Abstract
Objectives
To examine the underlying mechanisms through which steady state emotions, specifically affect and emotion regulation, influence sleep quality among young adult low-income women.
Design
Cross-sectional
Setting
Stress and Health Study (2006–2012) in southeast Texas
Participants
A subgroup (n=392) of racially and ethnically diverse young adult women ages 18–31.
Measurements
Participants provided measures of positive and negative affect, difficulties in emotion regulation, and sleep quality. Structural equation models were designed to identify differential mediating roles of emotion dysregulation in the association between both positive and negative affect and sleep quality.
Results
The relationship between positive affect and improved sleep quality operated completely through domains of emotion regulation (β= −0.054, 95% CI: −0.08 to −0.03), whereas the adverse effects of negative affect exhibited both direct (β= 0.142, 95% CI: 0.06 to 0.23) and indirect (β= 0.124, 95% CI: 0.08 to 0.16) effects on poor sleep. Negative affect was associated with poor sleep quality via two pathways—it directly influenced sleep quality and it indirectly influenced sleep quality among women experiencing difficulties in emotion regulation.
Conclusions
Therapies targeting improvement and maintenance of healthy emotion regulation domains, while delineating the positive affect state from the negative affect state, may lessen the burden of poor sleep quality among low-income women.
Keywords: emotion regulation, affect, sleep quality, mediation model, women
INTRODUCTION
Overall health and psychological functioning are often linked to poor sleep-related outcomes (1). Poor sleep quality is a common complaint among individuals with physical conditions as well as affective disorders including depression, anxiety, and bipolar disorder (2,3). While emotion regulation has been implicated A growing body of research supports the hypothesis that regulatory emotional processes contribute to sleep outcomes (2,4). An interplay between affect and emotion regulation has been proposed in predicting sleep quality, but the roles of positive and negative emotions and their subsequent dysregulation to distinguish sleep quality remain largely unknown and have been highlighted as a research priority (2,5).
The effects of sleep, specifically sleep deprivation, on emotions and moods has been well documented in the experimental literature, but despite acknowledgement in the literature of a bidirectional relationship between emotions and sleep, the mechanisms through which emotions impact sleep has received less attention (6). Maladaptive strategies for managing affect are associated with difficulties in emotion regulation, which in turn may increase the risk for poor sleep quality (6–8). In a recent time-lagged analysis using daily diary data, Kouros and El-Sheikh (2015) examined bidirectional associations between sleep and mood in a community sample of 142 elementary school children (9). Findings suggested that within individuals, a day with worse mood than usual predicted poorer sleep quality that night, but between individuals poor sleep increased negative mood (9).
Positive affect and negative affect are two dominant and distinct dimensions of mood, associated with different regional activities in the prefrontal cortex (10). Conceptual models suggest that high negative affect, characterized by adverse mood states, is an independent predictor of chronic pain and cardiovascular disease, whereas high positive affect, characterized by high energy and full concentration, may buffer the influence of stress on health outcomes (11–14). Both high negative affect and low positive affect have been proposed as direct predictors of poor sleep, and high positive affect may additionally act as a buffer of negative affect, as well as other psychosocial risk factors (chronic life stress, social relationships, and psychological distress) on sleep problems (2,15).
The relationship between high negative affect and poor sleep may also be mediated by stress, coping strategies, and emotion regulation (16,17). Gross and John (2003) hypothesized that positive and negative affect are related to different emotion regulation strategies—increased positive affective experience and expression is associated with reappraisal regulation, whereas increased negative emotion expression is related to suppression regulation (18). Although often considered a symptom of sleep problems, emotion dysregulation is also a contributor to psychopathology and clinical disorders, including those related to sleep (4,6,19,20). Tsypes et al. (2013) identified difficulties with emotion regulation as a mediator of the relationship between generalized anxiety disorder diagnosis, which is correlated with both dimensions of affect, and problems with sleep (21). Thomsen et al. (2005) highlighted the need to investigate emotion regulation for individual differences in negative affect after finding that it accounted for more variation in negative affect than either age or gender (22). Both theoretical and empirical support exists for a model where affective states prompt emotion regulation. Calkins (1994) detailed a theoretical framework in which behavioral traits influence emotion regulation and argued that positive or negative affect act as sources of individual variation in emotion regulation (23). More recently, empirical investigations have investigated emotion regulation as a mediator between negative affect and aggression (24). Kim-Spoon, Cicchetti, and Rogosch (2013) found the effects of emotion negativity on internalizing symptoms were completely mediated through emotion regulation (25).
We have focused the present study on the role of emotion dysregulation as a mediator of the relationship between positive and negative affect and sleep quality on a racially diverse group of low-income women. Problems with sleep quality and sleep duration are more common among individuals with low income and education levels (26–28). In a sample of over 150,000 participants from the 2006 Behavioral Risk Factor Surveillance System, lower income was associated with a higher likelihood of sleep complaints, and this association was stronger among women (29). Poor sleep is often considered in the causal pathway between low income and socioeconomic status and increased disease risk, likely due to a combination of both mediating and moderating effects of psychosocial and physical health factors, as well as the built environment.(30) There has been a paucity of research, however, focusing specifically on mechanisms through which sleep is impacted among low-income groups. We hypothesized that negative affect is positively associated with worse sleep quality, and that this relationship is mediated by distinct domains of emotion dysregulation. In contrast, we hypothesized that positive affect is negatively associated with worse sleep quality, also mediated by emotion dysregulation. Based on previous studies looking only at direct associations, we expected negative affect to have a greater overall influence than positive affect on emotion dysregulation, as well as on sleep (31).
METHODS
Participants
A subgroup of low-income women attending one of six University of Texas Medical Branch (UTMB) family planning clinics and participating in the Stress and Health Study (2006–2012) provided data for this analysis (32). Inclusion criteria were: female, not pregnant, age ≥ 18 years; non-Hispanic white, non-Hispanic black, or Hispanic; able to speak English or Spanish; and able to consent. Participants completed questionnaires related to demographics, positive affect, negative affect, and emotion dysregulation. All survey instruments and consent forms were translated into Spanish by bilingual research assistants (all RAs were bilingual), and all instruments have been previously validated in Spanish (33–35). All participants had follow-up bi-monthly telephone interviews as a part of the larger longitudinal study (n = 886). A subgroup of 409 women were sequentially consented from telephone interviews to provide information on sleep quality, with the number of subgroup participants limited by research assistant availability. Participants with complete data (n = 392) on positive affect, negative affect, and emotion dysregulation were retained for analysis and did not differ from the larger sample (n =409) in age, race, education, employment status, and income. The study was approved by UTMB’s IRB and all participants provided written informed consent.
Measures
The Positive and Negative Affect Schedule (PANAS) is a valid and reliable self-report measure of positive affect and negative affect, consisting of two 10-item scales to capture the respective dimensions of affect (36). For each item, participants were asked to indicate on a five-point scale the extent to which they had experienced each item in the past 8 weeks. Responses were labeled “very slightly or not at all,” “a little,” “moderately,” quite a bit,” or “extremely”. The internal consistency estimate from the present study (Cronbach’s α = 0.85 for positive affect and α = 0.87 for negative affect), as well as correlation between the two scales (r = −0.09, p > 0.05) matches previous estimates of the orthogonal relationship between positive affect and negative affect as measured by the PANAS (36), and scores did not vary based on timing of entry to the study (p > 0.05, data not shown but available upon request).
The Difficulties in Emotion Regulation Scale (DERS) is a 36-item self-administered Likert-type scale used to assess emotion dysregulation trait, comprising six related dimensions including nonacceptance of emotional responses, difficulty concentrating on and accomplishing goals, impulsive behavior, lack of awareness of emotion responses, limited access to effective strategies to regulate emotions, and a lack of clarity about the emotions being experienced (37). Participants were instructed to indicate how often the items applied to themselves, with responses ranging from 1 (“almost never”) to 5 (“almost always”). In order to assess dysregulation specifically, many DERS items prompted participants to respond to situations in which they felt distress. DERS items were recoded so high scores on each item reflected greater dysregulation. The internal consistency estimate of reliability for the DERS items was excellent (Cronbach’s α = 0.92), and mean emotion dysregulation scores did not significantly vary based on timing of entry to the study.
The Pittsburgh Sleep Quality Index (PSQI) is a 19-item questionnaire which measures seven components of self-rated sleep quality and habits on a 0 to 3 scale, with higher scores indicating poorer sleep (38). The PSQI was self-administered—participants were asked to answer items based on their sleep during the previous month. A global index of sleep quality was created by summing component scores, and was treated as a continuous variable and the primary outcome of the study. The PSQI showed good internal consistency (Cronbach’s α = 0.84) and scores did not significantly vary based on timing of entry to the study (p > 0.05, data not shown).
Information on age, race and ethnicity, education, employment status, marital status, and income were collected and coded as dummy variables.
Data analysis
Initial bivariate associations were tested to examine relationships among sociodemographic characteristics, positive affect, negative affect, emotion dysregulation, and sleep quality. Group differences in sociodemographic characteristics were compared using one-way analysis of variance (ANOVA) with Bonferroni correction. Pair-wise Pearson correlation (r) was used to evaluate the association between continuous variables.
Mediation analysis was conducted using the default maximum likelihood estimator in the structural equation modeling (SEM) software program Mplus (39). The entire sample (n=392) was included in the model and considered relationships between positive affect and negative affect with emotion dysregulation and sleep quality. In addition to the primary model, which included emotion dysregulation as a mediator between positive and negative affect and sleep quality, several alternative models were also tested. The first considered positive affect and negative affect as mediators between emotion dysregulation and sleep quality, and the second considered sleep quality as a mediator between affect and emotion dysregulation. Positive affect was also included in a model as a moderator of the relationship between negative affect and emotion dysregulation.
Each model was adjusted for sociodemographic characteristics when they were marginally predictive (p< 0.10) of any of the main variables in the model. Model fit was evaluated through examination of test statistics: chi-square, comparative fit index (CFI, where values greater than 0.90 indicated good fit), and the root-mean-square error of approximation (RMSEA, where values less than 0.10 indicated good fit) with 90% confidence intervals (40,41). Indirect effects of positive affect and negative affect on sleep quality were also evaluated. To test for bias-corrected significance and to construct 95% confidence intervals, mediated effects were estimated using a bootstrapped sample of 1000 (42).
RESULTS
Descriptive statistics were examined for all study variables, as well as Pearson correlations for the main variables included in the mediation model. The study sample represented a racially and ethnically diverse group of participants—the majority of women identified as Black (n = 224, 57.1%), but White (n = 101, 25.6%) and Hispanic (n = 67, 17.1%) women were also well represented. The majority of the sample was categorized as extremely low-income, with an annual household income reported less than or equal to $5,000. Table 1 provides sociodemographic characteristics for the study sample.
Table 1.
Participant characteristics (n = 392)
| n | (%) | |
|---|---|---|
| Race | ||
| Black | 224 | (57.1) |
| Hispanic | 67 | (17.1) |
| White | 101 | (25.6) |
| Age (years) | ||
| 18 – 21 | 119 | (30.1) |
| 22 – 25 | 142 | (36.2) |
| 26 – 31 | 131 | (33.4) |
| Education | ||
| < 12th grade | 128 | (32.7) |
| High school graduate | 166 | (42.4) |
| Some college | 98 | (25.0) |
| Marital status | ||
| Married | 75 | (19.1) |
| Co-habitated | 76 | (19.4) |
| Boyfriend, not married | 146 | (37.2) |
| No boyfriend, not married |
95 | (24.2) |
| Employment | ||
| Full time | 107 | (27.3) |
| Part time | 57 | (14.5) |
| Homemaker | 70 | (17.9) |
| Unemployed | 158 | (40.3) |
| Annual household income | ||
| ≤ $5,000 | 267 | (68.1) |
| $5,000–$15,000 | 71 | (18.1) |
| > $15,000 | 54 | (13.8) |
No significant differences in sleep quality by any sociodemographic characteristics were observed in bivariate analyses. Some small yet statistically significant differences were observed, however, for positive affect—Black and White participants had significantly higher positive affect than Hispanic participants and women who worked full time reported higher positive affect than women who classified themselves as homemakers. Positive affect was moderately negatively correlated with emotion dysregulation, but was not correlated with negative affect or sleep quality. In contrast, negative affect exhibited moderate positive correlation with both emotion dysregulation and sleep quality (Table 2). Moderate positive correlation was also observed between emotion dysregulation and sleep quality.
Table 2.
Pearson correlation coefficients and descriptive statistics for study variables in the mediation model
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. Positive affect | 1.00 | |||
| 2. Negative affect | −0.09† | 1.00 | ||
| 3. Emotion dysregulation | −0.25 | 0.43 | 1.00 | |
| 4. Sleep quality | −0.09† | 0.26 | 0.37 | 1.00 |
| Mean | 31.1 | 21.6 | 79.7 | 4.9 |
| Standard deviation | 8.7 | 8.7 | 23.6 | 3.7 |
| Range | 0 – 50 | 0 – 48 | 36 – 161 | 0 – 17 |
Note: All correlations statistically significant (p < 0.001) except †.
Primary mediation model
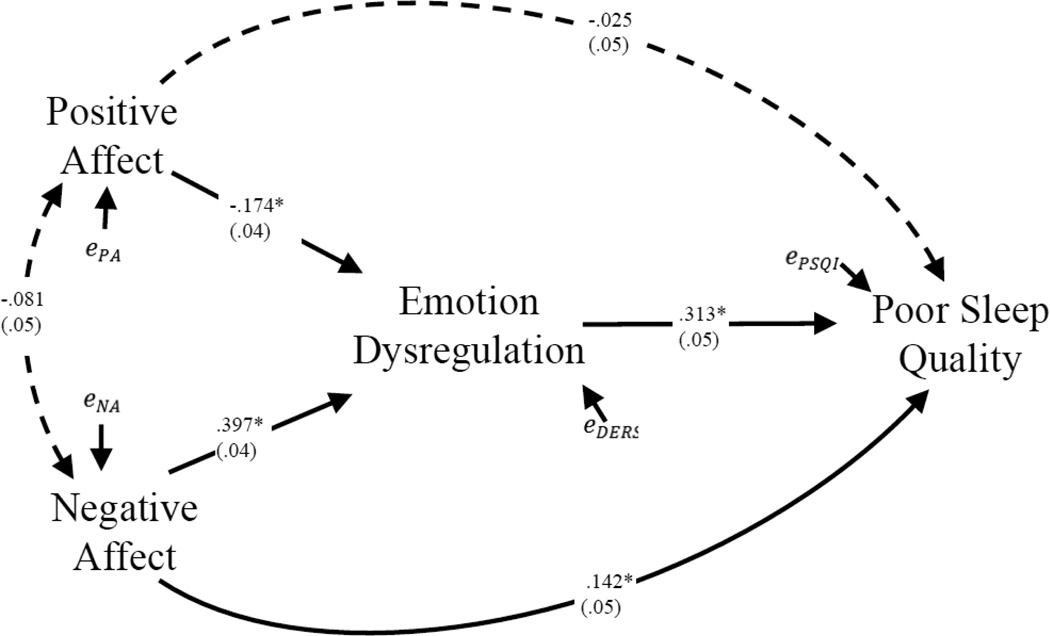
The final mediation model is presented in Figure 1. The model includes direct effects of positive affect and negative affect, respectively, on emotion dysregulation and sleep quality, as well as indirect effects of positive affect and negative affect on sleep quality, through emotion dysregulation. Model fit statistics indicated good overall model fit, χ2 (9) = 8.52, p > 0.05 (CFI = 1.00, RMSEA = <0.001, 90% CI: <0.001 to 0.055). The direct path from emotion dysregulation to sleep quality was highly significant (Figure 1). Positive affect was negatively associated with emotion dysregulation, whereas negative affect was positively associated with emotion dysregulation. Preliminary models testing the associations between affect and the six dimensions of emotion dysregulation suggested similar patterns as the overall emotion dysregulation score with few exceptions. Negative affect was directly associated with all six emotion dysregulation dimensions, and positive affect was directly associated with all six domains with the exception of “difficulty concentrating on and accomplishing goals.”
Figure 1.
Mediation effects of emotional dysregulation on the relationships from affect to sleep quality (n= 392)
Note: Coefficients (SE) are standardized; *p <.05; interrupted lines show non-significant coefficients. Models are adjusted for race, age, education, employment, marital status, and income. Fit: χ2 (9) = 8.52; p = 0.483, CFI= 1.00, RMSEA= <0.0001, 90% CI [<0.0001 to 0.055]; R2DERS=0.272; R2PSQI=0.181. Indirect effects through DERS: from NA: +0.124* (95% CI: 0.08 to 0.16); from PA: −0.054* (95% CI: −.08 to −.03), bootstrap CIs.
Both indirect effects of positive affect and negative affect, respectively, on sleep quality via emotion dysregulation were significant. The bias-corrected indirect standardized coefficient for negative affect was significant (β= 0.124, 95% bootstrap CI: 0.08 to 0.16, p< 0.001). The bias-corrected indirect standardized coefficient for positive affect was also significant (β =−0.054, 95% bootstrap CI: −0.08 to −0.03, p= 0.001), but more than two times smaller in magnitude than the indirect effect from negative affect. Only the direct effect to sleep quality from negative affect was significant (β = 0.142, 95% CI: 0.06 to 0.23, p= 0.005), indicating emotion dysregulation as a partial mediator for negative affect, and as a total mediator for positive affect. Moderated mediation analysis was also conducted to test whether the mediator, emotion dysregulation, also moderated the effect of positive affect and negative affect on sleep quality. This test for moderated mediation specifically assessed whether the mediational effects of emotion dysregulation varied across the levels of positive and negative affect, respectively,(43,44) and revealed no support for affect-by-emotion dysregulation interactions in separate models for positive affect and negative affect. Indirect and direct effects showed the same pattern as the classical approach from the final model reported, so we are confident in their estimates (44,45). Regarding the mediating effects of the six dimensions of emotion dysregulation, all dimensions except “lack of awareness of emotion responses” were indirectly associated with poorer sleep quality through negative affect; all dimensions except “difficulty concentrating on and accomplishing goals” were indirectly associated with poorer sleep quality through positive affect. In summary, negative affect was associated with poor sleep quality via two pathways—it directly reduced sleep quality and it indirectly reduced sleep quality among women experiencing difficulties in emotion regulation.
Alternative models
Several alternative models were also tested to determine other possible associations among variables. First, positive affect was included in a model as a moderator of the relationship between negative affect and emotion dysregulation. The fit of this model worsened dramatically in comparison to the final model, with no evidence of an interaction effect between positive affect and negative affect on emotion dysregulation or on sleep quality. A mediational model in which emotion dysregulation affects sleep quality through positive affect and negative affect was also considered, but model fit statistics (χ2 (14) = 21.53, p = 0.09) favored the model in Figure 1. Due to the cross-sectional nature of our study design, an equivalent model with sleep quality as a mediator of the relationship between affect and emotion dysregulation was also considered. Despite adequate fit statistics (χ2 (9) = 13.77, p = 0.13, the original mediation model (Figure 1) still had the best overall fit. We detail the alternative mediational models in Appendix A, and provide coefficients for all relationships between primary variables in the saturated model.
DISCUSSION
Overall, we have identified a mechanism through which emotional processes, specifically emotion dysregulation and affect, are related to poor sleep quality. Emotion dysregulation was found to be a larger contributor to poor sleep quality than the two dimensions of affect, which were more indirectly linked to sleep quality through emotion dysregulation. There has been some recent evidence in the literature proposing a similar conceptual framework, but our study adds further empirical support for an underlying mechanism linking emotional processes and sleep (4,6,46). In two recent studies, Brand et al. (2015) found that poor emotion regulation, stress, and coping completely mediated the relationship between perfectionism and poorer sleep.(47) In a similar analysis assuming a bidirectional link between sleep and emotional competence, Brand et al. (2015) found that whereas insomnia symptoms were associated with poorer emotion regulation and perception, insomnia was not associated with emotional expression, which are direct indicators of affect.(47) These results lend support to the theoretical framework that emotion regulation acts as a mediator in the association between personality traits or affect and sleep.
The strength of association between positive affect and negative affect, respectively, and emotion dysregulation is consistent with the literature, which suggests that negative affect and emotion dysregulation exhibit a greater association with poor sleep quality than positive affect does (4). We expected negative affect to have a greater overall influence than positive affect on emotion dysregulation, as well as on sleep, based on the body of evidence in the psychological literature suggesting that it is evolutionarily adaptive for negative stimuli and events to elicit stronger reactions and effects on health, well-being, and behavior than positive ones (31).
Our findings also suggest that the relationship between positive affect and poor sleep quality operates completely through emotion dysregulation—increasing positive affect has no direct effect on sleep quality, suggesting that any increase in positive affect may not attenuate poor sleep in an individual with high emotion dysregulation. When the positive affective state is identified, therapies aimed at improving sleep quality can target emotion regulation. In contrast, the adverse effects of increasing negative affect on poor sleep quality, which are more common in low-income populations, could be mitigated via more effective dimensions of emotion regulation (48). Our result suggests that in order to improve sleep quality among women with negative affect, more complex (multiple, or tiered) intervention strategies may be needed to focus simultaneously on negative affect and emotional dysregulation.
Limitations
The present study has several limitations. Participants were low-income women ages 18–31, which limits external generalizability. Second, since study design was cross-sectional, we made an assumption of temporal order in the model process with affect as an upstream predictor of emotion dysregulation. To justify the use of affect as a predictor of trait emotion dysregulation, we tested alternate mediational models where positive affect and negative affect mediated the relationship from emotion dysregulation to sleep quality, and where sleep quality was treated as the mediator. These alternative models did not perform as well as the model in Figure 1. Despite this finding, there is evidence to suggest that poor sleep quality or sleep loss inhibits neurocognitive processes, including emotional information processing and control over negative emotions (49). This is a complex problem—emotional distress can degrade sleep quality, and poor sleepers experience emotional consequences via cognitive change or altered behavior, which reinforces negative emotions such as reduced social engagement and activity (5). Future research should explore this alternate model prospectively.
It would be of interest for future investigations to determine if the significant pathways identified in Figure 1 can be generalized to other populations. Health providers’ ability to anticipate the risk of sleep problems if they are aware of patients’ affective states and emotion regulation strategies could help tailor cognitive-behavioral therapy (CBT) to function as a complement to interventions that specifically target sleep. In randomized controlled trials, CBT including sleep education, stimulus control, and time-in-bed restrictions have been compared to pharmacological treatment and placebo among patients with chronic insomnia—results suggest both acute and more long-term (6 months) benefits are associated with CBT (50). In the context of emotion regulation, CBT can be directed to operationalize concepts of cognitive reappraisal to change expectations and response to some negative exposure or outcome. Davies et al. (2015) also recommend acceptance and commitment therapy (ACT), which guides patients to increase their mindfulness, acceptance, and ability to “live in the moment” (51). A recent study examining the ability of CBT for anxiety to improve sleep related problems in an adolescent sample found parent-reported improvements in “bedtime resistance” and “sleep anxiety,” but adolescents did not report significant changes (52). For participants in our study—younger low income women, maybe the best approach is to try to address both the causes of distress in these women’s lives (improve clarity about the emotions being experienced), come to an acceptance of the emotions being experienced, and control impulsive behavior. Providers may additionally offer advice on how to achieve a “healthy” sleep environment (dim evenings, dark bedroom, do not turn on lights if awakens up in the middle of the night).
CONCLUSIONS
Overall, our findings suggest that emotion dysregulation mediates the relationship between affect and poor sleep quality in low-income women. This study has identified emotion dysregulation as a target for healthcare providers to potentially intervene in the cycle that operates when emotional processes compromise sleep quality, which in turn may lead to disrupted emotions. Further, it is also important for individuals to identify their own affective state, positive or negative, and attempt to target the different dimensions of emotion regulation that together can ultimately improve their sleep quality.
Supplementary Material
Acknowledgments
The authors wish to thank the UTMB Department of Obstetrics and Gynecology and Maternal Child Health Regional Program for the support of the study where Helen Wu was a faculty member (2000–2010). We thank Margarita Morgardo, Arely Duran, Didi Rivas, Diane Rosaly, Sultana Nasrin and Ebony Green (UTMB) for data collection; and Yimei Han (UTMB) for data management and analysis. These individuals were funded as part of the research team by Dr. Wu’s NIH grants. We also thank Zhuo Wang and Yu-Bo Wang, Department of Statistics, University of Connecticut, for their contributions to data management.
Grant support for this investigation came from the National Institutes of Health, National Institute on Drug Abuse (DA020058 and DA021814, PI: Helen Wu) and National Institute on Alcohol Abuse and Alcoholism (P30 AA019358, PI: Victor Hesselbrock).
Additional support for Dr. Wu and Ms. Hoag’s effort was provided by the Connecticut Institute for Clinical and Translational Science (CICATS) at UConn Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Smith MT, Huang MI, Manber R. Cognitive behavior therapy for chronic insomnia occurring within the context of medical and psychiatric disorders. Clin Psychol Rev. 2005;25(5):559–592. doi: 10.1016/j.cpr.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 2.Baglioni C, Spiegelhalder K, Lombardo C, Riemann D. Sleep and emotions: a focus on insomnia. Sleep medicine reviews. 2010;14(4):227–238. doi: 10.1016/j.smrv.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Stein MB, Belik SL, Jacobi F, Sareen J. Impairment associated with sleep problems in the community: relationship to physical and mental health comorbidity. Psychosom Med. 2008 Oct;70(8):913–919. doi: 10.1097/PSY.0b013e3181871405. [DOI] [PubMed] [Google Scholar]
- 4.Kahn M, Sheppes G, Sadeh A. Sleep and emotions: Bidirectional links and underlying mechanisms. International Journal of Psychophysiology. 2013;89(2):218–228. doi: 10.1016/j.ijpsycho.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Palmer CA, Alfano CA. Sleep and Emotion Regulation: An Organizing, Integrative Review. Sleep Medicine Reviews. 2016 doi: 10.1016/j.smrv.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Gruber R, Cassoff J. The Interplay Between Sleep and Emotion Regulation: Conceptual Framework Empirical Evidence and Future Directions. Curr Psychiatry Rep. 2014;16(11):1–9. doi: 10.1007/s11920-014-0500-x. [DOI] [PubMed] [Google Scholar]
- 7.Vandekerckhove M, Kestemont J, Weiss R, Schotte C, Exadaktylos V, Haex B, et al. Experiential versus analytical emotion regulation and sleep: Breaking the link between negative events and sleep disturbance. Emotion. 2012;12(6):1415. doi: 10.1037/a0028501. [DOI] [PubMed] [Google Scholar]
- 8.Gross JJ. Handbook of emotion regulation. Guilford Press; 2011. [Google Scholar]
- 9.Kouros CD, El-Sheikh M. Daily mood and sleep: reciprocal relations and links with adjustment problems. J Sleep Res. 2015;24(1):24–31. doi: 10.1111/jsr.12226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davidson RJ, Jackson DC, Kalin NH. Emotion, plasticity, context, and regulation: perspectives from affective neuroscience. Psychol Bull. 2000;126(6):890. doi: 10.1037/0033-2909.126.6.890. [DOI] [PubMed] [Google Scholar]
- 11.Pressman SD, Cohen S. Does positive affect influence health? Psychol Bull. 2005;131(6):925. doi: 10.1037/0033-2909.131.6.925. [DOI] [PubMed] [Google Scholar]
- 12.Nabi H, Kivimaki M, De Vogli R, Marmot MG, Singh-Manoux A Whitehall II Prospective Cohort Study. Positive and negative affect and risk of coronary heart disease: Whitehall II prospective cohort study. BMJ. 2008 Jun 30;337:a118. doi: 10.1136/bmj.a118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zautra A, Smith B, Affleck G, Tennen H. Examinations of chronic pain and affect relationships: Applications of a dynamic model of affect. J Consult Clin Psychol. 2001;69(5):786. doi: 10.1037//0022-006x.69.5.786. [DOI] [PubMed] [Google Scholar]
- 14.DeSteno D, Gross JJ, Kubzansky L. Affective science and health: The importance of emotion and emotion regulation. Health Psychology. 2013;32(5):474. doi: 10.1037/a0030259. [DOI] [PubMed] [Google Scholar]
- 15.Steptoe A, O'Donnell K, Marmot M, Wardle J. Positive affect, psychological well-being, and good sleep. J Psychosom Res. 2008;64(4):409–415. doi: 10.1016/j.jpsychores.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Ong JC, Carde NB, Gross JJ, Manber R. A two-dimensional approach to assessing affective states in good and poor sleepers. J Sleep Res. 2011;20(4):606–610. doi: 10.1111/j.1365-2869.2011.00907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kalmbach DA, Pillai V, Roth T, Drake CL. The interplay between daily affect and sleep: a 2-week study of young women. J Sleep Res. 2014 doi: 10.1111/jsr.12190. [DOI] [PubMed] [Google Scholar]
- 18.Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85(2):348. doi: 10.1037/0022-3514.85.2.348. [DOI] [PubMed] [Google Scholar]
- 19.Gross JJ. Emotion regulation: taking stock and moving forward. Emotion. 2013;13(3):359. doi: 10.1037/a0032135. [DOI] [PubMed] [Google Scholar]
- 20.van Middendorp H, Geenen R, Sorbi MJ, van Doornen LJ, Bijlsma JW. Emotion regulation predicts change of perceived health in patients with rheumatoid arthritis. Ann Rheum Dis. 2005 Jul;64(7):1071–1074. doi: 10.1136/ard.2004.020487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsypes A, Aldao A, Mennin DS. Emotion dysregulation and sleep difficulties in generalized anxiety disorder. J Anxiety Disord. 2013;27(2):197–203. doi: 10.1016/j.janxdis.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 22.Thomsen DK, Mehlsen MY, Viidik A, Sommerlund B, Zachariae R. Age and gender differences in negative affect—Is there a role for emotion regulation? Personality and Individual Differences. 2005;38(8):1935–1946. [Google Scholar]
- 23.Calkins SD. Origins and outcomes of individual differences in emotion regulation. Monogr Soc Res Child Dev. 1994;59(2–3):53–72. [PubMed] [Google Scholar]
- 24.Donahue JJ, Goranson AC, McClure KS, Van Male LM. Emotion dysregulation, negative affect, and aggression: A moderated, multiple mediator analysis. Personality and Individual Differences. 2014;70:23–28. [Google Scholar]
- 25.Kim-Spoon J, Cicchetti D, Rogosch FA. A longitudinal study of emotion regulation, emotion lability-negativity, and internalizing symptomatology in maltreated and nonmaltreated children. Child Dev. 2013;84(2):512–527. doi: 10.1111/j.1467-8624.2012.01857.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mezick EJ, Matthews KA, Hall M, Strollo PJ, Jr, Buysse DJ, Kamarck TW, et al. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project. Psychosom Med. 2008 May;70(4):410–416. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17(12):948–955. doi: 10.1016/j.annepidem.2007.07.096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Roberts RE, Roberts CR, Chan W. Ethnic differences in symptoms of insomnia among adolescents. SLEEP-NEW YORK THEN WESTCHESTER. 2006;29(3):359. doi: 10.1093/sleep/29.3.359. [DOI] [PubMed] [Google Scholar]
- 29.Grandner MA, Patel NP, Gehrman PR, Xie D, Sha D, Weaver T, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11(5):470–478. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006 Jul 1;164(1):5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 31.Baumeister RF, Bratslavsky E, Finkenauer C, Vohs KD. Bad is stronger than good. Review of general psychology. 2001;5(4):323. [Google Scholar]
- 32.Wu ZH, Tennen H, Hosain G, Coman E, Cullum J, Berenson AB. Stress Mediates the Relationship Between Past Drug Addiction and Current Risky Sexual Behaviour Among Low-income Women. Stress Health. 2014;32:138–144. doi: 10.1002/smi.2587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gómez-Simón I, Penelo E, De La Osa N. Factor structure and measurement invariance of the Difficulties Emotion Regulation Scale (DERS) in Spanish adolescents. Psicothema. 2014;26(3):401–408. doi: 10.7334/psicothema2013.324. [DOI] [PubMed] [Google Scholar]
- 34.Hita-Contreras F, Martínez-López E, Latorre-Román PA, Garrido F, Santos MA, Martínez-Amat A. Reliability and validity of the Spanish version of the Pittsburgh Sleep Quality Index (PSQI) in patients with fibromyalgia. Rheumatol Int. 2014;34(7):929–936. doi: 10.1007/s00296-014-2960-z. [DOI] [PubMed] [Google Scholar]
- 35.Ortuño-Sierra J, Santarén-Rosell M, Albéniz APd, Fonseca-Pedrero E. Dimensional structure of the Spanish version of the Positive and Negative Affect Schedule (PANAS) in adolescents and young adults. Psychol Assess. 2015;27(3):e1. doi: 10.1037/pas0000107. [DOI] [PubMed] [Google Scholar]
- 36.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 37.Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. [Google Scholar]
- 38.Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 39.Muthén LK, Muthén BO. Mplus User's Guide. (Sixth) 1998–2011 [Google Scholar]
- 40.Kenny DA, Kaniskan B, McCoach DB. The performance of RMSEA in models with small degrees of freedom. Sociological Methods & Research. 2014 0049124114543236. [Google Scholar]
- 41.Kline RB. Principles and practice of structural equation modeling. Guilford press; 2011. [Google Scholar]
- 42.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Imai K, Keele L, Tingley D. A general approach to causal mediation analysis. Psychol Methods. 2010;15(4):309. doi: 10.1037/a0020761. [DOI] [PubMed] [Google Scholar]
- 44.Muthén B, Asparouhov T. Causal effects in mediation modeling: an introduction with applications to latent variables. Structural Equation Modeling: A Multidisciplinary Journal. 2014:1–12. (ahead-of-print) [Google Scholar]
- 45.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 46.Markarian SA, Pickett SM, Deveson DF, Kanona BB. A model of BIS/BAS sensitivity, emotion regulation difficulties, and depression, anxiety, and stress symptoms in relation to sleep quality. Psychiatry Res. 2013;210(1):281–286. doi: 10.1016/j.psychres.2013.06.004. [DOI] [PubMed] [Google Scholar]
- 47.Brand S, Kirov R, Kalak N, Gerber M, Schmidt NB, Lemola S, et al. Poor sleep is related to lower emotional competence among adolescents. Behavioral sleep medicine. 2015:1–13. doi: 10.1080/15402002.2015.1048450. [DOI] [PubMed] [Google Scholar]
- 48.Adler NE, Snibbe AC. The role of psychosocial processes in explaining the gradient between socioeconomic status and health. Current Directions in Psychological Science. 2003;12(4):119–123. [Google Scholar]
- 49.Walker MP, van Der Helm E. Overnight therapy? The role of sleep in emotional brain processing. Psychol Bull. 2009;135(5):731. doi: 10.1037/a0016570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Morin CM, Vallières A, Guay B, Ivers H, Savard J, Mérette C, et al. Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia: a randomized controlled trial. JAMA. 2009;301(19):2005–2015. doi: 10.1001/jama.2009.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Davies CD, Niles AN, Pittig A, Arch JJ, Craske MG. Physiological and behavioral indices of emotion dysregulation as predictors of outcome from cognitive behavioral therapy and acceptance and commitment therapy for anxiety. J Behav Ther Exp Psychiatry. 2015;46:35–43. doi: 10.1016/j.jbtep.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 52.Peterman JS, Carper MM, Elkins RM, Comer JS, Pincus DB, Kendall PC. The effects of cognitive-behavioral therapy for youth anxiety on sleep problems. J Anxiety Disord. 2016;37:78–88. doi: 10.1016/j.janxdis.2015.11.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.