Abstract
Georgia has the lowest kidney transplant rates in the United States and substantial racial disparities in transplantation. We determined the effectiveness of a multicomponent intervention to increase referral of patients on dialysis for transplant evaluation in the Reducing Disparities in Access to kidNey Transplantation Community Study (RaDIANT), a randomized, dialysis facility–based, controlled trial involving >9000 patients receiving dialysis from 134 dialysis facilities in Georgia. In December of 2013, we selected dialysis facilities with either low transplant referral or racial disparity in referral. The intervention consisted of transplant education and engagement activities targeting dialysis facility leadership, staff, and patients conducted from January to December of 2014. We examined the proportion of patients with prevalent ESRD in each facility referred for transplant within 1 year as the primary outcome, and disparity in the referral of black and white patients as a secondary outcome. Compared with control facilities, intervention facilities referred a higher proportion of patients for transplant at 12 months (adjusted mean difference [aMD], 7.3%; 95% confidence interval [95% CI], 5.5% to 9.2%; odds ratio, 1.75; 95% CI, 1.36 to 2.26). The difference between intervention and control facilities in the proportion of patients referred for transplant was higher among black patients (aMD, 6.4%; 95% CI, 4.3% to 8.6%) than white patients (aMD, 3.7%; 95% CI, 1.6% to 5.9%; P<0.05). In conclusion, this intervention increased referral and improved equity in kidney transplant referral for patients on dialysis in Georgia; long-term follow-up is needed to determine whether these effects led to more transplants.
Keywords: kidney transplantation, dialysis facility, randomized trial, education, staff, community-based participatory research
Compared with white patients with ESRD, black patients with ESRD are 24% less likely to receive a kidney transplant.1 Racial disparities persist across the multiple complex steps of the transplantation process.2–9 There are numerous patient-, provider-, neighborhood-, and health system-level reasons10 for these racial disparities, and the most modifiable barriers exist in the steps before waitlisting.9,11 For patients already on dialysis, referral for kidney transplant evaluation represents a potentially modifiable, yet necessary, step in the transplantation process, in which dialysis facilities play a major role.
Prior studies have shown that multicomponent quality improvement interventions conducted at the dialysis facility level have improved the care of patients with ESRD.12–15 The 2012–2014 Statement of Work for ESRD Networks, which contract with the CMS and conduct quality initiatives,16 included a requirement for networks to conduct a Population Health Innovation Pilot Project to reduce disparities in one of several areas, including transplant referral. ESRD Network 6 covers the largest patient population of any ESRD network, overseeing the care of nearly 45,000 patients with ESRD treated in >650 dialysis facilities in Georgia, North Carolina, and South Carolina, and is the network with the lowest rate of kidney transplantation in the United States.11,17 The network chose increasing transplant referral among patients on dialysis as a target for quality improvement and racial disparity reduction.
Results of a needs assessment by the Southeastern Kidney Transplant (SEKTx) Coalition, an interdisciplinary community coalition formed in partnership with ESRD Network 6,17–21 suggested that disparities in transplant access were complex and multilevel, and that a single intervention would be insufficient to eliminate the major barriers that patients face to receiving a kidney transplant. The Reducing Disparities in Access to kidNey Transplantation (RaDIANT) Community Study, an ESRD network–led, dialysis facility–based, randomized, pragmatic trial, was designed to test the effectiveness of a multicomponent educational, outreach, and quality improvement intervention targeting dialysis facility patients, staff, and leadership to improve access to transplantation. The primary aim of the RaDIANT Community Study was to improve the proportion of patients referred for kidney transplantation in Georgia. The secondary aim was to evaluate whether the implementation of this intervention reduced black versus white racial disparities in kidney transplant referral.
Results
Study Population
Facilities selected for participation in the RaDIANT Community Study (Figure 1) had, on average, a higher percentage of black patients (65.4% versus 49.0%), patients with Medicaid-only insurance at ESRD start (11.0% versus 8.5%), and lower rates of waitlisting and transplantation compared with facilities not selected for randomization (Supplemental Table 1).
Figure 1.
The RaDIANT Community Study flow diagram for dialysis facility selection in Georgia.
Baseline Characteristics of Dialysis Facilities by Study Group
Baseline characteristics of the 67 intervention and 67 control facilities were assessed (Table 1). The intervention and control facilities did not meaningfully or statistically differ in any of the patient and facility characteristics assessed in this study, with the exception of the proportion of patients with diabetes and the mean number of comorbidities (Table 1).
Table 1.
Baseline characteristics of participating Georgia (2008–2011) dialysis facilities by intervention and control group
| Facility and Patient Characteristics (2008–2011) | Study Population (n=134) | Intervention (n=67) | Control (n=67) |
|---|---|---|---|
| Facility characteristics | |||
| No. of patients per facility, mean±SD | 46.6±25.5 | 44.3±24.0 | 48.9±27.0 |
| No. of staff, mean±SD | 10.1±6.5 | 9.5±5.5 | 10.7±7.4 |
| For profit, % | 88.7 | 88.1 | 89.39 |
| Characteristics of patients within facility | |||
| Age, mean±SD | 61.2±5.7 | 60.2±6.1 | 62.3±5.1 |
| % White | 33.5 | 32.8 | 34.2 |
| % Black | 65.4 | 66.3 | 64.5 |
| % Hispanic | 1.5 | 1.9 | 1.1 |
| % Hemodialysis modality | 94.0 | 95.0 | 92.9 |
| % Uninsured at ESRD start | 11.5 | 9.9 | 13.1 |
| % Medicaid only at ESRD start | 11.0 | 12.9 | 9.1 |
| % Unemployed | 70.0 | 69.3 | 70.7 |
| Average time on dialysis (yr), mean±SD | 5.0 | 5.0±1.21 | 4.9±2.1 |
| % Receiving no pre-ESRD nephrology care | 26.0 | 25.7 | 26.3 |
| % Not informed of transplant options | 3.1 | 3.1 | 3.0 |
| % With diabetes | 59.9 | 54.8 | 65.1 |
| % With hypertension | 91.4 | 92.0 | 90.8 |
| % With arteriovenous fistula | 28.7 | 14.6 | 13.0 |
| Average count of comorbidities, mean±SD | 3.0 | 2.8±0.8 | 3.1±0.7 |
| Standardized transplant ratio | 0.46 | 0.42 | 0.50 |
Primary Outcome Results: Facility-Level Referral for Transplantation
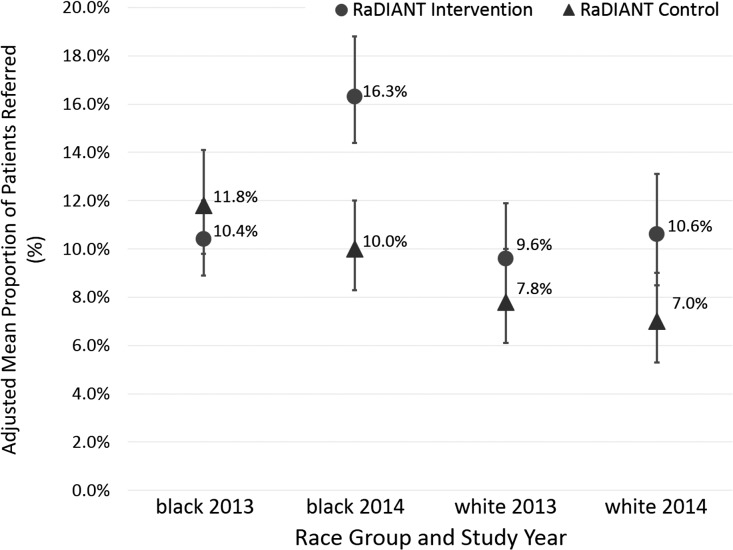
Across both study groups, dialysis facility referral for transplantation increased from 11.3% at baseline to 13.4% at 12 months. The number of referrals among the 67 intervention group facilities increased from 483 total referrals in 2013 to 767 referrals in 2014; in contrast, the number of referrals among the 67 control facilities decreased from 587 in 2013 to 521 in 2014. After adjusting for time trends and potential clustering effects of patients within facilities, the adjusted mean difference in the proportion of patients referred for transplant evaluation 1 year after intervention start was 7.3% (95% confidence interval [95% CI], 5.5% to 9.2%; P<0.001) between the intervention and control facilities (Table 2). Among black patients within a facility, the adjusted mean proportion of patients referred for transplant increased from 10.4% in 2013 to 16.3% in 2014 in the intervention group (P<0.001) versus a decrease from 11.8% to 10.0% in the control group. After 12 months, the mean difference in the proportion of black patients referred for transplant evaluation was 6.4% (95% CI, 4.3% to 8.6%). Among white patients within a facility, there was a small, nonsignificant increase in the adjusted mean proportion of patients referred for transplant: from 9.6% to 10.6% (P=0.45) in the intervention group versus 7.8% to 7.0% (P=0.51) in the control group. After 12 months, the mean difference in the proportion of white patients referred for transplant evaluation was 3.7% (95% CI, 1.6% to 5.9%) (Figure 2, Table 2).
Table 2.
Adjusted mean proportion of referrals for kidney transplant evaluation for RaDIANT Community Study intervention group versus control group among black and white patient populations within dialysis facilities at baseline (2013) and after the intervention (2014)
| Race | Year | Group | Mean Proportion of Patients Referred (95% CI) | Mean Difference in Proportion of Patients Referred between Intervention and Control (95% CI) |
|---|---|---|---|---|
| All races | 2013 | Control | 11.7 (9.9 to 13.8) | – |
| All races | 2013 | Intervention | 10.8 (9.4 to 12.4) | −0.9 (-0.6 to 2.5) |
| All races | 2014 | Control | 10.2 (8.6 to 12.2) | – |
| All races | 2014 | Intervention | 17.4 (15.0 to 20.0) | 7.3 (5.5 to 9.2) |
| Black | 2013 | Control | 11.8 (9.8 to 14.1) | – |
| Black | 2013 | Intervention | 10.4 (8.9 to 12.0) | −1.6 (-3.7 to 0.5) |
| Black | 2014 | Control | 10.0 (8.3 to 12.0) | – |
| Black | 2014 | Intervention | 16.3 (14.1 to 18.8) | 6.4 (4.3 to 8.6) |
| White | 2013 | Control | 7.8 (6.1 to 10.0) | – |
| White | 2013 | Intervention | 9.6 (7.7 to 11.9) | 1.8 (-0.4 to 3.9) |
| White | 2014 | Control | 7.0 (5.3 to 9.0) | – |
| White | 2014 | Intervention | 10.6 (8.5 to 13.1) | 3.7 (1.6 to 5.9) |
Mean proportions were adjusted for time and facility-level random effects. –, reference group.
Figure 2.
Adjusted mean proportion of dialysis facility referrals for RaDIANT Community Study intervention group versus control group among the black and white patient population within dialysis facilities at baseline (2013) and after the intervention (2014).
Whereas the adjusted odds of referral did not differ significantly between groups at baseline (odds ratio [OR], 0.94; 95% CI, 0.74 to 1.20), there was a significant difference in referral (interaction of intervention and time P<0.001) in the intervention versus control groups at 12 months postintervention (OR, 1.75; 95% CI, 1.36 to 2.26). The effectiveness of the intervention was higher among black patients (OR, 1.76; 95% CI, 1.35 to 2.30) compared with white patients (OR, 1.59; 95% CI, 1.10 to 2.29) (Table 3). Parameter estimates from mixed-effects logistic regression models are reported in Supplemental Table 2 (columns 1 and 2).
Table 3.
Effectiveness of the RaDIANT Community Study intervention stratified by race of patient population within Georgia dialysis facilities
| Adjusted OR for Transplant Referral (95% CI) | ||||
|---|---|---|---|---|
| Time | Comparison | Overall | White | Black |
| Baseline | Intervention versus control | 0.94 (0.74 to 1.20) | 1.25 (0.88 to 1.79) | 0.87 (0.67 to 1.12) |
| 12 Months | Intervention versus control | 1.75 (1.36 to 2.26) | 1.59 (1.10 to 2.29) | 1.76 (1.35 to 2.30) |
| Overall | Control | Intervention | ||
| Baseline | Black versus white | 1.31 (1.11 to 1.55) | 1.57 (1.22 to 2.03) | 1.09 (0.87 to 1.37) |
| 12 Months | Black versus white | 1.56 (1.31 to 1.86) | 1.48 (1.13 to 1.94) | 1.65 (1.31 to 2.06) |
ORs (95% CI) and group differences (95% CI) were adjusted for time and facility-level random effect.
In sensitivity analyses adjusting for the percentage of patients with diabetes and the mean number of comorbidities, results were similar to main analyses (data not shown).
Secondary Outcome Results: Disparity Reduction
As shown in Figure 2 and Table 2, the estimated mean proportion of transplant referrals for a black patient at baseline was not significantly different between the control and intervention groups; however, referral was significantly higher in the intervention group after 12 months (16.3%; 95% CI, 14.1% to 18.8%), compared with the control group (10.0%; 95% CI, 8.3% to 12.0%). In contrast, the probability of referral of a white patient did not significantly differ at baseline or postintervention between groups (Figure 2, Table 2).
The three-way race×time×intervention interaction was statistically significant (P=0.05), indicating the increase over time in the intervention versus control arm differed by race. Although black versus white referral was higher at both baseline (OR, 1.31; 95% CI, 1.11 to 1.55) and postintervention (OR, 1.56; 95% CI, 1.31 to 1.86), as some facilities had high proportions of black patients rather than a racial disparity, the ratio increased by 19% from baseline to 12 months postintervention (Table 3).
Black patients in control facilities were more likely to be referred than white patients in control facilities, both at baseline (OR, 1.57; 95% CI, 1.22 to 2.03) and postintervention (OR, 1.48; 95% CI, 1.13 to 1.94). However, in the intervention group, the OR increased from 1.09 (95% CI, 0.87 to 1.37) at baseline to 1.65 (95% CI, 1.31 to 2.06) at postintervention (a 1.5-fold increase over time) (Table 3).
Secondary Outcome Results: Evaluation and Waitlisting
By the end of the intervention (December of 2014), patients in intervention versus control facilities were more likely to have been evaluated (8.1% versus 4.8%; P<0.001) or waitlisted (1.9% versus 1.1%; P=0.002); effects were more pronounced among black versus white patients (Table 4).
Table 4.
Transplant evaluation and waitlisting among dialysis patients in the RaDIANT Community Study during the intervention year (2014)
| Patient Race | Evaluated at a Georgia Transplant Center | Waitlisted at a Georgia Transplant Center | ||||
|---|---|---|---|---|---|---|
| No. Evaluated/All Dialysis Patients (%) | No. Waitlisted/All Dialysis Patients (%) | |||||
| Intervention | Control | P-Valuea | Intervention | Control | P-Valuea | |
| All patients | 340/4203 (8.1) | 240/4817 (4.8) | <0.001 | 80/4203 (1.9) | 54/4817 (1.1) | 0.002 |
| Black | 262/3205 (8.2) | 169/3515 (4.8) | <0.001 | 58/3205 (1.8) | 34/3515 (1.0) | 0.003 |
| White | 51/963 (5.3) | 53/1268 (4.2) | 0.15 | 17/963 (1.8) | 15/1268 (1.2) | 0.25 |
Intervention versus control, by chi-squared test.
Fidelity Measures
A 20-item survey completed by 65 of 67 intervention facilities showed that participation in the nine “required” intervention components ranged from 56.9% (transplant education month) to 100% (facility in-service orientation to transplant) (Supplemental Table 3).22
Discussion
In this large, dialysis facility–based, randomized trial among 134 dialysis facilities treating >9000 patients with ESRD, we found that dialysis facilities that received a multicomponent educational and outreach intervention had a 75% increased adjusted odds of referral for kidney transplant evaluation over the 1-year time period. We also found that the intervention activities were more effective in increasing referrals among black versus white patients. For black patients, the absolute proportion of prevalent patients with ESRD referred for transplant evaluation increased from 10% at baseline to 16% at 1 year in the intervention group, resulting in a significant reduction in racial disparity in transplant referrals.
Long-standing research shows that black patients are less likely than white patients to receive a kidney transplant,1 and these racial disparities have been documented in the provision of patient education about transplantation within a dialysis facility,9 patient interest in receiving a transplant,9 referral from a dialysis facility to a transplant center for transplant evaluation,2 starting3 and completing the required transplant medical evaluation, waitlisting,4 and receipt of a living or deceased donor transplant.5–9 There are numerous reasons10 for these racial disparities, and the most modifiable barriers exist before waitlisting.9,11
However, few interventions have been conducted to reduce disparities in the early steps of the transplant process.23 A 2012 Agency for Healthcare Research & Quality report, Quality Improvement Interventions to Address Health Disparities, found in a review of 791 studies that no study was identified in the ESRD population that specifically examined health disparity reduction as an end point. Although numerous studies have described the effectiveness of interventions on improving transplant knowledge and education and increasing living donor transplantation,24–26 many have focused on the less advantaged population (e.g., the black population), making it difficult to know whether widespread adoption of the intervention would increase access to transplant for all groups, or whether it has the potential to reduce racial disparity. To our knowledge, this is the first study that has shown that the intervention studied was effective among both black and white patients with ESRD, but was more effective among black patients. These results suggest that, when targeted to dialysis facilities with low transplant performance and a high proportion of black patients with ESRD and/or racial disparity in transplant referral, a multicomponent educational and outreach intervention could reduce disparities in access to kidney transplantation.
There are several weaknesses to this study that should be noted. First, the intervention was multicomponent, and thus it is not possible to discern which specific components of the intervention are more or less effective in improving transplant referrals. Second, referrals for transplantation were reported by transplant centers, but the validity of this measure is unknown. Third, our analysis was not powered sufficiently to examine longer-term outcomes, such as waitlisting and transplantation. However, our preliminary results examining evaluation and waitlisting within the first year of the intervention show promising results, with a reduction in racial disparities at these later steps in the transplant process. Finally, the multipronged selection strategy of facilities (i.e., those that had racial disparity in referral as well as those that had low referral overall but may not have had a racial disparity) resulted in a sample in which baseline referral was higher among blacks compared with whites. Thus, the study did target some dialysis facilities that were already referring a greater proportion of blacks compared with whites at baseline. However, racial disparities in access to multiple steps of the kidney transplant process are well documented, and the interventions in this study emphasized both increased referral and a reduction in racial disparities.
Prior studies have suggested that targeting ESRD regions with the most racial disparity in transplant receipt could reduce the overall racial disparity in referral to the kidney transplant waiting list by 25% in the United States.27 The RaDIANT Community Study targeted one sixth of the black patients with ESRD receiving treatment from dialysis facilities in Georgia, showing that a multicomponent educational and outreach initiative improved kidney transplant referral and reduced racial disparity in referral in a state with the lowest rate of kidney transplantation and highest proportion of black patients with ESRD.17 This multicomponent intervention could be adapted for use by other ESRD networks and/or other members of the kidney community to improve access to transplantation and/or reduce racial disparities in access to kidney transplantation. Longer-term follow-up is needed to confirm whether the RaDIANT Community Study helped to reduce disparities in subsequent access to kidney transplantation.
Concise Methods
Study Design
The RaDIANT Community Study was a dialysis facility–level, randomized, clinical trial designed to test the effectiveness of a multicomponent intervention in increasing patient referral for kidney transplantation within dialysis facilities. Before initiation of intervention activities, the RaDIANT Community Study was registered on Clinicaltrials.gov (identifier: NCT02092727) and approved by Institutional Review Boards at Emory University, Georgia Regents University, and Piedmont Hospital.
Target Population and Setting
Approximately 47% of the dialysis facilities in ESRD Network 6’s service areas are located in Georgia, and facilities in Georgia treated >12,000 dialysis patients in 2012.28 The RaDIANT Community Study targeted 134 Georgia outpatient dialysis facilities, representing nearly half (47%) of all Georgia dialysis facilities and >9000 patients, including >5000 black patients with ESRD, according to data from the 2012 Dialysis Facility Report.
Sample Size, Inclusion/Exclusion Criteria, and Dialysis Facility Randomization
We estimated that a sample size of 134 dialysis facilities (67 facilities in each arm) would achieve 80% power to detect a moderate absolute difference of 4.8% in referral between the intervention and control groups, at 5% significance level. In 2012, there were 283 dialysis facilities open in Georgia. A total of nine facilities had a 6-month patient population count of ≤12 patients aged <70 years, and were excluded. The remaining facilities (n=274) were next classified by whether they had either (1) a black versus white racial disparity in referral (n=75 facilities), defined as an absolute proportion of referrals higher among white patients compared with black patients; or (2) a within-facility referral proportion <50th percentile of the 274 facilities (n=59 facilities). The 134 facilities that met either criteria were selected for randomization in a 1:1 fashion, using a random number generator (Figure 2).
Transplant Center Data Collection
Data on all patients referred from a dialysis facility to any of the three Georgia transplant centers were collected as previously described.18,29 Patient data included age, race/ethnicity, date of dialysis start, date of transplant referral, date of evaluation, and waitlist status. Referral date was defined as the date on which a faxed transplant referral form from a dialysis facility, referring physician, or self-referral was received by the transplant center. Each transplant center securely sent patient-level data to ESRD Network 6, where each referral was assigned a dialysis facility on the basis of the facility the patient was receiving care at the time of the referral. Patient data were deidentified and linked via unique provider number to dialysis facility–level data using publicly available 2012 Dialysis Facility Report data.
Control/Comparison Group (Study Arm 1)
Dialysis facilities randomized to the standard intervention did not receive any specific interventions related to transplant education. By law, all dialysis facilities are required to educate patients about transplantation as a treatment option within the first 60 days of ESRD start, and record the assessment of this on patients’ Medicare eligibility (CMS-2728) forms.
Multicomponent Intervention (Study Arm 2)
The SEKTx Coalition aimed to develop a sustainable, multicomponent, multilevel quality improvement intervention targeting dialysis facility staff and patients. SEKTx Coalition members participated in face-to-face and phone conference meetings over several months to design and choose intervention activities. Intervention components were developed by SEKTx Coalition members using core concepts of the Social Ecological Model, which proposes that individual, interpersonal, community, organizational, and societal factors should be taken into account when planning and implementing health promotion interventions.30 Final interventions were selected by Coalition members on the basis of the core tenets of prior quality improvement interventions at dialysis facilities, the feasibility of implementation, sustainability beyond the study, and perception of acceptance among stakeholders.
Intervention activities were delivered over a 1-year time period (January of 2014 to December of 2014) and were designed to target multiple levels, including patient, dialysis facility staff (e.g., nephrologists, social workers, and nurses), and facility leadership (i.e., Medical Director) levels. For example, several interventions targeted facility policies and protocols, including the requirements that facilities create their own transplant referral quality improvement plan, work with ESRD Network 6 on quality improvement assistance and review, and conduct their own transplant education activities. Medical Directors received facility-specific information about transplant referral rates and racial disparities in their referral. Facility staff were encouraged to participate in quality improvement activities and attend monthly educational webinars developed by SEKTx Coalition members.31 Patients were encouraged to participate in a patient and family transplantation advisory group, a mentoring program to speak with prior transplant recipients, and utilize a patient educational toolkit about transplantation that included patient educational material and a shared clinical decision aid for treatment options,32 and had the opportunity to participate in a movie night that showed a culturally sensitive living donor transplant education video focused on encouraging living donation among the black population.26 The major intervention activities are described in Supplemental Table 3 and are as previously described.18
Outcome Measures
The primary outcome of the RaDIANT Community Study was the change in facility-level transplant referral for patients aged <70 years from baseline to 12 months. Baseline referral for either the intervention or control group was calculated as the number of unique referrals in a dialysis facility over the 12-month period preceding the intervention (January of 2013 to December of 2013) divided by the total number of patients with ESRD within the facility for that time period. The postintervention crude referral rate was measured as the number of unique referrals generated from January of 2014 to December of 2014 divided by the total number of patients with ESRD within the facility for the same 12-month intervention period. Patient-level transplant referral data with facility identifiers were collected from all of the transplant centers in Georgia, and aggregated to summarize the total number of referrals to any transplant center in the state divided by the total number of adult patients with ESRD aged <70 years in the facility within the year.
A secondary outcome was the reduction in black versus white racial disparity in transplant referral from baseline to 1 year after the intervention. The reduction in racial disparity was measured as the difference between black and white patients in the proportion of patients referred for transplantation from baseline to 1 year.
Additional secondary outcomes of evaluation start and waitlisting during the intervention year (2014) were also examined by intervention status.
Fidelity Measures
ESRD Network 6 staff monitored participation in required activities on a monthly basis and by emailing a survey to project leadership at the end of the study to evaluate intervention uptake.
Statistical Analyses
All analyses were conducted as intention to treat, i.e., all facilities randomized to the intervention group at baseline were considered to have received the intervention, even if the facilities did not participate in intervention activities. Descriptive facility-level baseline characteristics were compared and differences between study arms at baseline were evaluated using either t tests or nonparametric equivalents for continuous variables, and chi-squared test for categorical variables. Any statistically significant differences in baseline characteristics were assumed to be by chance; sensitivity analyses were conducted to adjust for any chance differences in characteristics between study groups.
Due to the binomial nature of the outcomes (proportions of overall, white, and black referral rates), a generalized mixed-effects model was used to test for intervention effects on facility-level referral rates for the control and intervention group. Specifically, a random intercept model was used to account for clustering within facilities and test for differences in proportion of transplant referrals by study arm at 12 months (postintervention), after accounting for baseline referrals. A linear growth trajectory (between baseline and postintervention) was fitted to the observed data to evaluate whether individuals in the intervention group were referred at a faster linear rate compared with those in the control group. Treatment (intervention status: 0/1), time (baseline and postintervention), and treatment×time interaction were treated as fixed factors. A treatment contrast was estimated at each time point, as well as over time, for the two arms as a measure of likelihood of being referred in the intervention versus control group after adjustment for facility-level variation.
For our secondary outcome, disparity in black versus white referrals, we used facility-level referrals stratified by race (black versus white) as the outcome and repeated our mixed-effects model to include race as an independent factor. Race×time, race×intervention, and race×intervention×time interactions were included to test for racial differences in referrals over time, across the study arms, and the combination of the two factors. Using the white referral rate as the reference, the OR (and 95% CI) of referring a black patient was estimated postintervention relative to baseline. Similar ORs and 95% CIs stratified by study arms were also estimated.
SAS 9.4 and Stata v.14 software were used for data organization and analyses. All P values were two-sided and considered statistically significant at the P<0.05 level.
Disclosures
S.O.P. is a minority shareholder in Fresenius College Park Dialysis, College Park, GA.
Supplementary Material
Acknowledgments
The authors acknowledge the assistance of the Southeastern Kidney Council, Inc., and the Centers for Medicare & Medicaid Services (CMS) in providing data which made this research possible. The Southeastern Kidney Transplant Coalition performed a needs assessment that enabled the development of the multilevel intervention. The Coalition conceptualized the intervention, participated in data collection, and provided feedback for program evaluation. All authors have approved the final manuscript and certify that this manuscript represents valid work and has not been previously published.
The Reducing Disparities in Access to kidNey Transplantation Community Study was funded in part by NIMHD award R24MD008077. Support for the preparation of this document was provided by contract number HHSM-500-2013-NW006C from ESRD Network 6, funded by the CMS—an agency of the US Department of Health and Human Services.
The conclusions presented are solely those of the authors and do not represent those of Southeastern Kidney Council, Inc., or the CMS. The content of this publication does not necessarily reflect the policies or positions of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government.
In addition to the primary authors of this manuscript, we would like to acknowledge the other Coalition members here: Angela Adams (Fresenius Medical Care), Cynthia Allison (Patient Advocate), Emily Arnold (University of North Carolina), Prabhakar Baliga (Medical University of South Carolina), Brenda Banks (Patient Advocate), Mohua Basu (Emory University), Alex Berlin (Patient Advocate), Paul Broughton (Apex Health Innovations), Noreen Carew (Piedmont Hospital), Doreen Church (Georgia Medical Care Foundation), Diana Clynes (American Association of Kidney Patients), Marshia Coe (Emory Dialysis), Bradley H. Collins (Duke University), Randy Detwiler (University of North Carolina), Chris DiMotta (Emory University), Jil Dubbs (National Kidney Foundation), Matthew Ellis (Duke University), Jennifer Eubanks (DaVita), Debra Evans (ESRD Network 6), Shauna Flemming (Emory University), Christopher Fowler (Piedmont Hospital), Debbie Gibbs (LifePoint Health), JoVonn Givens (Georgia Medical Care Foundation), Gary Green (American Association of Kidney Patients), Jill Hall (LifeLink of Georgia), Brian Hardin (Pitt County Memorial Hospital), Erica Hartmann (Piedmont Hospital), Ben Hippen (Metro Atlanta Nephrology), Lisa Hobson (Dialysis Clinic, Inc), Amy Houser (Medical University of South Carolina), Ben Hymes (Fresenius Medical Care), Sandy Imundo (Fresenius Medical Care), Nancy A. Kay (LifePoint Health), Lauren Kearns (University of North Carolina), Heidari Khosrow (National Association of Chronic Disease Directors), Linda Kluge (Georgia Transplant Foundation), Leah Knowles (Carolinas Healthcare System Transplant Center), Tomsz Kozlowski (University of North Carolina), Nancy Kutner (Emory University), Scott Lloyd (DaVita Dialysis), Arietta Maney (Piedmont Hospital), Caitlin Mardis (Medical University of South Carolina), Leslie M. McAllister (Carolinas Healthcare System Transplant Center), Lisa McCanna (Carolinas Healthcare System Transplant Center), Sandy McMath (Georgia Transplant Foundation), Laura McPherson (Emory University), Leslie Mills (Carolinas Healthcare System Transplant Center), Adrienne Mims (Alliant Quality), Suzette Mitchell (Fresenius Medical Care), Linda Moore (The Carolinas Center for Medical Excellence), Rich Mutell (Apex Health Innovations), Danielle Niedfeldt (Carolina Donor Services), Kathy Oliver (Health Systems Management), Jennie Perryman (Emory University), Kim E. Phillips (Medical University of South Carolina), Alicia Porter (Georgia Transplant Foundation), Lillian Pryor (Loganville Dialysis Center), Amber Reeves-Daniel (Wake Forest Baptist Medical Center), Gary Renville (National Kidney Foundation), Bonnie Robbins (National Kidney Foundation), Jason Rolls (Pitt County Memorial Hospital), Martie Rudd (Georgia Transplant Foundation), Tory Scoggins (Fresenius Medical Care), Stephen R. Smith (Duke University), Titte Srivinas (Medical University of South Carolina), Theresa Tapley (Fresenius Medical Care), Stephani Tucker (National Kidney Foundation), Henry Well (National Kidney Foundation), John Jason White (Augusta University), Kellee White (University of South Carolina), Christina Wiggins (Augusta University), Myra Williams (Wake Forest Baptist Medical Center), Elijah Wise (Patient Advocate), and Amy Woodard (University of North Carolina).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Should Transplant Referral Be a Clinical Performance Measure?,” on pages 721–723.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2016030320/-/DCSupplemental.
Contributor Information
Collaborators: Rachel E. Patzer, Sudeshna Paul, Laura Plantinga, Jennifer Gander, Leighann Sauls, Jenna Krisher, Laura L. Mulloy, Eric M. Gibney, Teri Browne, Carlos F. Zayas, William M. McClellan, Kimberly Jacob Arriola, and Stephen O. Pastan
References
- 1.United States Renal Data System : United States Renal Data System, 2014 Annual Data Report: An overview of the epidemiology of kidney disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2014 [Google Scholar]
- 2.Garg PP, Frick KD, Diener-West M, Powe NR: Effect of the ownership of dialysis facilities on patients’ survival and referral for transplantation. N Engl J Med 341: 1653–1660, 1999 [DOI] [PubMed] [Google Scholar]
- 3.Weng FL, Joffe MM, Feldman HI, Mange KC: Rates of completion of the medical evaluation for renal transplantation. Am J Kidney Dis 46: 734–745, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Patzer RE, Amaral S, Wasse H, Volkova N, Kleinbaum D, McClellan WM: Neighborhood poverty and racial disparities in kidney transplant waitlisting. J Am Soc Nephrol 20: 1333–1340, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashby VB, Kalbfleisch JD, Wolfe RA, Lin MJ, Port FK, Leichtman AB: Geographic variability in access to primary kidney transplantation in the United States, 1996-2005. Am J Transplant 7: 1412–1423, 2007 [DOI] [PubMed] [Google Scholar]
- 6.Stolzmann KL, Bautista LE, Gangnon RE, McElroy JA, Becker BN, Remington PL: Trends in kidney transplantation rates and disparities. J Natl Med Assoc 99: 923–932, 2007 [PMC free article] [PubMed] [Google Scholar]
- 7.Waterman AD, Rodrigue JR, Purnell TS, Ladin K, Boulware LE: Addressing racial and ethnic disparities in live donor kidney transplantation: priorities for research and intervention. Semin Nephrol 30: 90–98, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weng FL, Reese PP, Mulgaonkar S, Patel AM: Barriers to living donor kidney transplantation among black or older transplant candidates. Clin J Am Soc Nephrol 5: 2338–2347, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Waterman AD, Peipert JD, Hyland SS, McCabe MS, Schenk EA, Liu J: Modifiable patient characteristics and racial disparities in evaluation completion and living donor transplant. Clin J Am Soc Nephrol 8: 995–1002, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patzer RE, McClellan WM: Influence of race, ethnicity and socioeconomic status on kidney disease. Nat Rev Nephrol 8: 533–541, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patzer RE, Pastan SO: Kidney transplant access in the Southeast: view from the bottom. Am J Transplant 14: 1499–1505, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bond TC, Patel PR, Krisher J, Sauls L, Deane J, Strott K, McClellan W: A group-randomized evaluation of a quality improvement intervention to improve influenza vaccination rates in dialysis centers. Am J Kidney Dis 57: 283–290, 2011 [DOI] [PubMed] [Google Scholar]
- 13.McClellan WM, Krisher JO: Collecting and using patient and treatment center data to improve care: Adequacy of hemodialysis and end-stage renal disease surveillance. Kidney Int 57[Suppl 74]: S7–S13, 2000 [Google Scholar]
- 14.McClellan WM, Hodgin E, Pastan S, McAdams L, Soucie M: A randomized evaluation of two health care quality improvement program (HCQIP) interventions to improve the adequacy of hemodialysis care of ESRD patients: feedback alone versus intensive intervention. J Am Soc Nephrol 15: 754–760, 2004 [DOI] [PubMed] [Google Scholar]
- 15.Lynch JR, Wasse H, Armistead NC, McClellan WM: Achieving the goal of the Fistula First breakthrough initiative for prevalent maintenance hemodialysis patients. Am J Kidney Dis 57: 78–89, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wish JB, Meyer KB: ESRD Networks: past, present, and challenges for the future. Clin J Am Soc Nephrol 7: 1907–1914, 2012 [DOI] [PubMed] [Google Scholar]
- 17.Patzer RE, Plantinga L, Krisher J, Pastan SO: Dialysis facility and network factors associated with low kidney transplantation rates among United States dialysis facilities. Am J Transplant 14: 1562–1572, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patzer RE, Gander J, Sauls L, Amamoo MA, Krisher J, Mulloy LL, Gibney E, Browne T, Plantinga L, Pastan SO; Southeastern Kidney Transplant Coalition : The RaDIANT community study protocol: community-based participatory research for reducing disparities in access to kidney transplantation. BMC Nephrol 15: 171, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Browne T, Amamoo A, Patzer RE, Krisher J, Well H, Gander J, Pastan SO: Everybody needs a cheerleader to get a kidney transplant: a qualitative study of the patient barriers and facilitators to kidney transplantation in the Southeastern United States. BMC Nephrol 17: 108, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Browne T, Patzer RE, Gander J, Amamoo MA, Krisher J, Sauls L, Pastan SO: Kidney transplant referral practices in southeastern dialysis units. Clin Transplant 30: 365–371, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gander J, Browne T, Plantinga L, Pastan SO, Sauls L, Krisher J, Patzer RE: Dialysis facility transplant philosphy and access to kidney transplantation in the Southeast. Am J Nephrol 41: 504–511, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gander JCSL, Browne T, Plantinga L, McPherson L, Gibney E, Mulloy LL, Pastan SO, Patzer RE: Feasibility and sustainability of the RaDIANT Community Study among Georgia dialysis facilities. J Am Soc Nephrol 26[Suppl]: 68A, 2015 [Google Scholar]
- 23.Asch WS, Bia MJ: Patient education to reduce disparities in renal transplantation. Clin J Am Soc Nephrol 7: 527–529, 2012 [DOI] [PubMed] [Google Scholar]
- 24.Sullivan C, Leon JB, Sayre SS, Marbury M, Ivers M, Pencak JA, Bodziak KA, Hricik DE, Morrison EJ, Albert JM, Navaneethan SD, Reyes CM, Sehgal AR: Impact of navigators on completion of steps in the kidney transplant process: a randomized, controlled trial. Clin J Am Soc Nephrol 7: 1639–1645, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodrigue JR, Paek MJ, Egbuna O, Waterman AD, Schold JD, Pavlakis M, Mandelbrot DA: Making house calls increases living donor inquiries and evaluations for blacks on the kidney transplant waiting list. Transplantation 98: 979–986, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arriola KR, Powell CL, Thompson NJ, Perryman JP, Basu M: Living donor transplant education for African American patients with end-stage renal disease. Prog Transplant 24: 362–370, 2014 [DOI] [PubMed] [Google Scholar]
- 27.Milda R, Saunders HT, Ross L, Alexander GC: Regional variation in transplant waitlist: a contributor to transplant disparities. Presented at Society of General Internal Medicine, Phoenix, AZ, May , 2012 [Google Scholar]
- 28.Southeastern Kidney Council, Inc. End Stage Renal Disease Network 6 2013 Annual Report. Raleigh, NC. Available at: http://esrd.ipro.org/wp-content/uploads/2016/06/2013-Network-6-SKC-Annual-Report-web.pdf. Accessed January 10, 2016
- 29.Patzer RE, Plantinga LC, Paul S, Gander J, Krisher J, Sauls L, Gibney EM, Mulloy L, Pastan SO: Variation in Dialysis Facility Referral for Kidney Transplantation Among Patients With End-Stage Renal Disease in Georgia. JAMA 314: 582–594, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McLeroy KRBD, Bibeau D, Steckler A, Glanz K: An ecological perspective on health promotion programs. Health Educ Q 15: 351–377, 1988 [DOI] [PubMed] [Google Scholar]
- 31.6 ESRD Networks: Transplant Health Innovation Project: Related Content, 2014. Available at: http://www.esrdnetwork6.org/improving-care/transplant.html. Accessed June 1, 2016
- 32.Patzer RE, Basu M, Larsen CP, Pastan SO, Mohan S, Patzer M, Konomos M, McClellan WM, Lea J, Howard D, Gander J, Arriola KJ: iChoose Kidney: A Clinical Decision Aid for Kidney Transplantation Versus Dialysis Treatment. Transplantation 100: 630–639, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.