Abstract
Background:
Many children with developmental dislocation of the hip especially in underdeveloped countries reach walking age and still remain undiagnosed, which can be detrimental to their growth and development. Because of the lack medical services often encountered in these regions, it would be attractive to find a cheap and effective treatment. Our work evaluated the results of treatment of these children by closed reduction with or without adductor tenotomy in a prospective study.
Methods:
We included 20 patients in this study with 29 affected hips (15 right and 14 left). Nine patients (45%) had bilateral DDH and 11 (55%) had unilateral DDH. There were 18 girls (90%) and two boys (10%) who were followed up for a mean of 21 mo (18-24 mo). Ages ranged from 9 to 36 mo (mean age 18.3 mo). Patients were divided according to age into two groups: between 9-18 mo and from 19-36 mo. The first group included nine patients (14 hips) while the second had 11 patients (15 hips).
Results:
In the first group, closed reduction failed in two patients (two hips) during the follow-up period (14.3%) and this necessitated shift to open reduction, while in the second group only one patient (bilateral DDH) had a similar failure (13.3%). We identified four hips with avascular necrosis. Three of them required no further treatment, the remaining hip was openly reduced.
Conclusions:
Closed reduction in older children offers a valid and reproducible treatment modality in the hands of an experienced pediatric orthopaedic surgeon as long as there is close follow-up and thorough knowledge of possible complications and their management including the ability to shift timely to open reduction.
Key Words: DDH, delayed diagnosis, closed reduction, walking age, conservative treatment, abductor brace
INTRODUCTION
Developmental dysplasia of the hip (DDH) describes pathological changes in the hip joint occurring in the early years of life that if left unmanaged can have a detrimental effect on the affected child. Hip dislocation at birth has been reported to occur in 0.1% to 0.5%, and subluxation has been described to occur in 1%. Higher incidences of 2.5% to 5% have been reported by ultrasound screening.1–3 Safe swaddling in a natural flexed and abducted position have been shown to lead to a six-fold decrease of dysplasia in some populations.4 Breech presentation is the most important risk factor for DDH. Other risk factors include female sex by virtue of ligamentous laxity induced by maternal relaxin hormone, first-born children, a history of clinical instability, postural deformities, oligohydramnios, and a positive family history.5 Prematurity has not been found to predispose to DDH.6 Left hip affection is noted in 60% of children theorized to occur by the left occiput anterior position of most nonbreech newborns in whom the hip is adducted against the mother’s spine. Right sided or bilateral hip involvement has been noted to occur in 20%.7 In managing DDH, the ultimate goal is to obtain a stable concentrically reduced hip as early as possible. In older children with dysplasia the goal is to delay or prevent the development of osteoarthritis and to preclude the need for arthroplasty at a relatively young age.8 Subluxation diagnosed in the first few weeks after birth can be observed for a further 3 wk without any active treatment because spontaneous reduction occurs in 88%.4 Thereafter, active treatment should be initiated if there are still physical and ultra-sonographic signs of subluxation. Complete hip dislocations are treated actively upon diagnosis.1 Shorter et al.9 showed in a Cochrane review that delaying treatment for 2 to 8 wk lessens the need for treatment without a significant increase in late diagnosed dysplasia or surgery.
The effectiveness of a Pavlik harness in DDH before 6 mo has been well documented and is reflected in its success rate of more than 90%. However, it still has dangers and complications such as development of avascular necrosis, Pavlik harness disease, which is an acetabular blunting that occurs when the femoral head presses against the posterior acetabular lip, and rarely femoral nerve palsy.10,11 If stable reduction can not be achieved by the Pavlik harness, closed reduction under general anesthesia is indicated. Better results are obtained when reduction is done before the age of 6 mo.1 Once believed to reduce the incidence of avascular necrosis, prereduction traction remains controversial.12 Several types of fixed abduction braces are used after successful reduction by Pavlik harness with residual instability and absent contracture of the hip, although the duration of abduction bracing remains disputed.13
Pivotal to closed or open treatment of DDH is the concept of the safe zone of Ramsey, which describes the angle between maximal abduction and minimal abduction in which the hip remains reduced. It should measure at least 25 degrees and can be increased with release of the adductor longus. Hip flexion, abduction, and internal or external rotation define a cone of stability and if this cone measures greater than 30 degrees, it is considered satisfactory.7
This study evaluates the results of closed treatment of DDH in children and compares results between two age groups.
MATERIALS AND METHODS
Institutional ethical board approval was obtained for this study. The parents of the children were thoroughly informed about the possible alternatives, complications, and disadvantages of closed reduction in this age group, and a written detailed consent was obtained especially about the possibility that at any time during the course of closed treatment an open reduction could become necessary.
We included 20 patients in this prospective study with 29 affected hips (15 right and 14). Inclusion criteria were no prior treatment and late presenting DDH between the age of 9 and 36 mo. Neurological, septic, traumatic, or syndromic hip dislocations were excluded from our study.
Nine patients (45%) had bilateral DDH and eleven (55%) had unilateral DDH. Single-side DDH was found in the right hip in six (30%) and in the left hip in five children (25%). There were 18 girls (90%) and two boys (10%) who were followed for a mean of 21 mo (18-24 mo). They ranged in age between 9 and 36 mo (mean age 18.3 mo). They were divided into two groups according to age. Group A were patients between the ages of 9 and 18 mo and Group B were between the ages of 19 and 36 mo. Group A included nine patients (14 hips) and Group B included 11 patients (15 hips).
Although three of our patients had a positive family history of DDH, they still missed early diagnosis. Six patients were born by caesarian section and the rest were born via spontaneous vaginal delivery. True limping was the most common complaint. In younger children perineal care was reported to be difficult.
When mild traction exerted during the preliminary examination upon admission showed marked soft-tissue contracture of the affected hip, especially adduction contracture, hindering a possible reduction maneuver, we applied preliminary skin traction for 4 days in six hips, two unilaterally and two bilaterally, in an attempt to overcome the capsular and muscular contractures. Standardized pelvic anteroposterior radiographs were obtained at the time of diagnosis, postoperatively, and at final follow-up visits. They were assessed for Shenton’s line, Hilgenreiner’s line, acetabular index angle, neck-shaft angle, Wiberg center-edge angle, and severity of dislocation as described by the Tönnis classification.14 The modified MacKay score was used to evaluate the functional results of the hips at the final follow-up.15
All children received general anesthesia and a caudal block, and their hips were examined, gently avoiding vigorous maneuvers. Hip reduction was achieved by flexion beyond 90 degrees and gradual abduction while lifting the greater trochanter quite similar to the Ortolani maneuver. To determine the safe zone of Ramsey, the hip was adducted to the point of redislocation, and that position was noted. The hip was again reduced and extended until it dislocated, and again the point of dislocation was noted as well as the required internal rotation to maintain reduction. The range of motion in which the hip remained reduced was compared with the maximal range of motion. From this information, a “safe zone” was constructed. If the zone was relatively wide, the reduction was considered stable. Alternatively, if wide abduction or more than 10 to 15 degrees of internal rotation was required to maintain reduction, the reduction was considered unstable.
To increase the safe zone by allowing for a wider range of abduction, an adductor tenotomy either in a percutaneous or an open adductor tenotomy was performed depending on the degree and longevity of the adduction contracture. Except for three hips, tenotomy was done in all the remaining 26 hips. Central reduction was confirmed by the image intensifier, and a hip spica cast was applied according to Kumar16 on a hip spica frame. First, we abducted the hip to 45 degrees and flexed it to about 95 degrees while maintaining the reduction at all times. The amount of hip flexion and abduction required to keep the hip in the most stable position was determined clinically and checked by the C-arm. The child was padded and the standard bilateral hip spica after Kumar16 was applied. A post-spica radiograph was obtained, and the child was observed for distal circulation to the next morning and discharged. Spica immobilization was continued for 4 mo but a cast change was done routinely after 2 mo. This allowed for re-examination of hip stability under general anesthesia and for proper skin care of the child. A new cast was applied and again hip position was verified by image intensification.
A hip abduction brace (Ottobock, Hip Abduction Brace, Germany) was routinely used on a full-time basis for further 6 mo. After that the abduction brace was worn during the night and napping hours for a further 6 mo. Follow-up was planned after 2, 4, 6, 12 and 18 mo. Statistical analysis was done by SPSS 17.0 (IBM, Chicago, Ill.)
RESULTS
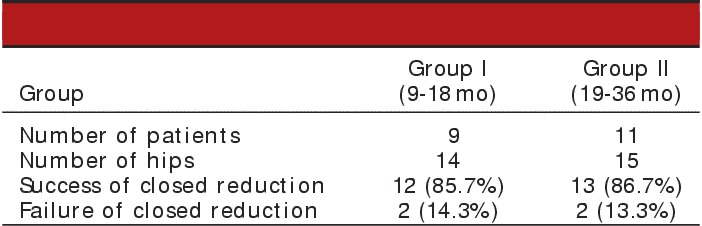
In group A, two patients (two hips) had failed closed reduction during the follow-up period (14.3%) and this necessitated a shift to open reduction, while in group B only one patient (bilateral DDH) had a similar failure (13.3%) and also required open reduction (Table 1).
TABLE 1.
Failure of closed reduction according to age group
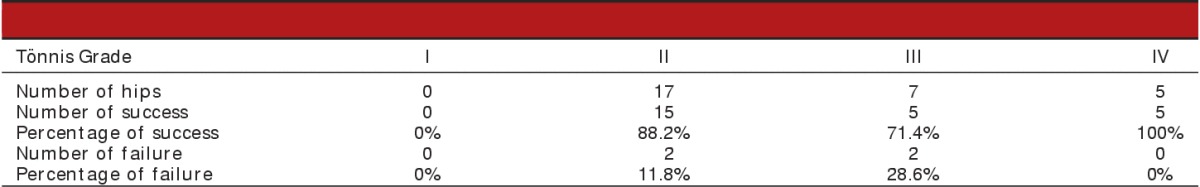
The success in maintaining reduction throughout the whole follow-up period without dislocation was a little higher in left-sided hips (92.9% compared with 80.0% for the right hips). Again, the success could not be linked to side affection (P value 0.598). We tried to find any significant relation between the severity of dislocation as described by Tönnis and failure of reduction, and surprisingly all failed cases did not belong to the highest grades of dislocation (two hips were grade II and two were grade III) (Table 2). Seventeen hips were grade II and success was 88.2% within this grade, while in grade III success was 71.4% in seven hips (Table 2). On the other hand, there were five grade IV cases none of which redislocated at the end of the procedure (P-value 0.342).
TABLE 2.
Relation between Tönnis grade and failure
The acetabular index (AI) angle was measured on initial radiographs and for all hips except two it was found to be above 30 degrees (mean angle 36.24 degrees). As by definition, acetabular dysplasia includes any AI angle above 30 degrees, and we considered a drop of AI below that level a significant result (Figure 1). For successful cases, we found the drop of the AI to be inversely related to the degree of dislocation. For example, all cases belonging to grade II or III of the Tönnis criteria decreased below 30 degrees, while cases with grade IV dropped under 30 degrees in 60%. This was statistically significant (P-value 0.013).
FIGURE 1.
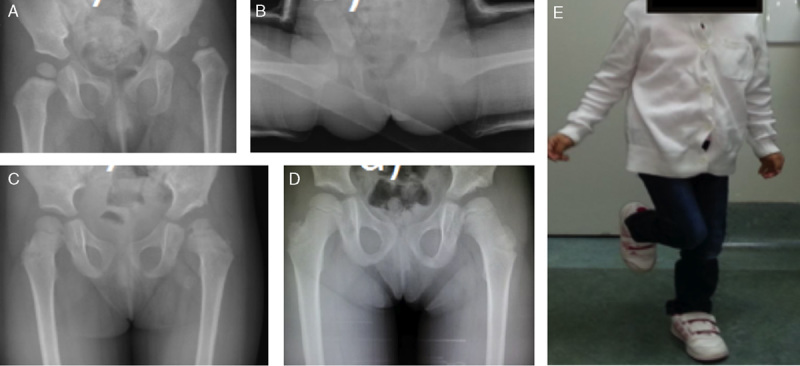
(A) Fourteen-month-old girl with left developmental hip dysplasia with acetabular index of 36 degrees. (B) Concentric reduction after adductor tenotomy and hip spica application. (C) After spica cast removal. (D) Six months after start of treatment (2 mo after spica casting). (E) Negative Trendelenburg test indicating good functional result.
According to the MacKay classification, excellent results were achieved in 10 hips (83.3% and 76.9%) in both groups. A good result was obtained in one (8.3%) group A hip and in two group B hips (15.4%). A fair result was found in one (8.3%) group A hip and in one group B hip (7.7%) (Table 3).
TABLE 3.
Functional result according to MacKay
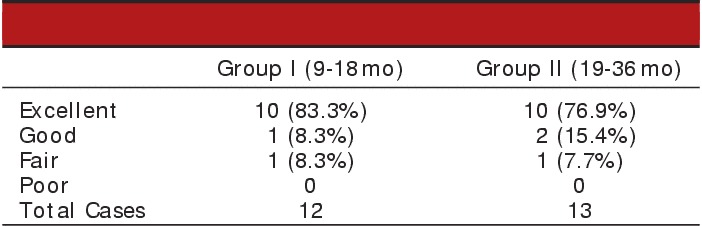
Excellent results were achieved in 12 left hips (92.3%) in comparison to the right hips which showed in eight hips (66.7%) an excellent outcome. Good results were recorded for the right in two hips (16.7%) and the left in one hip (7.7%). All Tönnis grade III hips had an excellent functional result according to MacKay classification at final follow-up, and 86.7 of grade II hips and 40% of grade IV had excellent results (P value of 0.142).
Of note, we observed in the bilateral hips that when one side failed and was shifted to open reduction the contralateral hip receiving conservative treatment tended to have a higher AI angle and higher center-edge angle as compared with other hips. We do not know the exact cause for this observation. One theory for this improved remodeling is that children prefer to bear weight on the less painful or less stiff joint, which consequently improves the hip joint molding capacity.
Complications
Avascular necrosis of the femoral head occurred in four of the remaining 25 hips during follow-up, with three of occurring in group A. The age factor in our series was statistically insignificant (P-value 0.265), indicating the contribution of other factors such as vigorous manipulation, tight reduction, or extreme positions to this complication. However, all AVN cases were type I and two of them resolved completely during the follow-up period. Interestingly, no cases of Tönnis type IV dislocation had AVN. We observed that skin traction did not prevent the occurrence of AVN. On the contrary, AVN was found in two of six hips for which traction was used before closed reduction based on our clinical perception of the presence of tight contractures (33%). However, no AVN occurred in Tönnis type IV hips suggesting that AVN is not related to the radiographic severity of dislocation, yet clinically perceived tightness or aggressive manipulation may be a factor for the development of AVN. Additionally, tenotomy did not prevent AVN as all cases of AVN had previous tenotomy (P-value 0.578).
One patient developed a right sided gluteal abscess from the edge of the cast pressing on the skin. This was discovered at the last week of spica cast treatment, and the abscess was drained under general anesthesia but required an adapted intravenous regimen of antibiotics for 1 wk. Nevertheless, the hip was found stable and the functional and radiographic outcomes were excellent.
One child suffered a right sided supracondylar buckle fracture early after initiating abductor brace therapy after falling from a standing height. A cast was applied for 6 wk and the fracture healed uneventfully. Other children developed muscle atrophy and skin indentation from the abductor brace so parents were instructed to pad the brace and to do thigh strengthening exercises.
DISCUSSION
After successful closed reduction in the first 6 mo acetabular development occurs most rapidly but it decelerates over the subsequent year.17 Although most authors do not recommend the use of the Pavlik harness after 6 mo of age,18 Pollet et al.19 treated late diagnosed infants between the ages of 6 and 24 mo with a harness claiming encouraging results in Graf type 3 hips but failure in Graf 4 hips.19 Van de Sande et al.20 reported successful treatment with a Pavlik harness in children between the ages of 5 to 13 mo with better results being achieved in initially less severe dislocated dysplastic hips.20 The modified Hoffmann-Daimler method used in late-presenting or neglected developmental dysplasia of the hip showed in a series involving 95 hips satisfactory radiographic results in 88 (93%) of the dislocated hips.21 Zionts and MacEwen22 reported the results in 51 congenitally dislocated hips in 42 children who were between 1 and 3 yr of age at the time of treatment. Thirty-eight hips (75%) were treated by traction prior to reduction, gentle closed reduction under anesthesia, selective adductor tenotomy, and immobilization in a hip spica cast. Thirteen hips (25%) required an open reduction when stable closed reduction could not be achieved. Secondary femoral or acetabular procedures were performed after either form of treatment if subluxation became apparent after the child had resumed walking. At an average 12-year follow-up (range 5 to 22 yr), 36 hips (71%) were rated according to Severin as class I, six as class II, eight as class III, and one as class IV. AVN developed in three hips. Our series had an average success rate of 86%, and we had four hips that developed AVN. Zionts and MacEwen believed that in this age group congenital dislocation of the hip is best treated by closed reduction followed by femoral or acetabular procedures as needed. Open reduction should be done only in those hips that cannot be reduced by closed methods.
Confounding factors of our study are limited statistical power, short follow-up, and lack of intraoperative arthrograms. Nevertheless, we conclude that closed reduction in children between 19 mo of age and 36 mo offers a valid and reproducible treatment modality in the hands of an experienced pediatric orthopaedic surgeon as long as there is close follow-up and thorough knowledge of possible complications and their management including the ability to shift timely to open reduction.
Footnotes
Financial Disclosure: The authors report no conflicts of interest.
REFERENCES
- 1.Guille JT, Pizzutillo PD, MacEwen GD. Development dysplasia of the hip from birth to six months. J Am Acad Orthop Surg. 2000; 8:232–242. [DOI] [PubMed] [Google Scholar]
- 2.Peled E, Eidelman M, Katzman A, et al. Neonatal incidence of hip dysplasia: ten years of experience. Clin Orthop Relat Res. 2008; 466:771–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wirth T, Stratmann L, Hinrichs F. Evolution of late presenting developmental dysplasia of the hip and associated surgical procedures after 14 years of neonatal ultrasound screening. J Bone Joint Surg Br. 2004; 86B:585–589. [PubMed] [Google Scholar]
- 4.Schwend RM, Shaw BA, Segal LS. Evaluation and treatment of developmental hip dysplasia in the newborn and infant. Pediatr Clin North Am. 2014; 61:1095–1107. [DOI] [PubMed] [Google Scholar]
- 5.Mulpuri K, Song KM, Goldberg MJ, et al. Detection and nonoperative management of pediatric developmental dysplasia of the hip in infants up to six months of age. J Am Acad Orthop Surg. 2015; 23:202–2055. [DOI] [PubMed] [Google Scholar]
- 6.Orak MM, Onay T, Orak MM, et al. Is prematurity a risk factor for developmental dysplasia of the hip? A prospective study. Bone Joint J. 2015; 97B:716–720. [DOI] [PubMed] [Google Scholar]
- 7.McCarthy J, Scoles P, MacEwen G. Developmental dysplasia of the hip (DDH). Current Orthopaedics. 2005; 19:223–230. [Google Scholar]
- 8.Vitale MG, Skaggs DL. Developmental dysplasia of the hip from six months to four years of age. J Am Acad Orthop Surg. 2001; 9:401–411. v. [DOI] [PubMed] [Google Scholar]
- 9.Shorter D, Hong T, Osborn D. Screening programmes for developmental dysplasia of the hip in newborn infants”. Cochrane database Syst Rev. 2011; 54:CD004595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kotlarsky P. Developmental dysplasia of the hip: What has changed in the last 20 years? World J Orthop. 2015; 6:886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clarke NMP, Castaneda P. Strategies to improve nonoperative childhood management. Orthop Clin North Am. 2012; 43:281–289. [DOI] [PubMed] [Google Scholar]
- 12.Fish DN, Herzenberg JE, Hensinger RN. Current practice in use of prereduction traction for congenital dislocation of the hip. J Pediatr Orthop. 1991; 11:149–153. [DOI] [PubMed] [Google Scholar]
- 13.Gans I, Flynn JM, Sankar WN. Abduction bracing for residual acetabular dysplasia in infantile DDH. J Pediatr Orthop. 2013; 33:714–718. [DOI] [PubMed] [Google Scholar]
- 14.Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. Berlin, Heidelberg: Springer Berlin Heidelberg; 1987:80–83. [Google Scholar]
- 15.McKay DW. A comparison of the innominate and the pericapsular osteotomy in the treatment of congenital dislocation of the hip. Clin Orthop Relat Res. 1974; 98:124–132. [DOI] [PubMed] [Google Scholar]
- 16.Kumar SJ. Hip spica application for the treatment of congenital dislocation of the hip. J Pediatr Orthop. 1981; 1:97–99. [DOI] [PubMed] [Google Scholar]
- 17.Lindstrom JR, Ponseti V, Wenger DR. Acetabular development after reduction in congenital dislocation of the hip. J Bone Joint Surg Am. 1979; 61:112–118. v. [PubMed] [Google Scholar]
- 18.Ömeroğlu H, Köse N, Akceylan A. Success of Pavlik harness treatment decreases in patients ≥4 months and in ultrasonographically dislocated hips in developmental dysplasia of the hip. Clin Orthop Relat Res. 2016; 474:1146–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pollet V, Pruijs H, Sakkers R, et al. Results of Pavlik harness treatment in children with dislocated hips between the age of six and twenty-four months. J Pediatr Orthop. 2010; 30:437–442. [DOI] [PubMed] [Google Scholar]
- 20.Van De Sande MAJ, Melisie F. Successful Pavlik treatment in late-diagnosed developmental dysplasia of the hip. Int Orthop. 2012; 36:1661–1668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Papadimitriou NG, Papadimitriou A, Christophorides JE, et al. Late-presenting developmental dysplasia of the hip treated with the modified Hoffmann-Daimler functional method. J Bone Joint Surg Am. 2007; 89:1258–1268. [DOI] [PubMed] [Google Scholar]
- 22.Zionts LE, MacEwen GD. Treatment of congenital dislocation of the hip in children between the ages of one and three years. J Bone Joint Surg Am. 1986; 68:829–846. [PubMed] [Google Scholar]


