Abstract
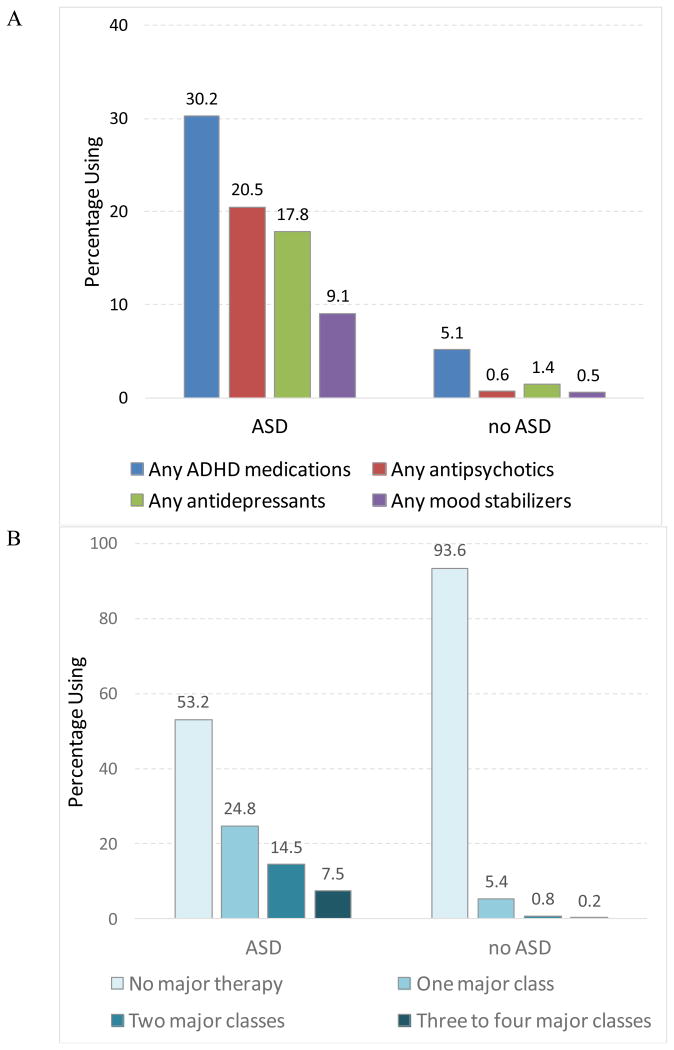
This study examined psychotropic medication use among 7901 children aged 1-17 with autism spectrum disorder (ASD) in five health systems, comparing to matched cohorts with no ASD. Nearly half (48.5%) of children with ASD received psychotropics in the year observed; the most common classes were stimulants, alpha-agonists, or atomoxetine (30.2%), antipsychotics (20.5%), and antidepressants (17.8%). Psychotropic treatment was far more prevalent among children with ASD, as compared to children with no ASD (7.7% overall), even within strata defined by the presence or absence of other psychiatric diagnoses. The widespread use of psychotropics we observed, particularly given weak evidence supporting the effectiveness of these medications for most children with ASD, highlights challenges in ASD treatment and the need for greater investment in its evaluation.
Keywords: autism spectrum disorder, medications, antipsychotics, comorbidities, epidemiological studies
Autism spectrum disorder (ASD) affects an estimated 1 in 68 children (Developmental, 2014). Steep increases in the prevalence of diagnosed ASD over recent decades have sharpened focus on the need to understand the causes, presentation, and potential treatments for ASD (Dawson, 2013; Matson & Kozlowski, 2011). The autism spectrum encompasses wide variation in severity and phenotype, with core features being social and communication impairments and restricted, repetitive behaviors or interests (Johnson & Myers, 2007). No pharmacologic treatments are effective for the core symptoms of ASD, but a range of psychotropic medications are used in practice to alleviate commonly associated symptoms and problem behaviors, such as irritability, tantrums, aggression, self-harm, hyperactivity, impulsivity, distractibility, mood dysregulation, and social withdrawal. Widespread psychotropic medication use is driven by the desire to assist children in achieving their potential in less restrictive settings and to ease the burdens of behavioral problems on caregivers and teachers (Karst & Van Hecke, 2012; Siegel & Beaulieu, 2012).
Previous studies of psychotropic medication utilization among children with ASD differ widely in populations and methodological approaches. Nevertheless, results have been reasonably consistent. The largest US study, among children on Medicaid, found that 56% had taken 1 or more psychotropic medications in 2001 (Mandell et al., 2008). The prevalence of use found in large studies of privately insured children (43%-57%) (Croen, Najjar, Ray, Lotspeich, & Bernal, 2006; Oswald & Sonenklar, 2007) and in smaller parent surveys and convenience samples (35% to 54%) (Aman, Lam, & Collier-Crespin, 2003; Esbensen, Greenberg, Seltzer, & Aman, 2009; Logan et al., 2012; Rosenberg et al., 2010) is comparable. Higher utilization has been consistently associated with older ages and the presence of comorbid psychiatric diagnoses, while the influence of other measurable factors has been less clear. There is a lack of recent data from large pediatric populations.
We examined psychotropic medication use among children with autism spectrum disorder (ASD) across 5 geographically diverse nonprofit US health plans, comparing results to a matched population without ASD. We predicted that psychotropic treatment would be more common among children with ASD regardless of the presence of other psychiatric diagnoses, which could suggest that psychotropics were targeted at ASD symptoms. Our comparative approach and explorations of polypharmacy, quantity dispensed, and the influence of age, sex, and psychiatric comorbidity on medication use provide new insights into current practices in ASD treatment.
Methods
Study Population and Setting
Our investigation was part of the Autism Registry project of the Mental Health Research Network (MHRN) (Ahmedani et al., 2014; Coleman et al., 2015; Cummings et al., 2016; Lu et al., 2014; MHRN; Penfold et al., 2013). MHRN aims to improve the quality and efficiency of mental health research, and is a subset of the Health Care Systems Research Network, a consortium of 18 public-domain research centers throughout the US. Five centers participated in the present investigation (Harvard Pilgrim Health Care, Kaiser Permanente Northern California, Kaiser Permanente Northwest, Kaiser Permanente Southern California, and Kaiser Permanente Georgia). In 2010, 1.9 million children under 18 had insurance coverage through these centers; over 90% of child members were employer-sponsored; less than 10% were sponsored by Medicaid.
All study subjects were aged <18 years in 2010 and enrolled in one of the 5 health plans for at least 10 months in 2010 and at least one month in 2009. We required medical, behavioral, and pharmacy coverage for more complete capture of data on utilization. We excluded children with institutional stays exceeding 30 days in 2010, in order to study community-based treatment. Children were included in the ASD cohort if they received at least one ASD diagnosis (ICD-9 code 299.0, 299.8, or 299.9) in 2009 and one additional ASD diagnosis in 2009 or 2010, ensuring that diagnosis preceded our observation of utilization. Chart reviews by our team (Coleman et al., 2015) and others (Burke et al., 2014) have determined that the presence of 2+ ASD diagnoses in administrative data is highly predictive of a valid case. A single ASD diagnosis from an autism specialty clinic within Kaiser Permanente Northern California (Coleman et al., 2015; Croen et al., 2006; Cummings et al., 2016) (where multidisciplinary assessments based on ADOS (Lord et al., 2000) and clinical interviews based on ADI-R (Le Couteur et al., 1989) are conducted) also sufficed to define a case. Children were eligible for the matched cohort with no ASD if they had a corresponding minimum number of health system contacts (1 in 2009, 1 additional in 2009-2010) and no ASD diagnosis in either year. We matched no-ASD to ASD children 10:1 on age, sex, and 2009 enrollment duration. The final study population included 7,901 children with ASD and 79,010 without ASD.
Study Measures
Age, sex, and enrollment information came from administrative files; data on diagnoses and utilization came from claims and electronic medical record extracts. We linked US census data to members' residential addresses to create neighborhood-level measures of educational attainment (proportion of adults in the neighborhood having attended some college) and household income (neighborhood median). The interval thresholds for these measures were approximate quartile values for the combined cohorts.
Children with ASD were categorized as ever diagnosed with Autistic Disorder [299.0, possibly (Lord et al., 2012) representing more severe cases] in 2009-2010 or only ever diagnosed with Asperger's (299.8) or Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS, 299.9). We disregarded the specialty of diagnosing providers because data on provider specialty are incomplete. For all subjects, we determined whether a diagnosis was ever received in 2009-2010 in the following psychiatric illness groupings: depression; anxiety; ADHD; bipolar disorder; schizophrenia or other psychoses; disruptive disorders; and, other psychiatric signs/symptoms (e.g., tics). We calculated 2010 utilization counts for outpatient visits, mental health specialist visits, emergency department visits, and all hospitalizations. Diagnosis and service codes are available in an appendix.
From pharmacy claims data, psychotropic medications dispensed in 2010 were identified by generic name (see appendix) and categorized into the following therapeutic classes by consensus among MHRN investigators: stimulants; other medications typically used to treat ADHD (alpha-agonists and atomoxetine); antipsychotics (first and second generation), antidepressants, anti-anxiety medications, anticonvulsants, lithium, benzodiazepines, and hypnotics. Data on prescription indication were not available; use was presumed to be psychiatric in nature, even though many study medications have multiple indications (e.g., anticonvulsants are used to treat mood disorders and epilepsy). Person-level medication utilization measures included any use (i.e., ever dispensed in the study year) and, to describe the overall intensity and constancy of use: the total number of major classes dispensed and total months of medication supplied.
Statistical Analyses
We examined characteristics of the ASD and non-ASD cohorts, and compared their neighborhood measures, psychiatric comorbidities, and service utilization. By therapeutic class, we compared the probability of any use of psychotropic medications in 2010 between children with and without ASD using multivariate logistic regression, controlling for neighborhood measures, age, sex, and health system site. We calculated the average months supplied by therapeutic class, contrasting results among users with and without ASD. We then compared the odds of medication use within strata defined by the presence of other specific common psychiatric conditions (e.g., antidepressant use among children with a formal diagnosis of depression and ASD versus children with depression and no ASD). For the four most prevalent and regularly used medication classes, we examined prevalence among children with ASD by age group and sex, contrasting results with those for similar children with no ASD.
Next, we determined the predictors of any psychotropic medication use among children with ASD, using multivariate logistic regression models that included age group, sex, neighborhood education and income, ASD diagnosis type, and selected psychiatric comorbidities, controlling for health system site.
Because ASD is usually diagnosed at a young age and may be treated with therapies beyond the medical setting or not at all, we expected that many children with history of ASD might have no ASD diagnosis recorded in 2009-2010. Although many of these children would likely still represent valid cases in 2010, they were nonetheless excluded from our main ASD cohort which required recent diagnoses to better ensure validity. In sensitivity analyses, we used longer-view cohorts (ASD and non-ASD) that considered ASD diagnoses received as far back as the year 2000 (see appendix).
Results
Characteristics of the Study Cohorts
Age and sex were distributed identically in the two cohorts because of the matched 10:1 design (Table 1). Each cohort was 82.3% male, reflecting the known higher prevalence of ASD among males.(Developmental, 2014) Children with ASD were somewhat more likely than peers without ASD to reside in neighborhoods with higher socioeconomic status.
Table 1. Characteristics of Study Cohorts of Children with and without ASD.
| Characteristic | ASD | no ASD | p-value |
|---|---|---|---|
|
| |||
| N=7,901 | N=79,010 | ||
| Age -- in January 2010 (%) | |||
| 1-2 years | 0.5 | 0.5 | -- |
| 3-4 years | 10.2 | 10.2 | |
| 5-7 years | 22.6 | 22.6 | |
| 8-11 years | 29.1 | 29.1 | |
| 12-14 years | 21.1 | 21.1 | |
| 15-17 years | 16.6 | 16.6 | |
|
| |||
| Male sex (%) | 82.3 | 82.3 | -- |
|
| |||
| Neighborhood SES: adults with any college (%) | |||
| 0% - 43% | 22.8 | 26.1 | <0.0001 |
| 44% - 58% | 23.5 | 24.4 | |
| 59% - 72% | 26.8 | 25.5 | |
| 73% + | 26.4 | 23.5 | |
|
| |||
| Neighborhood SES: median household income (%) | |||
| $0 - $44,000 | 21.3 | 24.5 | <0.0001 |
| $45,000 - $59,000 | 24.6 | 25.5 | |
| $60,000 - $77,000 | 26.3 | 25.1 | |
| $78,000 + | 27.2 | 24.3 | |
|
| |||
| Other psychiatric diagnosis -- in 2009-10 (%) | |||
| ADD/ADHD | 31.8 | 6.9 | <0.0001 |
| anxiety | 16.7 | 3.1 | <0.0001 |
| disruptive disorders | 13.4 | 2.4 | <0.0001 |
| depression | 7.6 | 3.1 | <0.0001 |
| intellectual disabilities | 5.6 | 0.1 | <0.0001 |
| other psychiatric signs/symptoms* | 3.3 | 0.5 | <0.0001 |
| bipolar disorder | 2.7 | 0.2 | <0.0001 |
| schizophrenia/psychoses | 1.3 | 0.1 | <0.0001 |
| any non-ASD psychiatric dx | 73.2 | 17.2 | <0.0001 |
|
| |||
| Service utilization -- in 2010 | |||
| outpatient visits, any (%) | 95.7 | 87.8 | <0.0001 |
| (mean no. of outpt visits) | (9.2) | (3.5) | <0 .0001 |
| MH outpatient visits, any (%) | 51.6 | 8.7 | <0.0001 |
| (mean no. of MH outpt visits) | (3.7) | (0.48) | <0 .0001 |
| ED visits, any (%) | 13.4 | 11.8 | <0.001 |
| Hospitalizations, any (%) | 2.6 | 0.9 | <0.0001 |
| Non-psychiatric Rx, any (%) | 63.7 | 58.7 | <0.0001 |
Notes: Other psychiatric signs/symptoms included tics, Tourette's, enuresis, encopresis, and trichotillomania. Hospitalizations included both medical and psychiatric hospitalizations. P-values presented are from Chi-squared tests for percentage differences and Student's T tests for differences in means.
Most children with ASD (71.8%) received at least one diagnosis of Autistic Disorder (299.0); 28.2% received only diagnoses of Asperger's or PDD-NOS. Nearly three quarters (73.2%) of children with ASD also received at least one other psychiatric diagnosis. The most common psychiatric comorbidities among children with ASD were attention disorders (31.8%), followed by anxiety (16.7%), disruptive disorders (13.4%), and depression (7.6%). Separate analyses (see Table 4 notes) determined that the prevalence of each psychiatric comorbidity of interest was higher among children who had only Asperger's or PDD-NOS diagnoses than among those diagnosed with Autistic Disorder.
Table 4. Predictors of Any Psychotropic Medication Use among Children with ASD in 2010.
| Characteristic | Adjusted O.R. from Multivariate Logistic Regression (95% c.i.) |
|---|---|
| Age | |
| 1-4 years | 0.32 (0.20, 0.52) |
| 5-11 years (ref) | -- |
| 12-17 years | 2.42 (2.10, 2.78) |
|
| |
| Sex | |
| Male (ref) | -- |
| Female | 0.99 (0.83, 1.18) |
|
| |
| Neighborhood SES: | |
| adults with any college | |
| 0%-<=43% | 0.90 (0.70, 1.16) |
| 44%-<=58% | 1.03 (0.83, 1.28) |
| 59%-<=72% | 1.09 (0.90, 1.32) |
| >72% (ref) | -- |
|
| |
| Neighborhood SES: | |
| median household income | |
| $0-<=$44,000 | 0.86 (0.67, 1.11) |
| $45,000-<=$59,000 | 0.87 (0.70, 1.08) |
| $60,000-<=$77,000 | 1.06 (0.88, 1.29) |
| >$77,000 (ref) | -- |
|
| |
| ASD dx type | |
| Autistic Disorder (ref) | -- |
| Asperger's/PDD-NOS only | 0.80 (0.69, 0.93) |
|
| |
| Other psychiatric diagnoses | |
| No ADHD, depr, or anx (ref) | -- |
| ADHD only | 13.63 (11.52, 16.14) |
| Depr or anx only | 3.97 (3.31, 4.77) |
| Both depr/anx and ADHD | 21.19 (16.39, 27.40) |
Notes: ASD cohort N=7,901. This logistic regression model also controlled for health system site.
When psychiatric comorbidities were not included in the model, the relationship between Aspergers's/PDD-NOS and psychotropic use was reversed (OR 1.43; 95% CI 1.28-1.60); the prevalence of psychiatric comorbidities was consistently higher among children with only Aspergers's/PDD-NOS versus those with autistic disorder (e.g., depression 16.1% vs 4.3%, anxiety 29.1% vs 11.9%, ADHD 51.3% vs 24.1%, and disruptive disorders 18.1% vs 11.5%). Other predictors were robust across sensitivity analyses (not shown).
All psychiatric comorbidities of interest were far more likely to be noted in children with ASD than among those without ASD: for example, depression was 2.5 times as common among ASD children; bipolar disorder, schizophrenia, and other psychoses were roughly 11 to 12 times more common. In addition, children with ASD were more likely to utilize mental health services: more than half of ASD children (51.6%) visited a mental health professional, as compared to 8.7% of children without ASD. Compared to peers, children with ASD also received more health services overall (e.g., outpatient and all hospital) and more non-psychotropic medications (Table 1).
Prevalence and Intensity of Medication Use by Psychotropic Class
Nearly half (48.5%) of all children with ASD took psychotropic medications (Table 2). Among children diagnosed with ASD, the most prevalent psychotropic treatments were medications that typically target ADHD (30.2% of the cohort, combining stimulants and non-stimulant ADHD therapies), antipsychotics (20.5%), antidepressants (17.8%), and mood stabilizers (9.1%, combining anticonvulsants and lithium). Use of benzodiazepines (4.3%), other anxiolytics (3.0%), and hypnotics (0.02%) was relatively rare. Among the ADHD medications, methylphenidate, amphetamine salts, and clonidine were the most frequently dispensed to children with ASD; risperidone and aripiprazole led among antipsychotics, and fluoxetine was the most frequent antidepressant. Other specific drug entities each represented less than 5% of total psychotropic prescription fills for the ASD cohort (details in appendix).
Table 2. Prevalence Psychotropic Medication Use and Average Months Supplied by Therapeutic Class, for Children with and without ASD in 2010.
| Therapeutic Class | Percentage receiving any medication in class | Difference in Likelihood of Any Use in Year, ASD vs no ASD | Average months supplied per user per year | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Children with ASD (n=7,901) | Children with no ASD (n=79,010) | Adjusted OR (95% c.i.) | P-value | Children with ASD and any use | Children with no ASD and any use | |
|
| ||||||
| All psychiatric medications | 48.47 | 7.7 | 11.44 (10.02,13.06) | <0.0001 | 18.3 | 9.3 |
|
| ||||||
| All ADHD medications | 30.24 | 5.13 | 8.44 (7.61, 9.37) | <0.0001 | 12.3 | 9.9 |
| S timulants | 22.73 | 4 .7 6 | 6.12 (5.51, 6.81) | <0 .0001 | 11.5 | 9.4 |
| Other ADHD* | 12.35 | 0 .8 4 | 17.53 (15.42,19.93) | <0 .0001 | 9.0 | 7.1 |
| Antipsychotics | 20.50 | 0.64 | 40.50 (35.25,46.53) | <0.0001 | 10.5 | 7.2 |
| 2nd generation | 20.30 | 0 .6 0 | 42.58 (36.99,49.01) | <0 .0001 | 10.4 | 7.4 |
| 1st generation | 0 .3 9 | 0 .0 4 | 9.55 (5.85,15.60) | <0 .0001 | 7.3 | 2.3 |
| Antidepressants | 17.83 | 1.42 | 13.65 (11.88,15.69) | <0.0001 | 9.5 | 6.7 |
| All mood stabilizers | 9.07 | 0.55 | 17.20 (14.77, 20.02) | <0.0001 | 11.7 | 9.3 |
| Anticonvulsants | 8 .7 2 | 0 .5 3 | 17.07 (14.67,19.88) | <0 .0001 | 11.5 | 9.1 |
| Lithium | 0 .5 8 | 0 .0 3 | 19.80 (12.24,32.02) | <0 .0001 | 9.5 | 10.4 |
| Benzodiazepines | 4.30 | 0.48 | 8.96 (7.68,10.46) | <0.0001 | 2.8 | 1.6 |
| Anti-anxiety medications | 3.00 | 1.16 | 2.62 (2.22, 3.10) | <0.0001 | 3.3 | 1.1 |
| Hypnotics | 0.20 | 0.02 | (nonconvergent) | -- | 2.9 | 1.6 |
Notes: ASD cohort N=7,901; no-ASD cohort N=79,010.
Medication months supplied are added across all dispensings in class.
Other ADHD medications included alpha-2 adrenergic agonists and norepinephrine reuptake inhibitors (see appendix).
Logistic regression models controlled for SES (neighborhood education attainment and median household income quartile), age, sex, & health system site.
Children with ASD were far more likely to use any psychotropic medication as compared to matched peers without ASD (Table 2; overall adjusted OR=11.4; 95% CI=10.0-13.1). Moreover, medication use was more prevalent among children with ASD within every therapeutic class of interest. The largest difference between cohorts was for antipsychotics (OR=40.5; 95% CI=35.3-46.5).
Total months of medication supplied among users in the year was highest in both cohorts for the four most prevalent broad classes: ADHD therapies, antipsychotics, antidepressants, and mood stabilizers (Table 2). On average, children with ASD who received medications in these classes received at least 9 months of supply. By contrast, months supplied per user were markedly lower for benzodiazepines, other anxiolytics, and hypnotics (range: 2.8 to 3.3 months in the ASD cohort). Except for lithium, users without ASD diagnoses received fewer months' supply of medication (Table 2).
Figure 1 contrasts the two cohorts in terms of the unadjusted prevalence of use in the four major psychotropic classes and the percentage of each cohort using one, two, three to four, or none of these classes. Children with ASD were more than seven times as likely to use any medication in the major classes and more than 21 times as likely to use two or more among the major classes.
Figure 1. Prevalence of Use of Psychotropic Medication among Children with and without ASD in 2010, by (A) Major Therapeutic Class and (B) Total Number of Major Classes.
Notes: ASD cohort N=7,901; no-ASD cohort N=79,010.
Medication Use and Presence of Other Psychiatric Diagnoses
In Table 3, for selected therapeutic classes, we present the prevalence of use among cohort subgroups defined by the presence of specific psychiatric diagnoses other than ASD, comparing the likelihood of use between children with and without ASD. As expected, for all children, the presence of another psychiatric diagnosis was associated with higher prevalence of the relevant treatment. Within each psychiatric comorbidity stratum, the odds of medication use were consistently higher among children with ASD than comparison children. Moreover, in the absence of other relevant recorded diagnoses, psychotropic treatments were rare among children without ASD and common among children with ASD. For example, 0.3% of children who had neither ASD nor ADHD diagnosis received an ADHD-associated medication, whereas 10.4% of children with ASD but no ADHD diagnosis received such medications; results for antipsychotics and antidepressants were similar. Where ASD was present without a comorbid psychiatric diagnosis, the psychotropic prescribing observed may have targeted ASD core symptoms, ASD associated symptoms (e.g., hyperactivity, irritability), and/or omitted psychiatric comorbidities (e.g., provider did not record diagnosis, diagnosis received outside of system in a nonreimbursed visit, comorbidity was not among those included in analysis).
Table 3. Prevalence of Medication Use in Selected Therapeutic Classes among Children with and without ASD, by the Presence of Other Psychiatric Diagnoses, in 2010.
| Medication Therapeutic Class | Percentage of full cohort in defined subgroup | Percentage in subgroup receiving medications | Difference in likelihood of use, ASD vs no ASD | |||
|---|---|---|---|---|---|---|
| Subgroup, defined by presence of other psychiatric diagnoses | Children with ASD (n=7,901) | Children with no ASD (n=79,010) | Children with ASD | Children with no ASD | Adjusted O.R. Estimate (95% c.i.) | p-value |
| Stimulants and other ADHD medications | ||||||
| with ADHD dx | 31.8 | 6.9 | 72.9 | 70.1 |
1.19 (1.07, 1.34) |
0.0023 |
| no ADHD dx | 68.2 | 93.1 | 10.4 | 0.3 |
37.93 (30.86, 46.61) |
<0.0001 |
| Antipsychotics | ||||||
| with psychosis dx only | 2.1 | 0.2 | 72.6 | 48.2 |
2.99 (1.78, 5.02) |
<0.0001 |
| with disruptive dx only | 11.9 | 2.3 | 45.1 | 8.9 |
8.81 (7.12, 10.90) |
<0.0001 |
| with psychosis dx or disruptive dx | 15.5 | 2.6 | 53.0 | 13.7 |
7.07 (5.97, 8.38) |
<0.0001 |
| no psychosis or disruptive dx | 84.5 | 97.4 | 14.5 | 0.3 |
59.40 (49.75, 70.92) |
<0.0001 |
| Antidepressants | ||||||
| with depression dx only | 3.9 | 2.2 | 40.2 | 15.8 |
5.10 (3.95, 6.59) |
<0.0001 |
| with anxiety dx only | 13.0 | 2.2 | 46.8 | 13.8 |
5.20 (4.32, 6.26) |
<0.0001 |
| with depression or anxiety dx | 20.6 | 5.3 | 51.3 | 19.8 |
4.33 (3.73, 5.02) |
<0.0001 |
| no depression or anxiety dx | 79.4 | 94.7 | 9.1 | 0.4 |
24.31 (20.74, 28.49) |
<0.0001 |
Notes: For simplicity, each of the 3 sets of analyses above considered only the listed diagnoses (detailed ICD-9 codes in appendix); e.g., we disregarded depression diagnoses in the analyses of antipsychotics use.
Logistic regression models controlled for SES (neighborhood education attainment and median household income quartile), age, sex, & health system site. For these stratified analyses, at least one match was required for inclusion in either the ASD or no-ASD group; unmatched subjects were dropped from analysis; sensitivity analyses (not shown) with no such exclusion yielded similar results.
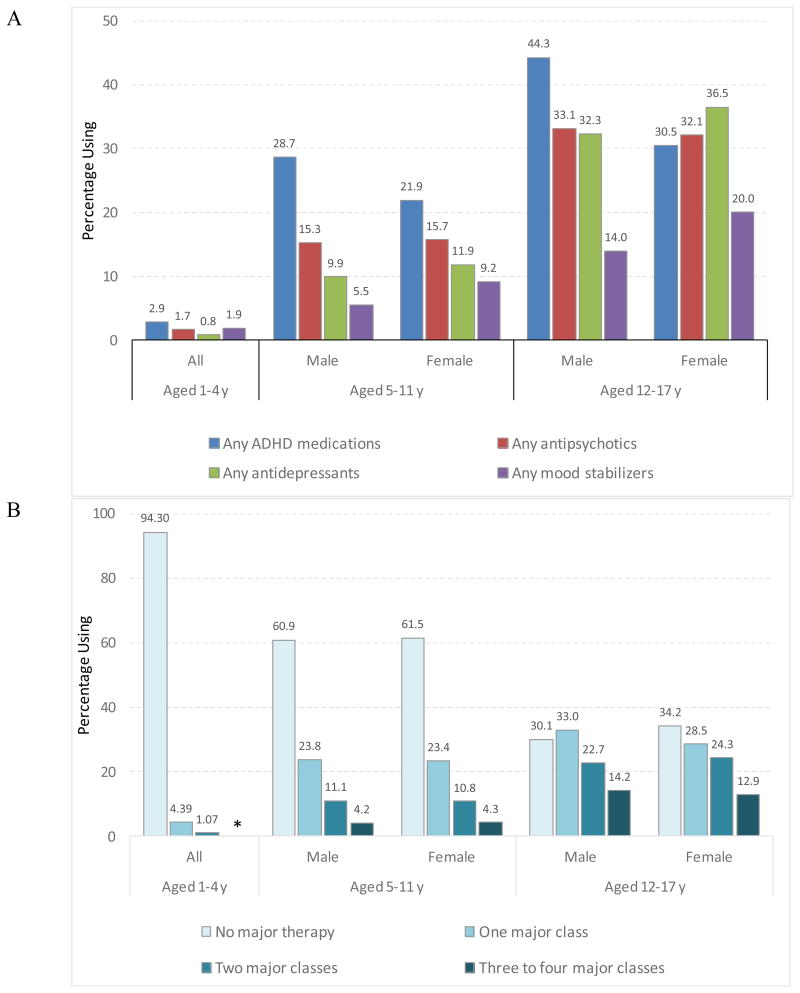
Use of Psychotropics by Age and Sex
Figure 2 presents data on use of the four major psychotropic classes for children with ASD by age group and sex. Psychotropics use was fairly rare among pre-school children with ASD (5.7%), and far higher among school-aged children (39.0%) and adolescents (59.1%). Although the percentage receiving any medication was similar among boys and girls, analyses by therapeutic class revealed that boys with ASD were far more likely than girls to be treated with ADHD medications (e.g., 44.3% vs 30.5% among adolescents), while girls were more likely than boys to take antidepressants or mood stabilizers (36.5% vs 32.3%, and 20.0% vs 14.0%, respectively). These sex differences by therapeutic class resembled differences observed among children without ASD (see appendix).
Figure 2. Prevalence of Use of Psychotropic Medication among Children with ASD in 2010, Comparing Age and Sex Groups, by (A) Major Therapeutic Class and (B) Number of Major Classes.
Notes: ASD cohort N=7,901.
*small cell count, <6 individuals.
Predictors of Use among Children with ASD
Multivariate analyses confirmed that, among children diagnosed with ASD, older age, a diagnosis of Autistic Disorder (299.0), and comorbid diagnosis of either depression or anxiety, or an attention disorder, were all significant positive independent predictors of any psychotropic medication use (Table 4). Sex and socioeconomic measures, on the other hand, were not statistically significant predictors in this fully-insured population.
Sensitivity Analyses Considering Pre-2009 ASD Diagnoses
When we allowed a more flexible period (2000-2010) for ASD diagnosis and case assignment, we identified an additional 4,732 ASD cases, including 771 children who served as controls in our main analyses. Results from sensitivity analyses using the longer-view cohorts were all similar to those from our main analyses and statistically significant, although differences between children with and without ASD were attenuated (see appendix).
Discussion
Using recent data from a very large insured pediatric population, we quantified psychotropic medication utilization among children with autism spectrum disorder. Just under half (48.5%) of all children with active ASD diagnoses were treated with psychotropic medications at some time in the study year. This overall prevalence was somewhat lower than that seen in earlier large studies of Medicaid and privately-insured children (Mandell et al., 2008; Oswald & Sonenklar, 2007) and somewhat higher than in a large parent survey (Rosenberg et al., 2010). Medications typically prescribed for attention disorders were the most commonly used in our study population, as in the parent survey (Rosenberg et al., 2010), whereas antipsychotics (Mandell et al., 2008) and antidepressants (Aman et al., 2003; Esbensen et al., 2009; Oswald & Sonenklar, 2007) led in other reports. The close associations we found between use and older age, and between use and the presence of comorbid psychiatric diagnoses, were consistent with earlier findings.
We carefully matched each ASD case to 10 children without ASD to provide context for our results and included a more thorough exploration of the roles of comorbidity and sex. On the whole, children with ASD were 11.4 times more likely to be treated with psychotropics as compared to non-ASD peers. When other psychiatric diagnoses were present in the record, children with ASD were consistently more likely than peers to receive psychotropics. Furthermore, in the absence of relevant comorbidity diagnoses, children with ASD had far higher rates of use than peers; children with neither ASD nor these specific comorbidities rarely received psychotropics. Nevertheless, several observations for children with ASD corresponded to our findings for peers without ASD. For example, in both cohorts, there was a strong positive relationship between use and age, much higher use of stimulants and other ADHD-related treatments among boys, and higher use of antidepressants and mood stabilizers among girls. These findings are consonant with previous research on sex differences in psychiatric epidemiology,(Biederman et al., 2002; Cohen et al., 1993; Kessler, Avenevoli, & Ries Merikangas, 2001) though little has been published regarding psychiatric comorbidities or phenotypes by sex specifically among children with ASD,(Hartley & Sikora, 2009; Solomon, Miller, Taylor, Hinshaw, & Carter, 2012) and studies of sex differences in child psychiatry frequently cite concerns about the possible role of referral bias.
As noted here and elsewhere (Esbensen et al., 2009; Logan et al., 2012; Mandell et al., 2008; Oswald & Sonenklar, 2007; Rosenberg et al., 2010), psychotropic medications use is extensive among children with ASD. Over a third of our adolescent cases received medications in multiple classes. Moreover, our unique data on months of medication supplied suggest that the extent of polypharmacy cannot be explained by serial trials of alternative medications; the average user was dispensed close to 12 months' worth of medication per class per year, suggesting widespread long-term use.
According to recent reviews of psychotropic treatments in youth with ASD (Dove et al., 2012; McPheeters et al., 2011; Siegel & Beaulieu, 2012), the most consistent evidence of efficacy has been shown for the antipsychotic medications risperidone and aripiprazole, which, while not effective for the core features of ASD (social and communication impairment), may reduce associated irritability, repetitive behavior, and hyperactivity. However, important adverse effects associated with antipsychotics, including weight gain, sedation, and extrapyramidal symptoms, have led to the recommendation that their use be reserved for patients with severe impairments or risk of injury (American Academy of Child and Adolescent Psychiatry, 2011; McPheeters et al., 2011). Evidence for the use of antidepressants, ADHD treatments, and mood stabilizers in children with ASD is mixed or lacking. In addition, despite the accelerating pace of ASD effectiveness research (Siegel & Beaulieu, 2012), there are almost no data on the benefits and harms of longer-term medication use or concurrent use of multiple classes, or on the effectiveness of psychotropics among the older children for whom use is most prevalent (Dove et al., 2012). Psychotropics use was fairly rare among children under 5, consonant with the complete lack of controlled trials in that age group.
Use of psychotropics in ASD is strongly associated with having a comorbid psychiatric diagnosis, and these diagnoses were common among our ASD cohort. Although the levels of comorbidity that we identified are consistent with published prevalence reports elsewhere (Costello, Egger, & Angold, 2005; Mazzone, Ruta, & Reale, 2012; Simonoff et al., 2008), our methods did not permit validation of these companion diagnoses. Some providers may enter diagnosis codes to indicate the presence of symptoms without a definitive separate diagnosis. Other authors have noted the lack of consensus on accepted practice for establishing co-occurring psychopathology in ASD populations (Siegel & Beaulieu, 2012), and have suggested that impaired emotional regulation, which may be an inherent feature of ASD, means that the true prevalence of co-occurring psychopathology is likely overestimated (Mazefsky et al., 2013). External pressures may also influence providers' decision to formally record comorbid psychiatric diagnoses. For example, the DSM-IV(American Psychiatric Association. & American Psychiatric Association. Task Force on DSM-IV., 2000), effective until 2013, strongly discouraged the simultaneous diagnosis of ASD and ADHD. Conversely, providers may be reluctant to prescribe without an FDA-approved indication, especially in the case of stimulants, which are controlled substances (Harstad, Levy, & Committee on Substance, 2014). Our data also underestimate psychiatric visits and diagnoses (but not medication use) if members saw psychiatrists outside their health system and paid entirely out-of-pocket. A national shortage of child psychiatrists, along with longer appointment wait times and lower insurance acceptance rates for this specialty, contribute to the phenomenon of outside self-paid utilization.(Bishop, Press, Keyhani, & Pincus, 2014; Glasser, 2010; Pletcher et al., 2010; Thomas & Holzer, 2006)
Given the very large size of our study population, and the lack of strong evidence in the published literature for the use of psychotropics to treat ASD in children, we could neither review cases individually nor determine the appropriateness of the medication use we observed. Widespread use of psychotropics points to the need for additional research on drug treatment for core ASD symptoms and for associated symptoms which may appear similar to other psychopathologies among non-ASD populations. In addition, re-evaluation of patients' need for medication continuation should be conducted routinely on a case-by-case basis by qualified clinicians. Clinicians, policymakers, and future studies must investigate whether families have adequate access to non-drug therapies and services, including behavioral approaches (Peters-Scheffer, Didden, Korzilius, & Sturmey, 2011) that may be effective in improving the function and well-being of children with ASD.
Our study limitations include inadequate data on severity of impairment. Although we identified the subset of ASD cases diagnosed specifically with Autistic Disorder, the validity of the distinction among different ICD-9 codes for ASD in our data is not known (Lord et al., 2012), and new ASD diagnostic procedures promulgated by the American Psychiatric Association in 2013 (American Psychiatric Association, 2013) may render our attempts to distinguish among these codes outdated. As noted above, the validity of our comorbidity codes is also uncertain, particularly for children with ASD. Other than diagnoses, our data included no information on signs or symptoms that may have been noted and targeted by prescribers.
This study captured dispensing of covered medications, not actual use. Further, dispensing data do not include information on indication, and several medicines targeted in our study have additional uses beyond the therapeutic category we have assigned them. To this extent, our results may both misclassify medications among psychiatric therapeutic categories and overestimate the overall rate of drug treatment that is “psychiatric.” Most prominently, anticonvulsants are mood stabilizers that are also used to treat seizure disorders,(Canitano, 2015) for which children with ASD are at higher risk (estimated at about 25% versus 2-3% among children in general(Canitano, 2007)). In our sample, 9.4% of children with ASD had 1 or more diagnosis code for epilepsy in 2009-10, versus 1.0% of children without ASD.
Our population included children enrolled in one of 5 insurance systems on the East and West coasts of the US, and the vast majority were privately insured. Furthermore, all subjects had clinical contact during the study period. Our findings may not be generalizable to other pediatric populations.
Conclusion
Our research demonstrates that psychotropic medications are used extensively and intensively among children with recently recorded ASD diagnoses in large health systems. There is currently a lack of strong published evidence to support the effectiveness and safety of the levels of use we observed; more research in this area is clearly necessary. In addition, population-based studies to understand the drivers behind the decision to medicate, the quality of follow-up care, and the availability of effective non-drug alternatives are merited.
Supplementary Material
Acknowledgments
This study was funded by the National Institutes of Health (grant U19MH092201X).
All phases of this study were supported by a grant from NIH, U19MH092201 (PI: Simon). The authors are grateful to Fang Zhang, PhD (Harvard Medical School and Harvard Pilgrim Health Care Institute, Boston) for statistical advice and Gregory E. Simon, MD, MPH (Group Health Research Institute, Seattle), Stephen B. Soumerai, ScD (HMS/HPHCI), and Elizabeth B. Caronna, MD (Harvard Vanguard Medical Associates, Developmental and Behavioral Pediatrics, Boston) for critical reading and content advice.
Footnotes
Conflict of interest: All authors declare that they have no conflicts of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of the Harvard Pilgrim Health Care Institute and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Human Subjects Committee of Harvard Pilgrim Health Care determined that our study met the regulatory requirements necessary in order to waive informed consent. This article does not contain any studies with animals performed by any of the authors.
References
- Ahmedani BK, Simon GE, Stewart C, Beck A, Waitzfelder BE, Rossom R, Solberg LI. Health care contacts in the year before suicide death. J Gen Intern Med. 2014;29(6):870–877. doi: 10.1007/s11606-014-2767-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aman MG, Lam KS, Collier-Crespin A. Prevalence and patterns of use of psychoactive medicines among individuals with autism in the Autism Society of Ohio. J Autism Dev Disord. 2003;33(5):527–534. doi: 10.1023/a:1025883612879. [DOI] [PubMed] [Google Scholar]
- American Academy of Child and Adolescent Psychiatry Practice Parameter for the Use of Atypical Antipsychotic Medications in Children and Adolescents. 2011 Retrieved from 3615 Wisconsin Ave., NW, Washington, D.C. 200016: https://www.aacap.org/App_Themes/AACAP/docs/practice_parameters/Atypical_Antipsychotic_Medications_Web.pdf.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, (DSM-5®) American Psychiatric Association; 2013. [Google Scholar]
- American Psychiatric Association & American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-IV-TR. 4. Washington, DC: American Psychiatric Association; 2000. Task Force on DSM-IV. [Google Scholar]
- Biederman J, Mick E, Faraone SV, Braaten E, Doyle A, Spencer T, Johnson MA. Influence of gender on attention deficit hyperactivity disorder in children referred to a psychiatric clinic. Am J Psychiatry. 2002;159(1):36–42. doi: 10.1176/appi.ajp.159.1.36. [DOI] [PubMed] [Google Scholar]
- Bishop TF, Press MJ, Keyhani S, Pincus HA. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176–181. doi: 10.1001/jamapsychiatry.2013.2862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JP, Jain A, Yang W, Kelly JP, Kaiser M, Becker L, Newschaffer CJ. Does a claims diagnosis of autism mean a true case? Autism. 2014;18(3):321–330. doi: 10.1177/1362361312467709. [DOI] [PubMed] [Google Scholar]
- Canitano R. Epilepsy in autism spectrum disorders. Eur Child Adolesc Psychiatry. 2007;16(1):61–66. doi: 10.1007/s00787-006-0563-2. [DOI] [PubMed] [Google Scholar]
- Canitano R. Mood Stabilizers in Children and Adolescents With Autism Spectrum Disorders. Clin Neuropharmacol. 2015;38(5):177–182. doi: 10.1097/WNF.0000000000000096. [DOI] [PubMed] [Google Scholar]
- Cohen P, Cohen J, Kasen S, Velez CN, Hartmark C, Johnson J, Streuning EL. An epidemiological study of disorders in late childhood and adolescence--I. Age- and gender-specific prevalence. J Child Psychol Psychiatry. 1993;34(6):851–867. doi: 10.1111/j.1469-7610.1993.tb01094.x. [DOI] [PubMed] [Google Scholar]
- Coleman KJ, Lutsky MA, Yau V, Qian Y, Pomichowski ME, Crawford PM, Croen LA. Validation of Autism Spectrum Disorder Diagnoses in Large Healthcare Systems with Electronic Medical Records. J Autism Dev Disord. 2015 doi: 10.1007/s10803-015-2358-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Egger H, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005;44(10):972–986. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- Croen LA, Najjar DV, Ray GT, Lotspeich L, Bernal P. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics. 2006;118(4):e1203–1211. doi: 10.1542/peds.2006-0127. [DOI] [PubMed] [Google Scholar]
- Cummings JR, Lynch FL, Rust KC, Coleman KJ, Madden JM, Owen-Smith AA, Croen LA. Health Services Utilization Among Children With and Without Autism Spectrum Disorders. J Autism Dev Disord. 2016;46(3):910–920. doi: 10.1007/s10803-015-2634-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson G. Dramatic increase in autism prevalence parallels explosion of research into its biology and causes. JAMA Psychiatry. 2013;70(1):9–10. doi: 10.1001/jamapsychiatry.2013.488. [DOI] [PubMed] [Google Scholar]
- Developmental DMNSY. Principal Investigators. (2014). Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveill Summ. 2010;63(2):1–21. [PubMed] [Google Scholar]
- Dove D, Warren Z, McPheeters ML, Taylor JL, Sathe NA, Veenstra-VanderWeele J. Medications for adolescents and young adults with autism spectrum disorders: a systematic review. Pediatrics. 2012;130(4):717–726. doi: 10.1542/peds.2012-0683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esbensen AJ, Greenberg JS, Seltzer MM, Aman MG. A longitudinal investigation of psychotropic and non-psychotropic medication use among adolescents and adults with autism spectrum disorders. J Autism Dev Disord. 2009;39(9):1339–1349. doi: 10.1007/s10803-009-0750-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasser M. The history of managed care and the role of the child and adolescent psychiatrist. Child Adolesc Psychiatr Clin N Am. 2010;19(1):63–74. doi: 10.1016/j.chc.2009.08.009. table of contents. [DOI] [PubMed] [Google Scholar]
- Harstad E, Levy S, Committee on Substance, A Attention-deficit/hyperactivity disorder and substance abuse. Pediatrics. 2014;134(1):e293–301. doi: 10.1542/peds.2014-0992. [DOI] [PubMed] [Google Scholar]
- Hartley SL, Sikora DM. Sex differences in autism spectrum disorder: an examination of developmental functioning, autistic symptoms, and coexisting behavior problems in toddlers. J Autism Dev Disord. 2009;39(12):1715–1722. doi: 10.1007/s10803-009-0810-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson CP, Myers SM. Identification and evaluation of children with autism spectrum disorders. Pediatrics. 2007;120(5):1183–1215. doi: 10.1542/peds.2007-2361. [DOI] [PubMed] [Google Scholar]
- Karst JS, Van Hecke AV. Parent and family impact of autism spectrum disorders: a review and proposed model for intervention evaluation. Clin Child Fam Psychol Rev. 2012;15(3):247–277. doi: 10.1007/s10567-012-0119-6. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Ries Merikangas K. Mood disorders in children and adolescents: an epidemiologic perspective. Biol Psychiatry. 2001;49(12):1002–1014. doi: 10.1016/s0006-3223(01)01129-5. [DOI] [PubMed] [Google Scholar]
- Le Couteur A, Rutter M, Lord C, Rios P, Robertson S, Holdgrafer M, McLennan J. Autism diagnostic interview: a standardized investigator-based instrument. J Autism Dev Disord. 1989;19(3):363–387. doi: 10.1007/BF02212936. [DOI] [PubMed] [Google Scholar]
- Logan SL, Nicholas JS, Carpenter LA, King LB, Garrett-Mayer E, Charles JM. High prescription drug use and associated costs among Medicaid-eligible children with autism spectrum disorders identified by a population-based surveillance network. Ann Epidemiol. 2012;22(1):1–8. doi: 10.1016/j.annepidem.2011.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Petkova E, Hus V, Gan W, Lu F, Martin DM, Risi S. A multisite study of the clinical diagnosis of different autism spectrum disorders. Arch Gen Psychiatry. 2012;69(3):306–313. doi: 10.1001/archgenpsychiatry.2011.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Jr, Leventhal BL, DiLavore PC, Rutter M. The autism diagnostic observation schedule-generic: a standard measure of social and communication deficits associated with the spectrum of autism. J Autism Dev Disord. 2000;30(3):205–223. [PubMed] [Google Scholar]
- Lu CY, Zhang F, Lakoma MD, Madden JM, Rusinak D, Penfold RB, Soumerai SB. Changes in antidepressant use by young people and suicidal behavior after FDA warnings and media coverage: quasi-experimental study. BMJ. 2014;348:g3596. doi: 10.1136/bmj.g3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell DS, Morales KH, Marcus SC, Stahmer AC, Doshi J, Polsky DE. Psychotropic medication use among Medicaid-enrolled children with autism spectrum disorders. Pediatrics. 2008;121(3):e441–448. doi: 10.1542/peds.2007-0984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matson JL, Kozlowski AM. The increasing prevalence of autism spectrum disorders. Research in Autism Spectrum Disorders. 2011;5.1:418–425. [Google Scholar]
- Mazefsky CA, Herrington J, Siegel M, Scarpa A, Maddox BB, Scahill L, White SW. The role of emotion regulation in autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2013;52(7):679–688. doi: 10.1016/j.jaac.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzone L, Ruta L, Reale L. Psychiatric comorbidities in asperger syndrome and high functioning autism: diagnostic challenges. Ann Gen Psychiatry. 2012;11(1):16. doi: 10.1186/1744-859x-11-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPheeters ML, Warren Z, Sathe N, Bruzek JL, Krishnaswami S, Jerome RN, Veenstra-Vanderweele J. A systematic review of medical treatments for children with autism spectrum disorders. Pediatrics. 2011;127(5):e1312–1321. doi: 10.1542/peds.2011-0427. [DOI] [PubMed] [Google Scholar]
- MHRN. Mental Health Research Network (website) Retrieved from www.mhresearchnetwork.org/
- Oswald DP, Sonenklar NA. Medication use among children with autism spectrum disorders. J Child Adolesc Psychopharmacol. 2007;17(3):348–355. doi: 10.1089/cap.2006.17303. [DOI] [PubMed] [Google Scholar]
- Penfold RB, Stewart C, Hunkeler EM, Madden JM, Cummings JR, Owen-Smith AA, Simon GE. Use of antipsychotic medications in pediatric populations: what do the data say? Curr Psychiatry Rep. 2013;15(12):426. doi: 10.1007/s11920-013-0426-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters-Scheffer N, Didden R, Korzilius H, Sturmey P. A meta-analytic study on the effectiveness of comprehensive ABA-based early intervention programs for children with autism spectrum disorders. Research in Autism Spectrum Disorders. 2011;5.1:60–69. [Google Scholar]
- Pletcher BA, Rimsza ME, Cull WL, Shipman SA, Shugerman RP, O'Connor KG. Primary care pediatricians' satisfaction with subspecialty care, perceived supply, and barriers to care. J Pediatr. 2010;156(6):1011–1015. doi: 10.1016/j.jpeds.2009.12.032. 1015 e1011. [DOI] [PubMed] [Google Scholar]
- Rosenberg RE, Mandell DS, Farmer JE, Law JK, Marvin AR, Law PA. Psychotropic medication use among children with autism spectrum disorders enrolled in a national registry, 2007-2008. J Autism Dev Disord. 2010;40(3):342–351. doi: 10.1007/s10803-009-0878-1. [DOI] [PubMed] [Google Scholar]
- Siegel M, Beaulieu AA. Psychotropic medications in children with autism spectrum disorders: a systematic review and synthesis for evidence-based practice. J Autism Dev Disord. 2012;42(8):1592–1605. doi: 10.1007/s10803-011-1399-2. [DOI] [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: prevalence, comorbidity, and associated factors in a population-derived sample. J Am Acad Child Adolesc Psychiatry. 2008;47(8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Solomon M, Miller M, Taylor SL, Hinshaw SP, Carter CS. Autism symptoms and internalizing psychopathology in girls and boys with autism spectrum disorders. J Autism Dev Disord. 2012;42(1):48–59. doi: 10.1007/s10803-011-1215-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas CR, Holzer CE., 3rd The continuing shortage of child and adolescent psychiatrists. J Am Acad Child Adolesc Psychiatry. 2006;45(9):1023–1031. doi: 10.1097/01.chi.0000225353.16831.5d. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.