Abstract
Alcohol, the most widely used substance among men who have sex with men (85%), remains an important factor in HIV research among this high-risk population. However, research on alcohol use among Black and Latino men who have sex with men (BLMSM), a population disproportionately affected by HIV in the United States, is limited and inconclusive. This study explored sociodemographic and HIV risk with daily heavy and low-risk drinking patterns among BLMSM. BLMSM (N = 188) aged 18 to 40 years were recruited through social media, local colleges, heteronormative clubs, private men’s groups, gay establishments, and organized events in Los Angeles County. Participants completed self-administered questionnaires. Fisher’s exact tests revealed significant relationships between drinking patterns and condomless insertive anal intercourse (p = .001), race (p < .001), age (p = .02), and perception of alcohol-related HIV risk (p = .007). The Fisher’s exact tests findings for age held true in the multiple regression model (p = .014). Findings suggest that BLMSM who engage in higher risk drinking also engage in alcohol-related HIV risk. Culturally competent interventions should consider including a combined focus to explore the synergy between risky drinking patterns and HIV risk among BLMSM.
Keywords: men of color, sexual health, gay health issues, alcohol use, risk behaviors
Introduction
Alcohol, the most widely used substance among men who have sex with men or (MSM; 85%), remains an important factor in HIV research among this high-risk population (Stall et al., 2001; Thiede et al., 2003; Wong, Kipke, & Weiss, 2008). Alcohol use rates among MSM are as high as the general male population and higher than men who have sex with women (Greene et al., 2014; Stall et al., 2001). Alcohol use may especially affect ethnic minorities among MSM such as African Americans and Latinos (Zapolski, Pedersen, McCarthy, & Smith, 2014). African American and Latino men face greater health and social consequences, despite drinking less, overall than non-Hispanic Whites (Zapolski et al., 2014; Zemore, Mulia, Ye, Borges, & Greenfield, 2009). Among these consequences, the impact of alcohol use on condomless sexual intercourse among Black and Latino men who have sex with men (BLMSM), the ethnicities of MSM most affected by HIV in the United States, is understudied. Combined, young BLMSM represent over 54% of all new HIV cases among MSM in the United States (Centers for Disease Control and Prevention, 2012). There have been theories developed over the past decades that explain a direct relationship between HIV risk and alcohol consumption from a behavioral psychological standpoint such as the alcohol myopia theory developed by Steele and Josephs (1990) and the alcohol expectancy theory (Fromme, D’Amico, & Katz, 1999; Mullens, Young, Dunne, & Norton, 2011; Weinhardt & Carey, 2000). While research has identified a positive relationship between alcohol use and HIV risk, a positive relationship is not consistently reported (Sander et al., 2013; Vosburgh, Mansergh, Sullivan, & Purcell, 2012; Woolf & Maisto, 2009). Though many studies have reported a relationship between alcohol misuse and sexually risky behaviors among MSM, the results are not conclusive. HIV is primarily transmitted through condomless anal intercourse (CAI; Centers for Disease Control and Prevention, 2012). This article will explore multiple daily drinking behaviors and their relationship to HIV risk, and demographic variables among BLMSM.
When comparing HIV risk between different stages of development, young MSM are at highest risk for HIV and are also more likely to misuse alcohol than their older counterparts (Zeigler et al., 2005).1 Because youth are generally less experienced with alcohol use when compared with older adults, they are more likely to become more easily impaired by alcohol than adults (Cherpitel, 1993; Keall, Frith, & Patterson, 2004; Peck, Gebers, Voas, & Romano, 2008). Not only are youth more likely to be impaired by alcohol than older adults, drinking is reported highest among youth in their late teens and early 20s (Bachman, Schulenberg, O’Malley, Wadsworth, & Johnston, 1996; Wong et al., 2008).
Although differences in drinking patterns have been identified between different stages of development, differences between Black MSM and Latino MSM have not been highlighted in the literature. Moreover, variability of social, cultural, and biological factors reported between individuals even within racial and ethnic groupings diminishes the differences reported between different ethnicities (Eaton et al., 2012; Newcomb, 2013). However, studies consistently report ethnic minorities such as African Americans and Latinos, in general, experiencing greater morbidity, mortality, and social consequences from their alcohol consumption as well as slightly lower consumption rates than their White or Caucasian counterparts (Chartier, Vaeth, & Caetano, 2014; Irwin, 2005; Mutchler, McDavitt, & Gordon, 2014; Wong et al., 2008; Zapolski et al., 2014; Zeigler et al., 2005). In addition, heavy drinking trends have slightly increasing and stabilized among Black and Latino men, respectively, while decreasing substantially among White men (Caetano & Clark, 1998; Eaton et al., 2012; Keyes & Miech, 2013). Zapolski et al. (2014) investigated the reasons why African Americans may drink less overall than their White counterparts, but experience greater negative social consequences. They theorized that African American culture, lower socioeconomic status, religiosity, legal problems, and a genetic factor (that approximately 33% of African Americans carry) were protective against heavy alcohol use. Protective factors against drinking such as familism, adherence to traditional family values, and being less acculturated to the United States may also limit daily alcohol use among some Latinos (Castro, Stein, & Bentler, 2009). Recent findings by Gilbert, Daniel-Ulloa, and Conron (2015) have reported that Black MSM had lower hazardous drinking rates than their heterosexual counterparts, whereas Latino MSM had greater binge drinking rates their heterosexual counterparts. Given this finding, it will be important to test the relationship between drinking patterns and race to see if young BLMSM in Los Angeles also exhibit these differences when compared to one another.
A plethora of literature indicates that heavy drinking poses greater health risks (including risky sexual behavior) than nonheavy drinking (Mustanski, 2008; Ramirez-Valles, Garcia, Campbell, Diaz, & Heckathorn, 2008; Woolf & Maisto, 2009). Additionally, event level analysis suggests binge drinking, a form of heavy drinking, increases sexual risk taking among MSM when done before or during sex (Irwin, 2005; Vosburgh et al., 2012). However, most of the literature only describes drinking patterns and sexual risk behaviors among the general population of MSM and much less among ethnic minorities like BLMSM. Although the literature on alcohol use and HIV risk among young MSM is growing, there is a scarcity of literature focusing specifically on heavy drinking, and nonheavy drinking patterns as well as HIV risk (CAI) among younger BLMSM and their effect on sexual risk taking (Irwin, 2005; Mutchler et al., 2014; Ramirez-Valles, Garcia, Campbell, Diaz, & Heckathorn, 2008; Wong et al., 2008). Wong et al. (2008) studied alcohol use patterns among an ethnically diverse sample of MSM in Los Angeles and identified frequent binge drinking to be prevalent in this population. Mutchler et al. (2014) further supplemented these findings with interviews among BLMSM. The authors describe alcohol use and sexual risk behavior intentionally going hand in hand (see Mutchler et al., 2014 for details).
The current study explores the intersection between heavy and nonheavy drinking patterns, sociodemographics, and CAI among BLMSM. Due to the protective factors against heavy levels of consumption among Blacks and Latinos, and their inexperience with alcohol relative to older men, young BLMSM who consume nonheavy or low risk (0-4 drinks per typical drinking day) amounts of alcohol may have directly or indirectly related HIV risk. Research on the levels of alcohol use that impose health risks to the general population have been studied in efforts to help establish guidelines for “risky drinking”. In efforts to help inform such drinking guidelines, Di Castelnuovo et al. (2006) conducted a meta-analysis including 26 studies on alcohol use and health risk identified a threshold of 2.7 standard drinks (considered “low-risk” drinking by the National Institute of Alcohol Abuse and Alcoholism [NIAAA]., n.d.) to most commonly accompany health risks. In a different study, Thompson, Stockwell, and Macdonald (2012) reported a “J” or “U” shaped curve when plotting drinking categories against the dependent variable, health risk odds ratios. The “J” shaped curve was a result of the odds ratios for engaging in health compromising behaviors (i.e., drunk driving, engaged in self-harm, and condomless sex) decreasing between the categories “0 drinks per day” (abstinence) and “1 to 2 drinks per day,” and increasing between “1 to 2 drinks per day,” “3 to 4 drinks per day,” and “5 or more drinks per day” (heavy drinking) categories. These studies suggest that health risks and risky behaviors are variable for a given “daily drinking” range even among “low-risk” drinking as is defined by the NIAAA (n.d.; up to 4 drinks per day or less than 14 drinks per week). Furthermore, studies have reported that among African Americans, there may not be a “J” shaped curve that shows health benefits with low-level drinking, but rather a pattern of growing health risks with any level of alcohol consumption (Kerr, Greenfield, Bond, Ye, & Rehm, 2011). The protective factors against daily heavy drinking among Black and Latino men as well as their greater risk for alcohol-related disease, death, and social issues also point to the importance of investigating drinking behaviors among BLMSM at moderate and low levels of use in addition to heavy use. Given that social, psychological, and biological factors contribute to differences in alcohol susceptibility between individuals even of the same race and ethnicity (Wong et al., 2008; Zapolski et al., 2014), alcohol consumption at any level (including “low-risk” consumption as defined by the NIAAA, n.d.) has the potential to impair one’s motor skills and cognitive ability (Calhoun, Pekar, & Pearlson, 2004; Moskowitz & Fiorentino, 2000; Peterson, Rothfleisch, Zelazo, & Pihl, 1990).
The present study explores the relationship between CAI and daily low-risk and heavy drinking limits as established by the NIAAA (n.d.). An advantage of this study is that it explores whether or not NIAAA (n.d.) guidelines for daily low-risk and heavy drinking limits (guidelines that are used in differentiating drinking patterns in multiple drinking behavior instruments; Cummings, Cooper, & Johnson, 2013; Palfai, Winter, Lu, Rosenbloom, & Saitz, 2014; M. Ryan et al., 2013; Soderstrom et al., 1998) may hold as risk markers for CAI among BLMSM. To further tease out differences in CAI risk between low-risk daily drinkers, the low-risk drinking variable (DV) was divided into two range categories or patterns of drinking: higher low-risk drinking and lower low-risk drinking (detailed in the Method section). The CAI risk between each of the two low-risk drinking patterns was subsequently compared with the heavy drinking categories. Although Latino men and Black men are not a culturally cohesive group, the data were aggregated to strengthen the statistical power of the results as well as to test the relationship between race and drinking patterns in the current study given that only a few studies focus on describing alcohol use among this population. The findings from this study provide a better understanding on the patterns of drinking that place BLMSM at higher risk for HIV. Studying alcohol use patterns and risky sexual practice among BLMSM has the potential to inform early education efforts to prevent substance abuse and HIV among young Black and Latino men. The findings may specifically inform future studies and interventions in in an area of Los Angeles County where the population of Black and Latino men is concentrated and wheresubstance abuse-related morbidity is high. The study can also inform researchers and community interventions of whether or not there may be thresholds of drinking that indicate increased HIV risk that should be established for the BLMSM population.
Method
The data used in this study were obtained through the HIV status awareness model (HSAM) study (Washington, Robles, & Malotte, 2013). Data were collected in two waves, between March 2010 and July 2010, and between November 2010 and March 2011 using nonprobability sampling. To involve a diverse cadre of BLMSM, aged 18 to 40 years, participants were recruited through local magazine and Internet (e.g., Facebook©, Craigslist) advertisements; palm cards distributed at local colleges and universities; private men’s groups; flyers distributed outside gay establishments and heteronormative clubs frequented by a mixed crowd of heterosexual, bisexual, and homosexual patrons; gay, lesbian, bisexual, and transgender clubs and lounges; and organized events, such as gay pride festivals and private parties.
Individuals were eligible for the study if they (a) identified as Black/African American or Hispanic/Latino, (b) identified as male, (c) reported living in Los Angeles County, (d) reported oral or anal sex with a man within the preceding 6 months, (e) reported being HIV negative or having unknown HIV status, (f) did not indicate they were HIV positive elsewhere in the application, and (g) were English or Spanish speaking. Even though a survey translated in Spanish was offered, all participants requested the English version.
Participants recruited at clubs, bars, and gay pride events completed the survey in real time at the site venue or were given information to contact HSAM staff to take the survey in a more private setting. Other participants who responded to the advertisements as part of a private men’s group meeting completed the survey at the location of their group meeting administered by HSAM staff. A total of 203 participants completed the survey. The exclusion criteria for BLMSM in the HSAM study was not having reported any alcohol use or refusing to answer any of the survey questions used in the analysis. List-wise deletion was used to remove participants who had missing responses, resulting in a total sample size of N = 188 (Howell, 2007). All participants completed a consent form and asked to complete the survey, which took approximately 25 to 30 minutes. Each participant was given an unmarked envelope in which to place the completed survey. Participants were compensated $10. The institutional review board of the principal investigator’s home institution approved the study protocol.
Measures
The HSAM study survey was adapted from the Risk Behavior for Gay Men (RBGM) survey used by the Center for AIDS Prevention Services (Heckathorn, 1997; Koblin et al., 2003). Of the 200 items on the RBGM survey, 97 were completed by participants in the HSAM Study. Additional questions were added in the HSAM Study.
Alcohol Use
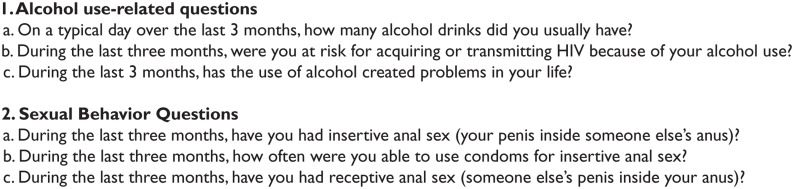
The RBGM survey included a continuous variable, which measured the number of alcohol drinks a participant consumed on a typical drinking day in the past 3 months (see Figure 1, 1a). The continuous DVused in the original RGBM and HSAM studies was recoded into the following categories for the present study: lower low-risk drinking (consuming 0 to 2 drinks per day), higher low-risk drinking (consuming more than 2, but less than or equal to 4 drinks per day), and heavy drinking (consuming more than 4 drinks per day). Low-risk or nonheavy daily drinking was defined by the NIAAA (n.d.) as consuming up to 4 alcoholic drinks on any day or consuming greater than or equal to 14 drinks per week. Heavy drinking was also defined by the NIAAA as drinking more than 4 drinks on a typical day or more than 14 drinks per week. However, the DV was limited to measuring daily heavy and low-risk drinking. The DV did not additionally predict weekly heavy drinking in accordance with NIAAA’s definition which takes daily and weekly drinking behaviors into consideration. Moving forward with a DV based on the NIAAA’s definition of heavy drinking on a typical day, the low-risk drinking category was divided into two further categories: lower low-risk or higher low-risk drinking. As young BLMSM may be susceptible to alcohol at any level, it was important to explore whether or not condomless anal intercourse or CAI was related to alcohol use patterns within the NIAAA definition of low risk drinking in addition to exploring the relationship between CAI and heavy drinking. Additional categorical variables were used to capture whether or not alcohol had created any problems in a participant’s life, and whether or not a participant perceived being at risk for acquiring or transmitting HIV risk because of their alcohol use (also referred to as alcohol-related HIV risk below; see Figure 1, 1b).
Figure 1.
Survey question bank for sexual behavior and alcohol-related questions.
Sexual Risk Behavior
The HSAM survey adapted in this study included items measuring the frequency of two types of sexual behaviors (condomless insertive anal intercourse [CIAI] and condomless receptive anal intercourse [CRAI]) and practices (frequency of condom use during sexual encounters) to establish sexual risk (see Figure 1, 2a-d). The survey specifically asked participants if they had insertive anal sex and receptive anal sex in the past 3 months. Sexual risk was defined as indicating that a condom was not used at least once during receptive or insertive anal intercourse in the past 3 months. (CIAI or CRAI; see Washington, Robles, & Malotte, 2013, for details).
Sociodemographic Variables
Participants reported the following: age, education level, and employment status. The response options for education were “less than high school,” “high school/GED,” and “at least some college.” For employment status, the response options were “full-time employed” and “part-time employed.” Data for whether or not a participant had got an HIV test in the past 12 months was also obtained.
Data Analysis
Descriptive analyses were conducted to estimate frequencies of the dependent variable, daily drinking patterns (lower low-risk, high low-risk, and heavy drinking), and the sample demographic variables, and other covariates. Fisher’s exact tests (FET) were conducted to examine an association between drinking patterns and the following categorical variables: age, race, educational level, employment status, alcohol-related problems, perceived alcohol-related HIV risk, CIAI, and CRAI.
Multiple regression analysis was run with drinking patterns as the dependent measure. The predictor variables included were as follows: age, race, educational level, employment status, alcohol-related problems, alcohol-related HIV risk, CIAI, and CRAI. The probability to enter the regression model was set at p < .25. Four predictor variables emerged. This generous criterion were used as a model building strategy as not all theoretically important predictors will have associations at the p < .05 level (Hosmer & Lemeshow, 2004). All analyses were performed using the statistical package PASW Statistics version 22 (SPSS).
Results
HSAM participant data were initially screened for those who consumed alcohol 3 months prior to survey completion (N = 188, Table 1). Those who consumed alcohol in the prior 3 months were screened in resulting in a sample size of 188 with nBlack = 94 and nLatino = 94. BLMSM in the sample were predominantly young adults with a mean age of 24.3 years. Moreover, 60.1% of the sample were youth aged 18 to 24 years compared with 39.9% of adults aged 25 years and older. Most of the sample also had at least some college/technical school education (63.3%), while 31.9% had a high school/GED education, and 4.80% had less than high school education. A total of 62.2% of the sample were employed (either part-time or full-time) and 37.8% were unemployed.
Table 1.
Descriptive Sociodemographic Characteristics of BLMSM Sample (N = 188).
| Variable | Frequency (%) |
|---|---|
| Race | |
| Latino | 94 (50.0%) |
| African American | 94 (50.0%) |
| Age | |
| Youth (aged 18-24 years) | 113 (60.1%) |
| Young adult (aged >25 years) | 75 (39.9%) |
| Mean age (years) | 24.3 |
| Standard deviation | 4.45 |
| Education level | |
| Less than high school | 9 (4.80%) |
| High school/GED | 60 (31.9%) |
| At least some college | 119 (63.3%) |
| Employment status | |
| Not employed | 71 (37.8%) |
| Employed (full-time/part-time) | 117 (62.2%) |
| Daily drinking patterns | |
| Lower low-risk (0-2 drinks per day) | 66 (35%) |
| Higher low-risk (2-4 drinks per day) | 51 (27.1%) |
| Heavy (4 or more drinks per day) | 71 (37.8%) |
Note. BLMSM = Black and Latino men who have sex with men.
A majority of BLMSM (96.5%) in the HSAM sample (aged 18-40 years) had alcohol use rates higher than national drinking rates for males aged 18 to 24 years (78.0%) and those aged 25 to 44 years (80.0%) from data collected between 2012 and 2013 (Dawson, Goldstein, Saha, & Grant, 2015). More BLMSM reported drinking heavily (n = 71, 37.8%) on a typical drinking day when compared with higher low-risk (n = 51, 27.1%) and lower low-risk drinking (n = 71, 37.8%), individually, but less than low-risk drinking, overall. The frequency of CIAI and CRAI behaviors were similar for BLMSM (see Figure 1 and Table 1).
As identified in Table 2, FET indicated that those who reported CIAI reported higher low-risk drinking more frequently than heavy drinking and lower low-risk drinking (p = .001). Furthermore, those who perceived increased risk of transmitting or acquiring HIV due to their alcohol use more frequently reported higher low-risk daily drinking than heavy drinking and lower low-risk drinking (p = .007). Conversely, more participants who did not perceive HIV risk due to their alcohol use reported heavy drinking than the lower low-risk patterns. Race was also significantly related to different alcohol use patterns (p < .001). Although Black and Latino men had similar rates of heavy drinking and low-risk drinking, overall, they differed in their rates of lower low-risk and higher low-risk drinking. Among Latinos, 38.3% engaged in higher low-risk drinking compared with 16.0% among Blacks, while 23.4% of Latinos engaged in lower low-risk drinking compared with 46.8% of Black men.
Table 2.
Differences Between Lower Low-Risk Daily Drinking of 0 to 2 Drinks Per Day, Higher Low-Risk Daily Drinking of Greater Than 2 to 4 Drinks Per Day, and Heavy Drinking of Greater Than 4 Drinks Per Day Among BLMSM and Selected Sample Characteristics (N = 188)a.
| Characteristics | Lower low-risk n (%) | Higher low-risk n (%) | Heavy drinking n (%) | p Value |
|---|---|---|---|---|
| Total | 66 (35.1) | 51 (27.1) | 71 (37.8) | |
| Age (years) | ||||
| 18-24 | 48 (42.5) | 30 (26.5) | 35 (31.0) | .020 |
| 25 or older | 18 (24.0) | 21 (28.0) | 36 (48.0) | |
| Race/ethnicity | ||||
| Black | 44 (46.8) | 15 (16.0) | 35 (37.2) | <.001 |
| Latino | 22 (23.4) | 36 (38.3) | 36 (38.3) | |
| Education level | ||||
| Less than high school | 3 (33.3) | 1 (11.1) | 5 (55.6) | .261 |
| High School/GED | 21 (35.0) | 12 (20.0) | 27 (45.0) | |
| At least some college | 42 (35.3) | 38 (31.9) | 39 (32.8) | |
| Employment status | ||||
| Not employed | 24 (26.4) | 17 (18.7) | 30 (32.9) | .480 |
| Part-time or full-time employed | 42 (35.9) | 34 (29.1) | 41 (35.0) | |
| Alcohol created problems | ||||
| No | 58 (36.5) | 42 (26.4) | 59 (37.1) | .648 |
| Yes | 8 (26.7) | 9 (30.0) | 12 (43.3) | |
| Had HIV test | ||||
| No | 20 (44.7) | 7 (14.9) | 19 (40.4) | .092 |
| Yes | 46 (32.4) | 44 (31.0) | 52 (36.6) | |
| Perceive HIV risk from alcohol use | ||||
| No | 61 (37.7) | 37 (22.8) | 64 (39.5) | .007 |
| Yes | 5 (19.2) | 14 (53.8%) | 7 (26.9) | |
| Insertive anal intercourse risk | ||||
| No risk (condom always used) | 43 (38.4) | 19 (17.0) | 50 (44.6) | .001 |
| Some risk (condom not always used) | 23 (30.3) | 32 (42.1) | 21 (27.6) | |
| Receptive anal intercourse risk | ||||
| No risk (condom always used) | 44 (38.3) | 26 (22.6) | 45 (39.1) | .194 |
| Some risk (condom not always used) | 22 (30.7) | 25 (33.3) | 26 (36.0) | |
Total cell counts may not represent total sample size due to missing data.
As reported in Table 3, age was a significant predictor of higher level drinking (p = .014). Educational level (p = .055) and race (p = .051) both remained marginally significant predictors of higher level drinking. Among BLMSM, drinking increased with age. However, drinking was seemingly lower for those with higher education. Compared with Latino MSM, Black MSM were more likely to have lower risk drinking patterns. CIAI was not significant in the final model (p = .111) suggesting that higher level drinking was not significantly different between those reporting no CIAI and those reporting having had CIAI.
Table 3.
Regression Analyses of the Prediction of Higher Level Drinking Among Young BLMSM.
| Β | SE Β | β | t | p | |
|---|---|---|---|---|---|
| Age | .32 | .13 | .19 | 2.47 | .014 |
| Educational level | −.21 | .11 | −.14 | −1.93 | .055 |
| Race (Black) | −.26 | .14 | −.16 | −1.97 | .051 |
| Insertive risk (CIAI) | −.21 | .13 | −.12 | −1.60 | .111 |
Note. BLMSM = Black and Latino men who have sex with men; CIAI = condomless insertive anal intercourse. Only the results from the final model (Step 4) are reported from these analyses (F = 3.89, p = .005).
Discussion
The major findings of this study were fourfold: First, FET indicated significant relationship between CIAI and daily higher low-risk drinking (p = .001; the higher of two NIAAA [n.d.] defined low-risk drinking patterns used in the current study or consuming greater than 2, but less than or equal to 4 drinks per day. Those who engaged in CIAI were also more likely to consume higher low-risk levels on a typical drinking day than heavy amounts of alcohol (daily heavy alcohol use was defined as consuming more than 4 drinks per day). Second, FET indicated BLMSM who perceived alcohol-related HIV risk also reported greater frequency of higher low-risk drinking than lower low-risk drinking (the lower of the two NIAAA [n.d.] defined low-risk drinking patterns in the present study or consuming 0-2 drinks per day) and heavy drinking (p = .007). Third, BLMSM had similar rates of daily heavy drinking, while a greater percentage of Latino MSM engaged in higher low-risk drinking and a greater percentage of Black MSM engaged in lower low-risk daily drinking (p < .001). Last, older aged BLMSM (aged 25 and older) were more likely to engage in heavy drinking than youth aged 18 to 24 years (p = .046). The FET findings for age held true in the multiple regression model.
The finding that BLMSM who engaged in CIAI were more likely to consume higher low-risk amounts per day is consistent with studies indicating that alcohol consumption among BLMSM is a risk factor for condomless sex (FET was p = .001; Ekstrand, Stall, Paul, Osmond, & Coates, 1999; Mutchler et al., 2014; Purcell, Parsons, Halkitis, Mizuno, & Woods, 2001; Stone et al., 1999). Thompson et al.’s (2012) findings indicate decreased risk for health compromising behaviors (including risky sexual behavior) among adults who consume 1 to 2 drinks per day (lower low-risk drinking in the present study) when compared to those who drink 3 to 4 drinks per day (within the higher low-risk drinking category in the present study). Even though alcohol consumption at lower low-risk and higher low-risk levels is considered “low-risk” drinking by the NIAAA (n.d.), the difference between lower low-risk and higher low-risk drinking patterns may indicate differences in the degree to which alcohol is a risk factor for condomless sex. As the analysis indicates the relationship between drinking patterns and sexual risk did not hold true in the multiple regression model and review, drinking may not directly increase sexual risk taking, but the relationship may be confounded by one or more other variables (Mutchler et al., 2014).
The FET findings further indicated that BLMSM who perceived alcohol-related HIV risk were more likely to report higher low-risk daily drinking behavior than heavy and lower low-risk drinking when compared with those who had not perceived such risk (p = .007). In support of this finding, a multisite, longitudinal study among MSM reported those who exhibited moderate risk drinking or heavy drinking (greater than 14 drinks per week or average of greater than 2 drinks per day) compared with low-risk (1-14 drinks per week or average of 0-2 drinks per day) behavior were at greater risk for acquiring HIV (Sander et al., 2013). If sexual behavior and alcohol consumption go hand in hand, Mutchler’s qualitative findings explain the function of alcohol in sexual risk-taking as making CAI feel more socially permissible for BLMSM by helping impair and inhibit internalized homophobia and related stigma that would otherwise impede sex between men (Mutchler et al., 2014; Steele & Josephs, 1990).
Race was significantly related to drinking patterns. It is important to note that even though heavy drinking and overall low risk drinking rates were very similar among Black and Latino men (37.3%, 38.3%, respectively; data not reported), they had different rates of lower low-risk drinking and higher low-risk daily drinking. More Latino MSM engaged in higher low-risk drinking (38.3%) than Black MSM (16.0%), while more Black MSM reported lower low-risk drinking (48.0%) than Latino MSM (23.4%). Given the differences in low-risk drinking patterns identified between Latino and Black MSM, various social, cultural, and biological factors may influence each ethnicity to an uncertain degree (Caetano & Clark, 2003; Abraido-Lanza, Chao, & Florez, 2005; Eaton et al., 2012; Hasin, Stinson, Ogburn, & Grant, 2007; Mutchler et al., 2014; Zapolski et al., 2014). Overall, the heavy and combined low-risk daily drinking rates were very similar between Black and Latino MSM, while differences in drinking patterns have been identified within the low-risk drinking category.
Last, older BLMSM aged 25 years and older were more likely to drink heavily than low-risk amounts of alcohol when compared with younger BLMSM aged 18 to 24 years. This is partially consistent with the reports of Black men drinking heavily later in life than men of other races (Catalano et al., 1993; Johnson, Richter, Kleber, McLellan, & Carise, 2005; Watt, 2005). As Black men were 50% of the sample, reports of heavy drinking at older ages among Black MSM may contribute to the aforementioned findings. Two studies have reported age as the moderator of alcohol consumption and condomless intercourse among MSM. Mustanski’s (2008) study had a majority White MSM sample, showing increasing age moderating the effect, while Newcomb’s (2013) study reports decreasing age moderating the effect. The latter study had a more similar sample type with 69% of the sample being young BLMSM (Newcomb, 2013). More event level studies that further characterize all instances of alcohol use and identify potential moderators of risk for CAI and various alcohol consumption patterns are needed.
Although the presented findings help elucidate the drinking patterns and associated factors among younger BLMSM in Los Angeles, there were limitations to this study. Gauging drinking frequencies and sexual behavior were limited by self-report. Self-reporting of alcohol use and risky sexual behavior may underestimate the true prevalence due to the negative social perceptions surrounding these behaviors (Schroder, Carey, & Vanable, 2003; Wong et al., 2008). Nonprobability sampling could have biased the results in a few ways. First, some HSAM participants were recruited from bars and club venues that serve alcohol and could have overestimated the number of drinks the young BLMSM sample has per day as compared with a more diverse BLMSM sample. The BLMSM sample had slightly higher level of educational attainment compared with the general Black and Latino population in the United States (C. L. Ryan & Siebens, 2012) making the study findings less generalizable to the larger BLMSM or Black and Latino population in the United States. Having recruited participants on college campuses could have yielded more Latino and Black men with at least some college education than would be found in the general population of BLMSM in the United States. Another limitation of the study is that the educational status questions could not distinguish former students, current students, part-time students, full-time students, and student-workers. Given the younger mean ages reported in the current sample, many young men may still be in college, thus implicating the inclusion of a demographic, who generally drink more heavily than those not in college (White & Hingson, 2014). Not being able to distinguish these two groups to compare them may ultimately skew the data and is a limitation to this study. Additionally, the Latino men in the sample, all requested the English version of the HSAM survey. Also, because the Latino sample were all English speaking, the current findings are less representative of Latinos in Los Angeles County, where approximately 49% of the population speaks Spanish as their primary language (Daniel, Lo, Sadhwani, Wang, & Yu, 2000). Nonprobability convenience sampling makes the study less generalizable to the BLMSM population in Los Angeles County. In addition, the current study’s DV did not allow the identification of all heavy drinkers as the DV only assessed daily heavy drinking and not weekly heavy drinking as the NIAAA (n.d.) includes in their definition of heavy drinking. However, the daily use range for heavy drinking (consuming greater than 4 drinks on a typical drinking day) can stand alone in identifying daily heavy drinkers. Also, the alcohol questions in the study did not gauge whether or not (and to what degree) alcohol use was proximal to sexual intercourse as well as where alcohol consumption took place (Jones-Webb, Smolenski, Brady, Wilkerson, & Rosser, 2013). Including such variables could better characterize the context of alcohol use among BLMSM. The HSAM survey did not contain questions to determine the relationship status of study participants. As relationship status is related to alcohol use and sexual risk behavior among MSM, it will be important to include in future studies on HIV and alcohol use among MSM(Hoff, Chakravarty, Beougher, Neilands, & Darbes, 2012; Vanable, McKirnan, Buchbinder, Bartholow, Douglas, Judson, & MacQueen., 2004). The recall time frame for consuming alcohol was 3 months and longer periods of drinking could not be gauged to better capture alcohol use history. On the other hand, a 3-month recall period would help mitigate recall issues than a longer time interval. Another limitation included having a small sample size and thus having to aggregate data from BLMSM to strengthen statistical results. As race does seem to have a significant role in drinking behaviors among BLMSM, it will be important to look at drinking patterns among younger BLMSM and the associated factors separately among Black MSM and Latino MSM.
The study indicated some demographic and drinking pattern differences between Latino and Black MSM, and each group will have to be studied independently to better describe drinking patterns among these racial and sexual minorities. Some young Black MSM who report consuming higher low-risk drinking drinks per day and engaging in CAI may suggest greater risk for drinking heavily and HIV seroconverting (Sander et al., 2013) later in life (Koblin et al., 2003) through a confounding variable such as relationship status. Continued qualitative research exploring the relationship between alcohol, risky sexual behavior, and sociodemographic variables should supplement future studies that explore alcohol-related HIV risk among BLMSM (Mutchler et al., 2014). In regard to the limitation of not inquiring about BLMSM’s relationship status in the present study, future studies would benefit from identifying demographic information for an individual’s most recent sexual partner. Black MSM, for example, may have higher HIV prevalence due to their sexual network being predominantly other Black MSM and such information may be of relevance to studies on HIV risk and alcohol use (Bingham, Harawa, Johnson, Secura, MacKellar, & Valleroy, 2003) Further research can ultimately inform wide-scale early alcohol prevention and HIV risk prevention education efforts in communities, where Black and Latino men are highly represented in Los Angeles, California.
Acknowledgments
A portion of the paper was presented at the 2014 International AIDS Conference, Melbourne, Australia.
Alcohol misuse can be defined as drinking that significantly poses harm to one’s health and well-being (Centers for Disease Control and Prevention, 2013).
Footnotes
Authors’ Note: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research reported in this publication was supported by the National Institute on Drug Abuse under Award Number 1R21DA033874-01A1 and the National Institute on Minority Health and Health Disparities under Award Number P20MD003942, both of the National Institutes of Health.
References
- Abraido-Lanza A. F., Chao M. T., Florez K. R. (2005). Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Social Science & Medicine, 61, 1243-1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachman J. G., Schulenberg J., O’Malley P. M., Wadsworth K. N., Johnston L. D. (1996). Getting drunk and growing up: Trajectories of frequent binge drinking during the transition to young adulthood. Journal of Studies on Alcohol and Drugs, 57, 289-304. [DOI] [PubMed] [Google Scholar]
- Bingham T. A., Harawa N. T., Johnson D. F., Secura G. M., MacKellar D. A., Valleroy L. A. (2003). The effect of partner characteristics on HIV infection among African American men who have sex with men in the young men’s survey, Los Angeles, 1999–2000. AIDS Education and Prevention, 15(1 Supplement), 39-52. [DOI] [PubMed] [Google Scholar]
- Caetano R., Clark C. L. (1998). Trends in alcohol consumption patterns among Whites, Blacks, and Hispanics: 1984 and 1995. Journal of Studies on Alcohol and Drugs, 59, 659-668. [DOI] [PubMed] [Google Scholar]
- Caetano R., Clark C. L. (2003). Acculturation, alcohol consumption, smoking, and drug use among Hispanics. In Chun K. M., Organista P. B., Marín G. (Eds.), Acculturation: Advances in theory, measurement, and applied research (pp. 223-260). Washington, DC: American Psychological Association. [Google Scholar]
- Calhoun V. D., Pekar J. J., Pearlson G. D. (2004). Alcohol intoxication effects on simulated driving: Exploring alcohol-dose effects on brain activation using functional MRI. Neuropsychopharmacology, 29, 2097-2017. [DOI] [PubMed] [Google Scholar]
- Castro F. G., Stein J. A., Bentler P. M. (2009). Ethnic pride, traditional family values, and acculturation in early cigarette and alcohol use among Latino adolescents. Journal of Primary Prevention, 30, 265-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano R. F., Hawkins J. D., Krenz C., Gillmore M., Morrison D., Wells E., Abbott R. (1993). Using research to guide culturally appropriate drug abuse prevention. Journal of Consulting and Clinical Psychology, 61, 804-811. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2012). Estimated HIV incidence in the United States, 2007–2010. HIV Surveillance Supplemental Report, 17(4). Retrieved from http://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf [Google Scholar]
- Centers for Disease Control and Prevention. (2013). Alcohol and substance misuse. Retrieved from http://www.cdc.gov/workplacehealthpromotion/implementation/topics/substance-abuse.html
- Chartier K. G., Vaeth P. A., Caetano R. (2014). Focus on: Ethnicity and the social and health harms from drinking. Alcohol Research: Current Reviews, 35, 229-237. [PMC free article] [PubMed] [Google Scholar]
- Cherpitel C. J. (1993). Alcohol and injuries: A review of international emergency room studies. Addiction, 88, 923-937. [DOI] [PubMed] [Google Scholar]
- Cummings S. M., Cooper R. L., Johnson C. (2013). Alcohol misuse among older adult public housing residents. Journal of Gerontological Social Work, 56, 407-422. [DOI] [PubMed] [Google Scholar]
- Daniel L., Lo W., Sadhwani S., Wang K., Yu N. W. (2000). L.A. speaks: Language diversity and English proficiency by Los Angeles County service planning area. Retrieved from http://advancingjustice-la.org/sites/default/files/LASpeaksLanguageDiversity.pdf
- Dawson D. A., Goldstein R. B., Saha T. D., Grant B. F. (2015). Changes in alcohol consumption: United States, 2001-2002 to 2012-2013. Drug and Alcohol Dependence, 148, 56-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Castelnuovo A., Costanzo S., Bagnardi V., Donati M. B., Iacoviello L., de Gaetano G. (2006). Alcohol dosing and total mortality in men and women: An updated meta-analysis of 34 prospective studies. Archives of Internal Medicine, 166, 2437-2445. [DOI] [PubMed] [Google Scholar]
- Eaton D. K., Kann L., Kinchen S., Shanklin S., Flint K. H., Hawkins J., . . . Wechsler H. (2012). Youth risk behavior surveillance–United States, 2011. Morbidity and Mortality Weekly Report, 61(SS04), 1-162. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/ss6104a1.htm [PubMed] [Google Scholar]
- Ekstrand M. L., Stall R. D., Paul J. P., Osmond D. H., Coates T. J. (1999). Gay men report high rates of unprotected anal sex with partners of unknown or discordant HIV status. AIDS, 13, 1525-1533. [DOI] [PubMed] [Google Scholar]
- Gilbert P. A., Daniel-Ulloa J., Conron K. J. (2015). Does comparing alcohol use along a single dimension obscure within-group differences? Investigating men’s hazardous drinking by sexual orientation and race/ethnicity. Drug and Alcohol Dependence, 151, 101-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene E. R., Frye V., Cerdá M., Ompad D. C., Nandi V., Hoover D., Koblin B. (2014). Patterns of recent alcohol consumption by race among a sample of urban men who have sex with men. Drug and Alcohol Dependence, 140, e74. [Google Scholar]
- Fromme K., D’Amico E. J., Katz E. C. (1999). Intoxicated sexual risk taking: An expectancy or cognitive impairment explanation? Journal of Studies on Alcohol and Drugs, 60, 54-63. [DOI] [PubMed] [Google Scholar]
- Hasin D. S., Stinson F. S., Ogburn E., Grant B. F. (2007). Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry, 64, 830-842. [DOI] [PubMed] [Google Scholar]
- Heckathorn D. D. (1997). Respondent-driven sampling: A new approach to the study of hidden populations. Social Problems, 44, 174-199. [Google Scholar]
- Hoff C. C., Chakravarty D., Beougher S. C., Neilands T. B., Darbes L. A. (2012). Relationship characteristics associated with sexual risk behavior among MSM in committed relationships. AIDS Patient Care and STDs, 26, 738-745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer D. W., Jr., Lemeshow S. (2004). Applied logistic regression. Hoboken, NJ: John Wiley. [Google Scholar]
- Howell D. C. (2007). The treatment of missing data. In Outhwaite W., Turner S. P. (Eds.), The Sage handbook of social science methodology (pp. 208-224). Thousand Oaks, CA: Sage. [Google Scholar]
- Irwin T. W. (2005). Drug-use patterns among men who have sex with men presenting for alcohol treatment: Differences in ethnic and sexual identity. Journal of Urban Health, 82, 127-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson P. B., Richter L., Kleber H. D., McLellan A. T., Carise D. (2005). Telescoping of drinking-related behaviors: Gender, racial/ethnic, and age comparisons. Substance Use & Misuse, 40, 1139-1151. [DOI] [PubMed] [Google Scholar]
- Jones-Webb R., Smolenski D., Brady S., Wilkerson M., Rosser B. R. (2013). Drinking settings, alcohol consumption, and sexual risk behavior among gay men. Addictive Behaviors, 38, 1824-1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keall M. D., Frith W. J., Patterson T. L. (2004). The influence of alcohol, age and number of passengers on the night-time risk of driver fatal injury in New Zealand. Accident Analysis & Prevention, 36, 49-61. [DOI] [PubMed] [Google Scholar]
- Kerr W. C., Greenfield T. K., Bond J., Ye Y., Rehm J. (2011). Racial and ethnic differences in all-cause mortality risk according to alcohol consumption patterns in the national alcohol surveys. American Journal of Epidemiology, 174, 769-778. doi: 10.1093/aje/kwr147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes K. M., Miech R. (2013). Age, period, and cohort effects in heavy episodic drinking in the U.S. from 1985 to 2009. Drug and Alcohol Dependence, 132, 140-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin B. A., Chesney M. A., Husnik M. J., Bozeman S., Celum C. L., Buchbinder S., . . . Coates T. J. (2003). High-risk behaviors among men who have sex with men in 6 US cities: Baseline data from the EXPLORE study. American Journal of Public Health, 93, 926-932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz H., Fiorentino D. (2000). A review of the literature on the effects of low doses of alcohol on driving-related skills. Retrieved from http://dfconsulting.info/AReviewoftheLiterature.pdf
- Mullens A. B., Young R. M., Dunne M. P., Norton G. (2011). The drinking expectancy questionnaire for men who have sex with men (DEQ-MSM): A measure of substance-related beliefs. Drug and Alcohol Review, 30, 372-380. [DOI] [PubMed] [Google Scholar]
- Mustanski B. (2008). Moderating effects of age on the alcohol and sexual risk taking association: An online daily diary study of men who have sex with men. AIDS and Behavior, 12, 118-126. [DOI] [PubMed] [Google Scholar]
- Mutchler M. G., McDavitt B., Gordon K. K. (2014). “Becoming bold”: Alcohol use and sexual exploration among Black and Latino young men who have sex with men (YMSM). Journal of Sex Research, 51, 696-710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Alcohol Abuse and Alcoholism. (n.d.). What’s “at-risk” or “heavy” drinking? Rethinking Drinking: Alcohol & Your Health. Retrieved from http://rethinkingdrinking.niaaa.nih.gov/isyourdrinkingpatternrisky/whatsatriskorheavydrinking.asp
- Newcomb M. E. (2013). Moderating effect of age on the association between alcohol use and sexual risk in MSM: Evidence for elevated risk among younger MSM. AIDS and Behavior, 17, 1746-1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palfai T. P., Winter M., Lu J., Rosenbloom D., Saitz R. (2014). Personalized feedback as a universal prevention approach for college drinking: A randomized trial of an e-mail linked universal web-based alcohol intervention. Journal of Primary Prevention, 35, 75-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peck R. C., Gebers M. A., Voas R. B., Romano E. (2008). The relationship between blood alcohol concentration (BAC), age, and crash risk. Journal of Safety Research, 39, 311-319. [DOI] [PubMed] [Google Scholar]
- Peterson J. B., Rothfleisch J., Zelazo P. D., Pihl R. (1990). Acute alcohol intoxication and cognitive functioning. Journal of Studies on Alcohol and Drugs, 51, 114-122. [DOI] [PubMed] [Google Scholar]
- Purcell D. W., Parsons J. T., Halkitis P. N., Mizuno Y., Woods W. J. (2001). Substance use and sexual transmission risk behavior of HIV-positive men who have sex with men. Journal of Substance Abuse, 13, 185-200. [DOI] [PubMed] [Google Scholar]
- Ramirez-Valles J., Garcia D., Campbell R. T., Diaz R. M., Heckathorn D. D. (2008). HIV infection, sexual risk behavior, and substance use among Latino gay and bisexual men and transgender persons. Journal Information, 98, 1036-1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan C. L., Siebens J. (2012). Educational attainment in the United States: 2009. Washington, DC: US Department of Commerce, Economics and Statistics Administration, US Census Bureau; Retrieved from http://www.census.gov/prod/2012pubs/p20-566.pdf [Google Scholar]
- Ryan M., Merrick E. L., Hodgkin D., Horgan C. M., Garnick D. W., Panas L., . . . Saitz R. (2013). Drinking patterns of older adults with chronic medical conditions. Journal of General Internal Medicine, 28, 1326-1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sander P. M., Cole S. R., Stall R. D., Jacobson L. P., Eron J. J., Napravnik S., . . . Ostrow D. G. (2013). Joint effects of alcohol consumption and high-risk sexual behavior on HIV seroconversion among men who have sex with men. AIDS, 27, 815-823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroder K. E., Carey M. P., Vanable P. A. (2003). Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Annals of Behavioral Medicine, 26, 104-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soderstrom C. A., Dischinger P. C., Kerns T. J., Kufera J. A., McDuff D. R., Gorelick D. A., Smith G. S. (1998). Screening trauma patients for alcoholism according to NLAAA guidelines with alcohol use disorders identification test questions. Alcoholism: Clinical and Experimental Research, 22, 1470-1475. [PubMed] [Google Scholar]
- Stall R., Paul J. P., Greenwood G., Pollack L. M., Bein E., Crosby G. M., . . . Catania J. A. (2001). Alcohol use, drug use and alcohol-related problems among men who have sex with men: The urban men’s health study. Addiction, 96, 1589-1601. [DOI] [PubMed] [Google Scholar]
- Steele C. M., Josephs R. A. (1990). Alcohol myopia: Its prized and dangerous effects. American Psychologist, 45, 921-933. [DOI] [PubMed] [Google Scholar]
- Stone E., Heagerty P., Vittinghoff E., Douglas J. M., Jr., Koblin B. A., Mayer K. H., . . . Buchbinder S. P. (1999). Correlates of condom failure in a sexually active cohort of men who have sex with men. Journal of Acquired Immune Deficiency Syndromes, 20, 495-501. [DOI] [PubMed] [Google Scholar]
- Thiede H., Valleroy L. A., MacKellar D. A., Celentano D. D., Ford W. L., Hagan H., . . . Torian L. V. (2003). Regional patterns and correlates of substance use among young men who have sex with men in 7 US urban areas. American Journal of Public Health, 93, 1915-1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson K. D., Stockwell T., Macdonald S. (2012). Is there a “low-risk” drinking level for youth? The risk of acute harm as a function of quantity and frequency of drinking. Drug and Alcohol Review, 31, 184-193. [DOI] [PubMed] [Google Scholar]
- Vanable P. A., McKirnan D. J., Buchbinder S. P., Bartholow B. N., Douglas J. M., Jr., Judson F. N., MacQueen K. M. (2004). Alcohol use and high-risk sexual behavior among men who have sex with men: The effects of consumption level and partner type. Health Psychology, 23, 525-532. [DOI] [PubMed] [Google Scholar]
- Vosburgh H. W., Mansergh G., Sullivan P. S., Purcell D. W. (2012). A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS and Behavior, 16, 1394-1410. [DOI] [PubMed] [Google Scholar]
- Washington T. A., Robles G., Malotte K. (2013). Factors associated with HIV testing history among Black men who have sex with men (BMSM) in Los Angeles County. Behavioral Medicine, 39, 52-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt T. T. (2005). Race/ethnic differences in alcohol abuse among youth: An examination of risk-taking attitudes as a mediating factor. Journal of Ethnicity in Substance Abuse, 3(3), 33-47. [DOI] [PubMed] [Google Scholar]
- Weinhardt L. S., Carey M. P. (2000). Does alcohol lead to sexual risk behavior? Findings from event-level research. Annual Review of Sex Research, 11, 125-157. [PMC free article] [PubMed] [Google Scholar]
- White A., Hingson R. (2014). The Burden of Alcohol Use: Excessive Alcohol Consumption and Related Consequences among College Students. Alcohol Research : Current Reviews, 35(2), 201–218. [PMC free article] [PubMed] [Google Scholar]
- Wong C. F., Kipke M. D., Weiss G. (2008). Risk factors for alcohol use, frequent use, and binge drinking among young men who have sex with men. Addictive Behaviors, 33, 1012-1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolf S. E., Maisto S. A. (2009). Alcohol use and risk of HIV infection among men who have sex with men. AIDS and Behavior, 13, 757-782. [DOI] [PubMed] [Google Scholar]
- Zapolski T. C., Pedersen S. L., McCarthy D. M., Smith G. T. (2014). Less drinking, yet more problems: Understanding African American drinking and related problems. Psychological Bulletin, 140, 188-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeigler D. W., Wang C. C., Yoast R. A., Dickinson B. D., McCaffree M. A., Robinowitz C. B., Sterling M. L. (2005). The neurocognitive effects of alcohol on adolescents and college students. Preventive Medicine, 40, 23-32. [DOI] [PubMed] [Google Scholar]
- Zemore S. E., Mulia N., Ye Y., Borges G., Greenfield T. K. (2009). Gender, acculturation, and other barriers to alcohol treatment utilization among Latinos in three national alcohol surveys. Journal of Substance Abuse Treatment, 36, 446-456. [DOI] [PMC free article] [PubMed] [Google Scholar]