Abstract
Background
Payers and policy makers rely on studies of trends in Acute Myocardial Infarction (AMI) hospitalizations and spending that count only hospitalizations where the AMI is the principal discharge diagnosis. Hospitalizations with AMI coded as a secondary diagnosis are ignored. The effects of excluding these hospitalizations on estimates of trends are unknown.
Methods
Observational study of all AMI hospitalizations in Fee-for-Service Medicare beneficiaries ages 65 and over, from 2002 through 2011.
Results
We studied 3,663,137 hospitalizations with any AMI discharge diagnosis over 288,873,509 beneficiary-years. Of these, 66% had AMI coded as principal (versus secondary). From 2002 to 2011, AMI hospitalization rates declined 24.5% (from 1,485 per 100,000 beneficiary-years in 2002 to 1,122 in 2011). Meanwhile, the proportion of these hospitalizations with a secondary AMI diagnosis increased from 28% to 40%; by 2011 these secondary AMI hospitalizations accounted for 43% of all expenditures for hospitalizations with AMI, or $2.8 billion. Major changes in comorbidities, principal diagnoses and mean costs for hospitalizations with a non-principal AMI diagnosis occurred in the 2006-2008 timeframe.
Conclusions
Current estimates of the burden of AMI ignore an increasingly large proportion of overall AMI hospitalizations and spending. Changes in the characteristics of hospitalizations that coincided with major payment and policy changes suggest that non-clinical factors affect AMI coding. Failing to consider all AMIs could inflate estimates of population health improvements, underestimate current and future AMI burden and expenditures, and overestimate the value of AMI prevention and treatment.
INTRODUCTION
Accounting for as much as 17% of all national healthcare expenditures, cardiovascular disease (CVD) remains a leading cause of morbidity, mortality and cost in the United States.1 Acute Myocardial Infarction (AMI), a common manifestation of CVD in the elderly, carries increased risks of morbidity, mortality, and excess costs.2,3,4 Policy makers use estimates of AMI burden to assess population health, to identify opportunities to improve health, and to set healthcare budgets. In turn, national data agencies, such as the Centers for Disease Control and Prevention (CDC), use these estimates to guide surveillance activities that monitor and evaluate health system performance,5-7 and funding agencies, like the National Institutes of Health (NIH), use them to set research priorities. Because nearly all AMI patients are hospitalized, hospitalization data are used to estimate morbidity, mortality and expenditures attributable to AMI,8,9,10,11,12,13 making accurate tracking of AMI hospitalizations important for national health accounting.
Several recent studies reporting steep declines in AMI hospitalization rates 9,11,12,14,15 have been interpreted as evidence of dramatic improvements in cardiovascular health. However, these studies count only a subset of AMIs – those that appear as the principal diagnosis on a hospital discharge abstract; they do not count hospitalizations when the AMI is coded in other positions. Most hospitalized patients receive care for multiple problems, and the principal diagnosis should reflect “the condition established after study to be chiefly responsible for the (patient’s) admission” while conditions that coexisted when the patient was admitted to the hospital – or developed during the hospitalization – should be coded as secondary diagnoses.16 The single, chief reason for a hospitalization, however, may be clinically ambiguous, particularly in patients with multiple, serious conditions, in which case non-clinical considerations can influence which diagnosis gets coded first. One important non-clinical consideration is that the principal diagnosis largely determines the Diagnosis Related Group (DRG) used by the Centers for Medicare and Medicaid Services (CMS) to calculate hospital payment. For example, in 2008, coding septicemia as principal and AMI second would lead to 3.3 times more reimbursement than if the codes were reversed, whereas in the 2006 Medicare reimbursement schema, reversing the order of these two diagnoses had minimal effect on payment.17,18 To the extent that reimbursement rules or other non-clinical factors affect hospital decisions to code AMI as the principal discharge diagnosis, national reports of AMI trends based only on principal diagnoses may overestimate the success of national AMI prevention efforts, underestimate the current burden of AMI, and understate opportunities to save both money and lives.
To describe the full burden of AMI hospitalizations, including those that usually go uncounted, we examined all hospitalizations with any discharge diagnosis for AMI from 2002 to 2011. Specifically, we calculated age-sex adjusted AMI hospitalization rates in total, and separately, for when the AMI is coded as principal versus secondary, that is, in any position other than the first-listed discharge diagnosis; we refer to these hospitalizations as principal and secondary AMI, respectively. To explore differences between the two kinds of admissions, we compared rates of cardiac- and non-cardiac-related comorbidities, and longitudinal changes in these rates, in patients with first- versus second-listed AMIs. Further, since CMS payments for hospitalizations are based primarily on the principal diagnosis, we examined changes in the distributions of principal diagnoses in patients with second-listed AMIs. We were especially interested in coding changes over the 2006-2008 timeframe, since CMS made major changes to its DRG methodology with the Medicare Severity (MS) DRGs, introduced in October, 2007.19
METHODS
Data
This investigation used the CMS 100% sample Medicare Provider Analysis and Review (MedPAR) files linked to Medicare Denominator files for the years 2002-2011. The MedPAR files contain hospital discharge abstracts for the acute-care hospitalizations of all Medicare beneficiaries with Part A coverage, including admission and discharge dates, admission source, International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes, discharge disposition, total charges, covered charges, and Medicare reimbursement. The Medicare denominator files include information on beneficiaries’ dates of birth, sex, race (categorized as black, white, or other), enrollment status, region of residence, and vital status (including date of death). To limit the potential effects of a change in the definition of AMI made by the American College of Cardiology and the European Society of Cardiology in 2000, we began our study with 2002 data.20
Study Population
We studied residents of U.S. states, the District of Columbia and Puerto Rico enrolled in Medicare fee-for-service (FFS) coverage between January 1, 2002 and December 31, 2011. We excluded beneficiaries during months in which they lacked Medicare Part A coverage or were enrolled in a Medicare HMO, since their hospitalization claims were only sporadically submitted for reimbursement. Because individuals can move in and out of FFS coverage, and because they become age-eligible for Medicare on the first day of the month in which they turn 65, we used a study denominator of eligible beneficiary months aggregated into beneficiary-years.
Outcomes
Our key outcomes were annual AMI hospitalization rates in each calendar year, 2002-2011, and expenditures for these hospitalizations, calculated separately for when AMI was coded as the principal or a secondary diagnosis. Expenditures, reported in nominal dollars, included Medicare reimbursements to hospitals and the required patient co-payments for hospitalizations. Our analysis counted each AMI hospitalization, including multiple admissions for the same patient in a year. We identified AMI hospitalizations as those with a discharge diagnosis of AMI (410.xx, excluding 410.x2) coded in any position. Hospital transfers within this set of AMI hospitalizations (i.e., admissions occurring within one day of discharge from another hospital) were linked and treated as a single episode of AMI hospitalization. When the episode included hospitalizations with AMI discharge diagnoses in both principal and secondary positions, we classified it using the diagnosis position of the AMI from the first hospitalization with a length of stay greater than one day. If each hospitalization contributing to an episode lasted just one day, we used the diagnosis position from the first hospitalization, unless the patient died, in which case, we used its position in the final hospitalization.
Following common practice, we excluded non-transfer hospitalizations with length of stay less than two days if the patient was discharged alive and not against medical advice, as these hospitalizations were unlikely to have been for an AMI.21 We attributed hospitalizations spanning more than one calendar year to the admission year.
Analyses
We calculated annual overall AMI hospitalization rates per 100,000 beneficiary-years for each year from 2002 to 2011 and, separately, rates for principal versus secondary AMIs. All rates were adjusted to the age-sex-race distribution of the 2007 Medicare population using direct standardization. To appraise trends in AMI hospitalization coding, we examined changes in the proportion of all AMI hospitalizations coded as secondary. To explore differences over time in patients with principal and secondary AMI, we compared rates of common cardiac- and non-cardiac-related comorbid conditions for admissions in which the AMI was either the first-listed (that is, principal) or second-listed discharge diagnosis. To identify these comorbidities, we first examined the top 10 ICD-9 diagnoses coded in any position in each year for hospitalizations with a principal AMI diagnosis, and, separately, for hospitalizations with a second position AMI diagnosis; we then grouped diagnoses for the same comorbidity, identified occurrences of additional ICD-9 diagnoses for that comorbidity, and used these ICD-9 codes to estimate the prevalence of each comorbidity in each year. We also examined changes in the most common first-listed diagnoses for AMI hospitalizations where the AMI was coded second, paying special attention to changes occurring between 2006, the last full year that the older DRG version was in place, and 2008, the first full year for the new version. We were concerned that AMIs coded in secondary positions might be consequent to non-cardiac surgical procedures. Although the discharge claim contains no information about timing, we explored this by examining the prevalence of admissions with cardiac and non-cardiac-related procedures (Appendix D includes the ICD-9 procedure codes), separately for AMIs coded as principal versus secondary diagnoses. Due to major changes in hospital procedure coding in 2005, we examined these data starting in 2006. Finally, we calculated expenditures for all hospitalizations with AMI, and the proportion of these expenditures when the AMI was coded as secondary.
All analyses used Stata version 13 (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP).
This study was supported by P01AG031098 from the National Institute of Aging (NIA) and 5UL1TR000161 from the National Center for Research Resources (NCRR) and by National Institutes of Health (NIH) grants U01HL05268-04 and UL1TR000161. The authors are solely responsible for the design and conduct of this study, all study analyses and drafting and editing of the paper and its final content.
RESULTS
Baseline Characteristics
Over the 10 year study timeframe, 3,663,137 hospitalizations had an AMI discharge diagnosis (1.27 per 100 beneficiary-years); of these, 2,425,179 (66%) were hospitalizations with AMI coded as principal, with the remaining having an AMI coded in a secondary position. Table 1 shows the characteristics of beneficiaries hospitalized for AMI in 2002 and 2011 (the first and last years studied), stratified by whether the AMI was principal or secondary. Principal AMI patients were younger than secondary (mean age of 78.3 years vs. 79.5 in 2002; 78.5 years vs. 80.1 in 2011), less likely to be female (50.7% vs. 53.7% in 2002; 48.2% vs. 53.0% in 2011) and more likely to be white (88.6% vs. 86.6% in 2002; 86.7% vs. 84.6% in 2011). These differences were not year-to-year fluctuations, but reflected consistent trends over the 10 year study period (see Appendix A).
TABLE 1.
AMI Patient Characteristics in 2002 and 2011 by AMI Discharge Diagnosis Position: Patients with secondary AMI hospitalizations are increasingly older, more likely to be female and less likely to be white
| 2002 | 2011 | |||
|---|---|---|---|---|
| Principal | Secondary | Principal | Secondary | |
| Beneficiary-years (#) | 28.8 million | 28.9 million | ||
| AMI Hospitalizations (#) | 302,829 | 119,943 | 194,002 | 127,478 |
| % of All by Dx Position | 72% | 28% | 60% | 40% |
| Mean Age in years (SD)* | 78.3 (7.9) | 79.5 (7.9) | 78.5 (8.5) | 80.1 (8.5) |
| Age 65-74, % | 35.2 | 28.8 | 37.0 | 29.1 |
| Age 75-84, % | 41.1 | 43.3 | 35.9 | 37.4 |
| Age ≥ 85, % | 23.7 | 27.9 | 27.0 | 33.5 |
| Female, % | 50.7 | 53.7 | 48.2 | 53.0 |
| White, % | 88.6 | 86.7 | 86.6 | 84.6 |
| Black, % | 7.4 | 8.8 | 8.4 | 10.0 |
AMI Hospitalizations
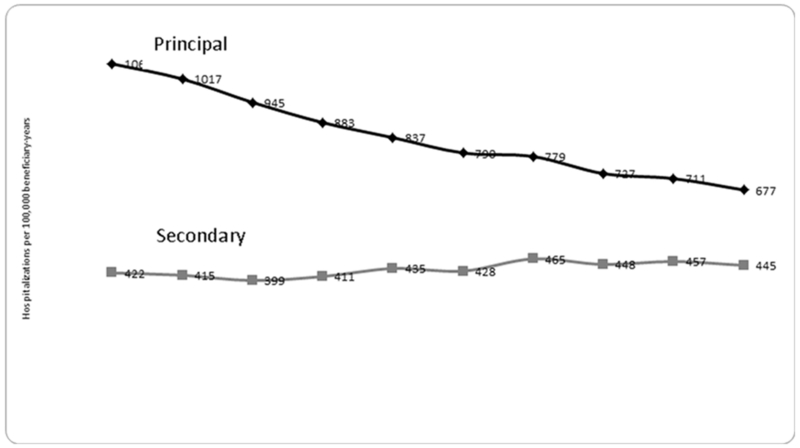
Overall, hospitalization rates declined 24.5% (from 1,485 per 100,000 beneficiary-years in 2002 to 1,122 in 2011). However, the decline in rates of principal AMI hospitalizations was much larger (36.4%, from 1,063 to 677), while the rate of secondary AMI hospitalizations actually increased (5.5%, from 422 to 445). (Figure 1) Consequently, the proportion of all AMI hospitalizations with a principal AMI diagnosis decreased from 72% in 2002 to 60% in 2011,and from 2002 to 2011 secondary AMI hospitalizations grew from 28% to 40% of all AMI hospitalization. The underlying data are in Appendix B.
Figure 1.
Hospitalization Rates with Principal vs. Secondary Diagnoses: Declines in principal AMI hospitalizations are partially offset by increases in those with secondary AMIs
Distribution of Principal, Second and Other Secondary Position AMI Hospitalizations
As shown in Table 2, much of the shift in the proportion of AMIs coded as principal vs. secondary reflected an increase in AMIs coded in the second position. In 2002, when AMI was present in any position, it was coded first 72% of the time and second 13% of the time; by 2011, it was coded first only 60% of the time and second 22% of the time. Thus, even though the distribution of first- versus second-position AMIs shifted, the percent of all AMIs coded either first or second remained fairly constant between 2002 and 2011, falling only slightly from 84% to 82% over the decade. Over the same period, very few AMIs in any year were coded in any single position other than first or second, and the proportion appearing in all other positions held steady at approximately 17%.
TABLE 2.
AMI Hospitalizations by Discharge Diagnosis Position: Second position AMI discharge diagnoses increased from 2002 – 2011
| 2002 | 2006 | 2008 | 2011 | |
|---|---|---|---|---|
| AMI Hospitalization Discharge Diagnosis Position | ||||
| ANY Position | 1,485 | 1,273 | 1,244 | 1,122 |
| PRINCIPAL Position | 1,063 | 837 | 779 | 677 |
| SECOND Position | 190 | 199 | 237 | 245 |
| THIRD or SUBSEQUENT Position | 232 | 237 | 228 | 200 |
| Percent of AMI Hospitalizations | ||||
| PRINCIPAL Position | 72% | 66% | 63% | 60% |
| SECOND Position | 13% | 16% | 19% | 22% |
| PRINCIPAL or SECOND Position | 84% | 81% | 82% | 82% |
Comparing Hospitalizations with AMI as Principal versus Second Position Diagnosis
Table 3 shows common comorbid conditions for principal and second-listed AMI hospitalizations in each year 2002, 2006, 2008, and 2011, organized as cardiac- and non-cardiac related conditions. The ICD-9 codes used to identify these comorbidities are also listed. Rates of cardiac-related comorbidities were relatively stable for principal AMI patients across these years but differed in the later versus earlier years for second-listed patients. Notable shifts often occurred for hospitalizations with second-listed AMI between 2006 and 2008; congestive heart failure (CHF), for example, affected more than half of these patients in 2002 (51%) and 2006 (54%), but less than 1/3 in 2008 (28%) and 2011 (31%). Rates of coronary atherosclerosis and atrial fibrillation were also lower for these hospitalizations in the second half of the study period (2011 vs. 2002: coronary atherosclerosis 26% vs. 36%; atrial fibrillation: 16% vs. 29%).
TABLE 3.
Cardiac and non-Cardiac-related Comorbidities* for Principal and Second Position AMI: Few big changes for Dx1 AMI hospitalizations between 2006 and 2008; many for Dx2**
| Comorbid Condition | Dx1 AMIs: Percent with Diagnoses for Comorbidity |
Second Position AMIs: Percent with Diagnoses for Comorbidity |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Diagnosis (ICD-9) Codes | Description | 2002 | 2006 | 2008 | 2011 | 2002 | 2006 | 2008 | 2011 |
| CARDIAC-RELATED | |||||||||
| 414.0×; 414.2×, 414.3×,414.8×,414.9× |
Coronary atherosclerosis | 63% | 64% | 73% | 71% | 36% | 38% | 29% | 26% |
| 401.×, 402.×, 404.× | Hypertension | 45% | 43% | 41% | 39% | 33% | 30% | 31% | 34% |
| 428.× | Congestive Heart Failure, unspecified | 39% | 41% | 38% | 41% | 51% | 54% | 28% | 31% |
| 427.31 | Atrial fibrillation | 22% | 23% | 18% | 19% | 29% | 31% | 19% | 16% |
| NON-CARDIAC RELATED | |||||||||
| 249.×, 250.× | Diabetes (Type 2) | 19% | 19% | 20% | 20% | 15% | 15% | 15% | 13% |
| 584.×, 585.× | Kidney disease (Kidney failure/CKD) | 4% | 15% | 23% | 26% | 9% | 29% | 23% | 35% |
| 038.*, 995.91, 995.92 | Sepsis/septicemia | - | - | - | - | 2% | 4% | 10% | 20% |
| 486 | Pneumonia | 6% | 7% | 9% | 8% | 13% | 15% | 13% | 15% |
| 518.81 | Acute respiratory failure | 6% | 6% | 8% | 10% | 15% | 18% | 16% | 18% |
| 496 | Chronic airway obstruction, not elsewhere classified |
13% | 14% | 9% | 9% | 15% | 16% | 7% | 6% |
Based on top 10 ICD-9 diagnoses in the non-principal or the non-second position for hospitalizations in that year with AMI coded as principal or second position discharge diagnosis, respectively.
2007 was the transition year for the new DRG payment system.
“-” indicates that no ICD-9 diagnosis codes for that comorbidity were not in the top 10 diagnosis codes in that year.
Among patients with a second position AMI diagnosis, sepsis and septicemia were increasingly common non-cardiac-related comorbidities, affecting 2% in 2002 and 20% in 2011; we did not observe sepsis or septicemia diagnoses for principal AMI patients, however. Rates of kidney disease (kidney failure and CKD) also increased dramatically over the 10-year study period in second-position AMI patients (from 9% in 2002 to 35% in 2011), although they increased in principal AMI patients as well (from 4% in 2002 to 26% in 2011). Rates of diabetes, acute respiratory failure and pneumonia were higher in patients with a second (versus principal) position AMI diagnosis throughout the study period, but otherwise showed no major changes in either group.
Principal Discharge Diagnoses for Second Position AMI Hospitalizations
Principal diagnoses for hospitalizations where the AMI was the second discharge diagnosis also differed in the earlier and later study years, with changes occurring especially in the 2006-2008 timeframe (Table 4). From 2002-2006, congestive heart failure (CHF, ICD-9 428.0) was the principal discharge diagnosis for more than 20% of these hospitalizations, followed by coronary atherosclerosis (5-6%) and pneumonia (3-5%). CHF, however, was rare after 2007, declining to 3.3% of all principal discharge diagnoses in 2008 and disappearing from the top 5 for the remainder of the study period. Septicemia (038.9), which was not in the top five in 2002-2005, increased from 3.5% of all principal discharge diagnoses in 2006 to 9.7% in 2011. Acute Respiratory Failure entered the top 5 comorbidities starting in 2005, albeit at a relatively stable rate through 2011. Notably, CHF was not replaced by another dominant principal discharge diagnosis. Consequently, the top 5 diagnosis codes accounted for 42-43% of all principal discharge diagnoses through 2006, but only 27% from 2008-2011.
TABLE 4.
Top 5 Principal Discharge Diagnoses When AMI Is Listed Second, By Year: No principal diagnosis dominates after 2007
| Dx Code | Description | 2002 | 2003 | 2004 | 2005 | 2006 | 2007* | 2008 | 2009 | 2010 | 2011 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 4280 | Congestive heart failure, unspecified | 24.8 | 25.9 | 26.4 | 23.6 | 20.5 | 14.5 | 3.3 | - | - | - |
| 41401 | Coronary atherosclerosis of native coronary artery |
6.4 | 6.0 | 5.2 | 5.1 | 6.4 | 6.3 | 5.8 | 4.6 | 3.3 | - |
| 486 | Pneumonia | 4.7 | 4.7 | 4.0 | 4.0 | - | 3.6 | 5.3 | 5.4 | 5.0 | 5.0 |
| 42731 | Atrial fibrillation | 3.8 | 3.9 | 4.1 | 4.0 | 4.1 | - | - | - | - | - |
| 5070 | Pneumonitis due to solids and liquids | 2.9 | 2.4 | - | - | - | - | - | 3.5 | 3.3 | 3.7 |
| 51881 | Acute respiratory failure | - | - | - | 5.6 | 7.8 | 7.8 | 7.5 | 7.4 | 6.1 | 5.6 |
| 389 | Septicemia | - | - | - | - | 3.5 | 4.3 | 5.4 | 6.0 | 9.6 | 9.7 |
| 43491 | Cerebral artery occlusion, w/infarc | - | - | 2.3 | - | - | - | - | - | - | - |
| 5849 | Acute kidney failure | - | - | - | - | - | - | - | - | - | 2.9 |
| Percent accounted for by: | |||||||||||
| Top Dx Code: | 24.8 | 25.9 | 26.4 | 23.6 | 20.5 | 14.5 | 7.5 | 7.4 | 9.6 | 9.7 | |
| Top 5 Dx Codes: | 42.6 | 42.8 | 42.0 | 42.2 | 42.3 | 36.4 | 27.3 | 26.8 | 27.3 | 27.0 | |
“-” indicates that diagnosis was not in the top 5 principal discharge diagnoses for second-position AMI hospitalizations in that year.
2007 was the transition year for the new DRG payment system
Cardiac- and non-Cardiac Related Procedures
Over the 6 year period 2006-2011, admissions with only non-cardiac procedures were more common when the AMI was secondary (about 1/3 of such admissions) than when it was listed first (about 1 in 9). However, there were only modest changes from 2006 to 2011 in the prevalence of cardiac and non-cardiac procedures for each kind of AMI hospitalization (Table 5). The largest change was among hospitalizations with a principal discharge diagnosis of AMI, where the proportion with any cardiac procedure grew by 5 percentage points (from 61% to 66%), counterbalanced by a decline from 27% to 22% in the proportion of hospitalizations with no listed procedure. Among hospitalizations with a secondary diagnosis of AMI during the same 6 years, the percent with any cardiac procedure fluctuated within a narrow range (starting at 45% and ending at 43%), matched by modest fluctuations in the percentage with only non-cardiac procedures, starting at 32% and ending at 34%. See Appendix C for more detail.
TABLE 5.
AMI Hospitalizations with Cardiac and Non-Cardiac Procedures Listed, by AMI Position and Year: Changes in proportions are small
| AMI Position | Any Cardiac Procedure |
Cardiac Procedures Only |
Cardiac and Non-Cardiac Procedures |
Non-Cardiac Procedures Only |
None |
|---|---|---|---|---|---|
| Principal | |||||
| 2006 | 61% | 16% | 45% | 12% | 27% |
| 2007 | 62% | 17% | 46% | 12% | 25% |
| 2008 | 62% | 16% | 46% | 12% | 26% |
| 2009 | 64% | 16% | 48% | 12% | 24% |
| 2010 | 66% | 17% | 49% | 11% | 23% |
| 2011 | 66% | 15% | 51% | 11% | 22% |
| Secondary | |||||
| 2006 | 45% | 7% | 38% | 32% | 23% |
| 2007 | 47% | 7% | 39% | 32% | 21% |
| 2008 | 47% | 8% | 40% | 32% | 21% |
| 2009 | 47% | 7% | 40% | 31% | 22% |
| 2010 | 46% | 7% | 39% | 32% | 22% |
| 2011 | 43% | 7% | 37% | 34% | 23% |
Expenditures for AMI Hospitalizations
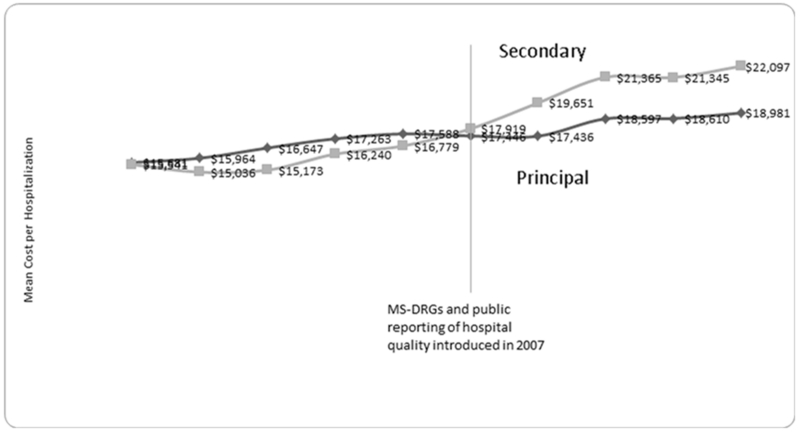
Expenditures for AMI hospitalizations with secondary discharge diagnoses of AMI accounted for an increasing proportion of the expenditures for all AMI hospitalizations over time (Figure 2). This increase reflected both the rising proportion of secondary AMIs and more rapid growth in mean costs for these hospitalizations. Notably, in 2002, the mean costs for principal versus secondary AMI hospitalizations were nearly identical (Principal: $15,581 vs. Secondary: $15,541), and remained similar for several years. However, starting in 2007, mean costs for secondary AMI hospitalizations surpassed principal AMI hospitalizations; by 2011, they were 16.4% higher (Principal: $18,981 vs. Secondary: $22,097). Thus, secondary AMI hospitalizations accounted for an increasing proportion of all AMI hospitalization expenditures, growing from 28% in 2002 to 43% in 2011 (Figure 2). Of the $6.5 billion spent on all AMI hospitalizations in 2011, $2.8 billion was spent on hospitalizations with secondary diagnoses of AMI.
Figure 2.
Mean Cost per AMI Hospitalization:* Principal vs. Secondary Discharge Diagnoses: Beginning in 2007, hospitalizations with secondary AMIs became more expensive than those with AMIs coded as principal
DISCUSSION
Hospitalizations with AMI coded as a secondary discharge diagnosis are usually absent from national reporting, leading to underestimates of the full burden of AMI. We found that this group of AMIs is substantial, and represents an increasing proportion of all AMI hospitalizations over time. Concomitantly, expenditures for these hospitalizations have increased, accounting for over $2.8 billion (43%) of the $6.5 billion spent on AMI hospitalizations in 2011 (compared to 28% of the total a decade earlier). Thus, when provided with data based only on hospitalizations with principal diagnoses of AMI, policy makers will fail to see a large and growing portion of the full AMI burden.
Researchers have reported marked declines in AMI hospitalizations,9,11,12,14,15 minimal increases in their average costs,9 and pronounced improvements in AMI treatment quality.22,23 However, these studies only count hospitalizations with a principal discharge diagnosis of AMI. We examine all hospitalizations in which an AMI occurred, finding that hospitalizations with AMI coded in secondary positions are a substantial and increasing proportion of all AMI hospitalizations. Consequently, estimates that ignore this growing subset of AMIs may overstate improvements in population health, underestimate current and future expenditures for AMI, and, in turn, overestimate the value of recent efforts in AMI prevention and treatment. As such, understanding and accounting for these AMIs will be increasingly important for health policy and research planning.
Increasingly sensitive troponin tests may be responsible for some of the increases in secondary AMIs. 24,25 Diagnostic code enhancements to distinguish AMI subtypes,26,27 as Shroff et al. propose,24,25 could help clarify the impact of these tests on trends in secondary AMIs. However, the sudden changes in comorbidities, principal discharge diagnoses and costs in the 2006-2008 timeframe are not consistent with marginal changes in test sensitivity, suggesting that changes in coding practice are also at play. It is also possible that the increase in the proportions of secondary AMI hospitalizations reflected an increase in AMIs occurring as a consequence of non-cardiac procedures. Yet, despite the dramatic shifts in various characteristics of principal and secondary AMI hospitalizations between 2006 and 2008, there was essentially no change in the fraction of hospitalizations with non-cardiac procedures (or cardiac procedures) listed from 2006-2011 for either type of AMI hospitalization.
Indeed, two major payment policy and quality reporting changes implemented during our study period could have affected how hospitals determine coding order on discharge abstracts. First, the October, 2007 introduction of the Medicare-Severity Diagnosis Related Groups (MS-DRGs) included major changes to the payment weights for AMI (and other hospitalizations).19,28 Second, public reporting of hospital-level post-AMI mortality began in the same year.13,29 Both the MS-DRGs and CMS’ Hospital Compare quality measure reporting for AMI consider only hospitalizations where the AMI is coded as principal. Thus, for patients admitted with AMI and at least one other serious condition, listing that other condition first removes the hospitalization from AMI quality reporting and could – depending upon what diagnosis replaces it – result in a higher MS-DRG payment. For example, although increases in hospitalizations with principal discharge diagnoses of sepsis (so AMI becomes secondary) could reflect increased troponin test sensitivity, coding sepsis or septicemia first will also lead to higher MS-DRG-based reimbursements and remove the sickest AMI patients from performance and other measures. 17 Thus, incentives for the order in which to code diagnoses of AMI and other serious conditions (such as CHF) on discharge abstracts changed in 2007; by 2008, abrupt changes appear in the frequencies of hospitalizations of AMIs coded first or second in combination with conditions such as CHF. Recent studies of Heart Failure (HF) and pneumonia, which, like AMI, are the target of CMS quality improvement and cost containment initiatives, suggest that code shifting has contributed to secular trends in diagnostic coding, and that including secondary discharge diagnoses can generate very different estimates of trends in these high profile conditions.30,31 The MS-DRG payment weights have also provided new incentives for hospitals to record more diagnoses on the discharge abstract, however, fueling secular growth in the coding of all secondary diagnoses.32,33,34 Identifying the extent to which increases in troponin test sensitivity, code shifting and coding intensity are driving the marked growth in the numbers and proportion of hospitalizations with secondary AMIs is important for epidemiologic research and has significant implications for population health and national accounting of AMI burden.
Limitations
Our study of hospitalizations with AMI in the Medicare over-65 population has only accounted for reimbursements to the hospital from Medicare and patients; we did not include payments for physicians and other services occurring during the hospitalization but billed separately. However, these services typically account for a small proportion of total hospitalization costs.3 We also studied only the Fee-for-Service population, as Medicare managed care plans were not required to submit claims to Medicare.
Further, we used administrative data, which provide minimal to no information on the severity of the AMI, other clinical risk factors, or troponin test findings, each of which would help interpret the clinical meaning of a secondary AMI. Although we observed changes in coding patterns coincident with the introduction of a new MS-DRG payment system version and public reporting of hospital quality in 2007, we do not know that the increasing proportions of secondary AMI hospitalizations are due to these payment and policy changes, and while plausible, we cannot definitively attribute the observed AMI trends to financial incentives or other non-clinical factors. Finally, although unlikely to be the sole driver of these trends, it is possible that the increase in secondary AMIs may simply reflect clinical reality.
CONCLUSION
Secondary AMI hospitalizations are a large and growing proportion of all AMI hospitalizations, and an even larger proportion of their expenditures. These hospitalizations increased over a decade surrounding 2007, during which time hospitalizations with AMI coded as the principal discharge diagnosis fell. Thus, estimates of trends in AMI hospitalization rates and expenditures that rely on principal discharge diagnosis alone fail to account for secular trends in coding, and thereby overstate national success in reducing the burden of heart attacks. Efforts to understand and improve cardiovascular health should start with a full accounting of the complete burden of AMI.
Appendix A
Medicare Beneficiary and AMI Patient Characteristics: 2002-2011
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
|
Denominator (Beneficiary- Years) |
28.8 mn | 29.3 mn | 29.6 mn | 29.7 mn | 29.1 mn | 28.6 mn | 28.3 mn | 28.2 mn | 28.5 mn | 28.9 mn | 288.9 mn |
| Mean Age* | 75.4 | 75.4 | 75.4 | 75.4 | 75.4 | 75.4 | 75.3 | 75.3 | 75.3 | 75.2 | 75.4 |
| Age 65-74, % | 46.7 | 46.7 | 46.9 | 46.9 | 46.9 | 47.2 | 48.0 | 48.6 | 49.1 | 49.8 | 47.7 |
| Age 75-84, % | 37.2 | 37.0 | 36.8 | 36.5 | 36.0 | 35.3 | 34.3 | 33.4 | 32.7 | 32.1 | 35.1 |
| Age ≥ 85, % | 16.2 | 16.3 | 16.3 | 16.6 | 17.1 | 17.5 | 17.7 | 18.0 | 18.2 | 18.2 | 17.2 |
| Male, % | 41.8 | 42.0 | 42.2 | 42.4 | 42.7 | 42.9 | 43.3 | 43.5 | 43.7 | 44.0 | 42.8 |
| Female, % | 58.2 | 58.0 | 57.8 | 57.6 | 57.3 | 57.1 | 56.7 | 56.5 | 56.3 | 56.0 | 57.2 |
| White, % | 87.5 | 87.3 | 87.1 | 86.9 | 87.0 | 86.9 | 86.8 | 86.5 | 86.2 | 85.9 | 86.8 |
| Black, % | 8.0 | 8.0 | 8.1 | 8.0 | 7.9 | 7.8 | 7.8 | 7.8 | 7.9 | 8.0 | 7.9 |
| Other, % | 4.6 | 4.7 | 4.8 | 5.1 | 5.1 | 5.3 | 5.5 | 5.7 | 5.9 | 6.2 | 5.3 |
|
AMI Hospitalizations (Principal Discharge Diagnosis) |
|||||||||||
| # Hospitalizations | 302,829 | 295,030 | 277,389 | 260,792 | 243,040 | 225,744 | 220,026 | 204,213 | 202,114 | 194,002 | 2,425,179 |
| % of All Hospitalizations w/AMI | 72% | 72% | 70% | 68% | 66% | 65% | 63% | 62% | 61% | 60% | 66% |
| Mean Age* | 78.3 | 78.5 | 78.5 | 78.6 | 78.7 | 79.7 | 78.8 | 78.6 | 78.6 | 78.5 | 78.6 |
| Age 65-74, % | 35.2 | 34.6 | 34.6 | 34.3 | 34.4 | 34.4 | 34.5 | 35.8 | 36.3 | 37.1 | 35.0 |
| Age 75-84, % | 41.2 | 41.0 | 41.0 | 40.4 | 39.5 | 38.9 | 38.1 | 36.9 | 36.5 | 36.0 | 39.2 |
| Age ≥ 85, % | 23.7 | 24.5 | 24.5 | 25.3 | 26.1 | 26.8 | 27.4 | 27.4 | 27.3 | 27.0 | 25.8 |
| Female, % | 50.7 | 50.6 | 50.5 | 50.1 | 50.1 | 49.7 | 49.9 | 49.1 | 48.9 | 48.2 | 49.9 |
| White, % | 88.7 | 88.3 | 88.0 | 88.0 | 87.9 | 87.9 | 87.6 | 87.3 | 87.0 | 86.7 | 87.7 |
| Black, % | 7.4 | 7.6 | 7.6 | 7.7 | 7.9 | 7.8 | 7.8 | 8.1 | 8.2 | 8.4 | 7.8 |
| AMI Hospitalizations (Secondary Discharge Diagnosis) |
2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| # Hospitalizations | 119,943 | 116,493 | 116,991 | 121,396 | 126,526 | 122,310 | 131,313 | 125,721 | 129,787 | 127,478 | 1,237,958 |
| % of All Hospitalizations w/AMI | 28% | 28% | 30% | 32% | 34% | 35% | 37% | 38% | 39% | 40% | 34% |
| Mean Age (SD, y)* | 79.6 | 79.7 | 79.8 | 79.9 | 79.9 | 79.8 | 80.0 | 80.0 | 80.1 | 80.2 | 79.9 |
| Age 65-74, % | 28.8 | 29.5 | 28.4 | 28.2 | 27.9 | 28.5 | 28.4 | 28.9 | 28.8 | 29.1 | 28.7 |
| Age 75-84, % | 43.3 | 44.3 | 42.9 | 42.5 | 41.8 | 40.8 | 39.8 | 39.1 | 38.2 | 37.4 | 40.9 |
| Age ≥ 85, % | 27.9 | 26.2 | 28.7 | 29.3 | 30.3 | 30.7 | 31.8 | 32.1 | 33.0 | 33.5 | 30.4 |
| Female, % | 53.7 | 52.2 | 54.1 | 54.0 | 54.2 | 53.4 | 53.5 | 53.3 | 53.2 | 53.0 | 53.5 |
| White, % | 86.7 | 86.2 | 86.2 | 85.9 | 86.0 | 85.7 | 85.6 | 85.4 | 84.9 | 84.6 | 85.7 |
| Black, % | 8.8 | 9.1 | 9.0 | 9.2 | 9.2 | 9.4 | 9.4 | 9.5 | 9.7 | 10.0 | 9.3 |
|
AMI Hospitalizations (Any Discharge Diagnosis) |
|||||||||||
| # Hospitalizations | 422,772 | 411,523 | 394,380 | 382,188 | 369,566 | 348,054 | 351,339 | 329,934 | 331,901 | 321,480 | 3,663,137 |
| Mean Age (SD, y)* | 78.7 | 78.8 | 78.9 | 79.0 | 79.1 | 79.8 | 79.2 | 79.2 | 79.2 | 79.1 | 79.1 |
| Age 65-74, % | 33.4 | 33.1 | 32.8 | 32.4 | 32.2 | 32.3 | 32.2 | 33.1 | 33.4 | 33.9 | 32.9 |
| Age 75-84, % | 41.8 | 41.9 | 41.5 | 41.1 | 40.3 | 39.6 | 38.8 | 37.7 | 37.2 | 36.5 | 39.8 |
| Age ≥ 85, % | 24.9 | 25.0 | 25.8 | 26.6 | 27.5 | 28.1 | 29.1 | 29.2 | 29.5 | 29.6 | 27.4 |
| Female, % | 51.6 | 51.0 | 51.6 | 51.3 | 51.5 | 51.0 | 51.2 | 50.7 | 50.6 | 50.1 | 51.1 |
| White, % | 88.1 | 87.7 | 87.5 | 87.3 | 87.3 | 87.1 | 86.9 | 86.6 | 86.2 | 85.8 | 87.1 |
| Black, % | 7.8 | 8.0 | 8.0 | 8.2 | 8.3 | 8.4 | 8.4 | 8.6 | 8.8 | 9.0 | 8.3 |
Mean age per hospitalization
Appendix B
AMI Hospitalization Rates by Diagnosis Position, 2002-2011.
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | Change 2002-2011 |
|
|---|---|---|---|---|---|---|---|---|---|---|---|
| Any AMI Hospitalization | |||||||||||
| Total | 1,485 | 1,432 | 1,344 | 1,294 | 1,273 | 1,218 | 1,244 | 1,175 | 1,169 | 1,122 | −24.5% |
| Age 65-74 | 960 | 910 | 850 | 812 | 795 | 762 | 761 | 730 | 725 | 696 | −27.5% |
| Age 75-84 | 1,730 | 1,663 | 1,567 | 1,507 | 1,476 | 1,415 | 1,452 | 1,366 | 1,360 | 1,302 | −24.7% |
| Age ≥ 85 | 2,812 | 2,772 | 2,600 | 2,538 | 2,518 | 2,400 | 2,500 | 2,328 | 2,313 | 2,224 | −20.9% |
| Female | 1,309 | 1,267 | 1,197 | 1,151 | 1,142 | 1,089 | 1,124 | 1,056 | 1,052 | 1,007 | −23.1% |
| Male | 1,720 | 1,651 | 1,539 | 1,484 | 1,446 | 1,390 | 1,404 | 1,333 | 1,324 | 1,274 | −25.9% |
| White | 1,500 | 1,443 | 1,352 | 1,302 | 1,278 | 1,221 | 1,245 | 1,174 | 1,167 | 1,119 | −25.4% |
| Black | 1,423 | 1,396 | 1,329 | 1,307 | 1,330 | 1,301 | 1,349 | 1,299 | 1,297 | 1,268 | −10.9% |
| Principal Diagnosis AMI Hospitalizations | |||||||||||
| Total | 1,063 | 1,017 | 945 | 883 | 837 | 790 | 779 | 727 | 711 | 677 | −36.4% |
| Age 65-74 | 725 | 681 | 632 | 588 | 559 | 526 | 510 | 487 | 480 | 459 | −36.7% |
| Age 75-84 | 1,221 | 1,166 | 1,087 | 1,012 | 952 | 903 | 894 | 827 | 814 | 774 | −36.6% |
| Age ≥ 85 | 1,918 | 1,880 | 1,742 | 1,649 | 1,571 | 1,481 | 1,478 | 1,353 | 1,303 | 1,226 | −36.1% |
| Female | 922 | 884 | 824 | 766 | 730 | 688 | 685 | 633 | 619 | 585 | −36.5% |
| Male | 1,252 | 1,194 | 1,106 | 1,039 | 979 | 926 | 904 | 852 | 834 | 798 | −36.2% |
| White | 1,081 | 1,030 | 956 | 895 | 847 | 799 | 786 | 732 | 717 | 681 | −37.0% |
| Black | 966 | 948 | 886 | 838 | 827 | 787 | 788 | 754 | 738 | 711 | −26.4% |
| Secondary Diagnosis AMI Hospiatlizations | |||||||||||
| Total | 422 | 415 | 399 | 411 | 436 | 428 | 465 | 448 | 457 | 445 | 5.5% |
| Age 65-74 | 235 | 229 | 219 | 224 | 236 | 236 | 251 | 243 | 245 | 237 | 0.8% |
| Age 75-84 | 509 | 497 | 480 | 495 | 524 | 513 | 558 | 539 | 547 | 528 | 3.8% |
| Age ≥ 85 | 894 | 892 | 858 | 889 | 947 | 920 | 1,022 | 975 | 1,010 | 998 | 11.7% |
| Female | 457 | 449 | 443 | 469 | 502 | 514 | 561 | 545 | 559 | 556 | 21.8% |
| Male | 387 | 383 | 373 | 385 | 412 | 401 | 439 | 423 | 433 | 422 | 9.1% |
| White | 468 | 457 | 433 | 445 | 467 | 464 | 500 | 481 | 490 | 476 | 1.6% |
| Black | 420 | 413 | 396 | 407 | 431 | 422 | 459 | 442 | 450 | 438 | 4.4% |
Appendix C
Cardiac- and Non-Cardiac Related Procedures by Year and AMI Diagnosis Position
| ANY CARDIAC PROCEDURES | CARDIAC PROCEDURES ONLY | NON-CARDIAC PROCEDURES ONLY | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TYPE | YEAR | NO | YES | TOTAL |
% ANY CARDIAC |
TYPE | YEAR | NO | YES | TOTAL |
% CARDIAC ONLY |
TYPE | YEAR | NO | YES | TOTAL |
% NON- CARDIAC ONLY |
| DX1 | 2006 | 94,741 | 148,299 | 243,040 | 61% | DX1 | 2006 | 204,448 | 38,592 | 243,040 | 16% | DX1 | 2006 | 214,010 | 29,030 | 243,040 | 12% |
| 2007 | 85,211 | 140,533 | 225,744 | 62% | 2007 | 188,186 | 37,558 | 225,744 | 17% | 2007 | 197,866 | 27,878 | 225,744 | 12% | |||
| 2008 | 83,492 | 136,534 | 220,026 | 62% | 2008 | 183,856 | 36,170 | 220,026 | 16% | 2008 | 193,000 | 27,026 | 220,026 | 12% | |||
| 2009 | 73,341 | 130,872 | 204,213 | 64% | 2009 | 170,592 | 33,621 | 204,213 | 16% | 2009 | 180,153 | 24,060 | 204,213 | 12% | |||
| 2010 | 69,339 | 132,775 | 202,114 | 66% | 2010 | 168,335 | 33,779 | 202,114 | 17% | 2010 | 179,180 | 22,934 | 202,114 | 11% | |||
| 2011 | 65,292 | 128,710 | 194,002 | 66% | 2011 | 163,987 | 30,015 | 194,002 | 15% | 2011 | 172,309 | 21,693 | 194,002 | 11% | |||
| TYPE | YEAR | NO | YES | TOTAL |
% ANY CARDIAC |
TYPE | YEAR | NO | YES | TOTAL |
% CARDIAC ONLY |
TYPE | YEAR | NO | YES | TOTAL |
% NON- CARDIAC ONLY |
| DX2+ | 2006 | 69,755 | 56,682 | 126,437 | 45% | DX2+ | 2006 | 117,259 | 9,178 | 126,437 | 7% | DX2+ | 2006 | 85,735 | 40,702 | 126,437 | 32% |
| 2007 | 65,184 | 57,026 | 122,210 | 47% | 2007 | 113,416 | 8,794 | 122,210 | 7% | 2007 | 83,007 | 39,203 | 122,210 | 32% | |||
| 2008 | 69,120 | 62,112 | 131,232 | 47% | 2008 | 121,352 | 9,880 | 131,232 | 8% | 2008 | 89,601 | 41,631 | 131,232 | 32% | |||
| 2009 | 66,567 | 59,069 | 125,636 | 47% | 2009 | 116,375 | 9,261 | 125,636 | 7% | 2009 | 86,232 | 39,404 | 125,636 | 31% | |||
| 2010 | 69,789 | 59,896 | 129,685 | 46% | 2010 | 120,186 | 9,499 | 129,685 | 7% | 2010 | 88,116 | 41,569 | 129,685 | 32% | |||
| 2011 | 72,170 | 55,172 | 127,342 | 43% | 2011 | 119,053 | 8,289 | 127,342 | 7% | 2011 | 83,920 | 43,422 | 127,342 | 34% | |||
| BOTH | NONE | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| TYPE | YEAR | NO | YES | TOTAL | % BOTH | YEAR | NO | YES | TOTAL | % NONE |
| DX1 | 2006 | 133,333 | 109,707 | 243,040 | 45% | 2006 | 177,329 | 65,711 | 243,040 | 27% |
| 2007 | 122,769 | 102,975 | 225,744 | 46% | 2007 | 168,411 | 57,333 | 225,744 | 25% | |
| 2008 | 119,662 | 100,364 | 220,026 | 46% | 2008 | 163,560 | 56,466 | 220,026 | 26% | |
| 2009 | 106,962 | 97,251 | 204,213 | 48% | 2009 | 154,932 | 49,281 | 204,213 | 24% | |
| 2010 | 103,118 | 98,996 | 202,114 | 49% | 2010 | 155,709 | 46,405 | 202,114 | 23% | |
| 2011 | 95,307 | 98,695 | 194,002 | 51% | 2011 | 150,403 | 43,599 | 194,002 | 22% | |
| TYPE | YEAR | NO | YES | TOTAL | % BOTH | YEAR | NO | YES | TOTAL | % NONE |
| DX2+ | 2006 | 78,933 | 47,504 | 126,437 | 38% | 2006 | 97,384 | 29,053 | 126,437 | 23% |
| 2007 | 73,978 | 48,232 | 122,210 | 39% | 2007 | 96,229 | 25,981 | 122,210 | 21% | |
| 2008 | 79,000 | 52,232 | 131,232 | 40% | 2008 | 103,743 | 27,489 | 131,232 | 21% | |
| 2009 | 75,828 | 49,808 | 125,636 | 40% | 2009 | 98,473 | 27,163 | 125,636 | 22% | |
| 2010 | 79,288 | 50,397 | 129,685 | 39% | 2010 | 101,465 | 28,220 | 129,685 | 22% | |
| 2011 | 80,459 | 46,883 | 127,342 | 37% | 2011 | 98,594 | 28,748 | 127,342 | 23% | |
Appendix D
Cardiac-Related ICD9 Procedure Codes
| Cardiac Procedures (ICD9 Code/Description) | ||
| 0002 THER ULTRASOUND OF HEART | 3752 IMPLANT TOT REP HRT SYS | 3869 LEG VEIN EXCISION |
| 0024 IVUS CORONARY VESSELS | 3753 REPL/REP THORAC UNIT HRT | 387 INTERRUPTION VENA CAVA |
| 0066 PTCA OR CORONARY ATHER | 3754 REPL/REP OTH TOT HRT SYS | 3880 SURG VESSEL OCCLUS NEC |
| 3500 CLOSED VALVOTOMY NOS | 3761 PULSATION BALLOON IMPLAN | 3881 OCCLUS INTRACRAN VES NEC |
| 3501 CLOSED AORTIC VALVOTOMY | 3762 INS NON-IMPL HRT ASSIST | 3882 OCCLUS HEAD/NECK VES NEC |
| 3502 CLOSED MITRAL VALVOTOMY | 3763 REPAIR HEART ASSIST SYS | 3883 OCCLUDE ARM VESSEL NEC |
| 3503 CLOSED PULMON VALVOTOMY | 3764 REMOVE HEART ASSIST SYS | 3884 OCCLUDE AORTA NEC |
| 3504 CLOSED TRICUSP VALVOTOMY | 3765 IMP EXT HRT ASSIST SYST | 3885 OCCLUDE THORACIC VES NEC |
| 3510 OPEN VALVULOPLASTY NOS | 3766 IMPLANTABLE HRT ASSIST | 3886 OCCLUDE ABD ARTERY NEC |
| 3511 OPN AORTIC VALVULOPLASTY | 3767 IMP CARDIOMYOSTIMUL SYS | 3887 OCCLUDE ABD VEIN NEC |
| 3512 OPN MITRAL VALVULOPLASTY | 3768 PERCUTAN HRT ASSIST SYST | 3888 OCCLUDE LEG ARTERY NEC |
| 3513 OPN PULMON VALVULOPLASTY | 3770 INT INSERT PACEMAK LEAD | 3889 OCCLUDE LEG VEIN NEC |
| 3514 OPN TRICUS VALVULOPLASTY | 3771 INT INSERT LEAD IN VENT | 3891 ARTERIAL CATHETERIZATION |
| 3520 REPLACE HEART VALVE NOS | 3772 INT INSER LEAD ATRI-VENT | 3892 UMBILICAL VEIN CATH |
| 3521 REPLACE AORT VALV-TISSUE | 3773 INT INSER LEAD IN ATRIUM | 3893 VENOUS CATH NEC |
| 3522 REPLACE AORTIC VALVE NEC | 3774 INT OR REPL LEAD EPICAR | 3894 VENOUS CUTDOWN |
| 3523 REPLACE MITR VALV-TISSUE | 3775 REVISION OF LEAD | 3895 VEN CATH RENAL DIALYSIS |
| 3524 REPLACE MITRAL VALVE NEC | 3776 REPL TV ATRI-VENT LEAD | 3898 ARTERIAL PUNCTURE NEC |
| 3525 REPLACE PULM VALV-TISSUE | 3777 REMOVAL OF LEAD W/O REPL | 3899 VENOUS PUNCTURE NEC |
| 3526 REPLACE PULMON VALVE NEC | 3778 INSER TEMP PACEMAKER SYS | 390 SYSTEMIC-PULM ART SHUNT |
| 3527 REPLACE TRIC VALV-TISSUE | 3779 REV/RELOC CARD DEV POCKT | 391 INTRA-ABD VENOUS SHUNT |
| 3528 REPLACE TRICUSP VALV NEC | 3780 INT OR REPL PERM PACEMKR | 3921 CAVAL-PULMON ART ANASTOM |
| 3531 PAPILLARY MUSCLE OPS | 3781 INT INSERT 1-CHAM, NON | 3922 AORTA-SUBCLV-CAROT BYPAS |
| 3532 CHORDAE TENDINEAE OPS | 3782 INT INSERT 1-CHAM, RATE | 3923 INTRATHORACIC SHUNT NEC |
| 3533 ANNULOPLASTY | 3783 INT INSERT DUAL-CHAM DEV | 3924 AORTA-RENAL BYPASS |
| 3534 INFUNDIBULECTOMY | 3785 REPL PACEM W 1-CHAM, NON | 3925 AORTA-ILIAC-FEMOR BYPASS |
| 3535 TRABECUL CARNEAE CORD OP | 3786 REPL PACEM 1-CHAM, RATE | 3926 INTRA-ABDOMIN SHUNT NEC |
| 3539 TISS ADJ TO VALV OPS NEC | 3787 REPL PACEM W DUAL-CHAM | 3927 DIALYSIS ARTERIOVENOSTOM |
| 3541 ENLARGE EXISTING SEP DEF | 3789 REVISE OR REMOVE PACEMAK | 3928 EXTRACRAN-INTRACR BYPASS |
| 3542 CREATE SEPTAL DEFECT | 3790 INS LEFT ATR APPEND DEV | 3929 VASC SHUNT & BYPASS NEC |
| 3550 PROSTH REP HRT SEPTA NOS | 3791 OPN CHEST CARDIAC MASSAG | 3930 SUTURE OF VESSEL NOS |
| 3551 PROS REP ATRIAL DEF-OPN | 3792 INJECTION INTO HEART | 3931 SUTURE OF ARTERY |
| 3552 PROS REPAIR ATRIA DEF-CL | 3793 INJECTION INTO PERICARD | 3932 SUTURE OF VEIN |
| 3553 PROST REPAIR VENTRIC DEF | 3794 IMPLT/REPL CARDDEFIB TOT | 3941 POSTOP VASC OP HEM CONTR |
| 3554 PROS REP ENDOCAR CUSHION | 3795 IMPLT CARDIODEFIB LEADS | 3942 REVIS REN DIALYSIS SHUNT |
| 3560 GRFT REPAIR HRT SEPT NOS | 3796 IMPLT CARDIODEFIB GENATR | 3943 REMOV REN DIALYSIS SHUNT |
| 3561 GRAFT REPAIR ATRIAL DEF | 3797 REPL CARDIODEFIB LEADS | 3949 VASC PROC REVISION NEC |
| 3562 GRAFT REPAIR VENTRIC DEF | 3798 REPL CARDIODEFIB GENRATR | 3950 ANGIO OTH NON-CORONARY |
| 3563 GRFT REP ENDOCAR CUSHION | 3799 OTHER HEART/PERICARD OPS | 3951 CLIPPING OF ANEURYSM |
| 3570 HEART SEPTA REPAIR NOS | 3800 INCISION OF VESSEL NOS | 3952 ANEURYSM REPAIR NEC |
| 3571 ATRIA SEPTA DEF REP NEC | 3801 INTRACRAN VESSEL INCIS | 3953 ARTERIOVEN FISTULA REP |
| 3572 VENTR SEPTA DEF REP NEC | 3802 HEAD/NECK VES INCIS NEC | 3954 RE-ENTRY OPERATION |
| 3573 ENDOCAR CUSHION REP NEC | 3803 UPPER LIMB VESSEL INCIS | 3955 REIMPLAN ABERR RENAL VES |
| 3581 TOT REPAIR TETRAL FALLOT | 3804 INCISION OF AORTA | 3956 REPAIR VESS W TIS PATCH |
| 3582 TOTAL REPAIR OF TAPVC | 3805 THORACIC VESSEL INC NEC | 3957 REP VESS W SYNTH PATCH |
| 3583 TOT REP TRUNCUS ARTERIOS | 3806 ABDOMEN ARTERY INCISION | 3958 REPAIR VESS W PATCH NOS |
| 3584 TOT COR TRANSPOS GRT VES | 3807 ABDOMINAL VEIN INCISION | 3959 REPAIR OF VESSEL NEC |
| 3591 INTERAT VEN RETRN TRANSP | 3808 LOWER LIMB ARTERY INCIS | 3961 EXTRACORPOREAL CIRCULAT |
| 3592 CONDUIT RT VENT-PUL ART | 3809 LOWER LIMB VEIN INCISION | 3962 HYPOTHERMIA W OPEN HEART |
| 3593 CONDUIT LEFT VENTR-AORTA | 3810 ENDARTERECTOMY NOS | 3963 CARDIOPLEGIA |
| 3594 CONDUIT ARTIUM-PULM ART | 3811 INTRACRAN ENDARTERECTOMY | 3964 INTRAOP CARDIAC PACEMAK |
| 3595 HEART REPAIR REVISION | 3812 HEAD & NECK ENDARTER NEC | 3965 EXTRACORPOREAL MEMB OXY |
| 3596 PERC HEART VALVULOPLASTY | 3813 UPPER LIMB ENDARTERECTOM | 3966 PER CARDIOPULMON BYPASS |
| 3598 OTHER HEART SEPTA OPS | 3814 ENDARTERECTOMY OF AORTA | 3971 ENDO IMPL GRFT ABD AORTA |
| 3599 OTHER HEART VALVE OPS | 3815 THORACIC ENDARTERECTOMY | 3972 ENDOVASC REPAIR HEAD VES |
| 3603 OPEN CORONRY ANGIOPLASTY | 3816 ABDOMINAL ENDARTERECTOMY | 3973 ENDO IMP GRFT THOR AORTA |
| 3604 INTRCORONRY THROMB INFUS | 3818 LOWER LIMB ENDARTERECT | 3979 ENDO REPAIR OTHER VESSEL |
| 3606 INS NONDRUG ELUT COR ST | 3821 BLOOD VESSEL BIOPSY | 398 VASCULAR BODY OPERATIONS |
| 3607 INS DRUG-ELUT CORONRY ST | 3822 PERCUTANEOUS ANGIOSCOPY | 3990 INS NON-D-E PERPHRL STEN |
| 3609 REM OF COR ART OBSTR NEC | 3829 BLOOD VESSEL DX PROC NEC | 3991 FREEING OF VESSEL |
| 3610 AORTOCORONARY BYPASS NOS | 3830 VESSEL RESECT/ANAST NOS | 3992 VEIN INJECT-SCLEROS AGNT |
| 3611 AORTOCOR BYPAS-1 COR ART | 3831 INTRACRAN VES RESEC-ANAS | 3993 INSERT VES-TO-VES CANNUL |
| 3612 AORTOCOR BYPAS-2 COR ART | 3832 HEAD/NECK VES RESEC-ANAS | 3994 REPLAC VES-TO-VES CANNUL |
| 3613 AORTOCOR BYPAS-3 COR ART | 3833 ARM VESSEL RESECT/ANAST | 8850 ANGIOCARDIOGRAPHY NOS |
| 3614 AORTCOR BYPAS-4+ COR ART | 3834 AORTA RESECTION & ANAST | 8851 VENA CAV ANGIOCARDIOGRAM |
| 3615 1 INT MAM-COR ART BYPASS | 3835 THOR VESSEL RESECT/ANAST | 8852 RT HEART ANGIOCARDIOGRAM |
| 3616 2 INT MAM-COR ART BYPASS | 3836 ABD VESSEL RESECT/ANAST | 8853 LT HEART ANGIOCARDIOGRAM |
| 3617 ABD-CORON ARTERY BYPASS | 3837 ABD VEIN RESECT & ANAST | 8854 RT & LT HEART ANGIOCARD |
| 3619 HRT REVAS BYPS ANAS NEC | 3838 LEG ARTERY RESECT/ANAST | 8855 CORONAR ARTERIOGR-1 CATH |
| 362 ARTERIAL IMPLANT REVASC | 3839 LEG VEIN RESECT/ANASTOM | 8856 CORONAR ARTERIOGR-2 CATH |
| 3631 OPEN CHEST TRANS REVASC | 3840 VESSEL RESECT/REPLAC NOS | 8857 CORONARY ARTERIOGRAM NEC |
| 3632 OTH TRANSMYO REVASCULAR | 3841 INTRACRAN VES RESEC-REPL | 8858 NEGATVE-CONTR CARDIOGRAM |
| 3639 OTH HEART REVASCULAR | 3842 HEAD/NECK VES RESEC-REPL | 8944 CARDIAC STRESS TEST NEC |
| 3691 CORON VESS ANEURYSM REP | 3843 ARM VES RESECT W REPLACE | 8945 PACEMAKER RATE CHECK |
| 3699 HEART VESSEL OP NEC | 3844 RESECT ABDM AORTA W REPL | 8946 PACEMAKER WAVE FORM CHCK |
| 370 PERICARDIOCENTESIS | 3845 RESECT THORAC VES W REPL | 8947 PACEMAKER IMPEDANCE CHCK |
| 3710 INCISION OF HEART NOS | 3846 ABD ARTERY RESEC W REPLA | 8948 PACEMAKER VOLT THRESHOLD |
| 3711 CARDIOTOMY | 3847 ABD VEIN RESECT W REPLAC | 8949 AICD CHECK |
| 3712 PERICARDIOTOMY | 3848 LEG ARTERY RESEC W REPLA | 8950 AMBU CARDIAC MONITORING |
| 3721 RT HEART CARDIAC CATH | 3849 LEG VEIN RESECT W REPLAC | 8951 RHYTHM ELECTROCARDIOGRAM |
| 3722 LEFT HEART CARDIAC CATH | 3850 VARICOSE V LIG-STRIP NOS | 8952 ELECTROCARDIOGRAM |
| 3723 RT/LEFT HEART CARD CATH | 3851 INTCRAN VAR V LIG-STRIP | 8953 VECTORCARDIOGRAM |
| 3724 PERICARDIAL BIOPSY | 3852 HEAD/NECK VAR V LIG-STR | 8954 ELECTROCARDIOGRAPH MONIT |
| 3725 CARDIAC BIOPSY | 3853 ARM VARICOSE V LIG-STRIP | 8955 PHONOCARDIOGRAM |
| 3726 CARDIAC ELECTROPHY STIM | 3855 THORAC VAR V LIG-STRIP | 8956 CAROTID PULSE TRACING |
| 3727 CARDIAC MAPPING | 3857 ABD VARICOS V LIGA-STRIP | 8957 APEXCARDIOGRAM |
| 3728 INTRACARDIAC ECHOCARDIO | 3859 LEG VARICOS V LIGA-STRIP | 8958 PLETHYSMOGRAM |
| 3729 HRT/PERICAR DX PROC NEC | 3860 EXCISION OF VESSEL NOS | 8959 NONOP CARDIAC/VASC EXAM |
| 3731 PERICARDIECTOMY | 3861 INTRACRAN VESSEL EXCIS | 8969 CORONARY BLD FLOW MONIT |
| 3732 HEART ANEURYSM EXCISION | 3862 HEAD/NECK VESSEL EXCIS | 9336 CARDIAC RETRAINING |
| 3733 EXC/DEST HRT LESION OPEN | 3863 ARM VESSEL EXCISION | 9960 CARDIOPULM RESUSCITA NOS |
| 3734 EXC/DEST HRT LES OTHER | 3864 EXCISION OF AORTA | 9961 ATRIAL CARDIOVERSION |
| 3735 PARTIAL VENTRICULECTOMY | 3865 THORACIC VESSEL EXCISION | 9962 HEART COUNTERSHOCK NEC |
| 3741 IMPL CARDIAC SUPPORT DEV | 3866 ABDOMINAL ARTERY EXCIS | 9963 CLOSED CHEST CARD MASSAG |
| 3749 HEART/PERICARD REPR NEC | 3867 ABDOMINAL VEIN EXCISION | 9964 CAROTID SINUS STIUMLAT |
| 3751 HEART TRANSPLANTATION | 3868 LEG ARTERY EXCISION | 9969 CARDIAC RHYTHM CONV NEC |
Footnotes
Conflicts of Interest: The authors report no conflicts of interest.
REFERENCES
- 1.Heidenreich PA, Trogdon JG, Khavjou OA, et al. Forecasting the Future of Cardiovascular Disease in the United States: A Policy Statement From the American Heart Association. Circulation. 2011 Mar 1;123(8):933–944. doi: 10.1161/CIR.0b013e31820a55f5. 2011. [DOI] [PubMed] [Google Scholar]
- 2.NHLBI Morbidity & Mortality: 2012 Chart Book on Cardiovascular, Lung and BloodDiseases. 2012 http://www.nhlbi.nih.gov/files/docs/research/2012_ChartBook.pdf.
- 3.Likosky DS, Zhou W, Malenka DJ, Borden WB, Nallamothu BK, Skinner JS. Growth in medicare expenditures for patients with acute myocardial infarction: a comparison of 1998 through 1999 and 2008. JAMA Intern Med. 2013 Dec 9-23;173(22):2055–2061. doi: 10.1001/jamainternmed.2013.10789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2013 update: a report from the American Heart Association. Circulation. 2013 Jan 1;127(1):e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Margaret Jean Hall PDCJD, Ph.D. Williams Sonja N., Aleksandr Golosinskiy, Alexander Schwartzman. National Hospital Discharge Survey: 2007 Summary. National Health Statistics Report. 2010 M.P.H. M.S. DoHCS. http://www.cdc.gov/nchs/data/nhsr/nhsr029.pdf. [PubMed]
- 6.CDC Tracking Heart Attacks. http://ephtracking.cdc.gov/showHeartCollectingData.action.
- 7.People.gov H Heart Disease and Stroke. http://www.healthypeople.gov/2020/topics-objectives/topic/heart-disease-and-stroke.
- 8.Suter LG, Li SX, Grady JN, et al. National Patterns of Risk-Standardized Mortality and Readmission After Hospitalization for Acute Myocardial Infarction, Heart Failure, and Pneumonia: Update on Publicly Reported Outcomes Measures Based on the 2013 Release. J. Gen. Intern. Med. 2014 May 14; doi: 10.1007/s11606-014-2862-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Krumholz HM, Normand SL, Wang Y. Trends in Hospitalizations and Outcomes for Acute Cardiovascular Disease and Stroke: 1999-2011. Circulation. 2014 Aug 18; doi: 10.1161/CIRCULATIONAHA.113.007787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Talbott EO, Rager JR, Brink LL, et al. Trends in acute myocardial infarction hospitalization rates for US States in the CDC tracking network. PLoS One. 2013;8(5):e64457. doi: 10.1371/journal.pone.0064457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang OJ, Wang Y, Chen J, Krumholz HM. Recent trends in hospitalization for acute myocardial infarction. AJC. 2012 Jun 1;109(11):1589–1593. doi: 10.1016/j.amjcard.2012.01.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010 Mar 23;121(11):1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 13.Krumholz HM, Merrill AR, Schone EM, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009 Sep;2(5):407–413. doi: 10.1161/CIRCOUTCOMES.109.883256. 2009. [DOI] [PubMed] [Google Scholar]
- 14.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. The New England journal of medicine. 2010 Jun 10;362(23):2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 15.Fang J, Alderman MH, Keenan NL, Ayala C. Acute myocardial infarction hospitalization in the United States, 1979 to 2005. The American journal of medicine. 2010 Mar;123(3):259–266. doi: 10.1016/j.amjmed.2009.08.018. [DOI] [PubMed] [Google Scholar]
- 16.Services CfMM [May 6, 2015];Medicare Claims Processing Manual: Chapter 23- Fee Schedule Administration and Coding Requirements. 2015 http://www.cms.gov/Regulations-and-Guidance/Guidance/Manuals/downloads/clm104c23.pdf.
- 17.CMS Files for FY 2008 Final Rule and Correction Notice. 2008 http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Acute-Inpatient-Files-for-Download-Items/CMS1247844.html.
- 18.Centers for Medicare & Medicaid Services [May 4, 2015];Details for title: Files for FY 2006 Final Rule and Correction Notice. 2015 http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Acute-Inpatient-Files-for-Download-Items/CMS1255496.html.
- 19.Register F. <Federal Register, Volume 72 Issue 162 (Wednesday, August 22, 2007).pdf>. 722007 [Google Scholar]
- 20.Alpert JS, Thygesen K. Myocardial Infarction Redefined—A Consensus Document of The Joint European Society of Cardiology/American College of Cardiology Committee for the Redefinition of Myocardial Infarction. JACC. 2000;36(3):959–969. doi: 10.1016/s0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- 21.Krumholz HM, Wang Y, Chen J, et al. Reduction in Acute Myocardial Infarction Mortality in the United States: Risk-Standardized Mortality Rates From 1995-2006. JAMA. 2009 Aug 19;:767–773. doi: 10.1001/jama.2009.1178. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Commission TJ Specifications Manual for Joint Commission National Quality Core Measures (2010A1) 2010 https://manual.jointcommission.org/releases/archive/TJC2010B/MIF0023.html.
- 23.Werner RM, Bradlow ET. Relationship Between Medicare’s Hospital Compare Performance Measures and Mortality Rates. JAMA. 2006 Dec 13;:2694–2702. doi: 10.1001/jama.296.22.2694. 2006. [DOI] [PubMed] [Google Scholar]
- 24.Shroff GR. Acute Myocardial Infarction: What’s in a Name? Ann. Intern. Med. 2015;162:448–449. doi: 10.7326/M14-2259. [DOI] [PubMed] [Google Scholar]
- 25.Shroff GR, Solid CA, Herzog CA. Medicare claims for myocardial infarction as primary vs. secondary diagnosis. Int. J. Cardiol. 2015 Mar 1;182:412–413. doi: 10.1016/j.ijcard.2014.12.141. [DOI] [PubMed] [Google Scholar]
- 26.Thygesen K, Alpert JS, White HD. Joint ESCAAHAWHFTFftRoMI. Universal definition of myocardial infarction. J. Am. Coll. Cardiol. 2007 Nov 27;50(22):2173–2195. doi: 10.1016/j.jacc.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 27.Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. J. Am. Coll. Cardiol. 2012 Oct 16;60(16):1581–1598. doi: 10.1016/j.jacc.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 28.CMS.gov. Details for title: Files for FY 2008 Final Rule and Correction Notice. 2008 http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Acute-Inpatient-Files-for-Download-Items/CMS1247844.html.
- 29.CMS Outcome Measures. 2013 10/02/2013: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/OutcomeMeasures.html.
- 30.Lindenauer PK, Lagu T, Shieh M, Pekow PS, Rothberg MB. Association of Diagnostic Coding With Trends in Hospitalizations and Mortality of Patients With Pneumonia, 2003-2009. JAMA. 2012 Apr 4;:1405–1413. doi: 10.1001/jama.2012.384. 2012. [DOI] [PubMed] [Google Scholar]
- 31.Blecker S, Paul M, Taksler G, Ogedegbe G, Katz S. Heart failure-associated hospitalizations in the United States. J. Am. Coll. Cardiol. 2013 Mar 26;61(12):1259–1267. doi: 10.1016/j.jacc.2012.12.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kronick R, Welch WP. Measuring Coding Intensity in the Medicare Advantage Program. Medicare Medicaid Res Rev. 2014:4–2. doi: 10.5600/mmrr2014-004-02-a06. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Song Y, Skinner J, Bynum J, Sutherland J, Wennberg JE, Fisher ES. Regional Variations in Diagnostic Practices. N. Engl. J. Med. 2010 Jul 1;:45–53. doi: 10.1056/NEJMsa0910881. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Welch HG, Sharp SM, Gottlieb DJ, Skinner JS, Wennberg JE. Geographic Variation in Diagnosis Frequency and Risk of Death Among Medicare Beneficiaries. JAMA. 2011 Mar 16;305(11):1113–1118. doi: 10.1001/jama.2011.307. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]