Abstract
The purpose of this study was to document predictors of long-term retention among minority participants in the Well Elderly 2 Study, a randomized controlled trial of a lifestyle intervention for community-dwelling older adults. The primary sample included 149 African American and 92 Hispanic men and women aged 60–95 years, recruited at senior activity centers and senior residences. Chi-square and logistic regression procedures were undertaken to examine study-based, psychosocial, and health-related predictors of retention at 18 months following study entry. For both African Americans and Hispanics, intervention adherence was the strongest predictor. Retention was also related to high active coping and average (vs. high or low) levels of activity participation among African Americans and high social network strength among Hispanics. The results suggest that improved knowledge of the predictors of retention among minority elders can spawn new retention strategies that can be applied at individual, subgroup, and sample-wide levels.
Keywords: retention, ethnicity, older adults
Introduction
Humans participate actively in their day-to-day lives by identifying self-relevant goals, formulating organized plans, strategizing in response to emergent problems, mulling over possible outcomes, relating situations to past personal experiences, and monitoring progress in relation to targeted goals (Kihlstrom & Cantor, 2000; Little, Salmela-Aro, & Phillips, 2007). These everyday navigational efforts are facilitated by aspects of human intelligence such as problem solving ability, emotional self-awareness, interpersonal relationship skills, and reality testing (Bar-On, 2005), and are further affected by person-relevant concerns such as coping styles, resource availability, and physical health status (Folkman & Moskowitz, 2004; Somerfield & McCrae, 2000).
Prior theory and research suggest that this notion of active involvement extends to older adults in their quest to maintain a healthy lifestyle. For example, Sabin (2005) has proposed a motivation equation model which specifies the critical role of individually perceived costs and opportunities, barriers such as safety and financial concerns, adherence to cultural expectations, and personality characteristics in accounting for older adults’ participation in exercise or therapy. In a similar vein, Fleury (1996), in a theory of wellness motivation, has emphasized the role of personal appraisals, comparison of targeted changes to existing life patterns, values and beliefs, and network affiliations in attempting to uncover the processes surrounding health behavior change in African American elders. In connection with this emphasis on active engagement in daily life choices, we conceptualize older adults’ continued participation in clinical research as a by-product of decision-making processes that are contextualized within an interactive dynamic that incorporates individual background characteristics and resources, psychological predilections, and emergent experiences during the course of a particular research involvement.
Retention of Minority Adults in Clinical Research
The rationale for including minority elders in clinical research is strong, and reflects the need to reduce health disparities by anchoring healthcare services to the results of controlled studies that generalize to groups that are underserved and typically at elevated risk (Areán, Alvidrez, Nery, Estes, & Linkins, 2003; Curry & Jackson, 2003; Stahl & Vasquez, 2004). Toward this end, culturally sensitive strategies such as ethnically matching research personnel to study participants or working with representatives from the local ethnic community have been identified to encourage research participation among minority elders (Moreno-John et al., 2004).
However, in addition to focusing on culturally relevant themes, it is potentially useful to attend to individual characteristics and experiences that predict research participation differences within a given pool of elders who share a common ethnic identity. Considerations such as coping style, activity patterns, physical functioning, or ongoing perceptions surrounding a research project can differ greatly among study participants who share the same ethnic background. Due to the complexity of everyday decision making, such considerations are likely to affect patterns of study involvement. Underscoring this notion, the recruitment of African American middle-aged and older adults in clinical research is related to psychosocially relevant individual difference variables such as motivation, depression, and spiritual beliefs (Advani et al., 2003; Woods et al., 2002).
Previously, very little research had been conducted on the relationship of psychosocial and health-related individual difference variables to the retention of minority older adults in clinical research. Such information on the person-based correlates of retention can serve at least two functions. First, it can spawn new strategies for retention by identifying the risk factors for discontinued participation among adults within specific ethnic groups. Second, knowledge of the predictors of participants’ perseverance in research can contribute to an understanding of biases that stem from sample attrition (Chatfield, Brayne, & Matthews, 2005).
Research on the psychosocially relevant correlates of retention in health intervention research is largely absent for minority older adults. However, several such studies have been conducted with African American or Hispanic younger adults. It is potentially useful to extrapolate this literature to older adults because as individuals age they will continue to manage a constellation of life factors that will likely influence their decisions about continued research participation (Tak, 2006). In studies of minority younger adults, correlates of retention have included greater social support, more education, lower levels of stress or depression, and non-smoker status (Chang, Brown, & Nitzke, 2009; El-Khorazaty et al., 2007; Senturia et al., 1998). However, in other such studies variables such as stress (Gross, Julion, & Fogg, 2001) or social support (Katz et al., 2001) have not been found to influence continued study involvement. Participants’ expressed reasons for discontinuance have underscored the everyday navigational interpretation of research involvement that is noted above, with withdrawal often prompted by study-relevant concerns such as lack of time, loss of interest in the study, denial of the need for intervention, difficulties in undergoing the intervention, or scheduling issues (El-Khorazaty et al., 2007; Janson, Alioto, & Boushey, 2001). In general, the above literature suggests that retention of minority participants is complex and contingent on factors such as the type and extent of study requirements, the particular characteristics of the study sample, and the specialized needs of participating individuals. In accord with such complexities, Chang et al. have opined that “extraordinary procedures” may be necessary to promote retention in studies that pose barriers to extended participation (2009, p. 9).
Purpose and Hypotheses
In this article, our purpose was twofold. First, we attempted to address a key knowledge gap by generating new information on the individual difference and study-relevant variables that potentially influence the retention of African American and Hispanic older adults in clinical research studies. Second, given the notion that the determinants of continued participation are multi-pronged and complex, we sought to develop a methodological framework for guiding the choice of retention strategies in specific studies.
Our assessment of retention predictors centered on two hypotheses. First, we hypothesized that, in a general sense, psychosocial and health-related individual difference variables are linked to ethnically diverse older adults’ long-term retention in clinical research. This expectation is based on: (a) the notion that such variables affect the active decision-making processes of such individuals, including the choice to continue participation in a study; and (b) the results of prior research on the retention of younger minority adults, as reviewed above. Our test of this hypothesis was largely exploratory, as the variables that we assessed (overall activity frequency, active coping, social support, social network strength, and physical and mental health-related quality of life) could, in principle, be either positively, negatively, or nonlinearly associated with retention. For instance, individuals who evidence a favorable psychosocial or health-related profile (e.g., more active, socially connected, or healthy) may have more resources available to support continued participation. Alternatively, such individuals could be less frequently retained due to having busier schedules or a reduced need for intervention services.
Our second hypothesis was that study-related variables (e.g. adherence to an intervention protocol or therapist-client ethnic matching) are associated with retention. In a manner similar to the first hypothesis, this expectation stems from the notion that retention reflects an evaluative decision that incorporates ongoing perceptions of the personal costs and benefits associated with a research project as it unfolds, as well as from the results of prior retention research involving minority adults.
Methods
Research Design
The data for this article stemmed from the Well Elderly 2 Study, a randomized controlled trial (RCT) which had a dual focus: (a) to test the effects of a lifestyle-based intervention for reducing health decline among ethnically diverse community-dwelling older adults; and (b) to uncover the mediating mechanisms that connect the intervention to its targeted outcomes. To achieve the second aim, the Well Elderly study team measured a number of psychosocial and health-related variables that are seldom included in RCT research. Consequently, the Well Elderly 2 Study afforded an excellent opportunity to examine the individual characteristics that predict continued study participation among minority elders.
The design entailed an exploratory correlation-based analysis of RCT data collected between 2004 and 2008. The RCT protocol contained a crossover feature in which all participants were scheduled to receive the intervention during either the first or the second six-month phase of their study participation (Clark et al., 2011). When not receiving the intervention, participants were not exposed to any experimental treatment. Study participation included longitudinal assessment at 6-month intervals (baseline and months 6, 12, and 18) on a variety of person-relevant variables. Further details of the Well Elderly 2 study design are reported in Jackson et al. (2009).
Sample
The total sample of Well Elderly 2 research participants consisted of 460 men and women aged 60 to 95 years who were residents of, users of, or visitors to the study sites. The sites were located in the greater Los Angeles area and included nine senior activity centers and 12 senior residences. Participants spoke either English or Spanish (the research protocol was administered in these two languages) and had an absence of severe cognitive impairment based on preliminary screening. Of 1,109 elders who were screened at the study sites, 838 (76%) were deemed study eligible. Of those who were eligible, 460 (54.8%) opted to enroll in the study. The chief sample for the present study consisted of participants who self-described their ethnic group as Black/African American (n = 149) or Hispanic or Latino (n = 92; among the 92 Hispanic/Latino participants, 67 undertook the study protocol in Spanish). The remaining RCT participants described their ethnic group as Asian (n = 18), White (n = 172), or Other/Refused (n = 29).
Recruitment, the Study Intervention, and Retention
Recruitment
Recruitment was overseen by a Project Manager who had significant prior experience in RCTs for older adults, as well as expertise in culturally sensitive research adaptations. As a first step, the research team established strong rapport with key study site personnel, which was critical insofar as prospective participants often relied upon the opinions of site staff members to evaluate the study’s legitimacy. At each study location, discussions were undertaken with staff members to identify a site-specific recruitment strategy that incorporated which meetings to target for recruitment presentations, which resident or visitor attitudes to consider, the best times to approach participants, and which subgroup leaders might be co-opted to support recruitment. Recruitment strategies that were applied at each of the sites included: (a) circulation of flyers and brochures; (b) delivery of presentations during site-based gatherings of residents or consumers; (c) sponsorship of festive gatherings with the distribution of raffle tickets on which prospective participants provided contact information and indicated their degree of willingness to participate; (d) scheduling of follow-up meetings to answer further questions about the study and provide an opportunity to enroll; and (e) employment of cultural adaptations such as the inclusion of ethnically relevant themes during recruitment functions.
Key cultural modifications to promote recruitment at the predominantly Hispanic sites included using translated recruitment materials, altering recruitment posters to include pictures of Hispanic elders, promoting a party-like atmosphere at recruitment events (e.g., through music and dancing), employing recruiters who did not merely speak Spanish but also shared the cultural background of the prospective participants, and enacting the consent process in a small group discussion format to reduce suspicion and facilitate the enrollment of elders with marginal reading skills. We undertook this latter adaptation because, prior to recruiting Spanish-speakers, qualitative interviews with leaders in the Hispanic community indicated that obtaining signatures on consent forms may be particularly problematic for this group due to having prior experiences of signing contracts that led to unexpected obligations.
Participants were recruited in two waves, separated by approximately 15 months, to allow for iteratively based solutions for obtaining the initially stipulated sample size (N = 440) in the event of unforeseen problems in procuring participants. Prior to recruitment, the research protocol was approved by the University of Southern California Institutional Review Board (IRB protocol no.HS-11-00521). The consent process was administered by the Project Manager or one of her assistants. To enroll in the study, participants provided informed consent at the respective study site after carefully reviewing the study requirements, having their study-related questions answered, and reading and signing the consent form.
The Study Intervention
The intervention, termed lifestyle redesign®, was a slightly modified version of a treatment approach found in a previous RCT to reduce declines in daily function, psychosocial well-being, and health-related quality of life among residents of low-income senior apartment complexes (Clark et al., 1997). In the current project, the intervention consisted of a six-month program involving weekly, two-hour small group meetings. In addition to group meetings, each elder was given the opportunity to participate in up to 10 individual sessions. The interveners were occupational therapists who, through didactic instruction and facilitation of self-reflection, helped elders grasp the importance of lifestyle and routine as a means of achieving health and well-being, led peer-based group discussions, organized outings into the community, and assisted each elder with the development of a personalized plan for healthy living. Modular content centered on such topics as the role of activity in promoting health, time use, conservation of energy, utilization of transportation options, home and community safety, social relationships, goal setting, and use of adaptive equipment. A culturally adapted variant of the intervention was administered to Hispanic elders who entered the Spanish language segment of the study.
Retention
Several strategies were used to retain participants. First, a strong (and successful) effort was made to avoid turnover among the project management personnel who interfaced with participants. The stability of these personnel enabled the participants to achieve sustained interpersonal familiarity with project staff, which we believe increased their comfort level and loyalty to the project. Second, during the intervention the treating therapists contacted the clients on a regular basis to inform them of upcoming events (e.g., group-based outings) and schedule treatment sessions. Third, the Project Manager sent reminder letters to participants three weeks in advance of their scheduled testing sessions. Fourth, the Project Manager and her assistant made repeated attempts to contact individuals who failed to attend testing sessions or appeared to have stopped contacting study staff. When participants were unreachable by phone, project staff visited the study sites in an effort to contact them informally for the purpose of scheduling appointments. Fifth, an attempt was made to be flexible in scheduling assessment sessions. For example, multiple group testing opportunities were made available at each study site, and in some cases individual sessions were undertaken to accommodate participants who were unable to attend group sessions. Finally, to compensate participants for their time and effort and thereby encourage continued adherence to the research protocol, each elder was provided with a $10 stipend each time his or her saliva samples (see below) were received, and a $20 stipend following each assessment session, except for the last session at which time a $40 disbursement was provided.
Measures
Typically, assessments were administered to small groups (n = 4 to 29) of participants in meeting rooms at the study sites. The assessment battery contained a general background survey (baseline assessment only) and psychosocial and health-related questionnaires. In addition, participants undertook cognitive performance tests, provided saliva-based biomarker specimens, and had their blood pressure recorded (data not analyzed in the current study).
Regarding the measure of retention, participants were considered to be retained if they undertook the study assessment battery at 18 months post study entry. It should be noted that African American and Hispanic elders who were assessed at 18 months completed the main study questionnaires at a rate of 99.9% during the session. The measurement of variables used to predict retention is summarized below, and is also reported elsewhere (Clark et al., 2011; Jackson et al., 2009). Except in the case of study-related variables (see below), participants’ baseline scores were used to define the predictors.
Self-reported demographic and background variables included ethnic group (see above categories), sex, age (60–69, 70–79, 80+ years), and educational level (less than high school, high school graduate, some college or more). An additional background variable, recorded by project staff, was site type (senior center or senior residence). Study-based predictors of retention included intervention timing (immediately following vs. 6 months following study entry), the number of group sessions attended and individual sessions attended, and client-therapist ethnic matching (matched or non-matched).
Six psychosocial and health-related constructs were included as predictors of retention. Each of these constructs was assessed via a self-rating questionnaire as described below.
Activity frequency was measured through the Meaningful Activity Participation Assessment (MAPA), a recently developed tool that includes an assessment of participation frequency for 28 different activities commonly performed by older adults (Eakman, Carlson, & Clark, 2010). Frequency of performance for each activity is scored on a 0 (not at all) to 6 (every day) scale, with the items summed to generate an overall frequency score. MAPA overall activity frequency scores have been shown to possess stability as well as construct validity within the ethnically diverse Well Elderly 2 sample (Carlson, Kuo, Chou, & Clark, 2012).
Active coping was assessed by the 4-item active coping subscale contained on the Coping Orientations to Problems Experienced (COPE) scale (Carver, Scheier, & Weintraub, 1989). Participants are asked to rate how they usually respond to stressful events in their life on a 1 to 4 scale, with a response of 4 indicating a high level of active, problem-focused coping. In studies of older adults, this scale has been shown to be internally consistent and has correlated in a theoretically predicted manner with multiple aspects of subjective well-being in late-life (e.g., Fisher, Segal, & Coolidge, 2003; Kling, Seltzer, Ryff, 1997). The COPE has also been used successfully in ethnically diverse samples (e.g., Njoku, Jason, & Torres-Harding, 2005).
Social support was measured using the 6-item version of Cohen, Mermelstein, Kamarck, and Hoberman’s (1985) Interpersonal Support Evaluation List (ISEL). This tool contains two items each for emotional, informational, and instrumental support. Following Martire, Schulz, Mittelmark, and Newson (1999), each item was rated on a 1 (definitely false) to a 4 (definitely true) scale. The ISEL has been shown to possess acceptable psychometric properties in use with older adults (e.g. Martire et al., 1999; Newsom & Schulz, 1996) and is applicable to ethnically diverse populations (Cooper, Ziegler, Nelesen, & Dimsdale, 2009).
Social network strength was assessed by administering the Lubben Social Network Scale (LSNS). The LSNS was developed to assess social network and isolation in elders (Lubben, 1988). Participants rate their access to and quantity of social networks involving family and friends on ten items that range from 0 (infrequently/none) to 5 (always/many). The LSNS has acceptable internal consistency in use with older adults (Gellis & Teguchi, 2004; Levy-Storms & Lubben, 2006), and has been used successfully in studies of older African Americans (e.g., Okwumabua, Baker, Wong, & Pilgram, 1997).
Physical health-related quality of life and mental health-related quality of life were assessed through the Physical Component Summary (PCS) and Mental Component Summary (MCS) scores stemming from Version 2 of the Short Form-36 Item Health Survey (SF-3v2). The SF-36v2 assesses self-perceptions of functional health and well-being (Ware, Kosinski, & Dewey, 2000), and has been shown to possess acceptable reliability and validity for use with older populations as well as ethnically diverse samples (Clark et al., 1997; Hayes, Morris, Wolfe, & Morgan, 1995; Madsen, 2000; Ngo-Metzger, Sorkin, Mangione, Gandek, & Hays, 2008).
Analysis Procedures
Separately for the African American and Hispanic subsamples, category frequencies or means were derived for all study variables at baseline, and chi-square tests and independent t-tests (Welch’s correction was used when the two groups had unequal variances) were conducted to assess possible differences between these two racial/ethnic groups. In addition, descriptive information was tabulated concerning the number of participants, by major ethnic group (African American, Hispanic, Caucasian), who were: (a) recruited into the study; and (b) subsequently retained at 6, 12, and 18 months, respectively. Chi-square tests were conducted to test for racial/ethnic differences in retention rates.
In assessing the hypothesized predictors, retention was analyzed over the interval stretching from study baseline to 18 months to allow for a maximally powerful and parsimonious analysis. The retention data at months 6 and 12 were not included, insofar as the individuals who dropped out at these intermediate time points were fewer in number and largely overlapped with those who dropped out by month 18. Two analytic strategies were used to document the predictors of retention. First, chi-square tests were conducted to examine patterns of association with retention, including nonlinear relationships, that pertain to discrete levels of a predictor. (Nonlinear relationships are a salient possibility due to complex substantive issues, which can create unknown or varying associations between a predictor and retention, depending on the particular level of the predictor.) The chi-square tests followed a three-step procedure. First, when a pre-existing categorization scheme was absent or not logically identifiable for a given predictor (i.e., for all predictors except sex, age [60–69, 70–79, 80+ yrs], education level, site type, intervention timing, and ethnic matching), the distribution was split into low, medium, and high groups, which respectively contained individuals below the 34th percentile, between the 34th and 66th percentiles, and above the 66th percentile of the full sample (N = 460). Second, a 2×2 or 3×2 chi-square test (or Fisher’s Exact Probability test when one or more cells had an expected frequency of 5 or less) was performed to examine the association between each predictor and retention. Finally, when a given 3×2 chi-square analysis was significant, separate 2×2 analyses were performed to test for differences in retention between each possible pair of predictor variable levels. This three-step procedure for identifying predictors was performed separately for African American and Hispanic participants.
To enable greater statistical control as well as assess the sensitivity of the results to an alternate analytic strategy, we also performed logistic regression analysis to test the predictors of retention at 18 months. In these analyses, which were conducted separately for the African American and Hispanic subsamples, we regressed the dichotomous retention variable onto each psychosocial, health-related, or study-based predictor after adjusting for sex, age group, education level, and site type. However, because substantial collinearity of predictor variables in regression models can cause erratic shifts in the estimation of beta values in response to minimal changes in the model or the data (Farrar & Glauber, 1967), in each model, we did not adjust simultaneously for more than one psychosocial, health-related, or study-based predictor.
All hypothesis tests were two-tailed and conducted at the .05 significance level. Due to the exploratory character of the analysis, in interpreting the results, emphasis was placed on identifying broad-based trends.
Results
Table 1 summarizes the predictor variable scores for minority study participants by ethnic group. Relative to African Americans, the Hispanic elders tended to have less education, reduced social support and social network strength, and poorer mental health-related quality of life, but were more likely to be ethnically matched with the intervener and attended more individual intervention sessions (all p’s < .05). No other predictor variables differed between the two groups.
Table 1.
Predictor Variable Means ± Standard Deviations or N (%) by Ethnic Group
| Predictor | African American (n=149) | Hispanic (n=92) | χ2 | pa |
|---|---|---|---|---|
| Sex | 0.00 | 1.00 | ||
| Male | 47 (31.5%) | 29 (31.5%) | ||
| Female | 102 (68.5%) | 63 (68.5%) | ||
| Age | 73.9 ± 7.1 | 73.2 ± 6.6 | 0.19 | .46 |
| 60–69 yrs | 55 (31.8%) | 76 (59.8%) | ||
| 70–79 yrs | 72 (41.6%) | 31 (24.4%) | ||
| 80+ yrs | 46 (26.6%) | 20 (15.8%) | ||
| Education level | 30.23 | < .0001 | ||
| < High school | 48 (32.2%) | 63 (68.5%) | ||
| High school | 39 (26.2%) | 10 (10.9%) | ||
| ≥ Some college | 62 (41.6%) | 19 (20.7%) | ||
| Site type | 2.22 | .14 | ||
| Senior center | 49 (32.9%) | 39 (42.4%) | ||
| Residence | 100 (67.1%) | 53 (57.6%) | ||
| Ethnic matching | 39.12 | < .0001 | ||
| Yes | 38 (25.5%) | 61 (66.3%) | ||
| No | 111 (74.5%) | 31 (33.7%) | ||
| Intervention Timing | 0.02 | .89 | ||
| Immediate | 78 (52.3%) | 49 (53.3%) | ||
| Delayed | 71 (47.7%) | 43 (46.7%) | ||
| Group sessions | 9.7 ± 8.3 | 11.6 ± 7.5 | .07 | |
| Individual sessions | 1.2 ± 1.5 | 4.0 ± 3.1 | < .0001 | |
| Activity frequency | 74.7 ± 22.2 | 70.4 ± 20.3 | .13 | |
| Active coping | 2.9 ± 0.8 | 2.8 ± 0.7 | .10 | |
| Social support | 11.1 ± 3.0 | 10.1 ± 2.3 | .004 | |
| Social network | 28.7 ± 8.5 | 26.3 ± 9.6 | .04 | |
| Physical HRQL | 40.5 ± 9.7 | 39.9 ± 10.0 | .66 | |
| Mental HRQL | 49.0 ± 11.2 | 43.5 ± 10.6 | .0002 |
p-values were calculated using t-tests for continuous variables and chi square tests for categorical variables.
Table 2 documents the number of African American, Hispanic, and Caucasian elders who were recruited into the study and retained at 6 months, 12 months, and 18 months. Combining all participants, retention was 78.7% at 6 months, 64.9% at 12 months, and 62.2% at 18 months. The percentage of participants who were retained did not differ by ethnic group at any of the three re-assessment time points (respective chi-square values for 6, 12, and 18 months = 1.48, 1.90, and 0.48, p-values >.40). Retention of African Americans and Hispanics combined was non-significantly higher than retention of Caucasians at 12 (66% vs. 66%, χ2 = 0.00, p = .98) and 18 (62% vs. 59%, χ2 = 0.52, p = .47) months.
Table 2.
Number and Percent Retained from Baseline at Four Six-Month Intervals According to Ethnic Group Membership
| Testing Points | Ethnic Group | χ2(2) | ||
|---|---|---|---|---|
|
| ||||
| African American | Hispanic | Caucasian | ||
| Baseline | 149 | 92 | 172 | |
| 6 months | 113 (75.8%) | 72 (78.3%) | 140 (81.4%) | 1.48, p = .48 |
| 12 months | 96 (64.4%) | 64 (69.6%) | 114 (66.3%) | 0.67, p = .71 |
| 18 months | 91 (61.7%) | 59 (64.1%) | 101 (58.7%) | 0.74, p = .69 |
Table 3 presents the test results for predictors of retention from baseline to 18 months. Significant predictors for African American elders included group sessions attended (p < .0001), individual sessions attended (p = .004), overall activity frequency (p = .02), and active coping (p = .04). Among Hispanic elders, significant predictors were the two intervention adherence variables (p < .0001 for both the group and individual sessions attended variables) and social network strength (p = .04). The two intervention adherence indicators had the strongest association with retention, with a contrast of 82% vs. 18% retention for high versus low group session attendance among Hispanics and of 87% vs. 33% for African Americans. Among African American or Hispanic elders, for psychosocial variables, the average degree of contrast in retention for the highest versus lowest levels among statistically significant predictors was 26.7% (75.7% minus 49.0% average rates for the high and low retention categories, respectively; Cohen’s d effect size = .75).
Table 3.
Percent Retained from 0 to 18 Months by Predictor Level
| Predictor | Ethnic Group | |||
|---|---|---|---|---|
|
| ||||
| African American (n = 149) | χ2 | Hispanic (n = 92) | χ2 | |
| Sex | 1.79, p = .18 | 0.56, p = .45 | ||
| Male | 53% (25/47) | 59% (17/29) | ||
| Female | 65% (66/102) | 67% (42/63) | ||
| Age | 0.21, p = .90 | 2.36, p = .31 | ||
| 60–69 yrs | 61% (28/46) | 73% (19/26) | ||
| 70–79 yrs | 60% (43/72) | 57% (26/46) | ||
| 80+ yrs | 65% (20/31) | 70% (14/20) | ||
| Educational level | 0.21, p = .90 | 0.24, p = .89 | ||
| <High school graduate | 60% (29/48) | 63% (40/63) | ||
| Complete high school | 64% (25/39) | 60% (6/10) | ||
| Some college or more | 60% (37/62) | 68% (13/19) | ||
| Site type | 0.15, p = .70 | 0.77, p = .38 | ||
| Senior center | 63% (31/49) | 69% (27/39) | ||
| Residence | 60% (60/100) | 60% (32/53) | ||
| Intervention Timing | 3.25, p = .07 | 0.06, p = .80 | ||
| Intermediate | 68% (53/78) | 65% (32/49) | ||
| Delayed | 54% (38/71) | 63% (27/43) | ||
| Number of group sessions | 32.74, p < .0001 | 26.95, p < .0001 | ||
| Low (0–2) | 33%a (18/55) | 18%a (4/22) | ||
| Medium (3–16) | 69%b (33/48) | 75%b (27/36) | ||
| High (17–22) | 87%c (40/46) | 82%b (28/34) | ||
| Number of individual sessions | 10.99, p = .004 | 21.55, p < .0001 | ||
| Low (0) | 48%a (36/75) | 23%a (5/22) | ||
| Medium (1–2) | 72%b (26/36) | 77%b (10/13) | ||
| High (3–15) | 76%b (29/38) | 77%b (44/57) | ||
| Ethnic Matching | 0.22, p = .64 | 0.75, p = .39 | ||
| Not matched | 62% (69/111) | 58% (18/31) | ||
| Matched | 58% (22/38) | 67% (41/61) | ||
| Overall activity frequency | 8.04, p = .02 | 1.99, p = .37 | ||
| Low (0–65) | 47%a (26/55) | 56% (20/36) | ||
| Medium (66–86) | 74%b (37/50) | 71% (27/38) | ||
| High (87–140) | 64%a,b (28/44) | 67% (12/18) | ||
| Active coping | 6.66, p = .04 | 0.19, p = .91 | ||
| Low (1.00–2.76) | 53%a (34/64) | 64% (32/50) | ||
| Medium (3.00–3.26) | 53%a (16/30) | 67% (18/27) | ||
| High (3.50–4.00) | 75%b (41/55) | 60% (9/15) | ||
| Social support (P) | 2.40, p = .30 | 1.76, p = .41 | ||
| Low (1–9) | 52% (23/44) | 63% (24/38) | ||
| Medium (10–12) | 67% (41/61) | 60% (26/43) | ||
| High (13–18) | 61% (27/44) | 82% (9/11) | ||
| Social network strength (P) | 0.90, p = .64 | 6.46, p = .04 | ||
| Low (2–22) | 55% (18/33) | 47%a (14/30) | ||
| Medium (23–30) | 61% (28/46) | 69%a,b (24/35) | ||
| High (31–50) | 64% (45/70) | 78%b (21/27) | ||
| Physical HRQL (H) | 4.07, p = .13 | 0.01, p = .99 | ||
| Low (14.89–36.21) | 59% (32/54) | 65% (22/34) | ||
| Medium (36.25–46.20) | 71% (37/52) | 63% (19/30) | ||
| High (46.23–65.43) | 51% (22/43) | 64% (18/28) | ||
| Mental HRQL (H) | 2.37, p = .31 | 0.79, p = .67 | ||
| Low (12.93–42.11) | 56% (24/43) | 67% (31/46) | ||
| Medium (42.18–54.16) | 70% (31/44) | 64% (18/28) | ||
| High (54.17–72.59) | 58% (36/62) | 56% (10/18) | ||
For significant predictors, pairs of levels that do not share a common superscript differ from each other.
The logistic regression results are provided in Table 4. Similar to the results obtained in the zero-order chi-square analyses, significant prediction of 18-month retention was present for group and individual session attendance (both African Americans and Hispanics), active coping (African Americans), and social network (Hispanics). However, unlike the chi-square results, the variable activity frequency was non-significant for African Americans.
Table 4.
Logistic Regression for Predictors of Retention at 18 Months (Adjusted for Sex, Age Group, Education Level, and Site Type)
| African American | Hispanic | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Predictors | Beta | 95% CI | Odds Ratio | OR 95% CI | p-value | Beta | 95% CI | Odds Ratio | OR 95% CI | p-value |
| Intervention timinga | −.65 | −1.33, 0.03 | 0.52 | 0.27, 1.03 | .06 | −.05 | −0.93, 0.83 | 0.95 | 0.39, 2.31 | .91 |
| Group sessions | .14 | 0.08, 0.19 | 1.15 | 1.09, 1.21 | < .0001 | .17 | 0.09, 0.26 | 1.19 | 1.10, 1.29 | < .0001 |
| Individual sessions | .40 | 0.14, 0.67 | 1.50 | 1.15, 1.95 | .003 | .35 | 0.17, 0.53 | 1.42 | 1.18, 1.71 | .0002 |
| Activity frequency | .01 | 0.00, 0.03 | 1.01 | 1.00, 1.03 | .17 | .01 | −0.01, 0.04 | 1.01 | 0.99, 1.04 | .30 |
| Active coping | .52 | 0.11, 0.94 | 1.69 | 1.12, 2.55 | .01 | −.19 | −0.81, 0.42 | 0.83 | 0.45, 1.53 | .54 |
| Social support | .03 | −0.09, 0.15 | 1.03 | 0.92, 1.16 | .61 | .09 | −0.11, 0.30 | 1.10 | 0.89, 1.35 | .38 |
| Social network | .02 | −0.02, 0.06 | 1.02 | 0.98, 1.06 | .34 | .07 | 0.02, 0.13 | 1.07 | 1.02, 1.13 | .01 |
| Physical HRQL | −.01 | −0.05, 0.02 | 0.99 | 0.95, 1.02 | .49 | −.03 | −0.08, 0.03 | 0.98 | 0.93, 1.03 | .32 |
| Mental HRQL | −.01 | −0.04, 0.02 | 0.99 | 0.96, 1.02 | .54 | −.004 | −0.05, 0.04 | 1.00 | 0.95, 1.05 | .86 |
Higher scores were used to indicate delayed intervention.
Discussion
The first research hypothesis received partial support insofar as, among minority older adults who enrolled in a large RCT, study retention was related to baseline measures of selected psychosocial variables. This overall result for African American and Hispanic elders is consistent with past research on younger adults which suggests that retention is a complex process that is sensitive to person-relevant considerations (Chang et al., 2009; Senturia et al., 1998). Further, the finding of a difference of 26.7% in retention between significantly different levels of psychosocial variables indicates that the influence of predictors is nontrivial and that this type of information can potentially be used to inform new approaches that facilitate retention.
In one case, a nonlinear pattern of association with retention was obtained. In particular, African Americans with an intermediate level of overall activity frequency had a higher retention rate than those with either a high or low activity level (although the difference between the medium and high groups did not achieve statistical significance), a trend which masked the ability to detect any association between these variables in the logistic regression analysis (in which non-monotonic relationships are precluded). One explanation for this curvilinear result is that individuals with low or high degrees of activity, respectively, may have faced separate issues that hindered continued participation. In particular, inactive elders may have withdrawn from the study as a result of special difficulties with continued participation, whereas highly active elders may have opted to discontinue because of an overcrowded schedule or perhaps as a result of having less vested interest in the study due to outside personal involvements.
Other psychosocial predictors were related to retention in a more straightforward manner, including social network strength among Hispanics and active coping among African Americans. Our preferred explanation for these latter results is that elders with high scores on these variables were more able, or more psychologically predisposed, to continue study participation.
The second study hypothesis was more firmly supported in that the two intervention adherence variables were strongly linked to continued study participation, a finding consistent with prior research in which individuals who encountered difficulties with an intervention were more likely to drop out (Janson et al., 2001). Considering African Americans and Hispanics combined, only 29% of the elders who were low in group session attendance were later retained at 18 months, as opposed to 79% of those who had medium or high attendance. Several reasons may underlie this robust pattern of association. First, participants’ experiences with the intervention may have affected their judgments about the merits of remaining in the study. Second, the result may reflect individual differences in perseverance or in the extent of keeping one’s perceived obligations, with elders who are high on this dimension opting to continue participation in both the intervention and the study. Additionally, it is also possible that, due to the weekly commitment required to continue intervention participation, emergent problems with attending sessions were sometimes encountered (e.g., lack of time), which had a parallel adverse effect on study retention.
The above finding suggests that retention of older adult minority participants in clinical research studies can be boosted by the use of strategies that promote intervention adherence. However, the results of subsidiary analyses indicate that the correlates of adherence, as well as the exact nature of the link between adherence and retention, are complex and nuanced. For example, in the combined sample of African Americans and Hispanics, group session attendance was associated with greater activity frequency (p = .031) and higher social network strength (p = .05), whereas individual session attendance was related to poorer mental health-related quality of life (p = .002). Further underscoring the complexity of the relationship between intervention adherence and retention, among individuals who participated in a low number of individual intervention sessions, a higher percentage of African American than Hispanic elders were retained at 18 months (48% vs. 23%; χ2 [1] = 7.88, p < .01). One explanation for this latter finding, consistent with therapists’ observations, is that African American participants frequently appeared to thrive in the group sessions and consequently may have felt less of a need for individual attention (J. Jackson, personal communication, February 2011). Therefore, although our overall results suggest that strategies for promoting adherence can potentially enhance retention, efforts to achieve adherence should ideally consider participants’ individual characteristics. Additionally, caution should be exercised to ensure that retention strategies do not reduce a study’s external validity by promoting adherence (as well as perhaps an enhanced experimental effect) through the use of procedures that do not typically accompany the non-research use of an intervention.
With respect to intervention timing, it is possible that the obtained null result occurred because all of the participants either began the intervention, or knew they would begin the intervention, relatively early during the course of the study. It is also possible that subtle cancelling effects were present – e.g., some elders may have dropped due to being disappointed with the intervention, some may have stayed due to satisfaction with the intervention, some may have been happy to have the intervention delayed due to time constraints, and some may have withdrawn in frustration due to not receiving the intervention right away. It is therefore conceivable that some sort of mixture of these concerns caused a cancelling effect which minimized the relevance of early versus later intervention as a predictor of retention when considered across the sample as a whole. This type of possibility illustrates the potential complexities in relating psychologically relevant processes to retention.
In interpreting the results for specific variables, it is important to note that various idiosyncrasies of the research design are likely to have significantly affected the predictive relationships. For example, exposure to the lifestyle intervention, which strongly emphasized the salubrious effects of continued activity involvement, may have directly influenced the decision to continue participation in the research project, thereby weakening the relative effect on retention of variables such as age or social support. Likewise, the absence of a positive effect for selected variables previously identified as important, such as ethnic matching and physical health (Chatfield et al., 2005; Levkoff, Levy, & Weitzman, 2000), may have been due to study design features such as the employment of interveners with strong cultural sensitivities, the inclusion of relatively healthy elders, or the conduct of the study at sites already frequented by participants. Therefore, the results for selected predictors may not extend to intervention studies that use alternate logistic procedures or that examine different types of interventions such as drug treatments. In a more general sense, we speculate that the predictors of minority retention are likely to vary greatly across studies in accordance with differences in sample composition, geographical location, intervention characteristics, measurement procedures, and research participation requirements. This expectation is supported by the relatively nuanced flavor of the current results, as well as the outcome of a prior investigation involving older African Americans in which retention was higher for males and younger participants in a community study, but higher for females and older participants in a clinic-based study (Hudson, Leventhal, Contrada, Leventhal, & Brownlee, 2000). Further research is needed to better understand the effect of various study characteristics on patterns of retention.
Limitations
An important limitation of the study pertains to its exploratory nature. Given the number of significance tests, as well as the limited degree of power (well below 80% for within-ethnic group comparisons of proportions that differ by 25%), the hypothesis test results should be viewed as preliminary and in need of replication. Despite this caveat, in an overall sense the results tentatively confirm the value of attending to individual difference variables in conceptualizing retention outcomes among minority elders.
Practical Implications
Despite potential limitations in the area of generality, it is important for investigators to accumulate knowledge about the person-centered predictors of minority retention within different research situations. Armed with such information, within a given study it would be possible in advance to better identify, and potentially remedy, the degree or pattern of dropout risk for participants with different personal characteristics or study-based experiences. Accordingly, selected authors have noted the potential value of using individually tailored or person-specific approaches to recruit (Vesey, 2003) or retain (Hazuda et al., 2000) ethnically diverse elders, despite the limited attention that is devoted to this possibility in more general reviews of strategies for increasing research participation (Robinson, Dennison, Wayman, Pronovost, & Needham, 2007; Yancey, Ortega, & Kumanyika, 2006). Whether obtained through specialized questionnaires or via interviews, individually based information could be used to design a personalized study retention strategy for each participating elder. In developing such plans, it would be critical for the participant to take an active role, with joint researcher-participant cooperation being paramount. Further research, including qualitative studies, on the psychosocial and decision-making processes that affect minority retention could facilitate this process by uncovering which variables should be addressed in specified research participation contexts.
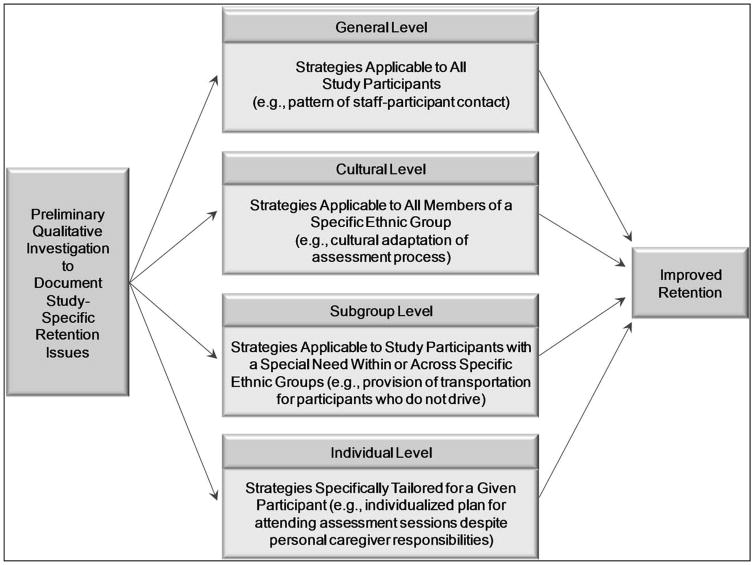
Figure 1 presents a four-tiered procedural model which could be applied as a prelude to conducting large clinical studies involving minority older adults. This model is consistent with the current findings, which reveal that individual difference variables that are not directly related to culture can predict retention among members of a given ethnic group. The model also reflects the expectation that the factors that affect retention can vary across studies in a non-obvious manner, and therefore need to be fleshed out through preliminary research. In the model, retention strategies are conceptualized at the general level (applicable to all participants), the cultural level (applicable to all participants from a particular ethnic group), the generalized subgroup level (applicable to subgroups of individuals with a special need within or across ethnic groups), and the individual level (applicable on a participant-by-participant basis).
Figure 1.
A model of comprehensive planning for the retention of minority older adults in behavioral and clinical research.
Based on the model, as part of the study planning process, a preliminary qualitative investigation could be conducted to uncover, within each of the four levels, salient issues that potentially affect elders’ decisions to continue participation. The results of such pilot work could be used to inform study protocol adaptations such as modifying participant stipends (general level), providing separately matched interveners for Mexican and Cuban participants (cultural level), offering transportation services to facilitate in-person testing to participants who do not drive (generalized subgroup level), or working out a plan for phone contact and assessment during a participant’s upcoming vacation (individual level). The aim would be to boost retention through use of a comprehensive approach that carefully incorporates the multi-tiered personal characteristics and perspectives of members of the study population. It is noteworthy that this approach is designed to increase minority retention not only through routes that directly focus on culture, but also through additional means that focus on personal considerations which may or may not have any clear relationship to culture. In this regard, it is expected that the procedural model portrayed in Figure 1 is applicable to elders of all racial/ethnic backgrounds. Future research is needed to test whether the application of comprehensive retention plans, such as the one advocated here, leads to enhanced retention.
Conclusion
In summary, this study underscores the potential value of attempting to document the fluid, person-centered considerations that influence minority older adults’ continued participation in behavioral or clinical research. Such information has the ability to spawn new retention strategies that are sensitive to the everyday concerns of participating elders, thereby helping to alleviate existing health disparities by promoting research that generalizes to all older adults.
Acknowledgments
We thank Ms. Ann Kuo and Mr. Danny Park for assisting in the preparation of this manuscript for submission.
Funding
This research was supported by National Institutes of Health grant R01 AG021108 from the National Institute on Aging.
Footnotes
IRB Protocol Number: HS-11-00521
Declaration of Conflicting Interests
The authors declared no potential conflicts of interests with respect to the authorship and/or publication of this article.
References
- Advani AS, Atkeson B, Brown CL, Peterson BL, Fish L, Johnson JL, Gockerman JP, Gautier M. Barriers to the participation of African-American patients with cancer in clinical trials. Cancer. 2003;97:1499–1506. doi: 10.1002/cncr.11213. [DOI] [PubMed] [Google Scholar]
- Areán PA, Alvidrez J, Nery R, Estes C, Linkins K. Recruitment and retention of older minorities in mental health services research. The Gerontologist. 2003;43:36–44. doi: 10.1093/geront/43.1.36. [DOI] [PubMed] [Google Scholar]
- Bar-On R. The Bar-On model of emotional-social intelligence. Fernández-Berrocal P, Extremera N, editors. Psicothema. 2005;17:1–28. Special Issue on Emotional Intelligence. Retrieved from http://www.ressourcesetmanagement.com/Article%20prof%20%20Baron%20.pdf.
- Carlson M, Kuo A, Chou CP, Clark F. Relationship of global activity evaluative ratings to psychosocial and health-related aging outcomes. 2012 Manuscript submitted for publication. [Google Scholar]
- Carver C, Scheier M, Weintraub J. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56:267–283. doi: 10.1037/0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves. Journal of Clinical Epidemiology. 2005;58:13–19. doi: 10.1016/j.jclinepi.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Chang M, Brown R, Nitzke S. Participant recruitment and retention in a pilot program to prevent weight gain in low-income overweight and obese mothers. BMC Public Health. 2009;9:424–435. doi: 10.1186/1471-2458-9-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark F, Azen SP, Zemke R, Jackson J, Carlson M, Mandel D, … Lipson L. Occupational therapy for independent-living older adults. A randomized controlled trial. Journal of the American Medical Association. 1997;278(16):1321–6. Retrieved from http://jama.ama-ssn.org.libproxy.usc.edu/cgi/reprint/278/16/1321. [PubMed] [Google Scholar]
- Clark F, Jackson J, Carlson M, Chou C, Cherry B, Jordan-Marsh M, … Azen SP. Effectiveness of a lifestyle intervention in promoting the well-being of independently living older people: Results of the Well Elderly 2 Randomised Controlled Trial. Journal of Epidemiology and Community Health. 2012;66:782–790. doi: 10.1136/jech.2009.099754. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social support: Theory, research, and application. The Hague, Holland: Martinus Nijhoff; 1985. [Google Scholar]
- Cooper DC, Ziegler MG, Nelesen RA, Dimsdale JE. Racial differences in the impact of social support on nocturnal blood pressure. Psychosomatic Medicine. 2009;71:524–531. doi: 10.1097/PSY.0b013e31819e3a93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry L, Jackson J, editors. The science of inclusion. Recruiting and retaining racial and ethnic elders in health research. Washington, DC: Gerontological Society of America; 2003. [Google Scholar]
- Eakman AM, Carlson M, Clark F. The Meaningful Activity Participation Assessment: A measure of engagement in personally valued activities. International Journal of Aging and Human Development. 2010;70(4):299–317. doi: 10.2190/AG.70.4.b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Khorazaty MN, Johnson AA, Kiely M, El-Mohandes AAE, Subramanian S, Laryea HA, Joseph JG. Recruitment and retention of low-income minority women in a behavioral intervention to reduce smoking, depression, and intimate partner violence during pregnancy. BMC Public Health. 2007;7:233–251. doi: 10.1186/1471-2458-7-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrar DE, Glauber RR. Multicollinearity in regression analysis: The problem revisited. The Review of Economics and Statistics. 1967;49(1):92–107. [Google Scholar]
- Fisher BM, Segal DL, Coolidge FL. Assessment of coping in cognitively impaired older adults: a preliminary study. Clinical Gerontologist. 2003;26(3/4):3–12. [Google Scholar]
- Fleury J. Wellness motivation theory: An exploration of theoretical relevance. Nursing Research. 1996;45(5):277–283. doi: 10.1097/00006199-199609000-00005. [DOI] [PubMed] [Google Scholar]
- Folkman S, Moskowitz JT. Coping: Pitfalls and promise. Annual Review of Psychology. 2004;55:745–774. doi: 10.1146/annurev.psych.55.090902.141456. [DOI] [PubMed] [Google Scholar]
- Gellis ZD, Taguchi A. Depression and health status among community-dwelling Japanese American elderly. Clinical Gerontologist. 2004;27(3):23–38. [Google Scholar]
- Gross D, Julion W, Fogg L. What motivates participation and dropout among low-income urban families of color in a prevention intervention? Family Relations. 2001;50(3):246–254. [Google Scholar]
- Hayes V, Morris J, Wolfe C, Morgan M. The SF-36 Health Survey Questionnaire: Is it suitable for use with older adults? Age and Ageing. 1995;24:120–125. doi: 10.1093/ageing/24.2.120. [DOI] [PubMed] [Google Scholar]
- Hazuda HP, Gerety M, Williams JW, Lawrence V, Calmbach W, Mulrow C. Health promotion research with Mexican American elders: Matching approaches to settings at the mediator- and micro-levels of recruitment. In: Levkoff SE, Prohaska TR, Weitzman PF, Ory MG, editors. Recruitment and retention in minority populations. New York, NY: Springer Publications; 2000. pp. 79–80. [Google Scholar]
- Hudson SV, Leventhal H, Contrada R, Leventhal EA, Brownlee S. Predicting retention for older African Americans in a community study and a clinical study: Does anything work? In: Levkoff SE, Prohaska TR, Weitzman PF, Ory MG, editors. Recruitment and retention in minority populations. New York, NY: Springer Publications; 2000. pp. 67–78. [Google Scholar]
- Jackson J, Mandel D, Blanchard J, Carlson M, Cherry B, Azen S, … Clark F. Confronting challenges in intervention research with ethnically diverse older adults: The USC Well Elderly II Trial. Clinical Trials. 2009;6(1):90–101. doi: 10.1177/1740774508101191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janson SL, Alioto ME, Boushey HA. Attrition and retention of ethnically diverse subjects in a multicenter randomized controlled research trial. Controlled Clinical Trials. 2001;22(6, Suppl 1):S236–S243. doi: 10.1016/s0197-2456(01)00171-4. [DOI] [PubMed] [Google Scholar]
- Katz KS, El-Mohandes A, McNeely Johnson D, Jarrett M, Rose A, Cober M. Retention of low income mothers in a parenting intervention study. Journal of Community Health. 2001;26(3):203–218. doi: 10.1023/a:1010373113060. [DOI] [PubMed] [Google Scholar]
- Kihlstrom JF, Cantor N. Social intelligence. In: Sternberg RJ, editor. Handbook of intelligence. 2. Cambridge, U.K: Cambridge University Press; 2000. pp. 359–379. [Google Scholar]
- Kling KC, Seltzer MM, Ryff CD. Distinctive late-life challenges: Implications for coping and well-being. Psychology and Aging. 1997;12(2):288–295. doi: 10.1037//0882-7974.12.2.288. [DOI] [PubMed] [Google Scholar]
- Levkoff SE, Levy BR, Weitzman PF. The matching model of recruitment. In: Levkoff SE, Prohaska TR, Weitzman PF, Ory MG, editors. Recruitment and retention in minority populations. New York, NY: Springer Publications; 2000. pp. 29–38. [Google Scholar]
- Levy-Storms L, Lubben JE. Network composition and health behaviors among older Samoan women. Journal of Aging and Health. 2006;18(6):814–836. doi: 10.1177/0898264306293263. [DOI] [PubMed] [Google Scholar]
- Little BR, Salmela-Aro K, Phillips SD, editors. Personal project pursuit: Goals, action and human flourishing. Malway, NJ: Lawrence Erlbaum Associates, Inc., Publishers; 2007. [Google Scholar]
- Lubben JE. Assessing social networks among elderly populations. Family and Community Health. 1988;11:42–52. [Google Scholar]
- Madsen F. Quality of life questionnaires for all respiratory diseases, every language suitable for use with older adults? Respiratory Medicine. 2000;94:187–189. doi: 10.1053/rmed.1999.0739. [DOI] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Mittelmark MB, Newson JT. Stability and change in older adults’ social contact and social support: The cardiovascular health study. Journal of Gerontology: Social Sciences. 1999;54:302–311. doi: 10.1093/geronb/54b.5.s302. [DOI] [PubMed] [Google Scholar]
- Moreno-John G, Gachie A, Fleming CM, Nápoles-Springer A, Mutran E, Manson SM, Pérez-Stable EJ. Ethnic minority older adults participating in clinical research: Developing trust. Journal of Aging and Health. 2004;16(Suppl 5):93S–123S. doi: 10.1177/0898264304268151. [DOI] [PubMed] [Google Scholar]
- Newsom JT, Schulz R. Social support as a mediator in the relation between functional status and quality of life in older adults. Psychology and Aging. 1996;11:34–44. doi: 10.1037/0882-7974.11.1.34. [DOI] [PubMed] [Google Scholar]
- Ngo-Metzger Q, Sorkin DH, Mangione C, Gandek B, Hays RD. Evaluating the SF-36 Health Survey (Version 2) in Older Vietnamese Americans. Journal of Aging and Health. 2008;20:420–436. doi: 10.1177/0898264308315855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Njoku MGC, Jason LA, Torres-Harding SR. The relationships among coping styles and fatigue in an ethnically diverse sample. Ethnicity and Health. 2005;10:263–278. doi: 10.1080/13557850500138613. [DOI] [PubMed] [Google Scholar]
- Okwumabua JO, Baker FM, Wong SP, Pilgram B. Characteristics of depressive symptoms in elderly urban and rural African American residents. Journal of Gerontology: Medical Sciences. 1997;52A:M241–M246. doi: 10.1093/gerona/52a.4.m241. [DOI] [PubMed] [Google Scholar]
- Robinson KA, Dennison CR, Wayman DM, Pronovost PJ, Needham DM. Systematic review identifies number of strategies important for retaining study participants. Journal of Clinical Epidemiology. 2007;60:757–765. doi: 10.1016/j.jclinepi.2006.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabin KL. Older adults and motivation for therapy and exercise: Issues, influences, and interventions. Topics in Geriatric Rehabilitation. 2005;21(3):215–220. [Google Scholar]
- Senturia YD, McNiff Mortimer K, Baker D, Gergen P, Mitchell H, Joseph C, Wedner HJ. Successful techniques for retention of study participants in an inner-city population. Controlled Clinical Trials. 1998;19(6):544–554. doi: 10.1016/s0197-2456(98)00032-4. [DOI] [PubMed] [Google Scholar]
- Somerfield MR, McCrae RR. Stress and coping research: Methodological challenges, theoretical advances, and clinical applications. American Psychologist. 2000;55(6):620–625. doi: 10.1037//0003-066X.55.6.620. [DOI] [PubMed] [Google Scholar]
- Stahl SM, Vasquez L. Approaches to improving recruitment and retention of minority elders participating in research: Examples from selected research groups including the National Institute on Aging’s Resource Centers for Minority Aging Research. Journal of Aging and Health. 2004;16(Suppl 5):9S–17S. doi: 10.1177/0898264304268146. [DOI] [PubMed] [Google Scholar]
- Tak SH. An insider perspective of daily stress and coping in elders with arthritis. Orthopaedic Nursing. 2006;25(2):127–132. doi: 10.1097/00006416-200603000-00010. [DOI] [PubMed] [Google Scholar]
- Vesey GA. Recruitment and retention of minority elders in health-related research: A community-based approach. In: Curry L, Jackson J, editors. The science of inclusion: Recruiting and retaining racial and ethnic elders in health research. Washington, DC: The Gerontological Society of America; 2003. pp. 82–89. [Google Scholar]
- Ware JE, Kosinski M, Dewey JE. How to score version two of the SF–36 Health Survey. Lincoln, RI: QualityMetric Incorporated; 2000. [Google Scholar]
- Woods MN, Harris KJ, Mayo MS, Catley D, Scheibmeir M, Ahluwalia JS. Participation of African Americans in a smoking cessation trial: A quantitative and qualitative study. Journal of the National Medical Association. 2002;94(7):609–618. [PMC free article] [PubMed] [Google Scholar]
- Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annual Review of Public Health. 2006;27:1–28. doi: 10.1146/annurev.publhealth.27.021405.102113. [DOI] [PubMed] [Google Scholar]