Abstract
Aims:
To assess the effect of zoledronic acid (ZOL) on fracture healing in osteoporotic patients with intertrochanteric fracture based on radiological evaluation and to study the correlations between severity of osteoporosis, age, gender, and time taken to fracture union.
Settings and Design:
An open label study was conducted on 43 patients at a tertiary care center.
Subjects and Methods:
The osteoporosis status of all the included patients was documented using a double-energy X-ray absorptiometry scan. A single dose of injection ZOL 5 mg was administered intravenously to all the patients after fixation during their hospital stay. Follow-up of the patients was done at 1, 3, and 6 months after surgery until union was seen radiologically.
Statistical Analysis Used:
Data were entered into Microsoft Office Excel version 2007, and interpretation and analysis of obtained data were done using summary statistics. Pearson correlation between age, gender, bone mineral density (BMD), and time taken to fracture union was done using the IBM SPSS Version 22.0 (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.).
Results:
The average age of the patients included in the study was 71.27 ± 11.48 and the average BMD was -4.58±1.42. All the fractures united by the 6th month of follow-up, which was similar to the union rate in comparison with the literature. The correlations between the gender, BMD, age, and time to union were calculated, and all the r values obtained showed very low correlation and the P values in all the variables were not significant.
Conclusion:
The bisphosphonate therapy did not adversely affect radiologically determined fracture union, and no correlations between severity of osteoporosis, age, gender, and time taken to fracture union were found to be significant.
Key words: Bisphosphonates, fracture healing, osteoporosis
INTRODUCTION
Osteoporosis is a metabolic bone disease caused by progressive bone loss. It is characterized by low bone mineral density (BMD) and structural deterioration of bone tissue leading to bone fragility and increased the risk of fractures.[1] The symptoms of osteoporosis, generally speaking, are from the fractures they cause. These can be microfractures, or they can be fragility fractures occurring from trivial trauma.[2]
Diagnosis of osteoporosis can be suspected on the basis of a plain X-ray evaluation, but the objective and internationally accepted method of diagnosing are a measurement of BMD by Double energy X-ray absorptiometry (DEXA).[3] Bisphosphonates have a major role in the management of osteoporosis as they reduce the overall risk of fracture among patients with osteoporosis, with a long-lasting beneficial effect.[4] Bisphosphonate pharmacology also makes possible monthly, intermittent, quarterly, or yearly dosing. Intravenous administration regimens (quarterly or yearly) are newer options available to patients.[5]
Intravenous bisphosphonate regimens provide alternative options for osteoporosis patients and extend the benefits of bisphosphonates to patients unable to take them orally. Zoledronic acid (ZOL) is an injectable aminobisphosphonate with potent antiresorptive activity and high affinity for mineralizing bone. It is administered as a 5 mg intravenous infusion through vented intravenous tubing over no <15 min.[4]
Since osteoclasts are essential to the normal remodeling activities in bone and are involved in bone growth, development, and repair, it is important to recognize situations in which the use of a bisphosphonate may inhibit or impair a normal physiological process. One of the most commonly asked questions is whether bisphosphonates affect fracture healing? As it is well known that bone formation and resorption are coupled through molecular and metabolic pathways[6] and as it is also known that the ability of newly formed fracture callus to be remodeled into mechanically competent lamellar bone is osteoclast-mediated,[7] several investigators have examined the role of bisphosphonates during fracture healing. An early study on the effects of ethane-1-hydroxy-1, 1-diphosphonate, a so-called first-generation bisphosphonate that inhibits mineralization at high doses, showed dose-dependent and reversible inhibition of fracture healing in mature beagle dogs.[8] An investigation in which mature beagle dogs were treated with therapeutic doses of alendronate 9 weeks preceding a radial osteotomy, 16 weeks after the osteotomy, or continuously from 9 weeks to 16 weeks after the osteotomy showed no adverse effects on fracture union, strength, or callus mineralization. However, dogs treated with alendronate during the healing period were found to have a delay in callus remodeling compared with the remodeling seen in dogs treated with a placebo.[9] More recent investigations in which incadronate was used showed similar findings, with high, continuously administered doses delaying the process of fracture healing but not impairing the ultimate recovery of mechanical integrity of the callus.[10]
These studies indicate that the effect of bisphosphonates in fracture healing is not yet fully defined. Since ZOL is a recent addition and it's very convenient once a year dosing provides a long-lasting effect, therefore this study has been undertaken to evaluate its effect on fracture healing in cancellous bone region in intertrochanteric (IT) fractures of the hip.
SUBJECTS AND METHODS
The study was conducted in the Department of Orthopaedics at a tertiary care centre from October 2013 to May 2015 after taking clearance from the Ethical Committee. Patients above 45 years of age presenting in Orthopaedic Outpatient Department and Emergency, having IT fracture of femur with underlying osteoporosis, after obtaining written informed consent, were included in the study. Men and women above 45 years of age, BMD documented osteoporosis (T-score ≤-2.5 at femoral neck or at anterior-posterior [AP] spine) and patients presenting within 3 weeks of an IT fracture were included in the study. Patients with nonosteoporotic pathological fractures, patients with head injury, creatinine clearance <35 ml/min, patients already using bisphosphonates for the treatment of osteoporosis or with chronic use of glucocorticoids, and patients with conditions associated with low bone density (e.g., diabetes mellitus, rheumatoid arthritis, cystic fibrosis, Parkinson's disease, etc.) were excluded from the study.
Total seventy patients above 45 years of age and presenting with an IT fracture were initially enrolled in the study. Forty-four patients ultimately met the inclusion criteria. Of these, one patient expired within 1 month of fracture fixation. Final study included 43 patients. Initially, radiographic diagnosis of an IT fracture was made on plain X-rays films in AP and lateral views of the affected hip with thigh. Diagnosis of osteoporosis was made on the WHO criteria through BMD by means of a DEXA scan using the lunar prodigy advance DXA system manufactured by GE Healthcare, UK. Intravenous ZOL 5 mg was administered to all the patients within 1 week of the fracture fixation. Patients were continued on osteoporosis treatment with calcium and Vitamin D supplements during and after hospital stay. Follow-up of the patients was done at 1, 3, and 6 months until union was seen radiologically. The progress of union was evaluated based on the presence of bridging callus and cortical continuity in AP and lateral radiographs of the fracture site. Union was defined when all three parameters were present in the radiographs.
RESULTS
The mean age of the study participants was 71.27 ± 11.48 years. The minimum age was 46 years and the maximum age was 90 years. The minimum number of patients, 4 (9.30%) were between 45 and 55 years of age, and the maximum number of patients, 16 (37.20%) were between 66 and 75 years.
Of the 43 patients evaluated, 19 (44.18%) were males and 24 (55.81%) were females. Twenty-four (55.81%) patients had a fracture of the right side and 19 (44.18%) of the left side. Fractures were classified as per (Arbeitsgemeinschaft für Osteosynthesefragen) (AO) classification, 15 (34.88%) patients fell into 31-A1 type of fracture, 20 (46.51%) into AO 31-A2, and 8 (18.61%) into AO 31-A3. A maximum number of patients had an AO 31-A2 type of fracture. The T-score, i.e. the number of standard deviations above or below the mean for a healthy 30-year-old adult of the same sex and ethnicity as the patient was calculated by means of a DEXA scan. The average BMD of the patients included in the study was -4.58±1.42.
Figure 1 shows a graph of bone mineral densitometry in different age groups in males and females.
Figure 1.
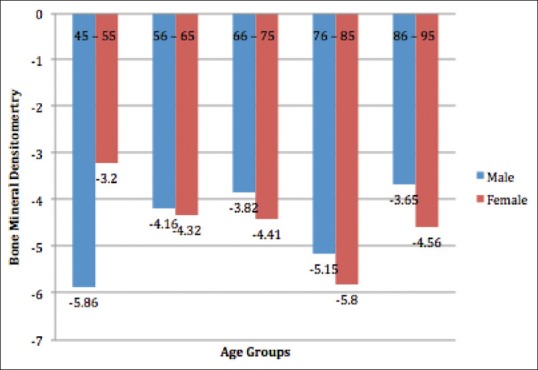
Bone mineral densitometry in different age groups in males and females
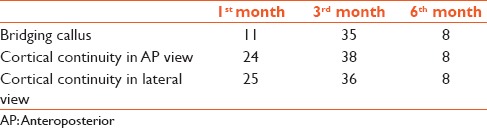
Follow-up of the patients was done at 1, 3, and 6 months after surgery by which time union was seen radiologically in all cases. Only eight patients were followed up till 6th month, most of the patients had radiological fracture healing by the 3rd month [Table 1].
Table 1.
Union as per radiological parameters
By 1st month, two patients showed the radiological union of which one was AO 31-A1 type and another one was AO 31-A2. By 3rd month, 33 patients showed the radiological union of which 11 were 31-A1 fracture type, 15 had AO 31-A2 type of fracture, and 7 had an AO 31-A3 type of fracture. Eight patients were followed up till 6th month of which three were AO 31-A1 type, four were AO 31-A2, and only one was AO 31-A3 type. Three patients with an AO 31-A1 fracture had to be followed up till 6th month for radiological signs of union, four patients with an AO 31-A2 type healed by the 6th month, and one patient with an AO 31-A3 united by 6th month. Two patients one from each AO 31-A1 and AO 31-A2 showed all the defined signs of radiological union at the first follow-up, i.e., at the 1st month [Table 2].
Table 2.
Union in different fracture types at follow-up
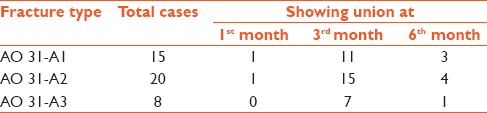
Figure 2 shows the preoperative, postoperative, and 3rd -month follow-up X-rays (AP and lateral views) of a patient with an IT fracture.
Figure 2.

Preoperative, postoperative, and at 3rd-month follow-up X-rays (anterior-posterior and lateral views) of a patient
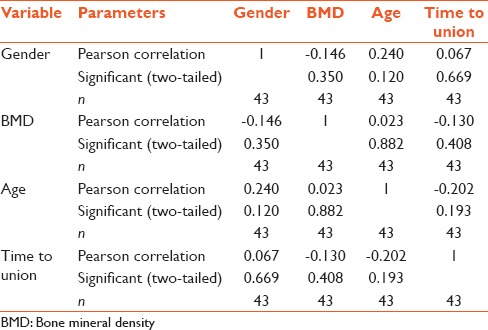
The correlations between the gender, bone mineral densitometry, age, and time to union were calculated using the Pearson correlation. The r value between gender and BMD was -0.146, between gender and age was 0.240, and between gender and time to union was 0.067. The r value between BMD and gender was -0.146, between BMD and age was 0.023, and between BMD and time to union was -0.130. The r value between age and gender was 0.240, between age and BMD was 0.023, and between age and time to union was -0.202. The r value between time to union and gender was 0.067, between time to union and BMD was -0.130, and between time to union and age was -0.202. The r value obtained between all the variables was lower than 0.3, so it showed low correlation. The P value between gender and BMD was 0.350, between gender and age was 0.120, and between gender and time to union was 0.669. The P value between BMD and gender was 0.350, between BMD and age was 0.882, and between BMD and time to union was 0.408. The P value between age and gender was 0.120, between age and BMD was 0.882, and between age and time to union was 0.193. The P value between time to union and gender was 0.669, between time to union and BMD was -0.408, and between time to union and age was 0.193. The P values in all the variables were not significant [Table 3].
Table 3.
Correlations between the gender, bone mineral density, age, and time to fracture union
DISCUSSION
Fracture healing has always been a major medical concern, and it has been the aim of physicians and basic scientists alike to find ways to shorten the healing time and to prevent nonunion.[11] Fleisch pointed out that in the majority of animal studies, callus size either was not influenced or was increased by bisphosphonates, and it never decreased due to the slowing of callus resorption.[12] Since hip fractures are commonly seen in the same age group as primary osteoporosis, so patients with hip fracture represent an important population to target for the prevention of secondary fractures.[13]
Amanat et al. demonstrated that a single dose of ZOL significantly increased callus volume and mechanical strength.[14] Poor adherence to oral bisphosphonate therapy has been shown to compromise the efficacy of this treatment for fracture reduction and to increase medical costs.[15] Gong et al. concluded that early initiation of bisphosphonate treatment for patients with an osteoporotic distal radial fracture treated with volar locking plate fixation did not affect fracture healing or radiographic or clinical outcomes.[16] The most common criterion for radiological union was bridging of the fracture site.[17]
The mean age of the patients included in the study was 71.27 years which was similar to Kim et al.'s study; they had three groups with a mean age of 75 years in Group A, 75.3 in Group B, and 78.1 in Group C. They included all the patients with a T-score of <-2.5. The mean BMD in Group A of their study was -3.2, in Group B -2.8, and -3.3 in Group C. In our study, the average T-score at femoral neck of the nonfractured side was -4.58 ± 1.42 which showed that osteoporosis was markedly more in our patients.[18]
Radiological healing was defined as bridging at the fracture site by a callus or a cortical continuity involving at least two cortices in the hip using AP and lateral views of the femur.[8] At 1st month follow-up, 11 patients in our study had bridging callus, 24 patients had cortical continuity in AP view, and 25 had cortical continuity in lateral view. At 3rd month most of the patients had radiologically defined union, out of 43 patients, 35 showed bridging callus, 38 showed cortical continuity in AP view, and 36 showed cortical continuity in lateral view. Only eight patients needed to be followed up till 6th month by which time all eight patients had all the radiological parameters to conclude definitive union.
Kim et al.'s study showed that all fractures united by 20 weeks in their Group A and by 24 weeks in their Group B and C.[18] In our study, at 1st month follow-up, 4.6% had evidence of radiological healing, 76.7% showed signs of healing at 3rd month, and 18.7% united by the 6th month of follow-up. Hence, by the 12th week, i.e., 3rd month, the majority of our patients had radiologically defined union, and at 24 weeks, all the patients included in our study had union.
Bridle et al. did a study on 100 patients with IT fractures at a time when bisphosphonates were not available, 49 of their patients were treated with intermedullary device and 51 with extramedullary device, i.e. dynamic hip screw. They concluded that all the internally fixed IT fractures heal by 6 months in the absence of any complications irrespective of the fixation device used.[11] Our results were comparable to Bridle et al.'s study as all the patients included in our study had radiologically defined union at the 6th -month follow-up irrespective of the type of implant used for fracture fixation, and administration of ZOL did not seem to give any different results in our study.
In addition to the above-mentioned studies, we studied the correlation between age, gender, BMD (severity of osteoporosis), and time taken to union. All the patients were given intravenous ZOL. However, no evidence of correlation was found statistically in these variables. Various studies have stated that the severity of osteoporosis increases with age, but in our study, the most osteoporotic patient was a male of 48 years with a BMD of -8.2. No evidence could be established between age and BMD values in our study as the r value had low correlation. Female preponderance was found probably due to postmenopausal osteoporosis but no statistical correlation could be established between gender of the patient and BMD values as the r values again showed low correlation. Although all the fractures united by the 6th month, statistically no correlation could be established between the time taken to union and age, gender or BMD of the patients as the r value had low correlation, and P values of all the variables were not significant.
CONCLUSION
Hence, we would like to conclude that the bisphosphonate therapy with ZOL after hip fracture surgery, in elderly osteoporotic patients, did not adversely affect radiologically determined fracture union. Although no significant correlation was seen in time taken to fracture union, age, gender, or severity of osteoporosis, due to the very small sample size of this study, these correlation results need to be further confirmed through a larger sample size study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17:1726–33. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 2.Shatrugna V, Kulkarni B, Kumar PA, Rani KU, Balakrishna N. Bone status of Indian women from a low-income group and its relationship to the nutritional status. Osteoporos Int. 2005;16:1827–35. doi: 10.1007/s00198-005-1933-1. [DOI] [PubMed] [Google Scholar]
- 3.Salamat MR, Rostampour N, Zofaghari J, Hoseyni-Panah H, Javdan M. Comparison of Singh index accuracy and dual energy X-ray absorptiometry bone mineral density measurement for evaluating osteoporosis. Iran J Radiat Res. 2010;8:123–8. [Google Scholar]
- 4.Lewiecki EM. Intravenous zoledronic acid for the treatment of osteoporosis: The evidence of its therapeutic effect. Core Evid. 2010;4:13–23. doi: 10.2147/ce.s6011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rogers MJ, Gordon S, Benford HL, Coxon FP, Luckman SP, Monkkonen J, et al. Cellular and molecular mechanisms of action of bisphosphonates. Cancer. 2000;88(12 Suppl):2961–78. doi: 10.1002/1097-0142(20000615)88:12+<2961::aid-cncr12>3.3.co;2-c. [DOI] [PubMed] [Google Scholar]
- 6.Favus MJ, editor. Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism. 5th ed. Washington, DC: American Society for Bone and Mineral Research; 2003. [Google Scholar]
- 7.Einhorn TA. The cell and molecular biology of fracture healing. Clin Orthop Relat Res. 1998;355(Suppl):S7–21. doi: 10.1097/00003086-199810001-00003. [DOI] [PubMed] [Google Scholar]
- 8.Lenehan TM, Balligand M, Nunamaker DM, Wood FE., Jr Effect of EHDP on fracture healing in dogs. J Orthop Res. 1985;3:499–507. doi: 10.1002/jor.1100030413. [DOI] [PubMed] [Google Scholar]
- 9.Peter CP, Cook WO, Nunamaker DM, Provost MT, Seedor JG, Rodan GA. Effect of alendronate on fracture healing and bone remodeling in dogs. J Orthop Res. 1996;14:74–9. doi: 10.1002/jor.1100140113. [DOI] [PubMed] [Google Scholar]
- 10.Li C, Mori S, Li J, Kaji Y, Akiyama T, Kawanishi J, et al. Long-term effect of incadronate disodium (YM-175) on fracture healing of femoral shaft in growing rats. J Bone Miner Res. 2001;16:429–36. doi: 10.1359/jbmr.2001.16.3.429. [DOI] [PubMed] [Google Scholar]
- 11.Bridle SH, Patel AD, Bircher M, Calvert PT. Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg Br. 1991;73:330–4. doi: 10.1302/0301-620X.73B2.2005167. [DOI] [PubMed] [Google Scholar]
- 12.Fleisch H. Can bisphosphonates be given to patients with fractures? J Bone Miner Res. 2001;16:437–40. doi: 10.1359/jbmr.2001.16.3.437. [DOI] [PubMed] [Google Scholar]
- 13.Lyles KW, Colón-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799–809. doi: 10.1056/NEJMoa074941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amanat N, McDonald M, Godfrey C, Bilston L, Little D. Optimal timing of a single dose of zoledronic acid to increase strength in rat fracture repair. J Bone Miner Res. 2007;22:867–76. doi: 10.1359/jbmr.070318. [DOI] [PubMed] [Google Scholar]
- 15.Huybrechts KF, Ishak KJ, Caro JJ. Assessment of compliance with osteoporosis treatment and its consequences in a managed care population. Bone. 2006;38:922–8. doi: 10.1016/j.bone.2005.10.022. [DOI] [PubMed] [Google Scholar]
- 16.Gong HS, Song CH, Lee YH, Rhee SH, Lee HJ, Baek GH. Early initiation of bisphosphonate does not affect healing and outcomes of volar plate fixation of osteoporotic distal radial fractures. J Bone Joint Surg Am. 2012;94:1729–36. doi: 10.2106/JBJS.K.01434. [DOI] [PubMed] [Google Scholar]
- 17.Corrales LA, Morshed S, Bhandari M, Miclau T., 3rd Variability in the assessment of fracture-healing in orthopaedic trauma studies. J Bone Joint Surg Am. 2008;90:1862–8. doi: 10.2106/JBJS.G.01580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim TY, Ha YC, Kang BJ, Lee YK, Koo KH. Does early administration of bisphosphonate affect fracture healing in patients with intertrochanteric fractures? J Bone Joint Surg Br. 2012;94:956–60. doi: 10.1302/0301-620X.94B7.29079. [DOI] [PubMed] [Google Scholar]


