Abstract
Objective
Gout and rheumatoid arthritis (RA) are the two most common forms of inflammatory arthritis worldwide. As hospitalizations for both conditions lead to substantial health resource use, contemporary inpatient trends and associated costs may provide important benchmarks of disease burden. However, relevant data are limited.
Methods
We used PopulationData BC, a population-based administrative dataset from Canada. We examined trends in the annual hospitalization and surgery rate of gout and RA from 2000-2011. We additionally examined annual trends in the inpatient cost burden of both conditions. We assessed annual trends in hospitalization and surgery rates using Poisson regression models and cost trends using linear regression models.
Results
From 2000 to 2011, the annual hospitalization rate for RA declined by 49% from 15.4 to 7.9 per 100,000 Canadian adults (p<0.001), whereas that for gout doubled from 3.8 to 7.6 per 100,000 Canadian adults (p<0.001). Approximately 31% of RA admissions were associated with hip or knee replacement surgery; the trend of these surgeries paralleled the declining trend in RA hospitalizations (p=0.0097). The inpatient costs also reflected the hospitalization trends, with a 40% decrease in RA hospital costs, while gout costs more than doubled over the study period.
Conclusion
Our findings indicate that hospitalization rates for gout have doubled over the past decade, while those for RA have decreased considerably. While these data provide an encouraging benchmark for RA care, they also highlight the critical need to improve gout management and prevention to mitigate its rising disease burden in Canada and beyond.
Keywords: Gout, Rheumatoid Arthritis, Hospitalization, Trend Analysis, Health Care Costs
INTRODUCTION
Gout and rheumatoid arthritis (RA) are the two most common forms of inflammatory arthritis worldwide. As hospitalizations for both conditions lead to substantial health resource use, contemporary inpatient trends and associated costs may provide important benchmarks of disease burden. For example, a previous study during the pre-biologic era found that hospital costs accounted for more than half of the total medical costs of RA [1]. Indeed, varying levels of perceived success in care and changing epidemiology may have substantially impacted the hospitalization trends of RA and gout over the past decade. For example, new potent drugs (e.g., biologics), effective combination therapy, and management strategies (e.g., treating to target, early RA intervention) have become increasingly adopted for RA care [2]; however, whether these perceived improvements have been translated into a reduction in hospitalization rates and costs among RA patients in recent years is largely unknown. In contrast, despite the availability of effective pharmacological options, gout management remains remarkably suboptimal with a high rate of recurrent attacks [3]. Further, the prevalence and incidence of gout have been increasing worldwide [4]. Nevertheless, as in RA, whether these factors have translated to rising hospitalization trends among gout patients also remains unclear.
Thus, to fill this important knowledge gap, we evaluated contemporary hospitalization trends for gout and RA in a Canadian general population context from 2000 to 2011. We examined both conditions concurrently as we hypothesized contrasting trends over the past decade, and as each condition could serve as the other's internal comparison group.
METHODS
Study Design and Population
We utilized PopulationData BC (PopData), a population-based dataset spanning the entire Canadian province of British Columbia (BC). PopData captures all provincially-funded health care services, including hospital admissions and discharges (http://www.popdata.bc.ca/data). We included patients at least 18 years of age who were hospitalized during the study period with a principal diagnosis of either gout (ICD-9-CM 274 or ICD-10-CA M10) or RA (ICD-9-CM 714 or ICD-10-CA M05 or M06). We studied the temporal hospitalization trends of RA and gout, both among the overall population as well as according to age and sex, using data from 2000-2011.
We also assessed the trend of hospitalizations for total hip and knee replacements among study patients, as we anticipated the main reason for hospitalization with a principal discharge diagnosis of RA would be for these joint-related surgeries. All joint surgeries were identified using the Canadian Classification of Diagnostic, Therapeutic, and Surgical Procedures (CCP) and Canadian Classification of Health Interventions (CCI). Furthermore, we evaluated the inpatient economic burden for both conditions using Resource Intensity Weights (a standardized provincial estimate of expected resource consumption that takes into account length of hospital stay, diagnoses, procedures performed, and patient demographics) determined by the Canadian Institute for Health Information.
Statistical Analysis
We calculated annual rates of hospitalizations (expressed per 100,000 Canadian adults) for gout and RA. We assessed annual trends in hospitalization and surgery rates using Poisson regression models that included a variable representing the linear trend from the baseline year of 2000; a similar analysis was conducted for hospitalization costs with linear regression . Costs were inflation-adjusted to 2011 Canadian dollars using the Consumer Price Index. All p-values were 2-sided with a significance threshold of p<0.05. Statistical analyses were performed using SAS Version 9.4 (SAS Institute, Cary, North Carolina).
No personal identifying information was made available as part of this study. All procedures used were conducted in compliance with BC's Freedom of Information and Privacy Protection Act. Ethics approval was obtained from the University of British Columbia.
RESULTS
Characteristics of the Study Populations
We identified 4604 and 2136 hospitalizations for RA and gout, respectively, between 2000 and 2011. Approximately 68% of hospitalizations with a principal diagnosis of gout were for males, and approximately 76% were 65 years or older. Conversely, 77% of hospitalizations with a principal diagnosis of RA were for females, and approximately 44% were 65 years or older. The demographics for both conditions were stable throughout the study period.
Hospitalization Trends of Gout and RA
From 2000 to 2011, the annual hospitalization rate for those with a principal diagnosis of RA declined by 49% from 15.4 to 7.9 per 100,000 Canadian adults (p<0.001), whereas that for gout increased by 100% (i.e., doubled) from 3.8 to 7.6 per 100,000 Canadian adults (p<0.001) (Figure 1 and Table 1). Thus, at the beginning of the study period, hospitalizations for RA were approximately 4 times more frequent than those for gout; however, these opposing trends of the two conditions led to similar hospitalization rates by 2011 (i.e., 7.9 and 7.6 per 100,000 Canadian adults for RA and gout, respectively). These trends persisted in subgroups according to age and sex (Table 1). The length of stay for both conditions remained stable over the study period, with a median stay of 4 and 5 days for RA and gout, respectively.
Figure 1.
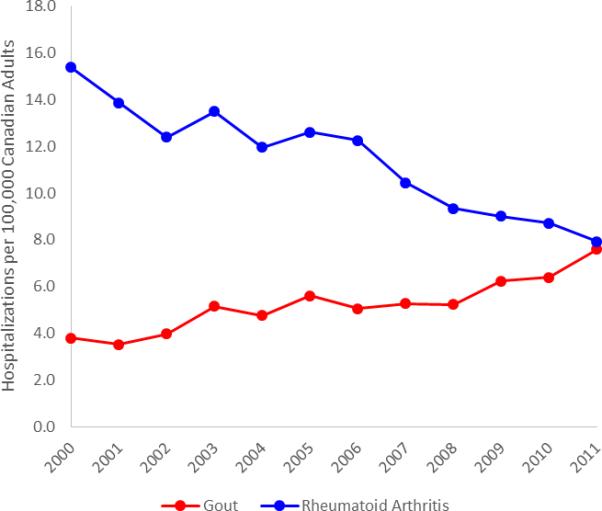
Annual rate of hospitalization for patients with a principal diagnosis of gout (red) or rheumatoid arthritis (blue)
Table 1.
Gout and Rheumatoid Arthritis Hospitalizations per 100,000 Canadian Adults
| Year | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | P for trend |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Gout
| |||||||||||||
| Overall | 3.8 | 3.5 | 4.0 | 5.2 | 4.8 | 5.6 | 5.1 | 5.3 | 5.2 | 6.2 | 6.4 | 7.6 | <0.001 |
| Sex | |||||||||||||
| Male | 5.0 | 4.9 | 5.5 | 7.3 | 7.1 | 7.6 | 7.0 | 6.6 | 7.7 | 8.5 | 8.8 | 10.7 | <0.001 |
| Female | 2.6 | 2.2 | 2.5 | 3.1 | 2.6 | 3.7 | 3.2 | 4.0 | 2.8 | 4.0 | 4.0 | 4.5 | <0.001 |
| Age Group | |||||||||||||
| <65 years | 1.1 | 1.1 | 1.2 | 1.5 | 1.6 | 1.6 | 1.3 | 1.6 | 1.6 | 1.8 | 1.8 | 2.2 | 0.001 |
| 65+ years | 16.9 | 15.2 | 17.3 | 22.9 | 20.0 | 24.8 | 22.5 | 22.3 | 22.0 | 26.5 | 26.8 | 30.7 | <0.001 |
|
Rheumatoid Arthritis
| |||||||||||||
| Overall | 15.4 | 13.9 | 12.4 | 13.5 | 12.0 | 12.6 | 12.3 | 10.4 | 9.3 | 9.0 | 8.7 | 7.9 | <0.001 |
| Sex | |||||||||||||
| Male | 6.9 | 6.2 | 5.3 | 6.3 | 5.5 | 6.2 | 6.2 | 5.0 | 4.1 | 3.9 | 3.8 | 3.7 | <0.001 |
| Female | 23.5 | 21.3 | 19.3 | 20.4 | 18.2 | 18.8 | 18.1 | 15.7 | 14.4 | 14.0 | 13.5 | 12.0 | <0.001 |
| Age Group | |||||||||||||
| <65 years | 10.9 | 9.3 | 8.2 | 9.4 | 7.6 | 8.3 | 8.0 | 7.2 | 6.3 | 6.6 | 6.3 | 5.2 | <0.001 |
| 65+ years | 37.5 | 36.3 | 32.7 | 33.3 | 32.7 | 33.2 | 32.3 | 25.4 | 23.3 | 20.1 | 19.4 | 19.5 | <0.001 |
Trends in Joint Replacement Surgery
Approximately 31% of hospitalizations with a principal discharge diagnosis of RA were associated with total hip or knee replacement. From 2000 to 2011, the rate of these surgeries in patients with a principal discharge diagnosis of RA decreased from 3.8 to 2.9 per 100,000 Canadian adults (p=0.0097).
Costs of Gout and RA Hospitalizations
The inflation-adjusted inpatient costs with a principal diagnosis of gout more than doubled over the study period from $19,426 to $43,783 (2011 CAD) per 100,000 Canadian adults (p<0.001), whereas those for RA decreased by 40% from $103,314 to $62,348 per 100,000 Canadian adults (p=0.0023) over the same period.
DISCUSSION
Our findings indicate that hospitalization rates for those with a principal diagnosis of gout have doubled over the past decade, while those for RA have decreased substantially. These opposing trends were also reflected by the inpatient cost burden. Our findings support perceived improvements in RA care over recent decades, including the use of effective therapies and management strategies [2]. Our data are also consistent with the widely-reported suboptimal care of gout patients [3], in addition to the increasing incidence and prevalence of the disease worldwide [4]. Thus, while these findings provide an encouraging benchmark for the improvement in RA care over the past decade, they also highlight the critical need to improve gout management and prevention to mitigate its rising disease burden in Canada and beyond.
From 2000 to 2011, we found that hospitalizations with a principal diagnosis of RA had progressively declined (i.e., nearly halved), and the corresponding costs showed a similar declining trend. These trends are meaningful as more than half of the total medical costs of RA during the pre-biologic era were for hospitalizations [1], and our data suggest that the contribution of hospitalizations to the costs of modern RA care (specifically during the biologic era) are substantially lower. As the incidence of RA among Canadians has previously been found to be stable during the study period [5], these trends should reflect the improvements in RA care over the past decade, including the use of effective therapies (e.g., methotrexate, combination therapy, and biologics) and management strategies (e.g., treating to target, early RA intervention) [2]. For example, a recent analysis of 57 UK hospitals found a 46% decline in RA inpatient days between 1996 and 2010, while also reporting a tripling in methotrexate prescriptions between 2001 and 2012 and a 156% annual increase in the use of TNF inhibitors [6]. These changes have likely contributed to the declining rates of severe systemic complications of RA (e.g., rheumatoid vasculitis, splenectomy for Felty's syndrome, and cervical fusion) observed previously [7], as well as reduced rates of major joint surgeries as observed in our study.
Our finding of a declining rate in joint replacement surgery in RA patients is generally consistent with the results of previous analyses from other settings, including California state data (1983-2007) [8], 57 UK hospitals (1996-2010) [6], and 8 German practices (2002-2011) [9]. Notably, these decreasing trends among RA patients contrast the overall dramatic increase of these surgeries among the Canadian general population [10]. For example, according to the Canadian Joint Replacement Registry, the number of hip and knee replacements increased by 101% between 1995-1996 and 2005-2006 (i.e., a 10-year period) and by 17% between 2004-2005 and 2005-2006 [10].
In contrast, we found a doubling of the annual hospitalization rate (adjusted for population growth) for patients with a principal diagnosis of gout over the study period. A recent study found a similarly increasing number of primary gout hospitalizations in New Zealand and England between 1999-2009, although hospitalization rates were not reported [11]. Moreover, our inpatient trends are consistent with the increasing incidence of gout in Canada over the same study period (i.e., a 30% increase) [12]. However, this magnitude of increase appears substantially smaller than that of gout hospitalizations, as above.
Thus, these increasing inpatient trends are highly likely due to suboptimal gout care [3], which has been shown to contribute to many avoidable hospitalizations. For example, a recent abstract highlighted that up to 89% of hospitalizations with a primary diagnosis of gout were preventable, owing to inefficient or inadequate care [13]. For example, although the vast majority of gout patients are indicated for urate-lowering therapy (ULT) (e.g., 87% within 5 years of diagnosis), only a small proportion receive treatment [14]. Further, despite the well-established serum uric acid target (i.e., ≤ 5 or 6mg/dL), the level is not even measured in the vast majority of patients in current practice, even after ULT prescription [3]. Moreover, many patients are often prescribed ULT at a single insufficient fixed dose [3]. Finally, few patients receive a clear explanation about their gout and treatment expectations (e.g., the ‘curable’ nature of the disease) or appropriate lifestyle advice to reduce risk factors [3]. As a consequence, only a minority become free of gout, with the majority continuing to experience acute attacks, thereby contributing to an increased inpatient burden as observed in our study.
Our study also provides contemporary data on the cost burden associated with hospitalizations for gout and RA. Reflecting the increase in annual hospitalization rates, the annual costs related to primary gout hospitalizations more than doubled over the study period. Similarly, a US-based study reported increasing charges of $38 million from 2006 to 2008 for emergency visits with gout as the principal diagnosis [15]. In contrast, we found that hospital costs related to primary RA admissions declined by 40% over the study period. These findings are consistent with a recent analysis of eight German clinics or practices that showed a 13% to 22% decrease in hospitalization costs per capita, which partially offset the increasing costs of biologic use in the same study population [9]. Indeed, a US-based study from the pre-biologic era found that more than half of the total medical costs of RA were for hospitalizations [1], while a more recent US study found that prescription costs were the primary cost driver of RA (i.e., 66% of costs), while hospitalizations accounted for only 17% of costs [16].
The strengths of our study deserve comment. First, we used a large population-based dataset spanning the entire province of BC, thereby ensuring capture of all residents covered by BC's universal healthcare program who were hospitalized for RA or gout during the study period. Further, our study simultaneously addressed the two most common inflammatory arthritic conditions using one dataset, which allowed for an internal control group for each condition to help protect against the potential limitations discussed further below. For example, because PopData is an administrative database, certain levels of misclassification of diagnostic codes are inevitable. However, to improve the validity of our case definition and thus minimize misclassification bias, we limited our case definitions to principal diagnoses. Thus, our study did not examine hospitalizations with other principal diagnoses, such as comorbidities of gout or RA, as the validity of gout or RA as a secondary diagnosis would be weaker. Next, as recurrent admissions still reflect the consumption of resources and contribute to the economic burden of each disease, we did not discriminate between unique and repeat admissions. Nevertheless, when we investigated the rate of recurrent admissions and found that 95% and 96% of RA and gout admissions were unique, respectively, in 2011. Finally, changes in hospital billing practices over time may account for changes in hospitalization trends; however, the observed contrasting trends of these two arthritic conditions would not be explained by such unlikely secular changes in coding arthritic conditions.
In conclusion, our findings based on these population-based data indicate that hospitalization rates and the inpatient economic burden of gout have increased substantially over the past decade, while those for RA have decreased considerably. Thus, while these findings provide an encouraging benchmark for the improvement in RA care over the past decade, they also highlight the critical need to improve gout management and prevention to mitigate its rising disease burden in Canada and beyond.
SIGNIFICANCE AND INNOVATION.
From 2000 to 2011, hospitalizations for RA declined by 49%, while those for gout doubled.
The RA inpatient economic burden decreased by 40%, while gout costs have more than doubled.
Worsening gout hospitalization and cost trends highlight the need to improve gout management and prevention.
Acknowledgments
Funding and Support: This study was funded by a Team Grant from the Canadian Institutes of Health Research (Grant ref. #: 135235). This study was also supported in part from a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01AR065944). Dr. Lacaille holds the Mary Pack Chair in Arthritis Research funded by The Arthritis Society and the University of British Columbia.
Role of the Funding Source: The funding sources had no role in the design, conduct, or reporting of the study or the decision to submit the manuscript for publication.
Footnotes
Competing Interest Statement: HKC has served on advisory boards for Takeda Pharmaceuticals and Astra-Zeneca Pharmaceuticals.
AUTHOR CONTRIBUTIONS
Study conception and design: Rai, Choi
Acquisition, analysis, and/or interpretation of data: All authors
Drafting or critical revision of manuscript: All authors
Final approval: All authors
DATA ACCESS, RESPONSIBILITY, AND ANALYSIS
SKR and HKC had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. The BC Ministry of Health approved access to and use of the data facilitated by PopulationData BC for this study.
REFERENCES
- 1.Yelin E, Wanke L. An assessment of the annual and long-term direct costs of rheumatoid arthritis: The impact of poor function and functional decline. Arthritis Rheum. 1999;42:1209–1218. doi: 10.1002/1529-0131(199906)42:6<1209::AID-ANR18>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 2.Singh JA, Furst DE, Bharat A, et al. 2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken) 2012;64:625–39. doi: 10.1002/acr.21641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edwards NL. Quality of care in patients with gout: why is management suboptimal and what can be done about it? Curr Rheumatol Rep. 2011;13:154–9. doi: 10.1007/s11926-010-0154-6. [DOI] [PubMed] [Google Scholar]
- 4.Kuo C-F, Grainge MJ, Zhang W, Doherty M. Global epidemiology of gout: prevalence, incidence and risk factors. Nat Rev Rheumatol. 2015;11:649–662. doi: 10.1038/nrrheum.2015.91. [DOI] [PubMed] [Google Scholar]
- 5.Widdifield J, Paterson JM, Bernatsky S, et al. The epidemiology of rheumatoid arthritis in Ontario, Canada. Arthritis Rheumatol. 2014;66:786–93. doi: 10.1002/art.38306. [DOI] [PubMed] [Google Scholar]
- 6.Harty L, O'Toole G, FitzGerald O. Profound reduction in hospital admissions and musculoskeletal surgical procedures for rheumatoid arthritis with concurrent changes in clinical practice (1995-2010). Rheumatology (Oxford) 2015;54:666–71. doi: 10.1093/rheumatology/keu340. [DOI] [PubMed] [Google Scholar]
- 7.Ward MM. Decreases in rates of hospitalizations for manifestations of severe rheumatoid arthritis, 1983-2001. Arthritis Rheum. 2004;50:1122–31. doi: 10.1002/art.20158. [DOI] [PubMed] [Google Scholar]
- 8.Louie GH, Ward MM. Changes in the rates of joint surgery among patients with rheumatoid arthritis in California, 1983-2007. Ann Rheum Dis. 2010;69:868–71. doi: 10.1136/ard.2009.112474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huscher D, Mittendorf T, von Hinuber U, et al. Evolution of cost structures in rheumatoid arthritis over the past decade. Ann Rheum Dis. 2015;74:738–45. doi: 10.1136/annrheumdis-2013-204311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Canadian Institute for Health Information . Hip and Knee Replacements in Canada 2007, Annual Report. Canadian Institute for Health Information; Ottawa: 2008. [Google Scholar]
- 11.Robinson PC, Merriman TR, Herbison P, Highton J. Hospital admissions associated with gout and their comorbidities in New Zealand and England 1999-2009. Rheumatology (Oxford) 2013;52:118–26. doi: 10.1093/rheumatology/kes253. [DOI] [PubMed] [Google Scholar]
- 12.Rai SK, Aviña-Zubieta JA, McCormick N, et al. Rising Incidence and Prevalence of Gout in the Canadian General Population [abstract]. Arthritis Rheumatol. 2015:67. [Google Scholar]
- 13.Sharma TS, Harrington TM, Olenginski TP. American College of Rheumatology Annual Meeting. Boston: 2014. Aim for Better Gout Control: A Retrospective Analysis of Preventable Hospital Admissions for Gout. [Google Scholar]
- 14.Kuo CF, Grainge MJ, Mallen C, Zhang W, Doherty M. Eligibility for and prescription of urate-lowering treatment in patients with incident gout in England. JAMA. 2014;312:2684–6. doi: 10.1001/jama.2014.14484. [DOI] [PubMed] [Google Scholar]
- 15.Garg R, Sayles HR, Yu F, et al. Gout-related health care utilization in US emergency departments, 2006 through 2008. Arthritis Care Res (Hoboken) 2013;65:571–7. doi: 10.1002/acr.21837. [DOI] [PubMed] [Google Scholar]
- 16.Michaud K, Messer J, Choi HK, Wolfe F. Direct medical costs and their predictors in patients with rheumatoid arthritis: a three-year study of 7,527 patients. Arthritis Rheum. 2003;48:2750–62. doi: 10.1002/art.11439. [DOI] [PubMed] [Google Scholar]


