Abstract
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is an X-linked disorder that affects as many as 400 million people worldwide, making it the most common enzymatic defect. Subjects with G6PD deficiency are more likely to develop neonatal hyperbilirubinemia potentially leading to kernicterus and are at increased risk for acute hemolytic anemia when exposed to pro-oxidant compounds such as anti-malarial drugs. We collected umbilical cord blood from 300 males born in Uganda to assess for novel markers of systemic oxidative stress. We determined that 10.7% of the samples collected were G6PD A- deficient (G202A/A376G) and when these were compared with unaffected controls, there was significantly higher 8-hydroxy-2’-deoxyguanosine (8-OHdG) concentration, elevated ferritin, increased leukocyte count and higher small molecule antioxidant capacity. These data suggest increased baseline oxidative stress and an elevated antioxidant response in umbilical cord blood of patients with G6PD deficiency.
Introduction
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is an X-linked disorder that affects as many as 400 million people worldwide, making it the most common human enzymatic defect. [1] It is prevalent in Sub-Saharan Africa, where an estimated 10–25% of individuals are G6PD deficient. [2] In this region, the G6PD A- (G202A/A376G) mutation is most prevalent. [2] G6PD is a key enzyme in the oxidative pentose phosphate pathway that leads to the generation of nicotinamide adenine dinucleotide phosphate (NADP)H allowing the regeneration of reduced glutathione (GSH) from it’s oxidized form glutathione disulfide (GSSG). GSH is an important reducing agent to neutralize reactive oxygen species via reducing equivalent donation. Exposure of G6PD deficient individuals to pro-oxidants such as anti-malarial medications, fava beans or infections can induce acute hemolytic anemia and potentially progression to shock. [1, 3] Newborns with G6PD deficiency are more likely to develop hyperbilirubinemia and jaundice, although this often occurs in the absence of any known trigger or hemolysis. Neonates exposed to pro-oxidants such as mentholatum, naphthalene, and henna. [4–8] As well, many newborns develop severe hyperbilirubinemia in the absence of any identifiable trigger of hemolysis. Severe neonatal hyperbilirubinemia can lead to kernicterus with significant morbidity and mortality. [9–11]
Currently, there is little data on other biomarkers associated with G6PD deficiency data outside of bilirubin. Our goal was to explore potential markers of oxidative stress that are associated with G6PD deficiency at birth. Identification of such markers may help us better understand the pathophysiology of G6PD deficiency.
Materials and methods
Sample collection
This study and the use of umbilical cord blood (UCB) were approved by the Committees on the Use of Human Subjects in Research at the University of Minnesota and at Mulago Hospital in Uganda and conducted according to the principles expressed in the Declaration of Helsinki. Umbilical cord blood from 300 consecutive males born at Mulago National Referral Hospital in Kampala, Uganda was collected into EDTA blood tubes and samples were de-identified. Each sample was initially tested for G6PD deficiency using the Beutler florescent spot test and confirmed later by PCR using protocols previously described. [2, 12] A complete blood count (CBC) was obtained using a Nihon Kohden hematology analyzer. Samples were stored at -25 degrees Celsius for later testing.
Assays for markers of oxidative stress
All assays were analyzed on a Tecan Sunrise microplate reader. The markers of inflammation/oxidative stress that we measured were as follows: 8-hydroxy-2’-deoxyguanosine (8-OHdG) (Trevigen, Gaithersburg, MD), protein carbonylation concentration (OxiSelect Protein Carbonyl ELISA Kit, Cell BioLabs), small molecule antioxidant capacity (Total Antioxidant Capacity Assay Kit, Abcam), catalase activity (StressXpress Colorimetric Activity Kit, StressMarq Biosciences Inc), and ferritin (Ramco Laboratories, Stafford, TX) according to the manufacturers’ protocol.
Statistical methods
Means for the G6PD deficient and control groups were each calculated and compared with a two-tailed Student’s t-test. Pearson’s was used for correlation of plasma 8-OHdG levels and absolute lymphocyte counts. The raw data for this study is contained in S1 Table.
Results and discussion
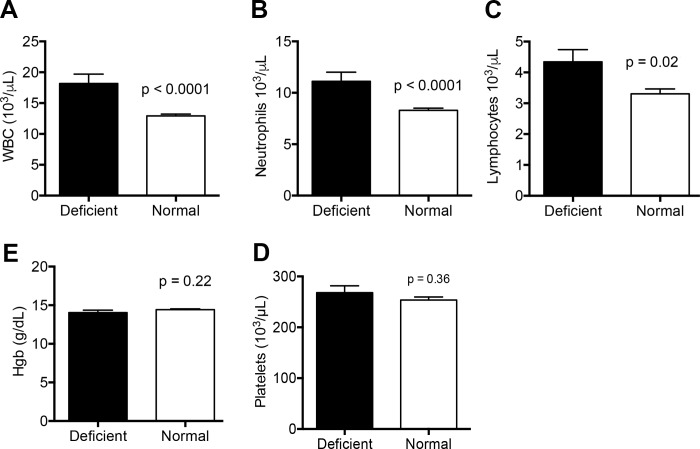
We collected umbilical cord blood from 300 males born at Mulago Hospital in Kampala, Uganda and found 32 were G6PD A- deficient (10.7%) using the fluorescent spot test and PCR confirmation. This is consistent with previously reported rates. [2] We measured CBCs from each sample and found significant elevations in the total number of lymphocytes (4.3 x 103/μL versus 3.3 x 103μL, p = 0.02) and neutrophils (11.1 x 103/μL versus 8.3 x 103μL, p < 0.0001) associated with G6PD deficiency (Fig 1A–1C). Increased lymphocytes and neutrophils contributed to a significantly elevated white blood cell count in G6PD deficient neonates (18.2 x103/μL versus 12.9 x103/μL, p < 0.0001; Fig 1). While clinical conditions such as infection or prolonged labor could account for such differences, these were not noted and most neonates were discharged 24 hours after delivery without follow-up. Hemoglobin and platelet levels were similar between G6PD deficient and unaffected neonates (14.0 g/dL versus 14.4 g/dL, p = 0.22; 268 x 103/μL versus 253 x 103/μL, p = 0.36; Fig 1D and 1E), consistent with previous reports. [13, 14] It is generally accepted that unless persons with G6PD deficiency are exposed to a pro-oxidant trigger, hemolysis is not observed. [15] Furthermore, several reports find that there is not necessarily any identifiable trigger for neonatal hyperbilirubinemia in G6PD deficient infants, and assessments of hemolysis just after birth do not correlate with total serum bilirubin levels.[16, 17] This is not always true for those with severe forms of G6PD deficiency, who may have chronic levels of hemolysis. [15]
Fig 1. Complete blood count indices in G6PD deficient UCB from male neonates.
(A-E) Total white blood cell (WBC), neutrophil, lymphocyte, platelet counts and hemoglobin were in G6PD deficient samples (n = 32) compared to normal controls (n = 240). Columns indicate the mean values and standard errors. P-values in two-way comparisons were derived from a Student’s t-test. Platelet values are from 23 G6PD deficient and 136 normal controls due to equipment malfunction. See also S1 Table.
G6PD deficiency is the prototypical disease in which oxidative stress incites a hemolytic crisis. While there was no evidence of hemolysis in the UCB samples in this study, we were interested to learn if there were markers of oxidative stress present at a subclinical level. Other biomarker studies have shown that end-tidal carbon monoxide and blood carboxyhemoglobin levels are elevated in newborns with G6PD deficiency, even in the absence of hemolysis. [18, 19] We investigated several known markers of oxidative stress and inflammation and found significant variation between G6PD deficient samples and the control group.
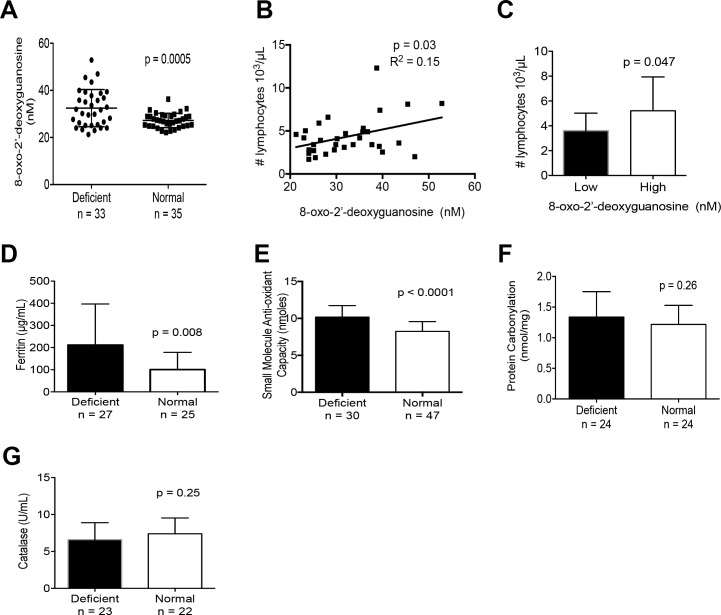
We quantified plasma 8-hydroxy-2’-deoxyguanosine (8-OHdG), an oxidized derivative of deoxyguanosine and commonly used as a nonspecific measure of oxidative stress. [20–22] The mean plasma 8-OHdG concentration was significantly elevated at 32.5 ng/mL in G6PD deficient samples compared to 27.2 ng/mL in controls (p = 0.0005; Fig 2A). We also found that higher levels of 8-OHdG correlated with elevated leukocytes in G6PD deficient neonates (Fig 1B and 1C). This observation suggests that 8-OHdG is linked to an inflammatory response in G6PD deficient neonates. In current literature, 8-OHdG has been interrelated to other measures of inflammation such as ferritin. [22, 23] Our study did also show significantly higher ferritin levels in UCB from G6PD deficient neonates (211.6 μg/mL vs 100.5 μg/mL, p = 0.008; Fig 2D), further supporting the hypothesis of a subclinical inflammatory response.
Fig 2. Markers of oxidative stress/inflammation in G6PD deficient UCB from male neonates.
(A) Levels of plasma 8-OHdG, n = 32 G6PD deficient, n = 35 Normal samples. (B) Pearson’s correlation analysis of plasma 8-OHdG levels and absolute lymphocyte counts. (C) Comparison of G6PD deficient UCB lymphocyte counts between high and low 8-OHdG levels determine by the median 8-OHdG value (31.9 nM). (D) Plasma ferritin concentration in UCB. (E) Plasma small molecule antioxidant capacity expressed in equivalents of Trolox. (F) Plasma protein carbonylation as nmol/mg. (G) Plasma catalase activity in UCB. See also S1 Table. Columns indicate the mean values and standard deviation. P-values in two-way comparisons were derived from a Student’s t-test.
By definition, persons with G6PD deficiency have erythrocytes that are much less capable to regenerate NADPH after it is oxidized to NADP leading to reduced anti-oxidant capacity. We performed a global assessment of the anti-oxidant capacity in plasma by measuring the amount of Cu2+ converted to Cu+ standardized against Trolox, an analog of Vitamin E. Interestingly, we found that the mean small molecule antioxidant capacity in G6PD deficient samples was elevated at 5.10 nmol/μl compared to 4.12 nmol/μl in control samples (p < 0.0001; Fig 2E). This data suggests that there may be a biologic response to the abnormally low levels of G6PD activity that includes increasing plasma levels of small molecule antioxidants such as ascorbate, uric acid and vitamin E in a compensatory effort.
Protein carbonylation involves the carbonyl modification of amino acids that occurs during free radical generation. [24, 25] We did not find a significant difference in carbonylation between G6PD deficient and control samples (p = 0.26; Fig 2F), thus we speculate that any preceding oxidative challenge may have been too brief to allow this modification to occur in UCB. Catalase has been previously reported to be reduced in Mediterranean men after fava bean ingestion [26], though we found no significant difference between G6PD deficient UCB samples and controls (p = 0.25; Fig 2G. The lack of G6PD deficiency’s effect on catalase activity has also been shown in a murine model of G6PD deficiency. [27]
This novel study in Sub-Saharan Africa shows the prevalence of G6PD deficiency in newborn males in Kampala, Uganda to be 10.7%. Our data suggest increased baseline oxidative stress and an elevated antioxidant response in UCB of patients with G6PD deficiency. Longitudinal follow-up was not a part of this study, however our results are the first to specify significant markers of oxidative stress in UCB of African newborns with G6PD deficiency. Further inquiry into the correlation between these markers and the development of clinically significant disease, such as hyperbilirubinemia, hemolysis, and the development of kernicterus, may allow us to better understand the pathophysiology of G6PD deficiency in the newborn.
Supporting information
(XLSX)
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
This work was supported by the Fulbright Foundation to PS. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Cappellini MD, Fiorelli G. Glucose-6-phosphate dehydrogenase deficiency. Lancet. 2008;371(9606):64–74. 10.1016/S0140-6736(08)60073-2 [DOI] [PubMed] [Google Scholar]
- 2.Hsu J, Fink D, Langer E, Carter ML, Bengo D, Ndidde S, et al. PCR-based allelic discrimination for glucose-6-phosphate dehydrogenase (G6PD) deficiency in Ugandan umbilical cord blood. Pediatric hematology and oncology. 2014;31(1):68–75. 10.3109/08880018.2013.860649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beutler E. Glucose-6-phosphate dehydrogenase deficiency: a historical perspective. Blood. 2008;111(1):16–24. Epub 2007/12/25. 10.1182/blood-2007-04-077412 [DOI] [PubMed] [Google Scholar]
- 4.Owa JA. Relationship between exposure to icterogenic agents, glucose-6-phosphate dehydrogenase deficiency and neonatal jaundice in Nigeria. Acta paediatrica Scandinavica. 1989;78(6):848–52. [DOI] [PubMed] [Google Scholar]
- 5.Sodeinde O, Chan MC, Maxwell SM, Familusi JB, Hendrickse RG. Neonatal jaundice, aflatoxins and naphthols: report of a study in Ibadan, Nigeria. Annals of tropical paediatrics. 1995;15(2):107–13. [DOI] [PubMed] [Google Scholar]
- 6.Kandil HH, al-Ghanem MM, Sarwat MA, al-Thallab FS. Henna (Lawsonia inermis Linn.) inducing haemolysis among G6PD-deficient newborns. A new clinical observation. Annals of tropical paediatrics. 1996;16(4):287–91. [DOI] [PubMed] [Google Scholar]
- 7.Tugwell P. Glucose-6-phosphate-dehydrogenase deficiency in Nigerians with jaundice associated with lobar pneumonia. Lancet. 1973;1(7810):968–9. [DOI] [PubMed] [Google Scholar]
- 8.Effiong CE, Aimaku VE, Bienzle U, Oyedeji GA, Ikpe DE. Neonatal jaundice in Ibadan. Incidence and etiologic factors in babies born in hospital. Journal of the National Medical Association. 1975;67(3):208–13. PubMed Central PMCID: PMC2609315. [PMC free article] [PubMed] [Google Scholar]
- 9.Kaplan M, Herschel M, Hammerman C, Hoyer JD, Stevenson DK. Hyperbilirubinemia among African American, glucose-6-phosphate dehydrogenase-deficient neonates. Pediatrics. 2004;114(2):e213–e9. [DOI] [PubMed] [Google Scholar]
- 10.Kaplan M, Hammerman C. Glucose-6-phosphate dehydrogenase deficiency: a potential source of severe neonatal hyperbilirubinaemia and kernicterus. Semin Neonatol. 2002;7(2):121–8. [DOI] [PubMed] [Google Scholar]
- 11.Slusher TM, Olusanya BO, Vreman HJ, Brearley AM, Vaucher YE, Lund TC, et al. A Randomized Trial of Phototherapy with Filtered Sunlight in African Neonates. N Engl J Med. 2015;373(12):1115–24. Epub 2015/09/17. 10.1056/NEJMoa1501074 [DOI] [PubMed] [Google Scholar]
- 12.Beutler E, Mitchell M. Special modifications of the fluorescent screening method for glucose-6-phosphate dehydrogenase deficiency. Blood. 1968;32(5):816–8. [PubMed] [Google Scholar]
- 13.Meloni T, Costa S, Cutillo S. Haptoglobin, hemopexin, hemoglobin and hematocrit in newborns with erythrocyte glucose-6-phosphate dehydrogenase deficiency. Acta haematologica. 1975;54(5):284–8. [DOI] [PubMed] [Google Scholar]
- 14.Meloni T, Cutillo S, Testa U, Luzzatto L. Neonatal jaundice and severity of glucose-6-phosphate dehydrogenase deficiency in Sardinian babies. Early human development. 1987;15(6):317–22. [DOI] [PubMed] [Google Scholar]
- 15.Cappellini MD, Fiorelli G. Glucose-6-phosphate dehydrogenase deficiency. The Lancet. 2008;371(9606):64–74. [DOI] [PubMed] [Google Scholar]
- 16.Kaplan M, Hammerman C, Renbaum P, Levy-Lahad E, Vreman HJ, Stevenson DK. Differing pathogenesis of perinatal bilirubinemia in glucose-6-phosphate dehydrogenase-deficient versus-normal neonates. Pediatric research. 2001;50(4):532–7. 10.1203/00006450-200110000-00018 [DOI] [PubMed] [Google Scholar]
- 17.Badejoko BO, Owa JA, Oseni SB, Badejoko O, Fatusi AO, Adejuyigbe EA. Early neonatal bilirubin, hematocrit, and glucose-6-phosphate dehydrogenase status. Pediatrics. 2014;134(4):e1082–8. 10.1542/peds.2014-0654 [DOI] [PubMed] [Google Scholar]
- 18.Kaplan M, Vreman HJ, Hammerman C, Leiter C, Abramov A, Stevenson DK. Contribution of haemolysis to jaundice in Sephardic Jewish glucose-6-phosphate dehydrogenase deficient neonates. Br J Haematol. 1996;93(4):822–7. [DOI] [PubMed] [Google Scholar]
- 19.Kaplan M, Herschel M, Hammerman C, Hoyer JD, Stevenson DK. Hyperbilirubinemia among African American, glucose-6-phosphate dehydrogenase-deficient neonates. Pediatrics. 2004;114(2):e213–9. [DOI] [PubMed] [Google Scholar]
- 20.Tsou TC, Chen CL, Liu TY, Yang JL. Induction of 8-hydroxydeoxyguanosine in DNA by chromium(III) plus hydrogen peroxide and its prevention by scavengers. Carcinogenesis. 1996;17(1):103–8. [DOI] [PubMed] [Google Scholar]
- 21.Nunomura A, Perry G, Pappolla MA, Wade R, Hirai K, Chiba S, et al. RNA oxidation is a prominent feature of vulnerable neurons in Alzheimer's disease. J Neurosci. 1999;19(6):1959–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maruyama Y, Nakayama M, Yoshimura K, Nakano H, Yamamoto H, Yokoyama K, et al. Effect of repeated intravenous iron administration in haemodialysis patients on serum 8-hydroxy-2'-deoxyguanosine levels. Nephrol Dial Transplant. 2007;22(5):1407–12. 10.1093/ndt/gfl789 [DOI] [PubMed] [Google Scholar]
- 23.Hori A, Mizoue T, Kasai H, Kawai K, Matsushita Y, Nanri A, et al. Body iron store as a predictor of oxidative DNA damage in healthy men and women. Cancer Sci. 2010;101(2):517–22. 10.1111/j.1349-7006.2009.01394.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buss H, Chan TP, Sluis KB, Domigan NM, Winterbourn CC. Protein carbonyl measurement by a sensitive ELISA method. Free radical biology & medicine. 1997;23(3):361–6. [DOI] [PubMed] [Google Scholar]
- 25.Suzuki YJ, Carini M, Butterfield DA. Protein carbonylation. Antioxid Redox Signal. 2010;12(3):323–5. PubMed Central PMCID: PMC2821144. 10.1089/ars.2009.2887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gaetani GF, Rolfo M, Arena S, Mangerini R, Meloni GF, Ferraris AM. Active involvement of catalase during hemolytic crises of favism. Blood. 1996;88(3):1084–8. [PubMed] [Google Scholar]
- 27.Xu Y, Zhang Z, Hu J, Stillman IE, Leopold JA, Handy DE, et al. Glucose-6-phosphate dehydrogenase-deficient mice have increased renal oxidative stress and increased albuminuria. Faseb J. 2010;24(2):609–16. PubMed Central PMCID: PMC2812032. 10.1096/fj.09-135731 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.