Abstract
Background
Although ventriculoperitoneal shunt (VPS) surgery is the most frequent surgical treatment for patients with hydrocephalus, modern rates of complications in adults are uncertain.
Methods
We performed a retrospective cohort study of adult patients hospitalized at the time of their first recorded procedure code for VPS surgery between 2005 and 2012 at nonfederal acute care hospitals in California, Florida, and New York. We excluded patients who during the index hospitalization for VPS surgery had concomitant codes for VPS revision, CNS infection, or died during the index hospitalization. Patients were followed for the primary outcome of a VPS complication, defined as the composite of CNS infection or VPS revision. Survival statistics were used to calculate the cumulative rate and incidence rate of VPS complications.
Results
17,035 patients underwent VPS surgery. During a mean follow-up of 3.9 (±1.8) years, at least one VPS complication occurred in 23.8% (95% CI, 22.9–24.7%) of patients. The cumulative rate of CNS infection was 6.1% (95% CI, 5.7–6.5%) and of VPS revision 22.0% (95% CI, 21.1–22.9%). The majority of complications occurred within the first year of hospitalization for VPS surgery. Complication rates were 21.3 (95% CI, 20.6–22.1) complications per 100 patients per year in the first year after VPS surgery, 5.7 (95% CI, 5.3–6.1) in the second year after VPS surgery, and 2.5 (95% CI, 2.1–3.0) in the fifth year after VPS surgery.
Conclusions
Complications are not infrequent following VPS surgery; however, the majority of complications appear to be clustered in the first year following VPS insertion.
Keywords: ventriculoperitoneal shunts, hydrocephalus, neurosurgery, central nervous system infections, brain abscess, epidemiology
Introduction
Ventriculoperitoneal shunt (VPS) insertion is the most frequently used surgical treatment for patients with hydrocephalus, with over 30,000 procedures performed yearly in the United States.1 VPS surgery was first reported in 18982 and since then has become the mainstay of treatment for hydrocephalus; however, complications including infection and shunt malfunction continue to occur leading to a significant number of hospital readmissions and 50 million dollars of economic expenditure per year.1,3
Although VPS insertion is a common neurosurgical procedure, complication rates in adults are poorly established with a reported range from 17–33%4–12 and the majority of these data come from small case series, single institution studies, or analyses from over a decade ago. Given the recent advances in medical care, the aim of this study was to evaluate the current rate of VPS complications in a large heterogeneous group of adult patients.
Materials and methods
Study Design
In order to evaluate the rate of complications after VPS surgery, we used administrative claims data on all discharges from nonfederal emergency departments (EDs) and acute care hospitals in three large and demographically heterogeneous states: California, New York, and Florida. Trained analysts at nonfederal emergency departments (EDs) and acute care hospitals used standardized methods to collect data about discharges and transmitted these to retrospective state agencies. After quality checking, these data were reported in a deidentified format to the Agency for Healthcare Research and Quality for its Healthcare Cost and Utilization Project.13 A unique record linkage number for each patient allowed longitudinal tracking of ED encounters and hospitalizations.14 This study was approved by the Weill Cornell Medical College institutional review board.
Study Patients
We identified all patients aged 18 years or older who were discharged from a nonfederal ED or acute care hospital in California from 2005–2011, Florida from 2005–2012, and New York from 2006–2011. These observational periods were chosen to ensure at least 1 year of follow-up data for all study patients. We included all patients at the time of their first recorded procedure code for VPS surgery as defined by previously validated International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) code 02.34.15 This code has a 95% sensitivity and 100% specificity based on medical record review.15 We excluded patients who during the index hospitalization for VPS surgery had concomitant codes for VPS revision, had documented central nervous system (CNS) infection (bacterial meningitis or brain abscess), or did not survive the index hospitalization. These exclusionary criteria were used as our objective was to evaluate the long-term risk of complications in patients who received VPS surgery and were discharged alive without known complications during the initial hospitalization when a VPS was inserted. In order to maximize our ability to assess longitudinal follow-up, we excluded patients who did not permanently reside in California, New York, or Florida.
Measurements
The primary outcome was the rate of VPS complications, defined as the composite of CNS infection and VPS revision. CNS infection was defined as meningitis or abscess using ICD-9-CM diagnosis codes (see supplemental appendix). A VPS revision or malfunction was defined using ICD-9-CM procedure and diagnosis codes as the presence of at least one of the following procedure codes: exploration of a ventricular shunt, replacement or revision of a ventricular shunt, removal of ventricular shunt, distal shunt revision, or shunt malfunction (see supplemental appendix). In a secondary analysis, we included non-traumatic subdural hematoma as another potential consequence of overdrainage from the VPS using ICD-9-CM code 432.1. Patients were censored at the time of their first complication, at death, or at the end of the follow-up period. We also evaluated predictors of VPS complications including demographic characteristics, insurance status, hospital volume of VPS surgery, and the baseline diagnosis for the VPS at the time of the initial VPS insertion. As we lacked data on out-of-hospital mortality, all patients without a documented in-hospital death were assumed to have survived throughout the follow-up period for which we had data; however, we also performed a sensitivity analysis that accounted for out-of-hospital mortality by censoring patients at time of their last ED visit or hospitalization.
Statistical Analysis
Descriptive statistics with exact confidence intervals (CIs) were used to report crude rates. For univariate analyses, variables were compared using chi-squared statistics for categorical variables and the t-test for continuous variables. Kaplan-Meier survival statistics were used to calculate the cumulative rate and incidence rate of VPS complications. Poisson regression with robust standard errors was used to evaluate factors associated with VPS complications while adjusting for demographic characteristics (age, sex, and insurance status). Statistical significance was defined using an alpha of 0.05. All analyses were performed with Stata/MP version 13 (College Station, TX).
Results
VPS complications
We identified 17,035 patients who underwent VPS surgery. The most common baseline diagnoses in patients requiring VPS were communicating hydrocephalus, idiopathic normal-pressure hydrocephalus, and obstructive hydrocephalus; these accounted for 64% of cases (Table 1). During a mean follow-up of 3.9 (±1.8) years, at least one VPS complication occurred in 23.8% (95% CI, 22.9–24.7%) of patients. The cumulative rate of CNS infection was 6.1% (95% CI, 5.7–6.5%) and that of VPS revision was 22.0% (95% CI, 21.1–22.9%). When non-traumatic subdural hematoma was included, the cumulative rate of any complication throughout follow-up was 33.4% (32.4–34.4%). The cumulative rate of non-traumatic subdural hematoma was 14.4% (95% CI, 13.5–15.3%). Hospitalization with a VPS complication was associated with a 2.7% mortality rate.
Table 1.
Characteristics of Patients with Ventriculoperitoneal Shunt Surgery, Stratified by Presence of Complications
| Characteristica | Complication (N = 3,376) | No Complication (N = 13,659) |
|---|---|---|
| Age, mean (SD), y | ||
| Female | 1,641 (48.6) | 6,686 (49.0) |
| Race | ||
| White | 2,417 (73.2) | 9,652 (72.4) |
| Black | 255 (7.7) | 1,075 (8.1) |
| Hispanic | 446 (13.5) | 1,600 (12.0) |
| Asian | 108 (3.3) | 547 (4.1) |
| Other | 76 (2.3) | 466 (3.5) |
| Payment source | ||
| Medicare | 1,635 (48.4) | 8,166 (59.8) |
| Medicaid | 412 (12.2) | 1,392 (10.2) |
| Private | 1,131 (33.5) | 3,481 (25.5) |
| Self-pay | 69 (2.0) | 273 (2.0) |
| Other | 129 (3.8) | 347 (2.5) |
| Type of Admission | ||
| Non-Elective | 826 (24.4) | 2,982 (21.8) |
| Elective | 833 (24.7) | 3,092 (22.6) |
| Unknown | 1,717 (50.9) | 7585 (55.6) |
| Admission Source | ||
| Emergency Department | 705 (20.9) | 2,758 (20.2) |
| Another Hospital | 168 (5.0) | 747 (5.5) |
| Transfer from Another Care Facilityb | 81(2.4) | 317 (2.3) |
| Unknown | 2,422 (71.7) | 9,837 (72.0) |
| Hospital Volume of Ventriculoperitoneal Shunts During Study Period | ||
| 0–75 | 993 (29.4) | 4,041 (29.6) |
| 76–150 | 807 (23.9) | 3,017 (22.1) |
| 151–500 | 1,383 (41.0) | 5,857 (42.9) |
| >500 | 193 (5.7) | 744 (5.5) |
Abbreviations: SD, standard deviation
Data are presented as number (%) unless otherwise specified.
Includes transfers from skilled nursing facilities, other health care facilities, and home health agencies.
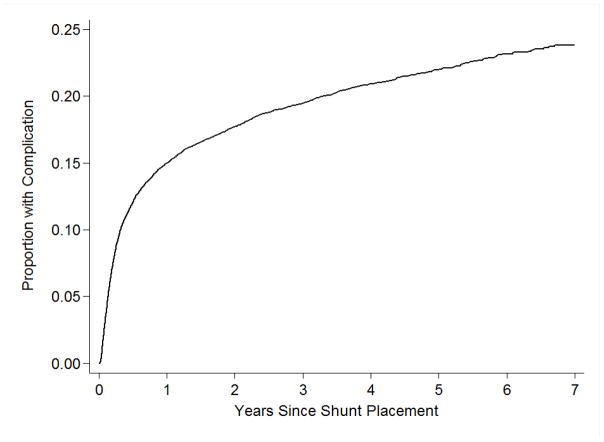
The majority of complications occurred within the first year of the initial VPS insertion (Figure 1). Complication rates were 21.3 (95% CI, 20.6–22.1) complications per 100 patients per year in the first year after VPS surgery, 5.7 (95% CI, 5.3–6.1) in the second year after VPS surgery, and 2.5 (95% CI, 2.1–3.0) in the fifth year after VPS surgery. Similar trends were seen when infection and VPS revision were assessed separately.
Figure 1.
Proportion of Patients with Ventriculoperitoneal Shunt Complications.
Legend: Ventriculoperitoneal shunt complications are clustered within the first year after ventriculoperitoneal shunt insertion.
Predictors of VPS complications
In a multivariable analysis, we found no association between sex, race, or hospital volume of VPS surgeries with VPS complications. On the other hand, younger age was associated with a higher rate of VPS complications (incidence rate ratio [IRR] per decade, 0.83; 95% CI, 0.81–0.86). Complications were more likely in those with benign intracranial hypertension, idiopathic normal pressure hydrocephalus, obstructive hydrocephalus, and communicating hydrocephalus (Table 2). In a sensitivity analysis that censored patients at the time of the last follow-up, our results were unchanged save for a new association between an underlying diagnosis of a brain tumor (as compared to other hydrocephalus diagnoses) and the development of a VPS complication (IRR, 2.84; 95% CI, 1.78–4.53).
Table 2.
Baseline Hydrocephalus Diagnosis of Patients Receiving a Ventriculoperitoneal Shunt, Stratified by Presence of Complications
| Baseline Hydrocephalus Diagnosis a | Complication (N = 3,376) | No Complication (N = 13,659) | IRR (95% CI) |
|---|---|---|---|
| Other | 683 (20.2) | 2,354 (17.2) | 1 |
| Communicating Hydrocephalus | 823 (24.4) | 3,251 (23.8) | 1.25 (1.04–1.51) |
| Idiopathic Normal Pressure Hydrocephalus | 548 (16.2) | 2,941 (21.5) | 1.67 (1.34–2.08) |
| Obstructive Hydrocephalus | 839 (24.9) | 2,625 (19.2 | 1.49 (1.28–1.75) |
| Subarachnoid Hemorrhage | 175 (5.2) | 1,315 (9.6) | 0.53 (0.41–0.70) |
| Intracerebral Hemorrhage | 60 (1.8) | 495 (3.6) | 0.54 (0.35–0.82) |
| Benign Intracranial Hypertension | 167 (5.0) | 257 (1.9) | 3.01 (2.24–4.03) |
| Secondary Malignancy of Brain | 33 (1.0) | 285 (2.1) | 0.88 (0.56–1.38) |
| Cerebral Cyst | 48 (1.4) | 136 (1.0) | 1.09 (0.73–1.62) |
Abbreviations: IRR, incidence rate ratio
Data are presented as number (%) unless otherwise specified.
Discussion
In a large, heterogeneous, population-based sample of patients who underwent VPS surgery, we found that the contemporary rate of VPS complications was 22.6% during a mean follow-up of 3.8 years. VPS revisions accounted for the majority of complications, while CNS infections were far less common. When subdural hematoma was included as a potential complication, one-third of patients experienced at least one complication. The majority of VPS complications occurred within the first year after VPS insertion.
Over the last forty years, multiple study groups have reported a complication rate between 17–33% after VPS surgery4–12 In this context, our results suggest that there has been no significant improvement in the rate of VPS complication over the last several decades. For example, one single-center study evaluated 356 patients from 1970–1988 and reported a VPS complication rate of 28.7%.6 Fifteen years later, an analysis using similar methods to ours reported a similar complication rate of 29% from 1990–2000.4 Our findings from a decade later confirm that VPS complications remain a common problem. Despite other advances in medicine, there appears to have been little improvement in reducing VPS complications over the past four decades. Furthermore, our study indicates that the highest-risk period for developing a VPS complication is within the first year of VPS insertion, arguing against a time-related failure of the device. This suggests that the ideal time frame for close surveillance and follow-up to decrease VPS related complications is in the first year following surgery.
The high frequency of non-traumatic subdural hematoma should be noted. Non-traumatic subdural hematoma is a known potential complication of overdrainage from the VPS16–17, but to our knowledge, no previous population-based study has defined its frequency. The rate of drainage may be altered so as to increase or decrease its speed, but if overdrainage occurs, a subdural hematoma may form which may lead to headache, confusion, seizures or focal neurological deficits.18 Treatment may include adjustments in the rate of drainage or may include subdural hematoma evacuation with surgery.16–17 The high rate of non-traumatic subdural hematoma after VPS surgery should motivate physicians to adopt a low threshold for obtaining head imaging in a patient with a VPS who complains of headache, focal neurological deficits, confusion, or seizures.
Previous literature has shown an inverse relationship between higher hospital volume of VPS surgery and mortality in the pediatric population.19 We therefore hypothesized that hospitals which perform more adult VPS surgeries would have fewer complications given more refined surgical techniques and institutional protocols in place; however, we found rates of complications were similar irrespective of the number of VPS surgeries performed at the hospital. One may surmise that patients admitted to higher case volume centers were more likely to be sicker and have more comorbidities, but further research will be needed to test this hypothesis.
Our results also indicate that patients with certain baseline hydrocephalus conditions are at higher risk for VPS complications. Consistent with the prior literature, benign intracranial hypertension was associated with a high rate of VPS complications.20–22 Woodworth et al. report a complication rate of 10% at three months after VPS surgery, 20% at six months, and 50% at twelve months.20 Rosenberg et al. report a 64% shunt failure rate at six months. VPS insertion is often required in refractory cases of benign intracranial hypertension.21 Although the exact pathogenesis of idiopathic intracranial hypertension is unclear, fluctuating CSF pressures and flow rates are typically present and may lead to overdrainage which is likely a leading cause for VPS revisions.21
Our study has several important limitations. First, as our study relied on ICD-9-CM codes, we lacked important clinical information regarding why patients underwent VPS revisions; however, we used well-validated VPS procedure codes, and it would be uncommon practice to revise a functioning VPS.15 Second, we relied on ICD-9-CM codes to diagnose VPS infections such as meningitis or abscess, but lacked both clinical and laboratory data such as fever, WBC count and CSF studies. Third, we lacked data on perioperative use of antibiotics during VPS surgery, which may have affected rates of infections. Fourth, prior studies have varying definitions of what constitutes a VPS complication. We defined a VPS complication as the composite of VPS revision and CNS infection, which is most consistent with the recent literature, but may not be directly comparable to every study. Fifth, as this is a large population-based study, we were not able to comment on surgical techniques. There are several case series from specific neurosurgical centers quoting varying VPS complication rates; these may be related to several different factors including surgical technique and underlying hydrocephalus diagnosis, but our results speak to the overall rate of complications on a national level. Sixth, we could not account for the type or model of VPS catheter used, which may have affected complication and infection rates. Seventh, we could not account for patients who had VPS complication outside of New York, Florida or California. This would have introduced an underestimation of the number of VPS complications, which we tried to minimize by only including patients who were permanent residents of these states. Lastly, we were unable to account for out-of-hospital deaths. Again, this would have led to over-inflation of follow-up time and therefore an underestimation of complication rates, which we tried to minimize by performing a sensitivity analysis that censored patients at the time of last follow-up, in which our results were largely unchanged.
Conclusions
Despite a long history of VPS surgery as treatment for hydrocephalus, complications are not uncommon and rates of complications have not changed significantly over the past several decades. Our findings indicate that further strategies are necessary to improve the long-term treatment of adults with hydrocephalus.
Supplementary Material
Highlights.
Complications are common after ventriculoperitoneal shunt (VPS) surgery.
Complications occur in 23.8% of patients after VPS surgery.
The majority of complications occur within the first year of insertion of VPS.
Acknowledgments
The authors are grateful to Monica Chen for copyediting and clerical assistance.
Funding: This work was supported by an NIH grant K23NS082367 (Kamel) and the Michael Goldberg Stroke Research Fund (Kamel).
Abbreviations list
- VPS
Ventriculopertioneal shunt
- CI
Confidence interval
- CNS
Central Nervous System
- ED
Emergency Department
- ICD-9-CM
International Classification of Diseases, 9th Revision, Clinical Modification
- IRR
Incidence Rate Ratio
Footnotes
Conflicts of Interest: The authors report no conflicts of interest involving the work under consideration for publication. Outside the submitted work, Dr. Kamel has served on a medical advisory board and serves on a speakers bureau for Genentech. The other authors report no potential competing interests outside the submitted work.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bondurant CP, Jimenez DF. Epidemiology of cerebrospinal fluid shunting. Pediatr Neurosurg. 1995;23:254–259. doi: 10.1159/000120968. [DOI] [PubMed] [Google Scholar]
- 2.Scarff JE. Treatment of hydrocephalus: an historical and critical review of methods and results. J Neurol Neurosurg & Psychiatry. 1963;26:1–26. doi: 10.1136/jnnp.26.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patwardhan RV, Nanda A. Implanted ventricular shunts in the United States: the billion-dollar-a-year cost of hydrocephalus treatment. Neurosurgery. 2005;56:139–144. doi: 10.1227/01.neu.0000146206.40375.41. discussion 144–135. [DOI] [PubMed] [Google Scholar]
- 4.Wu Y, Green NL, Wrensch MR, Zhao S, Gupta N. Ventriculoperitoneal shunt complications in California: 1990 to 2000. Neurosurgery. 2007;61:557–562. doi: 10.1227/01.NEU.0000290903.07943.AF. discussion 562–553. [DOI] [PubMed] [Google Scholar]
- 5.Korinek AM, Fulla-Oller L, Boch AL, Golmard JL, Hadiji B, Puybasset L. Morbidity of ventricular cerebrospinal fluid shunt surgery in adults: an 8-year study. Neurosurgery. 2011;68:985–994. doi: 10.1227/NEU.0b013e318208f360. discussion 994–985. [DOI] [PubMed] [Google Scholar]
- 6.Puca A, Anile C, Maira G, Rossi G. Cerebrospinal fluid shunting for hydrocephalus in the adult: factors related to shunt revision. Neurosurgery. 1991;29:822–826. doi: 10.1097/00006123-199112000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Khan F, Rehman A, Shamim MS, Bari ME. Factors affecting ventriculoperitoneal shunt survival in adult patients. Surg Neurol Int. 2015;6:25. doi: 10.4103/2152-7806.151388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reddy GK, Bollam P, Caldito G. Long-term outcomes of ventriculoperitoneal shunt surgery in patients with hydrocephalus. World Neurosurg. 2014;81:404–410. doi: 10.1016/j.wneu.2013.01.096. [DOI] [PubMed] [Google Scholar]
- 9.Reddy GK. Ventriculoperitoneal shunt surgery and the incidence of shunt revision in adult patients with hemorrhage-related hydrocephalus. Clin Neurol and Neurosurg. 2012;114:1211–1216. doi: 10.1016/j.clineuro.2012.02.050. [DOI] [PubMed] [Google Scholar]
- 10.Reddy GK, Bollam P, Caldito G. Ventriculoperitoneal shunt surgery and the risk of shunt infection in patients with hydrocephalus: long-term single institution experience. World Neurosurg. 2012;78:155–163. doi: 10.1016/j.wneu.2011.10.034. [DOI] [PubMed] [Google Scholar]
- 11.O’Kelly CJ, Kulkarni AV, Austin PC, Urbach D, Wallace MC. Shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage: incidence, predictors, and revision rates. Clinical article. J Neurosurg. 2009;111:1029–1035. doi: 10.3171/2008.9.JNS08881. [DOI] [PubMed] [Google Scholar]
- 12.George R, Leibrock L, Epstein M. Long-term analysis of cerebrospinal fluid shunt infections. A 25-year experience. J Neurosurg. 1979;51:804–811. doi: 10.3171/jns.1979.51.6.0804. [DOI] [PubMed] [Google Scholar]
- 13.Agency for Healthcare Research and Quality. [Accessed 21.07.15];Healthcare Cost and Utilization Project. Available at: http://hcupnet.ahrq.gov.
- 14.Agency for Healthcare Research and Quality. [Accessed 21.07.15];HCUP methods series: methodological issues when studying readmissions and revisits using hospital administrative data. Available at: http://www.ncup-us.ahrq.gov/reports/methods/2011_01.pdf.
- 15.Walcott BP, Iorgulescu JB, Stapleton CJ, Kamel H. Incidence, Timing, and Predictors of Delayed Shunting for Hydrocephalus After Aneurysmal Subarachnoid Hemorrhage. Neurocrit Care. 2015;23:54–58. doi: 10.1007/s12028-014-0072-y. [DOI] [PubMed] [Google Scholar]
- 16.Asopa S, Patel A, Khan OA, Sharma R, Ohri SK. Non-bacterial thrombotic endocarditis. Eur J Cardiothorac Surg. 2007;32:696–701. doi: 10.1016/j.ejcts.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 17.Saehle T, Farahmand D, Eide PK, Tisell M, Wikkelso C. A randomized controlled dual-center trial on shunt complications in idiopathic normal-pressure hydrocephalus treated with gradually reduced or “fixed” pressure valve settings. J Neurosurg. 2014;121:1257–1263. doi: 10.3171/2014.7.JNS14283. [DOI] [PubMed] [Google Scholar]
- 18.Samuelson S, Long DM, Chou SN. Subdural hematoma as a complication of shunting procedures for normal pressure hydrocephalus. J Neurosurg. 1972;37:548–551. doi: 10.3171/jns.1972.37.5.0548. [DOI] [PubMed] [Google Scholar]
- 19.Smith ER, Butler WE, Barker FG. In-hospital mortality rates after ventriculoperitoneal shunt procedures in the United States, 1998 to 2000: relation to hospital and surgeon volume of care. J Neurosurg. 2004;100:90–97. doi: 10.3171/ped.2004.100.2.0090. [DOI] [PubMed] [Google Scholar]
- 20.Woodworth GF, McGirt MJ, Elfert P, Sciubba DM, Rigamonti D. Frameless stereotactic ventricular shunt placement for idiopathic intracranial hypertension. Stereotact and Funct Neurosurg. 2005;83:12–16. doi: 10.1159/000084059. [DOI] [PubMed] [Google Scholar]
- 21.Rosenberg ML, Corbett JJ, Smith C, et al. Cerebrospinal fluid diversion procedures in pseudotumor cerebri. Neurology. 1993;43:1071–1072. doi: 10.1212/wnl.43.6.1071. [DOI] [PubMed] [Google Scholar]
- 22.Abu-Serieh B, Ghassempour K, Duprez T, Raftopoulos C. Stereotactic ventriculoperitoneal shunting for refractory idiopathic intracranial hypertension. Neurosurgery. 2007;60:1039–1044. doi: 10.1227/01.NEU.0000255456.12978.31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.