Abstract
Sugar-sweetened beverages (SSBs) are the single largest source of added sugar and the top source of energy intake in the US diet. In this review, we evaluate whether there is sufficient scientific evidence that decreasing SSB consumption will reduce the prevalence of obesity and its related diseases. Since prospective cohort studies address dietary determinants of long-term weight gain and chronic diseases, whereas randomized controlled trials (RCTs) typically evaluate short-term effects of specific interventions on weight change, both types of evidence are critical in evaluating causality. Findings from well-powered prospective cohorts have consistently shown a significant association, established temporality, and demonstrated a direct dose-response relationship between SSB consumption and long-term weight gain and risk of type 2 diabetes (T2D). A recently published meta-analysis of RCTs commissioned by the World Health Organization (WHO) found that decreased intake of added sugars significantly reduced body weight (0.80 kg, 95% CI 0.39 to 1.21; P<0.001), whereas increased sugar intake led to a comparable weight increase (0.75 kg, 0.30 to 1.19; P=0.001). A parallel meta-analysis of cohort studies also found that higher intake of SSBs among children was associated with 55% (95% CI 32%-82%) higher risk of being overweight or obese compared to those with lower intake. Another meta-analysis of eight prospective cohort studies found that 1–2 servings/day of SSB intake was associated with a 26% (95% CI 12–41%) greater risk of developing T2D compared to occasional intake (< 1 serving/month). Recently, two large RCTs with a high degree of compliance provided convincing data that reducing consumption of SSBs significantly decreases weight gain and adiposity in children and adolescents. Taken together, the evidence that decreasing SSBs will decrease the risk of obesity and related diseases such as T2D is compelling. Several additional issues warrant further discussion. First, prevention of long-term weight gain through dietary changes such as limiting consumption of SSBs is more important than short-term weight loss in reducing the prevalence of obesity in the population. This is because once an individual becomes obese, it is difficult to lose weight and keep it off. Second, we should consider the totality of evidence rather than selective pieces of evidence (e.g., from short-term RCTs only). Finally, while recognizing that the evidence of harm on health against SSBs is strong, we should avoid the trap of waiting for absolute proof before allowing public health action to be taken.
Keywords: Sugar-sweetened beverages, obesity, nutrition, diabetes
Introduction
Obesity has become a global pandemic. In 2005, approximately 1.6 billion adults were overweight (BMI ≥25 kg/m2) and at least 400 million were obese (BMI ≥ 30 kg/m2). These numbers are projected to reach 2.3 billion and 700 million, respectively, by 2015 (1). The percentage of overweight and obese adults in the US increased from 47% and 15% (respectively) in the late 1970s to nearly 69% and 36% in 2009–2010 (2). The magnitude of increase among children and adolescents is of particular concern. Over the past three decades, the prevalence of childhood obesity (sex- and age-specific BMI > 95th percentile of the 1970s standard) has more than doubled, with the prevalence of obesity in children and adolescents now at 16.9% (3). Furthermore, in the US alone, health care costs attributable to obesity were estimated at $147 billion per year in 2008 (4).
In parallel with the rising obesity epidemic, the prevalence of type 2 diabetes (T2D) has increased dramatically worldwide. In the US, the prevalence of T2D has nearly doubled, increasing from 5.3% during 1976–1980 to 11.3% in 2010 (5). The International Diabetes Federation (IDF) estimated that in 2012 there were over 366 million people worldwide with T2D, and that number is projected to reach 552 million by 2030. Approximately 80% of people with T2D live in low- and middle-income countries, which has enormous public health and economic consequences (6).
Obesity is a complex condition that is caused by a myriad of factors, including but not limited to genetics, epigenetics, eating behaviors, physical activity, metabolism, psychosocial influences, and environmental factors. Mounting epidemiologic and clinical-trial evidence indicates that there is no “magic bullet” for weight control. Rather, multiple factors each exert a modest effect in the daily energy balance, which over time accumulates to cause weight gain and obesity (7). Among numerous potential dietary determinants of obesity, sugar-sweetened beverages (SSBs) have recently received a great deal of attention, because they are the largest source of calories and added sugars in both children and adults in the US (8,9) (Table 1). SSBs include the full spectrum of soft drinks, fruit drinks, and energy and vitamin water drinks containing added sugars. These beverages are sweetened by high-fructose corn syrup (HFCS, the most common added sweetener in processed foods and beverages in the US), sucrose, or fruit juice concentrates. The HFCS that is commonly used in beverages contains 55% fructose and 45% glucose, while sucrose or table sugar consists of 50% fructose and 50% glucose.
Table 1.
Mean Intake of Added Sugars & Percentage Contribution of Various Foods Among US Population, by Age, NHANES 2005–06
| All Persons |
2–18 years |
19+ years |
||
|---|---|---|---|---|
| Sample Size | 8272 | 3553 | 4719 | |
| Mean Intake of Added Sugars (tsp) | 21 | 23 | 20 | |
| Ranka | Food Group | |||
| 1 | Soda/energy/sports drinks | 35.7 | 31.8 | 37.1 |
| 2 | Grain-based desserts | 12.9 | 10.9 | 13.7 |
| 3 | Fruit drinks | 10.5 | 15.0 | 8.9 |
| 4 | Dairy desserts | 6.6 | 7.9 | 6.1 |
| 5 | Candy | 6.1 | 6.8 | 5.8 |
| 6 | Ready-to-eat cereals | 3.8 | 6.4 | 2.9 |
| 7 | Sugars/honey | 3.5 | 1.4 | 4.2 |
| 8 | Tea | 3.5 | 2.1 | 4.0 |
| 9 | Yeast breads | 2.1 | 1.9 | 2.2 |
| 10 | Syrups/toppings | 1.9 | 2.8 | 1.5 |
Rank for all persons only. Columns for other age groups are ordered by this ranking. The top five food groups for each age group are bolded.
Consumption of SSBs has increased dramatically in the past several decades among both children and adults (10). Additionally, SSBs have been clearly identified as a suitable target for public health interventions, not only because SSB consumption is strongly associated with obesity, but also because they offer only “empty” calories and provide almost no nutritional value.
SSB Consumption Trends
Data from the National Health and Nutrition Examination Survey (2005–2008) show that half the U.S. population consumes SSBs on a given day; 1 in 4 obtain at least 200 calories from such beverages; and 5% obtain at least 567 calories—equivalent to four cans of soda (11). Consumption is particularly high among African Americans, Hispanics, and low-income individuals – the groups with disproportionally high prevalence of obesity and obesity-related chronic diseases. U.S. children and youth obtain on average 224 calories per day from SSBs, nearly 11% of their daily total caloric intake (12). Consumption is higher among boys than girls; 70% of boys aged 2–19 years consume SSBs daily. In the past several decades, the portion size of soft drinks has increased substantially (13), from a 6.5-ounce standard soft drink bottle in the 1950s to a typical 20-ounce bottle today.
Consumption of SSBs in the US appears to have decreased modestly in the past decade (14). However, soft drink sales are increasing rapidly in other parts of the world, especially developing countries. For example, the sales of Coca Cola and PepsiCo products have soared in China, increasing 145% and 127% (respectively) from 2000 to 2010 (15). Soft drink consumption trends strongly resemble tobacco consumption trends, as both soft drink companies and tobacco companies have a worldwide reach that includes aggressive marketing tactics designed to export unhealthy products to developing countries. Additionally, both soft drink and tobacco companies fund biased analyses and reviews and provide misleading information to consumers in order to increase consumption of unhealthy products (16).
SSBs and Obesity: Observational Evidence
Numerous epidemiologic studies have examined the relationship between SSB intake and obesity. Among the various types of epidemiologic studies, ecological studies (e.g., cross-population comparisons and time trends) are most susceptible to confounding and other biases. Cross-sectional analyses are also susceptible to confounding and reverse causation bias. Thus, the evidence from these two types of studies was not considered in this review. On the other hand, carefully conducted and analyzed prospective cohort or longitudinal studies are considered to be the strongest non-randomized study design. Several (8,17–20) but not all (21) systematic reviews have reported positive associations between intake of SSB and weight gain or risk of overweight and obesity among both children and adults. We found that the relationship is most consistent among large prospective cohort studies with long follow-up and without statistical adjustment for total energy intake (19). Because SSBs add extra calories to the diet, total energy intake is likely to mediate the association between SSB intake and weight gain. Thus, adjusting for total energy intake is equivalent to assessing the effects of SSB intake on body weight that do not occur through a change in total energy intake; such an analysis would artificially underestimate the association between SSBs and body weight. Discrepancies between some studies may be explained by whether or not they adjusted for total energy intake. In a meta-analysis of 10 longitudinal studies and two randomized clinical trials (RCTs), Forshee et al. found no relationship between SSB intake and BMI among children and adolescents (21). However, this meta-analysis is analytically flawed by failure to appropriately scale the estimates and standard errors from two studies. In particular, the meta-analysis expressed the overall results as the change in BMI units per 12-oz serving change in SSBs. However, two studies expressed their estimates as change per 1-oz serving in SSBs in their original publications, and these were not scaled in the meta-analysis. After correcting for these errors and analyzing only the available estimates that were not adjusted for total energy intake, our updated meta-analysis found a significant positive association between SSB intake and BMI among children (19).
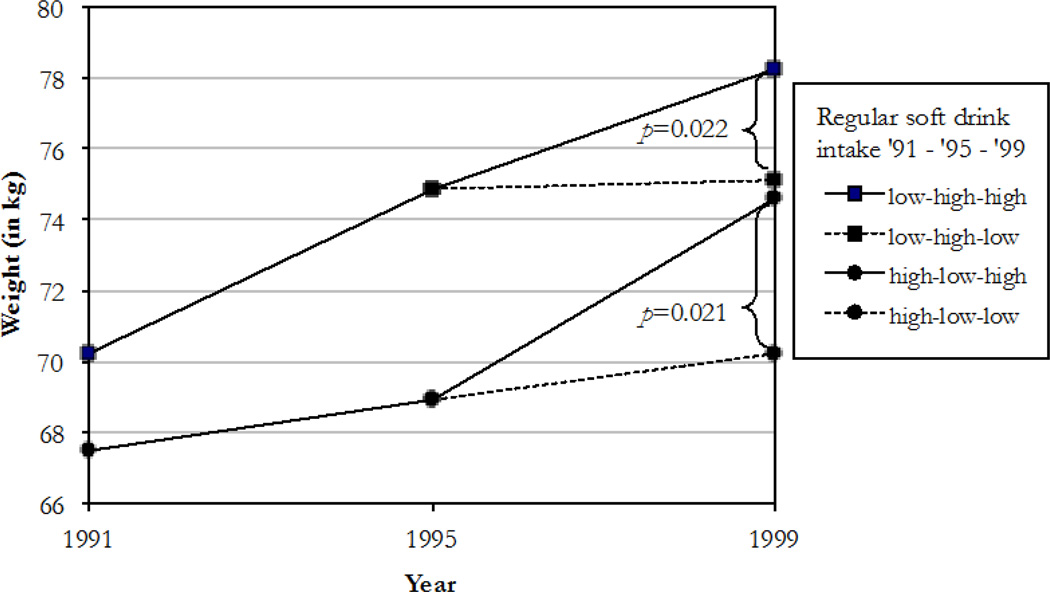
Among adults, several large prospective cohort studies have found significant positive associations between daily SSB consumption and weight gain. In a large cohort of over 50,000 female nurses, women who increased their SSB consumption and maintained a high level of intake gained on average 8.0 kg over 8 years, while women who decreased their SSB intake and maintained it gained on average only 2.8 kg (22) (Figure 1). Similar results were found among over 40,000 women in the Black Women’s Health Study (23) and in a cohort of over 43,000 Chinese adults in Singapore (24). Recently, we examined the relationships between changes in lifestyle factors and weight change among 120,877 initially non-obese women and men in our three observational cohorts (the Nurses’ Health Study, Nurses’ Health Study II, and Health Professionals’ Follow-up Study), using repeated measurements every four years. Each daily increase of one 12-oz (355 ml) serving of SSB was significantly associated with approximately 0.5 kg greater weight gain every 4 years, after adjustment for age, baseline BMI, sleep, and changes in physical activity, smoking, TV watching, and multiple other dietary factors (25). Other “obesogenic” foods identified in this study included potatoes, potato chips/French fries, red and processed meats, refined grains, and desserts. On the other hand, greater consumption of fruits, vegetables, whole grains, nuts, and yogurt was associated with less weight gain. These results suggest that obesity prevention should focus on improving overall dietary quality by consuming more healthful foods and beverages and fewer unhealthy ones. Because a large number of individuals consume multiple servings of SSBs daily, reducing consumption of these beverages is an important step in improving dietary quality and reducing long-term weight gain.
Figure 1.
Mean weight in 1991, 1995, and 1999 according to trends in sugar-sweetened soft drink consumption in 1,969 women who changed consumption between 1991 and 1995 and either changed or maintained level of consumption until 1999*
* Low and high intakes were defined as ≤1/week and ≥1/day. The number of subjects were: low-high-high=323, low-high-low=461, high-low-high=110, and high-low-low=746. Groups with similar intake in 1991 and 1995 were combined for estimates for these time points. Means were adjusted for age, alcohol intake, physical activity, smoking, postmenopausal hormone use, oral contraceptive use, cereal fiber intake, and total fat intake at each time point. From reference 21.
The repeated assessment of diet and lifestyle variables in our cohorts facilitates a “change-on-change” analysis. Although this method lacks the randomization of a clinical trial, it has many features of a quasi-experimental design. Additionally, our findings may be more generalizable to the real-world setting compared to a well-controlled laboratory setting. From a public health point of view, identifying dietary determinants of long-term weight gain is critical for reducing the prevalence of obesity in the population; once an individual becomes obese, it is difficult to lose weight and keep it off.
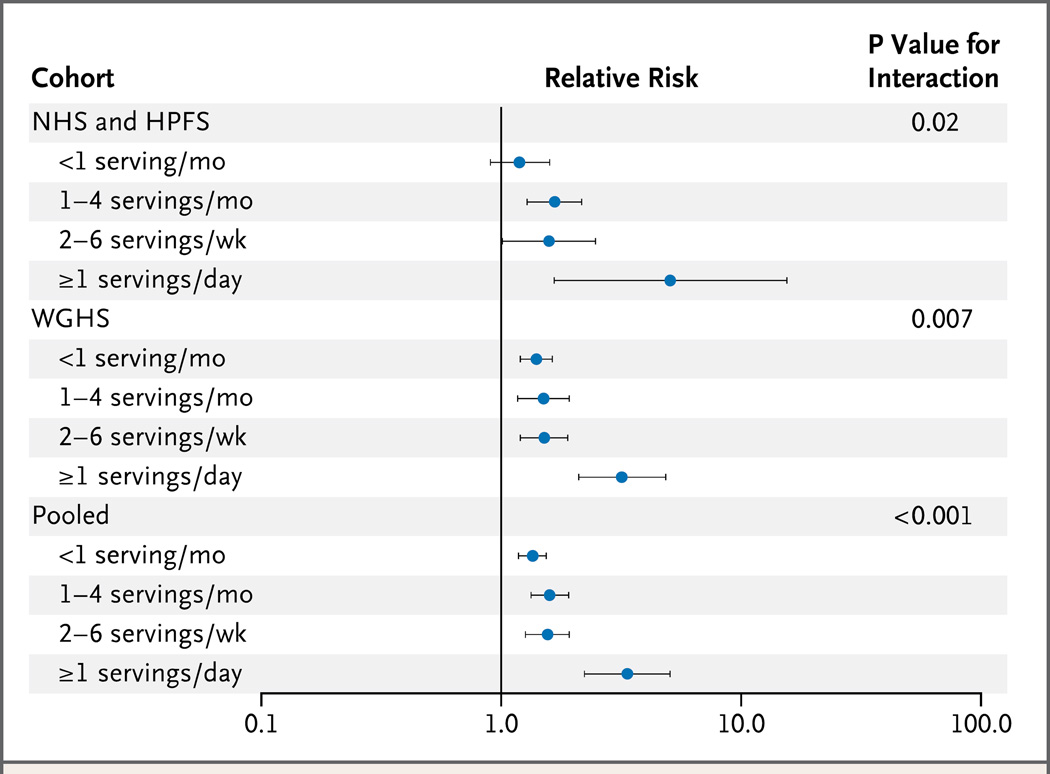
Evidence for a causal link between SSBs and obesity is strengthened by our recent analysis of gene-SSB interactions (26). We examined whether consumption of SSB can modify genetic risk of obesity, assessed using a genetic predisposition score based on 32 obesity genes identified from recent genome-wide association studies. With data from three large cohorts (Nurses’ Health Study, Health Professionals’ Follow-up Study, and Women’s Genome Health Study), we found that greater consumption of SSBs was associated with more pronounced genetic effects on elevated BMI and an increased risk of obesity. Individuals who consumed one or more servings of SSBs per day showed more than twice the genetic effect on obesity risk compared to those who consumed less than one serving per month (Figure 2). These data suggest that regular consumption of SSBs exacerbates the genetic risk of obesity, implying that a genetic predisposition to obesity can be partly offset by healthier beverage choices. Alternatively, persons with a greater genetic predisposition to obesity appear to be more susceptible to the deleterious effects of SSBs on BMI. These findings may help explain individual differences in the metabolic response to intake of SSBs.
Figure 2.
Relative Risk of the Development of Obesity per Increment of 10 Risk Alleles, According to Intake of Sugar-Sweetened Beverages
For the discovery phase, with data from the Nurses’ Health Study (NHS) and Health Professionals Follow-up Study (HPFS) cohorts, the analyses were based on 18 years of follow-up for 6402 initially nonobese women (1980 to 1998, 1107 incident cases of obesity) and 12 years of follow-up for 3889 initially nonobese men (1986 to 1998, 297 incident cases of obesity). Shown are the pooled relative risks of incident obesity, with adjustment for age, source of genotyping data, level of physical activity, status with respect to current smoking, alcohol intake, time spent watching television, Alternative Healthy Eating Index score, and total energy intake. For the replication phase, with data from the Women’s Genome Health Study (WGHS) cohort, the analyses were based on a median of 6 years of follow-up for 18,127 initially nonobese women (1992 to 1998, 2280 incident cases of obesity). Shown are the relative risks of incident obesity, with adjustment for age, geographic region, eigenvectors, level of physical activity, status with respect to current smoking, alcohol intake, and total energy intake. Horizontal bars indicate 95% confidence intervals.
From: Qi Q, Chu AY, Kang JH, Jensen MK, Curhan GC, Pasquale LR, et al. Sugar-sweetened beverages and genetic risk of obesity. The New England journal of medicine. 2012; 367: 1387–96.
SSBs and Body Weight: Clinical Trial Evidence
Evidence from RCTs is limited compared to the observational evidence. In 2011, Mattes et al. (27) conducted a meta-analysis of six RCTs and found that adding SSBs to participants’ diets significantly increased body weight in a dose-dependent manner. However, in a meta-analysis of another six RCTs aimed to reduce SSB consumption, there was no overall effect on BMI, but a significant benefit was seen among individuals who were initially overweight. Mattes et al. (27) pointed out the methodological limitations of these trials, including small sample sizes, short duration, poor compliance, lack of randomization at the individual level, lack of blinding, and the overstating of subgroup findings.
It should be noted that all these trials are “effectiveness trials” of behavioral modifications; such trials test intervention modalities more than causal relationships, because their findings are greatly affected by intervention intensity and are limited by adherence (28). One of the trials compared soda consumption isocalorically with sweetened milk, which not surprisingly revealed no difference in weight change between the intervention and control groups (29). This trial should, therefore, not be included in the meta-analysis. In addition, the school-based intervention by Sichieri et al. (30) was problematic in that the intervention group, which received health education to discourage consumption of carbonated SSBs, compensated by increasing their consumption of sugar-added juices and fruit drinks, which may explain the lack of significant findings.
In a cluster-randomized controlled trial testing a school-based soda reduction program, a significant reduction in childhood overweight and obesity rates was observed at the end of the 1-year intervention (31), but it became non-significant 2 years after the educational program’s discontinuation (32). This finding actually supports rather than refutes a benefit of reducing SSB consumption on childhood obesity. The 1-year rather than 2-year results reflect the more relevant effects of an active intervention program.
Recently, two large and rigorously conducted RCTs have been published. These two groundbreaking trials, which overcame many of the limitations of previous trials, provide strong evidence that decreasing consumption of SSBs significantly reduces weight gain and obesity in children and adolescents. Ebbeling et al. (33) randomly assigned 224 overweight and obese adolescents who regularly consumed SSBs to intervention and control groups. The intervention group received home delivery of water or diet drinks to replace SSBs for one year, at which point these participants had significant and beneficial changes in BMI (-0.57 kg/m2, P=0.045) and weight (-1.9 kg, P=0.04) compared to the control group. After one additional year of follow-up without active intervention, the intervention group still had less weight gain than the control group, although the between-group difference was not statistically significant. The intervention effects were significantly more pronounced among Hispanic than non-Hispanic participants. A major strength of this trial is the high retention rates (97% at 1 year and 93% at 2 years). The intervention was also very effective: reported intake of SSB decreased from 1.7 servings per day to nearly 0 in the intervention group at 1 year. Interestingly, the consumption in the control group also declined substantially, which might have led to underestimation of the true magnitude of the intervention effect. As was expected, the consumption of SSBs in both groups rebounded somewhat after the intervention ceased, suggesting that to achieve long-term benefits, the intervention needs to be sustained over time.
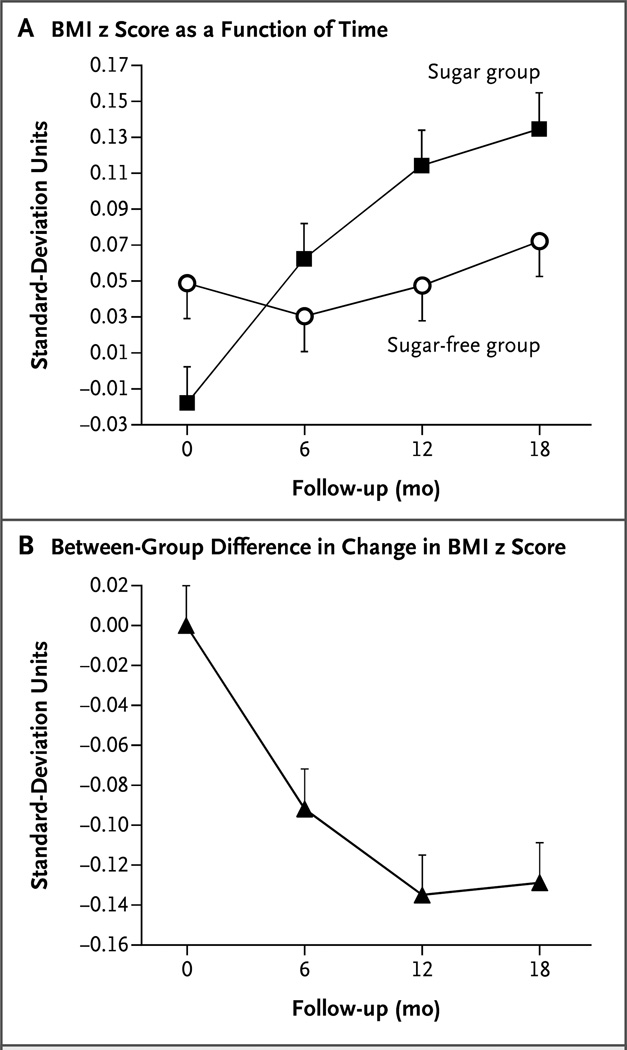
In a double-blinded placebo-controlled trial, de Ruyter et al. (34) randomized 641 normal-weight Dutch children to receive 250 ml (8 oz) per day of a sugar-free, artificially sweetened beverage (sugar-free group) or a similar sugar-containing beverage that provided 104 kcal per serving (sugar group). After 18 months of the intervention, compared to the sugar group, the sugar-free group had significant reductions in BMI z score (Figure 3), weight gain, and body fat change. A major advantage of this study is the double-blind design, which avoids potential biases due to psychological cues and social desirability. In addition, an objective biomarker (urinary sucralose) indicated a high degree of compliance. One limitation is that 26% of the participants did not complete the study, which may have led to underestimation of the true effects of the intervention. The results from this study, together with the findings from Ebbeling et al. (33), provide the strongest evidence to date that replacing SSBs with noncaloric beverages will significantly reduce childhood obesity.
Figure 3.
Body-Mass Index (BMI) z Score in the 477 Children Who Drank the Study Beverages for the Full 18 Months. The z score for BMI is the BMI expressed as the number of standard deviations by which a child differed from the mean in the Netherlands for his or her age and sex. Panel A shows mean z scores for the two study groups over the 18-month study period. Panel B shows the between-group difference in the mean change from baseline (the mean change in the BMI z score in the sugar-free group minus the mean change in the sugar group), as a function of time. T bars in both panels indicate standard errors.
From: de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. The New England Journal of Medicine. 2012; 367: 1397–406.
Meta-analyses of Added Sugar Consumption and Body Weight
Recently, the World Health Organization (WHO) commissioned a systematic review and meta-analysis to address the effects of added sugars on body weight and to determine whether the existing evidence supports its recommendation to limit added sugar intakes to less than 10% of total energy (35). This systematic review included 30 RCTs and 38 prospective cohort studies. The meta-analysis found that in trials of adults with ad libitum diets, decreased intake of added sugars significantly reduced body weight (0.80 kg, 95% CI 0.39 to 1.21; P<0.001), whereas increased consumption led to a comparable weight increase (0.75 kg, 95% CI 0.30 to 1.19; P=0.001). A meta-analysis of RCTs conducted among children did not show a significant effect of reducing added sugar consumption on body weight. However, the analysis did not include the two recently published large RCTs described above. A meta-analysis of prospective cohort studies conducted in children revealed that higher consumption of SSBs was associated with a 55% (95% CI 32%-82%) higher risk of becoming overweight and obese compared to those with the lowest intake. The authors concluded that “Among free living people involving ad libitum diets, intake of free sugars or sugar sweetened beverages is a determinant of body weight.” Furthermore, the authors noted, “When considering the rapid weight gain that occurs after an increased intake of sugars, it seems reasonable to conclude that advice relating to sugars intake is a relevant component of a strategy to reduce the high risk of overweight and obesity in most countries.”
Evidence Synthesis: A Causal Relationship between SSB intake and Obesity
We evaluated whether the available evidence on SSB intake and obesity meets the causality criteria commonly used in non-communicable disease epidemiology. Here we consider both observational evidence, which is relevant for long-term weight gain, and clinical trial evidence, which typically addresses short-term weight change. These two types of evidence are complementary, and both are indispensable when evaluating causality.
Strength: Prospective cohort studies have consistently shown a positive association between SSB intake and long-term weight gain and obesity in children and adults. RCTs have shown clinically significant benefits of reduction in SSB or added sugar consumption on body weight. Although the effect size appears to be modest, the unit of exposure is relatively small (typically 1 serving/day in most studies). For individuals consuming larger amounts, the benefits of reducing SSBs would be much greater. Furthermore, prevention of long-term excess weight gain by limiting SSB consumption is likely to be more effective in reducing prevalence of obesity than short-term weight loss among those who are already overweight or obese.
Consistency: The evidence from prospective cohort studies and RCTs is highly consistent in both children and adults.
Temporality: The temporal relationship between SSB intake and obesity risk is well established, given that the evidence reviewed here is derived from prospective cohort studies and RCTs.
Dose-response relationship: As SSB intake increases, the amount of weight gain increases in a dose-response manner.
Biological plausibility: SSBs contain large amounts of energy from rapidly absorbable sugars. Consumption of these calories in liquid form is associated with less satiety and an incomplete compensatory reduction in energy intake at subsequent meals (36), leading to the overconsumption of total daily calories. In this regard, regular consumption of SSBs is considered a unique dietary contributor to positive energy balance and weight gain.
Alternate explanations: The positive association between SSBs and obesity found in observational studies may be due to confounding by other correlated dietary and lifestyle factors; however, these factors were carefully adjusted for in multivariate analyses. Additionally, the results from well-conducted RCTs are not susceptible to such confounding and support the conclusions from observational analyses.
Experimental evidence: Rigorously conducted RCTs have shown that reducing consumption of SSBs significantly decreases weight gain and adiposity in children. Short-term mechanistic studies have shown that SSB consumption increases visceral adiposity, dyslipidemia, and plasma concentrations of uric acid and inflammatory cytokines (17).
Taken together, current evidence on SSBs and obesity meets all key criteria commonly used to evaluate causal relationships in epidemiology. In other words, there is compelling evidence that SSB intake is causally related to increased risk of obesity. Furthermore, there is also convincing evidence from recent RCTs that reducing SSB intake decreases risk of weight gain and obesity in children and adolescents.
Of course, no single study is perfect, and the scientific evidence will continue to evolve regarding the health effects of SSBs. In the meantime, we should avoid the trap of demanding absolute proof before allowing action to be taken (37). Sir Austin Bradford Hill’s thoughts on causality several decades ago are still relevant to today’s obesity epidemic (38):
“All scientific work is incomplete—whether it be observational or experimental. All scientific work is liable to be upset or modified by advancing knowledge. That does not confer upon us a freedom to ignore the knowledge we already have, or to postpone the action it appears to demand at a given time.”
SSBs and Type 2 Diabetes and Cardiovascular Risk
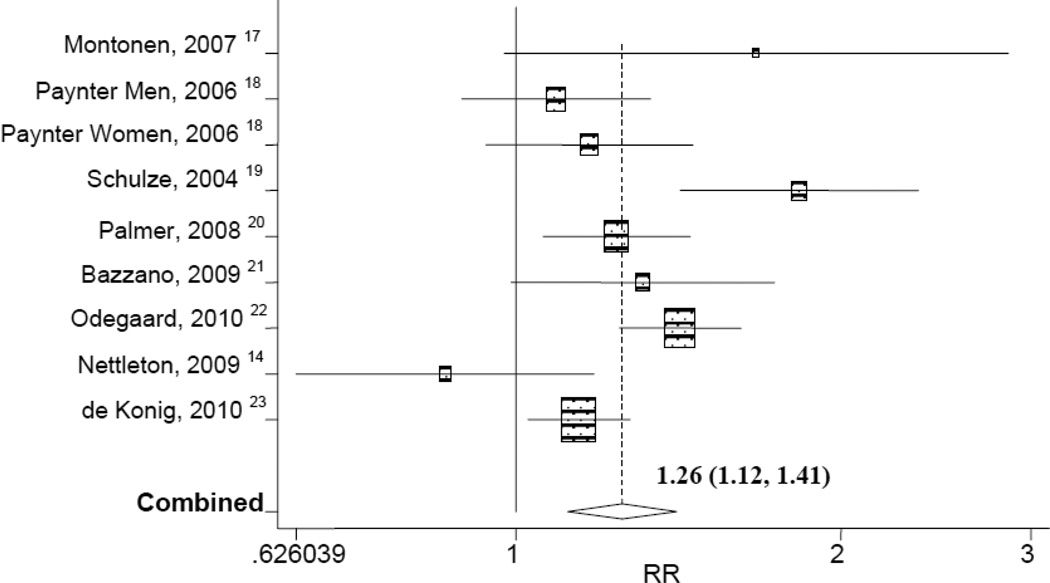
Growing evidence indicates that SSB consumption is associated with increased risk of T2D and cardiometabolic disorders. We conducted a meta-analysis of eight prospective cohort studies evaluating SSB intake and the risk of T2D (39). Based on 310,819 participants and 15,043 T2D cases, individuals in the highest category of SSB intake (usually 1–2 servings/day) had a 26% (RR 1.26, 95% CI 1.12–1.41) greater risk of developing T2D compared to those in the lowest category (none or < 1 per month) (39) (Figure 4). This association is consistent across ethnic groups (Caucasians, African Americans, and Asians), genders, and age groups. Experimental evidence from RCTs evaluating the effects of reducing SSBs on clinical T2D is lacking due to cost and other feasibility considerations. Nonetheless, findings from prospective cohort studies have shown a relatively strong and consistent association in well-powered studies, established temporality, and demonstrated a dose-response relationship (40). In addition, short-term mechanistic studies have established a biologic rationale and causal relationships with biomarkers of T2D such as insulin resistance and chronic inflammation. Several lines of evidence, taken together, meet the key Bradford Hill criteria to establish a causal relationship between SSB consumption and risk of T2D (38) (Table 2).
Figure 4.
Forrest plot of prospective cohort studies evaluating sugar-sweetened beverage consumption and risk of type 2 diabetes (310,819 participants and 15,043 incident diabetes cases), comparing extreme quantiles of intake.
From: Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. 2010; 33: 2477–83.
Table 2.
Bradford Hill Criteria for causality applied to evidence evaluating SSB consumption and risk of Type 2 Diabetes (T2D)
| Bradford Hill Criteria | SSB consumption and risk of T2D |
|---|---|
| 1) Strength of Association | Significant positive association RR: 1.26 (1.12, 1.41) for 1–2 servings/day |
| 2) Consistency | Consistent data from large prospective cohort studies |
| 3) Specificity | SSB has been shown to increase risk of related metabolic conditions and unrelated conditions such as dental caries and reductions in bone mineral density |
| 4) Temporality | Prospective studies have established temporality |
| 5) Biological Gradient (dose-response) | Increase 1 SSB/d associated with about 15% increased risk of T2D RR: 1.15 (1.11, 1.20) |
| 6) Biological Plausibility | Evidence regarding incomplete compensation for liquid calories, glycemic effects of consuming large amounts of rapidly absorbable sugars and metabolic effects of fructose provide biological plausibility |
| 7) Experimental Evidence | RCTs with clinical T2D as an endpoint are logistically difficult; however, experimental evidence from studies of biomarkers of T2D and cardiovascular risk provide support. |
Malik VS, Hu FB. Sweeteners and Risk of Obesity and Type 2 Diabetes: The Role of Sugar-Sweetened Beverages. Current Diabetes Reports. 2012.
There is increasing evidence that higher SSB consumption contributes to the development of several additional chronic diseases, including hypertension, dyslipidemia, inflammation, and coronary heart disease (CHD). In the Nurses’ Health Study and Nurses’ Health Study II cohorts, women who consumed ≥4 servings per day of SSBs had a 44% (RR=1.44, 95% CI: 0.98, 2.11) and 28% (RR=1.28, 95% CI: 1.01, 1.62) greater risk of developing hypertension, respectively, compared to infrequent consumers (41). In a post-hoc analysis of an 18-month behavioral intervention trial, a reduction in consumption of SSBs was significantly associated with reduced blood pressure, even after adjustment for weight change (42). Regarding lipid parameters, Dhingra and colleagues found that daily soft drink consumers had a 22% greater risk of developing hypertriglyceridemia (≥ 1.7 mmol/L or on treatment) (RR=1.22, 95% CI: 1.07, 1.41) and low-HDL cholesterol (<1.03 mmol/L for men and <1.3 mmol/L for women or on treatment) (RR=1.22, 95% CI: 1.04, 1.44) compared to non-consumers (43). Similarly, among participants in the Multi-Ethnic Study of Atherosclerosis (MESA), daily SSB consumers had a 28% greater risk of developing hypertriglyceridemia (RR=1.28, 95% CI 1.02, 1.60) and low HDL cholesterol (RR=1.28, 95% CI 0.99, 1.64) than non-consumers (44).
In the Nurses’ Health Study, we found that regular SSB intake was significantly associated with increased incidence of CHD (nonfatal myocardial infarction or fatal CHD) (45). In over 88,000 women followed for 24 years, those who consumed ≥2 servings per day of SSBs had a 35% greater risk of CHD compared to infrequent consumers, after adjusting for other unhealthy lifestyle factors (RR=1.35, 95% CI: 1.1, 1.7; p<0.01 for trend). Additional adjustment for potential mediating factors (including BMI, total energy intake, and incident T2D) attenuated the associations, but they remained statistically significant, suggesting that the effect of SSBs may not be entirely mediated by these factors. Similar results were found in the Health Professionals Follow-Up Study, a prospective cohort study including 42,883 men (46). In this study, the intake of SSBs but not artificially sweetened beverages was also significantly associated with increased plasma concentrations of inflammatory cytokines, including C-reactive protein, interleukin-6, and tumor necrosis factor receptors.
Some evidence suggests that consuming fructose, a constituent of sucrose and HFCS in relatively equal amounts, may exert additional adverse cardiometabolic effects. Fructose is preferentially metabolized to lipids in the liver, leading to increased hepatic de novo lipogenesis, atherogenic dyslipidemia, and insulin resistance (47). Fructose has also been shown to promote the accumulation of visceral adiposity and the deposition of ectopic fat (48–51). Fructose is the only sugar known to increase serum uric acid levels by increasing ATP degradation to AMP, a uric acid precursor (52). The production of uric acid in the liver may reduce endothelial nitric oxide, which may partly mediate the association between SSB and CHD (53). Regular consumption of SSB has also been associated with hyperuricemia (54) and risk of developing gout in large prospective cohort studies (55,56).
Healthier Alternatives to SSBs
Several beverages have been suggested as alternatives to SSBs, including plain water, 100% fruit juices, coffee, tea, and diet drinks. Unlike SSBs, water does not contain liquid calories, and small short-term studies have shown that water consumption before a meal is associated with an increase in satiety and a subsequent lower energy intake (57–59). In a recent analysis of three large cohort studies, we found that replacement of 1 serving per day of SSBs with 1 cup per day of water was associated with 0.49 kg (95% CI: 0.32–0.65) less weight gain over each 4-year period; the replacement estimate for fruit juices with water was 0.35 kg (95% CI: 0.23–0.46). Substitution of SSBs or fruit juices with other beverages (coffee, tea, diet beverages, low-fat milk) was significantly associated with less weight gain. In the Nurses’ Health Study II, we also found that substituting plain water for SSB was associated with a significantly lower risk of T2D (60). A randomized cluster trial conducted in 32 elementary schools in Germany found that health education combined with provision of drinking water in schools significantly reduced the risk of overweight in children (61). For most people, plain water is the optimal calorie-free beverage, because it is cheap and readily accessible. One of the strategies for childhood obesity prevention recommended by the Institute of Medicine of the National Academies is to “Increase access to free, safe drinking water in public places to encourage water consumption instead of SSBs” (62).
At first glance, 100% fruit juices appear to be a healthy alternative to SSBs, given that they contain some vitamins and other nutrients. However, fruit juices also contain a relatively high number of calories from natural sugars, and should therefore be consumed at most in moderation. Previous cohort studies have found positive associations between regular consumption of fruit juices and greater weight gain (22) and T2D (63). Thus, daily consumption of 100% fruit juices has been recommended to be limited to no more than 4–6 ounces.
Numerous prospective cohort studies have shown that regular consumption of coffee and tea can have favorable effects on T2D and CVD risk (64–66), possibly due to their high polyphenol content. Coffee and tea are therefore healthy alternatives to SSBs for those without contraindications, provided that caloric sweeteners and creamers are used sparingly. In the Nurses’ Health Study II, replacement of one serving of SSB with one cup of coffee daily was associated with a 17% lower risk of T2D (67). Decaffeinated and regular coffee appear to have similar benefits on incidence of T2D (68).
Diet sodas may be an acceptable alternative to SSB, as they provide few to no calories; however, little is known about the long-term health consequences of consuming artificial sweeteners. Unlike SSBs, diet beverages are sweetened with non-energy-bearing artificial sweeteners such as aspartame, sucralose, saccharine, acesulfame potassium, and neotame (69). Several epidemiologic studies have reported positive associations between diet soda consumption and weight gain and risk of metabolic syndrome and T2D (43,44,70). However, these findings may be due to reverse causation or residual confounding, since persons who consume diet soda are more likely to have a higher BMI and a greater prevalence of comorbidities and dieting behaviors. In our cohorts, after adjustment for these factors associated with diet soda consumption, we found non-significant associations between artificially sweetened beverages and T2D (22,67) and CHD (45). Also, the RCTs reviewed above have found weight control benefits of substituting diet soda for regular soda. On the other hand, some evidence suggests that the intense sweetness of artificial sweeteners (71) may condition towards a greater preference for sweets and thus may enhance appetite (72). Diet soda may also enhance appetite by cephalic phase stimulation, although this remains controversial (69). Consumers of diet soda may also use this choice as a rationale for consuming other higher-calorie foods, inevitably leading to weight gain (69). Although consumption of artificially sweetened beverages is preferable to use of SSBs, further studies are needed to evaluate the long-term metabolic consequences of using artificial sweeteners.
Implications for Public Health Policies
In light of the current obesity crisis and mounting evidence linking regular consumption of SSBs to obesity, national and international organizations have called for reductions in intake of SSBs to help prevent obesity and improve public health (73). In addition to strong and widespread public health recommendations, public policy interventions are often required to change food consumption patterns and individual behaviors, since they can bring about rapid and effective changes in the food environment (1). Several regulatory strategies to reduce intake of SSBs have recently been proposed, including taxation, enhanced nutrition labeling, vending machine restrictions, and limits on marketing to children. For cigarette smoking, imposing steep taxes has been a successful strategy in reducing their use, especially among young people, who are more sensitive to the price of cigarettes than adults. Current taxes on SSBs in most states are probably not at levels high enough to have an appreciable impact on purchasing behavior (74). Therefore, it has been suggested that imposing additional tax increases (e.g., 20%) will be necessary to change SSB consumption patterns. The revenue generated from the taxes could be used to offset some of the high health care costs attributed to obesity and implement childhood obesity prevention programs. Restrictions on access to soft drinks, especially those with a large portion size, should be considered in conjunction with health education campaigns and taxation. Together with education and public health campaigns, regulations and laws are an effective approach to changing social norms and improving food and beverage consumption patterns.
Further Issues Raised in the Debate
1. RCTs vs. Prospective cohort studies
Allison and colleagues claim that they have examined the highest-quality evidence available in the form of RCTs that either increased or decreased SSB consumption and that this type of evidence supersedes correlation or cohort studies. However, a major distinction needs to be made between most trials designed to evaluate short-term weight loss and cohort studies, which are designed to evaluate the prevention of long-term weight gain, thus addressing a different question altogether. From a public health point of view, identifying dietary determinants of long-term weight gain is critical for reducing the prevalence of obesity in the population, because once an individual becomes obese, it becomes difficult to achieve and maintain weight loss. In addition, it is not feasible to examine the relationship between SSBs consumption and risk of chronic diseases such as T2D through RCTs due to cost and compliance issues. On the other hand, large cohort studies are well suited to investigate long-term associations between dietary exposures and chronic disease risk. Therefore, to make an inference about causality between SSBs and obesity and its related diseases, it is essential to consider evidence from both RCTs and prospective cohort studies. Realistically, an ideal RCT may never be conducted in free-living populations for dietary behavioral changes; this is because almost all trials, no matter how well designed, will suffer from one or more major limitations, especially reduced compliance in the long run and infeasibility of blinding the interventions. Well-powered cohort studies, particularly those with repeated measures that carefully adjust for potential confounders, are powerful tools with which to assess diet and long-term weight patterns. By not considering cohort studies, the authors are missing the complete picture and have failed to examine the totality of the available evidence, which is essential for researchers aiming to arrive at data-driven conclusions and for clinicians and policymakers seeking to make informed evidence-based recommendations about SSBs.
2. How much evidence is considered sufficient?
By considering only one source of evidence, Allison and colleagues conclude that the evidence remains equivocal, although the results from their updated meta-analysis suggest otherwise. The meta-analysis clearly showed that adding SSBs to the diet significantly increased body weight (SMD 0.28 (95% CI 0.11, 0.44) and reducing SSBs conferred a marginally significant benefit on weight loss (SMD 0.06 (95% CI −0.01, 0.13); p=0.11). It is widely known that trials evaluating weight loss are complicated due to inherent difficulties in achieving and maintaining weight loss. Of particular note, the analysis restricted to studies among participants who were overweight at baseline showed a significant benefit of either more weight loss or less weight gain relative to controls (SMD 0.25 (95% CI 0.13, 0.38); p<0.0001). This has important implications from a public health point of view, because overweight and obese individuals tend to drink more SSBs and should be the target populations for interventions.
As described above, a recently published meta-analysis of RCTs commissioned by the WHO found that decreased intake of added sugars significantly reduced body weight (0.80 kg, P<0.001), whereas increased intake of added sugars led to a comparable weight increase (0.75 kg, P=0.001) (35). A parallel meta-analysis of cohort studies also found that higher intake of SSBs was associated with 55% (95% CI 32%-82%) increased risk of being overweight or obese among children compared to those with lower intake. In addition, two recent trials demonstrated that reducing SSBs significantly decreased weight gain in both children and adolescents (33,34). Therefore, when the totality of evidence is considered, a clear conclusion can be drawn that SSBs are an important determinant of obesity in children and adults.
3. How Strong is the Effect Size?
According to Allison and colleagues, “Among persons who are overweight or obese at baseline, reducing consumption of SSBs explains 1.54% of the variance in body weight or BMI change. … Therefore, we conclude that the debate proposition cannot be supported at this time.” However, the proportion of variance explained is a poor and inappropriate measure of effect size (75). It is not surprising that the relationship between SSBs and body weight is not dramatic, because obesity is a multifactorial condition. However, the magnitude of effects depends on the amount of exposure; most studies analyzed the effect of 1 serving per day of SSB consumption on weight gain, but a large number of people, especially teenagers, drink several servings of SSBs per day. The effect size also depends on the population; effects are much larger in susceptible groups such as those who are overweight or obese. Nonetheless, the effect size derived from both RCTs and observational studies is significant from both clinical and public health points of view. For instance, in the Dutch trial, a reduction of 104 kcal from SSBs per day was associated with 1.01 kg (2.2 lb) less weight gain during 1.5 years among normal-weight children (34). Clearly, this effect size would translate into substantial reduction in childhood obesity if the intervention were widely implemented, especially in the US, where many children consume multiple servings of SSBs per day. In our cohorts, we found that each additional daily serving of SSB added 1.00 lb over four years or 0.25 lb in one year, after adjustment for a number of dietary and lifestyle variables (25). Adult weight gain in the general population is a gradual process, occurring over decades and averaging about 1 pound per year. Thus, based on these data, eliminating 1 serving of SSB per day from the diet could be a cost-effective way to reduce annual weight gain by approximately 25%, which would have a huge public health impact.
4. What Are the Positions of National and International Organizations?
Allison and colleagues attempt to contextualize their results and provide support for their stance by cherry-picking quotes from various scientists, expert panels, and some US legislators. However, many of these quotes are outdated (including one quote from our earlier review paper published in 2006), because much of the evidence reviewed in this article was published recently. Some of the quotes are also misused. For example, the joint statement from the American Heart Association and American Diabetes Association that “there is insufficient data to determine whether use of non-nutritive sweeteners to displace caloric sweeteners benefits body weight or cardiometabolic risk factors” does not mean that they do not believe the benefits of SSB reduction on body weight. Moreover, a number of authoritative scientific associations and committees including the United States Department of Agriculture (76), the American Heart Association (77,78), the American Academy of Pediatrics (79), the American Medical Association (80), the American Diabetes Association (81), the Institute of Medicine of the National Academies (62), the World Health Organization, and the Centers for Disease Control and Prevention (82–85) are convinced of the evidence and are calling for reductions in consumption of SSBs for prevention of obesity and chronic diseases (Table 3).
Table 3.
Statements from scientific associations supporting a reduction of SSB
| Association | Statement |
|---|---|
| American Heart Association |
The American Heart Association recommends limiting the amount of added sugars you consume to no more than half of your daily discretionary calories allowance. For most American women, that’s no more than 100 calories per day, or about 6 teaspoons of sugar. For men, it’s 150 calories per day, or about 9 teaspoons. For reference, one 12-ounce can of cola contains 8–10 teaspoons of added sugar, for 130–150 calories. |
| American Heart Association Healthy Diet Goals: As part of a healthy diet, an adult consuming 2,000 calories daily should aim for no more than 450 calories (36 ounces) a week from sugar-sweetened beverages. | |
| American Diabetes Association |
Avoid sugary drinks like regular soda, fruit punch, fruit drinks, energy drinks, sweet tea, and other sugary drinks. These will raise blood glucose and can provide several hundred calories in just one serving! See for yourself: |
| |
| American Academy of Pediatrics |
Reduce the intake of sugar-sweetened beverages and foods. |
|
Sweetened beverages and naturally sweet beverages, such as fruit juice, should be limited to 4 to 6 oz per day for children 1 to 6 years old, and to 8 to 12 oz per day for children 7 to 18 years old. | |
| World Health Organization |
Added sugar should be limited to < 10% of a person’s caloric intake |
| For diet, recommendations for populations and individuals should include the following: …limit the intake of free sugars | |
| Purpose is to guide efforts by Member States in designing new and/or strengthening existing policies on food marketing communications to children in order to reduce the impact on children of marketing of foods high in saturated fats, trans-fatty acids, free sugars, or salt. | |
| Institute of Medicine of the National Academies |
Strategy 7: Increase access to free, safe drinking water in public places to encourage water consumption instead of sugar-sweetened beverages |
| United States Department of Agriculture Dietary Guidelines Advisory Committee |
Reduce the incidence and prevalence of overweight and obesity of the US population by reducing overall calorie intake and increasing physical activity….To achieve this, Americans should…avoid sugar-sweetened beverages…. |
| American Medical Association |
Limit sugar-sweetened beverages |
| Centers for Disease Control and Prevention |
Recommendation #10: Communities should discourage consumption of sugar-sweetened beverages. |
5. Red Herring Arguments?
The authors cast doubts on the validity of scientific evidence by raising a number of points that go beyond the scope of the scientific data (“emotion-raising language”, “distortion of scientific information” by the media and “the mere exposure effect”). However, cherry-picking quotes from individual researchers or media reports is problematic and distracts from the central issue. McKee et al. (86) have warned against using rhetorical arguments to give the appearance of legitimate and unresolved debate about matters generally accepted by the mainstream scientific community, such as the existence of global warming, health effects of passive smoking, and complications of vaccines. As indicated by Capewell (37), tactics often invoked by tobacco and beverage and food companies to deny scientific evidence of harm include selective use of evidence to support a position; creation of impossible expectations of research and public health advocates; and the use of red herrings and other tangential arguments to divert attention from the main issue. Such techniques can be used to manufacture doubt and argue against taking action. While we should devote our efforts to obtaining the best possible scientific evidence while keeping an open and constructively skeptical mind, we should also be vigilant against the red herring tactics that are commonly employed by the tobacco and beverage industries.
Conclusions
Consumption of SSBs has increased markedly across the globe in recent decades, tracking closely with the growing burdens of obesity. These beverages are currently the largest source of added sugar intake and the top source of daily energy in the US diet. The cumulative evidence from observational studies and experimental trials is sufficient to conclude that regular consumption of SSBs causes excess weight gain and these beverages are unique dietary contributors to obesity and T2D. Compelling evidence indicates that reducing SSBs will have significant impact on the prevalence of obesity and its related diseases, especially T2D. Despite strong resistance from the beverage industry, several public policies and regulatory strategies to reduce intake of SSBs are already in place or being developed. The combination of public health campaigns and regulations and laws is needed to change social norms and dietary behaviors. Although reducing SSB consumption alone is unlikely to solve the obesity epidemic entirely, limiting intake of SSBs is one simple change that could have a measurable impact on weight control and prevention of T2D and other metabolic diseases.
Acknowledgments
Dr. Hu’s research is supported by NIH grant DK58845, HL60712, P30 DK46200, and U54CA155626-01. Dr. Hu has received research support from the California Walnut Commission.
Footnotes
The paper was based on a presidential keynote presentation at Obesity 2012.
Potential conflicts of interest: None
References
- 1.Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications. Nature reviews Endocrinology. 2012 doi: 10.1038/nrendo.2012.199. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA : the journal of the American Medical Association. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA : the journal of the American Medical Association. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 5.CDC. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. [WWW document] URL http://www.cdc.gov/diabetes/pubs/estimates11.htm.
- 6.IDF. IDF DIABETES ATLAS UPDATE 2012. [WWW document] URL http://www.idf.org/diabetesatlas/5e/the-global-burden.
- 7.FB. H. Obesity Epidemiology. Oxford University Press; 2008. [Google Scholar]
- 8.Hu FB, Malik VS. Sugar-sweetened beverages and risk of obesity and type 2 diabetes: epidemiologic evidence. Physiology & behavior. 2010;100:47–54. doi: 10.1016/j.physbeh.2010.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Cancer Institute. Sources of Calories from Added Sugars among the US Population, 2005–06. Risk Factor Monitoring and Methods Branch Web site. Applied Research Program. Mean intake of added sugars & percentage contribution of various foods among us population. [WWW document] URL http://riskfactor.cancer.gov/diet/foodsources/added_sugars/
- 10.Brownell KD, Farley T, Willett WC, Popkin BM, Chaloupka FJ, Thompson JW, et al. The public health and economic benefits of taxing sugar-sweetened beverages. The New England journal of medicine. 2009;361:1599–1605. doi: 10.1056/NEJMhpr0905723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ogden CL, Kit BK, Carroll MD, Park S. Consumption of sugar drinks in the United States, 2005–2008. NCHS data brief. 2011:1–8. [PubMed] [Google Scholar]
- 12.Wang YC, Bleich SN, Gortmaker SL. Increasing caloric contribution from sugar-sweetened beverages and 100% fruit juices among US children and adolescents, 1988–2004. Pediatrics. 2008;121:e1604–e1614. doi: 10.1542/peds.2007-2834. [DOI] [PubMed] [Google Scholar]
- 13.Piernas C, Popkin BM. Food portion patterns and trends among U.S. children and the relationship to total eating occasion size, 1977–2006. The Journal of nutrition. 2011;141:1159–1164. doi: 10.3945/jn.111.138727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Welsh JA, Sharma AJ, Grellinger L, Vos MB. Consumption of added sugars is decreasing in the United States. The American journal of clinical nutrition. 2011;94:726–734. doi: 10.3945/ajcn.111.018366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kleiman S, Ng SW, Popkin B. Drinking to our health: can beverage companies cut calories while maintaining profits? Obesity reviews : an official journal of the International Association for the Study of Obesity. 2012;13:258–274. doi: 10.1111/j.1467-789X.2011.00949.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yngve A, Haapala I, Hodge A, McNeill G, Tseng M. Making soft drinks the dietary version of the cigarette. Public health nutrition. 2012;15:1329–1330. doi: 10.1017/S1368980012003242. [DOI] [PubMed] [Google Scholar]
- 17.Malik VS, Popkin BM, Bray GA, Despres JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121:1356–1364. doi: 10.1161/CIRCULATIONAHA.109.876185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. The American journal of clinical nutrition. 2006;84:274–288. doi: 10.1093/ajcn/84.1.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Malik VS, Willett WC, Hu FB. Sugar-sweetened beverages and BMI in children and adolescents: reanalyses of a meta-analysis. The American journal of clinical nutrition. 2009;89:438–439. doi: 10.3945/ajcn.2008.26980. author reply 39–40. [DOI] [PubMed] [Google Scholar]
- 20.Vartanian LR, Schwartz MB, Brownell KD. Effects of soft drink consumption on nutrition and health: a systematic review and meta-analysis. American journal of public health. 2007;97:667–675. doi: 10.2105/AJPH.2005.083782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Forshee RA, Anderson PA, Storey ML. Sugar-sweetened beverages and body mass index in children and adolescents: a meta-analysis. The American journal of clinical nutrition. 2008;87:1662–1671. doi: 10.1093/ajcn/87.6.1662. [DOI] [PubMed] [Google Scholar]
- 22.Schulze MB, Manson JE, Ludwig DS, Colditz GA, Stampfer MJ, Willett WC, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. JAMA : the journal of the American Medical Association. 2004;292:927–934. doi: 10.1001/jama.292.8.927. [DOI] [PubMed] [Google Scholar]
- 23.Palmer JR, Boggs DA, Krishnan S, Hu FB, Singer M, Rosenberg L. Sugar-sweetened beverages and incidence of type 2 diabetes mellitus in African American women. Archives of internal medicine. 2008;168:1487–1492. doi: 10.1001/archinte.168.14.1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Odegaard AO, Koh WP, Arakawa K, Yu MC, Pereira MA. Soft drink and juice consumption and risk of physician-diagnosed incident type 2 diabetes: the Singapore Chinese Health Study. American journal of epidemiology. 2010;171:701–708. doi: 10.1093/aje/kwp452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. The New England journal of medicine. 2011;364:2392–2404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qi Q, Chu AY, Kang JH, Jensen MK, Curhan GC, Pasquale LR, et al. Sugar-sweetened beverages and genetic risk of obesity. The New England journal of medicine. 2012;367:1387–1396. doi: 10.1056/NEJMoa1203039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mattes RD, Shikany JM, Kaiser KA, Allison DB. Nutritively sweetened beverage consumption and body weight: a systematic review and meta-analysis of randomized experiments. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2011;12:346–365. doi: 10.1111/j.1467-789X.2010.00755.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malik VS, Willett WC, Hu FB. Nutritively sweetened beverages and obesity. JAMA : the journal of the American Medical Association. 2009;301:2210. doi: 10.1001/jama.2009.743. author reply 10-1. [DOI] [PubMed] [Google Scholar]
- 29.Albala C, Ebbeling CB, Cifuentes M, Lera L, Bustos N, Ludwig DS. Effects of replacing the habitual consumption of sugar-sweetened beverages with milk in Chilean children. The American journal of clinical nutrition. 2008;88:605–611. doi: 10.1093/ajcn/88.3.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sichieri R, Paula Trotte A, de Souza RA, Veiga GV. School randomised trial on prevention of excessive weight gain by discouraging students from drinking sodas. Public health nutrition. 2009;12:197–202. doi: 10.1017/S1368980008002644. [DOI] [PubMed] [Google Scholar]
- 31.James J, Thomas P, Cavan D, Kerr D. Preventing childhood obesity by reducing consumption of carbonated drinks: cluster randomised controlled trial. Bmj. 2004;328:1237. doi: 10.1136/bmj.38077.458438.EE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.James J, Thomas P, Kerr D. Preventing childhood obesity: two year follow-up results from the Christchurch obesity prevention programme in schools (CHOPPS) Bmj. 2007;335:762. doi: 10.1136/bmj.39342.571806.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ebbeling CB, Feldman HA, Chomitz VR, Antonelli TA, Gortmaker SL, Osganian SK, et al. A randomized trial of sugar-sweetened beverages and adolescent body weight. The New England journal of medicine. 2012;367:1407–1416. doi: 10.1056/NEJMoa1203388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. The New England journal of medicine. 2012;367:1397–1406. doi: 10.1056/NEJMoa1203034. [DOI] [PubMed] [Google Scholar]
- 35.Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. Bmj. 2012;346:e7492. doi: 10.1136/bmj.e7492. [DOI] [PubMed] [Google Scholar]
- 36.DiMeglio DP, Mattes RD. Liquid versus solid carbohydrate: effects on food intake and body weight. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 2000;24:794–800. doi: 10.1038/sj.ijo.0801229. [DOI] [PubMed] [Google Scholar]
- 37.Capewell S, Capewell A. Denialism in public health. Beware SLEAZE tactics. Bmj. 2011;342 doi: 10.1136/bmj.d287. d287. [DOI] [PubMed] [Google Scholar]
- 38.Hill AB. The Environment and Disease: Association or Causation? Proceedings of the Royal Society of Medicine. 1965;58:295–300. doi: 10.1177/003591576505800503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Malik VS, Popkin BM, Bray GA, Despres JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes care. 2010;33:2477–2483. doi: 10.2337/dc10-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Malik VS, Hu FB. Sweeteners and Risk of Obesity and Type 2 Diabetes: The Role of Sugar-Sweetened Beverages. Current diabetes reports. 2012 doi: 10.1007/s11892-012-0259-6. [DOI] [PubMed] [Google Scholar]
- 41.Winkelmayer WC, Stampfer MJ, Willett WC, Curhan GC. Habitual caffeine intake and the risk of hypertension in women. JAMA : the journal of the American Medical Association. 2005;294:2330–2335. doi: 10.1001/jama.294.18.2330. [DOI] [PubMed] [Google Scholar]
- 42.Chen L, Caballero B, Mitchell DC, Loria C, Lin PH, Champagne CM, et al. Reducing consumption of sugar-sweetened beverages is associated with reduced blood pressure: a prospective study among United States adults. Circulation. 2010;121:2398–2406. doi: 10.1161/CIRCULATIONAHA.109.911164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dhingra R, Sullivan L, Jacques PF, Wang TJ, Fox CS, Meigs JB, et al. Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation. 2007;116:480–488. doi: 10.1161/CIRCULATIONAHA.107.689935. [DOI] [PubMed] [Google Scholar]
- 44.Nettleton JA, Lutsey PL, Wang Y, Lima JA, Michos ED, Jacobs DR., Jr Diet soda intake and risk of incident metabolic syndrome and type 2 diabetes in the Multi-Ethnic Study of Atherosclerosis (MESA) Diabetes Care. 2009;32:688–694. doi: 10.2337/dc08-1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fung TT, Malik V, Rexrode KM, Manson JE, Willett WC, Hu FB. Sweetened beverage consumption and risk of coronary heart disease in women. Am J Clin Nutr. 2009;89:1037–1042. doi: 10.3945/ajcn.2008.27140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.de Koning L, Malik VS, Kellogg MD, Rimm EB, Willett WC, Hu FB. Sweetened beverage consumption, incident coronary heart disease, and biomarkers of risk in men. Circulation. 2012;125:1735–1741. doi: 10.1161/CIRCULATIONAHA.111.067017. S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bray GA. How bad is fructose? Am J Clin Nutr. 2007;86:895–896. doi: 10.1093/ajcn/86.4.895. [DOI] [PubMed] [Google Scholar]
- 48.Teff KL, Grudziak J, Townsend RR, Dunn TN, Grant RW, Adams SH, et al. Endocrine and metabolic effects of consuming fructose- and glucose-sweetened beverages with meals in obese men and women: influence of insulin resistance on plasma triglyceride responses. J Clin Endocrinol Metab. 2009;94:1562–1569. doi: 10.1210/jc.2008-2192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stanhope KL, Schwarz JM, Keim NL, Griffen SC, Bremer AA, Graham JL, et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest. 2009;119:1322–1334. doi: 10.1172/JCI37385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stanhope KL, Griffen SC, Bair BR, Swarbrick MM, Keim NL, Havel PJ. Twenty-four-hour endocrine and metabolic profiles following consumption of high-fructose corn syrup-, sucrose-, fructose-, and glucose-sweetened beverages with meals. Am J Clin Nutr. 2008;87:1194–1203. doi: 10.1093/ajcn/87.5.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stanhope KL, Havel PJ. Endocrine and metabolic effects of consuming beverages sweetened with fructose, glucose, sucrose, or high-fructose corn syrup. Am J Clin Nutr. 2008;88:1733S–1737S. doi: 10.3945/ajcn.2008.25825D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Johnson RJ, Segal MS, Sautin Y, Nakagawa T, Feig DI, Kang DH, et al. Potential role of sugar (fructose) in the epidemic of hypertension, obesity and the metabolic syndrome, diabetes, kidney disease, and cardiovascular disease. Am J Clin Nutr. 2007;86:899–906. doi: 10.1093/ajcn/86.4.899. [DOI] [PubMed] [Google Scholar]
- 53.Nakagawa T, Hu H, Zharikov S, Tuttle KR, Short RA, Glushakova O, et al. A causal role for uric acid in fructose-induced metabolic syndrome. Am J Physiol Renal Physiol. 2006;290:F625–F631. doi: 10.1152/ajprenal.00140.2005. [DOI] [PubMed] [Google Scholar]
- 54.Gao X, Qi L, Qiao N, Choi HK, Curhan G, Tucker KL, et al. Intake of added sugar and sugar-sweetened drink and serum uric acid concentration in US men and women. Hypertension. 2007;50:306–312. doi: 10.1161/HYPERTENSIONAHA.107.091041. [DOI] [PubMed] [Google Scholar]
- 55.Choi HK, Willett W, Curhan G. Fructose-rich beverages and risk of gout in women. Jama. 2010;304:2270–2278. doi: 10.1001/jama.2010.1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Choi HK, Curhan G. Soft drinks, fructose consumption, and the risk of gout in men: prospective cohort study. Bmj. 2008;336:309–312. doi: 10.1136/bmj.39449.819271.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stookey JD, Constant F, Gardner CD, Popkin BM. Replacing sweetened caloric beverages with drinking water is associated with lower energy intake. Obesity (Silver Spring) 2007;15:3013–3022. doi: 10.1038/oby.2007.359. [DOI] [PubMed] [Google Scholar]
- 58.Dennis EA, Dengo AL, Comber DL, Flack KD, Savla J, Davy KP, et al. Water consumption increases weight loss during a hypocaloric diet intervention in middle-aged and older adults. Obesity (Silver Spring) 2010;18:300–307. doi: 10.1038/oby.2009.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Popkin BM, Barclay DV, Nielsen SJ. Water and food consumption patterns of U.S. adults from 1999 to 2001. Obes Res. 2005;13:2146–2152. doi: 10.1038/oby.2005.266. [DOI] [PubMed] [Google Scholar]
- 60.Pan A, Malik VS, Schulze MB, Manson JE, Willett WC, Hu FB. Plain-water intake and risk of type 2 diabetes in young and middle-aged women. The American journal of clinical nutrition. 2012;95:1454–1460. doi: 10.3945/ajcn.111.032698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Muckelbauer R, Libuda L, Clausen K, Toschke AM, Reinehr T, Kersting M. Promotion and provision of drinking water in schools for overweight prevention: randomized, controlled cluster trial. Pediatrics. 2009;123:e661–e667. doi: 10.1542/peds.2008-2186. [DOI] [PubMed] [Google Scholar]
- 62.Institute of Medicine of the National Academies. Local Government Actions to Prevent Childhood Obesity. Washington DC: 2009. p. 5. [PubMed] [Google Scholar]
- 63.Bazzano LA, Li TY, Joshipura KJ, Hu FB. Intake of fruit, vegetables, and fruit juices and risk of diabetes in women. Diabetes Care. 2008;31:1311–1317. doi: 10.2337/dc08-0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Huxley R, Lee CM, Barzi F, Timmermeister L, Czernichow S, Perkovic V, et al. Coffee, decaffeinated coffee, and tea consumption in relation to incident type 2 diabetes mellitus: a systematic review with meta-analysis. Archives of internal medicine. 2009;169:2053–2063. doi: 10.1001/archinternmed.2009.439. [DOI] [PubMed] [Google Scholar]
- 65.van Dam RM. Coffee consumption and risk of type 2 diabetes, cardiovascular diseases, and cancer. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme. 2008;33:1269–1283. doi: 10.1139/H08-120. [DOI] [PubMed] [Google Scholar]
- 66.van Dieren S, Uiterwaal CS, van der Schouw YT, van der AD, Boer JM, Spijkerman A, et al. Coffee and tea consumption and risk of type 2 diabetes. Diabetologia. 2009;52:2561–2569. doi: 10.1007/s00125-009-1516-3. [DOI] [PubMed] [Google Scholar]
- 67.de Koning L, Malik VS, Rimm EB, Willett WC, Hu FB. Sugar-sweetened and artificially sweetened beverage consumption and risk of type 2 diabetes in men. Am J Clin Nutr. 2011;93:1321–1327. doi: 10.3945/ajcn.110.007922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bhupathiraju SN, Pan A, Malik VS, Manson JE, Willett WC, van Dam RM, et al. Caffeinated and caffeine-free beverages and risk of type 2 diabetes. The American journal of clinical nutrition. 2012 doi: 10.3945/ajcn.112.048603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mattes RD, Popkin BM. Nonnutritive sweetener consumption in humans: effects on appetite and food intake and their putative mechanisms. Am J Clin Nutr. 2009;89:1–14. doi: 10.3945/ajcn.2008.26792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation. 2008;117:754–761. doi: 10.1161/CIRCULATIONAHA.107.716159. [DOI] [PubMed] [Google Scholar]
- 71.Brown RJ, de Banate MA, Rother KI. Artificial sweeteners: a systematic review of metabolic effects in youth. Int J Pediatr Obes. 2010;5:305–312. doi: 10.3109/17477160903497027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fowler SP, Williams K, Resendez RG, Hunt KJ, Hazuda HP, Stern MP. Fueling the obesity epidemic? Artificially sweetened beverage use and long-term weight gain. Obesity (Silver Spring) 2008;16:1894–1900. doi: 10.1038/oby.2008.284. [DOI] [PubMed] [Google Scholar]
- 73.Yale Rudd Center for Food Policy and Obesity. Sugar-Sweetened Beverage Taxes and Sugar Intake: Policy Statements, Endorsements, and Recommendations. [WWW document] URL http://www.yaleruddcenter.org/resources/upload/docs/what/policy/SSBtaxes/SSBTaxStatements.pdf.
- 74.Fletcher JM, Frisvold D, Tefft N. Taxing soft drinks and restricting access to vending machines to curb child obesity. Health affairs. 2010;29:1059–1066. doi: 10.1377/hlthaff.2009.0725. [DOI] [PubMed] [Google Scholar]
- 75.D’andrade R, Dart J. The interpretation of r versus r2 or why percent of variance accounted for is a poor measure of size of effect. Journal of Quantitative Anthropology. 1990;2:47–59. [Google Scholar]
- 76.Center for Nutrition Policy and Promotion. Report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans. [WWW document] URL http://www.cnpp.usda.gov/DGAs2010-DGACReport.htm.
- 77.Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, et al. Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2009;120:1011–1020. doi: 10.1161/CIRCULATIONAHA.109.192627. [DOI] [PubMed] [Google Scholar]
- 78.The American Heart Association. The American Heart Association Healthy Diet Goals. [WWW document] URL http://www.heart.org/HEARTORG/GettingHealthy/NutritionCenter/HealthyDietGoals/Healthy-Diet-Goals_UCM_310436_SubHomePage.jsp.
- 79.Gidding SS, Dennison BA, Birch LL, Daniels SR, Gillman MW, Lichtenstein AH, et al. Dietary recommendations for children and adolescents: a guide for practitioners. Pediatrics. 2006;117:544–559. doi: 10.1542/peds.2005-2374. [DOI] [PubMed] [Google Scholar]
- 80.Barlow SE, Expert C. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 81.The American Diabetes Association. What to Avoid. [WWW document] URL http://www.diabetes.org/food-and-fitness/food/what-can-i-eat/what-can-i-drink.html.
- 82.Nishida C, Uauy R, Kumanyika S, Shetty P. The joint WHO/FAO expert consultation on diet, nutrition and the prevention of chronic diseases: process, product and policy implications. Public health nutrition. 2004;7:245–250. doi: 10.1079/phn2003592. [DOI] [PubMed] [Google Scholar]
- 83.WHO. World Health Organization Global Strategy on Diet, Physical Activity and Health: Marketing of foods and non-alcoholic beverages to children. [WWW document] URL http://www.who.int/dietphysicalactivity/marketing-food-to-children/en/index.html.
- 84.WHO. World Health Organization Global Strategy on Diet, Physical Activity and Health. [WWW document] URL http://www.who.int/dietphysicalactivity/diet/en/index.html.
- 85.CDC. Morbidity and Mortality Weekly Report. Recommended Community Strategies and Measurements to Prevent Obesity in the United States. [WWW document] URL http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5807a1.htm. [PubMed]
- 86.McKee M, Diethelm P. How the growth of denialism undermines public health. Bmj. 2010;341 doi: 10.1136/bmj.c6950. c6950. [DOI] [PubMed] [Google Scholar]