Abstract
Secondary analyses were performed on data from two randomized controlled trials of a cognitive behavioral therapy (CBT) program for post-traumatic stress disorder (PTSD) in individuals with severe mental illness (SMI) to examine the feasibility, tolerability, and effectiveness for individuals with borderline personality disorder (BPD). In Study 1, 27 participants received CBT or treatment as usual. In Study 2, 55 participants received CBT or a Brief treatment. Feasibility and tolerability of CBT, PTSD symptoms, and other mental health and functional outcomes were examined, with assessments at baseline, post-treatment, and two follow-up time points. CBT was feasible and tolerable in this population. Study 1 participants in CBT improved significantly more in PTSD symptoms, depression, and self-reported physical health. Study 2 participants in both CBT and Brief improved significantly in PTSD symptoms, posttraumatic cognitions, depression, and overall functioning, with those in CBT acquiring significantly more PTSD knowledge, and having marginally significantly greater improvement in PTSD symptoms. CBT for PTSD was feasible and tolerated in individuals with SMI, BPD, and PTSD, and associated with improvements in PTSD symptoms and related outcomes. Prospective research is needed to evaluate CBT in individuals with BPD, including comparing it with staged interventions for this population.
1. Introduction
The development of borderline personality disorder (BPD) is thought to be molded by early traumatic experiences (Golier et al., 2003). BPD is thus frequently comorbid with posttraumatic stress disorder (PTSD), with the diagnostic overlap reported to be between 33% and 79% (Frías and Palma, 2015). Individuals with PTSD and co-occurring BPD have more severe PTSD symptoms than those with PTSD and other comorbid disorders (Bolton et al., 2006), leading to greater impairment, a worse prognosis, and higher healthcare utilization (Connor et al., 2002; Frías and Palma, 2015).
Despite the high prevalence of PTSD in individuals with BPD, treatment research on this comorbid population has lagged. Current recommendations suggest stage-based approaches for the treatment of PTSD in individuals with BPD and PTSD, with the stabilization of symptoms and affect regulation prioritized before moving onto trauma-focused treatment (Cloitre et al., 2012). These recommendations have been recently challenged, based on the limited evidence supporting staged approaches, and the need for further research on the effects of more conventional approaches to PTSD (e.g., cognitive restructuring or prolonged exposure) has been emphasized (de Jongh et al., 2016).
Recent research points to the promise of non-staged treatment approaches for vulnerable populations with PTSD. Two randomized controlled trials have demonstrated that a cognitive behavioral therapy (CBT) program based on cognitive restructuring is well tolerated and effective for individuals with both severe mental illness (i.e., schizophrenia, schizoaffective disorder, severe major depression, and bipolar disorder) and PTSD (Mueser et al., 2008, 2015). As such, cognitive restructuring may also be tolerated well in individuals with comorbid PTSD and BPD, many of whom also have other severe mental illnesses (Skodol et al., 2002). Furthermore, one randomized controlled trial reported similar benefits for prolonged exposure therapy and eye movement desensitization and reprocessing therapy in persons with psychotic disorders and PTSD (van den Berg et al., 2015a). Additionally, studies conducted in PTSD populations with complex presentations and comorbidities, in which participants with personality disorders were not excluded, have demonstrated the efficacy of prolonged exposure and cognitive processing therapy (e.g., Chard, 2005; see de Jongh et al., 2016 for review).
Although two studies have examined how persons with borderline characteristics fare in conventional CBT for PTSD, they were limited either the lack of a full diagnostic assessment of BPD (Clarke et al., 2008) or by small sample size (Feeny et al., 2002). In addition, both studies were efficacy trials conducted in academic settings with stringent exclusion criteria (e.g., current suicidal ideation, severe mental illness). To our knowledge, no studies have examined CBT for individuals with comorbid BPD and PTSD in the context of an effectiveness trial targeting a more severely ill population with minimal exclusion criteria for participation.
In this paper, we retrospectively examined the feasibility, tolerability, and clinical outcomes of individuals with severe mental illness, PTSD, and BPD who participated in two randomized controlled trials evaluating a CBT program based on cognitive restructuring for vulnerable individuals with PTSD. As these trials were conducted in community mental health centers with a severe mental illness population, they present a unique opportunity to examine the benefits of CBT for PTSD within a particularly severe sample of persons with comorbid BPD. Although limited research has focused on BPD in the context of severe mental illness (Bolton et al., 2006), it is highly comorbid with both major depression and bipolar disorder (Grant et al., 2008). Considering these high rates of comorbidity, and the high distress and persistent life interference associated with both BPD and severe mental illness, a CBT for PTSD program designed for the severe mental illness population could be particularly beneficial to people who also have BPD. We hypothesized that the CBT for PTSD program would be feasible and tolerable in this comorbid sample of persons with PTSD, severe mental illness and BPD and that participants who received CBT would show clinical improvements in PTSD symptoms and knowledge of PTSD compared to control groups.
2. Methods
Secondary analyses were conducted on persons with BPD who had participated in two randomized controlled trials evaluating a CBT for PTSD program in individuals with severe mental illness and PTSD. Study 1 (Mueser et al., 2008) compared CBT with treatment as usual (TAU). Study 2 (Mueser et al., 2015), compared CBT with a brief, 3-session intervention (Nishith et al., 2015). Both studies were conducted at routine, publically funded mental health centers and included obtaining informed consent from participants. All procedures were approved by Institutional Review Boards of the respective institutions. Detailed descriptions of the procedures for both studies are provided elsewhere (Mueser et al., 2008, 2015).
2.1. Participants
The inclusion criteria for both studies were: age 18 or older; severe mental illness diagnosis (i.e., DSM-IV major depression, bipolar disorder, schizoaffective disorder, or schizophrenia and meeting of NH, VT, or NJ state criteria for severe mental illness); and current DSM-IV diagnosis of PTSD. In addition, Study 2 required that participants meet criteria for severe PTSD (i.e., Clinician Administered PTSD Scale score ≥65; Weathers et al., 1999). The exclusion criteria for both studies were: psychiatric hospitalization or suicide attempt in the past 3 months, and current substance dependence. In both studies, participants were not excluded based on self-injurious or parasuicidal behavior, suicidal ideation, or suicidal intent.
A total of 108 individuals participated in Study 1, of which the current analyses examined 27 individuals who met criteria for BPD, of whom 15 were randomized to CBT and 12 to TAU. A total of 201 individuals participated in Study 2, of which the current analyses examined 55 individuals with BPD, of whom 29 were randomized to CBT and 26 to the Brief intervention. In Study 1, most participants were female (96%, n = 26), White/Non-Hispanic (88.9%, n = 24), and middle aged (M = 45.7, SD = 9.6). Participants in Study 2 were more diverse in terms of gender (78.2% female, n = 43) and race (43.6% White, n = 24), and were slightly younger (M = 40.4, SD = 9.5). The study samples included individuals with severe symptoms, as indicated by high baseline scores on clinical measures, comorbid diagnostic status, proportion of individuals endorsing suicidal ideation, and high rates of several types of trauma (Table 1).
Table 1.
Baseline Descriptive Characteristics
| Demographics | Study 1 (n = 27) | Study 2 (n = 55) | ||
|---|---|---|---|---|
| Age | 45.7 ± 9.6 | 40.4 ± 9.5 | ||
| Gender (% female) | 96% (n = 26) | 78.2% (n = 43) | ||
| Race/Ethnicity | White/Non- Hispanic | 88.9% (n = 24) | White | 43.6% (n = 24) |
| Hispanic | 3.7% (n = 1) | Not White | 56.4% (n = 31) | |
| American Indian/Alaska Native | 7.4% (n = 2) | |||
| Marital Status | ||||
| Has not been married | 33.3% (n = 9) | 54.5% (n = 30) | ||
| Has been married | 66.7% (n = 18) | 45.5% (n = 25) | ||
| Employment | ||||
| Unemployed | 89% (n = 24) | 92.7% (n = 51) | ||
| Employed in a competitive job | 3.7% (n = 1) | 5.5% (n = 3) | ||
| Sporadic part-time jobs | 3.7% (n = 1) | 0% (n = 0) | ||
| Employed in a volunteer job | 3.7% (n = 1) | 0% (n = 0) | ||
| Unknown | 0% (n = 0) | 1.8% (n = 1) | ||
| Education level | ||||
| Less than high school | 26% (n = 7) | 29.1% (n = 16) | ||
| High school or more | 74% (n = 20) | 70.9% (n = 39) | ||
| Trauma History | Study 1 | Study 2 | ||
| SES percentages | ||||
| Accident | 78% (n = 21) | 60.0% (n = 33) | ||
| Combat | 0% (n = 0) | 5.5% (n = 3) | ||
| Death | 93% (n = 25) | 85.5% (n = 47) | ||
| Witness | 89% (n = 24) | 85.5% (n = 47) | ||
| Physical abuse as a child | 82% (n = 22) | 90.9% (n = 50) | ||
| Sexual abuse as a child | 89% (n = 24) | 85.5% (n = 47) | ||
| Threat | 82% (n = 22) | 76.4% (n = 42) | ||
| Physical abuse as an adult | 96% (n = 26) | 92.7% (n = 51) | ||
| Sexual abuse as an adult | 85% (n = 23) | 81.8% (n = 45) | ||
| Other | n/a | 43.6% (n = 24) | ||
| Mental health diagnoses and symptoms | Study 1 | Study 2 | ||
| Comorbid Diagnosis | ||||
| MDD | 67% (n = 18) | 27.3% (n = 15) | ||
| Bipolar | 33% (n = 9) | 47.3% (n = 26) | ||
| Schizoaffective | 0% (n = 0) | 25.5% (n = 14) | ||
| SCID II Number of BPD items endorsed | 6.5 ± 1.3 | 6.2 ± 1.0 | ||
| CAPS Total | 83.8 ± 17.0 | 89.3 ± 14.9 | ||
| CAPS–re-experiencing | 22.9 ± 7.1 | 23.8 ± 7.2 | ||
| CAPS avoidance | 34.0 ± 9.1 | 38.4 ± 6.6 | ||
| CAPS hyperarousal | 27.0 ± 6.3 | 27.1 ± 5.9 | ||
| PTSD Knowledge score | 10.1 ± 2.9 | 10.0 ± 2.5 | ||
| PTCI total | 3.9 ± 1.1 | 4.7 ± 0.9 | ||
| BDI-II total | 34.7 ± 12.9 | 35.0 ± 11.8 | ||
| BDI-II suicidality item | ||||
| 0 (“I don’t have any thoughts of killing myself”) | 41% (n = 11) | 44% (n = 24) | ||
| 1 (“I have thoughts of killing myself, but I would not carry them out”) | 52% (n = 14) | 44% (n = 24) | ||
| 2 (“I would like to kill myself”) | 7% (n = 2) | 4% (n = 2) | ||
| 3 (“I would kill myself if I had the chance”) | 0% (n = 0) | 5% (n = 3) | ||
| BAI total | 52.3 ± 13.7 | 33.4 ± 15.3 | ||
| Treatment Information | Study 1 | Study 2 | ||
| Randomization | ||||
| CBT | 54% (n = 15) | 53% (n = 29) | ||
| TAU | 46% (n = 12) | n/a | ||
| Brief | n/a | 47% (n = 26) | ||
| Exposed to treatment (CBT) | 85.7% (n = 12) | 74% (n = 20) | ||
| Exposed to treatment (Brief) | n/a | 87% (n = 20) | ||
2.2. Assessment instruments
Trauma exposure was assessed at baseline using the Trauma History Questionnaire (Green, 1996) in Study 1, and an abbreviated Traumatic Life Events Questionnaire (Kubany et al., 2000) in Study 2. Psychiatric disorders were evaluated with the Structured Clinical Interview for DSM-IV (SCID; First et al., 1996a), and BPD was assessed using the SCID-II (First et al., 1996b). Primary and secondary outcomes were assessed at baseline, post-treatment, and two follow up time points (Study 1: 3- and 6-months post-treatment; Study 2: 6- and 12-months post-treatment).
2.2.1. Primary outcomes
PTSD severity and diagnosis was assessed by the Clinician Administered PTSD Scale for DSM-IV (CAPS; Blake et al., 1995) for Study 1, and the CAPS for DSM-IV-Schizophrenia version (Gearon et al., 2004) for Study 2. In addition, we examined rates of severe PTSD diagnosis (CAPS ≥65). Understanding of PTSD was assessed by the self-report PTSD Knowledge Test (Pratt et al., 2005).
2.2.2. Secondary outcomes
The Posttraumatic Cognitions Inventory (PTCI; Foa et al., 1999), Beck Depression Inventory-II (BDI-II; Beck et al., 1996), and the Beck Anxiety Inventory (BAI; Beck and Steer, 1990) were used in both studies. In addition, the Brief Psychiatric Rating Scale (BPRS; Lukoff et al., 1986) and the Short Form-12 (SF-12; Ware et al., 1994) was used in Study 1 and the Positive and Negative Syndrome Scale (PANSS; Kay et al., 1987), the Brief Quality of Life Interview (QOLI, Lehman et al., 1995), and the Global Assessment of Functioning (GAF; Jones et al., 1995) scale was used in Study 2.
In both studies, clinician-rated assessments were performed by Masters or Ph.D. level trained clinical interviewers who were blind to treatment condition. Monthly calls were conducted with interviewers, which included review of reliability checks based on audiotaped interviews. For Study 1, inter-rater reliability was high, with intraclass correlation coefficients of .97 for CAPS Total and κ = .91 for PTSD diagnosis based on the CAPS in Study 1 (Mueser et al., 2008). Reliability statistics were not computed for Study 2.
2.3. Treatments
Prior to study inclusion, all clients were receiving comprehensive treatment for their psychiatric illnesses at local community mental health centers (e.g., pharmacological treatment, case management, supportive counseling, psychiatric rehabilitation), which they continued to receive throughout the study. No other interventions were provided at the centers that specifically targeted PTSD during the course of these studies (e.g., cognitive restructuring or exposure therapy), although some supportive counseling for trauma-related problems was available.
2.3.1. Cognitive behavioral therapy (CBT)
CBT was provided in an individualized format and was comprised of three sessions teaching breathing retraining for anxiety, safety planning, and psychoeducation about trauma and PTSD, followed by 9–13 sessions of cognitive restructuring (i.e., identifying and correcting incorrect thoughts or beliefs contributing to upsetting feelings). Cognitive restructuring was applied to thoughts arising from day-to-day life as well as trauma-related thoughts and beliefs. The program included handouts, worksheets, and homework assignments adapted to fit the needs of individuals with severe mental illness. A more detailed description of the program is provided in Mueser et al. (2009).
2.3.2. Treatment as usual (TAU)
The comparison condition in Study 1 was TAU, in which clients continued to receive usual services from their local community mental health centers.
2.3.3. Brief intervention
The 3-session Brief program content was based on the first three sessions of the CBT program (Nishith et al., 2015). It involved breathing retraining and psychoeducation about trauma and PTSD, and utilized a video to facilitate discussion about PTSD, but did not involve cognitive restructuring.
In Study 1, CBT was provided mainly by academically trained Ph.D. level clinicians, whereas in Study 2 CBT and the Brief intervention were provided by front-line, mainly Masters level, clinicians. A portion of sessions were randomly reviewed for fidelity and adherence; results are reported elsewhere (Lu et al., 2014; Mueser et al., 2012) and generally indicated high fidelity and adherence.
2.4. Feasibility and tolerability
2.4.1. Feasibility
Rates of treatment initiation, exposure, and dropout in each condition were examined to evaluate feasibility. Initiation of CBT or Brief was defined a priori as completing at least 1 treatment session. Exposure to CBT was defined a priori as completion of at least 6 sessions. Exposure to the Brief treatment was defined a priori as completion of at least 2 of the 3 sessions. Treatment drop-out was defined as having initiated treatment but not meeting the threshold for exposure.
2.4.2. Tolerability
Rates of symptom exacerbation on the CAPS from baseline to post-treatment were examined to evaluate treatment tolerability. Using the same method to define a symptom exacerbation as van den Berg et al. (2015b), the CAPS cutoff for reliable exacerbation was calculated to be 15.86 points for Study 1 and 12.19 points for Study 2. Symptom exacerbations were only evaluated in individuals who completed at least one session.
2.5. Statistical analysis
Intent-to-treat analyses were conducted using mixed-effects linear regressions model continuous outcomes, and generalized linear models for dichotomous outcomes to evaluate the effect of CBT on the outcomes. Baseline was included as a covariate in these models, with post-treatment and follow-up assessments entered as repeated dependent variables. Treatment group, time, and group by time interaction were included as independent variables. Cross-time correlations were freely estimated using an unstructured variance-covariance matrix. Between group effect sizes (Cohen’s d) were calculated based on the average difference between the groups across all post-treatment and follow-up assessments, adjusting for baseline. To assess time effects, we conducted mixed-effects linear regression models and generalized linear models in which all time points, including baseline, were included as dependent variables. In Study 2, only group analyses were conducted for the number of BPD symptoms as assessed by the SCID-II given the varying time frames used for baseline versus post-treatment and follow-up assessments. χ2 analyses and t-tests were used to compare baseline characteristics and rates for feasibility and tolerability analyses.
3. Results
3.1. Baseline characteristics
No demographic, clinical, or functional differences were found between the groups at baseline.
3.2. Feasibility
Initiation of treatment was high in both studies (Study 1: CBT 14/15, 93.3%; Study 2: CBT 27/29, 93%, Brief 23/26, 88%). Among participants who initiated treatment, exposure rates were moderately high (Study 1: CBT 12/14, 85.7%; Study 2: CBT 20/27, 74%; Brief 20/23, 87%) and on par with rates for the entire sample (Study 1: CBT 81%; Study 2: CBT 73%, Brief 94%). In Study 2, the exposure rate did not differ significantly between groups (χ2(1, n = 50) = 1.29, p = .26). The dropout rate for CBT in Study 1 was 14.3% (2/14), CBT in Study 2 was 26% (7/27), and Brief in Study 2 was 13% (3/23). In Study 2, the participants who dropped out of the study did not differ from those who did not drop out on demographic or clinical characteristics (this was not assessed in Study 1 due to limited sample size).
3.3. Tolerability
Rates of symptom exacerbation on the CAPS from baseline to post-treatment were low (Study 1: CBT 1/8, 12.5%, TAU 0/5, 0%; Study 2: CBT 2/23, 9%, Brief 1/17, 6%), and did not significantly differ between groups (Study 2: χ2(1, n = 40) = 0.11, p = .74).
3.4. Primary outcomes
3.4.1. Study 1
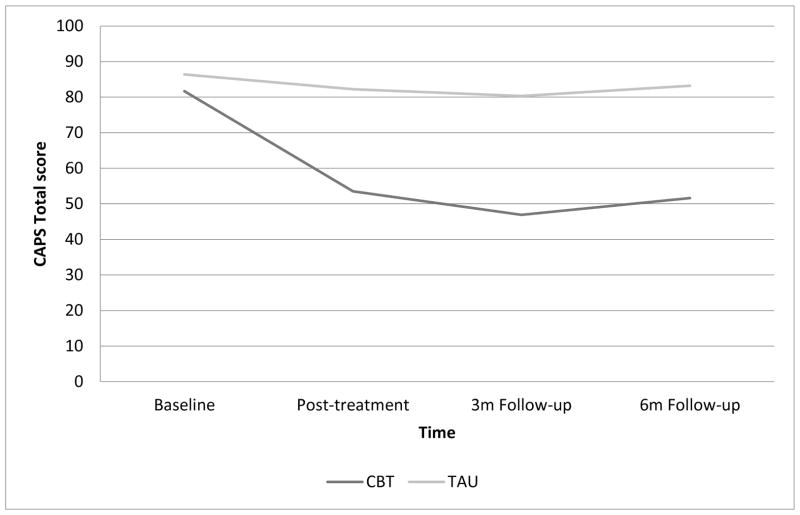
Significant treatment group effects favoring CBT over TAU for CAPS Total (F(1, 19.8) = 7.02, p = .02; Figure 1) and the CAPS re-experiencing subscale (F(1, 16.6) = 7.20, p = .02), and trends for the other two CAPS subscales (avoidance (F(1, 18.1) = 3.33, p = .08) and hyperarousal (F(1, 19.6) = 4.10, p = .06)) were observed. The effect size for CBT vs. TAU for CAPS Total was large (d = 1.07). Significant group effects favoring CBT over TAU were also observed for severe PTSD diagnostic status when controlling for baseline (Wald χ2(1, n = 27) = 4.69, p = .03; Supplemental Figure 1) and PTSD diagnosis (Wald χ2(1, n = 27) = 6.98, p = .01). The difference between the two groups in PTSD knowledge was not significant (F(1, 14.53) = 0.49, p = .50), nor were any of the group by time interactions.
Figure 1.
PTSD symptom severity scores across time for CBT vs. TAU groups (Study 1).
Examination of time effects for the combined CBT and TAU groups indicated significant improvements over time for CAPS Total (F(3, 11.8)= 5.15, p < .05) and all subscales: avoidance (F(3, 13.0) = 5.58, p = .01), hyperarousal (F(3, 17.1) = 7.54, p = .002), and re-experiencing (F(3, 191.0) = 8.22, p < .001). Significant time effects were also observed for PTSD diagnosis (Wald χ2(3, n = 27) = 13.11, p = .004), severe PTSD diagnosis (Wald χ2(3, n = 27) = 15.91, p = .001), and PTSD knowledge (F(3, 62.8) = 4.33, p = .008).
3.4.2. Study 2
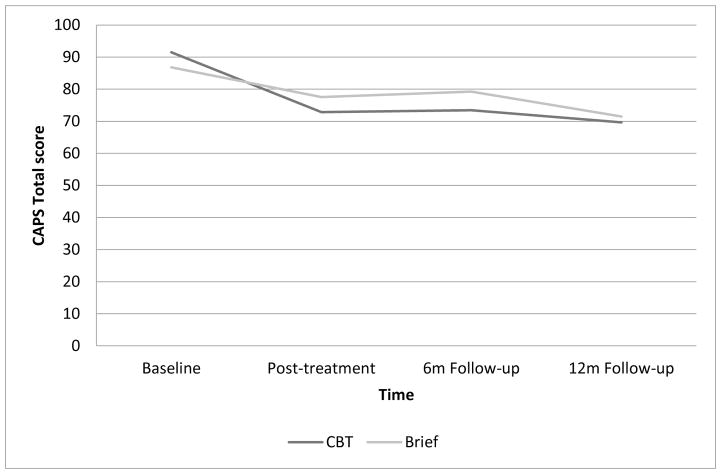
A significant group effect was observed for CBT over Brief on PTSD knowledge (F(1, 48.3) = 4.10, p < .05; Supplemental Figure 2). There was a trend level effect for CAPS Total (F(1, 53.8) = 3.53, p = .07; Figure 3), with a small-moderate effect size (d = .40). The groups did not differ significantly on the CAPS subscales (ps > .12) or PTSD or severe PTSD diagnosis (ps > .52), nor were any of the group by time interactions significant.
Figure 3.
PTSD symptom severity scores over time in CBT vs. Brief groups (Study 2).
Examination of time effects for the two groups combined indicated significant reductions on CAPS Total (F(3, 46.8) = 11.32, p < .001), and all subscales: avoidance (F(3, 44.3) = 9.70, p < .001), hyperarousal (F(3, 48.0) = 2.85, p = .047), and re-experiencing (F(3, 47.4) = 9.10, p < .001). A significant time effect was observed for PTSD diagnosis (Wald χ2(3, n = 55) = 18.61, p < .001) and severe PTSD diagnosis (Wald χ2(3, n = 55) = 36.30, p < .001). There was also a trend level improvement in PTSD knowledge over time (F(3, 40.0) = 2.64, p = .06).
3.5. Secondary outcomes
3.5.1. Study 1
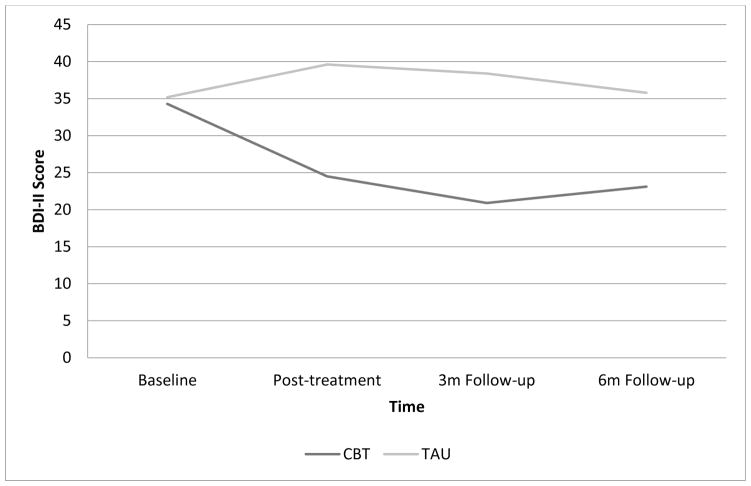
Significant group effects favoring CBT over TAU on depression (F(1,16.7) = 10.27, p = .005; Figure 2) and the physical component of the SF-12 (F(1, 11.6) = 9.88, p = .009) were observed. Group effects were not significant for any other variables, nor were any of the group by time interactions.
Figure 2.
Depressive symptoms over time in CBT vs. TAU groups (Study 1).
Analyses of secondary outcomes for the CBT and TAU groups combined indicated a worsening in general psychiatric symptoms on the BPRS over time (F(3, 11.1) = 11.73, p = .001); inspection of the means indicated that this was due to worsening scores in the TAU group but not the CBT group. The time effect was not significant for any other variables.
3.5.2. Study 2
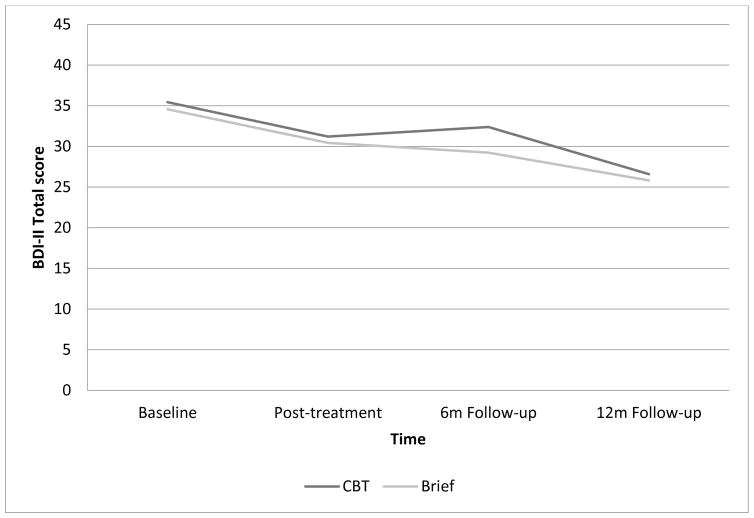
No significant group effects (ps > .16) or group by time interactions were observed for the secondary outcomes.
Analyses of secondary outcomes for both groups combined indicated significant improvements over time on posttraumatic cognitions (F(3, 43.7) = 5.28, p < .01), depressive symptoms (F(3, 41.9) = 7.73, p < .001; Figure 4), and overall functioning (F(3, 42.4) = 6.13, p = .001), and trend level improvement for anxiety symptoms (F(3, 42.7) = 2.72, p = .056) and quality of life (F(3, 43.1) = 2.74, p = .055). Time effects were not significant for the other secondary outcomes.
Figure 4.
Depressive symptoms over time in CBT vs. Brief groups (Study 2).
Descriptive statistics and effect sizes for all outcomes are summarized in Tables 2–5.
Table 2.
Primary Outcomes of CBT and TAU Groups (Study 1)
| Mean (s.d.) or %, n | Treatment group effect | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Primary Outcomes | Group | Baseline | Post-treatment | 3 months | 6 months | F (df)/ Wald χ2 (df, n) | p- value | Effect size |
| PTSD symptom severity (CAPS total)* | CBT | 81.7 (18.2) | 53.5 (31.7) | 46.9 (21.9) | 51.6 (29) | 7.02 (1, 19.81) | 0.02 | 1.07 |
| TAU | 86.4 (15.8) | 82.2 (25.8) | 80.3 (25.1) | 83.2 (13.8) | ||||
| CAPS - re- experiencing symptoms* | CBT | 23.3 (7.3) | 15.5 (8.9) | 9.3 (5.6) | 14.5 (10.4) | 7.20 (1, 16.63) | 0.02 | 1.17 |
| TAU | 22.4 (7.1) | 25.6 (8.1) | 23.1 (12.8) | 23.6 (8.2) | ||||
| CAPS - hyperarousal symptoms* | CBT | 26.3 (6.7) | 17.8 (12.1) | 18.1 (7.8) | 17.4 (10.6) | 4.10 (1, 19.6) | 0.06 | 0.71 |
| TAU | 27.8 (6.0) | 26.8 (11.4) | 26.1 (8.9) | 24.4 (6.0) | ||||
| CAPS - avoidance symptoms* | CBT | 32.1 (9.1) | 20.3 (13.6) | 19.4 (12) | 19.7 (12.7) | 3.33 (1, 18.06) | 0.08 | 0.76 |
| TAU | 36.3 (8.9) | 29.8 (8.2) | 31.0 (10.7) | 35.2 (5.8) | ||||
| PTSD diagnosis (%,n)* | CBT | 100, 15 | 75, 6 | 28.57, 2 | 60, 6 | 6.98 (1, n = 27) | 0.01 | 0.75 |
| TAU | 100, 12 | 80, 4 | 87.5, 7 | 100, 5 | ||||
| Severe PTSD diagnosis (%, n)* | CB T | 86.67, 15 | 37.50, 3 | 28.57, 2 | 40.00, 4 | 4.69 (1, n = 27) | 0.03 | 0.79 |
| TAU | 91.67, 11 | 80.00, 4 | 62.50, 5 | 100, 5 | ||||
| PTSD knowledge* | CBT | 9.9 (3.5) | 10.4 (2.8) | 11.1 (2.3) | 10.1 (2.4) | 0.49 (1, 14.53) | 0.50 | 0.31 |
| TAU | 10.4 (2.1) | 10 (1.4) | 9.3 (2.4) | 11.2 (0.8) | ||||
Time effects observed
Table 5.
Secondary Outcomes of CBT and Brief Treatment Groups (Study 2)
| Mean (s.d.) or %, n | Treatment group effect | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Secondary Outcomes | Group | Baseline | Post- treatment | 6 months | 12 months | F (df)/ Wald χ2 (df, n) | p-value | Effect size |
| Posttraumatic Cognitions Inventory* | CBT | 4.76 (0.97) | 4.20 (1.23) | 4.38 (1.17) | 4.21 (1.31) | 0.19 (1, 51.25) | 0.67 | −0.06 |
| Brief | 4.65 (0.91) | 4.21 (1.38) | 4.22 (1.37) | 3.82 (1.26) | ||||
| Beck Depression Inventory-II* | CBT | 35.45 (12.53) | 31.20 (14.49) | 32.38 (12.64) | 26.60 (14.63) | 0.51 (1, 50.31) | 0.48 | −0.05 |
| Brief | 34.58 (11.19) | 30.44 (17.38) | 29.25 (13.15) | 25.83 (13.67) | ||||
| Beck Anxiety Inventory | CBT | 34.32 (16.16) | 30.59 (15.58) | 34.50 (14.98) | 29.20 (17.46) | 1.10 (1, 50.14) | 0.30 | −0.07 |
| Brief | 32.46 (14.48) | 29.28 (16.23) | 30.25 (14.38) | 26.33 (18.21) | ||||
| PANSS Total | CBT | 68.74 (10.87) | 65.38 (15.25) | 69.68 (16.37) | 66.74 (14.83) | 1.01 (1, 39.28) | 0.32 | 0.24 |
| Brief | 66.58 (10.56) | 66.67 (12.41) | 70.13 (18.00) | 71.19 (21.82) | ||||
| Global Assessment of Functioning* | CBT | 47.61 (7.38) | 53.36 (8.28) | 50.04 (9.70) | 53.04 (8.10) | 0.07 (1, 42.49) | 0.79 | 0.09 |
| Brief | 48.27 (8.26) | 52.72 (9.94) | 48.81 (10.74) | 53.65 (11.52) | ||||
| Quality of Life - General | CBT | 2.90 (1.46) | 3.44 (1.86) | 3.48 (1.46) | 3.72 (1.61) | 0.001 (1, 50.16) | 0.97 | 0.25 |
| Brief | 3.63 (1.21) | 4.00 (1.92) | 3.72 (1.73) | 3.97 (1.84) | ||||
| SCID II BPD Items | CBT | 6.14 (1.00)a | 3.32 (1.70) | 3.42 (2.17) | 3.24 (1.54) | 0.19 (1, 47.80) | 0.66 | −0.01 |
| Brief | 6.19 (1.10)a | 3.58 (2.48) | 3.81 (2.40) | 2.67 (2.14) | ||||
Time effects observed
Baseline SCID II was conducted for lifetime whereas post-treatment, 6 month, and 12 month follow ups were conducted for current symptoms.
4. Discussion
The feasibility, tolerability and effectiveness of a CBT for PTSD program designed for individuals with severe mental illness and co-occurring PTSD (Mueser et al., 2008; 2015) was examined in individuals with BPD in two randomized controlled trials conducted in typical mental health settings. The results indicated that CBT for PTSD was feasible to implement with this population, with high rates of initiation of and exposure to treatment and low rates of dropout. Participants with BPD tolerated the CBT intervention well, with low rates of PTSD symptom exacerbation across both studies.
In Study 1, individuals with BPD who received CBT had significantly greater reductions in PTSD symptoms and rates of PTSD and severe PTSD diagnosis than those in TAU. In Study 2, individuals with BPD who received CBT learned more about PTSD, and experienced greater reductions in PTSD symptoms at a trend level compared to those who received the Brief (3-session) intervention, which included only breathing retraining and psychoeducation. The general pattern of findings for the BPD subsample in Study 2 is consistent with findings from the full sample (Mueser et al., 2015), in which the Brief intervention was also associated with improvements in PTSD and other symptoms, diminishing between-group differences between it and CBT. In addition to the direct impact on PTSD symptoms, there was some evidence that CBT had a broader impact in the BPD sample, resulting in reduction of other symptoms, most notably depression. These findings are promising given the high rate of comorbidity between major depression and PTSD (Campbell et al., 2007) and BPD (Zanarini et al., 1998).
In both studies, participants in CBT experienced clinically significant improvements in PTSD symptoms, defined as a 15 point CAPS change (Weathers et al., 2001). In Study 1, participants improved approximately 30 points in CAPS from baseline to post-treatment and follow-ups, and in Study 2, the improvement was about 20 points. Nonetheless, the percentages of clients no longer meeting criteria for PTSD at the end of these two studies were relatively high. This is due, in part, to the fact that participants entered these studies with more severe symptoms (average CAPS = 82–91) than is typical with other effectiveness (Forbes et al., 2012; average CAPS = 70) or efficacy (e.g., Resick et al., 2002; average CAPS = 70–77) trials. Furthermore, the effect size for PTSD symptom severity compared to TAU in our study was large (d = 1.07) and greater than the mean effect size for PTSD psychotherapy studies with active comparison (TAU) groups reported in a recent meta-analysis (d = 0.92; Watts et al., 2013).
In general, rates of drop out from psychotherapy in PTSD and BPD populations are reported to be in 21–29% range (Bradley et al., 2005; Barnicot et al., 2011). Concerns about dropout have led to recommendations for staged treatment of individuals with co-occurring PTSD and BPD (Cloitre et al., 2012), although these recommendations have been questioned (de Jongh et al., 2016). The relatively low rates of dropout from the CBT for PTSD program for individuals across both of these studies (14% in Study 1, 26% in Study 2) supports the feasibility of providing this trauma-focused treatment without a prior treatment phase aimed at stabilization and affect regulation. All of the participants were receiving some form of treatment and support from their mental health center community clinic at entry into the study, and it is possible that some of these clients were clinically stable. However, only the most limited inclusion/exclusion criteria were used to determine study eligibility, and the severity of symptoms at baseline was high, suggesting that most participants were not clinically stable at study entry. For example, the majority of participants in both study samples endorsed active suicidal ideation on the BDI at baseline (Table 1).
In comparing dropout rates across the studies and conditions, the CBT dropout rate in Study 2 is higher than that of Study 1. This is likely due to the fact that in contrast to the rural settings for Study 1 and the majority of White participants, Study 2 was conducted in inner city, urban settings with a majority of African American participants, where high rates of non-attendance at outpatient psychiatric treatment are common. Differences in dropout and exposure rates between the Brief and CBT conditions in Study 2 are also likely due to differences in treatment length (3 versus 16 sessions), as well as differences in how exposure was defined for each treatment. The low rates of PTSD symptom exacerbation in the BPD clients who received CBT (13% in Study 1, 9% in Study 2) are comparable to the rates reported in PTSD studies with general population samples that received Prolonged Exposure (Tarrier et al., 1999: 26%), Skills Training in Affect and Interpersonal Regulation/exposure (Cloitre et al., 2010, 15%) or cognitive restructuring (Tarrier et al., 1999: 8%). This is particularly notable given that this sample represented a more complex population than past trials in that in addition to BPD and PTSD, all participants also met NH, VT, or NJ state criteria for a severe mental illness, which included receiving disability benefits (i.e., SSI or SSDI).
The CBT program utilized in this study (Mueser et al., 2009) is distinct from other trauma-focused treatments for PTSD and from stage-based treatments for comorbid PTSD and BPD, and may prove to be a viable alternative. The CBT program is most similar to Cognitive Processing Therapy (Resick et al., 2014) in that both approaches focus primarily on cognitive restructuring, but it differs in several important ways. First, the CBT program was initially designed for individuals with severe mental illness, and thus it accommodates for challenges such as cognitive impairment, higher sensitivity to stress, psychotic symptoms, and greater emotion dysregulation. For example, early on in treatment clients are taught breathing retraining to manage distress and engage in safety planning around suicidal ideation and intent. Second, the CBT program does not begin with participants writing narrative(s) of their traumatic event(s) and addressing cognitions about the trauma(s). The primary focus in the CBT program is on teaching cognitive restructuring as a self-management skill for dealing with negative emotions through identifying, examining, and changing associated inaccurate thoughts. This typically starts with upsetting non-trauma related thoughts then moves onto trauma-related thoughts later in treatment, as participants develop mastery over the cognitive restructuring skill. The CBT program also incorporates problem-solving training for addressing upsetting feelings in situations in which the underlying thoughts are found to be supported by the available evidence, and an action plan is called for to address that life circumstance. The latter component differs from other treatments for PTSD and may be particularly helpful for individuals with BPD, given the high rates of negative life events (Powers et al., 2013).
In comparison to staged approaches to treatment, the CBT program is considerably shorter in duration and initiates trauma-focused cognitive restructuring sooner. For example, the newly proposed combined Dialectical Behavior Therapy and Prolonged Exposure protocol (Harned et al., 2014) is designed to take place over one year and involves 4.5–5 hours of therapy per week (234–260 therapy hours total). In contrast, the CBT program requires 12–16 therapy hours. In addition, although the aim of Dialectical Behavior Therapy and Prolonged Exposure protocol is to treat PTSD earlier in treatment than traditional Dialectical Behavior Therapy, a staged approach is still employed, with trauma-focused work delayed until stabilization criteria are met, a process that took an average of five months in the most recent trial (Harned et al., 2014). In the CBT program, cognitive restructuring is initiated in session 4. Treatment duration is important to consider in that shorter programs both reduce burden on clients and mental health providers, and the time in which a client is living with PTSD symptoms. Also, unlike Dialectical Behavior Therapy and Prolonged Exposure or traditional Prolonged Exposure for PTSD, the CBT program does not involve an exposure component.
It is important to note some limitations of these analyses. Given that this was a secondary analysis, we were limited to the data available and thus were unable to examine some relevant outcomes. For example, given the high prevalence of suicidal behavior and non-suicidal self-injury in BPD (Black et al., 2004), we would have liked to examine these symptoms more closely. Nonetheless, our study was more inclusive than past trials (Clarke et al., 2008; Feeny et al., 2002) in that we included individuals with active suicidal ideation, suicidal intent, parasuicidal behavior, and non-suicidal self-injury. We were also limited in our ability to examine the impact of the treatments in Study 2 on BPD symptoms. Although this is of interest, the aim of the current treatment was not to target BPD symptoms, but PTSD symptoms. In addition, we were able to examine this question in Study 1 and did not observe a group or time effect, indicating that the treatment did not lead to improvements or decrements in BPD symptoms. This is reassuring as a concern could be that treating PTSD in this population without specifically targeting BPD symptoms could lead to exacerbation of BPD symptoms. Additionally, the frequency of assessments for examining exacerbations was relatively low and was not sensitive to exacerbations during the course of treatment. Given the results of these secondary analyses, a prospective randomized controlled trial with a larger sample of clients with comorbid PTSD and BPD, comprehensive measures, and more frequent assessments is warranted. There is also a need for additional research in this area due to the large percentage of participants who still retained a PTSD diagnosis at the end of treatment in the current studies, including comparing the current approach to exposure therapy or staged approaches that address suicidality or other symptoms prior to initiating trauma-focused work.
4.1. Implications
The results of the current analyses suggest that individuals with comorbid PTSD and BPD can tolerate and benefit from a non-staged trauma-focused CBT for PTSD. In our study, CBT was superior to TAU for reducing PTSD symptoms and improving PTSD knowledge in a comorbid PTSD, BPD, and severe mental illness sample. The cognitive restructuring component of CBT demonstrated some increased benefit in PTSD symptoms above the psychoeducation and breathing retraining provided in Brief treatment, although not significantly so given a surprisingly positive impact of the Brief intervention. In addition, in comparison to TAU, CBT also had a favorable impact on depression and self-reported physical health. The CBT treatment was feasible and well-tolerated in that the majority of participants, and few dropped out of treatment or experienced PTSD symptom exacerbations. Overall, these results provide support for further investigation of non-staged CBTs for PTSD in comorbid PTSD and BPD populations.
Supplementary Material
Table 3.
Secondary Outcomes of CBT and TAU Groups (Study 1)
| Mean (s.d.) or %, n | Treatment group effect | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Secondary Outcomes | Group | Baseline | Post-treatment | 3 months | 6 months | F (df)/ Wald χ2 (df, n) | p- value | Effect size |
| Posttraumatic Cognitions Inventory | CBT | 3.9 (1.1) | 3.9 (1.3) | 2.6 (1.3) | 2.8 (1.3) | 2.77 (1, 16.31) | 0.11 | 0.89 |
| TAU | 3.9 (1.2) | 4.5 (1.1) | 4.2 (1.5) | 3.7 (1.1) | ||||
| Beck Depression Inventory-II | CBT | 34.3 (11.2) | 24.5 (14.4) | 20.9 (13) | 23.1 (12.7) | 10.27 (1, 16.71) | 0.005 | 1.22 |
| TAU | 35.2 (15.4) | 39.6 (13.6) | 38.4 (13) | 35.8 (13) | ||||
| Beck Anxiety Inventory | CBT | 51.8 (16.3) | 41.9 (13.4) | 33 (8.3) | 43 (14.8) | 2.26 (1, 18.14) | 0.15 | 0.97 |
| TAU | 52.8 (11.2) | 50.2 (18.5) | 55.7 (17.3) | 48 (16.7) | ||||
| BPRS Total* | CBT | 43.3 (7.4) | 39 (8.7) | 37.9 (8.2) | 42 (7.6) | 1.06 (1, 14.89) | 0.32 | 0.65 |
| TAU | 47.5 (6.1) | 41.3 (8.3) | 51.5 (14.1) | 55.4 (18.3) | ||||
| SF-12 Physical Subscale | CBT | 42.0 (8.0) | 46.7 (9.2) | 42.9 (12.5) | 44.4 (12.6) | 9.88 (1, 11.55) | 0.009 | 1.64 |
| TAU | 44.0 (12.6) | 35.2 (14.1) | 32.3 (10.3) | 33.3 (12.3) | ||||
| SF-12 Mental Subscale | CBT | 29.7 (9.9) | 31.1 (8.2) | 33.3 (11) | 34.1 (8) | 1.39 (1, 10.48) | 0.26 | 0.49 |
| TAU | 27.9 (9.6) | 26.3 (4.5) | 27.3 (10) | 23.8 (11.3) | ||||
| SCID II BPD Items | CBT | 3.89 (2.2) | 1.17 (1.17) | 3.3 (2.3) | 2.86 (2.7) | 2.42 (1, 0.001) | 0.12 | 0.68 |
| TAU | 4.42 (2.2) | 4.25 (3.2) | 4.31 (2.6) | 4.88 (3.0) | ||||
Time effects observed
Table 4.
Primary Outcomes of CBT and Brief Treatment Groups (Study 2)
| Mean (s.d.) or %, n | Treatment group effect | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Primary Outcomes | Group | Baseline | Post- treatment | 6 months | 12 months | F (df)/ Wald χ2 (df, n) | p- value | Effect size |
| PTSD symptom severity (CAPS total)* | CBT | 91.52 (14.49) | 73.19 (25.67) | 72.81 (23.38) | 69.64 (27.97) | 3.53 (1, 53.81) | 0.07 | 0.40 |
| Brief | 86.81 (15.27) | 77.53 (25.31) | 79.25 (23.51) | 71.50 (26.30) | ||||
| CAPS–re- experiencing symptoms* | CBT | 23.66 (7.23) | 18.12 (9.56) | 18.00 (9.10) | 15.60 (11.65) | 0.61 (1, 54.28) | 0.44 | 0.14 |
| Brief | 23.88 (7.26) | 19.42 (8.49) | 18.94 (7.82) | 17.72 (8.00) | ||||
| CAPS–hyperarousal symptoms* | CBT | 27.34 (6.52) | 24.19 (9.36) | 22.62 (9.33) | 23.52 (10.12) | 1.41 (1, 54.31) | 0.24 | 0.31 |
| Brief | 26.85 (5.29) | 24.79 (8.69) | 27.25 (7.00) | 24.72 (9.40) | ||||
| CAPS–avoidance symptoms* | CBT | 40.52 (5.17) | 30.88 (11.85) | 32.19 (9.88) | 30.52 (11.68) | 2.43 (1, 53.49) | 0.13 | 0.45 |
| Brief | 35.96 (7.32) | 33.32 (11.17) | 33.06 (12.37) | 29.06 (12.18) | ||||
| PTSD diagnosis (%,n)* | CBT | 100, 29 | 76.92, 19 | 80.77, 19 | 72.00, 18 | 0.41 (1, n = 55) | 0.52 | 0.16 |
| Brief | 100, 26 | 89.47, 17 | 81.25, 13 | 77.78, 14 | ||||
| Severe PTSD diagnosis (%, n)* | CBT | 100, 29 | 69.23, 17 | 65.38, 16 | 60.00, 15 | 0.07 (1, n = 55) | 0.80 | 0.06 |
| Brief | 100, 26 | 73.68, 14 | 68.75, 11 | 61.11, 11 | ||||
| PTSD knowledge | CBT | 9.79 (2.73) | 10.79 (2.23) | 10.96 (2.44) | 10.28 (2.26) | 4.10 (1, 48.33) | 0.048 | 0.48 |
| Brief | 10.27 (2.22) | 10.17 (1.98) | 10.06 (2.26) | 9.72 (2.67) | ||||
Time effects observed
Highlights.
PTSD in borderline personality disorder (BPD) can be treated effectively with CBT.
CBT was feasible to provide and well tolerated by persons with severe BPD and PTSD.
In 2 studies, CBT reduced PTSD symptoms more than in the control groups.
Treatment benefits lasted for follow-up periods ranging from 6 to 12 months.
PTSD can be treated with CBT in BPD patients without a stabilization phase.
Acknowledgments
This work was supported by the National Institutes of Health [R01MH064662, F31MH103969, F31MH100773] and the Center for Substance Abuse Prevention.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barnicot K, Katsakou C, Marougka S, Priebe S. Treatment completion in psychotherapy for borderline personality disorder – a systematic review and meta-analysis. Acta Psychiat Scand. 2011;123:327–338. doi: 10.1111/j.1600-0447.2010.01652.x. http://dx.doi.org/10.1111/j.1600-0447.2010.01652.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the Beck Anxiety Inventory. Psychological Corporation; San Antonio, TX: 1990. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. Psychological Corporation; San Antonio, TX: 1996. [Google Scholar]
- Black DW, Blum N, Pfohl B, Hale N. Suicidal behavior in borderline personality disorder: prevalence, risk factors, prediction, and prevention. J Pers Disord. 2004;18:226–239. doi: 10.1521/pedi.18.3.226.35445. http://dx.doi.org/10.1521/pedi.18.3.226.35445. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Charney DS, Keane TM. Clinician Administered PTSD Scale for DSM-IV. National Center for Posttraumatic Stress Disorder; Boston, MA: 1995. [DOI] [PubMed] [Google Scholar]
- Bolton EE, Mueser KT, Rosenberg SD. Symptom correlates of posttraumatic stress disorder in clients with borderline personality disorder. Compr Psychiat. 2006;47:357–361. doi: 10.1016/j.comppsych.2005.12.002. http://dx.doi.org/10.1016/j.comppsych.2005.12.002. [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiat. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. http://dx.doi.org/10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Campbell DG, Felker BL, Liu CF, Yano EM, Kirchner JE, Chan D, … Chaney EF. Prevalence of depression–PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. J Gen Intern Med. 2007;22:711–718. doi: 10.1007/s11606-006-0101-4. http://dx.doi.org/10.1007/s11606-006-0101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chard KM. An evaluation of cognitive processing therapy for the treatment of posttraumatic stress disorder related to childhood sexual abuse. J Consult Clin Psychol. 2005;73:965–971. doi: 10.1037/0022-006X.73.5.965. http://dx.doi.org/10.1037/0022-006X.73.5.965. [DOI] [PubMed] [Google Scholar]
- Clarke SB, Rizvi SL, Resick PA. Borderline personality characteristics and treatment outcome in cognitive-behavioral treatments for PTSD in female rape victims. Behav Ther. 2008;39:72–78. doi: 10.1016/j.beth.2007.05.002. http://dx.doi.org/10.1016/j.beth.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M, Courtois C, Ford J, Green B, Alexander P, Briere J, … Spinazzola J. The ISTSS expert consensus treatment guidelines for complex PTSD in adults. 2012 Retrieved from www.istss.org.
- Cloitre M, Stovall-McClough KC, Nooner K, Zorbas P, Cherry S, Jackson CL, … Petkova E. Treatment for PTSD related to childhood abuse: A randomized controlled trial. Am J Psychiat. 2010;167:915–924. doi: 10.1176/appi.ajp.2010.09081247. http://dx.doi.org/10.1176/appi.ajp.2010.09081247. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JR, Hughes DC, Swartz MS, Blazer DG, George LK. The impact of borderline personality disorder on post-traumatic stress in the community: A study of health status, health utilization, and functioning. Compr Psychiatry. 2002;43:41–48. doi: 10.1053/comp.2002.29846. http://dx.doi.org/10.1053/comp.2002.29846. [DOI] [PubMed] [Google Scholar]
- de Jongh A, Resick P, Zoellner LA, van Minnen A, Lee CW, Monson CM, … Rauch SA. A critical analysis of the current treatment guidelines for complex PTSD in adults. Depress Anxiety. 2016;33:359–369. doi: 10.1002/da.22469. http://dx.doi.org/10.1002/da.22469. [DOI] [PubMed] [Google Scholar]
- Feeny NC, Zoellner LA, Foa EB. Treatment outcome for chronic PTSD among female assault victims with borderline personality characteristics: A preliminary examination. J Personal Disord. 2002;16:30–40. doi: 10.1521/pedi.16.1.30.22555. http://dx.doi.org/10.1521/pedi.16.1.30.22555. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis-I Disorders–Patient Edition (SCID-I/P , Version 2.0) New York State Psychiatric Institute; 1996a. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. User’s guide for the structured clinical interview for DSM-IV personality disorders (SCID-II) Washington, DC: 1996b. [Google Scholar]
- Foa EB, Ehlers A, Clark DM, Tolin DF, Orsillo SM. The posttraumatic cognitions inventory (PTCI): Development and validation. Psychol Assessment. 1999;11:303. http://dx.doi.org/10.1037/1040-3590.11.3.303. [Google Scholar]
- Forbes D, Lloyd D, Nixon RDV, Elliott P, Varker T, Perry D, … Creamer M. A multisite randomized controlled effectiveness trial of cognitive processing therapy for military-related posttraumatic stress disorder. J Anxiety Disord. 2012;26:442–452. doi: 10.1016/j.janxdis.2012.01.006. http://dx.doi.org/10.1016/j.janxdis.2012.01.006. [DOI] [PubMed] [Google Scholar]
- Frías Á, Palma C. Comorbidity between post-traumatic stress disorder and borderline personality disorder: A review. Psychopath. 2015;48:1–10. doi: 10.1159/000363145. http://dx.doi.org/10.1159/000363145. [DOI] [PubMed] [Google Scholar]
- Gearon JS, Bellack AS, Tenhula WN. Preliminary reliability and validity of the Clinician-Administered PTSD Scale for schizophrenia. J Consult Clin Psychol. 2004;72:121–25. doi: 10.1037/0022-006X.72.1.121. http://dx.doi.org/10.1037/0022-006X.72.1.121. [DOI] [PubMed] [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, … Ruan WJ. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiat. 2008;69:533–545. doi: 10.4088/jcp.v69n0404. http://dx.doi.org/10.4088/JCP.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green BL. Trauma History Questionnaire. In: Stamm BH, editor. Measurement of Stress, Self-Report Trauma, and Adaptation. Sidran Press; Lutherville, MD: 1996. [Google Scholar]
- Harned MS, Korslund KE, Linehan MM. A pilot randomized controlled trial of Dialectical Behavior Therapy with and without the Dialectical Behavior Therapy Prolonged Exposure protocol for suicidal and self-injuring women with borderline personality disorder and PTSD. Behav Res Ther. 2014;55:7–17. doi: 10.1016/j.brat.2014.01.008. http://dx.doi.org/10.1016/j.brat.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones SH, Thornicroft G, Coffey M, Dunn G. A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning (GAF) Brit J Psychiat. 1995;166:654–659. doi: 10.1192/bjp.166.5.654. http://dx.doi.org/10.1192/bjp.166.5.654. [DOI] [PubMed] [Google Scholar]
- Kay SR, Flszbein A, Opfer LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bulletin. 1987;13:261. doi: 10.1093/schbul/13.2.261. http://dx.doi.org/10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Leisen MB, Kaplan AS, Watson SB, Haynes SN, Owens JA, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychol Assessment. 2000;12:210. doi: 10.1037//1040-3590.12.2.210. http://dx.doi.org/10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Lehman A, Kernan E, Postrado L. Toolkit for Evaluating Quality of Life for Persons with Severe Mental Illness. The Evaluation Center at HSRI; 1995. [Google Scholar]
- Lu W, Yanos PT, Gottlieb JD, Duva SM, Silverstein SM, Xie H, … Mueser KT. Using fidelity assessments to train frontline clinicians in the delivery of cognitive-behavioral therapy for PTSD in persons with serious mental illness. Psychiatr Serv. 2012;63:785. doi: 10.1176/appi.ps.201000458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukoff D, Nuechterlein KH, Ventura J. Manual for the expanded Brief Psychiatric Rating Scale (BPRS) Schizophr Bull. 1986;12:594–602. [Google Scholar]
- Mueser KT, Gottlieb JD, Xie H, Lu W, Yanos PT, Rosenberg SD, … McHugo GJ. Evaluation of cognitive restructuring for post-traumatic stress disorder in people with severe mental illness. Brit J Psychiat. 2015;206:501–508. doi: 10.1192/bjp.bp.114.147926. http://dx.doi.org/10.1192/bjp.bp.114.147926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueser KT, Rosenberg SD, Rosenberg HJ. Treatment of posttraumatic stress disorder in special populations: A cognitive restructuring program. American Psychological Association; Washington, DC: 2009. [Google Scholar]
- Mueser KT, Rosenberg SD, Xie H, Jankowski MK, Bolton EE, Lu W, … Wolfe R. A randomized controlled trial of cognitive-behavioral treatment for posttraumatic stress disorder in severe mental illness. J Consult Clin Psychol. 2008;76:259. doi: 10.1037/0022-006X.76.2.259. http://dx.doi.org/10.1037/0022-006X.76.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishith P, Mueser KT, Morse GA. A brief intervention for posttraumatic stress disorder in persons with a serious mental illness. Psychiat Rehabil J. 2015;38:314–19. doi: 10.1037/prj0000158. http://dx.doi.org/10.1037/prj0000158. [DOI] [PubMed] [Google Scholar]
- Powers AD, Gleason ME, Oltmanns TF. Symptoms of borderline personality disorder predict interpersonal (but not independent) stressful life events in a community sample of older adults. J Abnorm Psychol. 2013;122:469. doi: 10.1037/a0032363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pratt SI, Rosenberg S, Mueser KT, Brancato J, Salyers M, Jankowski MK, Descamps M. Evaluation of a PTSD psychoeducational program for psychiatric inpatients. J Ment Health. 2005;14:121–127. http://dx.doi.org/10.1080/09638230500066356. [Google Scholar]
- Resick PA, Monson CM, Chard KM. Cognitive processing therapy Veteran/military version: Therapist's manual. Department of Veterans' Affairs; Washington, DC: 2014. [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. J Consult Clin Psychol. 2002;70:867. doi: 10.1037//0022-006x.70.4.867. http://dx.doi.org/10.1037/0022-006X.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skodol AE, Gunderson JG, McGlashan TH, Dyck IR, Stout RL, Bender DS, … Oldham JM. Functional impairment in patients with schizotypal, borderline, avoidant, or obsessive-compulsive personality disorder. Am J Psychiat. 2002;159:276–283. doi: 10.1176/appi.ajp.159.2.276. http://dx.doi.org/10.1176/appi.ajp.159.2.276. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Pilgrim H, Sommerfield C, Faragher B, Reynolds M, Graham E, Barrowclough C. A randomized trial of cognitive therapy and imaginal exposure in the treatment of chronic posttraumatic stress disorder. J Consult Clin Psychol. 1999;67:13–18. doi: 10.1037//0022-006x.67.1.13. http://dx.doi.org/10.1037/0022-006X.67.1.13. [DOI] [PubMed] [Google Scholar]
- Van den Berg DPG, de Bont PAJM, van der Vleugel BM, de Roos A, de Jongh A, van Minnen A, van der Gaag M. Prolonged exposure versus eye movement desensitization and reprocessing versus waiting list for posttraumatic stress disorder in patients with a psychotic disorder. JAMA Psychiatry. 2015a;72:259–67. doi: 10.1001/jamapsychiatry.2014.2637. [DOI] [PubMed] [Google Scholar]
- van den Berg DP, de Bont PA, van der Vleugel BM, de Roos C, de Jongh A, van Minnen A, van der Gaag M. Trauma-focused treatment in PTSD patients with psychosis: Symptom exacerbation, adverse events, and revictimization. Schizophr Bull. 2015b doi: 10.1093/schbul/sbv172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Keller SD. SF-36 physical and mental health summary scales: A user’s manual. Health Assessment Lab; Boston, MA: 1994. [Google Scholar]
- Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, Friedman MJ. Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. J Clin Psychiat. 2013;74:e541–550. doi: 10.4088/JCP.12r08225. http://dx.doi.org/10.4088/JCP.12r08225. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: A review of the first ten years of research. Depress Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. http://dx.doi.org/10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychol Assess. 1999;11:124–33. [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, Reynolds V. Axis I comorbidity of borderline personality disorder. Am J Psychiat. 1998;155:1733–1739. doi: 10.1176/ajp.155.12.1733. http://dx.doi.org/10.1176/ajp.155.12.1733. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.