Abstract
Aim:
The present randomized study was aimed to compare the efficacy 5% potassium nitrate (KNO3) toothpaste, low-level laser therapy (LLLT), and LLLT with 5% KNO3 toothpaste in the treatment of dentinal hypersensitivity (DH).
Materials and Methods:
Total of 45 patients complaining of DH with visual analog scale (VAS) score being ≥2 were recruited and were divided into three groups. Group A was treated with 5% KNO3 toothpaste, Group B using LLLT along with the application of 5% KNO3 toothpaste, and Group C using LLLT alone. VAS scores were recorded at the baseline, 1st, 2nd, and 3rd weeks by the examiner who is blinded toward the treatment. The sensitivity response was evaluated using air spray and tactile sensation (explorer).
Results:
A greater reduction of DH was recorded at the end of 3 weeks in Group C and Group B when compared to Group A. Better results were noted in Group C at the end of the 1st week when compared to Group B. According to this study, there was no additional benefit of using toothpaste along with LLLT.
Conclusion:
A greater reduction of DH was recorded at the end of 3 weeks in Group C and Group B when compared to Group A. Better results were noted in Group C at the end of the 1st week when compared to Group B. According to this study, there was no additional benefit of using toothpaste along with LLLT.
Key words: Dentinal hypersensitivity, diode Laser, low-level laser therapy
INTRODUCTION
Dentinal hypersensitivity (DH) is a common problem which is attributed in daily dental practice observed mostly from the second to sixth decade of life. DH can arise through the improper bushing, receding gums, inappropriate diet, and because of various other factors.[1] Varying hypothesis has been put forward for explaining the cause of DH but most accepted being Brannstrom's hydrodynamics theory of DH in 1962, according to which sensitivity results when stimulus is applied to dentine displaces the fluid inside the tubule inwardly and outwardly,[2] leading to deformation of nerve endings at the pulp/dentine interface, which is transmitted as a painful sensation.[3] Any treatment modality which can block or reduce the movement of fluid,[4] blocks the pain transmission, or occludes the dentinal tubule and precipitates the proteins can prove beneficial in the treatment of DH.
Various methods such as traditional therapeutic toothpaste containing fluorides and nitrates, desensitizing topical agents (fluoride salts, potassium nitrate [KNO3 ], oxalate, calcium phosphate, and arginine), iontophoresis, adhesives, resins, and lasers have been tried to block the DH with varying success rates.[5]
KNO3 was introduced for treating DH by Hodosh in 1974[6] and accepted by the American Dental Association (1986), the mechanism is still unexplained but it seems to be of a neural type.[7] Potassium ion tends to accumulate in dentinal tubules leading to depolarization of cellular membrane of terminal nerve endings leading to the refractory period with decreased sensitivity.[8]
Laser technology has been studied widely for treating DH since the mid-1980s though results were divergent.[5] Different lasers He-Ne, neodymium or erbium doped yttrium-aluminum garnet, CO2, and diodes (GaAlAs) have been tested for treating DH though the results mostly depended on the action of lasers on dentinal tubules.
Low-level laser therapy (LLLT) has been explored widely in treating DH. Its action is due to its analgesic, biostimulatory, and anti-inflammatory properties also regulates the cellular metabolism which makes it effective.[9] LLLT has also been further used in treating aphthous, endodontic intervention, and after surgeries.
In this study, LLLT, KNO3 5% toothpaste, and combination of 5% KNO3 along with LLLT have been used in treating DH.
MATERIALS AND METHODS
The study is three armed parallel, single-blinded, and randomized trial. The total of 45 patients (23 males and 22 females) with a mean age of 35 years from the outpatient department were selected using randomized selection. Patients who matched the study criteria and complained of sensitivity were allocated to three different groups (15 patients in each group). Allocation of patients into each group was done using computerized generated randomization, 15 each. The study was approved by the Institutional Ethical Committee review board 557/sscds/IRB-E/OS/2015.
Subjects with minimum one tooth having DH due to gingival recession with visual analog scale (VAS) score of ≥2, no previous history of flap surgery for minimum 6 months, no usage of analgesic, anticonvulsants, sedatives, tranquilizers, and anti-inflammatory drugs within 72 h, desensitizing toothpaste, or mouthwash for at least 3 months were included in the study. Pregnant or lactating mothers, smokers, systemically unhealthy, subjects whose teeth had evidence of carious, wear facets, cracked teeth, and mobile teeth were excluded from the study.
Group A was given paste containing 5% KNO3 (Sensodyne K®) to be used twice daily. Group B was treated using paste which was applied for 1 min on hypersensitive area, LLLT was given using diode laser (Picassa 810 nm) at 0.5 watts and tip of diameter 300 μ in non contact mode starting at a distance of 5–6 mm away from the hypersensitive tooth area and slowly approaching within a distance of 2–3mm in a scanning motion covering the entire hypersensitive tooth area for a period of 30 seconds to 1 minute [Figure 1]. Group C was treated using LLLT in the same way as mentioned above without any paste application. Group B and C subjects were given DH treatment at the end of the 1st and 2nd week as well and were instructed to continue the same toothpaste which they were using before treatment.
Figure 1.

Laser application in cervical abrasion in relation to 14
DH for all study groups was recorded at different time intervals 1st, 2nd, and 3rd week using VAS scores ranging between 0 and 10. Hypersensitivity perceived by subjects was recorded when subjected to air spray and tactile sensation using explorer. The power of the study was calculated by statistician and was set at 80%.
Statistical analyses
The statistical analysis was done using Statistical Packages for Social Science version 20 (SPSS Inc., Chicago, IL, USA). The comparison of VAS scores between three groups at different time intervals was done using post hoc ANOVA, to know the effect of each variable and reveal statistical significance. The confidence level of the study was proposed to be 99% with P < 0.001, which is highly significant.
RESULTS
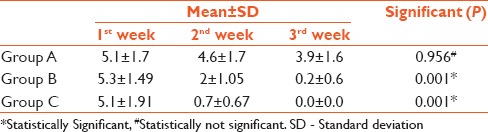
All test teeth presented DH before the desensitizing treatment, i.e., at the baseline, levels of hypersensitivity were statistically not significant among all three groups [Table 1]. At the end of the 1st week, Groups B and C showed a significant reduction in DH when compared to Group A [Table 1]. However, Group C showed a better reduction in DH at the end of the 1st week when compared with Group B [Table 1 and Figure 2]. However, at the end of the 3rd week, both Groups B and C were equally effective in reducing DH and results showed no statistically significant difference between them [Table 2]. On intra-group comparison, Group A did not show a significant reduction from the baseline to different time intervals, Groups B and C showed a significant reduction in DH at the end of the 1st week and at the subsequent time periods of the study [Table 2].
Table 1.
Comparison of dentinal hypersensitivity between the groups
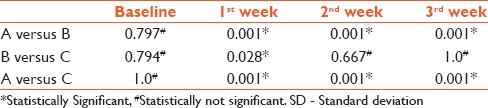
Figure 2.
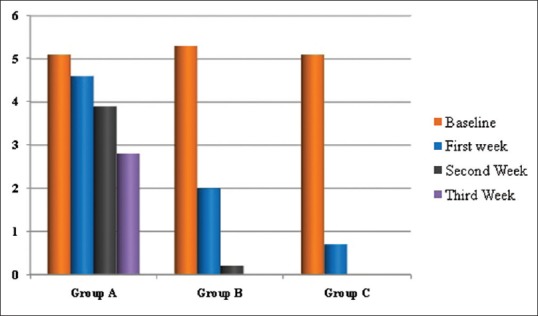
Comparison of dentinal hypersensitivity between the groups
Table 2.
Visual analog scale value assessment between the groups at different intervals
DISCUSSION
The DH has been the most explored topic in dentistry and always been an enigma. In the present study, LLLT, LLLT along with KNO3, has given better results when compared to the use of KNO3 toothpaste alone.
The reduction in DH can be attributed to the property of LLLT that it acts on biostimulation because of the increased production of mitochondrial ATP, increasing the threshold of the free nerve endings, providing an analgesic effect due to a surge in b-endorphin in the cephalorachidian liquid.[9] The decrease of pain occurs due to inhibition of cyclooxygenase enzyme, which tests the transformation of the arachidonic acid to prostaglandins. The laser also increases the formation of the secondary dentin by odontoblasts in the process of biostimulation.
No contrary effects were reported using LLLT in the treatment of DH. In addition to the biological effect of increasing the potential of an action of the pulp tissue,[10] authors advocate that LLLT is also safer to the pulp because they stimulate circulation and cellular activity and does not cause any change to the hypermineralized structure.
In a similar study by Dilsiz et al. in 2010 in which two groups were compared, one desensitizer paste and other was LLLT along with desensitizing paste the latter showed the significant effect in desensitization of teeth with gingival recession.[11]
The use of LLLT in this study has played a beneficial role which is in accordance with Furuko et al. 1989, Basford et al. 1989, Yamaguchi et al. 1990, Groth et al. 1993, Greshman et al. 1994, and Yui et al. 2003.[9]
Contrasting results were shown in Vieira et al. study in which diode laser with placebo oxalate gel, placebo laser along with oxalate gel, and pacebo oxalate and placebo laser were compared did not show any significant differences in reduction of sensitivity after 3 months follow-up; nevertheless, these results can be subjected to the presence of placebo effect.[12]
In the present study, KNO3 did not give any beneficial results which are in accordance with Poulsen et al.[13] However, studies results of Hodosh 1974, Green et al. 1977, Tarbet et al. 1982, Blong et al. 1985, Reinhert et al. 1990, Echeverria et al. 1991, etc., have shown that KNO3 is efficacious in reducing DH.[14]
The addition of KNO3 to LLLT did not prove beneficial over LLLT group, the 1st week LLLT showed a significant reduction in DH. Fourteen subjects showed no symptoms of DH at the end of 2 weeks when compared to the combination group in which 13 patients showed resolution at the end of 3 weeks. Both the Groups B and C showed a reduction in DH at the end of the study period. There was no additional benefit of using 5% KNO3 toothpaste in the present study and was noted when compared to LLLT and combination.
CONCLUSION
There was no additional benefit of using toothpaste along with LLLT. To validate the present study results long-term studies with bigger sample size is needed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kimura Y, Wilder-Smith P, Yonaga K, Matsumoto K. Treatment of dentine hypersensitivity by lasers: A review. J Clin Periodontol. 2000;27:715–21. doi: 10.1034/j.1600-051x.2000.027010715.x. [DOI] [PubMed] [Google Scholar]
- 2.Wichgers TG, Emert RL. Dentin hypersensitivity. Gen Dent. 1996;44:225–30. [PubMed] [Google Scholar]
- 3.Corona SA, Nascimento TN, Catirse AB, Lizarelli RF, Dinelli W, Palma-Dibb RG. Clinical evaluation of low-level laser therapy and fluoride varnish for treating cervical dentinal hypersensitivity. J Oral Rehabil. 2003;30:1183–9. doi: 10.1111/j.1365-2842.2003.01185.x. [DOI] [PubMed] [Google Scholar]
- 4.Pashley DH. Mechanisms of dentin sensitivity. Dent Clin North Am. 1990;34:449–73. [PubMed] [Google Scholar]
- 5.Sgolastra F, Petrucci A, Gatto R, Monaco A. Effectiveness of laser in dentinal hypersensitivity treatment: A systematic review. J Endod. 2011;37:297–303. doi: 10.1016/j.joen.2010.11.034. [DOI] [PubMed] [Google Scholar]
- 6.Hodosh M. A superior desensitizer – Potassium nitrate. J Am Dent Assoc. 1974;88:831–2. doi: 10.14219/jada.archive.1974.0174. [DOI] [PubMed] [Google Scholar]
- 7.Pashley DH. Dentin permeability, dentin sensitivity, and treatment through tubule occlusion. J Endod. 1986;12:465–74. doi: 10.1016/S0099-2399(86)80201-1. [DOI] [PubMed] [Google Scholar]
- 8.Pashley DH, O’Meara JA, Kepler EE, Galloway SE, Thompson SM, Stewart FP. Dentin permeability. Effects of desensitizing dentifrices in vitro. J Periodontol. 1984;55:522–5. doi: 10.1902/jop.1984.55.9.522. [DOI] [PubMed] [Google Scholar]
- 9.Yui KCK, Jorge ALC, Gonçalves SEP, Rodrigues JR, Nicoló DR. Low level laser therapy for dentine hypersensitivity. Braz Oral Res. 2003;6:17–24. [Google Scholar]
- 10.Benneti AR, Franco EB, Franco EJ, Pereira JC. Laser therapy for dentin hypersensitivity: A critical Appraisal. J Oral Laser Appl. 2004;4:271–8. [Google Scholar]
- 11.Dilsiz A, Aydin T, Emrem G. Effects of the combined desensitizing dentifrice and diode laser therapy in the treatment of desensitization of teeth with gingival recession. Photomed Laser Surg. 2010;28(Suppl 2):S69–74. doi: 10.1089/pho.2009.2640. [DOI] [PubMed] [Google Scholar]
- 12.Vieira AH, Passos VF, de Assis JS, Mendonça JS, Santiago SL. Clinical evaluation of a 3% potassium oxalate gel and a GaAlAs laser for the treatment of dentinal hypersensitivity. Photomed Laser Surg. 2009;27:807–12. doi: 10.1089/pho.2008.2364. [DOI] [PubMed] [Google Scholar]
- 13.Poulsen S, Errboe M, Lescay Mevil Y, Glenny AM. Potassium containing toothpastes for dentine hypersensitivity. Cochrane Database Syst Rev. 2006;3:CD001476. doi: 10.1002/14651858.CD001476.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Frechoso SC, Menéndez M, Guisasola C, Arregui I, Tejerina JM. Sicilia A Evaluation of the efficacy of two potassium nitrate bioadhesive gels (5% and 10%) in the treatment of dentine hypersensitivity. A randomised clinical trial. J Clin Periodontol. 2003;30:315–20. doi: 10.1034/j.1600-051x.2003.20077.x. [DOI] [PubMed] [Google Scholar]


