Abstract
This is the first meta-analysis of the pooled prevalence of insomnia in the general population of China. A systematic literature search was conducted via the following databases: PubMed, PsycINFO, EMBASE and Chinese databases (China National Knowledge Interne (CNKI), WanFang Data and SinoMed). Statistical analyses were performed using the Comprehensive Meta-Analysis program. A total of 17 studies with 115,988 participants met the inclusion criteria for the analysis. The pooled prevalence of insomnia in China was 15.0% (95% Confidence interval [CI]: 12.1%-18.5%). No significant difference was found in the prevalence between genders or across time period. The pooled prevalence of insomnia in population with a mean age of 43.7 years and older (11.6%; 95% CI: 7.5%-17.6%) was significantly lower than in those with a mean age younger than 43.7 years (20.4%; 95% CI: 14.2%-28.2%). The prevalence of insomnia was significantly affected by the type of assessment tools (Q = 14.1, P = 0.001). The general population prevalence of insomnia in China is lower than those reported in Western countries but similar to those in Asian countries. Younger Chinese adults appear to suffer from more insomnia than older adults.
Trial Registration: CRD 42016043620
Introduction
Insomnia, which is characterized by difficulty initiating and maintaining sleep and/or waking up too early, appears to be one of the most frequent sleep complaints in the general population [1]. For example, approximately a third of the adult population in the USA suffer from insomnia [2]. It has been shown that insomnia has significant negative impact on daily functioning and is associated with work absenteeism, considerable impairment of quality of life, and increased medical and societal costs [3,4]. In addition, insomnia is frequently associated with a variety of psychiatric disorders, especially depression and anxiety [1,5,6].
Examining the prevalence of insomnia is essential for health professionals and policymakers to understand its influence on the general population and enact appropriate preventive strategies as well as to make reasonable health resource allocations and funding decisions based on the cost-burden to society. However, the prevalence of insomnia in the general population varies greatly across studies, ranging from 6% to 50% [7,8]. Such wide variation could be due to several factors, such as differences in the definition of insomnia, assessment tools and geographical locations. A systematic review of population studies on insomnia from Western countries interestingly found relatively low prevalence of insomnia (6%) using insomnia criteria according to Diagnostic and Statistical Manual of Mental Disorder-IV (DSM-IV) but high prevalence (30–48%) using insomnia symptoms [7]. Age and gender were the most commonly identified risk factors, with an increased prevalence in women and older adults [1].
To the best of our knowledge, no systematic review or meta-analysis of studies examining the prevalence of insomnia in China has been published. This study is a systematic, quantitative meta-analysis of the pooled prevalence of insomnia in the general adult population in China. In addition to the international literature, Chinese databases, which are not usually reviewed in the international literature, were also searched.
Methods
Inclusion and exclusion criteria
Studies fulfilling the following criteria were included: (a) cross-sectional studies examining prevalence of insomnia in the general population in mainland China (China thereafter); (b) available information on insomnia prevalence and sample size; (c) publications in full text either written in English or in Chinese. Studies conducted in specific subgroups (e.g., children, adolescents, and the elderly) or in special settings (e.g. hospitals, military) and studies used census sampling were excluded.
Search strategy
A search was conducted for relevant papers for further detailed review in PubMed (S1 File), PsycINFO, EMBASE and Chinese databases (China National Knowledge Interne (CNKI), WanFang Data and SinoMed from database inception to April 10, 2016. Search words were listed as follows: (“insomnia” or “sleep problem” or “sleep disturbance” or “sleep disorder” or “sleep quality”) and (“prevalence” or “rate” or “epidemiology” or “survey” or “risk factor”) and (“China” or “Chinese”). Manual searches were also conducted by reviewing the reference lists from retrieved papers to find further relevant articles. Two reviewers independently screened the hits by reviewing titles and abstracts. The complete relevant articles were downloaded for further screening. If the same data were reported in more than one publication, only the paper with more complete data was included. Any disagreement was settled by discussion with the third author.
Data extraction and quality assessment
Data extraction was independently performed by the two reviewers. A data extraction sheet included first author, year of publication, year of the study conducted, study setting, sample size, response rate, sampling method, measurement and criteria of insomnia, mean age, number and prevalence of insomnia for the whole sample and different demographic subgroups. To date, there have been no well-defined tools for assessing quality of observational epidemiological studies [9]. In line with other studies [10], sample size, sampling method and response rate were used as the criteria to assess the quality of included studies; i.e., those with larger sample size, random sampling and higher response rate were considered as having higher quality.
Statistical analysis
All statistical analyses were conducted using the Comprehensive Meta-Analysis software, Version 2 (Biosta, Inc. USA). As the prevalence estimates of insomnia in most included studies were neither close to 50%, nor close to 0 or 100%, the logit transformation was used to form an unbounded estimate for analyses and the back transformation to proportion was performed for the final presentation [11,12]. The I2 statistic was used to evaluate heterogeneity of the studies. When the I2 statistic was greater than 50%, the random effect model was used for the meta-analysis [13], although being more conservative than the fixed effect model [14]. Forest plots were drawn to visualize the extent of heterogeneity across studies. Furthermore, the following 7 subgroup analyses were conducted in order to assess if any of them could reduce/explain the observed heterogeneity of the findings: (1) male vs. female; (2) mean age of study sample, using the median split of the mean age of study samples (≤43.7 yrs vs. >43.7 yrs); (3) survey year, using the median split of the survey years (≤2006 vs. >2006); (4) assessment tool: PSQI vs. AIS vs. standardized question; (5) sample size, using the median of sample size of included studies (≤5,358 vs. >5,358); (6) sampling method (convenience vs. random sampling); (7) response rate: ≥80% vs. <80%. Following other studies [15,16], in subgroup analyses some continuous variables (age, survey year and sample size) were dichotomized by a median split approach. Publication bias was estimated using Egger’s linear regression test and Funnel plots. All reported probabilities (p value) were two-sided, and p<0.05 was regarded statistically significant.
Results
Study characteristics
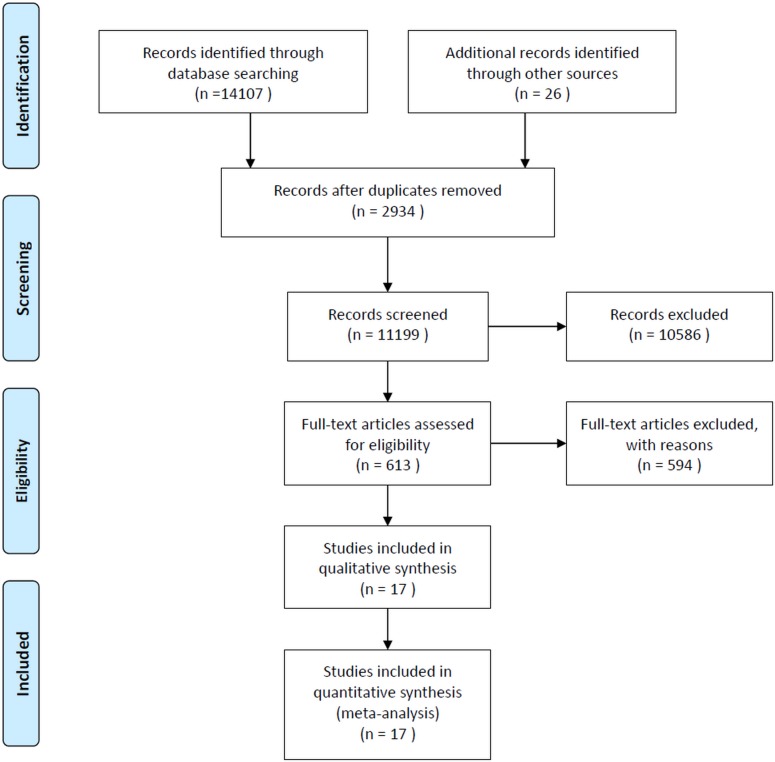
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (S1 Table). A total of 11,199 eligible papers were identified by the initial literature search and 11,182 of them were excluded for various reasons (see Fig 1). Finally, 17 studies (2 in English and 15 in Chinese) met the inclusion criteria and were included for analyses [17–33]. Characteristics of the included studies are shown in Table 1. The studies were conducted between 1996 and 2011. Sample size ranged between 306 and 22,551, with a total number of 115,988 and a median of 5,385. The mean age of the study sample ranged from 28 to 49.4 years with the median age of 43.7 years. The Pittsburgh sleep quality index (PSQI) was the most commonly used tool to assess insomnia, followed by standardized questions designed by researchers, e.g., “Do you have insomnia during the last month” and Athens insomnia scale (ASI). Fourteen studies were conducted in northern or southern China [17–27,29,31,32], and only 3 studies [28,30,33] were in western China.
Fig 1. PRISMA flow diagram.
Table 1. Characteristics of studies included in the meta-analysis.
| Authors and Publication year | Study site | Conducted year | Sampling method | Insomnia measures | Insomnia criteria | Response rate% | Mean age (range, yrs) | Sample size | Prevalence of insomnia % |
|---|---|---|---|---|---|---|---|---|---|
| Lu 2003 | Shenzhen | 1996 | Multistage stratified random sampling | PSQI | PSQI>7 | NR | 43.3 (15–86) | 948 | 10.8 |
| Chen 2004 | Xiamen | 2004 | Stratified random sampling | PSQI | PSQI>7 | 90.7 | NR | 2539 | 22.4 |
| Li 2005 | Gansu, Henan and Shandong province | 2000 | Multistage stratified random sampling | Do you have sleep disorder during past month? | Self-reported as yes | 97.8 | (≥18) | 9777 | 6.9 |
| Xiang 2008 | Beijing | 2003 | Multistage, stratified, systematic, and probability sampling | yes-no questions about whether they had each of three classic forms of sleep disturbance specified in the DSM-IV | Lasting two weeks or longer in the past 12 months | 94.8 | (≥15) | 5926 | 9.2 |
| Su 2008 |
Hebei Province | 2004 | Multistage stratified random sampling | PSQI | PSQI>7 | 86.3 | 44 (18–95) | 20716 | 11.6 |
| Zhang 2008 | Shandong Province | 2004 | Multistage stratified random sampling | PSQI | PSQI>7 | 94.0 | (>18) | 22551 | 13.18 |
| Wen 2010 | Xiamen | 2010 | Convenience sampling | PSQI | PSQI>7 | 88.3 | 33.5 (8–81) | 497 | 29.38 |
| Xie 2010 | Henan Province | 2006 | Stratified random sampling | PSQI | PSQI≥7 | 99.1 | 28 (14–84) | 1500 | 21.3 |
| Dai 2011 | Rizhao | 2010 | Stratified random sampling | AIS | AIS>6 | 96.4 | 45.2 (18–96) | 9732 | 21.66 |
| Liu 2011 | Beijing | 2010 | Stratified random sampling | PSQI | PSQI>7 | 95.6 | (22–82) | 306 | 40.5 |
| Sun 2011 | Shanghai | NR | Stratified sampling | Do you have difficulty in falling sleep? | ≥3 times/week and last at least 1 month or above | NR | (21–80) | 980 | 32.86 |
| Xu 2011 | Bozhou, Xinjiang, | 2009 | Stratified random sampling | AIS | AIS>6 | 89.2 | 38.4 (18–79) | 803 | 23.9 |
| Ye 2014 | Fujian Province | 2009 | Multistage stratified random sampling | PSQI | PSQI>7 | NR | 46.8±12.6(18–80) | 5358 | 4.5 |
| You 2014 | Chongqing | NR | Multistage stratified random sampling | PSQI | PSQI>7 | 94.82 | <18 - ≥60 | 1429 | 15.89 |
| Gu 2015 | Tianjin | 2011 | Multistage stratified random sampling | PSQI | PSQI>7 | 75.30 | ≥18 | 11618 | 6.6 |
| Zhang 2015 | Yibin, Sichuan, | NR | Multistage stratified random sampling | Do you have insomnia during the last month? | ≥12 d in the past month | 93.60 | 49.4±15.2 (18–98) | 11227 | 14.9 |
| Zhan 2016 | Beijing | 2007 | Multistage stratified random sampling | During the last month, have you had insomnia? | ≥3 times/week) | 83.50 | ≥18 | 10054 | 8.7 |
AIS: Athens insomnia scale; NR: not report; PSQI: Pittsburgh sleep quality index
Evaluation quality of the studies
Sixteen studies used stratified random sampling and only one used convenience sampling. While thirteen studies reported high response rates (≥80%), one study had a response rate of 75.3% and three did not report any response rate. Eight of the studies had a sample size larger than the median of 5,358 participants.
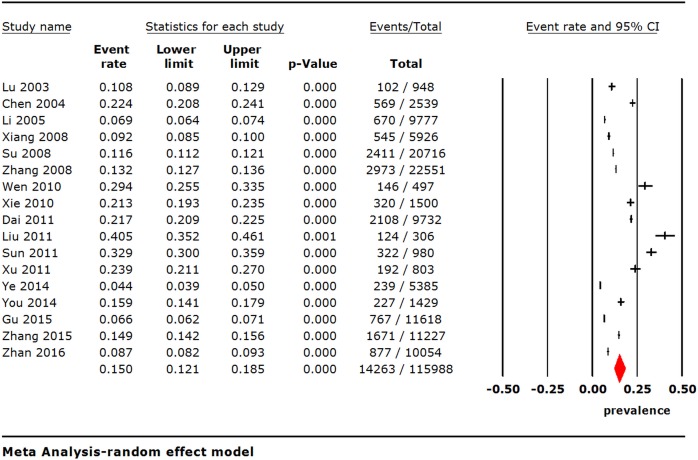
Heterogeneity of studies and summary of insomnia prevalence
Using the random effects model, the pooled point prevalence of insomnia with a total sample size of 115,988 in Chinese general population was 15.0% (95% Confidence interval [CI], 12.1%-18.5%; I2 = 99.5%) (Fig 2).
Fig 2. Point prevalence of insomnia in Chinese general population.
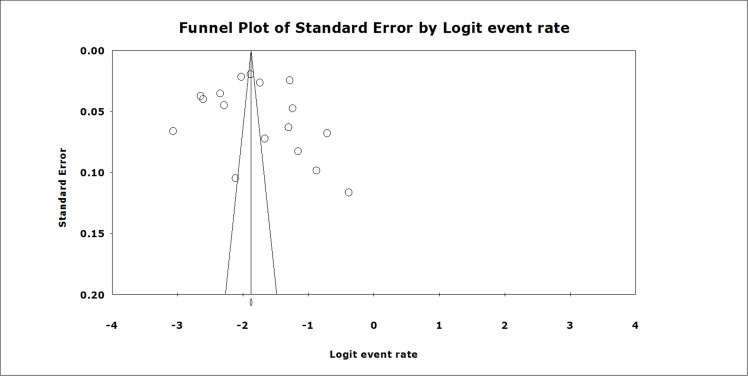
Publication bias
As Fig 3 shows, the funnel plots seem to be symmetrical as confirmed by Egger’s linear regression test (t = 0.54, p = 0.60), indicating that there is no publication bias.
Fig 3. Funnel plot of publication bias for the included studies.
Subgroup analyses
There were no significant associations between prevalence of insomnia and gender and the year in which the survey was done. The median of mean age of participants in the studies was 43.7 years. The pooled prevalence of insomnia in the older subject group was 11.6% (95% CI: 7.5%-17.6%), which was significantly lower than the figure (20.4%; 95% CI: 14.2%-28.2%) in the younger subject group. In ten studies which used the PSQI to assess insomnia, their pooled prevalence of insomnia was 15.1% (95% CI: 11.4%-19.6%). From the five studies that assessed insomnia with standardized questions, e.g., “Did you have insomnia in the past month”, the pooled prevalence of insomnia was 12.5% (95% CI: 8.1%-18.9%). Only two studies used the AIS to assess insomnia which resulted in a pooled prevalence of 22.3% (95% CI: 20.4%-24.4%). There was significant difference in the pooled prevalence of insomnia between the above three groups (Q = 14.1, P = 0.001) (Table 2).
Table 2. Prevalence of insomnia according to socio-demographic characteristics.
| Subgroups | Number of studies | Sample size | Sample size | Prevalence (%) | 95% CI | I2 (%) | Q-value (p-value) |
|---|---|---|---|---|---|---|---|
| Male | 14 | 45930 | 5046 | 14.2 | 11.1–18.0 | 98.8 | 2.84 (0.092) |
| Female | 14 | 53396 | 7934 | 18.5 | 15.2–22.4 | 98.9 | |
| Mean age of study samples ≤43.7 yrs | 4 | 3748 | 760 | 20.4 | 14.2–28.2 | 96.3 | 4.0 (0.046) |
| Mean age of study samples >43.7 yrs | 4 | 47060 | 6429 | 11.6 | 7.5–17.6 | 99.6 | |
| Survey year≤2006 | 7 | 63957 | 7590 | 12.7 | 9.9–16.2 | 99.1 | 0.47(0.49) |
| Survey year>2006 | 7 | 38395 | 4453 | 15.6 | 9.1–25.6 | 99.7 | |
| Assessment tool | |||||||
| PSQI | 10 | 67489 | 7878 | 15.1 | 11.4–19.6 | 99.3 | 14.1 (0.001) |
| AIS | 2 | 10535 | 2300 | 22.3 | 20.4–24.4 | 54.5 | |
| Standardized questions | 5 | 37964 | 4085 | 12.5 | 8.1–18.9 | 99.5 | |
| Sample size≤5358 | 9 | 14387 | 2241 | 19.9 | 12.9–29.3 | 99.1 | 5.48 (0.019) |
| Sample size>5358 | 8 | 101601 | 12022 | 10.9 | 8.3–14.1 | 99.6 | |
| Convenience sampling | 1 | 15349 | 3288 | 29.4 | 25.5–33.5 | 0 | 31.2 (<0.001) |
| Random sampling | 16 | 115491 | 14117 | 14.4 | 11.5–17.8 | 99.5 | |
| Response rate≥80% | 13 | 11618 | 767 | 6.6 | 6.2–7.1 | 0 | 64.4 (<0.001) |
| Response rate <80% | 1 | 97057 | 12833 | 16.6 | 13.5–20.3 | 99.3 | |
AIS: Athens insomnia scale; PSQI: Pittsburgh sleep quality index
In this meta-analysis, the quality of studies was assessed by sample size, sampling method and response rate. In order to examine the effects of the study quality on the results, further subgroup analyses were performed. The subgroups of “sample size ≤5,358 participants”, “convenience sampling” and “response rate <80%” were significantly associated with higher prevalence of insomnia (p<0.05) (Table 2).
Discussion
This was the first meta-analysis of the general population in China examining the prevalence of insomnia. Most studies assessed the prevalence of insomnia symptoms using the PSQI or AIS, while five studies used standardized questions “yes-no” answers without any restrictive criteria or their frequency. No studies used insomnia diagnoses according to DSM-IV. The pooled prevalence of insomnia in China was 15.0%, which was lower than those in many Western countries (e.g., 37.2% in France and Italy, 27.1% in USA and 50.5% in Poland) [2,8], but similar to findings reported from other Asian countries (e.g., 15.3% in Japan and 17.3% in Singapore) [7]. However, the results of studies should be viewed with caution due to the confounding effects caused by discrepancy in sample sizes, response rates, sampling methods and measures on insomnia. In addition, no publication bias was found in this study which may be related to the nature of prevalence studies. Unlike meta-analysis comparing two treatments where negative results are often not published, prevalence studies in the general population are less likely to be subjected to publication bias especially if the sample size is adequate.
No gender difference in the prevalence of insomnia was observed in our study, which was inconsistent with other studies [34–36]. There was also no significant difference pre- or post-2006 in the prevalence of insomnia, indicating a lack of change over time. This was not consistent with other cross-sectional studies, which showed a steady increase in the prevalence of insomnia in the general population over time [37–39].
Many studies consistently reported an increased prevalence of insomnia with age [1,7]. This study found that the pooled prevalence of insomnia in younger subjects was significantly higher than in older subjects, which clearly indicates that young people are more likely to suffer insomnia. Due to the rapid urbanization and industrialization younger adults often face career stress and work long hours frequently at night, which disrupts their biological sleep rhythm and lead to insomnia [40]. In addition, the widespread use of new media, such as computers and smart phones in younger adults in China, may be associated with an increasing risk of insomnia. Also, in a meta-analysis the potential impact of ecological bias on the results could not be excluded [41,42].
The PSQI was the most common tool used to measure insomnia, followed by standardized questions and the AIS. The pooled prevalence of insomnia differed significantly between different assessment tools, thus supporting the notion that the prevalence could be largely determined by measurement tools [7]. Not surprisingly, the pooled prevalence in high quality epidemiology studies (larger sample size, random sampling and higher response rate) was lower than that of low quality studies, suggesting that well-designed studies are needed to accurately evaluate the prevalence of insomnia in future. The studies with lower response rate reported relatively higher prevalence of insomnia, which suggests that non-responders were less likely to have insomnia leading to selection bias to an uncertain degree. In addition, the prevalence of insomnia was relatively higher in studies with smaller sample size. While there is no known external factor that could cause a systemic distortion in smaller studies, we can only assume that the results of smaller studies may be relatively more unstable. This observation however requires further clarification.
There are several limitations to this meta-analysis. First, none of the studies used the DSM-IV insomnia diagnoses. Second, large heterogeneity was still present in the subgroup analyses, although heterogeneity is difficult to avoid in large meta-analysis of epidemiological surveys [43,44]. Third, some important information, such as comorbid psychiatric disorders, substance use and dependence, marital status and education level, were not available or incomplete in the publications, therefore could not be included in the analyses. Fourth, different definitions of insomnia were used in the studies, which made it difficult to interpret the results. However, this is a common challenge many studies face in the field of sleep medicine. In addition, the discrepancy in study characteristics, such as study sizes, response rates and sampling methods, made direct comparisons between studies difficult. Finally, although the logit transformation to pool the prevalence was performed as default in the Comprehensive Meta-Analysis software, potential variance stability may potentially exist in such transformation [12].
Conclusions
This was the first meta-analysis of the pooled prevalence of insomnia in the general population of China. The pooled prevalence of insomnia is lower than those reported in Western countries, but similar to those in other Asian countries. Younger adults are more likely to suffer from insomnia than older adults.
Supporting information
(DOC)
(DOCX)
Acknowledgments
The study was supported by the Shenzhen Science and technology Innovation Committee (JCYJ 20140415092628039; JCYJ 20160429185235132; JCYJ 20160429185854999).
Data Availability
All the data used in this meta-analysis have been included in the Tables, Figures, and Supporting Information.
Funding Statement
The study was supported by the Shenzhen Science and Technology Innovation Committee (JCYJ 20140415092628039; JCYJ 20160429185235132; JCYJ 20160429185854999), http://www.szsti.gov.cn/.
References
- 1.Roth T (2007) Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med 3: S7–10. [PMC free article] [PubMed] [Google Scholar]
- 2.Leger D, Poursain B (2005) An international survey of insomnia: under-recognition and under-treatment of a polysymptomatic condition. Curr Med Res Opin 21: 1785–1792. 10.1185/030079905X65637 [DOI] [PubMed] [Google Scholar]
- 3.Fullagar HH, Skorski S, Duffield R, Hammes D, Coutts AJ, Meyer T. (2015) Sleep and athletic performance: the effects of sleep loss on exercise performance, and physiological and cognitive responses to exercise. Sports Med 45: 161–186. 10.1007/s40279-014-0260-0 [DOI] [PubMed] [Google Scholar]
- 4.Scott JP, McNaughton LR, Polman RC (2006) Effects of sleep deprivation and exercise on cognitive, motor performance and mood. Physiol Behav 87: 396–408. 10.1016/j.physbeh.2005.11.009 [DOI] [PubMed] [Google Scholar]
- 5.Benca RM (2001) Consequences of insomnia and its therapies. J Clin Psychiatry 62 Suppl 10: 33–38. [PubMed] [Google Scholar]
- 6.Staner L (2010) Comorbidity of insomnia and depression. Sleep Med Rev 14: 35–46. 10.1016/j.smrv.2009.09.003 [DOI] [PubMed] [Google Scholar]
- 7.Ohayon MM (2002) Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev 6: 97–111. [DOI] [PubMed] [Google Scholar]
- 8.Nowicki Z, Grabowski K, Cubala WJ, Nowicka-Sauer K, Zdrojewski T, Rutkowski M, et al. (2016) Prevalence of self-reported insomnia in general population of Poland. Psychiatr Pol 50: 165–173. 10.12740/PP/58771 [DOI] [PubMed] [Google Scholar]
- 9.Sanderson S, Tatt ID, Higgins JP (2007) Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol 36: 666–676. 10.1093/ije/dym018 [DOI] [PubMed] [Google Scholar]
- 10.Zhong BL, Liu TB, Chiu HFK, Chan SSM, Hu CY, Hu XF, et al. (2013) Prevalence of psychological symptoms in contemporary Chinese rural-to-urban migrant workers: an exploratory meta-analysis of observational studies using the SCL-90-R. Soc Psychiatry Psychiatr Epidemiol 48: 1569–1581. 10.1007/s00127-013-0672-4 [DOI] [PubMed] [Google Scholar]
- 11.Paulson JF, Bazemore SD (2010) Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA 303: 1961–1969. 10.1001/jama.2010.605 [DOI] [PubMed] [Google Scholar]
- 12.Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T (2013) Meta-analysis of prevalence. J Epidemiol Community Health 67: 974–978. 10.1136/jech-2013-203104 [DOI] [PubMed] [Google Scholar]
- 13.Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327: 557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 15.Li Y, Cao XL, Zhong BL, Ungvari GS, Chiu HF, Lai KY, et al. (2016) Smoking in male patients with schizophrenia in China: A meta-analysis. Drug Alcohol Depend 162: 146–153. 10.1016/j.drugalcdep.2016.02.040 [DOI] [PubMed] [Google Scholar]
- 16.Zheng W, Xiang YT, Xiang YQ, Li XB, Ungvari GS, Chiu HF, et al. (2016) Efficacy and safety of adjunctive topiramate for schizophrenia: a meta-analysis of randomized controlled trials. Acta Psychiatr Scand 134: 385–398. 10.1111/acps.12631 [DOI] [PubMed] [Google Scholar]
- 17.Chen YL, Yang XJ, Shi CF (2004) Elementary study on sleep quality and influence factors for common population in Xiamen, China (in Chinese). Strait Journal of Preventive Medicine 10: 4–6. [Google Scholar]
- 18.Dai FX (2011) Sleep quality and functional dyspepsia in community population (in Chinese). Journal of Shandong Medical College 33: 266–268. [Google Scholar]
- 19.Gu Y, Xu GM, Yin HF (2015) Epidemiplogic study on sleep quality of community population aged 18 years or over in Tianjin (in Chinese). Chinese Mental Health Journal 29: 199–203. [Google Scholar]
- 20.Li SX (2005) The performance assessment in health and responsiveness sectors of Chinese health system (in Chinese): Shandong University. [Google Scholar]
- 21.Liu CS, Liu YJ, Li YH, Wang QG, Kou HQ (2011) Primary investigation of sleep quality of community population in Zhoukou Dian town, Beijing (in Chinese). Chinese Journal of Basic Medicine in Traditional Chinese Medicine 17: 1028–1029. [Google Scholar]
- 22.Lu YW, Cheng ZR, Li YX, Gao H, Tang ZR, Zhao YF. (2003) Sleep quality's epidemiologic investigation in Shenzhen city (in Chinese). Medical Journal of Chinese People Health 15: 584–587. [Google Scholar]
- 23.Su KQ, Sun XL, Cui LJ, Jiang QP, Cui Z, Gao LH, et al. (2008) A survey on sleep quality of the people aged 18 years old in Hebei province (in Chinese). Chin Ment Health J 22: 302–305,318. [Google Scholar]
- 24.Sun FY, Wei QH, Xiao JW, Zhu Y, Zhang XH, Li P, et al. (2011) The investigation of insomnia of community population in Wusong Street, Baoshan District, Shanghai (in Chinese). Shanxi Chinese Medicine 32: 298–299. [Google Scholar]
- 25.Wen C, Ding LJ (2010) Study on the sleep quality of common population in Xiamen City (in Chinese). Chinese Journal of Health Education 26: 832–834, 844. [Google Scholar]
- 26.Xiang YT, Ma X, Cai ZJ, Li S-R, Xiang YQ, Guo HL, et al. (2008) The prevalence of insomnia, its sociodemographic and clinical correlates, and treatment in rural and urban regions of Beijing, China: A general population-based survey. Sleep 31: 1655–1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xie ZL, Li J (2010) Prevalence of sleep disorders in Henan province: a cross-sectional study (in Chinese). Journal of Chinese Medicine 25: 131–132. [Google Scholar]
- 28.Xu JC (2011) A survey on sleep disorder and sleep habits of the adult in Bozhou region (in Chinese): Xinjiang Medical University. [Google Scholar]
- 29.Ye LF, Hou JX, Yao LT, Huang GB, Wu XY, Liao XL, et al. (2014) Relaion between sleep quality and diabetes in the She ethnic minority group in Fujian province, China (in Chinese). chin J Clinicians (Electronic Edition) 8: 3469–3473. [Google Scholar]
- 30.You LN, Jiang HD, Wang XH, Li Q, Shen GH, Li XJ. (2014) Investigation of sleep disorder condition of population in Chongqing (in Chinese). Chin J Clinicians (Electronic Edition) 8: 2051–2053. [Google Scholar]
- 31.Zhan Y, Chen R, Zhang F, Wang J, Sun Y, Ding R, et al. (2014) Insomnia and its association with hypertension in a community-based population in China: A cross-sectional study. Heart Asia 6: 88–93. 10.1136/heartasia-2013-010440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang JX, Lu CH, Tang JS, Qiu HM, Liu LF, Wang SB, et al. (2008) The epidemiological study of sleep quality of people aged 18 years and above in Shandong province (in Chinese). Chinese Journal of Psychiatry 41: 161–167, 182. [Google Scholar]
- 33.Zhang RZ, Wang ZQ, Liu DM, Yang YH, Xiang DH, Liao H, et al. (2015) An epidemiological study on insomnia in permanent residents over the age of 18 years old in YiBin City (in Chinese). Chin J Nerv Dis 141: 150–154. [Google Scholar]
- 34.Krystal AD (2003) Insomnia in women. Clin Cornerstone 5: 41–50. [DOI] [PubMed] [Google Scholar]
- 35.Ohayon MM, Roth T (2003) Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res 37: 9–15. [DOI] [PubMed] [Google Scholar]
- 36.Sivertsen B, Krokstad S, Overland S, Mykletun A (2009) The epidemiology of insomnia: associations with physical and mental health. The HUNT-2 study. J Psychosom Res 67: 109–116. 10.1016/j.jpsychores.2009.05.001 [DOI] [PubMed] [Google Scholar]
- 37.Calem M, Bisla J, Begum A, Dewey M, Bebbington PE, Brugha T, et al. (2012) Increased prevalence of insomnia and changes in hypnotics use in England over 15 years: analysis of the 1993, 2000, and 2007 National Psychiatric Morbidity Surveys. Sleep 35: 377–384. 10.5665/sleep.1700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ford ES, Wheaton AG, Cunningham TJ, Giles WH, Chapman DP, Croft JB. (2014) Trends in outpatient visits for insomnia, sleep apnea, and prescriptions for sleep medications among US adults: findings from the National Ambulatory Medical Care survey 1999–2010. Sleep 37: 1283–1293. 10.5665/sleep.3914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kronholm E, Partonen T, Harma M, Hublin C, Lallukka T, Peltonen M, et al. (2016) Prevalence of insomnia-related symptoms continues to increase in the Finnish working-age population. J Sleep Res. 25:454–457. 10.1111/jsr.12398 [DOI] [PubMed] [Google Scholar]
- 40.Voelker R (2004) Stress, sleep loss, and substance abuse create potent recipe for college depression. JAMA 291: 2177–2179. 10.1001/jama.291.18.2177 [DOI] [PubMed] [Google Scholar]
- 41.Sterne JA, Egger M, Smith GD (2001) Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ 323: 101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Greenland S, Morgenstern H (1989) Ecological bias, confounding, and effect modification. Int J Epidemiol 18: 269–274. [DOI] [PubMed] [Google Scholar]
- 43.Long J, Huang G, Liang W, Liang B, Chen Q, Xie J, et al. (2014) The prevalence of schizophrenia in mainland China: evidence from epidemiological surveys. Acta Psychiatr Scand 130: 244–256. 10.1111/acps.12296 [DOI] [PubMed] [Google Scholar]
- 44.Winsper C, Ganapathy R, Marwaha S, Large M, Birchwood M, Singh SP. (2013) A systematic review and meta-regression analysis of aggression during the first episode of psychosis. Acta Psychiatr Scand 128: 413–421. 10.1111/acps.12113 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
Data Availability Statement
All the data used in this meta-analysis have been included in the Tables, Figures, and Supporting Information.