ABSTRACT
Background: Migrant health is receiving increasing international attention, reflecting recognition of the health inequities experienced among many migrant populations and the need for health systems to adapt to diverse migrant populations. In the Greater Mekong Subregion (GMS) there is increasing migration associated with uneven economic integration and growth, socio-economic vulnerabilities, and disparities between countries. There has been limited progress, however, in improving migrant access to health services in the Subregion. This paper examines the health needs, access barriers, and policy responses to cross-border migrants in five GMS countries.
Methods: A review of published literature and research was conducted on migrant health and health service access in Cambodia, Lao People’s Democratic Republic, Myanmar, Thailand, and Viet Nam, as well as analysis of current migration trends and universal health coverage (UHC) indicators in the Subregion. The review included different migrant types: i.e. migrant workers, irregular migrants, victims of trafficking, refugees and asylum seekers, and casual cross-border migrants.
Results: There is substantial diversity in the capacity of GMS health systems to address migrant populations. Thailand has sought to enhance migrant health coverage, including development of migrant health policies/programs, bilateral migrant worker agreements, and migrant health insurance schemes; Viet Nam provides health protection for emigrant workers. Overall, however, access to good quality health care remains weak for many citizens in GMS countries let alone migrants. Migrant workers – and irregular migrants in particular – face elevated health risks yet are not adequately covered and incur high out-of-pocket (OOP) payments for health services.
Conclusions: UHC implies equity: UHC is only achieved when everyone has the opportunity to access and use good-quality health care. Efforts to achieve UHC in the GMS require deliberate policy decisions to include migrants. The emergence of the UHC agenda, and the focus on migrant health among policy makers and partners, present an opportunity to tackle barriers to health service access, extend coverage, and strengthen partnerships in order to improve migrant health. This is an opportune time for GMS countries to develop migrant-inclusive health systems.
KEYWORDS: Migrant, migration, universal health coverage, Greater Mekong Subregion, South-Eastern Asia, health equity
Background
Migrants and health equity in the Greater Mekong Subregion
Health inequities are common among disadvantaged population subgroups, including migrants, a group who commonly encounter many forms of disadvantage. With increasing population mobility and displacement in our rapidly globalising world, migrants warrant more attention if countries are to meet the Sustainable Development Goals (SDGs) by 2030, in particular Goal 10 which aims to ‘reduce inequality within and among countries’, and Goal 3 that aims to ‘ensure healthy lives and promote well-being for all at all ages’ [1]. Migrants, especially irregular migrants, experience considerable health inequity, defined as ‘unjust and avoidable differences in health that stem from some form of discrimination or lack of access to certain resources’ [2]. Improving health care is a key pathway towards health equity, as set out in SDG target 3.8 which aims to ‘achieve universal health coverage (UHC), including financial risk protection, access to quality essential health care services, and access to safe, effective, quality, and affordable essential medicines and vaccines for all’ [1]. Achieving UHC will require low- and middle-income countries, in particular, to strengthen their health care systems [3] and to pay more attention to the broader goal of health equity [4,5].
In 2010, the Asia-Pacific region had an estimated 27.5 million international migrants and an unknown number of irregular migrants [6]. Yet there has been limited progress in improving migrant health and access to health services, and documents surrounding SDGs and UHC seldom specifically mention migrants. The 2010 Global Consultation on Migrant Health directed attention to the need to develop migrant-sensitive health systems [7], however, and migrants are now receiving more attention under World Health Organization (WHO) regional frameworks for advancing SDGs and UHC in the Asian region [8,9].
Migrant health, however, remains a vexed issue in low- and middle-income countries that struggle to provide adequate health services for their citizens, let alone migrants who are often regarded as having a lesser claim. Cross-border migrants – particularly irregular migrants – are difficult to count, typically have multiple health needs, and are seldom embraced as a responsibility by either origin or destination countries in Asia.
This paper examines the health needs, access barriers, and policy responses of relevance to cross-border migrants in the Greater Mekong Subregion (GMS) (see Figure 1). While the focus is on international migration in the GMS, key messages are relevant to other regions with migrant populations. The paper concentrates on the role of destination-country health systems, drawing on examples from Cambodia, Lao People’s Democratic Republic (Lao PDR), Myanmar, Thailand, and Viet Nam, while recognising that migrant health requires action from both origin countries and destination countries, as well as via bilateral and regional collaborations.
Figure 1.
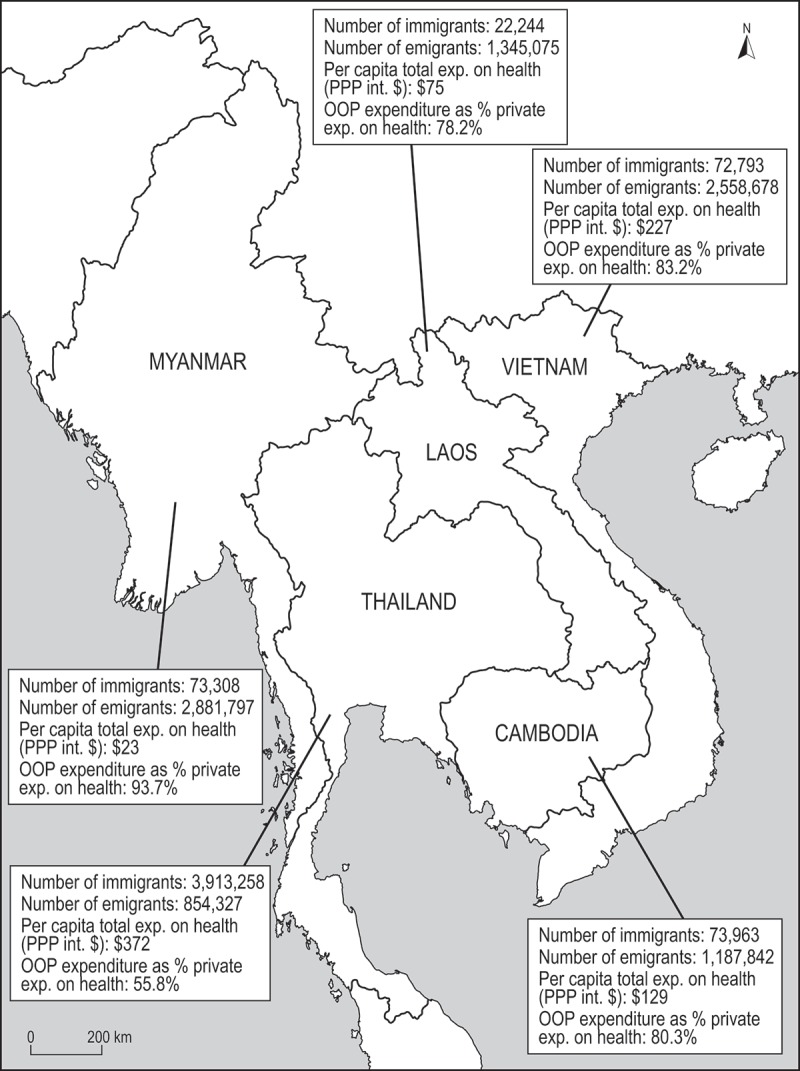
The Greater Mekong Subregion (GMS).
Methods
The paper focuses on international migrants, including international labour migrants and irregular migrants; internal migrants (i.e. people displaced within national boundaries) are not included in the analysis. Five GMS countries are included for analysis: Cambodia, Lao PDR, Myanmar, Thailand, and Viet Nam. The analysis does not include Yunnan Province and Guangxi Zhuang Autonomous Region of Southern China (also regarded as part of the GMS). As this is an emerging area of policy focus and research, a scoping review approach was used. Reviewed literature included published articles, book chapters, reports and publications by international institutions, policy documents, and media articles. The search strategy included Google, Google Scholar, Web of Science, PubMed, and WHO websites. Key search terms were selected based on the focus of the scoping review, and included: (1) ‘migrant’ and specific migrant types (e.g. refugee, labor migrant); (2) Greater Mekong Subregion and the names of the five countries; (3) UHC, universal health coverage, health coverage, health financing, health insurance, out-of-pocket health expenditure, service delivery, and health equity. The references of retrieved publications were checked for relevant literature that was not otherwise identified by the search strategy. Current migration and UHC-related data in the GMS were compiled from relevant sources (e.g. World Bank, WHO). The status of ratification of key international legal instruments on international migration and health was examined for GMS member states, through reference to the United Nations Treaty Collection. Publications were reviewed for information relevant to the topic of migrants and UHC in the GMS, including the health of migrant populations in the subregion and challenges and opportunities for including migrants in UHC efforts. This paper develops the theme of health equity and migrants in the GMS and is informed by a report prepared in 2014 for the WHO Western Pacific Regional Office [19].
Results
Migration in the GMS
The GMS is experiencing increasing migration associated with rapid and uneven regional economic integration and economic growth, socio-economic vulnerabilities, and demographic disparities between countries [20,21]. The GMS countries have increased political and economic engagement through participation in the Association of Southeast Asian Nations (ASEAN) and the ASEAN Free Trade Agreement (AFTA) (with the exception of China), membership in the World Trade Organization (WTO), trade and foreign direct investment (FDI), and the creation of ‘economic corridors’ to facilitate cross-border trade [21,22]. Cambodia, Lao PDR, Myanmar, and Viet Nam are predominantly sending countries, while Thailand is predominantly a receiving country due to labour shortages and higher wage opportunities (see Table 1) [6].
Table 1.
Immigrant and emigrant populations by country, GMS, 2015.
| Country | Cambodia | Lao PDR | Myanmar | Viet Nam | Thailand |
|---|---|---|---|---|---|
| General trend | Sending | Sending | Sending | Sending | Receiving |
| Number of immigrants into country [10] | 73,963 | 22,244 | 73,308 | 72,793 | 3,913,258 |
| Females as % of immigrants [10] | 46.1 | 46.3 | 45.2 | 42.1 | 49.7 |
| Immigrants as % of national population [10] | 0.5 | 0.3 | 0.1 | 0.1 | 5.8 |
| Estimated number of refugees [10] | 104 | 0 | 0 | 0 | 132,838 |
| Estimated number of emigrants [11,12] | 1,187,842 | 1,345,075 | 2,881,797 | 2,558,678 | 854,327 |
| Main destination countries for emigrants | Malaysia, Thailand | Thailand | Thailand | Japan, Republic of Korea, Malaysia | Brunei Darussalam, Malaysia, Myanmar, Saudi Arabia, Singapore |
An estimated 3–5 million labour migrants have migrated across borders in the Subregion, primarily for remunerated employment [21]. Irregular migrants in the GMS (i.e. people without required documents or permits) include large numbers of labour migrants who take on low-paid and low-status jobs and victims of human trafficking, especially women and children trafficked for forced labour and the sex industry [21,23,24]. Stateless persons, members of marginalised ethnic groups, and second-generation migrants without citizenship also resort to irregular migration [6,25]. Casual cross-border migration is widespread and typically occurs in remote areas [21]. Environmental and climate change-related displacement and migration are expected to increase in the Subregion, although much of this movement will occur within countries rather than across borders [20]. Thailand hosts approximately 133,000 refugees and asylum seekers, a large proportion of whom have fled Myanmar [10]. In addition, many displaced people live in border areas surrounding the refugee ‘camp’ areas in Thailand.
International declarations and policy instruments
Migrants, as with all people, have a right to the highest attainable standard of health [26]. As enshrined in international human rights law, countries have an obligation to respect, protect, and fulfil the human rights of all individuals under their jurisdiction, regardless of their nationality of origin or immigration status [27]. For example, the 1990 International Convention on the Protection of the Rights of All Migrant Workers and Members of Their Families assures migrant workers access to ‘any medical care that is urgently required for the preservation of their life or the avoidance of irreparable harm to their health … on the basis of equality of treatment with nationals of the State concerned’ [28]. Yet despite such international declarations, stateless individuals often are denied ‘medical citizenship’ in their country of residence [25]. While GMS countries have ratified few international instruments relating to migration, all have ratified at least one international instrument protecting the right to health and other health-related human rights, thus providing a potential legal framework for action. There are increasing efforts to prioritise migrant rights in Asia, including a specific focus on migrants’ right to health (e.g. Joint United Nations Initiative on Migration, Health and HIV in Asia; 2007 ASEAN Declaration on the Protection and Promotion of the Rights of Migrant Workers; the 2011 Dhaka Declaration to promote migrant-inclusive health policies). The 10 ASEAN countries are now under pressure to make their health services more migrant-inclusive. The concept of ‘One ASEAN’ requires countries to facilitate the movement of people and trade and to move towards greater economic and social integration and harmonisation of legislation and standards [29,30].
Health of migrants in the GMS
The conditions in which many migrants travel, live, and work carry significant risks for their health. Many migrants experience threats to their health due to inadequate access to social and health services, precarious migration status, lack of legal rights, restrictive immigration and employment policies, unsafe and exploitative working conditions, inadequate housing, low income, inadequate social security arrangements, social exclusion, separation from family, and anti‐migrant sentiments [7,31]. Health consequences include infectious diseases, occupational health hazards and injuries, poor mental health, non-communicable diseases (such as cardiovascular disease and diabetes), and maternal and child health problems. Infectious diseases including HIV/AIDS, tuberculosis, and malaria are major concerns, particularly among migrant workers entering Thailand and migrants in remote border regions [32–34]. For example, migrants in GMS border areas are at increased risk of malaria infection, as they are exposed to new vectors and malaria ecologies in host communities, and are typically under-served by health services [35]. Some migrants (e.g. victims of trafficking and low-skilled irregular migrants) are vulnerable to violence and exploitation, including sexual exploitation, which can lead to physical, mental, sexual, and behavioural health consequences including injury, depression, sexually transmissible infections (STIs), and harmful alcohol and substance use [25,36]. One report estimated that HIV rates were approximately two to three times higher among trafficked sex workers from Myanmar in Thailand (usually from Myanmar’s ethnic minority groups) than among Thai women working in the industry [37]. While there is inadequate understanding of migrant health vulnerabilities, it is clear that limited access to health services is a major challenge for migrants in the Subregion [29].
UHC and migrants
As the United Nations Resolution ‘Transforming Our World’ highlights, ‘to promote physical and mental health and well-being and to extend life expectancy for all, we must achieve universal health coverage and access to quality health care’ [38]. Countries in the Asian region are at very different stages of UHC development, however, and many low- and middle-income countries are struggling to extend health coverage and to measure progress [39–41]. Accelerating progress on ‘coverage’ or ‘access’ are highly challenging goals, especially in low-income countries where supply and quality of services are inadequate, and ‘universal’ government health services usually require co-payments [19]. National health plans refer to UHC for ‘citizens’ or ‘the population’, the latter in practice usually excluding migrants (regular or irregular). There is a need to reframe debates in and beyond the health sector, to ensure that the commitment to ‘leave no-one behind’ – a feature of the SDG agenda – can be put into practice, including for migrants.
The discourse has moved beyond regarding UHC as mainly a matter of improving financial access and proposed indicators of progress now include measures of quantity, quality, and equity of services [42,43]. For example, the WHO Western Pacific Regional Action Framework views UHC as a whole-of-system approach to improving health system performance and health outcomes and lists five attributes of effective health systems: quality, efficiency, equity, accountability, and resilience [8]. It urges prevention of discrimination, including on the basis of migration status. The most basic measure of UHC progress however, remains problematic. Many of the world’s poor, particularly irregular migrants, are ‘invisible’ and not counted in official statistics [44]; for example, migrant populations are seldom mentioned in health impact assessments [10,45].
GMS countries, UHC progress, and cross-border migrants
The capacity of GMS health systems to respond to migrant populations varies greatly. Table 2 summarises the migrant-inclusive features of health coverage in five GMS countries. Thailand has put the most effort into migrant health coverage; it has signed Memoranda of Understanding (MoU) with Cambodia, Myanmar, and Lao PDR to support labour migration management, which provide a foundation to support migrant access to health services in Thailand [46]. Viet Nam has developed health protection for citizens who emigrate for work. However, in the GMS overall (except Thailand), UHC remains weak for citizens let alone migrants. Migrant workers, and irregular migrants in particular, are not adequately covered and incur high out-of-pocket (OOP) payments: these populations are at-risk and disadvantaged in terms of health and have great need to be included in UHC. This is certainly advantageous from a public health perspective, but is politically and socially sensitive [29].
Table 2.
Migrant-inclusive features of UHC in five GMS countries.
| Indicators | Cambodia | Lao PDR | Myanmar | Viet Nam | Thailand |
|---|---|---|---|---|---|
| Policy and national-level frameworks | Constitution 2008 (Article 72) ‘All Cambodians’; Ministry of Health goal of UHC | National Health Strategy on UHC 2015–2020 | National Health Plan UHC goal for citizens and designated ethnic groups | Health policies refer to citizens. Health Insurance Law 2008 aims for UHC | National Health Act 2002 set up UHC for those not covered by SHI schemes. National Health System Charter (Article 16) extends to everyone living in Thailand regardless of nationality. |
| Service models and coverage | HEFs cover 90% target of population (i.e. poor population) and 20% of national population | Limited SHI schemes. HEFs cover 41% of population | No specific programs | Govt. SHI covers 60% of population. Govt. subsidises premiums in poor areas | Mainly tax-financed: pay-roll tax SHI schemes, tax-based UHC for informal sector and poor. UHC covers 75% of Thai population who must register with district provider |
| UHC developments | HEFs scaling up across districts | HEFs being extended | UHC an accepted concept | Private health insurance allowed from 2011 | Less OOP payment and increased out-patient visits for UHC beneficiaries |
| Migrant-inclusive features | District HEFs unlikely to enrol migrants. Some programs for emigrant workers, and some infectious disease programs | HEFs unlikely to enrol migrants. Some donor-funded programs for migrant workers | Not a national priority | Emigrant worker programs; joint government and donor infectious disease programs in border areas | MHI Scheme: legal migrant workers registered; irregular migrants can opt in. Targeted policies address migrant health: e.g. the National Master Plan for HIV/AIDS Prevention; Care and Support for Migrants and Mobile Populations (2007–2011); 2003 Thai Migrant Health Program |
| Current challenges | Huge challenge to fund and rebuild health system. High OOP payment | High OOP payment and inadequate health services | Huge challenge to improve health services. High OOP payment | Govt. services under-resourced. User fees for public and private health services | Migrant workers pay annual fees for MHI. Many irregular migrants do not register for MHI. MHI benefits are not portable and are less comprehensive than for Thai nationals |
All GMS countries are seeking sustainable ways to fund their health systems. Most are moving towards social health insurance (SHI) models, with subsidies for the poor funded from general tax revenue or by international donors [19]. Thailand’s government spends comparatively more per capita on health (PPP int. $) than other GMS countries (see Table 3). People in all GMS countries, however, encounter substantial OOP payments for health services and medicines (see Table 3).
Table 3.
Socioeconomic, health system, and UHC indicators by country, 2012 or latest year.
| Indicators | Cambodia | Lao PDR | Myanmar | Viet Nam | Thailand |
|---|---|---|---|---|---|
| Population (000s) | 14,865 | 6,646 | 52,797 | 90,796 | 66,785 |
| GNI per capita (Atlas method), current USD | 1,360 | 1,650 | 1,270 | 1,890 | 5,370 |
| Life expectancy at birth (years) | 72 | 66 | 66 | 76 | 75 |
| Under-5 mortality rate (per 1,000 live births) | 40 | 72 | 52 | 23 | 13 |
| Total health expenditure (THE) as % of GDP | 5.6 | 2.8 | 1.8 | 6.8 | 4.1 |
| Private expenditure on health as % of THE | 77.4 | 50.6 | 84.1 | 54.8 | 22.3 |
| OOP expenditure as % of private expenditure on health | 80.3 | 78.2 | 93.7 | 83.2 | 55.8 |
| Per capita total expenditure on health (PPP int. $) | 129 | 75 | 23 | 227 | 372 |
| Physicians (per 10,000 population) | 1.7 | 1.8 | 6.1 | 11.9 | 3.9 |
Access to health services by migrant type
Migrant workers
The flow of labour migration in Asia is from low-income to higher-income countries, but it is in the interests of both sides to support labour mobility and a flow of remittances [6]. Migrant workers have limited access to health services, however, and many workers are not aware of provisions even when these exist [47]. Thailand has made particular advances in enhancing migrant health coverage. In 2015, an estimated 3.9 million migrants were living and working in Thailand (see Table 1). Regular migrants – often labour migrants – are covered by the national Social Security Scheme (SSS). Further, the Migrant Health Insurance (MHI) scheme enrols regular migrant workers following pre-employment health screening, with annual premiums deducted from the migrant’s wage; health services are available only at the hospital where the migrant was registered, and some services available to Thai citizens are not accessible to migrants [29]. In 2014, approximately 1.6 million MHI cards had been issued. Thailand has also established specific policies/programs to address migrant health, including the Migrant Health Program. They focus on, but are not limited to, international labour migrants and seek to strengthen the migrant sensitivity of existing health services and develop migrant health services [48]. Other GMS countries with large overseas worker populations have legislation, bilateral MoU, and government structures to manage labour outflow including the welfare of migrant workers and their families. Viet Nam (predominantly migrant sending) has established a Law on Vietnamese Guest Workers (2007) which has provisions for mandatory vocational training, pre-departure language training and orientation, and the Overseas Jobs Support Fund [49].
Irregular migrants
Thailand has established policies and good practices that relate to health services for some irregular migrants. From August 2013, irregular migrants were allowed to register for the MHI with annual fees attached (1,500 Baht plus 500 Baht health check – or approximately 56 USD – as of 2014) [29]. However, irregular migrants face legal restrictions and limited access to health services, for example migrant workers in the fishing industry continue to be exploited and have little access to services and many irregular migrants (e.g. victims of trafficking) fear legal consequences from interacting with authorities and services [50,51]. Further barriers to the scheme’s uptake include the annual fees (for the health exam and insurance costs), lack of awareness of the scheme among irregular migrants, and reluctance of some hospitals to promote and implement the policy [29]. This illustrates the difficulty of achieving UHC even in a country with developed migrant health policies and programs. There is a paucity of research focused on access to health services among irregular migrants in other GMS countries, including because there are apparently few policies/programs that enable irregular migrants to access health services or that seek to ensure their health is protected while working overseas and upon return.
Victims of trafficking
Reliable data on trafficking in the GMS are unavailable due to its illegal and often undetected nature, but the Subregion is known to have diverse forms of trafficking. For example, men and boys from Cambodia, Lao PDR, and Myanmar are trafficked to work on fishing boats in Thailand, Malaysia, and Indonesia; women and girls from Lao PDR and Myanmar are trafficked for sex-work and domestic work in Thailand [52]. Victims of trafficking experience substantial barriers to health services due to fear of discriminatory treatment, fear of being reported to officials, fear of arrest and deportation, and the belief or knowledge that they are not entitled to or could not afford health services [34]. In 2004, leaders of all six GMS nations signed the MoU on Cooperation Against Trafficking in Persons in the GMS, an agreement that led to the Coordinated Mekong Ministerial Initiative Against Trafficking (COMMIT) [53]. It states a commitment to ‘providing all victims of trafficking with shelter, and appropriate physical, psycho-social, legal, educational and health-care assistance’. Yet it is primarily non-governmental organisations (NGOs) that work to meet the health and welfare needs of trafficked people in the Subregion [52]. For example, World Vision’s End Trafficking in Persons (ETIP) program in the GMS supports bilateral repatriation through case management, referral to services, and follow-up.
Refugees and asylum seekers
There are an estimated 452,000 refugees from Myanmar (the eighth-largest refugee source country, 2014–15), many of whom have fled to Bangladesh and Thailand [54]. Approximately 120,000 refugees and asylum seekers, as well as several thousand internally displaced people, live in nine so-called temporary camps along the Thai–Myanmar border [54]. Thailand is not a signatory to international conventions on refugees, and the Thai Government does not use the term ‘refugee’. Primary health services for refugees are funded by the Thai Ministry of Interior, Thai provincial/district authorities, NGOs, and international agencies [54]. During 2015, the election campaign in Myanmar raised the possibility for voluntary return of refugees and internally displaced persons; due to the landslide victory for the National League for Democracy (NLD), however, the potential for planned return of religious and ethnic minority refugees remains undefined.
Casual cross-border migrants
Casual cross-border migration in the GMS is widespread, i.e. movement of border residents between countries, either with or without passing border control checkpoints. Border regions are under-served with respect to health services. Migrants within border regions are likely to seek health services from unregulated private vendors, which can increase exposure to substandard drugs [55,56]. Artemisinin-resistant malaria has emerged in GMS border areas including the Cambodia–Thai and Myanmar–Thai border areas where there are high rates of migration [55]. Migration from and to areas where the disease is prevalent contributes to increased malaria transmission and incidence. A 2011 outbreak assessment in Attapeu Province in Lao PDR found that migrant workers accounted for 70% of confirmed malaria cases [57]. Cross-border collaboration and coordination are critical to vector control and improved malaria prevention, testing, and treatment for migrants [56]. The WHO Emergency Response to Artemesinin Resistance (ERAR) in the GMS targets high-risk migrant and mobile populations, including casual cross-border migrants. Containment strategies include scaling-up of prevention, diagnosis, and control activities that cover difficult-to-reach and mobile populations (e.g. screening and treatment at bus stations and work-site interventions), training community or village volunteers for diagnostic testing, referral and surveillance, treatment, coordinated cross-border activities, and improving drug quality and drug regulation [56].
Discussion
Improving migrant access to health services in the context of UHC
Health coverage for migrants in the GMS poses challenges for governments. Governments are seeking to improve the supply and quality of mainstream health services (e.g. through continued investment of funds, resources, and staff) and implement programs that address the health needs and health service access of migrants [7] and other vulnerable groups. National health laws and legal frameworks are required in order to extend social protection and health coverage, including for migrants [58].
Partnerships, networks, and multi-country frameworks are essential in order to ensure cross-border cooperation and collaboration on migrant health. Regional and subregional initiatives that address migrant health include: the Mekong Basin Disease Surveillance network; Joint United Nations Initiative on Mobility and HIV/AIDS (JUNIMA); WHO Mekong Malaria Program; WHO Regional Strategy to Stop Tuberculosis in the Western Pacific; bilateral collaboration and MoUs between Thailand and neighbouring GMS countries that focus on migrant workers; and the WHO Regional Action Framework on Universal Health Coverage. These examples of bilateral and regional cooperation highlight the growing focus on migrant health and UHC. Attention to cross-border migrant health is likely to increase, given the linkages to the SDGs and other international, regional, and national agendas. The ongoing move by countries towards integration under ASEAN, for example, will add momentum to extending health equity to their migrant populations [29].
While health service entitlements need to be expanded, improving the capacity of health services to address migrant health is equally important. Current access barriers for migrants include legal/administrative restrictions, language barriers, cultural constructs around illness and treatment, discriminatory attitudes amongst health service staff, and limited experience among health workers of migrant health issues. Increasing the migrant sensitivity of health services can support equivalence of care between migrant populations and local populations, e.g. through addressing language and cultural barriers, increasing the cultural competence of the workforce (both clinical and public health), and improving migrant health literacy. Universal access is a concept that goes beyond UHC, in that it requires health systems to remove geographical, financial, organisational, and socio-cultural barriers to care [59]. GMS governments face particular challenges in extending services to border areas, which are remote, mountainous, and often inaccessible. In Thailand, the Border Health Development Master Plan (2012–16) aims to improve the health and health services among people living in border areas (e.g. Thais, ethnic minorities, registered and non-registered migrants, displaced persons, and asylum seekers) [48]. It is important to further increase the quality and availability of health services in border areas where migrant and mobile populations reside.
Whether migrant health services should be separate or integrated into mainstream services is much debated. It is argued that health services that target migrant groups are important, particularly where infectious diseases (e.g. malaria, tuberculosis) pose substantial risks to migrants, the surrounding population, and beyond [60,61]. Currently, a few health initiatives target high-risk migrant and mobile populations in the Subregion, such as the WHO Emergency Response to Artemesinin Resistance in the GMS. Whether migrant health services/responses are integrated or separate, the involvement of migrant communities in decision-making (e.g. defining health concerns and service delivery needs) can reduce barriers to access, enhance integration, and improve population health. There is growing emphasis on creating opportunities for vulnerable groups, including migrants, to have a voice in health policy and practice [8]. Yet it is important to acknowledge that the health service users who are most reluctant and/or constrained in their engagement with services are usually the most disadvantaged [62].
Health coverage for irregular migrants is of particular concern, as they are rarely included in UHC frameworks yet comprise some of the most vulnerable migrant groups [29]. In order to achieve truly universal health coverage, entitlement and access to essential health services are necessary regardless of migration status. Governments will need to set the vision and direction to address inequities in health service access and to ensure the highest attainable standard of health among irregular migrants. This, however, remains a socially and politically sensitive issue.
There is limited research that examines migrant health in the GMS (other than Thailand). Further research at the country and subregional levels can contribute to understanding and supporting migrant inclusion in UHC efforts. Indicators to measure UHC progress should be disaggregated by relevant socioeconomic ‘stratifiers’, including migration status [4,63]. Migrant health and service use data can support governments to assess health disparities, make evidence-based decisions, and improve equity of service provision. Table 4 proposes solutions to overcome barriers to health coverage and health service access among cross-border migrants in the GMS.
Table 4.
Cross-border migrants: examples of health system access barriers, problems, and solutions.
| Type of barrier | Access problems | Access solutions |
|---|---|---|
| Human rights and laws | A country may not be a signatory to international and regional legal instruments on migration and health Migrants are not mentioned in the national constitution, national laws, or health policies |
Advocate signing international and regional legal instruments on migration and health Make explicit reference to migrants’ health in health policies and plans, including diverse groups of migrants |
| Geographic | Migrant populations based in geographically remote areas Inadequate supply/standard of equipment and medicines Inadequate supply of staff in remote services |
Send outreach services and staff to remote health facilities Improve supply/standard of equipment and medicine Cross-border programs in border regions that address joint health policy, financing, and health service delivery |
| Service delivery (availability, quality) | Restrictive eligibility for health services Lack of expert/relevant health knowledge on migrant health Limited data monitoring migrant health needs, health status, and service use |
Lift or reduce restrictions for migrants; promote primary care services as entry point for migrant populations Train appropriate staff to understand and address migrant-related health issues, including both clinical and public health/health promotion workforce Introduce and improve migrant health data collection |
| Financial (affordability) | Migrants are not included in health insurance schemes Migrant health programmes are underfunded High user fees exist |
Include coverage for migrants in health insurance schemes and HEFs Seek funding priority and new sources, including through private sector engagement, and regional and cross-border financing schemes Reduce OOP expenses and subsidise fees; introduce portal health insurance schemes for migrant workers |
| Sociocultural (acceptability, responsiveness) | Mono-cultural/mono-lingual services Lack of community engagement Health service/administrative staff have limited knowledge of social/cultural determinants of migrant health Migrants not literate and/or health literate Migrants have different cultural constructs around illness causation and treatment |
Employ migrant/multicultural staff to act as intermediaries/facilitators Provide interpretation services Promote community participation Develop culturally tailored health programmes Provide cultural competency training and standards to staff Translate materials into formats that are acceptable to diverse migrant groups (including visual information and social marketing) |
Conclusions
The GMS will continue to experience migration in the coming years and decades. The emergence of a health equity agenda under international SDGs, and more focus on migrant health, provide an opportune time for GMS countries to develop migrant-inclusive health systems and strategies. It is of great importance that migrants are included. First, health coverage is not truly ‘universal’ unless migrants are included. Second, the health needs of migrants should be addressed as a matter of human rights. Third, it is in the GMS’s interests to protect the health of migrants as it pursues national and regional economic growth and social progress [29]. Yet for countries striving to achieve health equity, without specific efforts to include marginalised populations, there is a risk that poorer and disadvantaged segments of a population could be excluded from health service access and health promotion, leading to increasing inequities in health [59,63,65]. Health equity requires deliberate policy decisions that support health services and population health initiatives for irregular migrants and casual cross-border migrants, who remain amongst the most vulnerable and disadvantaged migrant groups. The ultimate goal of health equity is to improve population health outcomes. UHC represents an important opportunity to reduce barriers to health service access, extend coverage of curative services and health promotion efforts, and strengthen partnerships in order to improve the health of migrant populations.
Acknowledgments
We thank Anjana Bhushan and Britta Baer, from World Health Organization Western Pacific Regional Office, for their comments on an earlier version of this paper. This paper draws in part from a 2014 paper on access to health care among cross-border migrants in the Greater Mekong Subregion written for the World Health Organization Western Pacific Regional Office.
Biography
CM and JH developed the focus for the paper, and undertook the review of published literature and analysis. CM wrote the first draft of the manuscript. JH led development of Tables 2-4 and revised the manuscript. Both authors reviewed the final manuscript.
Responsible Editor Jennifer Stewart Williams, Umeå University, Sweden
Funding Statement
None.
Disclosure statement
No potential conflict of interest was reported by the authors.
Ethics and consent
None.
Paper context
Health coverage is only truly equitable and ‘ universal’ where migrants are included. This paper examines health needs and health care access among cross-border migrants in the Greater Mekong Subregion, and reviews associated policy responses. It argues that universal health coverage and health equity require deliberate policy decisions that support migrant access to health services, extend coverage of curative services and health promotion initiatives, and strengthen partnerships in order to improve the health of migrant populations.
References
- UNDP http://www.undp.org/content/dam/undp/library/SDGs/SDG%20Implementation%20and%20UNDP_Policy_and_Programme_Brief.pdf UNDP support to the implementation of the 2030 agenda for sustainable development. New York: United Nations Development Programme; 2016. [cited 2016 Sep 12]. Available from.
- Hosseinpoor AR, Bergen N, Schlotheuber A. Promoting health equity: WHO health inequality monitoring at global and national level. Global Health Act. 2015;8:29034. doi: 10.3402/gha.v8.29034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutzin J, Sparkes SP. Editorial: health systems strengthening, universal health coverage, health security and resilience. Bull World Health Organ. 2016;94:2. doi: 10.2471/BLT.15.165050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodney AM, Hill PS. Achieving equity within universal health coverage: a narrative review of progress and resources for measuring success. Int J Equity Health. 2014;13:72. doi: 10.1186/s12939-014-0072-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangcharoensathien V, Mills A, Palu T. Accelerating health equity: the key role of universal health coverage in the sustainable development goals. BMC Med. 2015;13:101. doi: 10.1186/s12916-015-0342-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IOM . Regional strategy for Asia and the Pacific 2012–2015. Bangkok: International Organization for Migration Regional Office for Asia and the Pacific; 2010. [Google Scholar]
- WHO . (Report of a Global Consultation) Madrid: World Health Organization; 2010. Health of migrants - the way forward. [Google Scholar]
- WHO Regional Office for the Western Pacific http://www.wpro.who.int/about/regional_committee/66/documents/wpr_rc66_06_uhc_7sep.pdf Universal health coverage. 2015 [cited 2016 Feb 15]. Available from.
- WHO Regional Office for South East Asia http://www.searo.who.int/publications/en/ Health in the sustainable development goals: where we are now in the South-East Asia region? What next? 2016 [cited 2016 Aug 31]. Available from.
- United Nations Population Division Trends in international migrant stock: the 2015 revision. 2016 Aug 25; http://www.un.org/en/development/desa/population/migration/data/estimates2/estimates15.shtml cited. 2016. Available from.
- Spoorenberg T. Demographic changes in Myanmar since 1983: an examination of official data. Popul Dev Rev. 2013;39:309–10. doi: 10.1111/j.1728-4457.2013.00593.x. [DOI] [Google Scholar]
- United Nations Population Division International migrant stock by destination and origin, 2015. 2016 Aug 25; http://www.un.org/en/development/desa/population/migration/data/estimates2/estimates15.shtml cited. 2016. Available from. [Google Scholar]
- Akkhavong K, Paphassarang C, Phoxay C. The Lao people’s democratic republic health system review (Health Systems in Transition, Vol. 4 No. 1) Manila: World Health Organization (Asia Pacific Observatory on Health Systems and Policies); 2014. [Google Scholar]
- Annear P, Grundy J, Ir P. The Kingdom of Cambodia health system review (Health Systems in Transition, Vol. 5 No. 2) Manila: World Health Organization (Asia Pacific Observatory on Health Systems and Policies); 2015. [Google Scholar]
- Jongudomsuk P, Srithamrongsawat S, Patcharanarumol W. The Kingdom of Thailand health system review. Manila: World Health Organization (Asia Pacific Observatory on Health Systems and Policies); 2015. Health Systems in Transition, Vol 5 No 5. [Google Scholar]
- Sein TT, Myint P, Tin L. The Republic of the Union of Myanmar: health systems in transition. Vol. 4 No. 3. Manila: World Health Organization (Asia Pacific Observatory on Health Systems and Policies); 2014. [Google Scholar]
- WHO http://www.who.int/features/qa/universal_health_coverage/en/ What is universal health coverage?’ World Health Organization; 2014 [cited 2015 Aug 7]. Available from.
- World Bank Country and lending groups. 2015 http://data.worldbank.org/about/country-and-lending-groups#East_Asia_and_Pacific [cited 2015 Oct 22]. Available from.
- World Health Organization Regional Office for the Western Pacific (McMichael C, Healy J) Cross-border migration in the Greater Mekong Subregion (GMS) and health service access. Manila (Philippines): World Health Organization Regional Office for the Western Pacific; Forthcoming. [Google Scholar]
- ADB . Climate change and migration in Asia and the Pacific: draft edition. Manila (Philippines): Asian Development Bank; 2012. [Google Scholar]
- ADB . Facilitating safe labor migration in the Greater Mekong Subregion. Manila (Philippines): Asian Development Bank; 2013. [Google Scholar]
- ASEAN . ASEAN economic community blueprint. Jakarta: Association of Southeast Asian Nations; 2007. [Google Scholar]
- Frederico S. Migration in the Greater Mekong Subregion. Manila (Philippines): Asian Development Bank; 2009. Background Paper. [Google Scholar]
- Hugo G. Migration in the Asia-Pacific region. Geneva: International Organization for Migration; 2005. Global Commission on international migration. [Google Scholar]
- Kingston L, Cohen E, Morley C. doi: 10.1186/1472-698X-10-11. http://www.biomedcentral.com/1472-698X/10/11 Debate: limitations on universality: the “right to health” and the necessity of legal nationality. BMC Int Health Hum Rights. 2010 [cited 2014 May 29];10:11. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IOM, WHO, OHCHR . International migration, health and human rights. Geneva: International Organization for Migration; 2013. [Google Scholar]
- OHCHR Human rights framework. http://www.ohchr.org/EN/Issues/Migration/Pages/HumanRightsFramework.aspx Office of the High Commissioner for Human Rights; 2014 [cited 2014 Aug 25]. Available from.
- United Nations General Assembly http://www.unhcr.org/refworld/docid/3ae6b3980.html international convention on the protection of the rights of all migrant workers and members of their families. 18 December 1990, A/RES/45/158; [cited 2014 May 29]. Available from.
- Guinto RLLR, Curran UZ, Suphanchaimat R. Universal health coverage in ‘One ASEAN’: are migrants included? Global Health Act. 2015;8:25749. doi: 10.3402/gha.v8.25749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sriratanaban J. ASEAN integration and health services. Global Health Act. 2015;8:27199. doi: 10.3402/gha.v8.27199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IOM https://www.iom.int/files/live/sites/iom/files/What-We-Do/docs/Health-in-the-Post-2015-Development-Agenda.pdf Health in the post-2015 development agenda: the importance of migrants’ health for sustainable and equitable development. 2015 [cited 2016 Feb 15]. Available from.
- Gushulak B, MacPherson D. The basic principles of migration health: population mobility and gaps in disease prevalence. Emerg Themes Epidemiol. 2006;3:3. doi: 10.1186/1742-7622-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin M. When crossing borders: recognising the sexual and reproductive health and rights of women migrant workers. Arrows Change. 2013;19:2–5. [Google Scholar]
- Zimmerman C, Kiss L, Hossain M. Migration and health: a framework for 21st century policy-making. Plos Med. 2011;8:e1001034. doi: 10.1371/journal.pmed.1001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui L, Yan G, Sattabongkot J. Malaria in the Greater Mekong Subregion: heterogeneity and complexity. Acta Tropica. 2012;121:227–239. doi: 10.1016/j.actatropica.2011.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaikittiporn C, Laohaudomchok W, Weik K. Thailand Myanmar migrant workers in Thailand. Asian-Pacific Newsl Occup Health Saf. 2012;19:10–13. [Google Scholar]
- Beyrer C. HIV/AIDS in Asia: accelerating and disseminating. Washington Quarter Winter. 2001;24:211–225. doi: 10.1162/016366001561483. [DOI] [Google Scholar]
- United Nations General Assembly http://www.un.org/ga/search/view_doc.asp?symbol=A/RES/70/1&Lang=E Transforming our world: the 2030 agenda for sustainable development. 25 September 2015, A/RES/70/1; [cited 2016 Sep 12]. Available from.
- WHO . The World Health Report 2013: research for universal health coverage. Geneva: World Health Organization; 2013. [Google Scholar]
- Hipgrave DB, Hort K. Will current health reforms in south and east Asia improve equity? Med J Aust. 2014;200:514–516. doi: 10.5694/mja13.10870. [DOI] [PubMed] [Google Scholar]
- Annear PL, Comrie-Thomson L, Dayal P. The challenge of extending universal coverage to low- and middle-income countries in Asia Policy Brief. Asia Pacific Observatory Health Systems Policies. 2015;4(3) [Google Scholar]
- Ng M, Fullman N, Dieleman JL. Effective coverage: a metric for monitoring universal health coverage. PLoS Med. 2014;11:1–8. doi: 10.1371/journal.pmed.1001730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2016 http://indicators.report/targets/3-8/ UN Sustainable Development Solutions Network. Indicators and a monitoring framework.
- Wong J. Achieving universal health coverage. Bull World Health Organ. 2015;93:663–664. doi: 10.2471/BLT.14.149070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miramontes L, Pottie K, Jandu MB. Including migrant populations in health impact assessments. Bull World Health Organ. 2015;93:888–889. doi: 10.2471/BLT.14.142315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ASEAN/JUNIMA . Multi-stakeholder dialogue on migrants’ health and access to HIV services in the ASEAN region - meeting report. Bangkok: ASEAN; 2011. [Google Scholar]
- Low WY, Tong WT, Binns C. Migrant workers in Asia Pacific and their rights to health. Asia Pac J Public Health. 2015;27:584–587. doi: 10.1177/1010539515600007. [DOI] [PubMed] [Google Scholar]
- IOM . Healthy migrants, healthy Thailand: a migrant health program model. Bangkok: International Organization for Migration and the Thai Ministry of Public Health; 2009. [Google Scholar]
- ILO . Labour migration from Colombo process countries: good practices, challenges and way forward. Geneva: International Labour Organization; 2013. [Google Scholar]
- EJF . Slavery at sea: the continued plight of trafficked migrants in Thailand’s fishing industry. London: Environmental Justice Foundation; 2014. [Google Scholar]
- http://www.state.gov/j/tip/rls/tiprpt/countries/2014/226832.htm US Department of State. Thailand: 2014 trafficking in persons report. 2014 [cited 2014 Aug 11]. Available from. [Google Scholar]
- World Vision International . Tackling human trafficking in the Greater Mekong Subregion. Bangkok: World Vision International; 2013. [Google Scholar]
- UNIAP http://www.no-trafficking.org/commit.html COMMIT: the coordinated Mekong ministerial initiative against trafficking. 2014 [cited 2014 Aug 18]. Available from. [Google Scholar]
- UNHCR http://www.unhcr.org/en-au/statistics/unhcrstats/576408cd7/unhcr-global-trends-2015.html Global trends: forced displacement in 2015. 2016 [cited 2016 Dec 5]. Available from.
- Carrara VI, Lwin KM, Phyo AP. Malaria burden and artemisinin resistance in the mobile and migrant population on the Thai-Myanmar Border, 19992011: an observational study. PLoS Med. 2013;10:e10001398. doi: 10.1371/journal.pmed.1001398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . Emergency response to artemisinin resistance in the Greater Mekong Subregion: regional framework for action 2013–15. Geneva (Switzerland): World Health Organization; 2013. [Google Scholar]
- Hewitt S, Delacollette C, Chavex I. Malaria situation in the Greater Mekong Subregion. Southeast Asian J Trop Med Public Health. 2013;44:46–72. [PubMed] [Google Scholar]
- Clarke D, Rajan D, Schmets G. Creating a supportive legal environment for universal health coverage. Bull World Health Organ. 2016;94:482. doi: 10.2471/BLT.16.173591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravindran TKS. Universal access: making health systems work for women. BMC Public Health. 2012;12:S4. doi: 10.1186/1471-2458-12-S1-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy J, McKee M. Delivering health services in diverse societies. In: Healy J, McKee M, editors. Accessing health care: responding to diversity. Oxford: Oxford University Press; 2004. [Google Scholar]
- Fortier J. Health of migrants: the way forward. Madrid: World Health Organization; 2010. Migrant-sensitive health systems; pp. 61–70. (Report of a global consultation) [Google Scholar]
- García-Ramirez M, Hatzidimitriadou E. User involvement and empowerment in health care practices with ethnic minority and migrant groups: a community approach. Int J Migration Health Soc Care. 2009;5:2–4. [Google Scholar]
- Boerma T, Evans D, Kieny M. doi: 10.1371/journal.pmed.1001731. http://apps.who.int/iris/bitstream/10665/112824/1/WHO_HIS_HIA_14.1_eng.pdf Monitoring progress towards universal health coverage at country and global levels. World Health Organization/World Bank Group; 2014 [cited 2015 Nov 12]. Available from. [DOI] [PMC free article] [PubMed]
- Jacobs B, Ir P, Bigdeli M. Addressing access barriers to health services an analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan. 2011:1–13. doi: 10.1093/heapol/czr038. [DOI] [PubMed] [Google Scholar]
- Moreno-Serra R, Smith PC. Does progress towards universal health coverage improve population health? Lancet. 2012;380:917–923. doi: 10.1016/S0140-6736(12)61039-3. [DOI] [PubMed] [Google Scholar]


