ABSTRACT
Active-duty military service members have a significant risk of sustaining physical and psychological trauma resulting in traumatic brain injury (TBI) and post-traumatic stress disorder (PTSD). Within an interdisciplinary treatment approach at the National Intrepid Center of Excellence, service members participated in mask making during art therapy sessions. This study presents an analysis of the mask-making experiences of service members (n = 370) with persistent symptoms from combat- and mission-related TBI, PTSD, and other concurrent mood issues. Data sources included mask images and therapist notes collected over a five-year period. The data were coded and analyzed using grounded theory methods. Findings indicated that mask making offered visual representations of the self related to individual personhood, relationships, community, and society. Imagery themes referenced the injury, relational supports/losses, identity transitions/questions, cultural metaphors, existential reflections, and conflicted sense of self. These visual insights provided an increased understanding of the experiences of service members, facilitating their recovery.
KEYWORDS: Post-traumatic stress disorder, traumatic brain injury, art therapy, masks, active duty military
Man is least himself when he talks in his own person. Give him a mask and he will tell you the truth. (Oscar Wilde)
Introduction
Deployment of manpower to fight the war on global terrorism has exposed millions of combat troops from dozens of countries across the world to concussive forces and operational stressors for more than a decade and a half. As of 30 September 2011, the US Government Accountability Office reported that approximately 2.6 million US military service members had already been deployed during the Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) era (US Government Accountability Office, 2011). The North Atlantic Treaty Organization (NATO) commanded the United-Nations mandated International Security Force (ISAF) in Afghanistan from August 2003 to December 2014. At its height, ISAF was more than 130,000 strong, with troops from 51 NATO and partner nations (North Atlanta Treaty Organization, 2016). As of 12 August 2016, the Defense and Veterans Brain Injury Center (2016) reported that 352,619 US military service members worldwide have been diagnosed with TBI, with 82.3% cases classified as mild. The UK reported 4.4% mild TBI post-deployment (Rona et al., 2012). Incidences of PTSD increase with combat exposure (Jain et al., 2012; Stein et al., 2015), while TBI can be sustained from deployment settings as well as non-deployed settings such as military training, vehicle crashes, recreational activities, or falls (Blakeley & Jansen, 2013).
Recent research across the globe has highlighted the co-occurrence of PTSD and TBI in military service members, with TBIs sustained during deployment considered significant predictors of the service member developing symptoms of PTSD (Yurgil et al., 2014). Multinational troop presence during OEF and OIF, combined with the prevalence of PTSD and TBI, makes finding effective therapeutic strategies for medical care a global imperative. Prevalence rates of PTSD were reported as high as 13.5% in a large population-based cohort of OEF/OIF-era US veterans (Dursa, Reinhard, Barth, & Schneiderman, 2014) and up to 9% in Dutch military personnel 6 months post-deployment to Afghanistan (Reijnen, Rademaker, Vermetten, & Geuze, 2015), while in the UK prevalence varied from 1.3–4.8% in veterans returning from OEF/OIF (Fear et al., 2010). In the US, treatment costs have been estimated at $6 billion for PTSD and $910 billion for TBI (Bahraini et al., 2014; Wall, 2012).
Background
Military service members’ PTSD and TBI experiences
Individuals with PTSD, an anxiety disorder, have typically experienced a traumatic event or exposure to extended periods of stressful or traumatic conditions causing behaviors of hyperarousal, negative mood or cognitive associations, avoidance, and a re-experiencing of the traumatic event (Bahraini et al., 2014). Traumatic brain injury involves altered or disrupted brain functioning caused by an external force (e.g., being hit by an object in the head, exposure to blasts), where memory loss, loss of consciousness, altered mental states (e.g., confusion), or neurological deficits (e.g., aphasia or loss of balance) are experienced after the event (Bahraini et al., 2014; Wall, 2012) and PTSD and TBI symptoms often overlap causing individuals to experience anxiety, depression, cognitive deficits (e.g., memory loss, attention difficulties), irritability, and sleep disruptions, among other symptoms (Dolan et al., 2012).
Service members living with PTSD and/or TBI experience a range of physical and psychological symptoms. In a phenomenological inquiry of military-related PTSD, Kroch (2009) found several major themes in the experience: trauma remembering; encountering death; hypervigilance in an unsafe world; dualistic psychological ideas (e.g., inner vs. outer worlds, public vs. private life, night vs. day); and feeling alien to oneself and others, as if living in the dark. Delgado Martinez’s (2013) phenomenological investigation of blast-induced TBI in active-duty service members displayed isolated and sad feelings mixed with the challenge of accepting one’s injury.
To aid in addressing these injury-related challenges, a number of evidence-based treatment options exist for PTSD and TBI with service members and veterans (e.g., cognitive-behavioral therapy, pharmacotherapy, psychological debriefing [Tanielian & Jaycox, 2008]). Art therapy has been increasingly accepted as a form of complementary care for military veterans with PTSD symptoms (Nanda, Gaydos, Hathron, & Watkins, 2010). Interventions such as mask making have been shown to offer important psychosocial support for these diagnoses (Kopytin & Lebedev, 2013; Lande, Tarpley, Francis, & Boucher, 2010; Malchiodi, 2012; Sargent, Campbell, Richter, McLay, & Koffman, 2013). Art therapy has been viewed as a successful assessment tool in helping to describe psychological states and behaviors before and after TBI (Pachalska et al., 2013). In addition, art therapy is a treatment tool because the creation and transformation of symbols of the military experience helps to achieve self-integration and mastery of trauma (Golub, 1985). Image-making in art therapy helps pave the way for the integration of memories and development of a coherent narrative given that traumatic experiences impact verbal self-expression, as evidenced by reduced activity in Broca’s area (Lobban, 2014; Van Der Kolk, 2014). This image-making also helps to alleviate recurring nightmares (Hines-Martin & Ising, 1993), reduce arousal, reactivate positive emotion, enhance emotional self-efficacy, and improve self-esteem for veterans with combat-related PTSD (Collie, Backos, Malchiodi, & Spiegel, 2006), as well as improve concentration, memory, attention, and organization in patients (David, 1999). There are still gaps in the literature about PTSD and TBI treatment across the military continuum. While many studies focus on retired veterans, there are fewer studies on active-duty service members.
Mask making in art therapy treatment and recovery
Mask making has had historical significance in human society. In many cultures around the world, masks have been used to represent political issues (Agberia, 2006), spirituality (Agberia, 2006; Andrew, 2014; Jiachiao, 2013) a sense of fear, power, or control (Akpan, 1994), cosmic harmony (Diakparomre, 2010), hidden or private feelings (Furuki, 2011; Paoletti, 1992), cultural identity (Medina & Koui, 2009), transformation (Pollock, 1995), and death (Paoletti, 1992). In art therapy, mask making has been used to address communication and social skills in education (Fiet, 2014), improve psychopathology and personal orientation in psychotherapy (Fryrear & Stephens, 1988), and help process identity (Hinz & Ragsdell, 1990). Specifically with military service members, “trauma masks” have assisted in visualizing and communicating the effects of combat-related trauma to help build a sense of self-efficacy and promote normalization (Sargent et al., 2013). Mask making is a commonly used method in art therapy clinical practice and is used with a range of populations affected by trauma since it is a medium that allows for some psychological distance for expression and externalization. The standardized use of mask making for active duty service members is more recent and the visual community created through this project is unique. To the best of our knowledge, this is the first study to systematically analyze a large database of masks made by individuals suffering from PTSD and TBI. The term “art therapy” is thought to have been first coined by British soldier and artist Adrian Hill in 1942, during WWII (Hogan, 2001). In parallel, art therapists were hired in 1945 by the Department of Veterans Affairs to treat returning veterans (American Art Therapy Association, 2009). Because mask making is a common art therapy method, it is likely that art therapists have utilized the process in numerous settings. However, the authors were not able to find documentation of use with military service members and veterans until recent years.
In a detailed case study on art therapy for PTSD and TBI with a senior active-duty service member (Walker, Kaimal, Koffman, & DeGraba, 2016), a positive example of the use of mask-making to externalize and alleviate intrusive thoughts, hallucinations, and flashbacks associated with trauma is described. Masks can symbolize duality and the ability to take on different personas. For example, the duality of “being another to oneself and others,” living in the space between military and civilian life and experiencing the symptoms of military-related trauma relating to past and present identity presents a powerful phenomenon to explore further (Frenz, 2007).
Mask making as part of art therapy sessions appears to help these service members with PTSD and TBI. However, the physical representation of ideas portrayed in the masks and the meanings associated with the imagery have not been systematically studied. This study aims to use a grounded theory approach to categorized masks as a behavioral health assessment strategy to identify unspoken ideations of guilt, loss, and shame that perpetuate the presence of PTSD, depression, and anxiety in service members with combat-related TBI. The visual representations along with the patients’ interpretation of the images they created may provide insight into the range of experiences when living with unseen and previously inexpressible wounds of war. In clinical interactions, service members who engaged in art therapy often state that art therapy helps them verbalize and express their experiences in ways that they were previously unable to do. When asked to describe his art therapy product for an online gallery, one past patient anonymously stated, “Often, I’m asked what it feels like to have PTSD or TBI. In the past, I’ve been at a loss for how to describe these feelings—until I made my mask” (Chen, 2016). This study presents findings from the analysis of several hundred such masks, highlighting the various emotions and experiences of living with combat related PTSD and TBI.
Methods
This study used a grounded theory approach to analyze visual and narrative data from military service members with chronic PTSD symptoms and mild-to-moderate TBI, who participated in a 4-week interdisciplinary intensive outpatient program at the National Intrepid Center of Excellence (NICoE), at the Walter Reed National Military Medical Center, in Bethesda, Maryland, USA. All participating institutions approved the study including the Department of Defense and the Departments of Army/Navy/Air Force and Drexel University through a data sharing agreement approved by the Institutional Review Board (IRB) of both institutions. The IRBs provide oversight to ensure ethical conduct of research and human subjects protection. Participants were patients at the NICoE and provided informed consent for analysis of their de-identified retrospective data.
Study setting and art therapy context
Upon referral, each week an average of five-to-six US military service members and their families, as available, are admitted to the NICoE 4-week interdisciplinary intensive outpatient program as a cohort. Patients and families are provided housing on campus to immerse the service members in a therapeutic environment. Upon arrival at the NICoE, each service member has a group meeting on the first morning with his/her entire patient-centered core team of providers, which includes an internist, neurologist, psychiatrist, neuropsychologist, family therapist, and nurse specialist. Service members then undergo a standardized evaluation and treatment program comprised of 17 conventional and integrative disciplines. In the NICoE patient-centric model, the clinical schedule is tailored to the individual service member who engages in 6–7 hours per day (Monday through Friday) of clinical evaluation and care, totaling approximately 104 hours over the 4 weeks.
The service members attend art therapy as an integral part of this 4-week model of comprehensive care at a military care center. The center utilizes state of the art medical evaluations and treatments, psychotherapy, as well as an array of integrative therapies, such as the creative arts therapies including art therapy, music therapy, and dance/movement therapy. Other integrative techniques such as yoga, meditation, acupuncture, canine-assisted therapy, therapeutic writing, guided imagery, Heart-math, Tai-chi, and biofeedback-assisted relaxation breathing techniques are available to provide the service members with a variety of choices.
Description of the art therapy experience
During the first week of care, in a dedicated studio space, an art therapist works with service members in a group art therapy session to create masks. The directive is to create masks representing any aspects of their experiences and/or identities. The primary goal of the mask-making session in the first week is to provide an opportunity for a service member to artistically externalize parts of themselves in a safe and non-judgmental environment. The sessions encourage self-expression and group cohesion, empathy, and mutual support. They are offered a range of art supplies including paint, clay, collage, and print materials and are also supported in bringing in additional materials that enable them to create personal symbols and metaphors within their masks. Most service members completed their masks within the two-hour sessions, while others choose to continue work on their masks during individual art therapy sessions over the course of their stay at the center. The clinical notes and images describing the completed masks for all patients are included in the medical records and shared with interdisciplinary team members.
Study participants
Study participants included service members from all branches of the Armed Services, including the National Guard who had unremitting symptoms from combat-related TBI and psychological health conditions. Participants (n = 370) ranged in age from 20 to 50 years (M = 36.19; SD = 7.53) and were almost all (97.5%) men. Racial and ethnic demographics included 89.1% Caucasian, 4.2% Hispanic, 3.6% African American, 2.2% Asian or Pacific Islander, and 0.8% who identified as “other.” Participants’ time in service ranged from 1.5 to 33 years (average time of 14 years, 7 months). Participants came from all five military service branches, with the most frequently serving in the Navy (45.1%; n = 167). The most frequent participant pay grade was E7 (21.6%; n = 80; E7 titles vary across service branches—Army, Sergeant First Class; Marine, Gunnery Sergeant; Navy, Chief Petty Officer; Air Force, Master Sergeant).
Data sources
Data sources for the study included images of artwork and clinical notes written on art therapy sessions. The art therapist created clinical notes and documented participants’ verbal descriptions of the symbolism embedded in their masks and their experiences with making the masks. These notes and mask images were uploaded as part of electronic medical records documentation into a common military patient charting and medical information database. The notes were about 50–100 words each. Additional demographic information was also available on participants’ age, gender, military rank, and number of deployments. Over 1000 masks have been made over the past 5 years. Complete data including consent for analysis, pictures of their masks, concurrent notes, and participant demographic information were available for 370 participants and these were included in the analyses.
Data analysis
The data were analyzed using grounded theory (Corbin & Strauss, 2008). The analysis first involved an initial review of the entire database of clinical notes and images. The mask images extracted from the database were matched with relevant clinical notes. These were then combined and integrated into a mixed-methods software tool. Once this database was set up, a comprehensive list of open codes was created by the lead authors. They coded the clinical notes describing patient descriptions of the artwork—patients’ self-reports on symptoms, experiences with art-making, and descriptions of the masks’ associations and content. They also coded visual elements of each mask for representations, composition, color, media used, and visual symbols. Each mask was classified and then grouped under the appropriate thematic category. Additional members of the research team also reviewed these codes, and refinements were made as the first masks were coded. The research team members coded the masks individually and created memos during the analysis to flag any potential discrepancies. These discrepancies were then highlighted and resolved through discussion during group research team meetings. Once the coding process was completed, the codes were clustered together to identify overarching recurring themes and reviewed together to attain consensus by the research team. This led to the development of an overall framework for the structure of the themes as they related to self-representation and identity.
Results
Analysis of the masks and notes indicated that these visual representations follow a pattern of representations of the self. This theoretical framework is not hierarchical; rather it represents the categories in terms of how participants represented aspects of self in the masks. Thus representations of self included: self as an individual, self in relationships, self in communities, self representing societal and philosophical value systems, and self in/over time. The references to self could be focused on personal strengths and/or challenges as a result of injury and often referred to past, present, or future. See Figure 1 for the framework.
Figure 1.
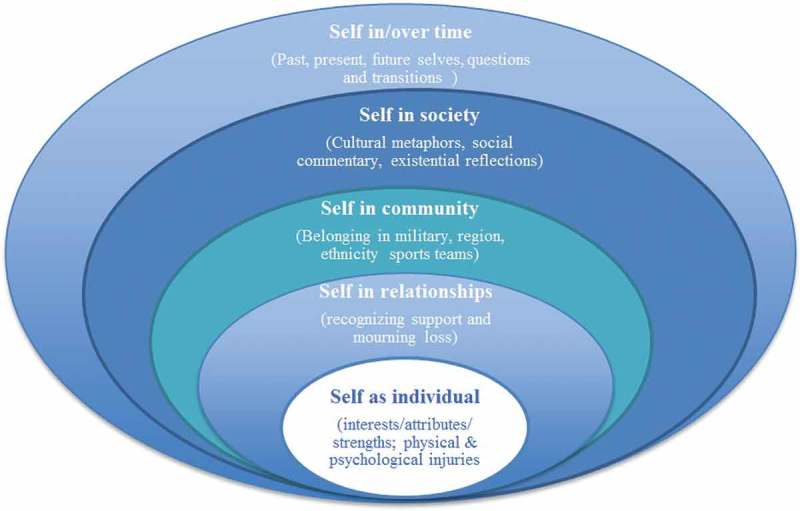
Framework of representations of self as seen in mask imagery.
Table 1 depicts the themes from the framework above and the number of participants who included these themes in their masks. Note that each mask might represent more than one theme.
Table 1.
Number of participants related to types of representation of self (n = 370).
| Type of representation of self | Number of participants |
|---|---|
| Self as individual | |
| Physical injuries | 116 |
| Psychological injuries | 106 |
| References to positive attributes of self and interests | 13 |
| Self in relationships | |
| Recognizing support | 29 |
| Mourning loss (lost or difficult relationships) | 28 |
| Self in community | |
| References to belonging in military identity/division/unit | 102 |
| References to regional/ethnicity/teams etc. | 42 |
| Self in society | |
| Cultural metaphors | 77 |
| Existential reflections | 26 |
| Self over time | |
| Mask representing life story | 51 |
| Questions and transitions | 24 |
| Conflicted or split sense of self | |
| Representing two selves from any of the above categories | 84 |
Physical injuries
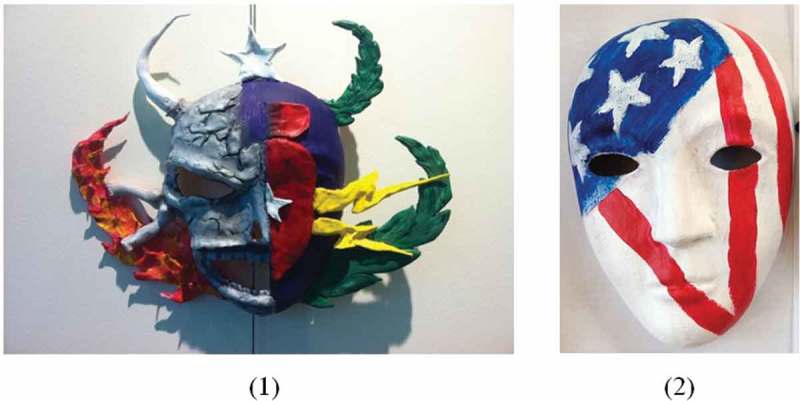
Two of the most common themes, physical and psychological injuries, were evident in the masks related to different manifestations of the injured self, with only a few participants referring to individual strengths and personal interests (n = 13). Many participants, however, referred to the individual self as injured and included graphic representations of both physical (n = 116) and psychological (n = 106) injuries to their brains. They symbolized their physical and/or brain injury experiences through graphic representations of the injury location, representations of physical pain (e.g., bruises, scars, and ongoing challenges with cognitive and sensory functioning). See Figure 2.
Figure 2.
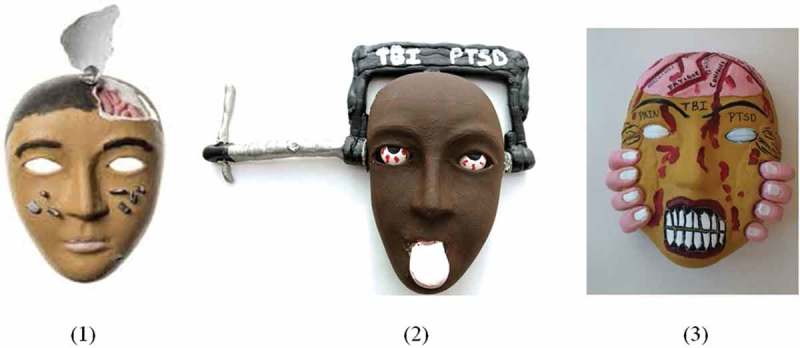
Examples of masks imaging injuries sustained during deployment representing: (1) where the service member’s skull was removed, the metal pieces on the cheeks represent shrapnel; (2) the pain and pressure of headaches resulting from TBI and PTSD; (3) the service member’s frustration with the pain caused by the injuries.
Psychological injuries and challenges
Many participants (n = 106) referred to the psychological and emotional challenges and TBI/PTSD symptoms resulting from their wartime experiences (e.g., an inability to express oneself; struggles with managing depression, anxiety, and anger). The inability to express oneself was frequently represented with lips sealed, stitched, or locked. Figure 3 provides examples of these injuries represented through color, stitches, and facial expressions of sadness and/or anger.
Figure 3.
Examples of masks showing psychological injuries and challenges representing: (1) the inability to speak and communicate about traumatic memories; (2) the service member’s feeling of being “broken” after seven deployments (represented through seven fragments) and his process of healing and being “stitched back together.”
Relationships—recognizing support and mourning loss
Some participants (n = 29) made masks in honor of living family members who might have been suffering from the impact of the injury on their familial relationships. These references recognized the support family members provided and a sense of guilt and remorse for relationships impaired due to the mood and functional struggles associated with PTSD and TBI. Some participants (n = 28) referred to their loss of comrades in the warzone, feelings of guilt about being a survivor in a raid or attack that killed several of their peers, and grief for many relational losses among their peers and relationships with family members. This grief was represented in the masks through imagery that memorializes comrades killed in action (see Figure 4).
Figure 4.
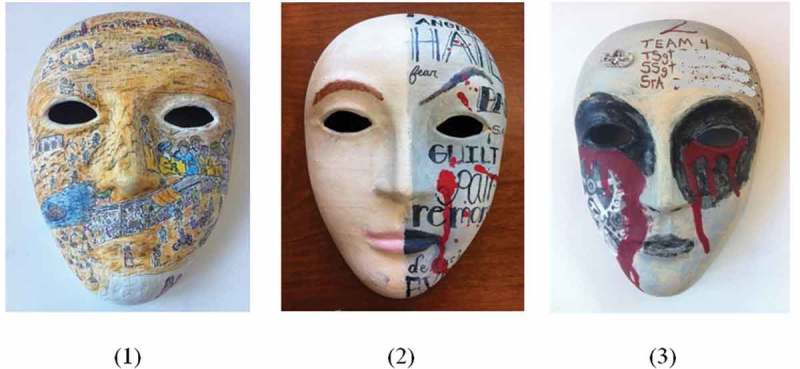
Masks with references to family, comrades killed in action: (1) a recreation of several scenes from deployment on the mask with a white patch with his family drawn in on the chin to represent how he felt the family “took the brunt” of his injuries, (2) reference to moral injuries including feelings of guilt and remorse surrounding wartime losses; (3) a memorial to comrades (names blurred for confidentiality) with tears of blood from the eyes and names of those killed or injured when he sustained his TBI.
Military and community identity
Reflecting the strong sense of pride and belonging to the military community, many participants (n = 102) referred to their military branch using symbols (e.g., US flag, camouflage cloth, colors, weapons, insignia). Others (n = 42) referred to their home state, geographical region, ethnicity, or even sports teams to represent an aspect of self as belonging to a group or community (see Figure 5).
Figure 5.
Masks related to a military and community identity: (1) a recreation of the Explosive Ordnance Disposal (EOD) badge, often referred to as an “EOD crab,” signifying his military occupation—he also chose to display his mask in the clinic as a way to connect with and “inspire others”; (2) the military unit SEAL Team VI (six), symbolized using the stars and stripes of the US flag and the Roman numeral for six.
Cultural metaphors and existential reflections
Some participants (n = 77) used the mask to represent themselves in relation to aspects of society, including metaphorical use of cultural symbols like superheroes and/or villains from movies. In describing the masks, participants referred to the masks as representing an aspect of themselves, but seen metaphorically through a societal symbol (see Figure 6).
Figure 6.
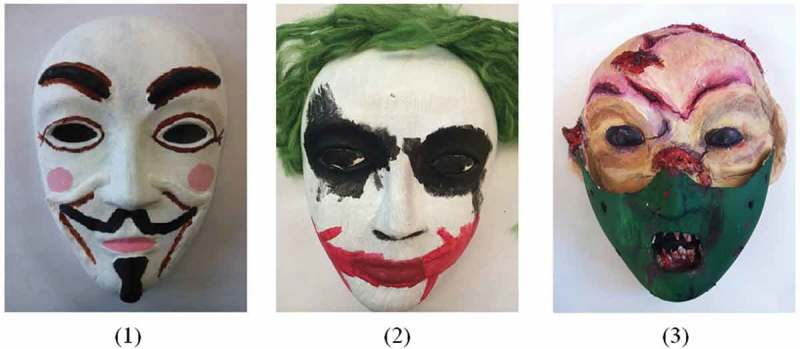
These images include characters from popular films with antagonistic roles: (1) a recreation of the Guy Fawkes mask worn in the movie V for Vendetta–Guy Fawkes also has cultural resonance with service members in Explosive Ordnance Disposal due to his historical ties to a plot involving explosives; (2) the Joker from Batman; (3) a mix between the character Hannibal Lecter from Silence of the Lambs and an evil clown.
A few service members (n = 26) commented on their political thoughts reflecting disillusionment and existential concerns. These references included existential reflections on the purpose of the wars and deployments including deaths of comrades and injuries sustained, struggling to return to life in peacetime after deployment, struggling to receive quality healthcare and support after sustaining injuries, and feeling alienated from society and/or frustrated by the lack of understanding of the military experience, and the perception that there is too much importance placed on superficial concerns (see Figure 7). Some representative examples are included in Figure 7. The service member who created the third mask (7c) stated “the evils of war wounded my soul pieced and held together by past hopes, dreams, and happiness with loved ones that no longer exist the way they did before the experiences of its horrors” (NICoE patient, personal communication, 31 May 2016).
Figure 7.
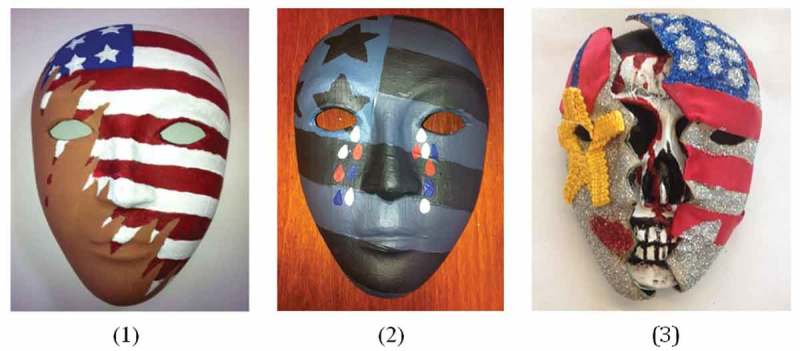
The masks above represent some of the service members’ frustrations and existential reflections with military experiences: (1 and 2) these represent sadness (tears) and the conflict between the suffering experienced and the desire to perform their patriotic duties as represented by shredded and colorless flags; (3) represents an exterior of honor and passion when serving in the military (i.e., a glittering US flag and Bronze Star Medal he earned for heroic actions in combat). The mask opens up to reveal a bloody skull which symbolizes war and the underlying injuries and exposure to death/evil.
Mask as life story, questions, transitions
Some participants (n = 51) used the mask-making to reflect on and represent their life as a story over time, representing aspects of their past, present, and/or future self. Some (n = 24) were hopeful for their future as a result of treatment at NICoE, while others (n = 24) had lingering questions and struggled with the uncertainties of their future in the military or as retired veterans (see Figure 8).
Figure 8.

These masks depict uncertainty regarding current clinical symptoms and future prognosis: (1) represents questions around his condition and uncertainty about his future; (2) represents the service member’s feeling that part of him is confused and unsure of his condition while the rest of him is hopeful for the future and possibilities for recovery.
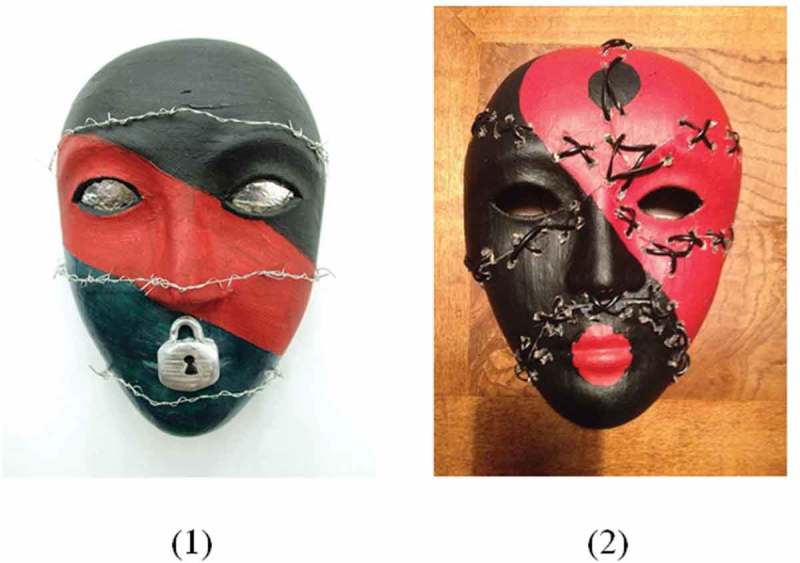
Conflicted/split sense of self
Many participants (n = 84) represented the recurring theme of a divided or split sense of self. This was visually depicted most often by a vertical demarcation on the mask dividing it into two sections. The divided self could depict a variety of different representations of self (e.g., injured/healthy, angry/peaceful, past/present, deployed self/family self). The divided masks were represented as two aspects of self that exist in tandem or as two conflicting parts of self (see Figure 9).
Figure 9.

Mask examples representations of conflicted/divided aspects of self. (1) represents the service member’s experiences of dramatic anger and intense sadness; (2) represents the service member’s struggle to keep his angry side (left) from taking over his peaceful side (right).
As presented in Figures 1 through 9, patients used mask making to represent a spectrum of experiences and perspectives. Several service members referred to the challenges of identity, pain, and personal and relational struggles sustained as a result of combat experiences, while others reflected on existential questions and referred to community as a source of pride and belonging. In the absence of readily expressible verbal language, the masks provided service members with an opportunity to express their experiences artistically through non-verbal media.
Discussion and implications
This study highlights, in particular, some of the “invisible wounds” of war (Lobban, 2014) and the toll these experiences have taken on the lives of the study’s participants, injured in combat or mission related activities, and their families. The images also highlighted the graphic experience of PTSD and TBI and connections to aspects of functioning that are not represented in the literature. For example, the cognitive and physical tasks involved in art-making can offer assessment opportunities, outcome improvement, and therapeutic, artistic, and verbal processing of these physical and brain injury experiences (David, 1999). Art therapy can uncover unconscious material through art-making, which can then be cognitively and verbally decoded, thus reducing some of the symptoms associated with psychological injury, such as avoidance, to help improve insight and tolerance of trauma-related emotions (Lobban, 2014). The externalization of some these internal struggles offered many participants a way to talk about their unseen wounds and struggles by referring to an object—an integrated visual image in the form of a mask. It also offered an alternative visual mode of communication with caregivers and family (e.g., talking about the mask and taking it home) and comrades (e.g., building a virtual community through the masks when exhibited in the studio). When combined with an interdisciplinary team approach (e.g., NICoE), discoveries made by the patient and art therapist can then be shared and incorporated into a comprehensive treatment plan.
Several of the masks referred to emotional struggles around managing overwhelming emotions (e.g., anger and sadness represented frequently in shades of “darker” colors; explosive emotions in the form of fire, lightning, or explosions referring to anxiety as being “on edge”). Symptoms of PTSD (e.g., hyper vigilance) were represented in exaggerated bloodshot eyes and eyeballs creating visceral imagery that highlighted these unseen struggles and their inability to express them in words (e.g., mouths “sealed” or “locked”) in ways not adequately covered in the literature. Furthermore, engaging in a group art therapy setting provided an opportunity for others suffering with similar feelings the chance to provide positive feedback in a nonjudgmental and safe environment.
Many service members also represented a feeling of being “broken” (e.g., literally cutting up and piecing together their masks). For any individual, memories may be recalled in fragments, where important pieces of a story, narrative, or memory may be missing (Rubin, Feldman, & Beckham, 2004). When considering PTSD’s traumatic psychological experiences and TBI’s traumatic brain and physical experiences, this problematic recall and fragmentation may be exacerbated. Some components of a trauma memory may be unprocessed, remaining in the unconscious, while others may be more vividly and readily accessible for recall (Rubin et al., 2004). Fragmentation can also manifest with regards to the sense of self in complex trauma cases (Herman, 1992). Mask-making then becomes more than an activity. It has the potential to be a therapeutic modality that literally and metaphorically pieces together the fragments of the traumatic memory into an externalized coherent narrative representation of self. This in turn helps the service member communicate with family, clinicians, and caregivers about their vulnerabilities and challenges externalizing their thoughts with masks.
Moral struggles related to combat action and the expression of grief and loss were themes that emerged through some of the masks. Losing comrades in combat may be an inevitable experience for a military service member. Toblin and colleagues (2012) found that 21.3% of soldiers (n = 1522) experienced challenges when coping with and grieving the loss of someone close and that grief significantly contributed to poor general health and occupational impairment (e.g., physical task challenges, missed work). Sensitivity to the bereavement process, acknowledgement and validation of loss experience, and accommodations for treating grief alongside PTSD and TBI symptoms are imperative for any mental health practitioner working with military service members and combat veterans (Coll, Weiss, & Yarvis, 2011). The masks in our study highlighted the relational aspect of many of the moral injuries as they explored feelings of survivor’s guilt when comrades were killed, being an angry or unavailable partner or parent, and guilt and shame related to wartime actions. Making these masks enabled the service members in our study to create an external visible image which in turn helped them reference their experiences to their family and clinicians.
Many service members created masks that included symbols of military identity and references to patriotism, pride, and a sense of belonging to a specific military branch or unit (e.g., US flag, camouflage designs, unit symbols, weapons, helmets, dog tags). Some also left the mask behind “to inspire” others from their units implicitly communicating a strong sense of camaraderie and community within the military identity. Symbols can take a personal and/or universal form, where the intention of the symbolic expression may not yet be conscious to the mask maker.
In some cases, the military identity was used to link broader existential questions and concerns. For example, service members made masks with ripped flags or made the stripes on the flag look like streaks of blood, highlighting the struggle with what is perceived as a disconnect with society and the country after the service member returned home from deployment. The subjective and existential nature of this theme is an important finding and is an area for future in-depth inquiry. The brief clinical documentation notes used for analysis in this study, however, limit further interpretation of this theme in this paper.
While at the NICoE, many service members sought answers to questions regarding their health and recovery, as well as treatment concerns. This has been found to be related to previous or current distrust in healthcare providers, symptom and medication concerns, and uncertainty about length or outcome of treatment—all of which can be additional burdens on service members struggling with PTSD and/or TBI (Zinzow et al., 2013). Career or future expectations may change from the traumatic injury or event. Adjustments may be needed to learn how to recover, bringing about a great deal of questioning and uncertainty during this process (Hyatt, Davis, & Barros, 2015). Some service members represented hope for the future via new career options and potential for recovery, while others struggled with questions and uncertainty about the future, including their loss of a professional identity. Physical, traumatic injury can leave permanent memories, where artwork, such as mask making, can provide a space to explore experiences nonverbally. Mask making can offer service members the opportunity to explore feelings of duality, conflict, and divide, which can later be verbally processed and integrated into treatment.
A large number of service members represented a divided or dual sense of self; that is, the mask might be visually divided into two segments (e.g., past/present, health/injured, military/civilian). This duality might be aspects of self in alignment or in conflict, as in the cases of service members who represented duality in an angry and peaceful side or work and family side. Post-traumatic stress disorder can cause a personality dissociation where the normally functioning daily self that is presented to the world conflicts with the emotional, traumatized, internal self, which causes veterans to feel as if they are coping through a mask rather than their real selves (Lobban, 2014). Feelings of duality or a split sense of self are reported in the literature (Delgado Martinez, 2013; Kroch, 2009). The masks made by the service members in our study served the unique role of literally and metaphorically externalizing these inner experiences and helping communicate these struggles.
The authors also recognize that while this study analysed masks made by US military service members with TBI and PTSD, there are broader implications for the global use of art therapy with this population. In her report, Churchill Fellow Lobban (2016) stated that “there is a strong resonance” between the symbolism expressed by US service members at the NICoE and British service members who engaged in art therapy for PTSD at Combat Stress in the UK. Furthermore, after visiting facilities in both Israel and the USA, to include the NICoE, Australian Churchill Fellow Dena Lawrence (2012) published a similar report recognizing the need for art therapy treatment for Australian service members.
Conclusion
Art therapy imagery provides a graphic representation of some of the unseen struggles, challenges, and lived experiences of active-duty military service members who have sustained TBI, PTSD, and comorbid psychological disorders. This paper identified themes in service members’ visual representations of self through masks including: references to physical, psychological, and moral injuries; grief for lost abilities and lost comrades; struggles with transitions and questions about future; and a divided sense of self and disillusionment with their role in and outcomes of war. The findings serve to highlight the lived experience and “unseen” struggles of active-duty service members with PTSD, TBI, and co-morbid mood disorders. This in turn offers clinicians in integrative medical care settings an avenue to understand service members’ experiences beyond narrative descriptions alone.
Acknowledgments
The first and second authors contributed equally to this manuscript. The authors would like to thank Dr Jesus Caban, Ms Kathy Williams, Col Geoffrey Grammer, Dr Barbara Granger, and Ms Kendra Ray for helping with various stages of the manuscript.
Funding Statement
This work was supported by the National Endowment for the Arts.
Disclosure statement
No potential conflict of interest was reported by the authors. The views expressed in this analysis are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Army, or Air Force, the Department of Defense, nor any agency of the U.S. Government. The identification of institutional logos, specific products, or scientific instrumentation does not constitute endorsement or implied endorsement on the part of the authors, DoD, or any component agency.
References
- Agberia J. T. Aesthetics and rituals of the opha ceremony among the Urhobo people. Journal of Asian and African Studies. 2006;41:249–12. doi: 10.1177/0021909606063880. [DOI] [Google Scholar]
- Akpan J. J. Ekpo society masks of the Ibibio. African Arts. 1994;27(4) doi: 10.2307/3337318. [DOI] [Google Scholar]
- American Art Therapy Association Use of art therapy in the treatment of veterans [PDF file] 2009 http://www.arttherapy.org/upload/useofarttherapywithveterans.pdf Retrieved from. [Google Scholar]
- Andrew E. H.2014Cross-Cultural Communication104211–216.Retrieved fromhttp://www.cscanada.net/index.php/css/article/view/5100 10.3968/5100 [DOI] [Google Scholar]
- Bahraini N. H., Breshears R. E., Hernández T. D., Schneider A. L., Forster J. E., Brenner L. A. Traumatic brain injury and posttraumatic stress disorder. Psychiatric Clinics of North America. 2014;37(1):55–75. doi: 10.1016/j.psc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- Blakeley K, Jansen D. J. Post-traumatic stress disorder and other mental health problems in the military: Oversight issues for Congress. Washington, DC: Congressional Research Service, Library of Congress; 2013. [Google Scholar]
- Chen D. Gallery: How these powerful masks are helping combat veterans heal [Web log post] 2016 Nov 11; http://ideas.ted.com/gallery-how-these-powerful-masks-are-helping-combat-veterans-heal/ Retrieved from. [Google Scholar]
- Coll J. E., Weiss E. L., Yarvis J. S. No one leaves unchanged: Insights for civilian mental health care professionals into the military experience and culture. Social Work in Health Care. 2011;50(7):487–500. doi: 10.1080/00981389.2010.528727. [DOI] [PubMed] [Google Scholar]
- Collie K., Backos A., Malchiodi M. 4. Vol. 23. Art therapy for combat-related PTSD: Recommendations for research and practice. Art Therapy: Journal of the American Art Therapy Association; 2006. pp. 157–164. Spiegel, D. [Google Scholar]
- Corbin J. M., Strauss A. Basics of qualitative research: Techniques and procedures for developing grounded theory (3rd ed.) Los Angeles, CA: Sage; 2008. [Google Scholar]
- David I. R. 1999 http://search.proquest.com/docview/304569092 [Google Scholar]
- Defense and Veterans Brain Injury Center DoD Worldwide numbers for TBI [PDF file] 2016 http://dvbic.dcoe.mil/sites/default/files/DoD-TBI-Worldwide-Totals_2000-2015_Q1-Q4_March-30-2016_v1.0_2016-04-14.pdf Retrieved from. [Google Scholar]
- Delgado Martinez R. E. Phenomenology of blast-induced traumatic brain injury in military personnel. University of Texas; El Paso: 2013. Doctoral dissertation. [Google Scholar]
- Diakparomre A. M. Symbolism in Urhobo masks and mask performances. Journal of Asian and African Studies. 2010;45(5):467–484. doi: 10.1177/0021909610373220. [DOI] [Google Scholar]
- Dolan S., Martindale S., Robinson J., Kimbrel N. A., Meyer E. C., Kruse M. I., Gulliver S. B. Neuropsychological sequelea of PTSD and TBI following war deployment among OEF/IEF veterans. Neuropsychological Review. 2012;22(1):21–34. doi: 10.1007/s11065-012-9190-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dursa E. K., Reinhard M. J., Barth S. K., Schneiderman A. I. Prevalence of a positive screen for PTSD among OEF/OIF and OEF/OIF‐era veterans in a large population‐based cohort. Journal of Traumatic Stress. 2014;27(5):542–549. doi: 10.1002/jts.21956. [DOI] [PubMed] [Google Scholar]
- Fear N. T., Jones M., Murphy D., Hull L., Iversen A. C., Coker B., Wessely S. What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? A cohort study. The Lancet. 2010;375(9728):1783–1797. doi: 10.1016/S0140-6736(10)60672-1. [DOI] [PubMed] [Google Scholar]
- Fiet L. Mask-making and creative intelligence in transcultural education. Caribbean Quarterly. 2014;60(3):58–72. doi: 10.1080/00086495.2014.11672526. [DOI] [Google Scholar]
- Frenz M. Combat veterans diagnosed with posttraumatic stress disorder: The effect on their children: A phenomenological study. (Order No. 3289584) 2007 http://search.proquest.com/docview/304730772?accountid=10559 Available from ProQuest Dissertations & Theses Global. (304730772) Retrieved from.
- Fryrear J. L., Stephens B. C. Group psychotherapy using masks and video to facilitate intrapersonal communication. The Arts in Psychotherapy. 1988;15:227–234. doi: 10.1016/0197-4556(88)90007-X. [DOI] [Google Scholar]
- Furuki K. “Masking” and “unmasking” Korean adoptees–on Rick Shiomi’s mask dance. Euramerica. 2011;41(4):949–976. [Google Scholar]
- Golub D. Symbolic expression in post-traumatic stress disorder: Vietnam combat veterans in art therapy. The Arts in Psychotherapy. 1985;12:285–296. doi: 10.1016/0197-4556(85)90041-3. [DOI] [Google Scholar]
- Herman J. L. Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress. 1992;5(3):377–391. doi: 10.1002/(ISSN)1573-6598. [DOI] [Google Scholar]
- Hines-Martin V. P., Ising M. The use of art therapy with post-traumatic stress disordered veteran clients. Journal of Psychosocial Nursing and Mental Health Services. 1993;31(9):29–36. doi: 10.3928/0279-3695-19930901-09. [DOI] [PubMed] [Google Scholar]
- Hinz L. D., Ragsdell V. Using masks and video in group psychotherapy with bulimics. The Arts in Psychotherapy. 1990;17:259–261. doi: 10.1016/0197-4556(90)90009-F. [DOI] [Google Scholar]
- Hogan S. Healing arts: The history of art therapy. London: Jessica Kingsley; 2001. [Google Scholar]
- Hyatt K. S., Davis L. L., Barroso J. Finding the new normal: Accepting changes after combat-related mild traumatic brain injury. Journal of Nursing Scholarship. 2015;47(4):300–309. doi: 10.1111/jnu.2015.47.issue-4. [DOI] [PubMed] [Google Scholar]
- Jain S., McMahon G. F., Hasen P., Kozub M. P., Porter V., King R., Guarneri E. M. Healing touch with guided imagery for PTSD in returning active duty military: A randomized controlled trial. Military Medicine. 2012;177(9):1015–1021. doi: 10.7205/MILMED-D-11-00290. [DOI] [PubMed] [Google Scholar]
- Jiachiao L. Sculpture-mask under the environment of Chinese rock painting art. Cross Cultural Communications. 2013;9(5):47–54. [Google Scholar]
- Kopytin A., Lebedev A. Humor, self-attitude, emotions, and cognitions in group art therapy with war veterans. Art therapy: Journal of the American Art Therapy Association. 2013;30(1):20–29. doi: 10.1080/07421656.2013.757758. [DOI] [Google Scholar]
- Kroch R. Living with military-related Posttraumatic Stress Disorder (PTSD) - A hermeneutic phenomenological study [Doctoral thesis] 2009. http://www.collectionscanada.gc.ca/obj/thesescanada/vol2/002/NR54472.PDF Retrieved from. [Google Scholar]
- Lande R. G, Tarpley V, Francis J. L, Boucher R. Combat trauma art therapy scale. The Arts in Psychotherapy . 2010;37(1):42–45. [Google Scholar]
- Lawrence D. To investigate the use of art therapy for post traumatic stress disorder in hospitals, clinics and centers in USA and Israel [PDF file] 2012 https://www.churchilltrust.com.au/media/fellows/2012_Lawrence_Dena_1.pdf Retrieved from. [Google Scholar]
- Lobban J. The invisible wound: Veterans’ art therapy. International Journal of Art Therapy: Formerly Inscape. 2014;19(1):3–18. doi: 10.1080/17454832.2012.725547. [DOI] [Google Scholar]
- Lobban J. Art therapy for military veterans with PTSD [PDF file] 2016 http://www.wcmt.org.uk/sites/default/files/reportdocuments/Lobban%20J%20Report%202016%20Final.pdf Retrieved from. [Google Scholar]
- Malchiodi C. A. Art therapy with combat veterans and military personnel. In: Malchiodi C. A., editor. Handbook of art therapy. 2nd. New York, NY: Guilford Press; 2012. pp. 320–334. [Google Scholar]
- Medina V., Koui T. After the we mask in Ivory coast: Preliminary study about its origin, symbolism and value as element of communication. Coolabah. 2009;3:235–243. [Google Scholar]
- Nanda U., Gaydos H. L. B., Hathron K., Watkins N. Art and posttraumatic stress: A review of the empirical literature on the therapeutic implications of artwork with war veterans with posttraumatic stress disorder. Environment and Behavior. 2010;42(3):376–390. doi: 10.1177/0013916510361874. [DOI] [Google Scholar]
- North Atlanta Treaty Organization NATO and Afghanistan. 2016 http://www.nato.int/cps/en/natohq/topics_8189.htm Retrieved from. [Google Scholar]
- Pachalska M., Pronina M. V., Manko G., Chantsoulis M., Luckos M., Kroptov J. D. Evaluation of neurotherapy program for a patient with clinical symptoms of schizophrenia and severe TBI using even-related potentials. Neuropsychologica. 2013;11:435–449. [Google Scholar]
- Paoletti J. T. Michelangelo’s masks. The Art Bulletin. 1992;74(3):423–435. doi: 10.2307/3045891. [DOI] [Google Scholar]
- Pollock D. Masks and the semiotics of identity. The Journal of the Royal Anthropological Institute. 1995;1(3):581–597. doi: 10.2307/3034576. [DOI] [Google Scholar]
- Reijnen A., Rademaker A. R., Vermetten E., Geuze E. Prevalence of mental health symptoms in Dutch military personnel returning from deployment to Afghanistan: A 2-year longitudinal analysis. European Psychiatry. 2015;30(2):341–346. doi: 10.1016/j.eurpsy.2014.05.003. [DOI] [PubMed] [Google Scholar]
- Rona R. J., Jones M., Fear N. T., Hull L., Murphy D., Machell L., Wessely S. Mild traumatic brain injury in UK Military personnel returning from Afghanistan and Iraq: Cohort and cross-sectional analyses. Journal of Head Trauma Rehabilitation. 2012;27(1):33–44. doi: 10.1097/HTR.0b013e318212f814. [DOI] [PubMed] [Google Scholar]
- Rubin D. C., Feldman M. E., Beckham J. C. Reliving, emotions, and fragmentation in the autobiographical memories of veterans diagnosed with PTSD. Applied Cognitive Psychology. 2004;18(1):17–35. doi: 10.1002/(ISSN)1099-0720. [DOI] [Google Scholar]
- Sargent P., Campbell J., Richter K. E., McLay R. N., Koffman R. L. Integrative medical practices for combat-related posttraumatic stress disorder. Psychiatric Annals. 2013;43:181–187. doi: 10.3928/00485713-20130403-10. [DOI] [Google Scholar]
- Stein M. B., Kessler R. C., Heeringa S. G., Jain S., Campbell-Sills L., Colpe L. J., Army STARRS Collaborators Prospective longitudinal evaluation of the effect of deployment-acquired traumatic brain injury on posttraumatic stress and related disorders: Results from the Army Study to Assess Risk and Resilience in Service members (Army STARRS) American Journal of Psychiatry. 2015;172(11):1101–1111. doi: 10.1176/appi.ajp.2015.14121572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanielian T, Jaycox L. Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. Pittsburgh, PA: RAND Corporation; 2008. [Google Scholar]
- Toblin R. L., Riviere L. A., Thomas J. L., Adler A. B., Kok B. C., Hoge C. W. Grief and physical health outcomes in US soldiers returning from combat. Journal of Affective Disorders. 2012;136(3):469–475. doi: 10.1016/j.jad.2011.10.048. [DOI] [PubMed] [Google Scholar]
- U.S. Government Accountability Office VA mental health: Number of veterans receiving care, barriers faced, and efforts to increase access (GAO-12-12) [PDF file] 2011 http://www.gao.gov/assets/590/585743.pdf Retrieved from. [Google Scholar]
- Van Der Kolk B. The body keeps the score: Brain, mind, and body in the healing of trauma. New York, NY: Sage; 2014. [Google Scholar]
- Walker M., Kaimal G., Koffman R., DeGraba T. J. Art therapy for PTSD and TBI: A senior active duty military service member’s therapeutic journey. The Arts In Psychotherapy. 2016 doi: 10.1016/j.aip.2016.05.015. [DOI] [Google Scholar]
- Wall P. L. Posttraumatic stress disorder and traumatic brain injury in current military populations: A critical analysis. Journal of the American Psychiatric Nurses Association. 2012;18(5):278–298. doi: 10.1177/1078390312460578. [DOI] [PubMed] [Google Scholar]
- Yurgil K., Barkauskas D., Vasterling J. J., Nivergelt C., Larsan G., Schork N., Baker D. G. Association between traumatic brain injury and risk of posttraumatic stress disorder in active-duty marines. JAMA: The journal of the American Medical Association. 2014;71(2):149–157. doi: 10.1001/jamapsychiatry.2013.3080. [DOI] [PubMed] [Google Scholar]
- Zinzow H. M., Britt T. W., Pury C. L., Raymond M. A., McFadden A. C., Burnette C. M. Barriers and facilitators of mental health treatment seeking among active-duty army personnel. Military Psychology. 2013;25(5):514–535. doi: 10.1037/mil0000015. [DOI] [Google Scholar]


