Summary
Because of global epidemics of obesity and type 2 diabetes, the prevalence of non-alcoholic fatty liver disease (NAFLD) is increasing both in Europe and the United States, becoming one of the most frequent causes of chronic liver disease and predictably, one of the leading causes of liver transplantation both for end-stage liver disease and hepatocellular carcinoma. For most transplant teams around the world this will raise many challenges in terms of preand post-transplant management. Here we review the multifaceted impact of NAFLD on liver transplantation and will discuss: (1) NAFLD as a frequent cause of cryptogenic cirrhosis, end-stage chronic liver disease, and hepatocellular carcinoma; (2) prevalence of NAFLD as an indication for liver transplantation both in Europe and the United States; (3) the impact of NAFLD on the donor pool; (4) the access of NAFLD patients to liver transplantation and their management on the waiting list in regard to metabolic, renal and vascular comorbidities; (5) the prevalence and consequences of post-transplant metabolic syndrome, recurrent and de novo NAFLD; (6) the alternative management and therapeutic options to improve the long-term outcomes with particular emphasis on the correction and control of metabolic comorbidities.
Keywords: Fatty liver, Steatohepatitis, Liver transplantation
Introduction
Since its first description in the early 1980s as “a poorly understood and hitherto unnamed liver disease” [1], non-alcoholic fatty liver disease (NAFLD) has considerably evolved and progressively gained recognition among hepatologists, and has become, 30 years later, one of the most common causes of chronic liver disease [2–4]. Owing to its association with insulin resistance and metabolic risk factors, NAFLD is now considered the “hepatic manifestation” of metabolic syndrome (MS) and closely mirrors the global epidemics of obesity and type 2 diabetes [5–8]. In addition, NAFLD is the most common cause of elevated transaminases in the general population [2,9–11]. The prevalence of NAFLD in the general population ranges from 20% to 30% in Europe [12,13] and is as high as 46% in the United States [14]. Although initially considered as a disease of developed countries, due to emerging economies and adoption of a sedentary lifestyle and Western diet, the disease is also becoming increasingly prevalent in developing countries [11,15,16]. Nevertheless, because of the lack of reliable non-invasive diagnostic methods suitable for screening the general population, the real prevalence of NAFLD is likely still underestimated [11,17–19].
The spectrum of NAFLD covers two entities: simple steatosis and steatohepatitis (NASH), which is a progressive, fibrotic liver disease evolving to cirrhosis and its complications: hepatocellular carcinoma (HCC) and end-stage liver disease (ESLD) potentially requiring liver transplantation (LT). Owing to its increasing prevalence worldwide and to its recognition as a progressive severe liver disease, NAFLD has become the second leading cause of liver LT in the United States [20]. The absolute number of LT performed is roughly 6000 per year in both Europe and the United States [21,22]. However, the frequency of transplant for NAFLD has steadily increased and is expected to continue to do so, while that for other etiologies of chronic liver disease have decreased or remained unchanged in recent years [20,23]. If the pool of donors decreases, these trends will probably further accentuate the gap between the needs of patients with ESLD and the availability of donors.
In light of the growing impact of NAFLD on all facets of LT the purpose of this review is to discuss NAFLD in the context of LT, with particular emphasis on its rising frequency as an indication for LT, the outcome and management of patients with NAFLD on the waiting list, its impact on the LT donor pool, short and long-term outcomes after LT for patients with NAFLD, and finally, optimal management options.
Before liver transplantation
NAFLD as a common cause of cryptogenic cirrhosis, end-stage liver disease and hepatocellular carcinoma
For many years there was no recognition of a possible link between cardiometabolic risk factors and the development of “cryptogenic cirrhosis”, i.e., cirrhosis without an identifiable cause [24]. As a result cryptogenic cirrhosis was responsible for 3–30% of cirrhosis cases in the past series [25]. For the first time Powell et al. reported a gradual loss of steatosis during the progression of NASH towards cirrhosis, thus suggesting that some cases of “cryptogenic” cirrhosis may in fact be due to burned-out NASH lacking the distinctive steatotic features of NAFLD [26]. The demonstration that these cases of cryptogenic cirrhosis are bona-fide cases of advanced NASH was brought by Caldwell et al. who first reported a high prevalence of metabolic risk factors in these individuals [24]. The majority of patients initially defined as having cryptogenic cirrhosis were older females with previous or current history of obesity and type 2 diabetes. As the metabolic status is often modified in cirrhosis (altered glucose metabolism, malnutrition, ascites), it is difficult to evaluate the presence of concomitant metabolic risk factors. Therefore, past exposure to the metabolic risk factors should often be considered in cirrhotic patients. Using these criteria (either isolated histological features of NAFLD or past exposure to metabolic risk factors), NAFLD has been retrospectively identified as the underlying cause in 30%–75% of cryptogenic cirrhosis [24,27,28]. Supporting the hypothesis that NAFLD is a frequent cause of cryptogenic cirrhosis, an analysis of UNOS data between 1995 and 2005 revealed that during this period the proportion of NAFLD cirrhosis as an indication for LT increased from 0.01% to 3.5% while the proportion of cryptogenic cirrhosis proportionally decreased (from 9.6% to 6.6%). Physician awareness for NAFLD increased during the time period and more cases of cryptogenic cirrhosis are recognized as burned-out NASH [29].
Compared with other etiologies, NAFLD cirrhosis is diagnosed at an older age probably because of a slower fibrosis progression rate (on average 1 stage over 14 years) and decompensates later in life [30]. Due to its silent course, liver failure is often the first presentation at diagnosis of NAFLD-related cirrhosis (38%–45% of cases). In the early stages, (Child-Pugh A cirrhosis), the liver-related mortality rates are lower in NAFLD patients. Once cirrhosis decompensates (Child-Pugh B and C), patients with NAFLD have a rapidly progressive hepatic deterioration leading to similar overall and liver-related mortality as cirrhosis of other etiologies [31]. The main causes of death in patients with NAFLD were the same: infections and cirrhosis-related complications, mainly variceal hemorrhage, renal failure and HCC [31–33]. What differentiates the long-term prognosis of NAFLD from the other etiologies of cirrhosis is the cardiovascular (CV) mortality which is higher in patients with NAFLD [33].
A growing number of publications have linked insulin resistance, NAFLD, cryptogenic cirrhosis and HCC [31,34–36]. Although cirrhosis per se is a preneoplastic condition, both obesity and type 2 diabetes mellitus are recognized risk factors for HCC irrespective of the presence or the etiology of cirrhosis [36–40].
In the United States, the number of NAFLD-related HCC cases increased 9% annually between 2004 and 2009 [41]. In a European study, the referral for NAFLD-related HCC significantly increased during the same period (2005–2010) and accounted for 35% of all HCC recorded cases in 2010 [42]. Both American and European studies underline several characteristics of NAFLD-related HCC: (1) older age and higher prevalence of associated comorbidities; (2) occurrence in the absence of cirrhosis in 23%– 50% of cases; (3) lack of specific HCC surveillance in almost half of the cases; (4) more advanced stage at diagnosis, and (5) less accessibility to curative therapeutic options [41–44]. As HCC specific surveillance has not been proven to be cost-effective and it is not recommended by the current guidelines in the absence of cirrhosis [45], early diagnosis of NAFLD HCC in non-cirrhotic patients remains an unsolved issue.
NAFLD as indication for LT
The prevalence of NAFLD as an indication for LT for both ESLD and HCC has significantly increased both in Europe and in the United States. Based on a recent analysis of UNOS/OPTN registry, NAFLD is now the second most common etiology of chronic liver disease among individuals listed for LT in the United States [21]. Remarkably, during the past 10 years, the prevalence of NAFLD as an indication for LT has increased by 170%. During the same period, hepatitis C virus (HCV) and alcoholic cirrhosis as an indication for LT only increased by 14% and 45% respectively [20]. The percent of HCC cases attributable to NASH and cryptogenic cirrhosis has also significantly increased, from 8.2% in 2002 to 13.5% in 2012. While HCV is still the primary etiology of liver disease in HCC-related LT recipients, NAFLD has become the second leading etiology of liver disease in HCC-related LT recipients [46]. Furthermore, NAFLD accounted for a significant increase in simultaneous liver-kidney transplantation, from 8.2% in 2002 to 22% in 2011, while the proportion of simultaneous liver-kidney transplantation performed for HCV/alcoholic liver disease (ALD) decreased from 52% to 40% in the same period [47].
In contrast to UNOS data there is less information available from the European LT Registry regarding NAFLD as indication for LT. A total of 145 transplant centres in 26 European countries have performed 93,634 LT since 1968 (mostly in France 16,366 LT, Spain 15,714 LT, Great Britain 13,684 LT and Italy 11,697 LT) [22]. Over the last decades, alcoholic liver disease was the leading cause of LT (20%) followed by HCV and hepatitis B virus (HBV) (14% and 5%), while cryptogenic cirrhosis only accounted for 4% [22].
In the years to come, NAFLD will probably become the leading indication for LT because of: (1) the worldwide increasing prevalence of NAFLD paralleling the increasing prevalence of MS, diabetes and obesity; (2) the absence of a valid noninvasive diagnostic tool to allow the early diagnosis of the disease leading to the under recognition of NAFLD before the cirrhotic stage; (3) the absence of therapies that can effectively prevent disease progression; (4) the new direct-acting antiviral era and the possibility to cure HCV resulting in a stabilization or in a decreasing of the number of cases of HCV-related ESLD.
Outcomes of NAFLD on the waiting list for LT
Globally, patients with NAFLD on the waiting list for LT are older, have higher body mass index (BMI), higher prevalence of type 2 diabetes, metabolic comorbidities and lower glomerular filtration rate [20].
Several aspects should be particularly considered for NAFLD patients listed for LT. Morbid obesity (BMI ≥ 40 kg/m2) is often considered a contraindication for LT. Nevertheless, according to the 2013 OTPN/scientific registry of transplant patients (SRTR) annual data report [21], the proportion of obese (BMI ≥ 30 kg/m2) patients undergoing LT significantly increased over the past decade from 28% to 35.5%, with 3.6% patients having a BMI >40 kg/m2. While on the waiting list, patients with morbid obesity have a significantly higher model for end-stage liver disease (MELD) score, are less likely to be transplanted with MELD exception points and have a significant increase in resource utilization (altered functional status and physical capacity due to sarcopenic obesity, requiring hospitalization and specific management) [48]. Second, if listed with a MELD score of less than 15, NAFLD patients seem to have a longer waiting list period because of a slower disease progression rate (annual progression rate of 1.3 vs. 3.2 MELD points in NAFLD vs. HCV patients) [49]. Third, NAFLD patients are more likely to be removed from the waiting list because of associated comorbidities. Whereas HCV patients are removed from the waiting list mostly for psychological reasons and lack of social support, NAFLD patients are removed because of associated comorbidities, older age, impaired renal function and lower MELD [49]. After adjusting for MELD score, the short and long-term survival (90 day and 1 year, respectively) on the waiting list were lower in NAFLD than in alcoholic liver disease [20]. Fourth, a recent analysis of UNOS/OPTN database from 2003 to 2012 found a higher prevalence of portal vein thrombosis in patients with NAFLD cirrhosis when compared with other etiologies [50]. This is probably due to a procoagulant imbalance in NAFLD patients [51]. Portal vein thrombosis is associated with more complicated surgical procedures, increased post-transplant mortality and morbidity and, if extensive, may lead to patient’s drop out from the waiting list for LT [52,53]. Finally, owing to excess body weight, patients with NAFLD are more likely to develop the “small for size syndrome” and therefore are less likely to be eligible for living donors and split LT. As a consequence of the above-discussed aspects, the 1-year probability of receiving LT is significantly lower in NAFLD (40.5%) than in HCV or ALD (47% for both) [20].
Impact of NAFLD on the pool of potential donors
Recent data based on expected demographic trends in the United States and past donor utilization indicate a further exacerbation of the donor shortage for LT [54]. Older donor age, higher BMI and higher prevalence of diabetes were independent predictors for declining liver utilization in 21% of organ donors in United States in 2010 [55]. Assuming the actual trends in the prevalence of diabetes and obesity, it has been estimated that the overall liver graft utilization in 2030 will fall from 78% to 44% [56]. As the prevalence of fatty liver is increasing, it is expected that a higher proportion of potential donors will have steatosis or steatohepatitis and might be declined for LT use. The prevalence of biopsy-proven NAFLD among potential living donors ranged from 15% to 53% in different studies and disqualified 3%–21% of potential liver grafts [57].
Although an accurate assessment of liver steatosis in potential donors is required, there is no standard protocol for this evaluation. Some centers perform routine liver biopsy for all potential donors, while other centres only perform liver biopsy in selected high risk donors (older age, comorbidities, abnormal liver function tests). Assessment of steatosis through visual inspection of the graft has a positive predictive value of less than 20% for mild steatosis and only 70% for severe steatosis [58]. Surrogate markers of steatosis, like liver ultrasound coexisting with normal transaminases have also been proposed. However, among 492 living liver donors with normal transaminases and no evidence of steatosis at ultrasound, the prevalence of moderate to severe steatosis was 10% and 0.6% [59]. Computed tomography liver-to-spleen attenuation ratio is a reliable method to detect significant steatosis of >30% (sensitivity of 79% and specificity of 97%) [60]. However, these methods do not allow the qualitative assessment of steatosis and do not distinguish between microvesicular and macrovesicular steatosis.
Steatotic livers have reduced tolerance to ischemia due to lower adenosine triphosphate (ATP) stores and are at high risk of reperfusion injury mediated by a complex inflammatory response involving NFκB, Kupffer cells, cytokines and oxidative stress [61]. In contrast with macrovesicular steatosis, microvesicular steatosis does not have deleterious effects on graft survival and does not predispose to hepatic ischemia reperfusion injury [62].
Whereas liver grafts with <30% steatosis can be safely used for LT, livers with >60% steatosis are usually discarded because of increased probability of primary non-function (PNF). The use of grafts with 30–60% steatosis is controversial, as there are large discrepancies in reported PNF rates and 12-month graft survival [63]. In the largest study performed so far, macrovesicular steatosis of 20–30% in conjunction with prolonged cold ischemia of >11 h was an independent predictor for graft loss [64].
A recent study from Hong Kong provides insight into situations where severely steatotic (>60%) grafts may be used under certain conditions. Nineteen patients received severely steatotic grafts over a 24-year study period. There were no episodes of PNF and 1- and 3-year survival rates were similar to the control group. MELD scores among recipients were low (median 20), however, and cold ischemia times were short (384 min) [65]. Whether such excellent outcomes are generalizable to transplants performed with higher MELD recipients and longer cold ischemia times is unclear.
Several strategies have been developed to optimize results when using fatty liver grafts: shortened ischemia time, ischemic and pharmacological preconditioning of liver grafts to improve microcirculation and mitochondrial function [66,67] and the use of machine-based liver perfusion systems [68]. In addition to improving graft preservation, hypothermic and normothermic machines could also promote fat loss [69]. Promising experimental results have been obtained with hypothermic machine perfusion [70] and several randomized clinical trials are now ongoing to prospectively validate their use in clinical practice (NCT01317342, NCT02584283, NCT01274520, clinicaltrials.gov) [71]. As highlighted by a recent European experience, it is likely that the impact of reconditioning severely steatotic grafts by machine perfusion techniques is one of the paramount challenges in LT in the very next future [72].
After liver transplantation
Short and long-term outcomes and overall survival
The current results of LT in general are excellent, with 1-, 3-, and 6-month survival of 94%, 91%, and 88% respectively. The critical period after LT is the first 6 months with 49% of deaths and 65% of retransplantations occurring during this time interval [22].
Obesity, type 2 diabetes and CV morbidities are frequently associated with NAFLD and may also have a negative impact on short and long-term outcomes after LT. There have been several studies reporting conflicting results on the effects of obesity on post- LT outcomes with some of them showing a survival benefit after LT [73,74] or combined liver-kidney transplantation [75] regardless of the BMI. In a recent analysis of the UNOS database from 1987 through 2007, among 73,538 LT recipients, extreme BMI (<18.5 kg/m2 and >40 kg/m2) was a significant predictor of death after LT [76]. Nair et al., also reported that severe obesity (BMI >40 kg/m2) was an independent predictor of death among 18,172 transplant recipients both in the postoperative period but also at 1, 3, and 5 years after LT [77]. The negative impact of BMI seems to be even higher in conjunction with the severity of liver disease or associated comorbidities. High BMI (≥ 40 kg/m2) combined with a MELD score ≥ 22 was associated with 40% increase in mortality rate after LT [76]. In another study, combined obesity and type 2 diabetes was associated with a fourfold increase in the risk of early postoperative infections, CV events and acute renal failure, suggesting an additive negative impact of metabolic comorbidities [78]. Most of the studies both in Europe and US agree that morbid obesity increases LT resource utilization (longer operative time and transfusion requirements and longer intensive care unit and hospital stay) due to higher prevalence of early infections resulting in significantly higher costs ($134,000 for obese patients vs. 100,000 for non-obese patients) [77,79,80]. Because of a high prevalence of obesity, patients with NASH have a 50% increase in the length of hospital stay compared with other etiologies [81].
Long-term outcomes of LT in patients with NAFLD have been reported in several single-centre studies or analysis of national registries. Despite increased operative difficulties and a higher rate of postoperative complications, the overall long-term patient and graft survival at 1, 3, and 5 years seem to be similar to those of other indications in most studies [23,81–91] (Table 1). Instead, patients transplanted for NASH-HCC have decreased 5-year survival when compared with patients without NASH [92]. This could be due to the older age and more advanced stages of HCC in patients with NAFLD. Older age, BMI and associated metabolic comorbidities are the main modifiers of survival in NAFLD patients. Malik et al., described that in NAFLD patients, a BMI ≥ 30 kg/m2, together with type 2 diabetes, high blood pressure and age older than 60 years is associated with a one-year mortality of 50% after LT [82].
Table 1.
Long-term outcomes after LT for NASH.
| Author, year | Country, Period | Population, sample size | Mean MELD score |
Patient survival, % | Leading cause of death | ||
|---|---|---|---|---|---|---|---|
| 1 yr | 3 yr | 5 yr | |||||
| Malik, 2009 | US single center 1997–2008 |
NASH = 98 | 17 | 79% | 74% | 72% | Infections: 57% CV: 21% |
| Yalamanchili, 2010 | US single center 1986–2004 |
NASH = 18, CC = 239 | - | 85% | - | 71%* | CV: 21% Malignancies: 18% Infections: 15% |
| Bhagat, 2009 | US single center 1997–2007 |
NASH = 71 | - | 82% | 79% | 75% | Infections: 53% CV: 26% |
| Barritt, 2011 | US single center 2004–2007 |
NASH = 21 | 23 | 76% | 76% | - | Infections: 20% CV: 20% |
| Houlihan, 2011 | Israel, single center 2000–2008 |
NASH = 48 | 15 | 88% | - | 82% | CV events, sepsis |
| Park, 2011 | US single center 1998–2008 |
NASH = 9 | 13 | 78% | - | - | n.r. |
| Charlton, 2011 | US, SRTR registry 2001–2009 |
NASH = 1840 | - | 84% | 78% | No accurate information on causes of death or graft loss |
|
| Agopian 2012 | US single center 2002–2011 |
NASH = 144 | 33 | 84% | 75% | 70% | n.r. |
| Reddy, 2012 | US single center 2000–2010 |
NASH-HCC (LT) = 20 | 9 | - | 83% | - | Liver failure. Similar overall survival in patients with NASH and HCV/ ALD-related HCC |
| Van Wagner 2012 | US single center 1993–2010 |
NASH = 115 | 24 | 81% | 73% | 60% | Infections: 11% CV events: 9% |
| Kennedy 2012 | US single center 1999–2009 |
NASH = 129 | 23 | 90% | 88% | 85% | Infections: 38% CV events: 19% |
| Afzali 2012* | US, UNOS data- base 1997–2010 |
NASH = 1810; CC = 3843. | 21 | 87% | 81% | 75%* | Primary cause of death missing or unknown in 25% of the cases. CV events: 19% |
NASH and CC combined.
ALD, alcoholic liver disease; CC, cryptogenic cirrhosis; CV, cardiovascular; HBV, hepatitis B; HCV, hepatitis C; NASH, non-alcoholic steatohepatitis; PBC, primary biliary cirrhosis; PSC, primary sclerosing cholangitis; UNOS, United Network for organ sharing; SRTR, Scientific Registry for Transplant Recipients.
The main causes of death in patients with NAFLD following LT are sepsis and CV disease [92]. On the one hand, because of common metabolic risk factors and shared pathogenic pathways, patients with NAFLD have high prevalence of CV disease [93] and increased risk of CV mortality as compared with general population [94]. On the other hand, the 10-year probability for coronary heart disease and CV death is higher in LT patients as compared with the general population [95,96]. CV disease has emerged as the leading cause of non-graft related mortality and accounts for 11% of deaths at 1 year among LT recipients, regardless the etiology of chronic liver disease [97]. In a single-centre experience at the Mayo Clinic, the prevalence of CV events at 1, 5, and 8 years after LT was 10%, 21%, and 30%, with 40% of them being related to coronary artery disease and myocardial infarction [98]. As metabolic risk factors are still present after LT, it is expected that patients with NAFLD would remain at increased risk of CV disease following LT. One study reported that despite similar overall mortality, patients with NAFLD are more likely to develop CV complications within 1 year after LT (26%), even after controlling for traditional CV risk factors (age, sex, smoking status, pretransplant diabetes, and CV disease) [89]. These results emphasize the need for an individual approach and risk stratification according to the etiology of chronic liver disease and associated comorbidities. Current guidelines recommend further CV investigations with dobutamine stress, echocardiography and coronary angiography in patients older than 50 years with chronic smoking history, past medical or family history of heart disease or type 2 diabetes [99].
Post-transplant metabolic syndrome, recurrent and de novo NAFLD
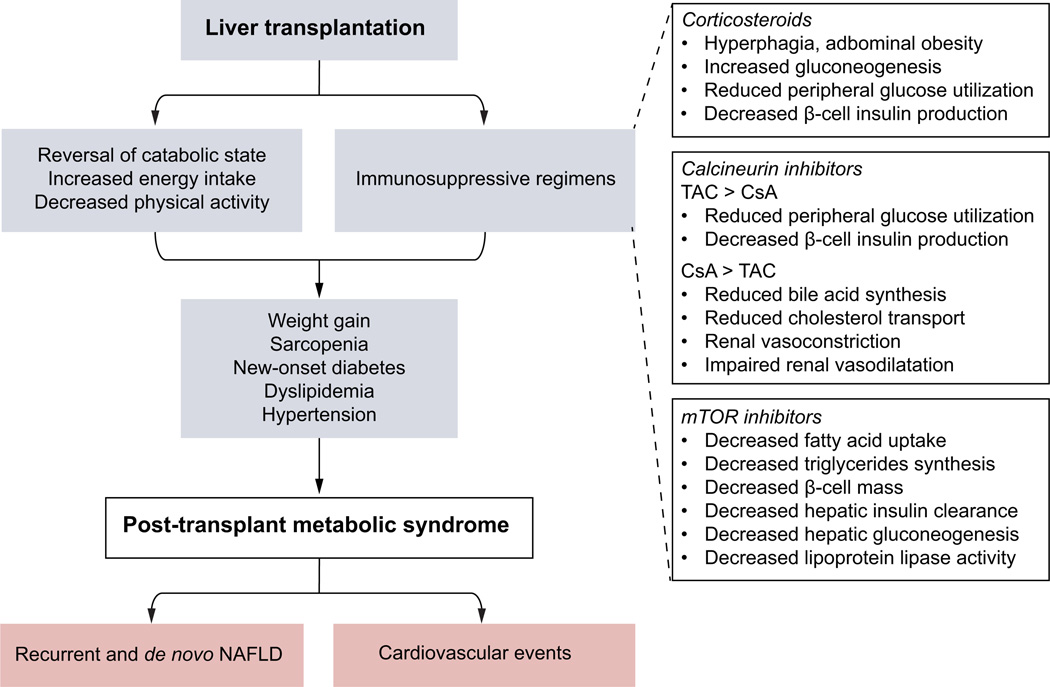
While LT treats the hepatic disease, the metabolic syndrome and associated extrahepatic comorbidities will obviously persist in the transplanted patient. Therefore, patients transplanted for NAFLD are at risk of developing recurrent NAFLD after LT, a risk that persists as long as the metabolic risk factors are still present. Moreover, the reversal of the cirrhosis-related catabolic state and the systemic effects of immunosuppressive regimens could promote the emergence or the worsening of metabolic abnormalities (Table 2). This may result in a posttransplant metabolic syndrome (PTMS) and de novo NAFLD (Fig. 1).
Table 2.
Effects of immunosuppressive regimens on PTMS components.
| PTMS features | Corticosteroids | Calcineurin inhibitors | mTOR inhibitors (sirolimus, everolimus) |
|
|---|---|---|---|---|
| Tacrolimus | Cyclosporine | |||
| Abdominal obesity | + | − | − | − |
| New-onset diabetes | +++ | ++ | + | − |
| Dyslipidemia | + | + | + | +++ |
| Hypertension | + | ++ | ++ | + |
Fig. 1.
Mechanisms and consequences of PTMS.
Post-transplant metabolic syndrome
Weight gain is common after LT and 30%–70% of patients become overweight or obese. The most rapid weight gain occurs in the first year following LT despite rapid tapering of corticosteroids: an average weight gain of 5 kg within the first year and 10 kg by 3 years after LT was noticed, mostly in patients older than 50 years and obese prior to LT [100]. Sarcopenic obesity (high fat mass and low muscle mass) after LT, owing to excess energy intake, decreased physical activity and older age [101], further induces insulin resistance and favors cardiometabolic comorbidities [102].
Because of glucose metabolism deregulation in cirrhosis, impaired glucose tolerance or type 2 diabetes are frequent before LT. Although glycogen synthesis ameliorates after LT, only a minority of patients will improve insulin sensitivity. The prevalence of post-transplant new onset diabetes ranges between 10% and 30% and is associated with corticosteroids and tacrolimus use [103,104]. Dyslipidemia occurs in 40%–70% of patients, mainly in relation with mammalian target of rapamycin (mTOR) inhibitors. Hypertension occurs in 65% of patients and is mostly related with the use of calcineurin inhibitors [105].
MS occurs in 40%–50% of patients after LT, both in patients with previous NAFLD but also in patients undergoing LT for other etiologies of chronic liver disease [106]. The risk of developing MS increases by 10% for each point-increase in BMI and is closely related with the immunosuppressive regimen. The commonly used immunosuppressive regimens (calcineurin inhibitors and mTORs) have been associated with an exacerbation of preexisting as well as the development of de novo MS [107].
Recurrent and de novo NAFLD
NAFLD is an emerging and prevalent condition after LT either in patients transplanted for NAFLD or cryptogenic cirrhosis (recurrent NAFLD) or in patients undergoing LT for other causes of chronic liver disease (de novo NAFLD) (Table 3). Recurrent NAFLD developed in 30%–60% of patients following LT during a follow-up period of 1–5 years [83,108]. One study reported 100% recurrence of NAFLD at 5 years post-LT in 27 patients transplanted for NASH or cryptogenic cirrhosis [109]. Although most of these patients have mild histological lesions, recurrent NASH may occur in 10%–33% of patients and advanced fibrosis in 5–10% (Table 3) [82–84,108–112]. De novo NAFLD occurs in 20%–30% of patients, but only a minority (5%–10%) will develop NASH and advanced fibrosis (2%–4%) (Table 3) [113–115]. However, most of these studies have important limitations: retrospective design, variable and short follow-up period, small number of patients and an important heterogeneity in patients’ selection and histological diagnosis of NAFLD.
Table 3.
Recurrent, de novo NAFLD and advanced fibrosis after LT.
| Study | Population, N | Time after LT |
NAFLD**,# | NASH# | Fibrosis# | Comments |
|---|---|---|---|---|---|---|
| Contos 2001* | NASH and CC N = 27 |
1 year | 52% | 11% | ≥F3: 4% | Time-dependent risk of allograft steatosis: at 5 years 100% of assessable patients developed fatty liver. Recurrent NASH developed later than fatty liver alone. Cumulative dose of steroids correlated with time to NAFLD development. |
| Charlton 2001* | NASH N = 15 |
1 year | 60% | 33% | ≥F2: 33% | Cirrhosis developed in 12.5% of patients. 1 patient required re-transplantation for graft failure after 27 months. |
| Ong 2001* | CC N = 51 |
2 years | 25.4% | 16% | ≥F3:4% | Bridging fibrosis occurred in patients with post LT NASH. |
| Seo 2007§ | Non-NAFLD CLD N = 68 |
2 years | 18% | 9% | - | Increase of BMI of >10% was associated with post LT NAFLD |
| Bhagat 2009* | NASH N = 64 |
>6 months | - | 33% | - | No cirrhosis or re-transplantation because of recurrent disease. 24% of patients developed graft failure over follow-up. |
| Malik 2009* | NASH N = 98 |
5 years | - | 25% | - | Recurrent NASH did not adversely affect survival. 6 patients in NASH group were re-transplanted within 60 days after LT. |
| Yalamanchili 2010* | NASH and CC N = 257 |
5 years | 31% (45% in NASH cirrhosis; 23% in CC) |
4% | ≥F3: 5% at 5 years; 10% at 10 years |
Advanced fibrosis was more frequent amount those with post LT NASH (31%) than simple steatosis (6%) |
| Dumortier 2010§ | Non-NAFLD CLD N = 421 |
>6 months | 31% | 5.3% | ≥F3: 2.25% | Most of the patients (52%) had grade 1 steatosis. The evolution of NAFLD during follow-up was: regression (48%), stability (22%), progression (30%). PTMS and liver graft steatosis were independent predictors of de novo NAFLD. |
| Dureja 2011* | NASH or CC N = 88 |
1 year | 39% | 28% | ≥F2: 9% | Only 9% of recurrent NAFLD had NAS ≥5. NAFLD recurrence was associated with increased risk for CV disease and correlated with post-transplant BMI, post LT TG levels and corticosteroids dose at 6 month. |
| El Attrache 2012* | NASH and CC N = 83 |
1.5 years | - | 24% | ≥F3: 3.6% | The recurrence rate was significantly higher amoung patients with PTMS (34% vs. 13% in patients without MS). 3 patients were re-transplanted secondary to graft failure from NASH recurrence. |
| Kim 2014§ | Non-NAFLD CLD N = 156 |
>1 year | 27.1% | 6.7% | F2: 4.4% | Obesity and donor graft steatosis were independent predictors for post LT NAFLD. |
Recurrent NAFLD;
de novo NAFLD;
NAFLD includes NASH;
% of patients with the outcome.
LT, liver transplantation; PTMS, post-transplant metabolic syndrome.
Several aspects need further attention. First, it is important to identify factors associated with NAFLD occurrence after LT. As the pathogenesis of NAFLD is closely linked to MS and insulin resistance and patients transplanted for NAFLD cirrhosis already have MS before LT, it is expected that the recurrence rate would be much higher than the occurrence rate of de novo NAFLD. Most of the studies concluded that the risk of developing NAFLD after LT is time-dependent and closely related to the presence of the MS or its individual components. In one study, the recurrence rate was significantly higher (34%) in patients with PTMS [112]. Dumortier et al., demonstrated a dose-dependent relationship between the number of MS components and the risk of developing de novo NAFLD: if one, two, three, four, five, or six metabolic risk factors were present the proportion of patients with de novo NAFLD gradually increased from 12% to 22%, 29%, 65%, 81%, and 100% respectively.
Obesity and donor graft steatosis seem to be also associated with a higher risk of NAFLD occurrence and suggests for a role of genetic predisposition [114,115]. This hypothesis has been confirmed by a recent study demonstrating that recipient’s but not donor’s PNPLA3 genotype was associated with increased risk of steatosis, supporting the role of extrahepatic (adipocyte) PNPLA3 activity in liver fat accumulation [116]. These results are reinforced by the study of Watt et al., that demonstrated that recipient but not the donor PNPLA3 genotype is associated with the risk of obesity and type 2 diabetes after LT [117].
Second, it is important to determine if the natural history of NAFLD is similar in pre- and post-transplant settings. Although direct evidence is lacking, indirect data suggest that the natural history of NAFLD is accelerated after LT. A minority of patients progressed from none to bridging fibrosis and cirrhosis in 1 or 2 years after LT outstripping the fibrosis progression rate from natural history studies in NAFLD patients [118].
Third, de novo and recurrent NAFLD seem to be two distinct entities with different natural course. A French study suggests that recurrent NAFLD is a more severe disease with an earlier onset than de novo NAFLD. In this study, steatosis disappeared in 22% of patients with de novo NAFLD and none of the patients with recurrent NAFLD, while bridging fibrosis occurred at 5 years in 71% of patients with recurrent NAFLD vs. 12.5% of patients with de novo NAFLD [119]. The fibrosis progression rate seems to be higher in patients with recurrent vs. de novo NAFLD, possibly in relation with a longer exposure to metabolic risk factors and a more severe insulin resistance. However, prospective studies with longer follow-up are needed to determine the impact of recurrent and de novo NAFLD on longterm outcomes of patients undergoing LT.
How to optimize the outcome of NAFLD patients undergoing LT
Because of the increasing prevalence of NAFLD and its impact on LT, efforts should be done both to facilitate the access of patients with NAFLD to LT and to prevent them developing metabolic-related complications following LT.
Before liver transplantation
The first step would be to prevent NAFLD patients to develop ESLD. This requires an early diagnosis and appropriate therapeutic management. 10–15% of patients with NAFLD have cirrhosis at diagnosis, which reflect the absence of a reliable screening tool [120]. Therefore, it is important to increase the awareness for NAFLD and to develop reliable diagnostic and prognostic models to identify patients at risk for disease progression.
Unfortunately, none of the pharmacological agents now on the market proved any efficacy in reversing NASH or significant fibrosis. Glitazones were the most promising drugs tested so far in NASH, with reversal of histological features (except fibrosis) [121,122] but with a concern on their safety profile (weight gain and congestive heart failure) that warranted a black box warning. Vitamin E has also shown some efficacy in the treatment of NASH, however only a minority of patients studied showed histological improvements. Besides the long-term safety of vitamin E is also unknown [123–125]. Several promising drugs targeting various pathogenic pathways (farnesoid × receptor (FXR) and TGR5 – obeticholic acid, dual peroxisome proliferator-activated receptor alpha/delta agonists – GFT505, CCR2 – CCR5 antagonist – cenicriviroc, anti-LOXL2 monoclonal antibodies – simtuzumab) are now in the pipeline and are being tested in phase IIb clinical trials, with promising effect on the reversal of fibrosis and resolution of NASH [126].
Second, among patients with end-stage NAFLD it is important to select those that will best benefit from LT. This can be challenging and different transplant centres may have different risk tolerances depending on transplant volume and experience. As NAFLD has only recently been recognized as a significant liver transplant issue, guidelines for the transplant assessment of the NAFLD patient have been slow to evolve. European Association for the Study of the Liver (EASL) recommends that MS comorbidities be assessed and controlled in the pre- and post-transplant setting [127]. In the American Association for the Study of Liver Diseases (AASLD) and American Society for Transplantation practice guidelines [128] for LT in adults, there are no NAFLD specific directives, other than LT is an effective therapy for NAFLD cirrhosis. However, many of the comorbidities found in NAFLD patients deserve particular attention during the evaluation.
Obesity is highly prevalent among patients with NAFLD and is considered a relative contraindication to transplantation [128] due to poor operative outcomes [79]. In the United States, Medicaid policy limits evaluation to those with a BMI less than 35 kg/m2 and many centres will not transplant or even evaluate patients with a BMI above 40 kg/m2 [129]. All obese patients (BMI >30 kg/m2) should receive dietary counselling prior to LT. Dietary and lifestyle changes proved an acceptable efficacy in patients with NAFLD but the effect is difficult to sustain even in non-cirrhotic patients [130,131]. A small pilot study demonstrated that adapted physical activity may improve the index of fitness and the quality of life in cirrhotic patients listed for LT [132]. Additionally, weight loss may reduce portal hypertension as well [133]. However, if lifestyle changes alone can reverse severe cirrhotic NASH is still unproven.
Bariatric surgery prior to LT could be considered as it could both induce weight loss and improve NASH. Significant weight loss following bariatric surgery results in a reduction of obesity-related comorbid conditions (such as hypertension, type 2 diabetes, sleep apnea) and also in histological improvement in NAFLD patients [134]. In cirrhotic patients awaiting LT, portal hypertension is one of the major limits for bariatric surgery. In a retrospective analysis that included almost 4000 cirrhotic patients undergoing bariatric surgery, the mortality rates in patients with compensated cirrhosis were 0.9% but increased to 16% in patients with decompensated cirrhosis [135]. A recent study reported excellent results of combined LT and sleeve gastrectomy. None of the patients died or developed post- LT diabetes or steatosis and all have a sustained weight loss (from a mean BMI of 48 kg/m2 to a mean BMI of 29 kg/m2) [136]. Only limited experience is available for bariatric surgery performed after LT. 22 cases have been reported with a complication rate following the procedure of 32% and an overall mortality rate of 13.6% [137].
Diabetes is associated with post-transplant infections and worse patient outcomes [85,138] and should be optimally controlled prior to transplant. Some centres consider poorly controlled diabetes with end organ damage (e.g., neuropathy, retinopathy) a contraindication for transplantation.
Elements of the MS also increase the risk of significant coronary artery disease (CAD) and NAFLD itself is considered an independent risk factor for CAD and atherosclerosis [139,140]. The transplant evaluation requires a thorough cardiovascular work up and coronary stenoses >70% should be considered for revascularization [128]. A clear strategy for revascularization can be challenging and controversial, however. Stent placement will require one and occasionally two anti-platelet agents, potentially delaying transplant and revascularization by coronary artery bypass grafting is associated with high morbidity and mortality in patients with decompensated cirrhosis [141,142].
Many patients with NAFLD cirrhosis are older and while chronologic age is not a contraindication for LT, the physiologic age should be considered as these patients likely will have multiple comorbidities.
Overall it is up to the transplant centre to decide what level of risk is reasonable for patient and program alike, but it is nearly universally agreed that obese patients with poorly controlled diabetes and risk factors for CAD make poor transplant candidates.
After liver transplantation
The present guidelines make no specific recommendation for the prevention or treatment of NAFLD in LT recipients other than the correction and the optimal control of individual components of MS and CV risk factors [99,127].
Despite an improved functional status after LT, only one quarter of patients are physically active [143,144]. A systematic review of randomised control trial comparing the outcomes of exercise training programs in solid organ recipients found no significant improvements in exercise capacity, CV risk factors or the incidence of new onset type 2 diabetes [145]. Smaller studies have shown improvements in body composition and exercise capacity when diet and exercise programs are initiated early after transplant [146].
Up to two-thirds of patients have increased caloric intake after LT [147] but little data are available about nutritional composition [146]. Nutritional interventions in the peri-operative time period have not demonstrated any benefits [148]. As the greatest weight gain occurs in the first year following LT [100], the dietary interventions should be implemented early after LT following the recommendations of specific guidelines for the management of overweight and obesity [149]. However, it makes intuitive sense that longer-term programs might be helpful, especially for NAFLD patients.
Because of the metabolic side effects of immunosuppressive regimens (weight gain and insulin resistance, hypertension, atherogenic dyslipidemia), modulating immunosuppressive regimens may partially avoid the PTMS and contribute to the reduction of CV risk in LT recipients [107]. Although there are increasing evidences that steroids avoidance and minimization of calcineurins inhibitors may reduce the risk of PTMS, further prospective studies are needed.
Conclusion
NAFLD has a multifaceted impact on LT that extends to both transplant recipients and organ donors. The increasing prevalence of NAFLD along with the prevalence of obesity and diabetes will likely result in a higher proportion of steatotic livers proposed for LT. Therefore, the LT community will have to face the choice of either accepting lower quality steatotic livers with possibly higher post-LT complication rates and inferior outcomes, or to discard these livers with the risk of further accentuating the shortage of the donor pool leading to a longer wait-list time, more complications related to ESLD on the waiting list and probably higher wait-list mortality. Both scenarios are likely to increase the health care resource utilization and costs related to LT.
NAFLD is now the second indication for LT in the United States. Following the actual trends in the prevalence of obesity and diabetes worldwide it is likely that NAFLD will become the leading cause of LT both in Europe and in United States. The long-term outcomes of patients transplanted for NAFLD cirrhosis are not inferior to patients transplanted for other etiologies. However, patients with NAFLD have some particularities – mainly older age, obesity and other metabolic comorbidities that most likely impact either the wait-list period or the short term-outcomes. Both short and long-term outcomes of patients with NAFLD are marked by a higher risk to develop CV complications. Therefore, further efforts should be focused on the assessment and the management of NAFLD patients on the waiting list in order to maximize their chances to access to LT and to minimize the risk of complications after LT. Although LT ameliorates liver-related morbidity, as metabolic risk factors are still present, these patients are at increased risk of disease recurrence after LT. Further efforts should be done to manage and prevent the PTMS and the risk of occurrence/recurrence of NAFLD after LT. Long-term follow-up studies should be conducted in LT recipients to allow a better understanding of the mechanisms underlying the disease recurrence and to develop strategies to improve outcomes.
Key point.
NAFLD is becoming the leading cause of liver transplantation for both end-stage liver disease and hepatocellular carcinoma in the United States.
Patients with NAFLD listed for liver transplantation are more often removed from the waiting list because of associated comorbidities and older age.
Because of the rising prevalence of steatosis in the general population, the shortage of liver grafts will increase in the future. The use of fatty liver grafts will require optimization of surgical and graft preservation techniques.
Patients with NAFLD are at higher risk of cardiovascular morbidity and mortality following liver transplantation.
NAFLD recurrence is frequent after liver transplantation, mostly because of the persistence of metabolic risk factors. Further efforts should be done for an optimal control of metabolic comorbidities after liver transplantation.
Footnotes
Conflict of interest
The authors who have taken part in this study declared that they do not have anything to disclose regarding funding or conflict of interest with respect to this manuscript.
Authors’ contributions
Raluca Pais, Sidney Barritt, and Vlad Ratziu: wrote the manuscript; Raluca Pais, Vlad Ratziu, and Filomena Conti: manuscript design and conception; Yvon Calmus, Olivier Scatton, Thomas Runge, Pascal Lebray, Thierry Poynard: critical revision of the manuscript.
References
- 1.Ludwig J, Viggiano TR, McGill DB, et al. Nonalcoholic steatohepatitis: Mayo Clinic experiences with a hitherto unnamed disease. Mayo Clin Proc. 1980;55:434–438. [PubMed] [Google Scholar]
- 2.Ekstedt M, Franzen LE, Mathiesen UL, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44:865–873. doi: 10.1002/hep.21327. [DOI] [PubMed] [Google Scholar]
- 3.Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34:274–285. doi: 10.1111/j.1365-2036.2011.04724.x. [DOI] [PubMed] [Google Scholar]
- 4.Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10:686–690. doi: 10.1038/nrgastro.2013.171. [DOI] [PubMed] [Google Scholar]
- 5.Kotronen A, Yki-Jarvinen H. Fatty liver: a novel component of the metabolic syndrome. Arterioscler Thromb Vasc Biol. 2008;28:27–38. doi: 10.1161/ATVBAHA.107.147538. [DOI] [PubMed] [Google Scholar]
- 6.Leite NC, Salles GF, Araujo AL, et al. Prevalence and associated factors of nonalcoholic fatty liver disease in patients with type-2 diabetes mellitus. Liver Int. 2009;29:113–119. doi: 10.1111/j.1478-3231.2008.01718.x. [DOI] [PubMed] [Google Scholar]
- 7.Adams LA, Waters OR, Knuiman MW, et al. NAFLD as a risk factor for the development of diabetes and the metabolic syndrome: an eleven-year follow-up study. Am J Gastroenterol. 2009;104:861–867. doi: 10.1038/ajg.2009.67. [DOI] [PubMed] [Google Scholar]
- 8.Younossi ZM, Stepanova M, Afendy M, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol. 2011;9:524.e1–530.e1. doi: 10.1016/j.cgh.2011.03.020. quiz e60. [DOI] [PubMed] [Google Scholar]
- 9.Clark J. The prevalence and etiology of elevated aminotransferase levels in the United States. Am J Gastroenterol. 2003;98:960–967. doi: 10.1111/j.1572-0241.2003.07486.x. [DOI] [PubMed] [Google Scholar]
- 10.Ioannou GN, Weiss NS, Boyko EJ, et al. Elevated serum alanine aminotransferase activity and calculated risk of coronary heart disease in the United States. Hepatology. 2006;43:1145–1151. doi: 10.1002/hep.21171. [DOI] [PubMed] [Google Scholar]
- 11.Lazo M, Clark JM. The epidemiology of nonalcoholic fatty liver disease: a global perspective. Semin Liver Dis. 2008;28:339–350. doi: 10.1055/s-0028-1091978. [DOI] [PubMed] [Google Scholar]
- 12.Armstrong MJ, Houlihan DD, Bentham L, et al. Presence and severity of nonalcoholic fatty liver disease in a large prospective primary care cohort. J Hepatol. 2012;56:234–240. doi: 10.1016/j.jhep.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 13.Bedogni G, Miglioli L, Masutti F, et al. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Hepatology. 2005;42:44–52. doi: 10.1002/hep.20734. [DOI] [PubMed] [Google Scholar]
- 14.Williams CD, Stengel J, Asike MI, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140:124–131. doi: 10.1053/j.gastro.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 15.Das K, Das K, Mukherjee PS, et al. Nonobese population in a developing country has a high prevalence of nonalcoholic fatty liver and significant liver disease. Hepatology. 2010;51:1593–1602. doi: 10.1002/hep.23567. [DOI] [PubMed] [Google Scholar]
- 16.Farrell GC, Wong VW, Chitturi S. NAFLD in Asia–as common and important as in the West. Nat Rev Gastroenterol Hepatol. 2013;10:307–318. doi: 10.1038/nrgastro.2013.34. [DOI] [PubMed] [Google Scholar]
- 17.Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592–1609. doi: 10.1053/j.gastro.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Lazo M, Hernaez R, Eberhardt MS, et al. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988–1994. Am J Epidemiol. 2013;178:38–45. doi: 10.1093/aje/kws448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ratziu V, Voiculescu M, Poynard T. Touching some firm ground in the epidemiology of NASH. J Hepatol. 2012;56:23–25. doi: 10.1016/j.jhep.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 20.Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148:547–555. doi: 10.1053/j.gastro.2014.11.039. [DOI] [PubMed] [Google Scholar]
- 21.Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2013 Annual Data Report: liver. Am J Transplant. 2015;15:1–28. doi: 10.1111/ajt.13197. [DOI] [PubMed] [Google Scholar]
- 22.Adam R, Karam V, Delvart V, et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR) J Hepatol. 2012;57:675–688. doi: 10.1016/j.jhep.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 23.Charlton MR, Burns JM, Pedersen RA, et al. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology. 2011;141:1249–1253. doi: 10.1053/j.gastro.2011.06.061. [DOI] [PubMed] [Google Scholar]
- 24.Caldwell SH, Oelsner DH, Iezzoni JC, et al. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology. 1999;29:664–669. doi: 10.1002/hep.510290347. [DOI] [PubMed] [Google Scholar]
- 25.Greeve M, Ferrell L, Kim M, et al. Cirrhosis of undefined pathogenesis: absence of evidence for unknown viruses or autoimmune processes. Hepatology. 1993;17:593–598. doi: 10.1002/hep.1840170411. [DOI] [PubMed] [Google Scholar]
- 26.Powell EE, Cooksley WGE, Hanson R, et al. The natural history of nonalcoholic steatohepatitis: a follow-up study of forty-two patients for up to 21 years. Hepatology. 1990;11:74–80. doi: 10.1002/hep.1840110114. [DOI] [PubMed] [Google Scholar]
- 27.Poonawala A, Nair SP, Thuluvath PJ. Prevalence of obesity and diabetes in patients with cryptogenic cirrhosis: a case-control study. Hepatology. 2000;32:689–692. doi: 10.1053/jhep.2000.17894. [DOI] [PubMed] [Google Scholar]
- 28.Ayata G, Gordon FD, Lewis WD, et al. Cryptogenic cirrhosis: clinicopathologic findings at and after liver transplantation. Hum Pathol. 2002;33:1098–1104. doi: 10.1053/hupa.2002.129419. [DOI] [PubMed] [Google Scholar]
- 29.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–1231. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 30.Younossi ZM, Gramlich T, Bacon BR, et al. Hepatic iron and nonalcoholic fatty liver disease. Hepatology. 1999;30:847–850. doi: 10.1002/hep.510300407. [DOI] [PubMed] [Google Scholar]
- 31.Ratziu V, Bonyhay L, Di Martino V, et al. Survival, liver failure, and hepatocellular carcinoma in obesity-related cryptogenic cirrhosis. Hepatology. 2002;35:1485–1493. doi: 10.1053/jhep.2002.33324. [DOI] [PubMed] [Google Scholar]
- 32.Bhala N, Angulo P, van der Poorten D, et al. The natural history of nonalcoholic fatty liver disease with advanced fibrosis or cirrhosis: an international collaborative study. Hepatology. 2011;54:1208–1216. doi: 10.1002/hep.24491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sanyal AJ, Banas C, Sargeant C, et al. Similarities and differences in outcomes of cirrhosis due to nonalcoholic steatohepatitis and hepatitis C. Hepatology. 2006;43:682–689. doi: 10.1002/hep.21103. [DOI] [PubMed] [Google Scholar]
- 34.Ong JP, Pitts A, Younossi ZM. Increased overall mortality and liver-related mortality in non-alcoholic fatty liver disease. J Hepatol. 2008;49:608–612. doi: 10.1016/j.jhep.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 35.Bugianesi E. Expanding the natural history of nonalcoholic steatohepatitis: from cryptogenic cirrhosis to hepatocellular carcinoma. Gastroenterology. 2002;123:134–140. doi: 10.1053/gast.2002.34168. [DOI] [PubMed] [Google Scholar]
- 36.Marrero JA, Fontana RJ, Fu S, et al. Alcohol, tobacco and obesity are synergistic risk factors for hepatocellular carcinoma. J Hepatol. 2005;42:218–224. doi: 10.1016/j.jhep.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 37.Nair S, Mason A, Eason J, et al. Is obesity an independent risk factor for hepatocellular carcinoma in cirrhosis? Hepatology. 2002;36:150–155. doi: 10.1053/jhep.2002.33713. [DOI] [PubMed] [Google Scholar]
- 38.Hassan MM, Curley SA, Li D, et al. Association of diabetes duration and diabetes treatment with the risk of hepatocellular carcinoma. Cancer. 2010;116:1938–1946. doi: 10.1002/cncr.24982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ascha MS, Hanouneh IA, Lopez R, et al. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology. 2010;51:1972–1978. doi: 10.1002/hep.23527. [DOI] [PubMed] [Google Scholar]
- 40.Pais R, Lebray P, Rousseau G, et al. Nonalcoholic fatty liver disease increases the risk of hepatocellular carcinoma in patients with alcohol-associated cirrhosis awaiting liver transplants. Clin Gastroenterol Hepatol. 2015;13:992.e2–999.e2. doi: 10.1016/j.cgh.2014.10.011. [DOI] [PubMed] [Google Scholar]
- 41.Younossi ZM, Otgonsuren M, Henry L, et al. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004 to 2009. Hepatology. 2015;62:1723–1730. doi: 10.1002/hep.28123. [DOI] [PubMed] [Google Scholar]
- 42.Dyson J, Jaques B, Chattopadyhay D, et al. Hepatocellular cancer – the impact of obesity, type 2 diabetes and a multidisciplinary team. J Hepatol. 2014;60:110–117. doi: 10.1016/j.jhep.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 43.Mittal S, Sada YH, El-Serag HB, et al. Temporal trends of nonalcoholic fatty liver disease-related hepatocellular carcinoma in the veteran affairs population. Clin Gastroenterol Hepatol. 2015;13:594.e1–601.e1. doi: 10.1016/j.cgh.2014.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Piscaglia F, Svegliati-Baroni G, Barchetti A, et al. Clinical patterns of hepatocellular carcinoma (hcc) in non alcoholic fatty liver disease (NAFLD): a multicenter prospective study. Hepatology. 2016;63:827–838. doi: 10.1002/hep.28368. [DOI] [PubMed] [Google Scholar]
- 45.EASL clinical practical guidelines: management of alcoholic liver disease. J Hepatol. 2012;57:399–420. doi: 10.1016/j.jhep.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 46.Wong RJ, Cheung R, Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology. 2014;59:2188–2195. doi: 10.1002/hep.26986. [DOI] [PubMed] [Google Scholar]
- 47.Singal AK, Salameh H, Kuo YF, et al. Evolving frequency and outcomes of simultaneous liver kidney transplants based on liver disease etiology. Transplantation. 2014;98:216–221. doi: 10.1097/TP.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 48.Singhal A, Wilson GC, Wima K, et al. Impact of recipient morbid obesity on outcomes after liver transplantation. Transpl Int. 2015;28:148–155. doi: 10.1111/tri.12483. [DOI] [PubMed] [Google Scholar]
- 49.O’Leary JG, Landaverde C, Jennings L, et al. Patients with NASH and cryptogenic cirrhosis are less likely than those with hepatitis C to receive liver transplants. Clin Gastroenterol Hepatol. 2011;9:700.e1–704.e1. doi: 10.1016/j.cgh.2011.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stine JG, Shah NL, Argo CK, et al. Increased risk of portal vein thrombosis in patients with cirrhosis due to Non-Alcoholic Steatohepatitis (NASH) Liver Transpl. 2015;21:1016–1021. doi: 10.1002/lt.24134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tripodi A, Fracanzani AL, Primignani M, et al. Procoagulant imbalance in patients with non-alcoholic fatty liver disease. J Hepatol. 2014;61:148–154. doi: 10.1016/j.jhep.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 52.Englesbe MJ, Schaubel DE, Cai S, et al. Portal vein thrombosis and liver transplant survival benefit. Liver Transpl. 2010;16:999–1005. doi: 10.1002/lt.22105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Francoz C, Valla D, Durand F. Portal vein thrombosis, cirrhosis, and liver transplantation. J Hepatol. 2012;57:203–212. doi: 10.1016/j.jhep.2011.12.034. [DOI] [PubMed] [Google Scholar]
- 54.Parikh ND, Hutton D, Marrero W, et al. Projections in donor organs available for liver transplantation in the United States: 2014–2025. Liver Transpl. 2015;21:855–863. doi: 10.1002/lt.24136. [DOI] [PubMed] [Google Scholar]
- 55.Orman ES, Barritt ASt, Wheeler SB, et al. Declining liver utilization for transplantation in the United States and the impact of donation after cardiac death. Liver Transpl. 2013;19:59–68. doi: 10.1002/lt.23547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Orman ES, Mayorga ME, Wheeler SB, et al. Declining liver graft quality threatens the future of liver transplantation in the United States. Liver Transpl. 2015;21:1040–1050. doi: 10.1002/lt.24160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Minervini MI, Ruppert K, Fontes P, et al. Liver biopsy findings from healthy potential living liver donors: reasons for disqualification, silent diseases and correlation with liver injury tests. J Hepatol. 2009;50:501–510. doi: 10.1016/j.jhep.2008.10.030. [DOI] [PubMed] [Google Scholar]
- 58.Jun MJ, Shim JH, Kim SY, et al. Clinical implications of preoperative and intraoperative liver biopsies for evaluating donor steatosis in living related liver transplantation. Liver Transpl. 2014;20:437–445. doi: 10.1002/lt.23832. [DOI] [PubMed] [Google Scholar]
- 59.Ahn JS, Sinn DH, Gwak GY, et al. Steatosis among living liver donors without evidence of fatty liver on ultrasonography: potential implications for preoperative liver biopsy. Transplantation. 2013;95:1404–1409. doi: 10.1097/TP.0b013e31828d1588. [DOI] [PubMed] [Google Scholar]
- 60.Rogier J, Roullet S, Cornelis F, et al. Noninvasive assessment of macrovesicular liver steatosis in cadaveric donors based on computed tomography liverto- spleen attenuation ratio. Liver Transpl. 2015;21:690–695. doi: 10.1002/lt.24105. [DOI] [PubMed] [Google Scholar]
- 61.Abu-Amara M, Yang SY, Tapuria N, et al. Liver ischemia/reperfusion injury: processes in inflammatory networks–a review. Liver Transpl. 2010;16:1016–1032. doi: 10.1002/lt.22117. [DOI] [PubMed] [Google Scholar]
- 62.Han S, Ha SY, Park CK, et al. Microsteatosis may not interact with macrosteatosis in living donor liver transplantation. J Hepatol. 2015;62:556–562. doi: 10.1016/j.jhep.2014.10.027. [DOI] [PubMed] [Google Scholar]
- 63.McCormack L, Dutkowski P, El-Badry AM, et al. Liver transplantation using fatty livers: always feasible? J Hepatol. 2011;54:1055–1062. doi: 10.1016/j.jhep.2010.11.004. [DOI] [PubMed] [Google Scholar]
- 64.Spitzer AL, Lao OB, Dick AA, et al. The biopsied donor liver: incorporating macrosteatosis into high-risk donor assessment. Liver Transpl. 2010;16:874–884. doi: 10.1002/lt.22085. [DOI] [PubMed] [Google Scholar]
- 65.Wong TC, Fung JY, Chok KS, et al. Excellent outcomes of liver transplantation using severely steatotic grafts from brain-dead donors. Liver Transpl. 2016;22:226–236. doi: 10.1002/lt.24335. [DOI] [PubMed] [Google Scholar]
- 66.Bejaoui M, Pantazi E, Folch-Puy E, et al. Emerging concepts in liver graft preservation. World J Gastroenterol. 2015;21:396–407. doi: 10.3748/wjg.v21.i2.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Compagnon P, Lindell S, Ametani MS, et al. Ischemic preconditioning and liver tolerance to warm or cold ischemia: experimental studies in large animals. Transplantation. 2005;79:1393–1400. doi: 10.1097/01.tp.0000164146.21136.0b. [DOI] [PubMed] [Google Scholar]
- 68.Weeder PD, van Rijn R, Porte RJ. Machine perfusion in liver transplantation as a tool to prevent non-anastomotic biliary strictures: rationale, current evidence and future directions. J Hepatol. 2015;63:265–275. doi: 10.1016/j.jhep.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 69.Nagrath D, Xu H, Tanimura Y, et al. Metabolic preconditioning of donor organs: defatting fatty livers by normothermic perfusion ex vivo. Metab Eng. 2009;11:274–283. doi: 10.1016/j.ymben.2009.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Compagnon P, Clement B, Campion JP, et al. Effects of hypothermic machine perfusion on rat liver function depending on the route of perfusion. Transplantation. 2001;72:606–614. doi: 10.1097/00007890-200108270-00008. [DOI] [PubMed] [Google Scholar]
- 71.Dutkowski P, Schlegel A, de Oliveira M, et al. HOPE for human liver grafts obtained from donors after cardiac death. J Hepatol. 2014;60:765–772. doi: 10.1016/j.jhep.2013.11.023. [DOI] [PubMed] [Google Scholar]
- 72.Tandoi F, Salizzoni M, Brunati A, et al. Excellent outcomes of liver transplantation using severely steatotic grafts from brain-dead donors. Liver Transpl. 2016;22:377–378. doi: 10.1002/lt.24362. [DOI] [PubMed] [Google Scholar]
- 73.Leonard J, Heimbach JK, Malinchoc M, et al. The impact of obesity on long-term outcomes in liver transplant recipients-results of the NIDDK liver transplant database. Am J Transplant. 2008;8:667–672. doi: 10.1111/j.1600-6143.2007.02100.x. [DOI] [PubMed] [Google Scholar]
- 74.Pelletier SJ, Schaubel DE, Wei G, et al. Effect of body mass index on the survival benefit of liver transplantation. Liver Transpl. 2007;13:1678–1683. doi: 10.1002/lt.21183. [DOI] [PubMed] [Google Scholar]
- 75.Pelletier SJ, Maraschio MA, Schaubel DE, et al. Survival benefit of kidney and liver transplantation for obese patients on the waiting list. Clin Transpl. 2003:77–88. [PubMed] [Google Scholar]
- 76.Dick AA, Spitzer AL, Seifert CF, et al. Liver transplantation at the extremes of the body mass index. Liver Transpl. 2009;15:968–977. doi: 10.1002/lt.21785. [DOI] [PubMed] [Google Scholar]
- 77.Nair S, Verma S, Thuluvath PJ. Obesity and its effect on survival in patients undergoing orthotopic liver transplantation in the United States. Hepatology. 2002;35:105–109. doi: 10.1053/jhep.2002.30318. [DOI] [PubMed] [Google Scholar]
- 78.Dare AJ, Plank LD, Phillips AR, et al. Additive effect of pretransplant obesity, diabetes, and cardiovascular risk factors on outcomes after liver transplantation. Liver Transpl. 2014;20:281–290. doi: 10.1002/lt.23818. [DOI] [PubMed] [Google Scholar]
- 79.Hakeem AR, Cockbain AJ, Raza SS, et al. Increased morbidity in overweight and obese liver transplant recipients: a single-center experience of 1325 patients from the United Kingdom. Liver Transpl. 2013;19:551–562. doi: 10.1002/lt.23618. [DOI] [PubMed] [Google Scholar]
- 80.Nair S, Cohen DB, Cohen MP, et al. Postoperative morbidity, mortality, costs, and long-term survival in severely obese patients undergoing orthotopic liver transplantation. Am J Gastroenterol. 2001;96:842–845. doi: 10.1111/j.1572-0241.2001.03629.x. [DOI] [PubMed] [Google Scholar]
- 81.Agopian VG, Kaldas FM, Hong JC, et al. Liver transplantation for nonalcoholic steatohepatitis: the new epidemic. Ann Surg. 2012;256:624–633. doi: 10.1097/SLA.0b013e31826b4b7e. [DOI] [PubMed] [Google Scholar]
- 82.Malik SM, Devera ME, Fontes P, et al. Recurrent disease following liver transplantation for nonalcoholic steatohepatitis cirrhosis. Liver Transpl. 2009;15:1843–1851. doi: 10.1002/lt.21943. [DOI] [PubMed] [Google Scholar]
- 83.Yalamanchili K, Saadeh S, Klintmalm GB, et al. Nonalcoholic fatty liver disease after liver transplantation for cryptogenic cirrhosis or nonalcoholic fatty liver disease. Liver Transpl. 2010;16:431–439. doi: 10.1002/lt.22004. [DOI] [PubMed] [Google Scholar]
- 84.Bhagat V, Mindikoglu AL, Nudo CG, et al. Outcomes of liver transplantation in patients with cirrhosis due to nonalcoholic steatohepatitis versus patients with cirrhosis due to alcoholic liver disease. Liver Transpl. 2009;15:1814–1820. doi: 10.1002/lt.21927. [DOI] [PubMed] [Google Scholar]
- 85.Barritt ASt, Dellon ES, Kozlowski T, et al. The influence of nonalcoholic fatty liver disease and its associated comorbidities on liver transplant outcomes. J Clin Gastroenterol. 2011;45:372–378. doi: 10.1097/MCG.0b013e3181eeaff0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Houlihan DD, Armstrong MJ, Davidov Y, et al. Renal function in patients undergoing transplantation for nonalcoholic steatohepatitis cirrhosis: time to reconsider immunosuppression regimens? Liver Transpl. 2011;17:1292–1298. doi: 10.1002/lt.22382. [DOI] [PubMed] [Google Scholar]
- 87.Park CW, Tsai NT, Wong LL. Implications of worse renal dysfunction and medical comorbidities in patients with NASH undergoing liver transplant evaluation: impact on MELD and more. Clin Transplant. 2011;25:E606–E611. doi: 10.1111/j.1399-0012.2011.01497.x. [DOI] [PubMed] [Google Scholar]
- 88.Reddy SK, Steel JL, Chen HW, et al. Outcomes of curative treatment for hepatocellular cancer in nonalcoholic steatohepatitis versus hepatitis C and alcoholic liver disease. Hepatology. 2012;55:1809–1819. doi: 10.1002/hep.25536. [DOI] [PubMed] [Google Scholar]
- 89.Vanwagner LB, Bhave M, Te HS, et al. Patients transplanted for nonalcoholic steatohepatitis are at increased risk for postoperative cardiovascular events. Hepatology. 2012;56:1741–1750. doi: 10.1002/hep.25855. [DOI] [PubMed] [Google Scholar]
- 90.Kennedy C, Redden D, Gray S, et al. Equivalent survival following liver transplantation in patients with non-alcoholic steatohepatitis compared with patients with other liver diseases. HPB (Oxford) 2012;14:625–634. doi: 10.1111/j.1477-2574.2012.00497.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Afzali A, Berry K, Ioannou GN. Excellent posttransplant survival for patients with nonalcoholic steatohepatitis in the United States. Liver Transpl. 2012;18:29–37. doi: 10.1002/lt.22435. [DOI] [PubMed] [Google Scholar]
- 92.Wang X, Li J, Riaz DR, et al. Outcomes of liver transplantation for nonalcoholic steatohepatitis: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2014;12:394.e1–402.e1. doi: 10.1016/j.cgh.2013.09.023. [DOI] [PubMed] [Google Scholar]
- 93.Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013;10:330–344. doi: 10.1038/nrgastro.2013.41. [DOI] [PubMed] [Google Scholar]
- 94.Soderberg C, Stal P, Askling J, et al. Decreased survival of subjects with elevated liver function tests during a 28-year follow-up. Hepatology. 2010;51:595–602. doi: 10.1002/hep.23314. [DOI] [PubMed] [Google Scholar]
- 95.Johnston SD, Morris JK, Cramb R, et al. Cardiovascular morbidity and mortality after orthotopic liver transplantation. Transplantation. 2002;73:901–906. doi: 10.1097/00007890-200203270-00012. [DOI] [PubMed] [Google Scholar]
- 96.Neal DA, Tom BD, Luan J, et al. Is there disparity between risk and incidence of cardiovascular disease after liver transplant? Transplantation. 2004;77:93–99. doi: 10.1097/01.TP.0000100685.70064.90. [DOI] [PubMed] [Google Scholar]
- 97.Watt KD, Pedersen RA, Kremers WK, et al. Evolution of causes and risk factors for mortality post-liver transplant: results of the NIDDK long-term follow-up study. Am J Transplant. 2010;10:1420–1427. doi: 10.1111/j.1600-6143.2010.03126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Fussner LA, Heimbach JK, Fan C, et al. Cardiovascular disease after liver transplantation. When, what and who is at risk. Liver Transpl. 2015;21:889–896. doi: 10.1002/lt.24137. [DOI] [PubMed] [Google Scholar]
- 99.Newsome PN, Allison ME, Andrews PA, et al. Guidelines for liver transplantation for patients with non-alcoholic steatohepatitis. Gut. 2012;61:484–500. doi: 10.1136/gutjnl-2011-300886. [DOI] [PubMed] [Google Scholar]
- 100.Richards J, Gunson B, Johnson J, et al. Weight gain and obesity after liver transplantation. Transpl Int. 2005;18:461–466. doi: 10.1111/j.1432-2277.2004.00067.x. [DOI] [PubMed] [Google Scholar]
- 101.Choudhary NS, Saigal S, Saraf N, et al. Sarcopenic obesity with metabolic syndrome: a newly recognized entity following living donor liver transplantation. Clin Transplant. 2015;29:211–215. doi: 10.1111/ctr.12505. [DOI] [PubMed] [Google Scholar]
- 102.Hong HC, Hwang SY, Choi HY, et al. Relationship between sarcopenia and nonalcoholic fatty liver disease: the Korean Sarcopenic Obesity Study. Hepatology. 2014;59:1772–1778. doi: 10.1002/hep.26716. [DOI] [PubMed] [Google Scholar]
- 103.Bianchi G, Marchesini G, Marzocchi R, et al. Metabolic syndrome in liver transplantation: relation to etiology and immunosuppression. Liver Transpl. 2008;14:1648–1654. doi: 10.1002/lt.21588. [DOI] [PubMed] [Google Scholar]
- 104.Heisel O, Heisel R, Balshaw R, et al. New onset diabetes mellitus in patients receiving calcineurin inhibitors: a systematic review and meta-analysis. Am J Transplant. 2004;4:583–595. doi: 10.1046/j.1600-6143.2003.00372.x. [DOI] [PubMed] [Google Scholar]
- 105.Pagadala M, Dasarathy S, Eghtesad B, et al. Posttransplant metabolic syndrome: an epidemic waiting to happen. Liver Transpl. 2009;15:1662–1670. doi: 10.1002/lt.21952. [DOI] [PubMed] [Google Scholar]
- 106.Watt KD, Charlton MR. Metabolic syndrome and liver transplantation: a review and guide to management. J Hepatol. 2010;53:199–206. doi: 10.1016/j.jhep.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 107.Watt KD. Metabolic syndrome: is immunosuppression to blame? Liver Transpl. 2011;17:S38–S42. doi: 10.1002/lt.22386. [DOI] [PubMed] [Google Scholar]
- 108.Charlton M, Kasparova P, Weston S, et al. Frequency of nonalcoholic steatohepatitis as a cause of advanced liver disease. Liver Transpl. 2001;7:608–614. doi: 10.1053/jlts.2001.25453. [DOI] [PubMed] [Google Scholar]
- 109.Contos MJ, Cales W, Sterling RK, et al. Development of nonalcoholic fatty liver disease after orthotopic liver transplantation for cryptogenic cirrhosis. Liver Transpl. 2001;7:363–373. doi: 10.1053/jlts.2001.23011. [DOI] [PubMed] [Google Scholar]
- 110.Ong J, Younossi ZM, Reddy V, et al. Cryptogenic cirrhosis and posttransplantation nonalcoholic fatty liver disease. Liver Transpl. 2001;7:797–801. doi: 10.1053/jlts.2001.24644. [DOI] [PubMed] [Google Scholar]
- 111.Dureja P, Mellinger J, Agni R, et al. NAFLD recurrence in liver transplant recipients. Transplantation. 2011;91:684–689. doi: 10.1097/TP.0b013e31820b6b84. [DOI] [PubMed] [Google Scholar]
- 112.El Atrache MM, Abouljoud MS, Divine G, et al. Recurrence of non-alcoholic steatohepatitis and cryptogenic cirrhosis following orthotopic liver transplantation in the context of the metabolic syndrome. Clin Transplant. 2012;26:E505–E512. doi: 10.1111/ctr.12014. [DOI] [PubMed] [Google Scholar]
- 113.Dumortier J, Giostra E, Belbouab S, et al. Non-alcoholic fatty liver disease in liver transplant recipients: another story of “seed and soil”. Am J Gastroenterol. 2010;105:613–620. doi: 10.1038/ajg.2009.717. [DOI] [PubMed] [Google Scholar]
- 114.Seo S, Maganti K, Khehra M, et al. De novo nonalcoholic fatty liver disease after liver transplantation. Liver Transpl. 2007;13:844–847. doi: 10.1002/lt.20932. [DOI] [PubMed] [Google Scholar]
- 115.Kim H, Lee K, Lee KW, et al. Histologically proven non-alcoholic fatty liver disease and clinically related factors in recipients after liver transplantation. Clin Transplant. 2014;28:521–529. doi: 10.1111/ctr.12343. [DOI] [PubMed] [Google Scholar]
- 116.Finkenstedt A, Auer C, Glodny B, et al. Patatin-like phospholipase domain-containing protein 3 rs738409-G in recipients of liver transplants is a risk factor for graft steatosis. Clin Gastroenterol Hepatol. 2013;11:1667–1672. doi: 10.1016/j.cgh.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 117.Watt KD, Dierkhising R, Fan C, et al. Investigation of PNPLA3 and IL28B genotypes on diabetes and obesity after liver transplantation: insight into mechanisms of disease. Am J Transplant. 2013;13:2450–2457. doi: 10.1111/ajt.12355. [DOI] [PubMed] [Google Scholar]
- 118.Singh S, Allen AM, Wang Z, et al. Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol. 2015;13:643.e9–654.e9. doi: 10.1016/j.cgh.2014.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Vallin M, Guillaud O, Boillot O, et al. Recurrent or de novo nonalcoholic fatty liver disease after liver transplantation: natural history based on liver biopsy analysis. Liver Transpl. 2014;20:1064–1071. doi: 10.1002/lt.23936. [DOI] [PubMed] [Google Scholar]
- 120.Cusi K, Chang Z, Harrison S, et al. Limited value of plasma cytokeratin-18 as a biomarker for NASH and fibrosis in patients with non-alcoholic fatty liver disease. J Hepatol. 2014;60:167–174. doi: 10.1016/j.jhep.2013.07.042. [DOI] [PubMed] [Google Scholar]
- 121.Ratziu V, Charlotte F, Bernhardt C, et al. Long-term efficacy of rosiglitazone in nonalcoholic steatohepatitis: results of the fatty liver improvement by rosiglitazone therapy (FLIRT 2) extension trial. Hepatology. 2010;51:445–453. doi: 10.1002/hep.23270. [DOI] [PubMed] [Google Scholar]
- 122.Aithal GP, Thomas JA, Kaye PV, et al. Randomized, placebo-controlled trial of pioglitazone in nondiabetic subjects with nonalcoholic steatohepatitis. Gastroenterology. 2008;135:1176–1184. doi: 10.1053/j.gastro.2008.06.047. [DOI] [PubMed] [Google Scholar]
- 123.Lippman SM, Klein EA, Goodman PJ, et al. Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the Selenium and Vitamin E Cancer Prevention Trial (SELECT) JAMA. 2009;301:39–51. doi: 10.1001/jama.2008.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Schurks M, Glynn RJ, Rist PM, et al. Effects of vitamin E on stroke subtypes: meta-analysis of randomised controlled trials. BMJ. 2010;341:c5702. doi: 10.1136/bmj.c5702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bjelakovic G, Nikolova D, Simonetti RG, et al. Antioxidant supplements for preventing gastrointestinal cancers. Cochrane Database Syst Rev. 2008:Cd004183. doi: 10.1002/14651858.CD004183.pub3. [DOI] [PubMed] [Google Scholar]
- 126.Ratziu V, Goodman Z, Sanyal A. Current efforts and trends in the treatment of NASH. J Hepatol. 2015;62:S65–S75. doi: 10.1016/j.jhep.2015.02.041. [DOI] [PubMed] [Google Scholar]
- 127.EASL Clinical Practice Guidelines: Liver transplantation. J Hepatol. 2016;64:433–485. doi: 10.1016/j.jhep.2015.10.006. [DOI] [PubMed] [Google Scholar]
- 128.Martin P, DiMartini A, Feng S, et al. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59:1144–1165. doi: 10.1002/hep.26972. [DOI] [PubMed] [Google Scholar]
- 129.Halegoua-De Marzio DL, Wong SY, Fenkel JM, et al. Listing practices for morbidly obese patients at liver transplantation centers in the United States. Exp Clin Transplant. 2016 doi: 10.6002/ect.2015.0247. [DOI] [PubMed] [Google Scholar]
- 130.Promrat K, Kleiner DE, Niemeier HM, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010;51:121–129. doi: 10.1002/hep.23276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Sacks FM, Bray GA, Carey VJ, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360:859–873. doi: 10.1056/NEJMoa0804748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Debette-Gratien M, Tabouret T, Antonini MT, et al. Personalized adapted physical activity before liver transplantation: acceptability and results. Transplantation. 2015;99:145–150. doi: 10.1097/TP.0000000000000245. [DOI] [PubMed] [Google Scholar]
- 133.Berzigotti A, Albillos A, Villanueva C, et al. Lifestyle intervention by a 16-week programme of supervised diet and physical exercise ameliorates portal hypertension in patients with cirrhosis and obesity-the SportDiet study. Hepatology. 2014;60:253A. doi: 10.1002/hep.28992. [DOI] [PubMed] [Google Scholar]
- 134.Lassailly G, Caiazzo R, Buob D, et al. Bariatric surgery reduces features of non-alcoholic steatohepatitis in morbidly obese patients. Gastroenterology. 2015;149:379–388. doi: 10.1053/j.gastro.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 135.Mosko JD, Nguyen GC. Increased perioperative mortality following bariatric surgery among patients with cirrhosis. Clin Gastroenterol Hepatol. 2011;9:897–901. doi: 10.1016/j.cgh.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 136.Heimbach JK, Watt KD, Poterucha JJ, et al. Combined liver transplantation and gastric sleeve resection for patients with medically complicated obesity and end-stage liver disease. Am J Transplant. 2013;13:363–368. doi: 10.1111/j.1600-6143.2012.04318.x. [DOI] [PubMed] [Google Scholar]
- 137.Lazzati A, Iannelli A, Schneck AS, et al. Bariatric surgery and liver transplantation: a systematic review a new frontier for bariatric surgery. Obes Surg. 2015;25:134–142. doi: 10.1007/s11695-014-1430-8. [DOI] [PubMed] [Google Scholar]
- 138.Yoo HY, Thuluvath PJ. The effect of insulin-dependent diabetes mellitus on outcome of liver transplantation. Transplantation. 2002;74:1007–1012. doi: 10.1097/00007890-200210150-00019. [DOI] [PubMed] [Google Scholar]
- 139.Francque SM, van der Graaff D, Kwanten WJ. Non-alcoholic fatty liver disease and cardiovascular risk: Pathophysiological mechanisms and implications. J Hepatol. 2016;65:425–443. doi: 10.1016/j.jhep.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 140.Pais R, Giral P, Khan JF, et al. Fatty liver is an independent predictor of early carotid atherosclerosis. J Hepatol. 2016;65:95–102. doi: 10.1016/j.jhep.2016.02.023. [DOI] [PubMed] [Google Scholar]
- 141.Azarbal B, Poommipanit P, Arbit B, et al. Feasibility and safety of percutaneous coronary intervention in patients with end-stage liver disease referred for liver transplantation. Liver Transpl. 2011;17:809–813. doi: 10.1002/lt.22301. [DOI] [PubMed] [Google Scholar]
- 142.Marui A, Kimura T, Tanaka S, et al. Coronary revascularization in patients with liver cirrhosis. Ann Thorac Surg. 2011;91:1393–1399. doi: 10.1016/j.athoracsur.2011.01.022. [DOI] [PubMed] [Google Scholar]
- 143.Robinson LR, Switala J, Tarter RE, et al. Functional outcome after liver transplantation: a preliminary report. Arch Phys Med Rehabil. 1990;71:426–427. [PubMed] [Google Scholar]
- 144.Aadahl M, Hansen BA, Kirkegaard P, et al. Fatigue and physical function after orthotopic liver transplantation. Liver Transpl. 2002;8:251–259. doi: 10.1053/jlts.2002.31743. [DOI] [PubMed] [Google Scholar]
- 145.Didsbury M, McGee RG, Tong A, et al. Exercise training in solid organ transplant recipients: a systematic review and meta-analysis. Transplantation. 2013;95:679–687. doi: 10.1097/TP.0b013e31827a3d3e. [DOI] [PubMed] [Google Scholar]
- 146.Krasnoff JB, Vintro AQ, Ascher NL, et al. A randomized trial of exercise and dietary counseling after liver transplantation. Am J Transplant. 2006;6:1896–1905. doi: 10.1111/j.1600-6143.2006.01391.x. [DOI] [PubMed] [Google Scholar]
- 147.Roske AE, Plauth M. Liver transplantation, body composition, and substrate utilization: does organ transplantation normalize the metabolic situation of the patient? Nutrition. 1999;15:504–505. doi: 10.1016/s0899-9007(99)00058-1. [DOI] [PubMed] [Google Scholar]
- 148.Langer G, Grossmann K, Fleischer S, et al. Nutritional interventions for liver-transplanted patients. Cochrane Database Syst Rev. 2012:Cd007605. doi: 10.1002/14651858.CD007605.pub2. [DOI] [PubMed] [Google Scholar]
- 149.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63:2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]