Abstract
Background
Brain derived neurotrophic factor (BDNF) is one of the most important regulatory proteins in the pathophysiology of major depressive disorder (MDD). Increasing numbers of studies have reported the relationship between serum/plasma BDNF and antidepressants (ADs). However, the potential effects of several classes of antidepressants on BDNF concentrations are not well known. Hence, our meta-analyses aims to review the effects of differential antidepressant drugs on peripheral BDNF levels in MDD and make some recommendations for future research.
Methods
Electronic databases including PubMed, EMBASE, the Cochrane Library, Web of Science, and PsycINFO were searched from 1980 to June 2016. The change in BDNF levels were compared between baseline and post-antidepressants treatment by use of the standardized mean difference (SMD) with 95% confidence intervals (CIs). All statistical tests were two-sided.
Results
We identified 20 eligible trials of antidepressants treatments for BDNF in MDD. The overall effect size for all drug classes showed that BDNF levels were elevated following a course of antidepressants use. For between-study heterogeneity by stratification analyses, we detect that length of treatment and blood samples are significant effect modifiers for BDNF levels during antidepressants treatment. While both SSRIs and SNRIs could increase the BDNF levels after a period of antidepressant medication treatment, sertraline was superior to other three drugs (venlafaxine, paroxetine or escitalopram) in the early increase of BDNF concentrations with SMD 0.53(95% CI = 0.13–0.93; P = 0.009).
Conclusions
There is some evidence that treatment of antidepressants appears to be effective in the increase of peripheral BDNF levels. More robust evidence indicates that different types of antidepressants appear to induce differential effects on the BDNF levels. Since sertraline makes a particular effect on BDNF concentration within a short amount of time, there is potential value in exploring its relationship with BDNF and its pharmacological mechanism concerning peripheral blood BDNF. Further confirmatory trials are required for both observations.
Introduction
Major depressive disorder (MDD) is a chronic mental illness that is characterized by persistent sadness and loss of interests for a minimum of two weeks [1–2]. Brain derived neurotrophic factor (BDNF) is a neurotrophic protein that has an important role in axonal growth, synaptic plasticity, and neuronal repair, and its levels are affected by stress [3–5]. There is growing evidence indicating that BDNF is related to many psychiatric disorders such as MDD in human studies [6–8].
Ever since Karege et al [9] demonstrated lower serum BDNF levels in depressed patients, considerable work has been carried out to investigate the relationship between decreased peripheral BDNF levels and pathogenesis of MDD [10–13]. Alternatively, several clinical studies pointed out that the down-regulation of peripheral BDNF levels in MDD patients could be reversed after a period of antidepressants (ADs) treatment. In parallel, earlier meta-analyses showed that peripheral BDNF levels were increased after pharmacological treatments [13, 14]. Moreover, several studies have investigated that ECT and different classes of antidepressants such as the serotonin selective reuptake inhibitors (SSRIs), serotonin norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants (TCAs) have effects on the peripheral BDNF in MDD patients [15–18]. However, whether all the antidepressants have effects on the BDNF levels remains controversial. For instance, Matrisciano et al found that both sertraline (an SSRI) and venlafaxine (an SNRI) could increase BDNF levels, while escitalopram (an SSRI) did not affect BDNF levels at either time point [19]. Başterzi et al. found that fluoxetine (an SSRI) changed the BDNF levels of the patient group with treatment, but venlafaxin could not [20]. Molendijk et al. previously observed that the use of SSRIs was related to the increase in serum BDNF level [10]. These results suggested that differential antidepressants may have variable effects on peripheral BDNF levels during treatment, which is still not well known.
Accordingly, BDNF may have potential use as a predictor of antidepressant efficacy, and abundant clinical data from pre-antidepressant and antidepressant-treated depressed patients motivated us to investigate the differential effects of antidepressant drugs on BDNF concentrations. We therefore performed a systematic review and meta-analysis aiming to examine the action of various reported antidepressant drugs on peripheral BDNF levels in MDD patients.
Methods
The study design was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement guidelines (S1 Text).
Search strategy
Electronic databases (PubMed, EMBASE, the Cochrane Library, Web of Science, and PsycINFO) were systematically searched (S2 Text, which summarizes the applied search strategies). All previous human studies through June 2016 (published original clinical studies, conference proceedings, meta-analyses) comparing pre- and post-antidepressant treatment peripheral BDNF levels were considered. The search terms were settled as: (“brain derived neurotrophic factor” OR BDNF), “antidepressant”, AND (“major depression” OR “major depressive disorder” OR MDD OR “depressive episode” OR “depression”).
Study selection strategy
Three independent researchers (TL, JJZ, and XD) selected studies for inclusion with discrepancies resolved by discussion. The titles and abstracts were scanned, and potentially relevant studies were reviewed in full. We included eligible studies examining plasma or serum BDNF levels in patients pre- and post-antidepressant treatment. Furthermore, each included study should make descriptions of the antidepressant use and time points in the therapy. Since we focused on the effect of pharmacological treatments on BDNF levels, studies using antidepressant treatment such as electroconvulsive therapy (ECT) or deep brain stimulation (DBS) were not suitable for this meta-analysis. Abstracts, case studies, family-based designs, population-based studies on healthy subjects, reviews, and duplicate cohorts were excluded.
Data extraction and outcome measures
Three authors (TL, CJZ, and BZ) independently extracted data to avoid extraction errors. The following parameters were extracted from each eligible article: first author, publication year, country of origin, diagnostic system, number of subjects (male/female), antidepressants use, measuring sample (plasma or serum), BDNF levels, and Hamilton Depression Rating Scale (HDRS) scores. The primary outcome was BDNF levels from baseline to post-treatment and we extracted the data for short-term (1 to 12 weeks) in each study. If one study reported BDNF concentrations for more than one time point within our pre-defined periods, we considered the data recorded at baseline and the last time point within the range for the overall effect analysis.
Statistical methods
First, all statistical analyses for meta-analysis were conducted using Rev Man 5.0.1 and STATA software (version 12.1; Stata Corporation, College Station, Texas, USA). All P-values were two-sided with a P<0.05 considered statistically significant. The alterations before and after antidepressant medication were assessed by SMDs (and their 95% CIs) for each study. A chi-squared-based Q-statistic test was used to detect the heterogeneity among studies, and a random-effects model was applied. We used a Z-test to determine the significance of the pooled SMDs with a P<0.05 considered statistically significant. Stratification-based analyses were carried out to evaluate heterogeneity and the possible moderating effects of between-study differences on outcomes.
In order to evaluate possible biases, a sensitivity analysis was conducted by leave–one-out methods to assess the contribution of each individual dataset to the pooled OR. Finally, we estimated publication bias by Egger’s test with a P<0.05 considered statistically significant.
Result
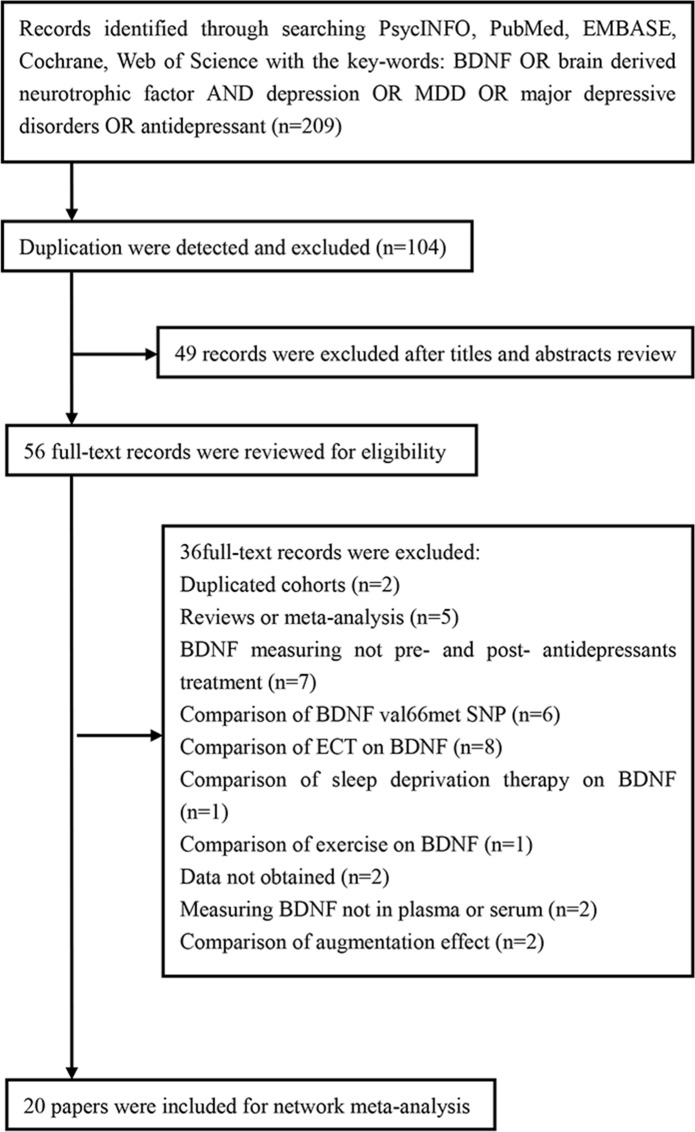
The study selection procedure is shown in Fig 1 (Fig 1). The literature search identified 206 potentially relevant records. After screening titles and abstracts, 56 full-text articles were reviewed, of which 36 were excluded for the following reasons: (i) two studies were duplicated cohorts; (ii) five studies were reviews or meta-analyses; (iii) seven studies did not assess BDNF pre- and post- antidepressant treatment; (iv) six studies compared the BDNF val66met SNP; (v) twelve studies did not compare antidepressant medication but analyzed effects of other methods(ECT, sleep deprivation therapy, exercise et al) on BDNF; (vi) data from two studies could not be obtained; (vii) two studies did not measure BDNF, either in plasma or serum. Hence, twenty studies were ultimately included in this meta-analysis based on our inclusion criteria [19, 21–39]. The study characteristics are displayed in Table 1. The characteristics of antidepressants such as antidepressants types, dose of antidepressants and duration of antidepressants treatment et al. are displayed in Table 2.
Fig 1. Flowchart of Study Selection.
Table 1. Characteristics of 20 included studies (studies are sorted by year and month of publication).
| Study | Year | Country | Diagnostic | Antidepressants | Number(F/M) | Mean age | BDNF | HDRS | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample | Pre-treatment | Post-treatment | Pre-treatment | Post-treatment | |||||||
| Mikoteit | 2015 | Switzerland | DSM-IV | SNRI | 25(8/17) | 43.7±12.5 | serum | 5.01±3.64 | 7.3±5.6 | 22.2±4.9 | 9.0±6.6 |
| Ghosh | 2015 | India | DSM-IV | SSRI,SNRI | 60(32/28) | 33.6±8.9 | plasma | 767.91±29.455 | 848.05±28.87 | 18.5±3.92 | 9.62±3.865 |
| Yoshimura | 2014 | Japan | DSM-IV | SSRI | 60 | 50.4±15.1 | serum | 8.6±7.2 | 11.2±8.4 | 21.0±4.3 | 10.0±5.6 |
| Brunoni | 2014 | Brazil | MINI | SSRI | 18 | 41.0±1.0 | plasma | 1331±786 | 1620±672 | 22.0±4.0 | 14.0±8.0 |
| Martocchia | 2014 | Switzerland | DSM-IV | SSRI | 5 | 74.0±6.8 | serum | 11.5 ± 0.6 | 16.0 ± 2.7 | — | — |
| Munno | 2013 | Italy | DSM-IV | SSRI | 16 | 48.19±10.3 | serum | 14.87±2.9 | 14.69±1.6 | 19.20±1.83 | 12.44±2.40 |
| plasma | 231.4±90.1 | 312.9±109.4 | 19.20±1.83 | 12.44±2.40 | |||||||
| Ladea | 2013 | Romania | DSM-IV | SSRI | 20 | 36.6±8.1 | serum | 35.6±12.7 | 35.7±13.2 | — | — |
| Deuschle | 2013 | Germany | DSM-IV | SNRI, Mirtazapine | 56(41/15) | 52.3±15.9 | serum | 7.73±6.99 | 7.84±5.49 | 22.85±4.35 | 8.15±5.65 |
| Dreimüller | 2012 | Germany | DSM-IV | SSNRI, SNRI, TCA, Mirtazapine | 39(19/20) | 44.9±13.9 | plasma | 298±196 | 334±157 | 19 | 12 |
| Wolkowitz | 2011 | USA | DSM-IV | SSRI | 30(9/21) | 39.1±9.6 | serum | 14.85±5.34 | 19.12±7.05 | 25.2±5.95 | 12.1±8.05 |
| Rojas | 2011 | Chile | DSM-IV | SNRI | 34(24/10) | 41.05±11.15 | serum | 12.2±9.95 | 8.85±2.44 | 22.8±3.65 | 11.43±1.48 |
| Matrisciano | 2009 | Italy | DSM-IV | SSRI,SNRI | 21(10/11) | 42.5±8.3 | serum | 35.37±14.33 | 39.43±14.97 | 17.6±5.3 | — |
| Piccinni | 2008 | Italy | DSM-IV | SSNRI,SNRI,TCA | 15 | 47.0±10.8 | serum | 19.3±8.8 | 24.457±9.921 | — | — |
| plasma | 290±190 | 456.3±198.5 | — | — | |||||||
| Huang | 2008 | China | DSM-IV | Mirtazapine. SSRI, SNRI | 79(61/18) | 37.3±10.0 | serum | 10.7±7.3 | 12.0±8.9 | 35.1±4.9 | 12.1±10.8 |
| Hellweg | 2007 | Germany | DSM-IV | TCA,SSRI | 20(17/3) | 50.5±14.4 | serum | 13.13±4.43 | 13.60±5.41 | 23.4±4.5 | 11.35±8.25 |
| Yoshimura | 2007 | Japan | DSM-IV | SSRI,SNRI | 42(26/16) | 46±20.5 | serum | 9.6±8.8 | 16.85±7.85 | 23.5±6.5 | — |
| Aydemir | 2006 | Turkey | DSM-IV | SSRI | 20(20/0) | 35.55±7.58 | serum | 27.68±13.74 | 38.57±15.30 | 39.75±7.40 | 9.31±6.05 |
| Gonul | 2005 | Turkey | DSM-IV | SSRI,SNRI | 28(21/7) | 35.5±8.1 | serum | 20.8 ± 6.7 | 33.3±9.89 | 27.28 ± 3.53 | 8.85±3.15 |
| Aydemir | 2005 | Turkey | DSM-IV | SNRI | 10(8/2) | 31.8±14.3 | serum | 17.9±9.1 | 34.6±7.1 | 23.2±4.6 | 8.2±3.9 |
| Shimizu | 2003 | Japan | DSM-IV | SSRI,SNRI | 4(2/2) | 46.0±12.2 | serum | 13.32±11.97 | 28.79±6.23 | 33.5±10.5 | 2.8±1.0 |
BDNF concentration: Serum, ng/ml; Plasma, pg/ml. SSRI, Selective Serotonin Reuptake Inhibitor. SNRI, selective noradrenalin reuptake inhibitors. TCA, tricyclic antipsychotics.
Table 2. BDNF levels of different point times and antidepressant treatment.
| Study | Drug group | Dose | Sample | Outcome | BL | 1 week | 2 week | 4 week | 6 week | 8 week | 12 week |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mikoteit | Duloxetine (SNRI) | 65.8±16.1mg/day | Serum | BDNF | 5.01±3.64 | 8.66±5.93 | 11.03±8.0 | 7.3±5.6 | |||
| HDRS | 22.2±4.9 | 16.8±7.5 | 13.8±7.5 | 9.0±6.6 | |||||||
| Ghosh | Fluoxetine (SSRI) | 20mg/day | Plasma | BDNF | 775.32±30.38 | N/A | 850.3±24.92 | ||||
| HDRS | 19±4.09 | 12.2±4.58 | 9.24±3.98 | ||||||||
| Venlafaxine (SNRI) | 50mg/day | Plasma | BDNF | 760.5±28.53 | N/A | 845.8±32.82 | |||||
| HDRS | 18±3.75 | 13.5±3.86 | 10±3.75 | ||||||||
| Yoshimura | Paroxetin (SSRI) | 30.5±12.4 mg/day | Serum | BDNF | 8.6±7.2 | 9.2±6.1 | 11.2±8.4 | ||||
| Sertraline (SSRI) | 76.7±24.0mg/day | HDRS | 21.0±4.3 | 13.8±4.9 | 10.0±5.6 | ||||||
| Fluvoxamin (SSRI) | 100±26.3 mg/day | ||||||||||
| Martocchia | Escitalopram (SSRI) | 10mg/day | Serum | BDNF | 11.5±0.6 | 16.0±2.7 | |||||
| GDS | 9.6±3.4 | 6.4±3.6 | |||||||||
| Brunoni | Sertraline (SSRI) | 50mg/day | plasma | BDNF | 1331±786 | 1620±672 | |||||
| HDRS | 22.0±4.0 | 14.0±8.0 | |||||||||
| Munno | Paroxetin (SSRI) | 20-50mg/day | Serum | BDNF | 14.87±2.9 | 14.69±1.6 | |||||
| HDRS | 19.20±1.83 | 12.44±2.40 | |||||||||
| Plasma | BDNF | 231.45±90.08 | 312.95±109.42 | ||||||||
| HDRS | 19.20±1.83 | 12.44±2.40 | |||||||||
| Ladea | Escitalopram(SSRI) | 10mg/day | Serum | BDNF | 35.6±12.7 | 34.7±11.8 | 35.7±13.2 | ||||
| MADRS | 29.6±2.3 | ||||||||||
| Deuschle | Venlafaxine (SNRI) | 203±47mg/day | Serum | BDNF | 7.82±3.75 | 7.18±5.64 | |||||
| HDRS | 23.0±4.5 | 7.4±5.3 | |||||||||
| Mirtazapine | 46±9mg/day | BDNF | 7.64±6.23 | 8.50±5.37 | |||||||
| HDRS | 22.7±4.2 | 8.9±6.0 | |||||||||
| Dreimüller | SSNRI, SNRI, TCA, Mirtazapine, Tranylcypromine | N/A | Plasma | BDNF | 298±196 | 334±157 | |||||
| HDRS | 19 | 12 | |||||||||
| Wolkowitz | Escitalopram (SSRI) | 10-20mg/day | Serum | BDNF | 15.28 ± 3.55 | 17.46 ± 3.96 | |||||
| HDRS | 31.2 ± 7.9 | 14.5 ± 11.2 | |||||||||
| Sertraline (SSRI) | 50-200mg/day | BDNF | 14.43 ± 7.12 | 20.77 ± 10.15 | |||||||
| HDRS | 19.2 ± 4.0 | 9.7 ± 4.9 | |||||||||
| Rojas | Venlafaxine (SNRI) | 75mg/day | Serum | BDNF | 12.2±9.95 | 8.85±2.44 | |||||
| HDRS | 22.8±3.65 | 11.43±1.48 | |||||||||
| Matrisciano | Sertraline (SSRI) | 96.4±50.8 mg/day | Serum | BDNF | 29.4±12.6 | 50.6±14.2 | |||||
| HDRS | 19±5.3 | N/A | |||||||||
| Escitalopram (SSRI) | 16.4±3.8 mg/day | BDNF | 44.4±16.4 | 38.6±14.4 | |||||||
| HDRS | 14.3±5.9 | N/A | |||||||||
| Venlafaxine (SNRI) | 150±61 mg/day | BDNF | 32.3±14.0 | 29.1±16.3 | |||||||
| HDRS | 19.4±4.5 | N/A | |||||||||
| Piccinni | Citalopram, Sertraline, Paroxetine, Amitriptyline, Imipramine, Trimipramine, Desipramine | N/A | Serum | BDNF | 19.3±8.8 | 22.09±8.37 | 24.46±9.92 | ||||
| HDRS | 22.8±5.3 | ||||||||||
| Plasma | BDNF | 290.0±190.0 | 444.8±20.95 | 456.3±19.85 | |||||||
| HDRS | 22.8±5.3 | ||||||||||
| Huang | Mirtazapine. Fluoxetine, Paroxetine, Venlafaxine | N/A | Serum | BDNF | 10.7±7.3 | 12.0±8.9 | |||||
| HDRS | 35.1±4.9 | 12.1±10.8 | |||||||||
| Hellweg | Amitriptyline (TCA) | 150mg/day | Serum | BDNF | 13.001±3.744 | 15.18±5.98 | |||||
| HDRS | 23.8±5.1 | 11.0±8.1 | |||||||||
| Paroxetine (SSRI) | 40mg/day | BDNF | 13.250±5.112 | 12.02±4.85 | |||||||
| HDRS | 22.6±3.9 | 11.7±8.4 | |||||||||
| Yoshimura | Paroxetine (SSRI) | 31±13mg/day | Serum | BDNF | 9.4±7.9 | 10.4±8.2 | 17.9±7.6 | ||||
| HDRS | 24±7 | ||||||||||
| Milnacipran (SNRI) | 83±31mg/day | BDNF | 9.8±9.7 | 10.3±7.5 | 15.8±8.1 | ||||||
| HDRS | 23±6 | ||||||||||
| Aydemir | Escitalopram (SSRI) | 10 mg/day | Serum | BDNF | 27.68±13.74 | 38.57±15.30 | |||||
| HDRS | 39.75±7.40 | 9.31±6.05 | |||||||||
| Gonul | Fluoxetine, Venlafaxine | N/A | Serum | BDNF | 20.8±6.7 | 33.3±9.89 | |||||
| HDRS | 27.28±3.53 | 8.85±3.15 | |||||||||
| Aydemir | Venlafaxine (SNRI) | 75 mg/day | Serum | BDNF | 17.9±9.1 | 34.6±7.1 | |||||
| HDRS | 23.2±4.6 | 8.2±3.9 | |||||||||
| Shimizu | Amoxapine, Milnacipran, Paroxetine | N/A | Serum | BDNF | 13.32±11.97 | 28.79±6.23 | |||||
| HDRS | 33.5±10.5 | 2.8±1.0 | |||||||||
BDNF concentration: Serum, ng/ml; Plasma, pg/ml. SSRI, Selective Serotonin Reuptake Inhibitor. SNRI, selective noradrenalin reuptake inhibitors. TCA, tricyclic antipsychotics.
Studies of antidepressants types
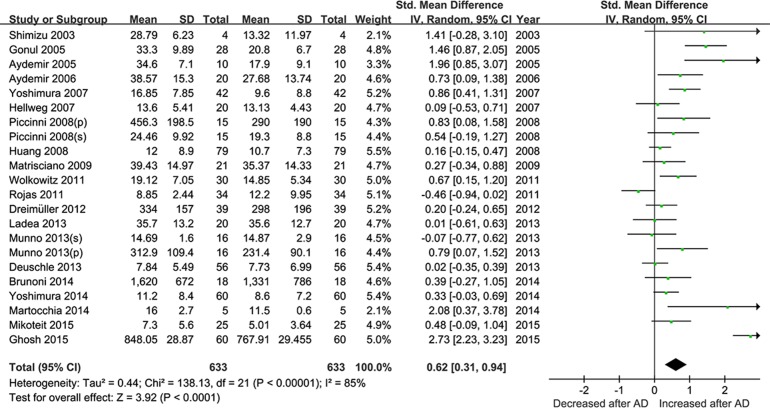
The twenty studies were pooled together to assess the effect of antidepressant drugs on the BDNF levels before and after treatment. The random effects model was applied, and a pooled analysis of 20 studies showed a significant effect of antidepressants therapy on elevation of BDNF levels (SMD = 0.62, 95% CI = 0.31–0.94, Z = 3.92, P<0.0001; Fig 2), as well as depressive symptoms amelioration with a significant decreased HDRS score (SMD = 2.78, 95% CI = 2.31–3.26, Z = 11.57, P < 0.00001; Fig 3). I2 were respectively 85%and 83% suggesting strong heterogeneity.
Fig 2. Meta-Analyses for the levels of BDNF pre- and post- antidepressant drugs treatment (less than 12 week).
Fig 3. Meta-Analyses for the improvement of depressive symptoms after ADs (less than 12 week).
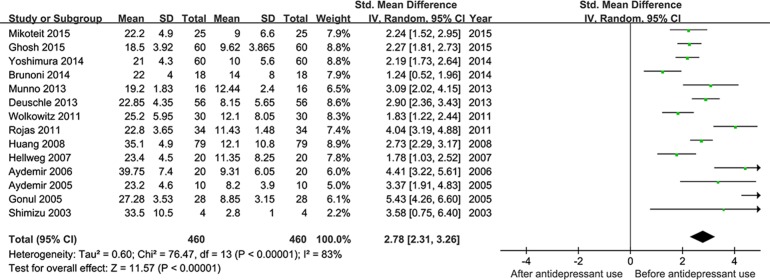
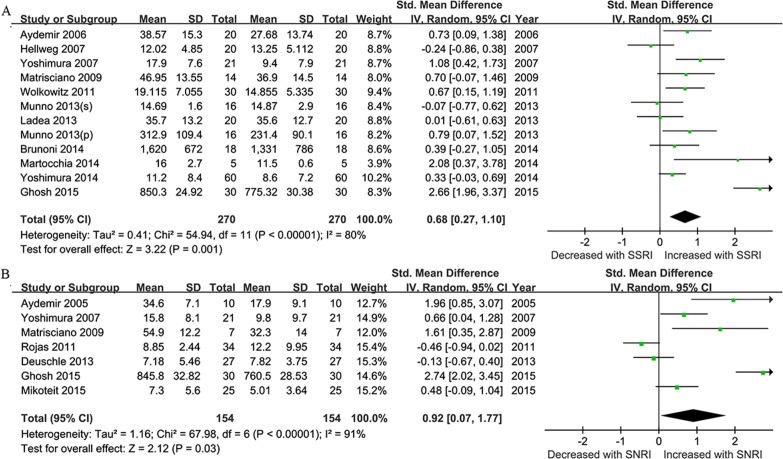
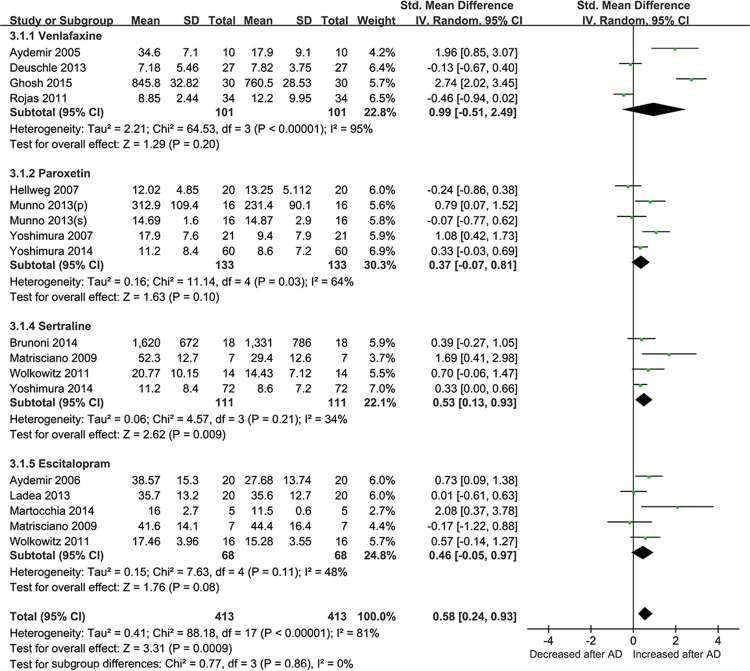
We next conducted an analysis from the studies based on the antidepressant drugs use. After stratification with SSRIs and SNRIs, the effect size as the changes in BDNF concentrations pre and post-treatment was 0.68 for SSRIs (95% CI = 0.27–1.10, Z = 3.22, P = 0.001; Fig 4A), and 0.92 for SNRIs (95% CI = 0.07–1.77, Z = 2.12, P = 0.03; Fig 4B). Then efficacy of differential drugs on the BDNF levels after treatment was analyzed. ADs that were only reported in single studies (fluoxetine, duloxetine, mirtazapine, amitriptyline, and milnacipran) or used in combination were excluded. Finally, four types of antidepressants (venlafaxine, paroxetine, sertraline and escltalopram) were analyzed for ease of analysis. According to the SMD and 95%CIs, sertraline showed a statistically significant effect on the BDNF levels pre- and post ADs treatment (SMD = 0.53,95% CI = 0.13–0.93, Z = 2.62, P = 0.009), while no evidence for paroxetine, sertraline and escltalopram in BDNF changes was observed (Fig 5)
Fig 4. Antidepressants- Stratified Subgroup Meta-Analyses.
Forest plots showing the summary effect sizes for levels of BDNF pre- and post- different kind of antidepressant drugs treatment (less than 12 week). (A) using SSRIs;(B) using SNRIs.
Fig 5. Meta-Analyses for the levels of BDNF pre- and post- antidepressant with differenti drugs treatment (less than 12 week).
Forest plots showing summary effect sizes of differential antidepressants (venlafaxine, paroxetine, sertraline and escitalopram) on BDNF concentration changes
Heterogeneity and moderation analyses
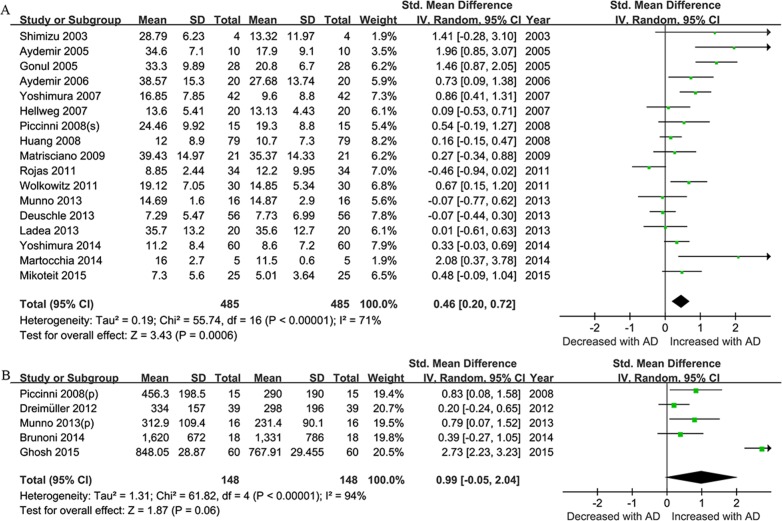
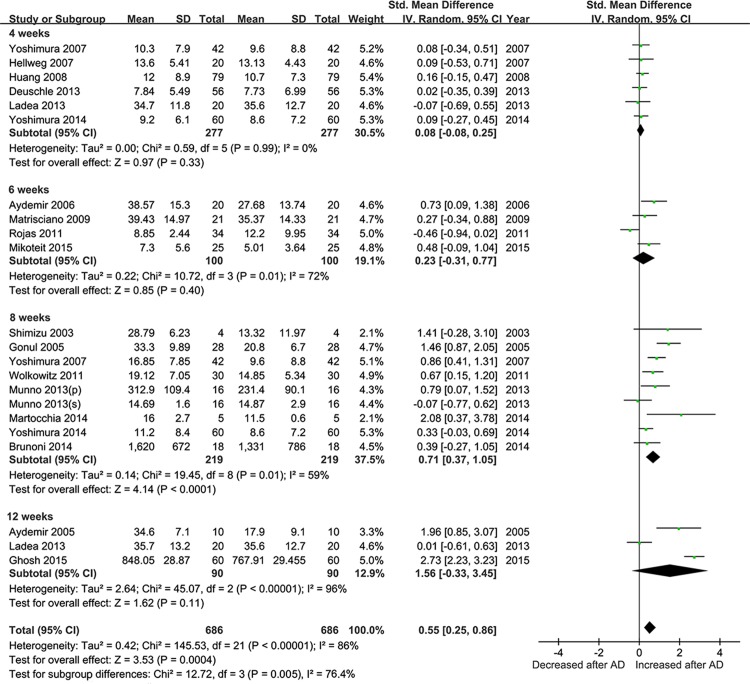
We performed the subgroup analysis based on the clinical samples used. Of all the included studies, seventeen described the alteration of BDNF levels in serum and five in plasma. The sample-stratified analysis indicated a significant higher level of BDNF concentration post-treatment with an effect-size estimate in serum (SMD = 0.46, 95% CI = 0.20–0.72, Z = 3.43, P = 0.0006), which was not observed in plasma (Fig 6). In the subgroup meta-analysis based on length of treatment, a statistically significant overall effect size was observed after 8 weeks of antidepressants treatment (SMD = 0.71, 95% CI = 0.37–1.05, Z = 4.14, P < 0.0001) for the elevation of BDNF levels (Fig 7).
Fig 6. Sample- Stratified Subgroup Meta-Analyses.
Forest plots showing the summary effect sizes for levels of BDNF pre- and post- antidepressant drugs treatment (less than 12 week) in serum (A) or plasma(B).
Fig 7. Meta-Analyses for BDNF concentrations at different treatment time points during antidepressants treatment (less than 12 week).
Forest plots showing the summary effect sizes for BDNF concentration changes at 4 weeks, 6 weeks, 8 weeks, and 12 weeks.
Sensitivity and publication bias
Sensitivity analyses were conducted using the leave-one-out method by removing studies one by one to assess the degree to which each individual study influenced the results of the overall analysis. The results of the sensitivity analysis confirmed that no single study influenced the pooled SMDs. No strong statistical evidence for publication bias was observed in Egger׳s test (all P>0.05).
Discussion
In the present study, we summarized the existing literature and conducted a systematic analysis to evaluate the association between BDNF levels and antidepressant drug treatment. We included 20 studies that described comparisons of average BDNF levels pre- and post-antidepressant treatment with SSRIs, SNRIs, TCAs et al. First, we performed systematic meta-analyses and found that subjects with MDD had significantly higher BDNF concentrations after a short-term period (less than 12 weeks) of antidepressants treatment, accompanied by reduced HDRS scores. Consistent with previous works by Molendijk et al, lower serum BDNF in MDD could be normalized during antidepressant treatment [10]. Although we did not discuss whether BDNF concentration was correlated with depressive symptom alleviation, a significant negative relevance between depressive symptom alleviation and BDNF concentrations has been reported [13].
Molendijk et al. previously observed that the use of SSRIs was related to the increase in serum BDNF levels, which suggested that increases in serum levels of BDNF during antidepressant treatment appear to be confined to some antidepressants [10]. To uncover potential differences between various classes of antidepressants, we compared BDNF levels in MDD after SSRIs and SNRIs treatment. In our present study, we found that not only SSRIs but also SNRIs could increase BDNF levels over the course of antidepressant treatment. Making comparisons of four ADs by performing meta-analyses, only sertraline (but not venlafaxine, paroxetine or escitalopram) increased the BDNF levels. Fluoxetine was not analyzed because there was only one study that reported detailed data involving fluoxetine and BDNF.
Length of antidepressants treatment from 4 to 12 weeks was analyzed for contributions to the origin of the heterogeneity in our subgroup meta-analysis, and antidepressants had significant effect on the increase in BDNF concentration after 8 weeks of treatment. Notably, the temporal correlation between serum BDNF levels and the antidepressant effect is not direct: ketamine and ECT treatment increase serum BDNF levels only gradually while their antidepressant effect appears to be quick. While response to ADs treatment in depression was mostly chronic, with subjects in most studies still presenting with depressive symptoms at follow-up, the effect of antidepressant drugs on the BDNF levels may take a long time [40].
After stratifying the subgroup analyses based on clinical blood sampling, serum BDNF levels (as opposed to plasma levels) increased significantly after ADs treatment, while the plasma BDNF levels did not show significant differences; however, a high level of heterogeneity still existed. The significances of the lower BDNF levels in the peripheral blood from subjects with depression were recently reported worldwide in many clinical studies. However, the underlying mechanisms remained unclear. BDNF in the plasma or serum could be released from blood platelets [41, 42]; on the other hand, BDNF could be derived from the brain across the blood-brain-barrier (BBB)[43,44]. Increases in serum BDNF levels with antidepressant treatment have been reported in multiple human and preclinical studies. Chronic administration of ADs could increase the expression of BDNF mRNA and protein in the prefrontal cortex, hippocampus, and other emotion-processing related regions [45–47]. In the overall meta-analysis, we found that the administration of ADs could alleviate the depressive symptoms, and increase the BDNF levels after a time period ranging from 2 to 12 weeks, indicating that changes in serum BDNF levels were significantly correlated with antidepressant treatment. Our subgroup-analysis results suggest that serum BDNF levels increased over the course of antidepressant treatment which was consistent with previous work, while plasma BDNF levels were not observed to be correlated with antidepressant treatment. Our results showed that the detection of BDNF in serum appears to be more reliable.
Mature brain-derived neurotrophic factor (BDNF) is initially synthesized and converted from its precursor protein proBDNF by tPA and extracellular proteases such as matrix metalloproteinase-9 (MMP-9)[48–50]. Both mature BDNF and proBDNF were proved to have important biological function in the pathology of psychiatric disorders such as MDD [51–53]. Mature BDNF and proBDNF in human blood could be distinguished with specific antibody by Western Blotting method. In fact, peripheral BDNF levels were mostly measured using an unspecific antibody BDNF ELISA kits for a larger sample size more conveniently and accurately. However, it was difficult to distinguish between proBDNF and mature BDNF in the ELISA kits due to the limited specificity of the BDNF antibody. A work by Yoshida et al. found that serum levels of mature BDNF, but not proBDNF were significantly lower in patients with MDD [54]. Serum mature BDNF levels in the MDD patients were significantly lower than those in the healthy controls, while no difference was found in serum proBDNF [55]. Therefore, it is likely that mature BDNF contributes to the decreased levels of BDNF in patients with MDD [17].
There exist some possible determinants that could influence serum BDNF. Serum BDNF concentrations systematically vary over the year, and decrease significantly over the autumn-winter period (Jan to May) while increasing in the spring-summer period [56]. Furthermore, other factors such as sampling, the number of sunlight hours, socio-demographics, lifestyle indicators, and disease can influence BDNF levels in humans [56–57]. In our meta-analyses, because of the limited information obtained from each included study, only the sample using and length of treatment duration were analyzed and shown to be potential factors that contribute to the pooled effects and the heterogeneity between studies. Nonetheless, serum levels of BDNF in humans may be influenced by seasonal variation, sex, sunshine hours, blood withdrawal, storage, smoking status, and food and alcohol intake [10, 56, 57].
There are several other limitations with respect to our findings. Firstly, we considered a treatment period within 12 weeks for BDNF analysis. Some ADs may take longer to affect BDNF levels once the depressive symptoms have improved. Secondly, BDNF is a hot topic in depression research worldwide. We only included the English studies in our meta-analysis, which may be a source of publication bias although no such publication bias was found in our meta-analysis. Thirdly, some ADs such as fluoxetine, duloxetine, mirtazapine, amitriptyline, and milnacipran were only reported in single study, so it was difficult to estimate their true effects on the increase of BDNF levels in our analyses. It is important to point out here that these drugs were reported to increase BDNF levels in their respective studies. In some clinical studies, drugs were used in combination which may explain the observed heterogeneity. In addition, drug dose of antidepressant should be analyzed as a modifier for changes of BDNF levels. Due to the limited information and a wide variation in dose, it is difficult to define and divide the dose, so the analysis was not able to be carried out.
In summary, our meta-analyses of 20 studies related to depression provided evidence that peripheral BDNF levels are increased during the course of antidepressant drug treatment (SSRIs and SNRIs). Our study also provided further evidence of the possible mechanisms and effects of different ADs on BDNF levels. Peripheral BDNF levels are better documented in serum than in plasma which would be useful in future research studies of BDNF and antidepressant treatment. Sertraline was shown to increase BDNF levels after a short-term period of treatment, and may be a good candidate for the exploration of ADs pharmacological mechanisms related to peripheral BDNF.
Supporting information
(DOC)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The work was supported by Scientific and Technological Research Program of Chongqing Municipal Education Commission (grant no. KJ1600223).
References
- 1.Belmaker R H, Agam G. Major depressive disorder. N Eng J Med. 2008, 358(1): 55–68. [DOI] [PubMed] [Google Scholar]
- 2.Otte C, Gold S M, Penninx B W, Pariante CM, Etkin A, Fava M, et al. Major depressive disorder. Nat Rev Dis Primers. 2016, 2: 16065 10.1038/nrdp.2016.65 [DOI] [PubMed] [Google Scholar]
- 3.Radecki D T, Brown L M, Martinez J, Teyler TJ. BDNF protects against stress‐induced impairments in spatial learning and memory and LTP. Hippocampus. 2005, 15(2): 246–253. 10.1002/hipo.20048 [DOI] [PubMed] [Google Scholar]
- 4.Lu B. BDNF and activity-dependent synaptic modulation. Learning Mem. 2003, 10(2): 86–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lindsay R M. Nerve growth factors (NGF, BDNF) enhance axonal regeneration but are not required for survival of adult sensory neurons. J Neurosci. 1988, 8(7): 2394–2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Martinowich K, Manji H, Lu B. New insights into BDNF function in depression and anxiety. Nat Neuroscir. 2007, 10(9): 1089–1093. [DOI] [PubMed] [Google Scholar]
- 7.Castrén E, Rantamäki T. The role of BDNF and its receptors in depression and antidepressant drug action: Reactivation of developmental plasticity. Dev Neurobiol. 2010, 70(5): 289–297. 10.1002/dneu.20758 [DOI] [PubMed] [Google Scholar]
- 8.Lee BH, Kim YK. The roles of BDNF in the pathophysiology of major depression and in antidepressant treatment. Psychiatry Investig. 2010, 7(4): 231–235. 10.4306/pi.2010.7.4.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karege F, Perret G, Bondolfi G, Schwald M, Bertschy G, Aubry JM. Decreased serum brain-derived neurotrophic factor levels in major depressed patients. Psychiatry Res. 2002, 109(2): 143–148. [DOI] [PubMed] [Google Scholar]
- 10.Molendijk M L, Bus B A A, Spinhoven P, Penninx BW, Kenis G, Prickaerts J, et al. Serum levels of brain-derived neurotrophic factor in major depressive disorder: state–trait issues, clinical features and pharmacological treatment. Mol Psychiatry. 2011, 16(11): 1088–1095. 10.1038/mp.2010.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee B H, Kim H, Park S H, Kim YK. Decreased plasma BDNF level in depressive patients. J Affect Disord. 2007, 101(1): 239–244. [DOI] [PubMed] [Google Scholar]
- 12.Bus B A A, Molendijk M L, Tendolkar I, Penninx BW, Prickaerts J, Elzinga BM, et al. Chronic depression is associated with a pronounced decrease in serum brain-derived neurotrophic factor over time. Mol Psychiatry. 2015, 20(5): 602–608. 10.1038/mp.2014.83 [DOI] [PubMed] [Google Scholar]
- 13.Molendijk M L, Spinhoven P, Polak M, Bus BA, Penninx BW, Elzinga BM. Serum BDNF concentrations as peripheral manifestations of depression: evidence from a systematic review and meta-analyses on 179 associations. Mol Psychiatry. 2014, 19(7): 791–800. 10.1038/mp.2013.105 [DOI] [PubMed] [Google Scholar]
- 14.Brunoni A R, Lopes M, Fregni F. A systematic review and meta-analysis of clinical studies on major depression and BDNF levels: implications for the role of neuroplasticity in depression. Int J Neuropsychopharmacol. 2008, 11(8): 1169–1180. 10.1017/S1461145708009309 [DOI] [PubMed] [Google Scholar]
- 15.Yoshimura R, Kishi T, Hori H, Atake K, Katsuki A, Nakano-Umene W, et al. Serum proBDNF/BDNF and response to fluvoxamine in drug-naïve first-episode major depressive disorder patients. Ann Gen Psychiatry. 2014, 13(1): 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Piccinni A, Marazziti D, Catena M, Domenici L, Del Debbio A, Bianchi C, et al. Plasma and serum brain-derived neurotrophic factor (BDNF) in depressed patients during 1 year of antidepressant treatments. J Affect Disord. 2008, 105(1): 279–283. [DOI] [PubMed] [Google Scholar]
- 17.Mikoteit T, Beck J, Hemmeter U M, Brand S, Schimitt K, Bischof R, et al. Mature brain-derived neurotrophic factor (BDNF) is the major player of total BDNF in serum regarding prediction of antidepressant treatment outcome. Psychopharmacology. 2016, 233(1): 153–155. 10.1007/s00213-015-4088-6 [DOI] [PubMed] [Google Scholar]
- 18.Polyakova M, Schroeter M L, Elzinga B M, Holiga S, Schioenknecht P, de Kloet ER, et al. Brain-derived neurotrophic factor and antidepressive effect of electroconvulsive therapy: systematic review and meta-analyses of the preclinical and clinical literature. PLoS one. 2015, 10(11): e0141564 10.1371/journal.pone.0141564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Matrisciano F, Bonaccorso S, Ricciardi A, Scaccianoce S, Panaccione I, Wang L, et al. Changes in BDNF serum levels in patients with major depression disorder (MDD) after 6 months treatment with sertraline, escitalopram, or venlafaxine. J Psychiatr Res. 2009, 43(3): 247–254. 10.1016/j.jpsychires.2008.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Başterzi A D, Yazici K, Aslan E, Delialioglu N, Tasdelen B, Tot Acar S, et al. Effects of fluoxetine and venlafaxine on serum brain derived neurotrophic factor levels in depressed patients. Prog Neuropsychopharmacol Biol Psychiatry. 2009, 33(2): 281–285. 10.1016/j.pnpbp.2008.11.016 [DOI] [PubMed] [Google Scholar]
- 21.Mikoteit T, Hemmeter U, Eckert A, Brand S, Bischof R, Delini-Stula A, et al. Improved alertness is associated with early increase in serum brain-derived neurotrophic factor and antidepressant treatment outcome in major depression. Neuropsychobiology. 2015, 72(1): 16–28. 10.1159/000437439 [DOI] [PubMed] [Google Scholar]
- 22.Ghosh R, Gupta R, Bhatia MS, Tripathi AK, Gupta LK. Comparison of efficacy, safety and brain derived neurotrophic factor (BDNF) levels in patients of major depressive disorder, treated with fluoxetine and desvenlafaxine. Asian J Psychiatr. 2015, 18: 37–41. 10.1016/j.ajp.2015.10.006 [DOI] [PubMed] [Google Scholar]
- 23.Yoshimura R, Kishi T, Hori H, Katsuki A, Sugita-Ikenouchi A, Umene-Nakano W, et al. Serum levels of brain-derived neurotrophic factor at 4 weeks and response to treatment with ssris. Psychiatry Investig. 2014, 11(1): 84–88. 10.4306/pi.2014.11.1.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martocchia A, Curto M, Scaccianoce S, Comite F, Xenos D, Nasca C, et al. Effects of escitalopram on serum BDNF levels in elderly patients with depression: a preliminary report. Aging Clin Exp Res. 2014, 26(4): 461–464. 10.1007/s40520-014-0194-2 [DOI] [PubMed] [Google Scholar]
- 25.Munno D, Sterpone S, Fania S, Cappellin F, Mengozzi G, Saroldi M, et al. Plasma brain derived neurotrophic factor levels and neuropsychological aspects of depressed patients treated with paroxetine. Panminerva Med. 2013, 55(4): 377–384. [PubMed] [Google Scholar]
- 26.Ladea M, Bran M. Brain derived neurotrophic factor (BDNF) levels in depressed women treated with open-label escitalopram. Psychiatr Danub. 2013, 25: 128–132. [PubMed] [Google Scholar]
- 27.Deuschle M, Gilles M, Scharnholz B, Lederbogen F, Lang UE, Hellweg R. Changes of serum concentrations of brain-derived neurotrophic factor (BDNF) during treatment with venlafaxine and mirtazapine: role of medication and response to treatment. Pharmacopsychiatry. 2013, 46(02): 54–58. [DOI] [PubMed] [Google Scholar]
- 28.Dreimüller N, Schlicht K F, Wagner S, Peetz D, Borysenko L, Hiemke C, et al. Early reactions of brain-derived neurotrophic factor in plasma (pBDNF) and outcome to acute antidepressant treatment in patients with Major Depression. Neuropharmacology. 2012, 62(1): 264–269. 10.1016/j.neuropharm.2011.07.017 [DOI] [PubMed] [Google Scholar]
- 29.Wolkowitz O M, Wolf J, Shelly W, Rosser R, Burke HM, Lerner GK, et al. Serum BDNF levels before treatment predict SSRI response in depression. Prog Neuropsychopharmacol Biol Psychiatry. 2011, 35(7): 1623–1630. 10.1016/j.pnpbp.2011.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rojas PS, Fritsch R, Rojas RA, Jara P, Fiedler JL. Serum brain-derived neurotrophic factor and glucocorticoid receptor levels in lymphocytes as markers of antidepressant response in major depressive patients: a pilot study. Psychiatry Res. 2011, 189(2): 239–245. 10.1016/j.psychres.2011.04.032 [DOI] [PubMed] [Google Scholar]
- 31.Piccinni A, Marazziti D, Catena M, Domenici L, Del Debbio A, Binanchi C, et al. Plasma and serum brain-derived neurotrophic factor (BDNF) in depressed patients during 1 year of antidepressant treatments[. J Affect Disord. 2008, 105(1): 279–283. [DOI] [PubMed] [Google Scholar]
- 32.Huang T L, Lee CT, Liu YL. Serum brain-derived neurotrophic factor levels in patients with major depression: effects of antidepressants. J Psychiatr Res. 2008, 42(7): 521–525. 10.1016/j.jpsychires.2007.05.007 [DOI] [PubMed] [Google Scholar]
- 33.Hellweg R, Ziegenhorn A, Heuser I, Deuschle M. Serum concentrations of nerve growth factor and brain-derived neurotrophic factor in depressed patients before and after antidepressant treatment. Pharmacopsychiatry. 2008, 41(02): 66–71. [DOI] [PubMed] [Google Scholar]
- 34.Yoshimura R, Mitoma M, Sugita A, Hori H, Okamoto T, Umene W, et al. Effects of paroxetine or milnacipran on serum brain-derived neurotrophic factor in depressed patients. Prog Neuropsychopharmacol Biol Psychiatry. 2007, 31(5): 1034–1037. 10.1016/j.pnpbp.2007.03.001 [DOI] [PubMed] [Google Scholar]
- 35.Aydemir C, Yalcin ES, Aksaray S, Kisa C, Yildirim SG, Uzbay T, et al. Brain-derived neurotrophic factor (BDNF) changes in the serum of depressed women. Prog Neuropsychopharmacol Biol Psychiatry. 2006, 30(7): 1256–1260. 10.1016/j.pnpbp.2006.03.025 [DOI] [PubMed] [Google Scholar]
- 36.Gonul A S, Akdeniz F, Taneli F, Donat O, Eker C, Vahip S. Effect of treatment on serum brain–derived neurotrophic factor levels in depressed patients. Eur Arch Psychiatry Clin Neurosci. 2005, 255(6): 381–386. 10.1007/s00406-005-0578-6 [DOI] [PubMed] [Google Scholar]
- 37.Aydemir O, Deveci A, Taneli F. The effect of chronic antidepressant treatment on serum brain-derived neurotrophic factor levels in depressed patients: a preliminary study. Prog Neuropsychopharmacol Biol Psychiatry. 2005, 29(2): 261–265. 10.1016/j.pnpbp.2004.11.009 [DOI] [PubMed] [Google Scholar]
- 38.Shimizu E, Hashimoto K, Okamura N, Koike K, Komatsu N, Kumakiri C, et al. Alterations of serum levels of brain-derived neurotrophic factor (BDNF) in depressed patients with or without antidepressants. Biol Psychiatry. 2003, 54(1): 70–75. [DOI] [PubMed] [Google Scholar]
- 39.Brunoni AR, Machado-Vieira R, Zarate CA Jr, Vieira EL, Vanderhasselt MA, Nitche MA, et al. BDNF plasma levels after antidepressant treatment with sertraline and transcranial direct current stimulation: results from a factorial, randomized, sham-controlled trial. Eur Neuropsychopharmacol. 2014, July, 24(7): 1144–1151. 10.1016/j.euroneuro.2014.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bus BA, Molendijk ML, Tendolkar I, Peeninx BW, Prickaerts J, Elzinga BM, et al. Chronic depression is associated with a pronounced decrease in serum brain-derived neurotrophic factor over time. Mol Psychiatry.2015, 20 (5):602–608. 10.1038/mp.2014.83 [DOI] [PubMed] [Google Scholar]
- 41.Karege F, Bondolfi G, Gervasoni N, Schwald M, Aubry JM, Bertschy G. Low brain-derived neurotrophic factor (BDNF) levels in serum of depressed patients probably results from lowered platelet BDNF release unrelated to platelet reactivity. Biol Psychiatry. 2005, 57(9): 1068–1072. 10.1016/j.biopsych.2005.01.008 [DOI] [PubMed] [Google Scholar]
- 42.Lommatzsch M, Zingler D, Schuhbaeck K, Schloetcke K, Zingler C, Schuff-Werner P, et al. The impact of age, weight and gender on BDNF levels in human platelets and plasma. Neuobiol Aging. 2005, 26(1): 115–123. [DOI] [PubMed] [Google Scholar]
- 43.Pan W, Banks WA, Fasold MB, Bluth J, Kastin AJ. Transport of brain-derived neurotrophic factor across the blood–brain barrier. Neuropharmacology. 1998, 37(12): 1553–1561. [DOI] [PubMed] [Google Scholar]
- 44.Poduslo JF, Curran GL. Permeability at the blood-brain and blood-nerve barriers of the neurotrophic factors: NGF, CNTF, NT-3, BDNF. Brain Res Mol Brain Res. 1996, 36(2): 280–286. [DOI] [PubMed] [Google Scholar]
- 45.Castrén E, Rantamäki T. The role of BDNF and its receptors in depression and antidepressant drug action: Reactivation of developmental plasticity. Dev Neurobiol. 2010, 70(5): 289–297. 10.1002/dneu.20758 [DOI] [PubMed] [Google Scholar]
- 46.Nibuya M, Morinobu S, Duman RS. Regulation of BDNF and trkB mRNA in rat brain by chronic electroconvulsive seizure and antidepressant drug treatments. J Neurosci. 1995, 15(11): 7539–7547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Balu DT, Hoshaw BA, Malberg JE, Rosenzweig-Lipson S, Schechter le, Lucki I. Differential regulation of central BDNF protein levels by antidepressant and non-antidepressant drug treatments. Brain Res. 2008, 1211: 37–43. 10.1016/j.brainres.2008.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hashimoto K. Brain‐derived neurotrophic factor as a biomarker for mood disorders: an historical overview and future directions. Psychiatry Clin Neurosci. 2010, 64(4): 341–357. 10.1111/j.1440-1819.2010.02113.x [DOI] [PubMed] [Google Scholar]
- 49.Greenberg ME, Xu B, Lu B, Hempstead BL. New insights in the biology of BDNF synthesis and release: implications in CNS function. J Neurosci. 2009, 29(41): 12764–12767. 10.1523/JNEUROSCI.3566-09.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pang PT, Teng HK, Zaitsev E, Woo NT, Sakata K, Zhen S, et al. Cleavage of proBDNF by tPA/plasmin is essential for long-term hippocampal plasticity. Science. 2004, 306(5695): 487–491. 10.1126/science.1100135 [DOI] [PubMed] [Google Scholar]
- 51.Hashimoto K. BDNF variant linked to anxiety‐related behaviors. Bioessays. 2007, 29(2): 116–119. 10.1002/bies.20534 [DOI] [PubMed] [Google Scholar]
- 52.Lu B. Pro-region of neurotrophins: role in synaptic modulation. Neuron. 2003, 39(5): 735–738. [DOI] [PubMed] [Google Scholar]
- 53.Teng HK, Teng KK, Lee R, Wright S, Tevar S, Almeida RD, et al. ProBDNF induces neuronal apoptosis via activation of a receptor complex of p75NTR and sortilin. J Neurosci. 2005, 25(22): 5455–5463. 10.1523/JNEUROSCI.5123-04.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yoshida T, Ishikawa M, Niitsu T, Nakazato M, Watanabe H, Shiraishi T, et al. Decreased serum levels of mature brain-derived neurotrophic factor (BDNF), but not its precursor proBDNF, in patients with major depressive disorder. PLoS one. 2012, 7(8): e42676 10.1371/journal.pone.0042676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yoshimura R, Kishi T, Hori H, Atake K, Katsuki A, Nakano-Umene W, et al. Serum proBDNF/BDNF and response to fluvoxamine in drug-naïve first-episode major depressive disorder patients. Ann Gen Psychiatry. 2014, 13(1): 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Molendijk ML, Haffmans J P, Bus B AA, Spinhoven P, Penninx BW, Prickaerts J, et al. Serum BDNF concentrations show strong seasonal variation and correlations with the amount of ambient sunlight. PLoS one. 2012, 7(11): e48046 10.1371/journal.pone.0048046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bus B AA, Molendijk ML, Penninx B, Buitelaar JK, Kenis G, Prickaerts J, et al. Determinants of serum brain-derived neurotrophic factor. Psychoneuroendocrinology. 2011, 36(2): 228–239. 10.1016/j.psyneuen.2010.07.013 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.