Abstract
Introduction:
Fracture fixation has become advanced with the advent of new and custom metal implants for each type of bone/fracture. After union though, the implant ceases to be important and may be removed. Routine removal is advocated by some and opposed by others. Nevertheless, some patients require removal of the hardware because of various implant-related problems. Our study was aimed at identifying the most common causes for implant removal.
Objective:
To investigate the common indications of orthopedic implant removal surgeries.
Methods:
Adult patients admitted for implant removal in our department were included in the study. They were operated in the next OT list. They were then followed for an average 4 months for resolutions of symptoms or appearance of new problems.
Results:
A total of 83 patients were studied. 71 of them were males. The mean age was 38 years. The reasons for removal of implants were found to lie in five categories: Pain/discomfort/prominent hardware, infected hardware, implant failure, elective (patient’s insistence), and other reasons. Overall, the most frequently removed implants in our series were distal tibial/ankle plates (14.45% of implants removed), femoral intramedullary (IM) nails (13.25%), olecranon wires and plates (12.04%), and tibial IM nails and patellar tension band wirings (9.53% each).
Discussion and Conclusion:
The clinical indications of implant removal are not well established, and few definitive data exist to guide whether routine implant removal is appropriate. Symptomatic hardware frequently needs removal. We found that pain and implant prominence (mechanical symptoms) are the most common indications. Infection is the next most common, followed by hardware failure. Other indications are implant failure, bone resorption due to excessive stress shielding and patient’s will. Removal is, however, not an easy surgery, and several factors such as bone ingrowth and wear of the implant may make its removal difficult.
Keywords: Failure, fracture, hardware removal, implant, infected, symptomatic
Introduction
Substantial growth has occurred in the options for operative fracture treatment in the last few decades.1 This, in proportion to newer and better internal fixation devices or implants. Specially designed intramedullary (IM) nails, and plates and screws for every bone and even parts of bones have helped increase treatment efficacy and union rates. Titanium alloys and stainless steel are generally employed for the manufacture of orthopedic implants.1 After fracture union, the implant loses its purpose and continues to exist only as a foreign object inside the patient’s body. Then, the question of whether to remove it or leave it be arises. Removal of asymptomatic hardware is still debated, and there is a lack of clear guidelines.2 Although there are several presumed benefits of implant removal, like functional improvement and pain relief, the surgical procedure can be challenging and may lead to complications such as neurovascular injury and refractures.2 There is wide country to country and surgeon to surgeon variations in the viewpoint on removal of hardware, with some advocating and many opposing routine removal.3 Add to this the patients’ demands owing to their own perceptions and fears about the “foreign device” inside their body. In children, though, routine implant removal after fracture union is still standard procedure.4 Implants may disturb function, and some theoretical long-term risks such as growth disturbance, foreign body reaction, chronic infection, and corrosion are used as arguments for removal. However, benefits should outweigh risks and removal should not require a more extensive operation than insertion.4
The consensus dilemmas over routine implant removal in adults notwithstanding, there are circumstances when removal of hardware does become necessary. These include pain and discomfort to the patient, infection and implant failure. In our center, routine removal of asymptomatic implants is not practiced. We designed this short study to investigate the commonest indications of implant removal, and to detect which implants were most likely to require removal.
Materials and Methods
The study was conducted prospectively on patients admitted for removal of implants in the orthopedics department of a teaching hospital. Prior ethical approval from the institutional committee was sought. Adult patients aged 18 years or more who presented in the outpatient department (OPD) with hardware related problems that necessitated removal was admitted. Patients admitted over a period of 7-month starting February 2013 were included in the study. Patients who had fixation devices intended to be removed after a definite interval to begin with, like percutaneous K-wires, external fixators and tarsal screws, were not included in the study. Patients requiring removal of joint prostheses were also excluded from the study.
At the time of admission, the potential risks of the operation and the possibility of non-favorable outcomes were explained to all patients. After admission, routine inpatient investigations were performed on all patients to evaluate their fitness for surgery. Implant removal was then done in the next OT list. All patients received prophylactic antibiotics and tourniquet was used wherever possible. Postoperatively, the patients were retained in the hospital for variable periods depending on the indication of removal and the condition of the wound. Antibiotics were continued for longer duration in patients with infected hardware. At discharge, all the patients were strictly advised to protect the extremity for a variable length of time as demanded by the bone and the implant removed. They were followed in the OPD for another 4 months and evaluated for symptom relief/persistence/new problems, and the data were collected. The data were analyzed by the authors and also by statistician using SPSS software and applying t-test, and results were compiled.
Results
Eighty-seven patients fulfilled the inclusion criteria, but four did not return for follow-up. That left us with eighty-three patients on whom to conduct the study (n = 83).
Seventy-one patients were males (85.55%) and 12 were females (14.45%). Their ages ranged from 20 years to 78 years, and the mean age was 38 years. The reasons for removal of implants were found to lie in five categories: Pain/discomfort/prominent hardware, infected hardware, implant failure, elective (patient’s insistence), and other reasons (Table 1).
Table 1.
Distribution of cases
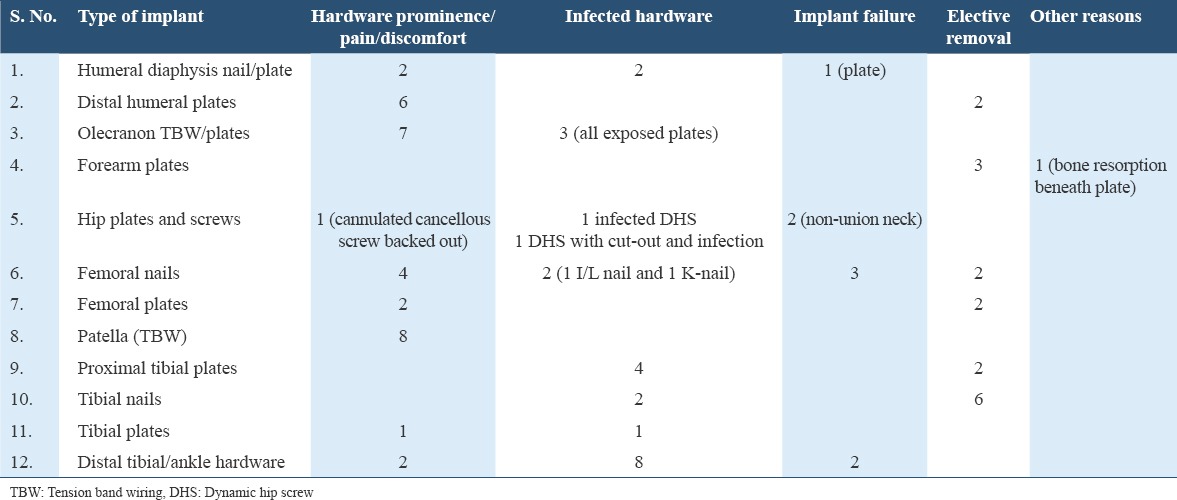
Thirty-three patients out of eighty-three had hardware pain or discomfort or prominence (39.75%). They ranged in age from 20 to 60 years (mean age 31.6 years). The time since fracture fixation ranged from 4 months to 96 months (average 38 months). The implants most commonly responsible in order of frequency were patella tension band wiring (TBW) (n = 8), olecranon TBW/plates (n = 7), distal humeral plates (n = 6), and femoral IM nails (n = 4). The mean duration of hospital stay in these patients was 5 days. At 4 months follow-up, 15 patients out of 34 reported complete relief of pain (44.11%). 19 patients had partial relief in pain or discomfort (55.89%). No patient in this group experienced an increase in pain. The average pain visual analog scale (VAS) score decreased from 5.2 preoperatively to 2.1 postoperatively, which was statistically significant (P < 0.05). No patient developed infection. One had an ulnar nerve palsy postoperatively, which recovered (Chart 1, Figure 1a and b).
Chart 1.
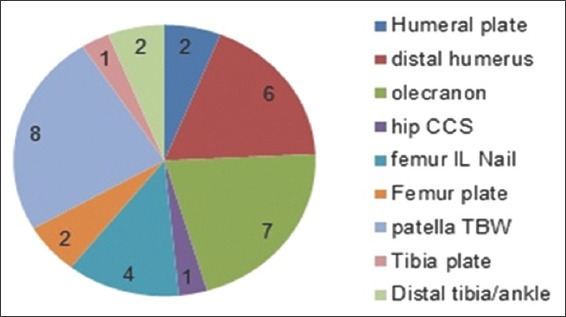
Distribution of painful prominent hardware
Figure 1.

(a) Prominent hardware in distal humerus. (b) Radiographs before and after removal of the implants
Twenty-four patients out of 83 (28.91%) needed hardware removal because they had developed infection at the implant site a variable duration after osteosynthesis. Their ages ranged from 26 years to 78 years (mean 49.33 years), and the duration since first surgery varied from 2 months to 156 months (mean 47.57 months). Union was present in 22 patients at the time of implant removal. One ununited fracture was managed with external fixator; the other was an infected olecranon which required repeat debridements followed by repeat osteosynthesis and flap coverage. In this group, the implants most commonly removed included distal tibial/ankle plates and screws (n = 8), proximal tibial plates (n = 4) and olecranon plates (n = 3). These patients were retained in the hospital for an average 7.6 days. After the removal, infection subsided in 21 patients out of 24 (87.5%). Three patients developed chronic osteomyelitis with persistent discharge. One of them had a refracture of the tibial shaft after sequestrectomy (Chart 2) (Figures 2 and 3).
Chart 2.
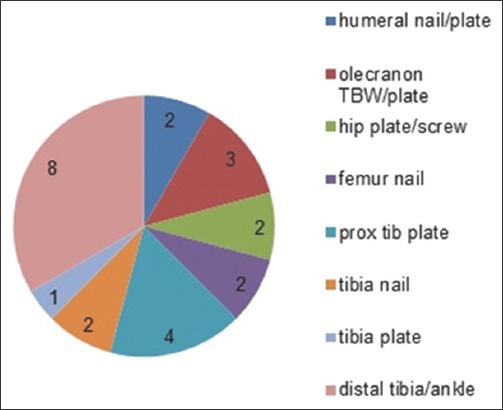
Distribution of infected hardware
Figure 2.

Exposed and infected medial plates in the distal tibia in three patients
Figure 3.

Infected and failed femoral locking nail
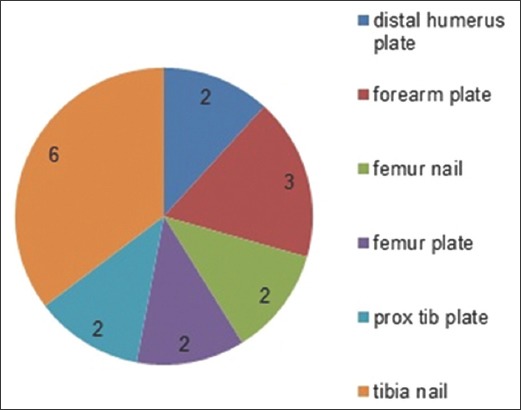
Eight (9.52%) patients required implant removal and revision osteosynthesis for implant failure. Their average age was 35 years (18-50 years), and the average time since the primary procedure was 7.6 months (2-12 months). These included 3 femoral IM nails, 2 distal tibial locked plates, 1 humeral shaft dynamic compression plate, and 2 patients with cannulated cancellous screws in the femoral neck (Chart 3, Figure 4).
Chart 3.
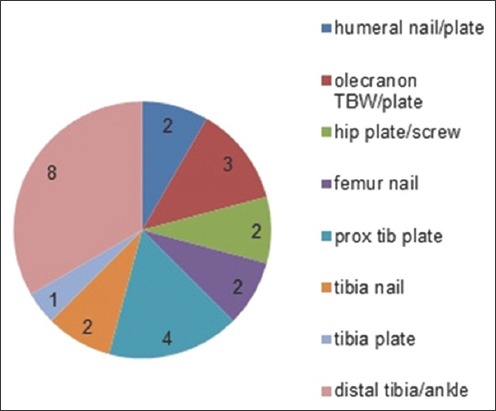
Distribution of failed hardware
Figure 4.
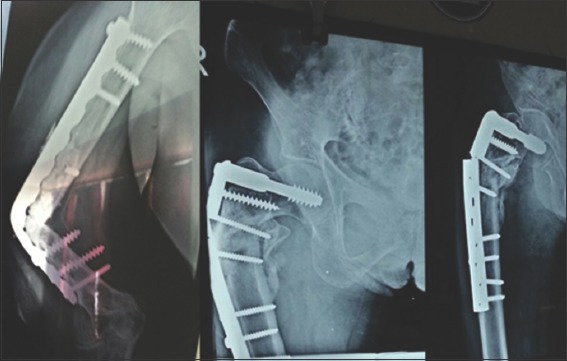
Plate failure in the humeral shaft and proximal femur
One patient during the routine course of his follow-up after plating of both forearm bones was found to have extensive bone resorption under the plates (Figure 5). These plates were removed. On follow-up, there was no fracture or other complications.
Figure 5.

Bone resorption beneath ulnar plate
Seventeen (20.48%) patients had their implants removed on demand, despite being asymptomatic. During the course of their follow-up, three of these had persistent pain at the operated site. Two developed superficial wound infections which prolonged their hospital stay but responded to intravenous antibiotics and wound lavage. None developed osteomyelitis (Chart 4).
Chart 4.
Distribution of implants removed on patient’s wish
The most consistently encountered obstacle during surgery was difficulty in removing the hardware from the bone. This was seen especially in locked plates of the distal humerus and forearm, with ingrowth of bone around the plate/screws. Loss of contour (“rounding”) of the screw head slot was also commonly encountered preventing the engagement of the driver in the screw head. Screw heads had to be cutoff to remove the plate in two patients because of this complication, and the shank left in the bone. In one patient who had presented for elective removal of an interlocked tibial nail, we failed to extract the nail despite best efforts. In another patient with a painful femoral nail, the nail broke just beneath the proximal locking bolts (Figure 6). Fortunately, we did not encounter any major vascular injury or iatrogenic fracture during the removal of any implant. One patient had an ulnar nerve neuropraxia after removal of distal humeral plates, which recovered. Another patient with infected tibial I/L nail developed chronic osteomyelitis. Sequestrectomy was done, and the patient presented with a refracture in follow-up. These last two, and persistent pain in three previously asymptomatic patients were the only true complications in our series.
Figure 6.
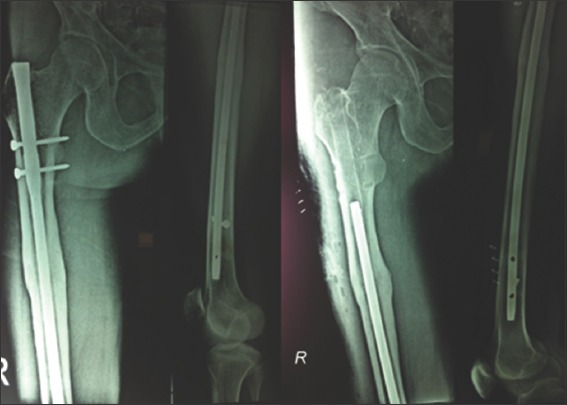
Femoral interlocking nail broken during removal
Overall, the most frequently removed implants in our series were distal tibial/ankle plates (14.45% of implants removed), femoral IM nails (13.25%), olecranon wires and plates (12.04%), and tibial IM nails and patellar TBWs (9.53% each). Pertinent to mention though that 6 of the 8 tibial nail removals were elective (asymptomatic patients) (Chart 5).
Chart 5.
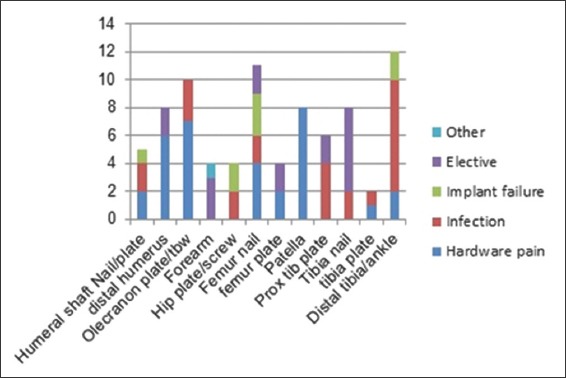
Overall distribution of removed implants
All implants except one removed in our series were made of stainless steel, and all were made by Indian manufacturers.
Discussion
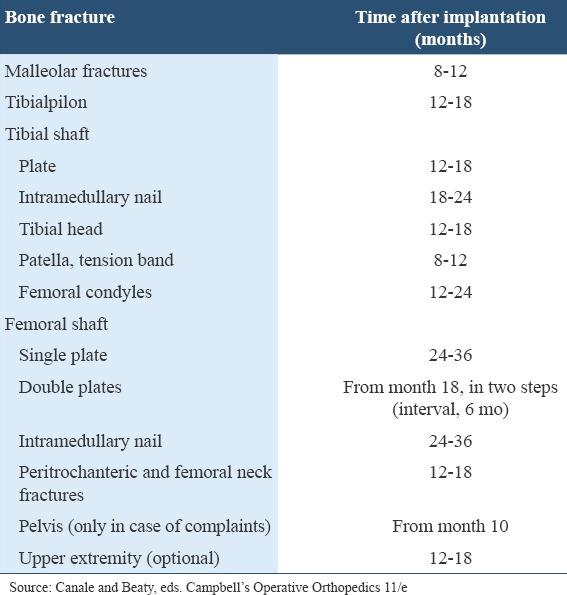
The issue of removing metallic implants used in fracture fixation has been oft discussed, and at length. Popular opinion probably still is that implant removal should not be considered a routine procedure.2,3,5 Although the AO-Association for the Study of Internal Fixation has published recommendations on the timing of hardware removal in recent fractures with uncomplicated healing (Table 2), the clinical indications for implant removal are not well established, and few definitive data exist to guide whether routine implant removal is appropriate. Furthermore, the surgical procedures for implant removal are fraught with risks of fracture, neurovascular injury, and infection. Various arguments have been made from time to time to justify removal of hardware after fracture union, e.g., metal allergy, corrosion, carcinogenesis and metal ion toxicity, but for none has concrete proof been produced.2 All the same, a lot of metal is removed from human bones every day. And that depicts that hardware does need to be removed in a significant subset of patients. Large studies on implant removal in symptomatic patients are lacking, though many patients get their implants removed for one reason or another. Our endeavor was to document the common indications for removal of internal fixation devices and highlight potential issues, even as most specialists are already well versed with them.
Table 2.
Timing of implant removal in uncomplicated fracture healing; AO guidelines
We found that majority of patients that needed removal of implant were men (85.5%). Shrestha et al. in their retrospective series also found a male preponderance (189 out of 275 patients) to the tune of 68.72%.6 Their study, however, also included children. Abidi et al. reviewed 40 patients with implant-related pain who required removal. 30 of these (75%) were males.7 There definitely seems to be a strong male preponderance in implant removal surgeries.
The mean age of patients requiring removal for infection was higher (49.33 years) than those with pain (31.6 years) or implant failure (35 years).
In our study, implant associated pain or discomfort was the most common reason necessitating removal (39.75%). Brown et al. found that 31% patient sunder going open reduction and internal fixation of ankle fractures had persistent lateral pain.8 They also found that only 11 of 22 patients who got their hardware removed had improvement in the pain. Minkowitz et al. prospectively studied 60 patients who had implant removal for hardware pain, and at 1 year follow-up all their patients were satisfied.9 Although we did not primarily aim to evaluate the outcome after removal, all our patients had at least some relief in their hardware pain at 4 months follow-up. About 44% had complete relief. There was a statistically significant improvement in the mean pain VAS after implant removal.
The next most common indication in our series was implant infection (about 29%). Some of these patients had been treated non-operatively for varying lengths of time to control the infection but without success. Others presented for the first time at such a stage, e.g., skin necrosis, that removing the implant was the only logical option. Trampuz and Widmer estimated that overall about 5% of all internal fixation devices become infected.10 They also impressed the role of biofilms in the resistance of pathogens to systemically administered antibiotics. None of the infections in our study requiring removal was “early,” i.e., within 2 weeks of index procedure. Only one was a delayed infection (2-10 weeks), a woman with an olecranon plate who developed skin necrosis and the plate had to be removed 2 months after surgery. All the others were “late” infections, caused by constant hematogenous seeding of the implant from skin, respiratory, dental and urogenital infections. Infection after internal fixation is associated with greatly increased morbidity and cost. The incidence of infections is likely to rise as more operations are performed by the day, and longevity increases translating into greater periods of possible bacterial implant seeding in the body. Trampuz and Widmer recommended stoppage of any antibiotics 2 weeks before the removal surgery, if possible, to get an accurate intraoperative tissue culture. They also suggested that the removed implant be sonicated in saline to dislodge microorganisms from its surface and the resultant sonicated fluid be sent for microbiologic examination. Kukla et al. in a study of implants removed from the proximal femur (dynamic hip screw and Gamma Nails) found that the most common indications were avascular necrosis of the femoral head, deep chronic infections, shaft fractures, and screw cut-out.11
Implant failure was the next most common indication in our series in symptomatic patients but it was less common than those in whom the hardware was removed at the patient’s behest. Reasons for failure of the implant include faulty implant (poor quality), faulty operative technique, inadequate implant, delayed healing, and patient noncompliance. Akhtar et al. cited the most common cause of failure as poor quality of the implant.12 Peivandi et al. also concluded that the most common reason for implant failure was poor manufacturing. They recommended that credible and trusted implant brands should be used in fracture fixation.13 Sharma et al. in a restrospective study of 41 failed upper and lower limb implants found that plate failure was more common than nail failure in the lower limb.14 In most cases in their series, the patient had a significant re-trauma causing failure of the implant. All patients except one in our series also had failures of lower limb implants.
Implant removal operations constitute a significant portion of elective orthopedic surgeries. Several studies have been carried out on the indications of removal of metalwork in asymptomatic patients. Although most authors agree that routine removal should not be practiced, they also agree that there is a need for the development of concrete indication guidelines for implant removal. At the same time, there is a paucity of literature assessing the relative frequency of the “usual” indications of implant removal, viz., in symptomatic patients. Our study was an attempt at filling this gap. We believe that routine removal in asymptomatic patients should not be practiced, and if at all necessary, the removal should not require a larger procedure than the index operation. We also agree that implant removal surgeries are fraught with risks, including fractures, bleeding, nerve injuries and infection, and should be done only after explaining to the patient the possibility of all these complications. In addition to the possible new problems, the removal surgery may not entirely fulfill the intended purpose, e.g., the pain may not completely go away, infection may not resolve, and additional surgeries may be required. All these factors must be borne in mind before embarking on such a process with high hopes of success.
Our study is limited by a small sample size and a short follow-up period. Furthermore, almost all implants removed in our series were local made stainless steel. This may falsely favor titanium implants, although the probable reason for this is the low affordability of patients catered to by our center. More studies with greater number of cases and wider study dimensions are needed to produce concrete literature on the patterns of removal surgeries in symptomatic implants.
Conclusion
Symptomatic hardware frequently needs removal. We found that pain and implant prominence (mechanical symptoms) are the most common indications. Infection is the next most common, followed by hardware failure. Other indications are implant failure, bone resorption due to excessive stress shielding and patient’s will. Males are more likely to develop symptoms requiring removal of hardware. The average age of patients requiring removal for infection is higher than that for other reasons. We also found that implants around the ankle are most likely to require removal. Others include heavy implants over the olecranon and femoral IM nails. Carefully done, the removal should be a safe procedure, and there is a low but definite possibility of complications. Several factors like bone ingrowth and wear of the implant may make its removal difficult. Operative complications like nerve and vessel injury and fracture may occur. The symptoms too may not completely disappear the following removal.
References
- 1.Vos DI, Verhofstad MH. Indications for implant removal following fracture healing: A review of literature. Eur J Trauma Emerg Surg. 2013;39:327–37. doi: 10.1007/s00068-013-0283-5. [DOI] [PubMed] [Google Scholar]
- 2.Busam ML, Esther RJ, Obremskey WT. Hardware removal: Indications and expectations. J Am Acad Orthop Surg. 2006;14:113–20. doi: 10.5435/00124635-200602000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Hanson B, van der Werken C, Stengel D. Surgeons’ beliefs and perceptions about removal of orthopaedic implants. BMC Musculoskelet Disord. 2008;24(9):73. doi: 10.1186/1471-2474-9-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schmittenbecher PP. Implant removal in children. Eur J Trauma Emerg Surg. 2013;39:345–52. doi: 10.1007/s00068-013-0286-2. [DOI] [PubMed] [Google Scholar]
- 5.Krettek C, Müller C, Meller R, Jagodzinski M, Hildebrand F, Gaulke R. Is routine implant removal after trauma surgery sensible? Unfallchirurg. 2012;115:315–22. doi: 10.1007/s00113-012-2159-2. [DOI] [PubMed] [Google Scholar]
- 6.Shrestha R, Shrestha D, Dhoju D, Parajuli N, Bhandari B, Kayastha SR. Epidemiological and outcome analysis of orthopedic implants removal in Kathmandu University Hospital. Kathmandu Univ Med J (KUMJ) 2013;11:139–43. doi: 10.3126/kumj.v11i2.12489. [DOI] [PubMed] [Google Scholar]
- 7.Abidi SA, Umer MF, Ashraf SM, Mehdi SH, Ahmed SK, Shaikh IA. Outcome of painful implant removal after fracture union. Pak J Surg. 2012;28:114–7. [Google Scholar]
- 8.Brown OL, Dirschl DR, Obremskey WT. Incidence of hardware-related pain and its effect on functional outcomes after open reduction and internal fixation of ankle fractures. J Orthop Trauma. 2001;15:271–4. doi: 10.1097/00005131-200105000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Minkowitz RB, Bhadsavle S, Walsh M, Egol KA. Removal of painful orthopaedic implants after fracture union. J Bone Joint Surg Am. 2007;89:1906–12. doi: 10.2106/JBJS.F.01536. [DOI] [PubMed] [Google Scholar]
- 10.Trampuz A, Widmer AF. Infections associated with orthopedic implants. Curr Opin Infect Dis. 2006;19:349–56. doi: 10.1097/01.qco.0000235161.85925.e8. [DOI] [PubMed] [Google Scholar]
- 11.Kukla C, Gaebler C, Mousavi M, Vecsei V, Heinz T. Indications for implant removal ater healed proximal femoral fractures. Acta Chir Austriaca. 2000;32:196–8. [Google Scholar]
- 12.Akhtar A, Shami A, Abbassi SH, Zimri F, Mateen MA. Broken orthopaedic implants: An exerience at PIMS. Ann Pak Inst Med Sci. 2009;5:136–40. [Google Scholar]
- 13.Peivandi MT, Yusof-Sani MR, Amel-Farzad H. Exploring the reasons for orthopedic implant failure in traumatic fractures of the lower limb. Arch Iran Med. 2013;16:478–82. [PubMed] [Google Scholar]
- 14.Sharma AK, Kumar A, Joshi GR, John JT. Retrospective study of implant failure in orthopaedic surgery. Med J Armed Forces India. 2006;62:70–2. doi: 10.1016/S0377-1237(06)80164-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


