Abstract
Objective
The postpartum period is associated with a high risk of psychiatric episodes. The authors studied mortality in women with first-onset severe psychiatric disorders following childbirth and compared their mortality rates with those in women from the background population including other female psychiatric patients (mothers and childless women).
Method
In a register-based cohort study with linked information from Danish population registers, the authors identified women with first psychiatric inpatient or outpatient contacts 0–3 months postpartum. The main outcome measure was mortality rate ratios (MRRs): deaths from natural causes (diseases and medical conditions) or unnatural causes (suicides, accidents, and homicides). The cohort included 1,545,857 women representing 68,473,423 person-years at risk.
Results
In total, 2,699 women had first-onset psychiatric disorders 0–3 months postpartum, and 96 of these died during follow-up. Women with postpartum psychiatric disorders had a higher MRR (3.74; 95% CI=3.06–4.57) than non-postpartum-onset mothers (MRR=2.73; 95% CI=2.67–2.79) when compared with mothers with no psychiatric history. However, childless women with psychiatric diagnoses had the highest MRR (6.15; 95% CI=5.94–6.38). Unnatural cause of death represented 40.6% of fatalities among women with postpartum psychiatric disorders, and within the first year after diagnosis, suicide risk was drastically increased (MRR=289.42; 95% CI=144.02–581.62) when compared with mothers with no psychiatric history.
Conclusions
Women with severe postpartum psychiatric disorders had increased MRRs compared with mothers without psychiatric diagnoses, and the first year after diagnosis represents a time of particularly high relative risk for suicide in this vulnerable group.
Psychiatric disorders following childbirth have diverse presentations, and the incidence of the most severe postpartum psychiatric disorders necessitating hospitalization is 1–2 per 1,000 births (1–6). Severe postpartum psychiatric disorders can have serious implications for the women, children, and families affected (7, 8). The first few months postpartum carry the highest risk of both first-onset episodes and recurrence of psychiatric disorders, with the highest risk at 10–19 days postpartum (3).
Rare but tragic outcomes of untreated psychiatric disorders among new mothers include suicide, suicide attempts, and infanticide (9, 10). A limited number of studies have investigated the prognosis and long-term survival of women with specific postpartum psychiatric disorders, and reports have identified suicide as one of the primary causes of death among British mothers (11–13). In addition, Appleby et al. (14) documented a 70-fold increased risk of suicide within the first postpartum year in women with postpartum psychoses.
Recently there has been an increased focus on long-term outcomes and prognoses of psychiatric patients. The life expectancy of psychiatric patients with severe psychiatric disorders (e.g., schizophrenia and affective disorders) is approximately 15–20 years shorter than in the general population (15). Building on this, a recent review investigating the risk of all-cause mortality in patients with psychiatric disorders showed that women with a postpartum psychiatric admission had the highest mortality rates in all of the diagnostic groups represented (16).
Using the Danish population registers, we sought to significantly expand the current limited knowledge on long-term survival in mothers with severe postpartum psychiatric disorders. The primary aims of our study were twofold:
To describe all-cause mortality by calculating mortality rates of natural causes of death (diseases and medical conditions) and of unnatural causes of death (suicides, accidents, and homicides) among women with first-onset episodes of severe postpartum psychiatric disorders; and
To compare mortality rates in this group of patients with mortality rates for women from a comparison population with no psychiatric history and for other female psychiatric patients (mothers and childless women).
METHOD
Study Design
We conducted an epidemiological register-based cohort study on women from the Danish population. The main exposure variable was defined as any first psychiatric inpatient or out-patient contact within the first 90 days postpartum.
The outcome variable was defined as death by any natural cause (mortality from internal causes, such as diseases and medical conditions) or unnatural cause (mortality from external causes, such as suicide, accidents, and homicide) within the follow-up period.
Data were collected on all women born in Denmark on Jan. 1, 1950, or later. A total of 1,545,857 women were included in the study cohort after excluding women who emigrated from Denmark or died before age 15.
The follow-up period started on the women's 15th birthday or on Jan. 1, 1970, whichever came later, to ensure as much as possible that there was complete information on cohort members. Follow-up ended at the date of emigration from Denmark, at the date of death, or on Dec. 31, 2011, whichever came first. This time frame provided a maximum follow-up period of 42 years and a maximum age of 62 for the women in the cohort.
Data Sources
Data on the women in our cohort were collected through the linkage of four Danish population registers, described below. Every individual in Denmark has a unique identification number registered through the Danish Civil Registration System (CRS) (17) that is used in every Danish national register. This personal identifier allows for accurate linkage of information between and within the registers used in this study.
The CRS was established in 1968 and contains information on CRS number, gender, date of birth, updated vital status, data on all legal children, and CRS numbers of parents. We used the CRS registry in the present study to identify members of the cohort.
The Danish Psychiatric Central Register (18) was computerized in 1969 and contains data on all admissions to Danish psychiatric inpatient facilities. Data covering outpatient contacts were added to the register in 1995. For the present study, the Danish Psychiatric Central Register provided information on all psychiatric inpatient and outpatient history for all cohort members as well as for their parents, thereby offering additional information on psychiatric family history. For the evaluation of psychiatric treatments in relation to childbirth, we observed women who gave birth on Jan. 1, 1970, or later to ensure as complete follow-up information as possible. As there are no private psychiatric inpatient facilities in Denmark, all admissions are represented in this register.
ICD-8 was the diagnostic system used in Denmark until Dec. 31, 1993 (19), and on Jan. 1, 1994, ICD-10 was introduced (20). We identified all diagnostic codes included in the chapter on mental and behavioral disorders in ICD-10 and the corresponding diagnostic codes in ICD-8 (21).
To characterize the variation of specific diagnoses in the postpartum period, the frequency of the following diagnostic groups was calculated: mental and behavioral disorders associated with the puerperium (ICD-10: F53.1, F53.9; ICD-8: 294.49); neurotic, stress-related, and somatoform disorders (ICD-10: F40.9, F43.02, F43.2, F43.22, F43.9; ICD-8: 300.09, 300.19, 307.99); mood (affective) disorders (ICD-10: F31.2, F32.1, F32.9; ICD-8: 296.29, 296.99, 298.09, 298.19, 300.49); schizophrenia, schizotypal, and delusional disorders (ICD-10: F23.01; ICD-8: 298.29, 298.39, 298.89, 298.99, 299.05, 299.09, 301.83); and remaining diagnoses (ICD-10: F06.0, F10.0, F10.2, F11.2, F13.24, F99.9; ICD-8: 301.80, 301.81, 304.09, 304.49, 304.99, 310.99, 793.09, Y119).
The Danish Register of Causes of Death (22) was computerized in 1970 and provides data on all causes of death for Danish citizens who die in Denmark. This register contained the data necessary to differentiate between natural and unnatural causes of death as well as information on the specific cause of death. Natural causes of death were defined as death from diseases and medical conditions. Specific subgroups of natural causes of death were defined as malignant neoplasm (ICD-10: C00–D09; ICD-8: 140–209), cardiovascular disease (ICD-10: I00–I25, I27, I30–I52; ICD-8: 390–429), and other natural causes of death (ICD-10: A15–A19, B90, A00–A09, A20–A99, B00–B89, B91–B99, F03.9, I60–I72, R54, J00–J99, K00–K93, N00–N99, Q00–Q99, P00–P96; ICD-8:000–019, 020–136, 430–438, 794, 290–315, 440–448, 460–577, 580–629, 740–779). Unnatural causes of death were suicides, homicides, and accidents (ICD-10: V01–Y98; ICD-8: E9500–9590, E9600–9790, E8100–8239, E8000–8079, E8250–9499). Information on natural and unnatural causes of death was missing in 713 of the 33,395 deaths in the cohort, but the information was available for all cases of fatality among women with post-partum psychiatric disorders. To calculate mortality rate ratios (MRRs) for suicide, we used the ICD-10 codes X60–X84 and the ICD-8 codes E950–E959. Note that these specific diagnostic codes in ICD-10 are named “intentional self-harm” and were defined as suicides for the present study. Accidental deaths were defined by the ICD-10 codes V01–X59, Y10–Y86, Y87.2, and Y88–Y89 and the ICD-8 codes E810–823, E800–807, and E825–949.
The Danish National Patient Register (23) contains information on medical inpatient contacts for all hospitals in Denmark from 1977 onward. Outpatient data were added to the register after 1995. This register offered the information necessary to calculate a Charlson comorbidity index for each of the women in the cohort. The Charlson index, an indicator of disease burden, consists of 19 severe chronic diseases, each assigned a weight from 1 to 6 corresponding to the severity of the disease. The score is then calculated by the sum of the weights (24).
To assess the interaction of comorbid alcohol and substance abuse among the women in the cohort, we combined information from the Danish National Patient Register (23) and the Danish Psychiatric Central Register (18) using the following codes: alcohol: ICD-8: 291, 303, 570, 57100, 57110, 57300, 57301, 57710, 979, 980; ICD-10: F10, T510, Z721, R780, K70, K711, K712, K86; substance abuse: ICD-8: 304, 2944; ICD-10: F11, F12, F13, F14, F15, F16, F18, F19.
Definition of Exposure Categories
To draw comparisons between women with postpartum psychiatric disorders, women with onset of psychiatric disorders unrelated to the postpartum period, and healthy women without a psychiatric history, we divided the study population into five categories. The women were categorized into a time-dependent variable depending on their mental health status and parity (no children, or one or more children) throughout the follow-up period.
Postpartum-onset mothers: women with postpartum psychiatric disorders, defined as first inpatient or outpatient psychiatric contact within the first 90 postpartum days.
Non-postpartum-onset mothers: women with psychiatric disorders with children, defined as first inpatient or outpatient psychiatric contact outside the postpartum period.
Non-postpartum-onset nonmothers: childless women with psychiatric disorders, defined as first inpatient or outpatient psychiatric contact and no record of childbirth.
Mothers with no psychiatric history: women with no registered history of psychiatric treatment and with a record of childbirth.
Nonmothers with no psychiatric history: women with no registered history of psychiatric treatment and no record of childbirth.
By defining group 1 (postpartum-onset mothers) within the short interval of 3 months after giving birth, we assumed that childbirth was the specific triggering factor causing the psychiatric episodes in the women affected.
Note that a woman could contribute person-time at risk in different exposure categories over time, depending on when and if she had her first psychiatric diagnosis in relation to a potential childbirth. Furthermore, the exposure categories of mothers with no psychiatric history and nonmothers with no psychiatric history (groups 4 and 5) were defined by the absence of a psychiatric diagnosis from inpatient or outpatient treatment at a psychiatric facility. In addition, women were at risk of first-onset postpartum psychiatric disorders after every potential childbirth, and we analyzed up to six childbirths for every woman included in the cohort.
Statistical Analysis
We conducted survival analyses with MRRs as the main outcome measure, using Cox regression in Stata, version 12 (StataCorp, College Station, Tex.), with age as the underlying time. Estimates were considered statistically significant if the corresponding 95% CIs did not overlap 1.00.
All analyses were adjusted for calendar time as a time-dependent variable. Calendar time was categorized in 5-year groups from 1970 to 1990 and in 2-year groups from 1990 to 2011.
We adjusted for the time-dependent variables of family history of mental illness and maternal medical comorbidity. Family history of mental illness was defined as any psychiatric inpatient or outpatient contact for either of a woman's parents. Medical comorbidity was defined as the presence of a Charlson score ≥1.
Cumulative survival curves were calculated as Aalen-Johansen curves.
RESULTS
From Jan. 1, 1970, to Dec. 31, 2011, a total of 1,545,857 women ages 15 and older were included in the study cohort, contributing 68,473,423 person-years at risk. The mean follow-up time for the women in the cohort was 26.26 years, and during the follow-up period, 33,395 women in our cohort died.
Of the 1,545,857 cohort members, 2,699 (0.17%) women had a first psychiatric contact recorded at an inpatient or outpatient treatment facility within 3 months after giving birth. Of these, a total of 96 women (3.56%) died during the follow-up period (Table 1).
TABLE 1.
Vital Status and Total Contributed Person-Years at Risk at End of Follow-Upa
| Exposure Categories | Deceased (N) | Person-Years at Risk |
|---|---|---|
| Postpartum-onset mothers | 96 | 33,891 |
| Non-postpartum-onset mothers | 5,475 | 2,324,419 |
| Non-postpartum-onset nonmothers | 3,531 | 929,621 |
| Mothers with no psychiatric history | 15,244 | 37,881,122 |
| Nonmothers with no psychiatric history | 9,049 | 27,304,371 |
| Charlson comorbidity index | ||
| Charlson score of 0b | 11,423 | 64,389,832 |
| Charlson score ≥1c | 21,972 | 4,083,593 |
| Family history of mental illness | ||
| Negative family historyd | 29,070 | 61,056,776 |
| Positive family historye | 4,325 | 7,416,649 |
| Alcohol or substance abuse | ||
| Negative historyf | 26,379 | 67,254,815 |
| Positive historyg | 7,016 | 1,218,610 |
Full definitions of categories are provided in text.
Women without medical comorbidities as defined by the absence of a Charlson comorbidity index.
Women with medical comorbidities as defined by the presence of a minimum score of 1 on the Charlson comorbidity index.
Women with a mother and father without inpatient or outpatient contact with a psychiatric facility.
Women with a mother and/or father with at least one inpatient or outpatient contact with a psychiatric facility.
Women without a diagnosis of alcohol or substance abuse.
Women with at least one diagnosis of alcohol or substance abuse, or with a diagnosis of somatic complications caused by alcohol or substance abuse.
All-Cause Mortality Rates
The fully adjusted all-cause MRR for women with post-partum psychiatric disorders was 3.74 (95% CI=3.06–4.57) (Table 2), compared with mothers with no psychiatric history. Additional MRRs were calculated to highlight further differences in mortality when compared with other groups (non-postpartum-onset mothers, non-postpartum-onset nonmothers, and nonmothers with no psychiatric history) and were placed in context of three models adjusted for calendar time, family history of mental illness, and medical comorbidity as measured by the Charlson comorbidity index. Mothers with onset of psychiatric disorders unrelated to the postpartum period had an MRR similar to those in women with postpartum psychiatric disorders (Table 2). In comparison, across all presented models, childless women with psychiatric diagnoses had the highest MRR (6.15, 95% CI=5.94–6.38) (Table 2), and mothers with no record of psychiatric disorders (reference group) had the lowest MRR.
TABLE 2.
Mortality Rate Ratios (MRRs) for Women With Postpartum Psychiatric Disorders and for Four Comparison Groupsa
| Model 1b |
Model 2c |
Model 3d |
||||
|---|---|---|---|---|---|---|
| Case Categories | MRR | 95% CI | MRR | 95% CI | MRR | 95% CI |
| Postpartum-onset mothers | 3.94 | 3.22–4.81 | 3.93 | 3.21–4.80 | 3.74 | 3.06–4.57 |
| Non-postpartum-onset mothers | 4.43 | 4.33–4.53 | 4.42 | 4.32–4.52 | 2.73 | 2.67–2.79 |
| Non-postpartum-onset nonmothers | 9.66 | 9.32–10.01 | 9.62 | 9.29–9.97 | 6.15 | 5.94–6.38 |
| Mothers with no psychiatric history | 1.00 | Reference | 1.00 | Reference | 1.00 | Reference |
| Nonmothers with no psychiatric history | 1.84 | 1.79–1.90 | 1.84 | 1.79–1.89 | 1.76 | 1.71–1.81 |
Full definitions of categories are provided in text.
Adjusted for calendar time.
Adjusted for calendar time and family history of mental illness.
Adjusted for calendar time, family history of mental illness, and medical comorbidity (Charlson comorbidity index).
When assessing the interaction of comorbid alcohol or substance abuse, we found that receiving these comorbid diagnoses increased the MRRs of all-cause mortality significantly in all five exposure categories (postpartum-onset mothers, non-postpartum-onset mothers, non-postpartum-onset nonmothers, mothers with no psychiatric history, and nonmothers with no psychiatric history) (Table 3).
TABLE 3.
Interaction of Alcohol or Substance Abuse on All-Cause Mortality in Women With Postpartum Psychiatric Disorders and in Four Comparison Groupsa
| Alcohol or Substance Abuseb |
No Alcohol or Substance Abusec |
|||
|---|---|---|---|---|
| Exposure Categories | MRR | 95% CI | MRR | 95% CI |
| Postpartum-onset mothers | 5.72 | 4.31–7.59 | 3.03 | 2.38–4.02 |
| Non-postpartum-onset mothers | 5.24 | 5.10–5.39 | 1.74 | 1.68–1.80 |
| Non-postpartum-onset nonmothers | 9.94 | 9.48–10.43 | 4.85 | 4.61–5.09 |
| Mothers with no psychiatric history | 4.43 | 4.25–4.62 | 1.00 | Reference |
| Nonmothers with no psychiatric history | 6.99 | 6.43–7.60 | 1.71 | 1.69–1.77 |
MRR=mortality rate ratio. Full definitions of categories are provided in text.
Women with at least one diagnosis of alcohol or substance abuse, or with a diagnosis of somatic complications caused by alcohol or substance abuse. Results adjusted for calendar time, family history of mental illness, and somatic comorbidity (Charlson comorbidity index).
Women without a diagnosis of alcohol or substance abuse, or without a diagnosis of somatic complications caused by alcohol or substance abuse. Results adjusted for calendar time, family history of mental illness, and somatic comorbidity (Charlson comorbidity index).
Natural and Unnatural Causes of Death
The 96 fatalities among the women with severe postpartum psychiatric disorders were categorized by cause of death and diagnostic group (Table 4).
TABLE 4.
Natural and Unnatural Causes of Death in Diagnostic Groups of Women With Postpartum Psychiatric Disorders
| Natural Causes of Death |
Unnatural Causes of Death |
||||
|---|---|---|---|---|---|
| Diagnostic Groups | N | % | N | % | Total |
| Mental and behavioral disorders associated with the puerperiuma | 7 | 12.3 | 9 | 23.1 | 16 |
| Neurotic, stress-related, and somatoform disordersb | 10 | 17.5 | 6 | 15.4 | 16 |
| Mood (affective) disordersc | 14 | 24.6 | 7 | 17.9 | 21 |
| Schizophrenia, schizotypal, and delusional disordersd | 13 | 22.8 | 10 | 25.6 | 23 |
| Other disorderse | 13 | 22.8 | 7 | 17.9 | 20 |
| Total | 57f | 100.0 | 39g | 100.0 | 96 |
ICD-10: F53.1, F53.9; ICD-8: 294.49.
ICD-10: F40.9, F43.02, F43.2, F43.22, F43.9; ICD-8: 300.09, 300.19, 307.99.
ICD-10: F31.2, F32.1, F32.9; ICD-8: 296.29, 296.99, 298.09, 298.19, 300.49.
ICD-10: F23.01; ICD-8: 298.29, 298.39, 298.89, 298.99, 299.05, 299.09, 301.83.
ICD-10: F06.0, F10.0, F10.2, F11.2, F13.24, F99.9; ICD-8: 301.80, 301.81, 304.09, 304.49, 304.99, 310.99, 793.09, Y119.
Proportion of all deaths: 57/96=59.4%.
Proportion of all deaths: 39/96=40.6%.
Overall, 57 (59.4%) women with post-partum psychiatric disorders died from natural causes. When classified into more specific subgroups, we found that malignant neoplasms (18 cases, 31.6%) and cardiovascular disease (eight cases, 14.0%) accounted for the largest proportion of natural deaths among women with postpartum psychiatric disorders (results not shown).
Thirty-nine (40.6%) of the women with postpartum psychiatric disorders died from unnatural causes, including suicides and accidents. No homicides were reported for this group. In comparison, only 9.34% of mothers with no history of psychiatric disorders died from unnatural causes (results not shown). Note that these proportions are unadjusted and do not take into account possible between-group differences in age distribution.
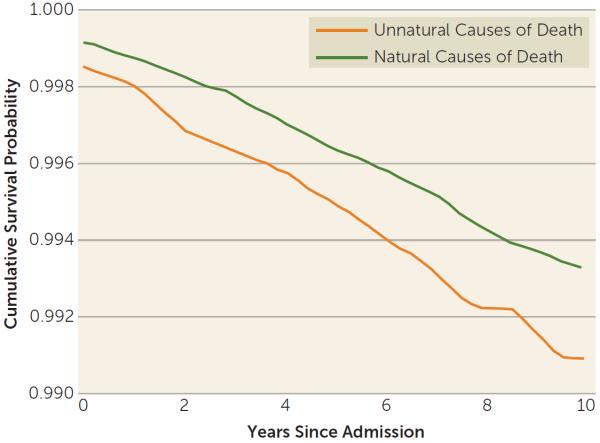
Cumulative survival curves showed that approximately 1% of the women with post-partum psychiatric disorders died of unnatural causes and that 0.75% died of natural causes within the first 10 years after onset (Figure 1).
FIGURE 1.
Smoothed Cumulative Survival Curves for Women With Postpartum Psychiatric Disorders During the First 10 Years After Onset
Suicide Rates
Table 5 lists short- and long-term suicide risk and combined risk of suicides and accidents in women with postpartum psychiatric disorders compared with the other groups of women in our study population. There were 29 cases (30.21%) of suicide among the deceased women with postpartum psychiatric disorders in the cohort. Eight women committed suicide within 1 year after diagnosis, equivalent to a short-term suicide risk of 289.42 (95% CI=144.02–581.62) compared with mothers with no psychiatric history. This suicide risk was similar to the short-term risk found in childless women with psychiatric diagnosis (MRR=228.91; 95% CI=192.37–272.40) and was significantly higher than the short-term risk found in mothers with psychiatric disorders unrelated to the post-partum period (MRR=120.62; 95% CI=105.24–138.26).
TABLE 5.
Short- and Long-Term Mortality Rate Ratios (MRRs) of Suicides (Model 1) and of Combined Suicides and Accidents (Model 2) in Women With Postpartum Psychiatric Disorders and in Four Comparison Groups
| Model 1 (suicides)a |
Model 2 (suicides and accidents)b |
|||||
|---|---|---|---|---|---|---|
| Exposure Categories | N | MRR | 95% CI | N | MRR | 95% CI |
| Short-term risk: ≤ 1 year after diagnosis of postpartum psychiatric disorderc | 8 | 289.42 | 144.02–581.62 | – d | 83.60 | 43.42–160.97 |
| Long-term risk: > 1 year after diagnosis of postpartum psychiatric disordere | 21 | 39.97 | 25.90–61.70 | 30 | 15.88 | 11.08–22.77 |
| Short-term risk: ≤ 1 year after diagnosis in non-postpartum-onset mothersf | 152 | 120.62 | 105.24–138.26 | 196 | 41.15 | 36.91–45.87 |
| Long-term risk: > 1 year after diagnosis in non-postpartum-onset mothersg | 651 | 29.14 | 26.52–32.02 | 1,305 | 15.78 | 14.89–16.73 |
| Short-term risk: ≤ 1 year after diagnosis in non-postpartum-onset nonmothersh | 175 | 228.91 | 192.37–272.40 | 222 | 60.13 | 52.08–69.42 |
| Long-term risk: > 1 year after diagnosis in non-postpartum-onset nonmothersi | 639 | 69.27 | 62.11–77.25 | 1,087 | 29.56 | 27.45–31.85 |
| Mothers with no psychiatric history | 390 | 1.00 | Reference | 1,272 | 1.00 | Reference |
| Nonmothers with no psychiatric history | 483 | 1.90 | 1.67–2.17 | 2,192 | 1.99 | 1.85–2.14 |
Adjusted for calendar time, family history of mental illness, and medical comorbidity (Charlson comorbidity index). Suicides defined by the following diagnostic codes: ICD-10: X60–X84; ICD-8: E950–E959.
Adjusted for calendar time, family history of mental illness, and medical comorbidity (Charlson comorbidity index). Suicides and accidents defined by the following diagnostic codes: ICD-10: X60–X84; V01–X59, Y10–Y86, Y87.2, Y88–Y89; ICD-8: E950–E959; 810–823, 800–807, 825–949.
The first 12 months after any first contact with a psychiatric inpatient or outpatient facility within the first 90 postpartum days.
To adhere to Danish data regulations and to protect anonymity of individuals, the exact number of cases cannot be provided in this category.
The remaining follow-up time for women with any first contact with a psychiatric inpatient or outpatient facility within the first 90 postpartum days.
The first 12 months after any first contact with a psychiatric inpatient or outpatient facility unrelated to the postpartum period, and a record of childbirth.
The remaining follow-up time for women with any first contact with a psychiatric inpatient or outpatient facility unrelated to the postpartum period, and a record of childbirth.
The first 12 months after any first contact with a psychiatric inpatient or outpatient facility, and no record of childbirth.
The remaining follow-up time for women with any first contact with a psychiatric inpatient or outpatient facility, and no record of childbirth.
Subsequently, the long-term MRR of suicide in women with postpartum psychiatric disorders decreased to 39.97 (95% CI=25.90–61.70) during the remaining follow-up period, and it was comparable to the risk seen in mothers with psychiatric disorders unrelated to childbirth (MRR=29.14; 95% CI=26.52–32.02).
In terms of suicide and accidental death combined, women with postpartum psychiatric disorders had a short-term risk of 83.60 (95% CI=43.42–160.97) within the first year after diagnosis; their long-term risk was reduced to 15.88 (95% CI=11.08–22.77). In comparison, childless women with psychiatric disorders had the highest long-term risk of suicide and accidental death (MRR=29.56; 95% CI=27.45–31.85).
DISCUSSION
Women with first-onset episodes of severe postpartum psychiatric disorders had higher all-cause mortality rates compared with mothers with no psychiatric history, but they had mortality rates similar to those of mothers experiencing psychiatric disorder onset outside the postpartum period. Importantly, the suicide risk was particularly high shortly after childbirth in women with postpartum psychiatric disorders.
All-Cause Mortality
Women with postpartum psychiatric disorders had MRRs that were approximately four times higher than mothers with no previous psychiatric history. In comparison, mothers with onset of psychiatric disorders unrelated to the postpartum period had MRRs that were similar to those of women with postpartum onset. The present study confirmed that contact with a psychiatric facility is associated with higher all-cause mortality, but interestingly, the timing of onset was not relevant for long-term survival.
Severe psychiatric disorders have been shown to be associated with an increased risk of medical comorbidity (25, 26), and previous studies have indicated that psychiatric patients may be underdiagnosed and undertreated for medical conditions (27, 28). The same might also be true for women in the present study, and therefore we adjusted for medical comorbidities defined as a time-dependent variable in the analyses (Charlson score).
A previous study found that comorbid substance abuse may be predictive of an increased suicide risk among women with postpartum psychiatric disorders (10). The present study showed that a comorbid diagnosis of alcohol or substance abuse was associated with higher all-cause mortality, including suicide, in women with postpartum psychiatric disorders as well as increased mortality in all four comparison groups.
Unnatural Causes of Death and Suicide Risk
In this study, unnatural causes, including suicide and accidents, accounted for 40.6% of all deaths among women with severe postpartum psychiatric disorders. We confirmed a very high suicide risk in women with postpartum psychiatric disorders, as previously described by Appleby et al. (14). Notably, the Appleby et al. study did not include comparisons with other groups of mothers and nonmothers, with and without psychiatric disorders. Our categorization of the five exposure categories (postpartum onset, nonpostpartum mothers, nonpostpartum nonmothers, mothers with no psychiatric history, and nonmothers with no psychiatric history) strengthens the present study by teasing apart the impact of postpartum-onset disorders from motherhood on overall mortality and on completed suicides. Furthermore, we included information on outpatient contacts and had a twofold longer follow-up period of up to 42 years. In the present study, the first year after diagnosis represented a time of very high relative suicide risk for the group of women with severe postpartum psychiatric disorders; there were eight cases of suicide within the first year after diagnosis (MRR=289.42; 95% CI=144.02–581.62).
Mortality Rates in Mothers Compared With Childless Women
Motherhood had a positive effect on mortality rates, both for women with and without psychiatric disorders (Table 2). This favorable relationship between parity and mortality in women has been shown in earlier studies, where childless women have been found to have a fourfold higher rate of death compared with women who gave birth (29).
A possible explanation for the lower mortality rates in mothers might be a so-called healthy-pregnant-woman effect. It has been suggested that women with children are healthier and may have higher fertility (30), thereby creating a selection effect among women, as mothers in general represent a healthier section of the overall population of women. Note that although we found that childless women had higher MRRs regardless of mental health status, childless women with a psychiatric diagnosis had the highest MRRs of all comparable groups. We speculate that a corresponding “healthy-pregnant-woman effect” exists in psychiatric patients, where those women who become mothers represent a healthier part of the patient population.
Individuals with severe mental disorders are less likely to have children than their healthy counterparts (31). Thus, the group of childless women with psychiatric diagnoses in our cohort likely comprises the most severely mentally ill patients, who also represent the group with the worst overall prognosis (32, 33).
Another possible explanation for lower mortality rates in mothers may be related to the responsibility they feel as a parent. In some cases, mothers describe that they feel life is not worth living but that their suicidal thoughts are mitigated by the thought of their child or children growing up without a mother. The responsibility they feel as a parent prevents them from taking their life and acting on suicidal ideation.
Methodological Considerations
Equal and free access to both medical and mental health care in Denmark ensured a broad diversity in our study population. We defined our cases from contacts at psychiatric facilities; consequently, we identified as cases only those women who sought help. Some women categorized as women in the nondiseased background population (mothers with no psychiatric history and nonmothers with no psychiatric history) in this study might have undergone treatment for mild to moderate psychiatric symptoms at their general practitioner without receiving a diagnosis in the Danish Psychiatric Central Register and therefore would not be captured in the data.
When evaluating suicides, it is possible that a woman might develop a postpartum psychiatric disorder and commit suicide before a psychiatric diagnosis can be given. In that case, the woman would be classified as a mother with no psychiatric history in the present study. A total of 16 women committed suicide within 12 months after childbirth without having a psychiatric contact, and a subsequent misclassification of case status cannot be ruled out in these individuals, as it is likely that a psychiatric diagnosis was missed in some or all of these women.
We defined onset of mental disorders as the admission date of the first psychiatric contact leading to a recorded diagnosis, bearing in mind that this date does not necessarily correspond with symptom onset. It is possible that some women with postpartum psychiatric disorders in this study experienced depressive symptoms during pregnancy and that these symptoms were then exacerbated by childbirth, leading to psychiatric admission. However, these women would still be categorized as nondiseased (mothers with no psychiatric history or nonmothers with no psychiatric history) until after their first contact with a psychiatric facility in the postpartum period.
We adjusted for possible confounders (calendar period, family history of mental illness, and medical comorbidity), but we cannot rule out potential residual confounding.
We had access to inpatient treatment contacts from 1969 and to outpatient contacts with psychiatric facilities from 1995 onward. These patients represent the most severe cases of postpartum psychiatric disorders. Consequently, generalizability to less severe psychiatric postpartum episodes treated solely in primary care is questionable.
The study of suicide inherently contains the risk of possible misclassification of cause of death. While most deaths classified as suicides are likely to be actual suicides, some accidents might be misreported and in reality be suicides. Therefore, we also included a combined estimate of MRRs for suicides and registered accidents as cause of death (Table 5).
Clinical Recommendations
The observed high relative risk of suicide in the postpartum period warrants special attention for this vulnerable group of women. We propose the following recommendations for diagnosis and treatment of mood episodes specifically occurring in the postpartum period. First, fluctuations in mood with accompanying anxiety symptoms are common following childbirth (7), and consequently assessment of mood at several postpartum time points is preferable to diagnose women correctly. Second, anxiety and activation will commonly occur in women with postpartum mood symptoms, and women with increased anxiety are at a higher risk of self-harm because of the uncomfortable agitation they experience. Third, in women with more severe postpartum psychiatric disorders, psychotic symptoms are highly prevalent (3, 34), but these symptoms can easily be overlooked because they either fluctuate or are well hidden, especially in patients with depression. If psychotic symptoms are present, patients require a much higher level of care, and often, inpatient psychiatric hospitalization is warranted for safety and intensive treatment. Fourth, the treatment of postpartum depression should also include an assessment of maternal-infant bonding. Mothers with depression often have dys-functional thoughts, such as, “I am a bad mother,” “My baby doesn't like me,” and “He or she is better off without me.” These thoughts can progress to suicidal thoughts. Fifth, severe postpartum depression should be treated with medication, but suicidality might increase transiently during the first few weeks of treatment with antidepressant medication, so extra vigilance is warranted. Lastly, the partner, family, and social environment are usually not prepared to consider the possibility of suicidal thoughts or suicidal behavior in the mother, because of the common belief that the postpartum period is associated with positive life experiences and joy. Increased education and awareness among the general public about perinatal mental health issues are needed. Screening programs of new mothers can increase awareness by providing important psychoeducation to mothers and by alerting health care providers of women who are experiencing suicidal thoughts (35).
Acknowledgments
Supported by the Lundbeck Foundation Initiative for Integrative Psychiatric Research, MEPRICA (Mental Health in Primary Care), and NIMH grant R01MH104468 to Dr. Meltzer-Brody and to Dr. Munk-Olsen. Dr. Laursen is supported by an unrestricted grant (R155-2012-11280) from the Lundbeck Foundation. Dr. Meltzer-Brody is supported by NIH grant 1R01MH104468-01.
Dr. Meltzer-Brody has received funding from the Foundation of Hope and Sage Therapeutics.
Footnotes
Presented in part at the International Marcé Society Biennial Scientific Conference, Swansea, U.K., Sept. 10–12, 2014.
The other authors report no financial relationships with commercial interests.
REFERENCES
- 1.Wisner KL, Sit DK, McShea MC, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70:490–498. doi: 10.1001/jamapsychiatry.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.O'Hara MW, Wisner KL. Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol. 2014;28:3–12. doi: 10.1016/j.bpobgyn.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Munk-Olsen T, Laursen TM, Pedersen CB, et al. New parents and mental disorders: a population-based register study. JAMA. 2006;296:2582–2589. doi: 10.1001/jama.296.21.2582. [DOI] [PubMed] [Google Scholar]
- 4.Kendell RE, Chalmers JC, Platz C. Epidemiology of puerperal psychoses. Br J Psychiatry. 1987;150:662–673. doi: 10.1192/bjp.150.5.662. [DOI] [PubMed] [Google Scholar]
- 5.Howard LM, Molyneaux E, Dennis CL, et al. Non-psychotic mental disorders in the perinatal period. Lancet. 2014;384:1775–1788. doi: 10.1016/S0140-6736(14)61276-9. [DOI] [PubMed] [Google Scholar]
- 6.Jones I, Chandra PS, Dazzan P, et al. Bipolar disorder, affective psychosis, and schizophrenia in pregnancy and the post-partum period. Lancet. 2014;384:1789–1799. doi: 10.1016/S0140-6736(14)61278-2. [DOI] [PubMed] [Google Scholar]
- 7.Brockington I. Postpartum psychiatric disorders. Lancet. 2004;363:303–310. doi: 10.1016/S0140-6736(03)15390-1. [DOI] [PubMed] [Google Scholar]
- 8.Stein A, Pearson RM, Goodman SH, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384:1800–1819. doi: 10.1016/S0140-6736(14)61277-0. [DOI] [PubMed] [Google Scholar]
- 9.Spinelli MG. Maternal infanticide associated with mental illness: prevention and the promise of saved lives. Am J Psychiatry. 2004;161:1548–1557. doi: 10.1176/appi.ajp.161.9.1548. [DOI] [PubMed] [Google Scholar]
- 10.Comtois KA, Schiff MA, Grossman DC. Psychiatric risk factors associated with postpartum suicide attempt in Washington State, 1992–2001. Am J Obstet Gynecol. 2008;199:120.e1–120.e5. doi: 10.1016/j.ajog.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 11.Lewis G. In: Introduction and key findings, in Why Mothers Die 1997–1999: Confidential Enquiry Into Maternal and Child Health. Lewis G, editor. chap 1. RCOG Press; London: 2001. p. 22. [Google Scholar]
- 12.Lewis G. In: Introduction and key findings 2000-2002, in Why Mothers Die 2000-2002: Confidential Enquiry Into Maternal and Child Health. Lewis G, editor. chap 1. RCOG Press; London: 2004. p. 25. [Google Scholar]
- 13.Cantwell R, Clutton-Brock T, Cooper G, et al. Saving mothers' lives: reviewing maternal deaths to make motherhood safer: 2006–2008: the eighth report of the confidential enquiries into maternal deaths in the United Kingdom. BJOG. 2011;118(suppl 1):1–203. doi: 10.1111/j.1471-0528.2010.02847.x. [DOI] [PubMed] [Google Scholar]
- 14.Appleby L, Mortensen PB, Faragher EB. Suicide and other causes of mortality after post-partum psychiatric admission. Br J Psychiatry. 1998;173:209–211. doi: 10.1192/bjp.173.3.209. [DOI] [PubMed] [Google Scholar]
- 15.Nordentoft M, Wahlbeck K, Hällgren J, et al. Excess mortality, causes of death and life expectancy in 270,770 patients with recent onset of mental disorders in Denmark, Finland and Sweden. PLoS One. 2013;8:e55176. doi: 10.1371/journal.pone.0055176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13:153–160. doi: 10.1002/wps.20128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39(suppl 7):22–25. doi: 10.1177/1403494810387965. [DOI] [PubMed] [Google Scholar]
- 18.Mors O, Perto GP, Mortensen PB. The Danish Psychiatric Central Research Register. Scand J Public Health. 2011;39(suppl 7):54–57. doi: 10.1177/1403494810395825. [DOI] [PubMed] [Google Scholar]
- 19.Sundhedsstyrelsen . V. Morbi mentis: Psykiske lidelser m.v. Klassifikation af Sygdomme: Systematisk Del. 8. revision ed Sundhedsstyrelsen; 1976. [Google Scholar]
- 20.World Health Organization Chapter V: Mental and Behavioural Disorders (F00–F99) 2010 available at: http://apps.who.int/classifications/icd10/browse/2010/en#/V.
- 21.Pedersen CB, Mors O, Bertelsen A, et al. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014;71:573–581. doi: 10.1001/jamapsychiatry.2014.16. [DOI] [PubMed] [Google Scholar]
- 22.Helweg-Larsen K. The Danish Register of Causes of Death. Scand J Public Health. 2011;39(suppl 7):26–29. doi: 10.1177/1403494811399958. [DOI] [PubMed] [Google Scholar]
- 23.Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(suppl 7):30–33. doi: 10.1177/1403494811401482. [DOI] [PubMed] [Google Scholar]
- 24.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 25.Laursen TM, Munk-Olsen T, Gasse C. Chronic somatic comorbidity and excess mortality due to natural causes in persons with schizophrenia or bipolar affective disorder. PLoS One. 2011;6:e24597. doi: 10.1371/journal.pone.0024597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Truyers C, Buntinx F, De Lepeleire J, et al. Incident somatic comorbidity after psychosis: results from a retrospective cohort study based on Flemish general practice data. BMC Fam Pract. 2011;12:132. doi: 10.1186/1471-2296-12-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laursen TM, Munk-Olsen T, Agerbo E, et al. Somatic hospital contacts, invasive cardiac procedures, and mortality from heart disease in patients with severe mental disorder. Arch Gen Psychiatry. 2009;66:713–720. doi: 10.1001/archgenpsychiatry.2009.61. [DOI] [PubMed] [Google Scholar]
- 28.Felker B, Yazel JJ, Short D. Mortality and medical comorbidity among psychiatric patients: a review. Psychiatr Serv. 1996;47:1356–1363. doi: 10.1176/ps.47.12.1356. [DOI] [PubMed] [Google Scholar]
- 29.Agerbo E, Mortensen PB, Munk-Olsen T. Childlessness, parental mortality and psychiatric illness: a natural experiment based on in vitro fertility treatment and adoption. J Epidemiol Community Health. 2013;67:374–376. doi: 10.1136/jech-2012-201387. [DOI] [PubMed] [Google Scholar]
- 30.Ronsmans C, Khlat M, Kodio B, et al. Evidence for a `healthy pregnant woman effect' in Niakhar, Senegal? Int J Epidemiol. 2001;30:467–473. doi: 10.1093/ije/30.3.467. [DOI] [PubMed] [Google Scholar]
- 31.Laursen TM, Munk-Olsen T. Reproductive patterns in psychotic patients. Schizophr Res. 2010;121:234–240. doi: 10.1016/j.schres.2010.05.018. [DOI] [PubMed] [Google Scholar]
- 32.Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry. 1998;173:11–53. doi: 10.1192/bjp.173.1.11. [DOI] [PubMed] [Google Scholar]
- 33.Laursen TM, Munk-Olsen T, Nordentoft M, et al. Increased mortality among patients admitted with major psychiatric disorders: a register-based study comparing mortality in unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia. J Clin Psychiatry. 2007;68:899–907. doi: 10.4088/jcp.v68n0612. [DOI] [PubMed] [Google Scholar]
- 34.Munk-Olsen T, Laursen TM, Meltzer-Brody S, et al. Psychiatric disorders with postpartum onset: possible early manifestations of bipolar affective disorders. Arch Gen Psychiatry. 2012;69:428–434. doi: 10.1001/archgenpsychiatry.2011.157. [DOI] [PubMed] [Google Scholar]
- 35.Chaudron LH, Wisner KL. Perinatal depression screening: let's not throw the baby out with the bath water! J Psychosom Res. 2014;76:489–491. doi: 10.1016/j.jpsychores.2014.03.011. [DOI] [PubMed] [Google Scholar]