Abstract
Delayed post-pancreatectomy hemorrhage (PPH) is a relatively uncommon, but feared, complication after pancreaticoduodenectomy (PD). A splenic artery pseudoaneurysm is a rare cause of delayed PPH after a PD. This paper describes the case of a patient with PD used to treat a distal bile duct cholangiocarcinoma complicated with a clinically significant pancreatic fistula and secondary intraabdominal abscess. Computed tomography-guided drainage of the abscess was performed with an apparently favourable outcome; the patient was discharged on postoperative day (POD) 35 and the abdominal drains were removed on POD 50. On POD 80, the patient was readmitted for a severe digestive hemorrhage. Computed tomography revealed a pseudoaneurysm of the splenic artery with a subsequent hematoma formation. Immediately, an angiography was performed and coils were successfully mounted. This case illustrates the rare possibility of the development of a splenic artery pseudoaneurysm with severe delayed PPH after PD complicated with a clinically significant pancreatic fistula, even after the patient was discharged from the hospital. An interventional radiology approach represents the first treatment option in hemodynamically stable patients with high success rates.
Keywords: Pancreaticoduodenectomy, Pancreatic fistula, Delayed hemorrhage, Splenic artery pseudoaneurysm, Interventional angiography
INTRODUCTION
Pancreaticoduodenectomy (PD) represents the standard approach for resectable periampullary malignancies.1 PD is a complex surgical procedure that is widely recognized to have increased rates of postoperative complications.1 Thus, morbidity rates around 40% and in-hospital mortality rates around 5% should be expected after a PD.1 Associated venous resections appear to increase both morbidity and mortality rates after a PD.2
Surgeon experience and annual hospital volume are important determinants of early outcomes after PD.3 However, a recent meta-analysis did not identify the surgeon caseload as a significant determinant of the postoperative mortality after PD.4 Analysis performed at the national level in the United States has shown that mortality rates reported at 90 days are double compared with the 30 day mortalities rates after pancreatectomies.5 Furthermore, in hospitals with an average annual volume of more than 40 PDs, the 90 day mortality rate was 4.7% while in hospitals with less than 5 PDs per year the 90 day mortality rate was significantly higher – 14.2%.5 Nevertheless, it appears that high-volume surgeons are associated with significantly lower in-hospital mortality rates, compared with low-volume surgeons, no matter what the hospital annual volume of PDs is.6 The largest, single surgeon, Western experience with a PD published so far belongs to John Cameron from the Johns Hopkins Hospital (USA).7 Thus, in a consecutive series of 2,000 PDs, periampullary malignancies represented 68% of the indications, with a morbidity rate of 45% and in-hospital mortality rate of 1.6%.7
The main source of morbidity after PD is represented by a pancreatic fistula, a complication that can be encountered in up to one-third of the patients.1 The high variability of the reported pancreatic fistula rates after PD is mainly related to the variability of definitions used.8 A pancreatic fistula remains an important issue after PD and can lead to other potentially life-threatening complications such as delayed hemorrhagic complications.8,9
A delayed hemorrhage is considered a relatively uncommon complication after PD. Thus, the reported rates of delayed hemorrhage after a PD in recent published large series vary between 2% and 8.4%.7,10,11,12,13,14,15,16,17,18 Although the post-pancreatectomy hemorrhage (PPH) accounts for only 1% to 13.2% of the postoperative complications, it is considered a severe complication because it is associated with very high mortality rates. PPH accounts for 10.5% to 38% of overall mortality after a PD.9,10,11,12,13,15,17,18 This paper presents the diagnosis and management of a patient with a delayed hemorrhage after a PD due to a pseudoaneurysm of the splenic artery.
CASE
A 57-year-old woman with arterial hypertension, was investigated in the Gastroenterology Department for jaundice and weight loss. Laboratory tests showed the following abnormalities:
Cholestasis – total/direct bilirubin serum level= 16.6/11.5 mg/dl (normal values, 0.3-1.2/0-0.4 mg/dl) and gamaglutamiltranspeptidase (GGT) serum level=424 U/L (normal values, 7-99 U/L);
Liver cytolysis – aspartate aminotransferase (AST) serum level=112 U/L (normal values, 0-35 U/L) and alanine aminotransferase (ALT) serum level=87 U/L (normal values, 0-45 U/L);
Hyperglycemia – glucose serum level=143 mg/dl (normal values 74-106 mg/dl).
The serum levels of the tumor markers were 287.5 U/ml for CA 19-9 (normal values, 0-39 U/ml) and 4.9 ng/ml for CEA (normal values, 0-3.4 ng/ml), respectively.
The abdominal ultrasound examination, magnetic resonance colangiopancreatography, and endoscopic ultrasound examinations suspected the diagnosis of a resectable distal bile duct cholangiocarcinoma. Thus, the patient was referred to the Department of Surgery for resection.
In February 2015, the patient underwent pylorus-preserving PD for a diagnosis of distal bile duct cholangiocarcinoma, without any significant intraoperative events. Intraoperatively, an accessory right hepatic artery with origin from the superior mesenteric artery was also observed and was spared during the resection. The reconstruction after PD was made using the modified Child's technique. Thus, the distal pancreatic stump (soft pancreas, tiny Wirsung duct that could not be identified to be stented) was anastomosed to the jejunum in an end-to-side fashion, using single-layer, interrupted, non-absorbable sutures. Furthermore, the bile duct was anastomosed to the jejunum in an end-to-side single-layer, continuous, absorbable suture, as it was the case also for duodenojejunal anastomosis. Three drains were left in place at the end of the operation.
At approximately 1 h after the end of the operation, the patient presented tachycardia, severe hypotension and significant external bleeding in one abdominal drain, with a 2 g/dl decrease in the hemoglobin serum level. Immediately the patient was readmitted into the operating room and, with the diagnosis of early severe PPH with secondary hemorrhagic shock, a re-laparotomy was performed. After the re-laparotomy, the diagnosis of early severe PPH with secondary hemorrhagic shock was changed to a diagnosis of hemoperitoneum due to a small arterial source branching from the accessory right hepatic artery, which was sutured to control the bleeding.
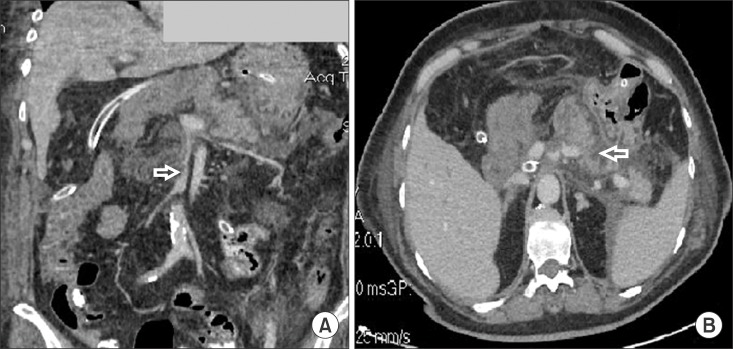
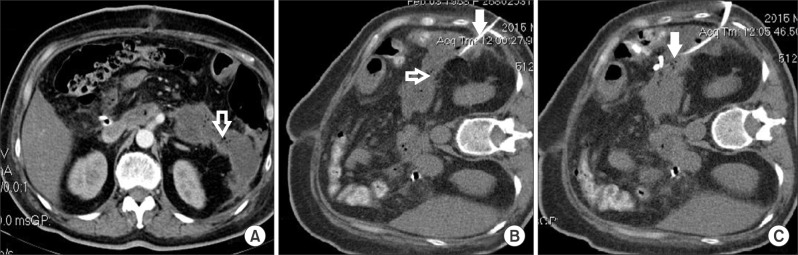
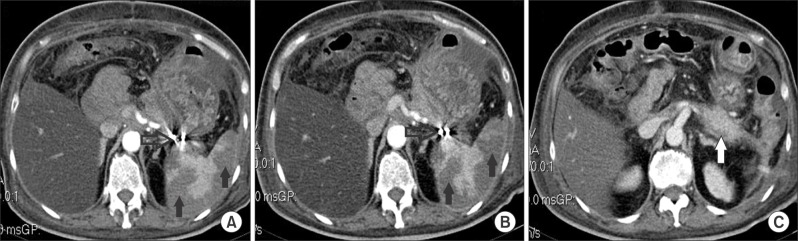
On POD 1, very high serum levels of amylase and lipase were encountered: 1,025 U/L and 3,682 U/L, respectively (normal values, 25-100 U/L and 0-60 U/L, respectively). Furthermore, the clinical course of the patient was relatively well, with good intake tolerance, presence of the intestinal transit, normalisation of the amylase and lipase serum levels and no other significant abnormalities on laboratory tests, except for mild anemia. However, on POD 7, the patient developed an external pancreatic fistula (debit of approximately 500 ml/day), without any change of clinical status. The contrast-enhanced computed tomography performed on POD 7 revealed partial thrombosis of the superior mesenteric vein (Fig. 1A, open white arrow), peripancreatic fluids and minor non-enhancing areas in the remnant pancreas (Fig. 1B, open white arrow), but no signs of abscesses or infected necrosis. Thus, a conservative approach was considered, including anticoagulant therapy and antibiotics. The contrast-enhanced computed tomography performed on POD 19 revealed no thrombosis of the superior mesenteric vein but thrombosis of the proximal splenic vein (Fig. 2, open white arrow) with distal peripancreatic fluids (Fig. 2, filled white arrow). But again, there were no signs of abscesses or infected necrosis. The patient was in relatively good clinical condition and no significant abnormalities were detected in the laboratory tests. The pancreatic fistula had a favourable outcome and, due to minimum drainage output, the drains were removed on POD 26. However, on POD 29 the patient presented with a fever and leukocytosis (a white cell count of 18,000 per cubic millimeter). The contrast-enhanced computed tomography performed on POD 30 revealed a large, peripancreatic distal collection with gas inside suggesting the formation of a peripancreatic abscess (Fig. 3A, open white arrow). A successful percutaneous drainage of the abscess was performed (Fig. 3B and 3C, filled white arrow).
Fig. 1. Abdominal contrast-enhanced computed tomography in the venous phase performed on post-operative day (POD) 7 (A) frontal slice showing partial thrombosis of the superior mesenteric vein (open white arrow); (B) axial slice showing peripancreatic fluids and minor non-enhancing areas in the remnant pancreas (open white arrow).
Fig. 2. Abdominal contrast-enhanced computed tomography axial slice in the venous phase performed on POD 19 showing thrombosis of the proximal splenic vein (open white arrow) and distal peripancreatic fluids (filled white arrow).
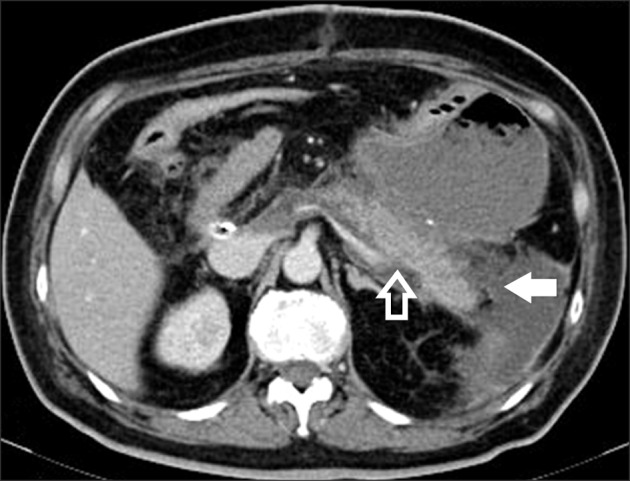
Fig. 3. Abdominal contrast-enhanced computed tomography axial slice in the venous phase performed on POD 30 showing (A) a large peripancreatic distal collection with gas inside suggesting the formation of a peripancreatic abscess (open white arrow); (B) the percutaneous drainage catheter (filled white arrow) toward the peripancreatic abscess (open white arrow); (C) the drainage catheter (filled white arrow) successfully inserted in the peripancreatic abscess.
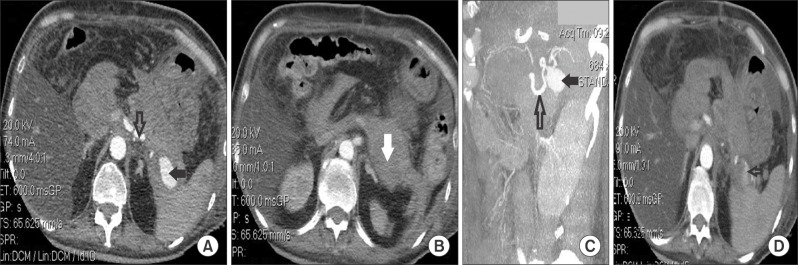
After that, the postoperative outcome was uneventful, and the patient was discharged on POD 35, with no fever, no abnormalities on the laboratory tests, and no collections at the abdominal ultrasound examination, but with an abdominal drain left in place (a daily purulent outflow of around 50 ml). The abdominal drain was removed on POD 50 in an outpatient ward after a contrast-enhanced computed tomography examination which showed complete regression of the peripancreatic abscess (Fig. 4).
Fig. 4. Abdominal contrast-enhanced computed tomography axial slice in the arterial phase performed on POD 50 showing complete regression of the peripancreatic abscess (open white arrow - the drainage catheter).

The final pathology examination of the operative specimen revealed a 0.5 cm-sized, poorly differentiated distal bile duct cholangiocarcinoma (pT3), with perineural and microvascular invasion. None of the 26 harvested lymph nodes presented metastases.
The postoperative outcome was uneventful for a while however, on POD 80, the patient was readmitted for melena without significant clinical impact. The physical examination was unremarkable except for the melena confirmation during the rectal examination. The laboratory tests revealed only anemia – hemoglobin serum level=7.4 g/dl (normal values, 11.5-17 g/dl). The upper endoscopy did not show any abnormalities. The abdominal ultrasound examination did not identify any abnormalities. With conservative treatment and transfusions, the melena was remitted within two days and the patient was discharged.
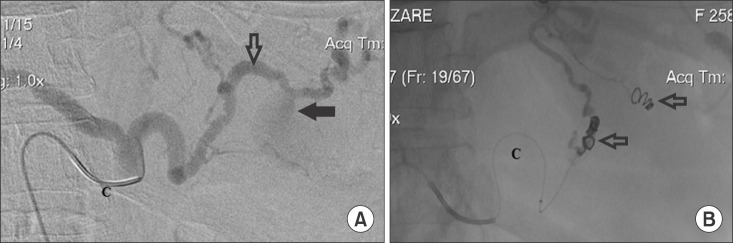
On POD 84, the patient was readmitted with recurrent melena with severe clinical impact (tachycardia, hypotension). The laboratory tests showed severe anemia (hemoglobin 4.7 g/dl). After rapid transfusions and fluid resuscitation, the patient underwent an enhanced-computed tomography that revealed a 3.2 cm×1.8 cm-sized pseudoaneurysm (Fig. 5A and 5C, filled black arrow) of the splenic artery (Fig. 5A and 5C, open black arrow) with a subsequent 9.5 cm×4.3 cm-sized hematoma formation (Fig. 5B, filled white arrow), and active bleeding in the distal part of the splenic artery (Fig. 5D, open black arrow). The patient was rapidly referred to the Interventional Radiology Department. A catheter was inserted via the right femoral artery and the splenic artery (Fig. 6A, open black arrow) where the pseudoaneurysm was identified (Fig. 6A, filled black arrow). After that, several pushable coils (Fig. 6B, open black arrow) were successfully mounted with no bleeding and no complications. The contrast-enhanced computed tomography control examinations, performed on day four and nine after the interventional procedure, showed no pseudoaneurysm (Fig. 7A and 7B, open black arrow), complete remission of the hematoma (Fig. 7C, filled white arrow), and several ischemic areas within the spleen, without a tendency of modification or abscesses at repeated examinations (Fig. 7A and 7B, filled black arrow). After the procedure, the clinical condition of the patient significantly improved with hemodynamic stability and no signs of hemorrhage.
Fig. 5. Abdominal contrast-enhanced computed tomography in the arterial phase performed on POD 84 (A) axial slice showing a 3.2 cm×1.8 cm-sized pseudoaneurysm (filled black arrow) of the splenic artery (open black arrow); (B) axial slice showing a high-density lesion indicating a subsequent 9.5 cm×4.3 cm-sized hematoma formation (filled white arrow); (C) frontal slice with reconstruction showing the pseudoaneurysm (filled black arrow) of the splenic artery (open black arrow); (D) axial slice showing extravasations of contrast agent suggesting active bleeding in the distal part of the splenic artery (open black arrow).
Fig. 6. (A) Digital subtraction angiogram obtained through the celiac trunk showing the splenic artery (open black arrow) with the pseudoaneurysm (filled black arrow) (C - the catheter positioned at the celiac ostium); (B) angiography showing pushable coils (open black arrow) on either side of a false aneurysm of the splenic artery, with no extravasations of contrast agent (C - the catheter positioned at the proximal part of the splenic artery).
Fig. 7. Check-up after embolization with an abdominal contrast-enhanced computed tomography axial slice in the arterial phase showing (A) on day 4 after the interventional radiology procedure the disappearance of the splenic artery pseudoaneurysm, presence of tiny arciform images due to the metal artifacts created by coils (open black arrow), and several ischemic areas within the spleen (filled black arrow); (B) on day 9 after the interventional radiology procedure the presence of tiny arciform images due to the metal artifacts created by coils (open black arrow) and stationary ischemic areas within the spleen (filled black arrow), without tendency of modification or abscesses; (C) on day 9 after the interventional radiology procedure the complete remission of the peripancreatic hematoma (filled white arrow).
Although the interventional radiology approach was a success for the splenic artery pseudoaneurysm, the patient died at a later time due to acute liver insufficiency not related to the pseudoaneurysm or interventional radiology procedure.
DISCUSSION
Delayed PPH is defined as bleeding that occurs more than 24 hours after the index operation, according to the International Study Group for Pancreatic Surgery.9 The median reported time between the pancreatic resection and appearance of a delayed PPH is around 12-39 days.11,12,13,16,17,19 A large part of these delayed PPHs occurred after the patient was discharged from the hospital.11,12 In the reported patient, the delayed PPH occurred on POD 80, after discharge. It appears that the mortality rate is higher in patients with a delayed PPH, at more than 39 days after surgery.19 A severe PPH implies a large volume of blood loss (a drop of hemoglobin level ≥3 g/dl) with clinically significant impairment, need for transfusions and an invasive treatment approach,9 as was the case in the above presented patient.
As it was previously mentioned, a delayed PPH represents a major concern after PD because it is an important source of postoperative mortality. Careful attention; a timely diagnosis of the source; and adequate, immediate therapy are of utmost importance for a successful outcome. A multidisciplinary approach created by experienced surgeons, interventional radiologists, endoscopists and intensivists is mandatory with these patients.
Delayed PPH is usually related to a local sepsis due to a pancreatic fistula, bile leak or intraabdominal abscess.9,15,17,20 Pathogenesis of a delayed PPH includes enzymatic digestion, local infection with secondary vascular wall erosion, or vascular injury at the time of resection.9,20 In the reported patient, the pathogenesis of the pseudoaneurysm was most likely the enzymatic/infectious erosion of the splenic artery wall secondary to the postoperative clinically significant pancreatic fistula. Clinically significant postoperative pancreatic fistula development after a PD was recently found to be an independent risk factor for a delayed PPH.10,15 Furthermore, postoperative pancreatic fistula is reported in up to 80% of the patients with a delayed PPH.11,13,17,19,21 The presence of bile in drainage and presence of clinical signs of infection (i.e., fever ≥38℃ and leukocytosis >10,000 per cubic millimeter for more than 5 consecutive days) were found to be independent risk factors for a massive delayed PPH after a PD.22
A splenic artery pseudoaneurysm is an uncommon pathology. Thus, as of 2007, no more than 200 patients with splenic artery pseudoaneurysms were described in the English literature.23 Furthermore, a splenic artery pseudoaneurysm represents an exceptional source for a delayed PPH after a PD.11,12,13,14,17,19,24,25 Most of the pseudoaneurysms that occur after PD are located at the level of the gastroduodenal artery stump or hepatic artery.9,10,11,13,14,16,17,19,20 Interestingly, a recent study suggested that the delayed PPH with origin from the splenic artery is more frequently encountered after pancreaticogastrostomy reconstruction than after PD.25
Sentinel bleeding, defined as minor blood loss via surgical drains or the gastrointestinal tract, with an asymptomatic interval of at least 12 hours until the development of hemorrhagic shock,10 is sometimes the only clinical sign that announces a massive PPH, as was the case with the reported patient. Sentinel bleeding is encountered in up to 77.8% of the patients with severe PPH.10,13,16,17,21 Some studies suggest mandatory angiographic exploration in every patient with sentinel bleeding after PD because a pseudoaneurysm is thus discovered in 35% of the patients.26
An upper digestive hemorrhage can be a clinical sign in an important proportion of patients with a false aneurysm of the splenic artery.23 An upper endoscopy sometimes does not identify the source of bleeding. Contrast-enhanced computed tomography with multiplanar reconstructions is mandatory in these situations to promptly identify the origin of hemorrhage,24 as was the case in the above presented patient.
The management of delayed PPH after PD represents a challenging problem, particularly when a pancreatic fistula is associated. An endovascular approach represents the first treatment option in patients with delayed PPH of an arterial origin and in patients without hemodynamic instability.11,13,15,16,19,20,21,24,25
Arterial embolization consists of an occlusion on either side of a false aneurysm in order to prevent further bleeding via reverse flow or anastomosis,24 as was the case in the above presented patient. The success rate of an arterial embolization used to stop the bleeding is up to 100%.24 Recurrence of the bleeding is usually related to persistence of the favouring factors (i.e., pancreatic/bile leak, persistent abscess).19
Spleen infarction is a reported complication after splenic artery embolization but rarely is associated with clinically significant consequences,27 as was the case in the reported patient.
Surgery represents an alternative treatment approach in patients with delayed PPH with massive bleeding and hemodynamic instability, in patients where it is mandatory to solve the underlying source of hemorrhage to prevent further arterial erosion (i.e., completion of a pancreatectomy for a severe pancreatic fistula),13,15,20,21,25 when interventional radiology procedures have failed13 or when immediate radiology interventions are not available.11,25 A recent meta-analysis associated surgery with significantly increased mortality rates compared with the interventional radiology approach for delayed PPH.17
In conclusion, this case illustrates the rare possibility of development of a splenic artery pseudoaneurysm with severe delayed PPH after PD complicated with a clinically significant pancreatic fistula, even after the patient was discharged from the hospital. Proper recognition of sentinel bleeding might play a major role for timely therapy of delayed PPH after PD. An interventional radiology approach represents the first treatment option in hemodynamically stable patients, with high success rates of stopping the bleeding.
References
- 1.Popescu I, Dumitraşcu T. Pancreatoduodenectomy--past, present and future. Chirurgia (Bucur) 2011;106:287–296. [PubMed] [Google Scholar]
- 2.Dumitrascu T, Dima S, Brasoveanu V, Stroescu C, Herlea V, Moldovan S, et al. Impact of a portal/superior mesenteric vein resection during pancreatico-duodenectomy for pancreatic head adenocarcinoma. Minerva Chir. 2014;69:301–313. [PubMed] [Google Scholar]
- 3.Schmidt CM, Turrini O, Parikh P, House MG, Zyromski NJ, Nakeeb A, et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Arch Surg. 2010;145:634–640. doi: 10.1001/archsurg.2010.118. [DOI] [PubMed] [Google Scholar]
- 4.Gooiker GA, van Gijn W, Wouters MW, Post PN, van de Velde CJ, Tollenaar RA Signalling Committee Cancer of the Dutch Cancer Society. Systematic review and meta-analysis of the volume-outcome relationship in pancreatic surgery. Br J Surg. 2011;98:485–494. doi: 10.1002/bjs.7413. [DOI] [PubMed] [Google Scholar]
- 5.Swanson RS, Pezzi CM, Mallin K, Loomis AM, Winchester DP. The 90-day mortality after pancreatectomy for cancer is double the 30-day mortality: more than 20,000 resections from the national cancer data base. Ann Surg Oncol. 2014;21:4059–4067. doi: 10.1245/s10434-014-4036-4. [DOI] [PubMed] [Google Scholar]
- 6.Mathur A, Luberice K, Ross S, Choung E, Rosemurgy A. Pancreaticoduodenectomy at high-volume centers: surgeon volume goes beyond the Leapfrog criteria. Ann Surg. 2015;262:e37–e39. doi: 10.1097/SLA.0000000000001330. [DOI] [PubMed] [Google Scholar]
- 7.Cameron JL, He J. Two thousand consecutive pancreaticoduodenectomies. J Am Coll Surg. 2015;220:530–536. doi: 10.1016/j.jamcollsurg.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 8.Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8–13. doi: 10.1016/j.surg.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery. 2007;142:20–25. doi: 10.1016/j.surg.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Ansari D, Tingstedt B, Lindell G, Keussen I, Ansari D, Andersson R. Hemorrhage after major pancreatic resection: incidence, risk factors, management, and outcome. Scand J Surg. 2016:pii: 1457496916631854. doi: 10.1177/1457496916631854. [in press] [DOI] [PubMed] [Google Scholar]
- 11.Asai K, Zaydfudim V, Truty M, Reid-Lombardo KM, Kendrick M, Que F, et al. Management of a delayed post-pancreatoduodenectomy haemorrhage using endovascular techniques. HPB (Oxford) 2015;17:902–908. doi: 10.1111/hpb.12464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Correa-Gallego C, Brennan MF, D'Angelica MI, DeMatteo RP, Fong Y, Kingham TP, et al. Contemporary experience with postpancreatectomy hemorrhage: results of 1,122 patients resected between 2006 and 2011. J Am Coll Surg. 2012;215:616–621. doi: 10.1016/j.jamcollsurg.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 13.Ding X, Zhu J, Zhu M, Li C, Jian W, Jiang J, et al. Therapeutic management of hemorrhage from visceral artery pseudoaneurysms after pancreatic surgery. J Gastrointest Surg. 2011;15:1417–1425. doi: 10.1007/s11605-011-1561-3. [DOI] [PubMed] [Google Scholar]
- 14.Huo Y, Chi J, Zhang J, Liu W, Liu D, Li J, et al. Endovascular intervention for delayed post-pancreaticoduodenectomy hemorrhage: clinical features and outcomes of transcatheter arterial embolization and covered stent placement. Int J Clin Exp Med. 2015;8:7457–7466. [PMC free article] [PubMed] [Google Scholar]
- 15.Jilesen AP, Tol JA, Busch OR, van Delden OM, van Gulik TM, Nieveen van Dijkum EJ, et al. Emergency management in patients with late hemorrhage after pancreatoduodenectomy for a periampullary tumor. World J Surg. 2014;38:2438–2447. doi: 10.1007/s00268-014-2593-0. [DOI] [PubMed] [Google Scholar]
- 16.Lee HG, Heo JS, Choi SH, Choi DW. Management of bleeding from pseudoaneurysms following pancreaticoduodenectomy. World J Gastroenterol. 2010;16:1239–1244. doi: 10.3748/wjg.v16.i10.1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roulin D, Cerantola Y, Demartines N, Schäfer M. Systematic review of delayed postoperative hemorrhage after pancreatic resection. J Gastrointest Surg. 2011;15:1055–1062. doi: 10.1007/s11605-011-1427-8. [DOI] [PubMed] [Google Scholar]
- 18.Wellner UF, Kulemann B, Lapshyn H, Hoeppner J, Sick O, Makowiec F, et al. Postpancreatectomy hemorrhage--incidence, treatment, and risk factors in over 1,000 pancreatic resections. J Gastrointest Surg. 2014;18:464–475. doi: 10.1007/s11605-013-2437-5. [DOI] [PubMed] [Google Scholar]
- 19.Ching KC, Santos E, McCluskey KM, Orons PD, Bandi R, Friend CJ, et al. Covered stents and coil embolization for treatment of postpancreatectomy arterial hemorrhage. J Vasc Interv Radiol. 2016;27:73–79. doi: 10.1016/j.jvir.2015.09.024. [DOI] [PubMed] [Google Scholar]
- 20.Camerlo A, Turrini O, Marciano S, Sarran A, Berdah S, Delpero JR, et al. Delayed arterial hemorrhage after pancreaticoduodenectomy: is conservation of hepatic arterial flow vital? Pancreas. 2010;39:260–262. doi: 10.1097/MPA.0b013e3181bdc1ff. [DOI] [PubMed] [Google Scholar]
- 21.Yekebas EF, Wolfram L, Cataldegirmen G, Habermann CR, Bogoevski D, Koenig AM, et al. Postpancreatectomy hemorrhage: diagnosis and treatment: an analysis in 1669 consecutive pancreatic resections. Ann Surg. 2007;246:269–280. doi: 10.1097/01.sla.0000262953.77735.db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tien YW, Lee PH, Yang CY, Ho MC, Chiu YF. Risk factors of massive bleeding related to pancreatic leak after pancreaticoduodenectomy. J Am Coll Surg. 2005;201:554–559. doi: 10.1016/j.jamcollsurg.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 23.Agrawal GA, Johnson PT, Fishman EK. Splenic artery aneurysms and pseudoaneurysms: clinical distinctions and CT appearances. AJR Am J Roentgenol. 2007;188:992–999. doi: 10.2214/AJR.06.0794. [DOI] [PubMed] [Google Scholar]
- 24.Cazejust J, Raynal M, Bessoud B, Tubiana JM, Menu Y. Diagnosis and radiological treatment of digestive haemorrhage following supramesocolic surgery. Diagn Interv Imaging. 2012;93:e148–e158. doi: 10.1016/j.diii.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 25.Darnis B, Lebeau R, Chopin-Laly X, Adham M. Postpancreatectomy hemorrhage (PPH): predictors and management from a prospective database. Langenbecks Arch Surg. 2013;398:441–448. doi: 10.1007/s00423-013-1047-8. [DOI] [PubMed] [Google Scholar]
- 26.Tien YW, Wu YM, Liu KL, Ho CM, Lee PH. Angiography is indicated for every sentinel bleed after pancreaticoduodenectomy. Ann Surg Oncol. 2008;15:1855–1861. doi: 10.1245/s10434-008-9894-1. [DOI] [PubMed] [Google Scholar]
- 27.Piffaretti G, Tozzi M, Lomazzi C, Rivolta N, Riva F, Caronno R, et al. Splenic artery aneurysms: postembolization syndrome and surgical complications. Am J Surg. 2007;193:166–170. doi: 10.1016/j.amjsurg.2006.09.007. [DOI] [PubMed] [Google Scholar]