |
| Anemic status | ||||
| Anemic | 23 (27.7) | 19 (26.4) | 5 (17.2) | 19 (47.5) |
| Nonanemic | 60 (72.3) | 53 (73.6) | 24 (82.8) | 21 (42.5) |
| Leukopenic status | ||||
| Leukopenic | 7 (8.4) | 3 (4.2) | 0 | 0 |
| Nonleukopenic | 76 (91.6) | 69 (95.8) | 29 (100) | 40 (100) |
| Neutropenic status | ||||
| Neutropenic | 10 (12) | 9 (12.5) | 0 | 1 (2.5) |
| Nonneutropenic | 73 (88) | 63 (87.5) | 29 (100) | 39 (97.5) |
| Thrombocytopenic status | ||||
| Thrombocytopenic | 7 (8.4) | 6 (8.3) | 1 (3.4) | 4 (10) |
| Nonthrombocytopenic | 76 (91.6) | 66 (91.7) | 28 (96.6) | 36 (90) |
Abbreviations: ART, antiretroviral treatment; HIV, human immunodeficiency virus.
Table 5.
Cytopenias and other hematologic abnormalities in HIV-infected children with respect to HAART status at Pediatric ART Clinic, Felege Hiwot Referral Hospital, Bahir Dar, northwest Ethiopia, 2013 (N=224)
| Variable | HAART status
|
Total (%) | p-value | |
|---|---|---|---|---|
| HAART-naïve (%) | HAART-experienced (%) | |||
| Anemic status | ||||
| Anemic | 34 (30.4) | 32 (28.6) | 66 (29.5) | 0.769 |
| Nonanemic | 78 (69.6) | 80 (71.4) | 158 (70.5) | – |
| Severity of anemia | ||||
| Mild | 16 (47.1) | 21 (65.6) | 37 (56.1) | 0.315# |
| Moderate | 17 (50) | 9 (28.1) | 26 (39.4) | – |
| Severe | 1 (2.9) | 2 (6.3) | 3 (4.5) | – |
| RBC size | ||||
| Microcytic RBC | 38 (33.9) | 18 (16.1) | 56 (25) | 0.016 |
| Normocytic RBC | 61 (54.5) | 76 (67.8) | 137 (61.2) | – |
| Macrocytic RBC | 13 (11.6) | 18 (16.1) | 31 (13.8) | – |
| RBC Hg content | ||||
| Hypochromic RBC | 28 (25) | 12 (10.7) | 40 (17.1) | – |
| Normochromic RBC | 75 (70) | 86 (75.8) | 161 (71.9) | 0.019 |
| Hyperchromic RBC | 9 (5) | 14 (12.5) | 23 (10.3) | – |
| Leukopenic status | ||||
| Leukopenic | 5 (4.5) | 5 (4.5) | 10 (4.5) | 0.63 |
| Nonleukopenic | 107 (95.5) | 107 (95.5) | 214 (95.5) | – |
| Neutropenic status | ||||
| Neutropenic | 9 (8) | 11 (9.8) | 20 (8.9) | 0.41 |
| Nonneutropenic | 103 (92) | 101 (90.2) | 104 (91.1) | – |
| Severity of neutropenia | ||||
| Mild | 8 (88.9) | 9 (81.8) | 17 (85) | 0.579# |
| Moderate | 1 (11.1) | 2 (18.2) | 3 (15) | – |
| Thrombocytopenic status | ||||
| Thrombocytosis | 8 (7.2) | 6 (5.3) | 14 (6.3) | 0.506 |
| Normal | 93 (83.0) | 99 (88.4) | 192 (85.7) | – |
| Thrombocytopenic | 11 (9.8) | 7 (6.3) | 18 (8) | – |
Note:
Analysis done by Fisher’s exact test.
Abbreviations: ART, antiretroviral treatment; HAART, highly active antiretroviral therapy; HIV, human immunodeficiency virus; Hg, hemoglobin; RBC, red blood cell.
Table 6.
Factors associated with anemia among HAART-naïve and HAART-experienced children at Pediatric ART Clinic, Felege Hiwot Referral Hospital, northwest Ethiopia, April–May 2013 (N=224)
| Variable | Anemic status
|
Total (%) | COR (95% CI) | p-value | AOR (95% CI) | p-value | |
|---|---|---|---|---|---|---|---|
| Anemic (%) | Nonanemic (%) | ||||||
| Age, years | |||||||
| <5 | 24 (42.9) | 32 (57.1) | 56 (25) | 4.42 (1.83–10.68) | 0.001 | 4.3 (1.7–10.9) | 0.002 |
| 6–10 | 33 (31.1) | 73 (68.9) | 106 (47.3) | 2.66 (1.18–6.03) | 0.019 | 3.1 (1.3–7.2) | 0.011 |
| 11–14 | 9 (14.5) | 53 (85.5) | 62 (27.7) | 1 | – | 1 | – |
| Gastroenteritis | |||||||
| Yes | 7 (53.8) | 6 (46.2) | 13 (5.9) | 3.01 (0.97–9.32) | 0.057 | 2.9 (0.3–1.05) | 0.092 |
| No | 59 (28) | 152 (72) | 152 (94.1) | 1 | – | 1 | – |
| Bleeding | |||||||
| Yes | 3 (11.5) | 23 (88.5) | 26 (11.6) | 0.28 (0.08–0.97) | 0.044 | 0.3 (0.08–1.05) | 0.059 |
| No | 63 (31.8) | 135 (68.2) | 198 (88.4) | 1 | – | 1 | – |
| Immunological status | |||||||
| Severe immunosuppression | 19 (47.5) | 21 (52.5) | 40 (17.9) | 2.36 (1.08–5.2) | 0.032 | 2.95 (1.26–6.9) | 0.041 |
| Advanced immunosuppression | 5 (17.5) | 24 (82.8) | 29 (12.9) | 0.54 (0.0.2–1.6) | 0.27 | 0.67 (0.22–2.06) | 0.48 |
| Mild immunosuppression | 19 (26.4) | 53 (73.6) | 72 (32.1) | 0.94 (0.5–1.9) | 0.85 | 1.25 (0.59–2.66) | 0.55 |
| No immunosuppression | 23 (27.7) | 60 (72.3) | 83 (37.1) | 1 | – | 1 | – |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; HAART, highly active antiretroviral therapy.
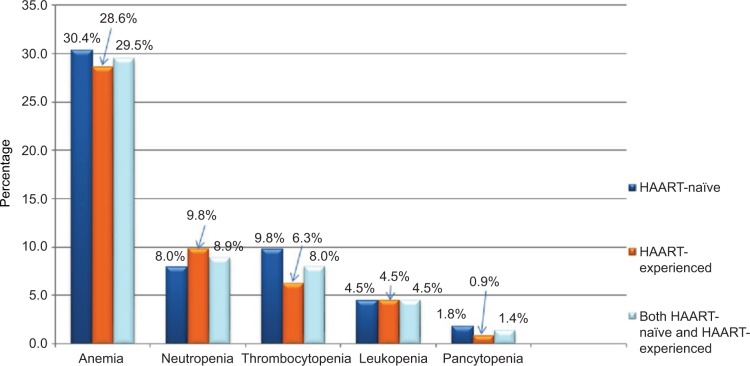
Figure 1.
Frequency of cytopenias in HIV-infected children at Pediatric ART Clinic, Felege Hiwot Referral Hospital, Bahir Dar, northwest Ethiopia.
Abbreviations: ART, antiretroviral treatment; HAART, highly active antiretroviral therapy; HIV, human immunodeficiency virus.
Ethical considerations
This study was approved by the College of Medicine and Health Sciences Research Ethical Committee and the Institutional Review Board of the University of Gondar. The purpose and importance of the study was explained to each caregiver. Informed written consent was taken from the caregivers, and in addition, assent was obtained from children aged >7 years before the commencement of the study. To ensure confidentiality of participants and their information, anonymous typing was used whereby the name of the participants and any participants’ identifiers were not written on the questionnaire. The participants were interviewed alone to maintain their privacy. Laboratory findings of study participants were communicated with the responsible clinicians assigned at the Pediatric ART Clinic.
Results
Sociodemographic characteristics
A total of 224 study participants were enrolled in this study. The median age of the study participant was 8 years (interquartile range: 6 years). More than half of the study participants, 126 (56.3%), were males. Among the study participants, 180 (80.4%) were from urban setting and 96 (42.9%) were attending primary school. A majority, 157 (70.1%), of caregivers earned monthly income <1,400 ETB (Table 1).
Medical characteristics of the study participants
Among the participants, 64 (57.2%) of HAART-naïve and 47 (41.9%) of HAART-experienced children were in WHO clinical stage I. Thirty (26.8%) and 39 (34.8%) of HAART-naïve children were underweight and stunted, respectively, whereas 44 (39.3%) and 31 (27.7%) HAART-experienced children were underweight and stunted, respectively. Moreover, 19 (17%), 16 (14.3%), 15 (13.4%), 15 (13.4%), 14 (12.5%) and 9 (8%) of HAART-naïve children presented with fever, skin rash, diarrhea, OIs, pneumonia and oral thrush, respectively. Likewise, 14 (12.5%), 13 (11.6%), 10 (9%), 10 (9%), 9 (8%) and 8 (7.1%) of HAART-experienced children presented with skin rash, fever, pneumonia, OIs, gastroenteritis and diarrhea, respectively. Severe, advanced and moderate immunosuppression was observed among 17.9%, 12.9% and 32.1% of the study participants, respectively (Table 2).
Cytopenias
Of the total study participants, 66 (29.5%), 20 (8.9%), 18 (8%), 10 (4.5%) and 3 (1.4%) were anemic, neutropenic, thrombocytopenic, leukopenic and pancytopenic, respectively. The occurrence of anemia, thrombocytopenia, neutropenia, leukopenia and pancytopenia among HAART-naïve HIV-infected children was reported to be 30.4% (n=34), 9.8% (n=11), 8% (n=9), 4.5% (n=5) and 1.8% (n=2), respectively (Figure 1).
Comparison of hematological profile
The mean values (±SD) of RBC, Hg, WBC, ANC, lymphocyte count, platelet count and absolute CD4 count in HAART-naïve children were 4.48±0.58 × 106/µL, 13.25±3.03 g/dL, 8.18±3.32 × 103/µL, 3.94±2.26 × 103/µL, 3.46±2.2 × 103/µL, 297.91±107.67 × 103/µL and 873.16±446.57/µL respectively. In children who were HAART-experienced, the mean values (±SD) were 4.94±4.75 × 106/µL, 13.21±1.6 g/dL, 8.01±3.26 × 103/µL, 3.84±2.16 × 103/µL, 3.75±5.17 × 103/µL, 300.99±106.16 × 103/µL and 767.86±486.6/µL, respectively.
On the basis of the mean values, the data indicated that Hg, RBC count, WBC count and platelet count did not show statistically significant differences between HAART-naïve and HAART-experienced HIV-infected children. However, there was a statistically significant difference in CD4% and MCV values between HAART-naïve and HAART-experienced children (p<0.05) (Table 3).
Immune status and cytopenias
In this study, the prevalence of anemia among cases with severe, advanced and mild immunosuppression was 19 (47.5%), 5 (17.2%) and 19 (26.4%), respectively. Furthermore, leukopenia and thrombocytopenia were found in 7 (17.5%) and 4 (10%) of cases with severe immune suppression (Table 4).
Comparison of cytopenias
The overall prevalence of anemia among HIV-infected children was 66 (29.5%). Anemia was found in 34 (30.5%) and 32 (28.6%) of HAART-naïve and HAART-experienced children, respectively. Among anemic cases, 1 (2.9%) of HAART-naïve and 2 (6.3%) of HAART-experienced children had severe anemia. About 11 (9.8%), 9 (8%) and 5 (4.5%) of HAART-naïve HIV-infected children were thrombocytopenic, neutropenic and leukopenic, respectively. Moreover, 11 (9.8%), 7 (6.2%) and 5 (4.5%) of HAART-experienced HIV-infected children were neutropenic, thrombocytopenic and leukopenic, respectively (Table 5).
Anemia and associated factors
In bivariate analysis, age, severe immunosuppression and presence of bleeding were significantly associated with anemia. But in multivariate logistic regression analysis, controlling the possible cofounders, age of ≤5 years (adjusted odds ratio [AOR] =4.3, 95% CI: 1.7–10.9), age of 6–10 years (AOR =3.1, 95% CI: 1.3–7.2) and severe immunosuppression (AOR =2.95, 95%CI: 1.26–6.9) remained risk factors of anemia in HIV-infected children (Table 6).
Discussion
Cytopenia is the most common manifestation of advanced HIV infection.13,17,34 It is proposed that they are caused by the impaired growth and development of hematopoietic progenitor cells in the bone marrow due to the presence of HIV proteins and changes in the cytokine expression, which potentially lead to an altered maturation process and increased cell death of ≥1 bone marrow cell lineages.13,35 These abnormalities have been directly correlated with the degree of immunosuppression and disease progression.15,36–38 It has also been documented that they potentially limit the efficacy of HAART treatment and strongly predict morbidity and mortality in HIV-infected individuals.39–43
In this study, the prevalence of anemia was found to be 29.5%, making it more common than neutropenia, thrombocytopenia, leukopenia and cytopenia. This is in agreement with most of the literatures.9,32,44 Experimental studies suggest that dyserythropoiesis and early apoptosis of red cell precursors are common features in HIV infection.45 In addition, HIV infection causes deficiency and defects in metabolism of iron, vitamin B12 and other micronutrients, which may lead to anemia.46,47 Moreover, immune suppression associated with HIV infection can be a cause for the onset of chronic inflammation and/or chronic disease, such as tuberculosis, recurrent diarrheal diseases, recurrent bacterial pneumonia and viral infections, which can result in anemia as well as other cytopenias. The prevalence of anemia (29.5%) is lower than that reported in Lagos (77.9%),9 Nepal (74.4%),48 West Bengal, India (69%),37 Uganda (57.6%)49 and Dar es Salaam, Tanzania (44%),18 and it is higher than that in Addis Ababa, Ethiopia (22.2%),50 Jimma, Ethiopia (21.9%),32 Gondar, Ethiopia (16.2%)51 and Enugu, Nigeria (3%).52 This variation might be attributed to the differences in ethnicity, study designs and time of study. In addition, variation in age of the study participants, HAART status and cutoff value in defining anemia, local prevalence of parasitic infections such as malaria or hookworms, as well as local nutritional patterns might contribute to the variation in magnitude of anemia.
In this study, the number of cases with mild, moderate and severe anemia was 37 (56.1%), 26 (39.4%) and 3 (4.5%), respectively. This is comparable with the results of another study done in Gondar, Ethiopia,51 where occurrence of mild, moderate and severe anemia was 60.5%, 37.2% and 2.3%, respectively. Similarly, it is in agreement with a study done in Addis Ababa, Ethiopia,50 where mild, moderate and severe anemia were reported to be 52.2%, 42.5% and 5%, respectively. The proportion of severe anemia in our studies is lower than that in studies conducted in Jimma, Ethiopia,32 and Dar es Salaam, Tanzania,18 which were reported to be 14.3% and 15%, respectively. The low magnitude of severe anemia in the current study might be related to the improved level of societal awareness about the positive implication of HIV monitoring and treatment, improved access to HIV monitoring and treatment facilities as well as updating of HIV monitoring and therapeutic modalities over time.
In the current study, the second most common cytopenia was neutropenia, which was observed in 8.9% HIV-infected children. The possible explanation may be the fact that HIV directly infects bone marrow and bone marrow stromal cell, which may reduce hematopoiesis. In addition, it is speculated that the decline in vitamin B12 and the presence of antibodies to HIV envelope glycoprotein 120 suppress bone marrow progenitor cells, in addition to being implicated as a causal factor of cytopenia, including neutropenia.20 Furthermore, ART used to suppress the viral load may adversely affect the hematopoietic capacity of bone marrow.12 Compared to studies done in Lagos, Nigeria, (17.5%)9 and West Bengal, India (19%),37 the prevalence of neutropenia is lower. The possible difference might be the difference in immunological status of the study participants and sample size. In the study from Lagos, Nigeria, of the total 68 children who participated in the study, about 75% were in the Centers for Disease Control and Prevention, USA (CDC) clinical stages B and C. Likewise, in the West Bengal study, of the total 100 children participating in the study, 50% were in WHO stages 3 and 4. But, in the current study, 20% of the study participants were in WHO stages 3 and 4.
In this study, thrombocytopenia was found to be 8%, which is the third most common cytopenia in HIV-infected children. The possible biological explanations for why thrombocytopenia is common in HIV infection might be due to an increased platelet destruction either caused by the nonspecific deposition of circulating immune complexes on platelets or the presence of specific antiplatelet glycoprotein antibodies, leading to immune-mediated thrombocytopenia, as well as direct HIV infection of megakaryocytes and their precursors, resulting in higher thrombocytopenia15,53 The result is comparable to studies done in Mumbai, India (10%)54 and West Bengal, India (11%).37 However, it is higher than that in the report from Lagos (2.5%);9 and lower than studies done in Nepal (17.9%),48 Kenya (21%)44 and Uttar Pradesh, India (29.78%).55 The variations in prevalence could be attributed to the difference in the reference range used to define thrombocytopenia as Adetifa et al9 used platelet count <100 × 103/mm3; HAART status, as Kibaru et al44 included children who were HAART-naïve; and sample size, as Poudel et al48 and Kumar et al55 used small sample size to determine the magnitude of thrombocytopenia.
In the current study, 4.5% of study participants were leukopenic. This is comparable with a study done in Lagos, Nigeria (6%).9 However, it is lower than that in studies done at Kenyatta hospital, Kenya (10%)44 and West Bengal, India (34%),37 and higher than that in the study done in Mumbai, India (2%).54 The possible reason for the variation in magnitude of leukopenia might be due to the differences in ethnicity, age of study participants included in study, HAART status as well as prevalence of infectious and noninfectious diseases.
In this study, severe immunosuppression (AOR =2.95, 95% CI: 1.26–6.9) was significantly associated with anemia. Similar findings had been reported previously in Addis Ababa, Ethiopia,50 Western Uganda,49 and South India,46 revealing that there was statistically significant association between immune suppression and anemia. This could be explained by the fact that immune suppression potentially leads to viral replication, which may cause anemia through increased cytokine-mediated myelosuppression and higher burden of OIs.13,56 Furthermore, age <5 years (AOR =4.3, 95% CI: 1.7–10.9) and age of 6–10 years (AOR =3.1, 95% CI: 1.3–7.2) also remained risk factors of anemia. This is also similar with other studies.18,49,57 The possible reason for increased risk of anemia in younger children may be related with the high nutritional requirement for production of RBCs and the high frequency of comorbidity because their immune status is not well developed. Unlike anemia, neutropenia, thrombocytopenia and leukopenia were not significantly associated with independent variables. The possible explanation could be the small number of cases of children who had these cytopenias and the small sample size; therefore, the number of observations in each category of independent variables would be small and these observations would have low power to predict association.
In the current study, the mean MCV value in HAART-experienced HIV-infected children was significantly higher than in children who were HAART naïve. The possible reason for the high MCV value in HAART-experienced HIV-infected children might be related with the use of zidovudine-based first-line HAART. In this study, of the total 18 children who were on first-line HAART having MCV value >100 fL, 11 (61%) were taking zidovudine-based ART regimen. Evidence suggests that zidovudine causes marrow erythroid hypoplasia, aplasia and megaloblastic maturation, which can be accompanied by a progressive raise in erythrocyte MCV.58,59 The other possible reason for the difference would be related to the nutritional deficiencies, particularly iron deficiency, the most common nutritional deficiency in developing countries,60 which causes microcytic–hypochromic RBC morphology in HAART-naïve children.
The MCV could show an increment due to iron supplements and nutritional modification provided after HAART initiation. Together with the macrocytosis that appears to be overt after they are initiated into zidovudine-containing regimens, the MCV value shows significant elevation. Our data also supported that microcytosis is significantly higher in HAART-naïve (33.9%), compared to HAART-experienced, HIV-infected children (16.1%). A retrospective study done in Kenya has shown that, compared with the baseline value, the mean MCV value of HIV-infected children was significantly raised at 6 months after initiation of HAART.61
However, the mean CD4% of HAART-experienced HIV-infected children was significantly lower than that of HAART-naïve ones. The possible reason for the low value of mean CD4% in HAART-experienced children might be delayed diagnosis and ART initiation, poor adherence to ART and delayed response to ART. These may limit the success of HAART and may be related with continued viral replication and immunological failure. Evidence also demonstrated that initiation of HAART in children with a low CD4 value is less likely to result in a robust increase in CD4 cells, thereby being less likely to achieve a successful treatment outcome.62 Moreover, poor adherence to ART in children is one of the challenges in resource-limited settings, including Ethiopia.63–65
Limitations
The main limitation of this study is the cross-sectional nature of its design, which makes relationships between cytopenias and associated factors difficult, as it is temporal association. In addition, we were unable to analyze serum ferritin, vitamin B12 and folate levels and unable to perform bone marrow examination, which potentially limit this study. Another limitation of this study is that we did not assess all modifiable risk factors, such as intestinal parasitic infection, malaria, viral infections and fungal infections, which could potentially influence the magnitude and severity of cytopenias. We did not include HIV-negative children as a control to compare the magnitude of cytopenias between HIV-infected and noninfected children. Furthermore, the study is a single-center institutional study that could not be generalized for HIV-infected children in the study area.
Conclusion
The prevalence of anemia was higher, meeting the WHO criteria for a moderate public health problem. Neutropenia was the second most common cytopenia among HIV-infected children in the study area. Severe immunosuppression and younger age were significantly associated with anemia. Moreover, the proportion of cytopenias did not significantly vary between HAART-naïve and HAART-experienced HIV-infected children. Therefore, emphasis should be given for investigation and management of hematological abnormalities in HIV-infected children, particularly those who are immunosuppressed and of younger age. Furthermore, multicentered prospective studies need to be conducted to explore modifiable associated factors of cytopenias, patterns of cytopenias over time, and the impact of HAART on cytopenia among HIV-infected children in resource-limited settings such as Ethiopia.
Acknowledgments
The authors thank the staff of the Pediatric ART Clinic, Felege Hiwot Referral Hospital, who actively participated during the data collection process. They are also grateful to and wish to thank the study participants and caregivers for their voluntary participation in this study. Finally, they thank the University of Gondar, Amhara Regional Health Bureau, Felege Hiwot Referral Hospital and Bahir Dar Regional Health Research Laboratory Center for financial and logistical support.
Abbreviations
- AIDS
acquired immune deficiency syndrome
- ANC
absolute neutrophil count
- ART
antiretroviral treatment
- CI
confidence interval
- CD4
cluster of differentiation-4
- ETB
Ethiopian birr
- HAART
highly active antiretroviral therapy
- HIV
human immunodeficiency virus
- Hg
hemoglobin
- MCH
mean corpuscular hemoglobin
- MCHC
mean corpuscular hemoglobin concentration
- MCV
mean corpuscular volume
- mid
mixed cell
- MPV
mean platelet volume
- OIs
opportunistic infections
- RBC
red blood cell
- RDW
red cell distribution width
- WBC
white blood cell
Footnotes
Author contributions
YGT participated in conceiving and designing the study; collecting, analyzing and interpreting the data as well as drafting the manuscript. MM participated in conceiving and designing the study; analyzing and interpreting the data and drafting the manuscript, in addition to being the lead author of the manuscript. ZA, AT and AA participated in study design and data analysis, as well as contributing toward drafting and review of the manuscript. All authors have read and approved the final manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Okolie MN, Eghafona NO, Omoregie R. Anti-human immunodeficiency virus (HIV) agents. J Med Lab Sci. 2003;12(1):1–4. [Google Scholar]
- 2.Enawgaw B, Alem M, Addis Z, Melku M. Determination of hematological and immunological parameters among HIV positive patients taking highly active antiretroviral treatment and treatment naïve in the antiretroviral therapy clinic of Gondar University Hospital, Gondar, Northwest Ethiopia: a comparative cross-sectional study. BMC Hematol. 2014;14:8. doi: 10.1186/2052-1839-14-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kam KM, Leung WL, Wong KH, Lee SS, Hung MY, Kwok MY. Maturational changes in peripheral lymphocyte subsets pertinent to monitoring human immunodeficiency virus-infected Chinese pediatric patients. Clin Diagn Lab Immunol. 2001;8(5):926–931. doi: 10.1128/CDLI.8.5.926-931.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moses A, Nelson J, Bagby GC. The influence of human immunodeficiency virus-1 on hematopoiesis. Blood. 1998;91(5):1479–1495. [PubMed] [Google Scholar]
- 5.Sloand E. Hematologic complications of HIV infection. AIDS Rev. 2004;7(4):187–196. [PubMed] [Google Scholar]
- 6.Cosby CD. Hematologic disorders associated with human immunodeficiency virus and AIDS. J Infus Nurs. 2007;30(1):22–32. doi: 10.1097/00129804-200701000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Coyle TE. Hematologic complications of human immunodeficiency virus infection and the acquired immunodeficiency syndrome. Med Clin North Am. 1997;81(2):449–470. doi: 10.1016/s0025-7125(05)70526-5. [DOI] [PubMed] [Google Scholar]
- 8.Sullivan AK, Raben D, Reekie J, et al. Feasibility and effectiveness of indicator condition-guided testing for HIV: results from HIDES I (HIV indicator diseases across Europe study) PLoS One. 2013;8(1):e52845. doi: 10.1371/journal.pone.0052845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Adetifa IMO, Temiye E, Akinsulie A, Ezeaka V, Iroha E. Haematological abnormalities associated with pediatric HIV/AIDS in Lagos. Ann Trop Paediatr. 2006;26:121–125. doi: 10.1179/146532806X107467. [DOI] [PubMed] [Google Scholar]
- 10.Akkina R. New insights into HIV impact on hematopoiesis. Blood. 2013;122(13):2144–2146. doi: 10.1182/blood-2013-08-518274. [DOI] [PubMed] [Google Scholar]
- 11.Kirchhoff F, Silvestri G. Is Nef the elusive cause of HIV-associated hematopoietic dysfunction? J Clin Invest. 2008;118(5):1622–1625. doi: 10.1172/JCI35487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choi SY, Kim I, Kim NJ, et al. Hematological manifestations of human immunodeficiency virus infection and the effect of highly active anti-retroviral therapy on cytopenia. Korean J Hematol. 2011;46(4):253–257. doi: 10.5045/kjh.2011.46.4.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alexaki A, Wigdahl B. HIV-1 infection of bone marrow hematopoietic progenitor cells and their role in trafficking and viral dissemination. PLoS Pathog. 2008;4(12):e1000215. doi: 10.1371/journal.ppat.1000215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quaye WK, Quaye L, Amidu N, Addai-Mensah AN. Prevalence of anaemia and immunological markers among Ghanaian HAART-naïve HIV-patients and those on HAART. Afr Health Sci. 2011;11(1):2–15. [PMC free article] [PubMed] [Google Scholar]
- 15.Attili SV, Singh VP, Rai M, Varma DV, Gulati AK, Sundar S. Hematological profile of HIV patients in relation to immune status – a hospital-based cohort from Varanasi, North India. Turk J Hematol. 2008;25(1):13–19. [PubMed] [Google Scholar]
- 16.Eley BS, Sive AA, Shuttleworth M, Hussey GD. A prospective, cross-sectional study of anaemia and peripheral iron status in antiretroviral naïve, HIV-1 infected children in Cape Town, South Africa. BMC Infect Dis. 2002;2:3. doi: 10.1186/1471-2334-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liebman HA. Viral-associated immune thrombocytopenic purpura. Hematology Am Soc Hematol Educ Program. 2008:212–218. doi: 10.1182/asheducation-2008.1.212. [DOI] [PubMed] [Google Scholar]
- 18.Makubi AN, Mugusi F, Magesa PM, Roberts D, Quaresh A. Risk factors for anaemia among HIV infected children attending care and treatment clinic at Muhimbili National Hospital in Dar es Salaam, Tanzania. Tanzan J Health Res. 2012;14(1):1–9. [PubMed] [Google Scholar]
- 19.Claster S. Biology of anemia, differential diagnosis, and treatment options in human immunodeficiency virus infection. J Infect Dis. 2002;185(suppl 2):S105–S109. doi: 10.1086/340202. [DOI] [PubMed] [Google Scholar]
- 20.Kuritzkes DR. Neutropenia, neutrophil dysfunction, and bacterial infection in patients with human immunodeficiency virus disease: the role of granulocyte colony-stimulating factor. Clin Infect Dis. 2000;30(2):256–260. doi: 10.1086/313642. [DOI] [PubMed] [Google Scholar]
- 21.Sieg SF, Bazdar DA, Harding CV, Lederman MM. Differential expression of interleukin-2 and gamma interferon in human immunodeficiency virus disease. J Virol. 2001;75(20):9983–9985. doi: 10.1128/JVI.75.20.9983-9985.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zon LI, Groopman JE. Hematologic manifestations of human immune deficiency virus (HIV) Semin Hematol. 1988;25(3):208–218. [PubMed] [Google Scholar]
- 23.Oshikoya KA, Lawal S, Oreagba IA, et al. Adverse events in HIV-infected children on antiretroviral therapy at a teaching hospital in Lagos, Nigeria: a retrospective study. Adv Pharmacoepidem Drug Safety. 2012;1(4):1000117. [Google Scholar]
- 24.Sutcliffe CG, Van Dijk JD, Bolton C, Persaud D, Moss WJ. Effectiveness of antiretroviral therapy among HIV-infected children in sub-Saharan Africa. Lancet Infect Dis. 2008;8(8):477–489. doi: 10.1016/S1473-3099(08)70180-4. [DOI] [PubMed] [Google Scholar]
- 25.Taye B, Shiferaw S, Enquselassie F. The impact of malnutrition in survival of HIV infected children after initiation of antiretroviral treatment (ART) Ethiop Med J. 2010;48(1):1–10. [PubMed] [Google Scholar]
- 26.Sunguya BF, Poudel KC, Otsuka K, et al. Undernutrition among HIV-positive children in Dar es Salaam, Tanzania: antiretroviral therapy alone is not enough. BMC Public Health. 2011;11:869. doi: 10.1186/1471-2458-11-869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bachou H, Tylleskär T, Downing R, Tumwine J. Severe malnutrition with and without HIV-1 infection in hospitalised children in Kampala, Uganda: differences in clinical features, haematological findings and CD4+ cell counts. Nutr J. 2006;5:27. doi: 10.1186/1475-2891-5-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heikens GT, Bunn J, Amadi B, et al. Case management of HIV-infected severely malnourished children: challenges in the area of highest prevalence. Lancet. 2008;371(9620):1305–1307. doi: 10.1016/S0140-6736(08)60565-6. [DOI] [PubMed] [Google Scholar]
- 29.Nielsen SD, Ersboll AK, Mathiesen L, Nielsen JO, Hansen JES. Highly active antiretroviral therapy normalizes the function of progenitor cells in human immunodeficiency virus–infected patients. J Infect Dis. 1998;178:1299–1305. doi: 10.1086/314464. [DOI] [PubMed] [Google Scholar]
- 30.Aurpibul L, Puthanakit T, Sirisanthana T, Sirisanthana V. Haematological changes after switching from Stavudine to Zidovudine in HIV-infected children receiving highly active antiretroviral therapy. HIV Med. 2008;9:317–321. doi: 10.1111/j.1468-1293.2008.00560.x. [DOI] [PubMed] [Google Scholar]
- 31.Molye G, Sawyer W, Law M, Amin J, Hil A. Changes in hematologic parameters and efficacy of thymidine analogue-based, highly active antiretroviral therapy: a meta-analysis of six prospective, randomized, comparative studies. Clin Ther. 2004;26(1):92–97. doi: 10.1016/s0149-2918(04)90009-4. [DOI] [PubMed] [Google Scholar]
- 32.Abebe M, Alemseged F. Hematologic abnormalities among children on HAART, in Jimma university specialized hospital, Southwestern Ethiopia. Ethiop J Health Sci. 2009;19(2):83–89. [Google Scholar]
- 33.WHO . Antiretroviral Therapy of HIV Infection in Infants and Children: Towards Universal Access. Recommendations for a Public Health Approach. Strengthening Health Services to Fight HIV/AIDS, WHO HIV/AIDS Program. Geneva: WHO; 2006. [Accessed November 18, 2015]. Available from: http://www.who.int/hiv/pub/guidelines/paediatric020907.pdf. [Google Scholar]
- 34.WHO [webpage on the Internet] Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity, Vitamin and Mineral Nutrition information System. Geneva: WHO; 2011. [Accessed November 20, 2015]. Available from: http://www.who.int/vmnis/indicators/haemoglobin/en/ [Google Scholar]
- 35.Koka PS, Reddy ST. Cytopenias in HIV infection: mechanisms and alleviation of hematopoietic inhibition. Curr HIV Res. 2004;2(3):275–282. doi: 10.2174/1570162043351282. [DOI] [PubMed] [Google Scholar]
- 36.Denue BA, Gashau W, Bello HS, Kida IM, Bakki B, Ajayi B. Relation between some haematological abnormalities, degree of immunosuppression and viral load in treatment-naïve HIV-infected patients. East Mediterr Health J. 2013;19(4):362–368. [PubMed] [Google Scholar]
- 37.Bhowmik A, Banerjee P. Hematological manifestation in HIV infected children. J Coll Physicians Surg Pak. 2015;25(2):119–123. [PubMed] [Google Scholar]
- 38.Ellaurie M, Burns ER, Rubinstein A. Hematological manifestations in pediatric HIV infection: severe anemia as a prognostic factor. Am J Pediatr Hematol Oncol. 1990;12(4):449–453. doi: 10.1097/00043426-199024000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Berhane K, Karim R, Cohen MH, et al. Impact of highly active antiretroviral therapy on anaemia and relationship between anemia and survival in a large cohort of HIV-infected women: women’s Interagency HIV Study. J Acquir Immune Defic Syndr. 2004;37(2):1245–1252. doi: 10.1097/01.qai.0000134759.01684.27. [DOI] [PubMed] [Google Scholar]
- 40.Anastos K, Shi Q, French AL, et al. Total lymphocyte count, hemoglobin and delayed-type hypersensitivity as predictors of death and AIDS illness in HIV-1 infected women receiving highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2004;35:383–392. doi: 10.1097/00126334-200404010-00008. [DOI] [PubMed] [Google Scholar]
- 41.Chatterjee A, Bosch RJ, Kupka R, Hunter DJ, Msamanga GI, Fawzi WW. Predictors and consequences of anaemia among antiretroviral-naïve HIV-infected and HIV-uninfected children in Tanzania. Public Health Nutr. 2009;13(2):289–296. doi: 10.1017/S1368980009990802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gebremedhin A, Gebremariam S, Haile F, Weldearegawi B, Decotelli C. Predictors of mortality among HIV infected children on anti-retroviral therapy in Mekelle Hospital, Northern Ethiopia: a retrospective cohort study. BMC Public Health. 2013;13:1047. doi: 10.1186/1471-2458-13-1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.De Santis GC, Brunetta DM, Vilar FC, et al. Hematological abnormalities in HIV-infected patients. Int J Infect Dis. 2011;15:e808–e811. doi: 10.1016/j.ijid.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 44.Kibaru EG, Nduati R, Wamalwa D, Kariuki N. Baseline hematological indices among HIV-1 infected children at Kenyatta National Hospital. Int J Novel Res Healthcare Nursing. 2014;1(1):21–26. doi: 10.1186/s12981-015-0069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Calis JC, Phiri K, Vet RJ, et al. Erythropoiesis in HIV-infected and uninfected Malawian children with severe anemia. AIDS. 2010;24(18):2883–2887. doi: 10.1097/QAD.0b013e32833fed27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shet A, Bhavani PK, Kumarasamy N, et al. Anemia, diet and therapeutic iron among children living with HIV: a prospective cohort study. BMC Pediatr. 2015;15:164. doi: 10.1186/s12887-015-0484-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anyabolu HC, Adejuyigbe EA, Adeodu OO. Serum micronutrient status of Haart-naive, HIV infected children in South Western Nigeria: a case controlled study. AIDS Res Treat. 2014;2014:8. doi: 10.1155/2014/351043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Poudel P, Pokharel R, Chitlangia M, Chaudhary S. Profile of HIV infected children: a hospital based study at Eastern Nepal. Asian Pac J Trop Dis. 2014;4(3):169–175. [Google Scholar]
- 49.Nyesigire Ruhinda E, Bajunirwe F, Kiwanuka J. Anaemia in HIV-infected children: severity, types and effect on response to HAART. BMC Pediatr. 2012;12:170. doi: 10.1186/1471-2431-12-170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mihiretie H, Taye B, Tsegaye A. Magnitude of anemia and associated factors among pediatric HIV/AIDS patients attending Zewditu Memorial Hospital ART Clinic, Addis Ababa, Ethiopia. Anemia. 2015;2015(479329):1–6. doi: 10.1155/2015/479329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Enawgaw B, Alem M, Melku M, Addis Z, Terefe B, Yitayew G. Prevalence and associated risk factors of anemia among HIV infected children attending Gondar university hospital, Northwest Ethiopia: a cross sectional study. BMC Hematol. 2015;15:12. doi: 10.1186/s12878-015-0032-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ezeonwu BU, Ikefuna AN, Oguonu T, Okafor HU. Prevalence of hematological abnormalities and malnutrition in HIV-infected under five children in Enugu. Niger J Clin Pract. 2014;17(3):303–308. doi: 10.4103/1119-3077.130230. [DOI] [PubMed] [Google Scholar]
- 53.Li Z, Nardi MA, Karpatkin S. Role of molecular mimicry to HIV-1 peptides in HIV-1-related immunologic thrombocytopenia. Blood. 2005;106:572–576. doi: 10.1182/blood-2005-01-0243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shah I, Katira B. Hematological manifestation in HAART naïve HIV-1 infected children in India in a resource limited setting. Pediatric Oncall J. 2011;8(5):35. [Google Scholar]
- 55.Kumar D, Kumar D, Singh DK, Rai R. Prevalence of thrombocytopenia and its relation with WHO clinical and immunological staging among human immunodeficiency virus-infected children. Indian J Child Health. 2014;1(3):140–142. [Google Scholar]
- 56.Yadav J, Nanda S, Sharma D. Opportunistic infections and complications in human immunodeficiency virus-1-infected children: correlation with immune status. Sultan Qaboos Univ Med J. 2014;14(4):e513–e521. [PMC free article] [PubMed] [Google Scholar]
- 57.Shet A, Mehta S, Rajagopalan N, et al. Anemia and growth failure among HIV-infected children in India: a retrospective analysis. BMC Pediatr. 2009;9:37. doi: 10.1186/1471-2431-9-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ssali F, Stohr W, Munderi P, et al. Prevalence, incidence and predictors of severe anaemia with zidovudine-containing regimens in African adults with HIV infection within the DART trial. Antivir Ther. 2006;11:741. doi: 10.1177/135965350601100612. [DOI] [PubMed] [Google Scholar]
- 59.Pryce C, Pierre RB, Steel-Duncan J, et al. Safety of antiretroviral drugs in Jamaican children with HIV. West Indian Med J. 2008;57(3):238–245. [PubMed] [Google Scholar]
- 60.WHO [webpage on the Internet] Iron Deficiency Anaemia: Assessment, Prevention and Control A Guide for Programme Managers. Geneva: World Health Organization; 2001. [Accessed January 10, 2016]. Available from: http://www.who.int/nutrition/publications/micronutrients/anaemia_iron_deficiency/WHO_NHD_01.3/en/ [Google Scholar]
- 61.Kibaru EG, Nduati R, Wamalwa D, Kariuki N. Impact of highly active antiretroviral therapy on hematological indices among HIV-1 infected children at Kenyatta National Hospital-Kenya: retrospective study. AIDS Res Ther. 2015;12:26. doi: 10.1186/s12981-015-0069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Musoke PM, Mudiope P, Barlow-Mosha LN, et al. Growth, immune and viral responses in HIV infected African children receiving highly active antiretroviral therapy: a prospective cohort study. BMC Pediatr. 2010;10:56. doi: 10.1186/1471-2431-10-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Biressaw S, Abegaz WE, Abebe M, Taye WA, Belay M. Adherence to antiretroviral therapy and associated factors among HIV infected children in Ethiopia: unannounced home-based pill count versus caregivers’ report. BMC Pediatr. 2013;13:132. doi: 10.1186/1471-2431-13-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Biadgilign S, Deribew A, Amberbir A, Deribe K. Adherence to highly active antiretroviral therapy and its correlates among HIV infected pediatric patients in Ethiopia. BMC Pediatr. 2008;8:53. doi: 10.1186/1471-2431-8-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Eticha T, Berhane L. Caregiver-reported adherence to antiretroviral therapy among HIV infected children in Mekelle, Ethiopia. BMC Pediatr. 2014;14:114. doi: 10.1186/1471-2431-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]