Abstract
Extensive evidence leads us to expect that health disparities by race and socioeconomic status found in one generation might be reproduced in the next. To the extent that this occurs it is important to assess life course processes responsible for the reproduction. Prospective evidence concerning such life course processes is hard to come by as it requires long-term follow-up of individuals from childhood through adult life. We present data from the Child Health and Development Disparities study that provides evidence relevant to this issue with respect to self-rated health. Mothers and offspring recruited in California's Bay Area between 1959 and 1967 were assessed during pregnancy with follow-up exams of offspring along with in-person interviews with mothers (at offspring ages 5, 9–11, 15–17) and offspring (at ages 15–17, ~50). Available data allow us to assess the importance of three potential life course pathways in the reproduction of inequalities in self-rated health – socioeconomic pathways, cognitive pathways and pathways involving emerging health itself. As expected we found that race and SES disparities in SRH are reproduced across generations. They are evident in mothers, not strong or significant in offspring at 15–17, but present once again in offspring at age ~50. Concerning potential pathways, we found that indicators of child health were related to adult SRH and played some role in accounting for race but not SES disparities in adult SRH. Cognitive abilities were unrelated to adult SRH with childhood SES controlled. Childhood SES was associated with adult SRH independent of other childhood factors and is reduced to non-significance only when offspring college attainment is controlled. Race and SES disparities in self-reported health in one generation are re-expressed in the next with strongest support for SES pathways in this transmission.
Keywords: Race and SES health disparities, Self-rated health, Life course
Extensive evidence concerning race and socioeconomic disparities in health across places, times and cohorts (Adler et al., 1994; Braverman and Barclay, 2009; Haas et al., 2012; Phelan et al., 2010; Mackenbach et al., 2015; Williams and Sternthal, 2010; Zheng et al., 2011) strongly suggest that such disparities are reproduced in successive generations through life course processes. Additionally, evidence that childhood experience has a “long arm” when it comes to the generation of adult health inequalities strongly implicates life course processes (Kuh et al., 2014; Hayward and Gorman, 2004; Haas, 2008; Pavalko and Caputo, 2013). Although many study designs can help understand which life course processes are most important in generating health disparities prospective studies that collect data at multiple time points throughout the life course allow the opportunity to assess factors that could not be accurately recalled in adult life. However, studies like the one we will describe that follow individuals from before birth through childhood and then at midlife (~50) are relatively rare. Whereas impressive studies exist in Great Britain (e.g. Power and Elliott, 2006; Kuh et al., 2011) and several Scandinavian countries (e.g. Padyab and Norberg, 2014) the populations studied were largely homogeneous with respect to race. Here we describe a study that prospectively assesses social conditions, cognitive abilities, and emerging health as life course processes that may be involved in the generation of health inequalities by race and SES in the adult life.
In this first report we focus on self-rated health (SRH) because it captures how “healthy” people feel and predicts objective outcomes like mortality (Idler and Benyamini, 1997; DeSalvo et al., 2006). Prior studies of SRH point to early experiences as important for initiating processes that continue through life to create disparities in adult life (Haas, 2008; Umberson et al., 2014; Bauldry et al., 2012; Luo and Waite, 2005). The present study builds on this prior literature in two ways. First, our study includes an assessment of mother's SRH that allows us to directly assess whether race and SES disparities in one generation (mothers) are also evident in the next (offspring) (see also Salsberry et al., 2013). Second, we use prospectively collected information concerning emerging health, cognitive abilities and family socioeconomic circumstances at multiple points during the life course that either could not have been ascertained in a retrospective study or would have been subject to possible recall biases.
1. Three potential life course pathways leading to race and SES disparities in adult life
Our primary goal is to use prospectively collected life-course data to evaluate the empirical yield of three potential pathways in the emergence of adult-life disparities in self-rated health – socioeconomic pathways, cognitive pathways and pathways involving emerging health itself. As a prelude to our analysis we briefly introduce the theoretical rationale for each of these pathways as they have been articulated in prior research.
If socioeconomic circumstances (SES) are an important pathway, relatively better positioned parents might confer superior socioeconomic circumstances to their offspring either directly through inheritance or indirectly by fostering educational and occupational attainment. Explanations as to how socioeconomic factors might then affect health involve many possible influences including the following prominent and inter-related possibilities. First, socioeconomic factors might broadly shape exposure to acute and chronic stressors that wear on the body ultimately leading to bodily system breakdown (Pearlin et al., 2005; Seeman et al., 2004; Geronimus et al., 2006). Second socioeconomic circumstances may also influence “health lifestyles” conceptualized as collective factors that characterize “status groups” (Weber, 1978) and influence behaviors such as smoking, diet, exercise, and preventive health behaviors (Mirowsky and Ross, 2003; Cockerham, 2005). Third, as argued by fundamental cause theory resources of knowledge, money power, prestige and beneficial social connections dynamically shape health by allowing better positioned people to avoid risks and adopt protective strategies even as such factors change over time (Link and Phelan, 1995; Phelan et al., 2010). Finally and also consistent with fundamental cause theory (Link and Phelan, 2010; Freese and Lutfe, 2011), access to socioeconomic related resources confers potential advantage through contextual influences on health such as through neighborhood and work environments that are on average less noxious in better resourced contexts (Williams and Collins, 2001; Sharkey and Faber, 2014). With respect to racial disparities, socioeconomic pathways like these are expected to account for some but not all of the health differences between Blacks and Whites in the United States because of socioeconomic inequalities between the two groups (Phelan and Link, 2015).
If cognitive abilities are an important pathway it could be that children from low SES backgrounds grow up in conditions that are less cognitively stimulating and with parents who are also lower in cognitive abilities than their higher SES counterparts. Together these circumstances could lead to truncated schooling and lower status jobs with lower earnings. The same cognitive limitations could hinder the understanding of basic health related facts and impede the capacity to weigh complex information thereby limiting an individual's ability to fashion a healthy life style across the life course. Individuals who are more cognitively adept are better able to identify health-relevant aspects of their lives, figure out the relevant information required to address the circumstances they experience, and resourcefully construct a plan to maximize their chances for a healthy outcome (Gottfredson, 2004; Deary et al., 2010). As Gottfredson (2004) puts it, “health self-management is inherently complex and thus puts a premium on the ability to learn and solve problems” (p. 189). With respect to racial disparities in health an explanation that focuses on cognitive abilities might explain such disparities by pointing to average differences between Blacks and Whites on tests of cognitive ability.
If emerging health itself is an important pathway we might expect children from low SES families to experience health conditions from the very beginning of life and through adolescence that compromise educational and occupational attainment while at the same time initiating a health trajectory that signals poor health in adult life (Palloni, 2006; Basch, 2011). Some aspects of early health like birth weight and gestational age have been studied extensively using twin studies sibling designs and quasi-experimental circumstances leading to the conclusion that early life is an “important predictor” of long term outcomes including education, income and disability (Aizer and Currie, 2014). If early health affects both the attainment of SES and future health it could be as Palloni (2006) suggests “a plausible explanatory factor for the intergenerational transmission of inequalities (p. 609).” With respect to racial disparities research identifies sizeable differences between Blacks and Whites in early-life health indicators such as birth weight; these same indicators have also been linked to educational attainment and adult health (Aizer and Currie, 2014).
In addition to their prominence in the literature as potential ways to understand why disparities emerge over the life course these three pathways are important for two other reasons. First, each might be conceptualized as a cause of many causes. If one is poor nutrition may be compromised, access to safe parks denied, and excessive family stress over financing experienced. Low cognitive ability could lead to disengagement from school, reduced ability to understand complex health information and the capacity to create a healthy life-style. Poor childhood health could decrease access to robust physical activity, lead to absences from school and be stressful if for example one is teased or bullied by peers. Each is a potential cause of a package of risk and protective factors. Second, each is modifiable. Childhood poverty rates vary dramatically across rich democracies and the types of policies implemented in these countries are strongly related to the amount of poverty their citizens experience (Brady and Bostic, 2015). A host of policies ranging from ones that influence playground safety to ones that influence nutrition and the ability to engage in physical activity are all likely to shape child health outcomes. Finally cognitive pathways are potentially influenced by policies that affect the quality and accessibility of excellent schooling and protect against risks such as lead or other contaminants. Thus the pathways we investigate are both modifiable and important to consider because of their capacity to affect many risk and protective factors.
Of course these three potential pathways are not mutually exclusive and could work in concert to reproduce health disparities across generations through the life course. At the same time a strong version of any one of these three explanations could predominate. Variation in childhood cognitive ability could explain both the attainment of socioeconomic status and the development of a healthy life style thereby casting doubt on the importance of the cascade of circumstances that social causation theorists have implicated as mechanisms linking SES and health. Similarly, poor health early in life could fully account for health inequalities later in life bringing the explanatory power of theories focused on SES or cognitive abilities into question. Finally, it is possible that, over the life course, SES-related processes predominate in explaining race and SES health disparities in adult life. Such a formulation would argue that as SES inequalities are reproduced so are health inequalities. The significance of this study is that it brings prospectively assessed life course data to bear in adjudicating which if any of these three pathways predominates in explaining the emergence of health inequalities across generations and through the life course.
2. The Child Health and Development Studies cohort
Participants are the adult offspring of families that were originally recruited as part of the Child Health and Development Studies (CHDS) (2016). Virtually all pregnant women receiving prenatal care from the Kaiser Foundation Health Plan at its facilities in Alameda County, California were recruited to the CHDS (19,044 live births 1959–1967) (van den Berg et al., 1988). Extensive demographic and behavioral information were collected from an in-person interview with the mother during her pregnancy. Clinical information was captured from medical records maintained by Kaiser. Follow-up exams of offspring along with in-person interviews with mothers (at offspring ages 5, 9–11, 15–17) and with offspring (at ages15–17) were conducted among subsets of the cohort. These assessments captured cognition, anthropometry, blood pressure, spirometry, behavior, and psychosocial factors. The Adolescent Study, based on all CHDS births that occurred from 1960 to 1963, includes participants with the maximum number of time points of observation during childhood, 87% were observed at birth, age 5, ages 9–11, and ages 15–17.
The CHDS cohort has been regularly monitored through linkage to the California Department of Motor Vehicles, the California Department of Vital Statistics and the California Cancer Registry (Cohn et al., 2001, 2007, 2010). This on-going surveillance facilitated our ability to locate cohort members at midlife (Susser et al., 2011, Cirillo et al., 2011; Terry et al., 2011; Janevic et al., 2014). Efforts to maintain information about the location of cohort families, the rich data on a relatively large subgroup through adolescence, and sufficient variation in race and SES (see online supplement) make the cohort a strong setting for studying the emergence of health disparities.
3. The CHDS Disparities Study sample
Our objectives were 1) to enroll 350 non-Blacks and 250 Blacks, distributed evenly by gender and 2) to maximize the time points of observation for study participants. To meet these objectives we constructed an eligibility pool of 3196 that was comprised of: 1) a 50% random sample of non-Black male and female participants in the CHDS Adolescent Study; 2) 100% of Black male and female participants in the CHDS Adolescent Study; and 3) a supplementary sample of 100% of Black male and female participants in CHDS follow-up studies at age 5 or ages 9–11. Eligibility requirements were expanded beyond the Adolescent Study for Blacks in order to meet sampling targets. We limited recruitment to California residents (79% of the eligible pool, N = 2514) due to the difficulty and cost of implementing home visits nationwide.
We were able to obtain phone numbers for 1,073 of the eligible pool and achieved target sample sizes after contacting 985 of them (see Fig. 1). Of the 985, 238 (24.5%) were deemed passive refusals when after multiple attempts (always more than 10) we were unable to contact them. A further 142 (14.5%) were contacted and actively refused participation. Of the 605 individuals who participated in the telephone interview 510 (84%) completed the home visit and 497 (82%) the self-administered questionnaire (see online supplement for more information). Human subjects review and approval was obtained from the IRB's at Columbia University and the Public Health Institute, Oakland California.
Fig. 1.
CHDS Disparities Study participation flowchart.
Table 1 describes the time-points in the life-course available for the present study. Because we relaxed the time-point eligibility criteria for Blacks to meet our sampling target, they have fewer time-points of observation than non-Blacks. In addition Blacks had lower response rates among the eligible Adolescent Study pool, 45% vs. 53% for males and 56% vs. 68% for females. Overall 61% of the individuals we sought to recruit agreed to participate (Fig. 1).
Table 1.
Time-points of prospective observation for the CHDS DISPAR Study Sample by Race and Gender.
| Time-points of observation | All
|
non-Black and Male
|
Black and Male
|
non-Black and Female
|
Black and Female
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total
|
Total
|
Total
|
Total
|
Total
|
|||||||||||
| n | N | % | n | N | % | n | N | % | n | N | % | n | N | % | |
| Four time points | |||||||||||||||
| Birth, Ages 5, 9–11, and 15–17 | 420 | 150 | 47 | 156 | 67 | ||||||||||
| Total | 420 | 69.4 | 150 | 84.7 | 47 | 37.3 | 156 | 88.6 | 67 | 53.2 | |||||
| Three time points | |||||||||||||||
| Birth, Ages 9–11 and 15–17 | 54 | 25 | 3 | 20 | 6 | ||||||||||
| Birth, Ages 5 and 9–11 | 42 | 0 | 17 | 0 | 25 | ||||||||||
| Birth, Ages 5 and 15–17 | 2 | 2 | 0 | 0 | 0 | ||||||||||
| Total | 98 | 16.2 | 27 | 15.3 | 20 | 15.9 | 20 | 11.4 | 31 | 24.6 | |||||
| Two time points | |||||||||||||||
| Birth, Age 5 | 49 | 0 | 42 | 0 | 7 | ||||||||||
| Birth, Ages 9–11 | 37 | 0 | 17 | 0 | 20 | ||||||||||
| Birth, Ages 15–17 | 1 | 0 | 0 | 0 | 1 | ||||||||||
| Total | 87 | 14.4 | 0 | 0.0 | 59 | 46.8 | 0 | 0.0 | 28 | 22.2 | |||||
| Total sample | 605 | 100.0 | 177 | 100.0 | 126 | 100.0 | 176 | 100.0 | 126 | 100.0 | |||||
4. Study protocol
We collected data using a 40-min computer assisted telephone interview, a home visit and a self-administered questionnaire. The telephone interview included assessments of socioeconomic circumstances, exposure to discrimination, measures of mental health status, physical activity, health behaviors and SRH, among others (See Table S1 for more details). A home visit involved the measurement of height, weight, blood pressure, spirometry, cognitive tests and a blood draw to obtain biomarker data. A self-administered questionnaire included numerous self-report psychosocial measures that could not be included in the telephone interview.
5. Comparison of recruited to non-recruited CHDS participants
Potential participants who moved out of California did not differ significantly from those who stayed on mother's age, education, employment, father's age, education and employment, family income and offspring birthweight in either Blacks or Whites (not shown). When we assessed differences on these same variables between those who participated and those who did not we found no significant differences (See Supplemental Table S2). Only a small number of cohort members we sought to contact had died (8 Whites, 8 Blacks).
6. Comparison to the National Health and Nutrition Examination Study (NHANES)
We assessed the representativeness of our California-based sample by comparing it to the nationally-representative NHANES (2011–2012). We restricted the NHANES to non-Hispanic White and non-Hispanic Black men and women spanning a similar age range as our study participants (46–52 years). In an online supplement (Tables S3 and S4) we find no differences between our sample and the selected NHANES comparison for BMI, Hemoglobin A1c, systolic and diastolic blood pressure and SRH. Additionally, we found that the disparities in our data were also present in the nationally representative NHANES data – in no instance was a race or education disparity significantly stronger in one sample than in the other.
7. Present study participants
We focus on mothers and offspring interviewed when offspring were 15–17 years old as this is the wave of data collection in which both mothers and offspring were asked questions about SRH. As described above all non-Black participants (N = 353) but only 124 (49.2%) of the Black participants had participated in the earlier adolescent wave of data collection. Using data from earlier waves we found no differences between Black participants included in the adolescent sample and those who were not except for gender (Black males had lower response rates than Black Females) (Table S5 in the online supplement).
8. Measures
Self-Rated Health of mothers was assessed at ages (34–61) when their offspring were ages 15–17. Offspring were assessed at ages 15–17 and again in midlife (ages 47–52). Adolescent SRH was categorized as poor = 4, fair = 3, good = 2, excellent = 1.
Race/Ethnicity was based on participant self-identification in adult life and grouped into non-Hispanic white, (N = 310, 65.0%), Black, (N = 121, 25.4%), and because of small numbers, other race/ethnicity, (N = 46, 9.6%).
Childhood SES assessed as a combination of maternal education at birth with reports of paternal occupation and family income at birth, 9–11 and 15–17 follow ups. Our procedure equally weights maternal education 0) less than high school (N = 53, 9%), 1) high school graduate (N = 187, 31%), 2) some college (N = 123, 20%), and 3) college or more (N = 114, 19%) with the average of the three assessments of paternal occupation and family income. We construct this measure to vary continuously between 0 and 3 as described in the Online Supplement.
Adult SES is assessed as college or more (N = 223, 46.9%) versus less than a college degree, and self-reported family income in 12 categories ranging from $2500 or below to $300,000. We assigned midpoint values to each category and then standardized income values.
Cognition. Peabody picture vocabulary tests (PPVT) were administered to participants at 9–11 and 15–17 assessments (Dunn and Dunn, 1959). We standardized scores from each assessment and averaged the standardized scores from 9 to 11 and 15–17. Scores on the two assessments were strongly correlated with each other (r = 0.70) and the composite measure was a robust predictor of college graduation (Odds Ratio of 8.02 associated with a 2SD change).
Obesity. In adolescence (ages 15–17) participants were weighed and measured and deemed obese if BMI values were above the 95th percentile for age and sex using Centers for Disease Control growth charts that are appropriately standardized based on data from the 1970's. Adolescents scoring between the 85th and 95th percentile were designated overweight.
Externalizing Mental Health Symptoms (21 items Cronbach alpha = 0.86) such as “talks back when told to do anything”, “flares up over nothing – gets mad easily”, and “fights to get his or her way” were assessed when the participants were 9–11 via mother's report of whether the question characterized their child “a lot,” “a little” or “not at all.”
A Child Health Index included the sum of multiple indicators of relatively rare events and conditions including: 1) gestational age 258 days or less, 2) one or more severe anomalies by age 5 (with severe defined as a threat to development or well-being; (see Christianson et al., 1981 for examples), 3) one or more hospitalizations by age 5, 4) heart problem identified at age 5 physical exam, 5) other health-related deviation identified at age 5 physical exam, 6) measured systolic blood pressure at 5 year exam greater than 95th percentile of norms developed from the Pediatric Task Force database and based on age, gender and height, 7) mother report at age 15–17 of child ever being diagnosed with high blood pressure or measured blood pressure above 95% of CDC norms, 8) mother's report at age 15–17 of child ever being diagnosed with asthma, 9) hospitalization during year before 15–17 interview. Each indicator is assigned a “1” for present and “0” for absent. About half (50.6%) of children experienced none of these problems, 35% experienced one, 10.1% two and only 4.3% three or more.
9. Statistical analysis
We first performed descriptive analyses to determine the percent of mothers, offspring during adolescence, and offspring in adulthood reporting fair or poor SRH by race/ethnicity and by quartiles of childhood SES.
We conducted logistic regression analyses to examine the extent to which identified racial and/or SES disparities in SRH among adult offspring were accounted for by measures associated with the three life-course pathways; 1) SES pathways as assessed by childhood SES, adult college attainment and adult family income, 2) cognitive pathways as assessed at ages 9 and 15–17, and 3) emerging health as assessed by childhood and adolescent physical and mental health indicators.
We first examined the independent association between each individual covariate and SRH adjusting for participant age and gender. Next, to determine the extent to which the sets of covariates accounted for the association between race and SRH, and between childhood SES and SRH, we conducted a series of five regressions that adjusted sequentially, in temporal order, for covariates of interest. Equation 1 first adjusted for childhood SES; as childhood SES is strongly related to race and a determinant of health disparities all subsequent equations adjusted for this variable. Equations 2–4 then additionally adjusted one at a time for childhood cognition, childhood health indicators, and adult educational attainment to determine their impact of racial and SES health disparities. A final regression model included all sets of covariates and additionally adjusted for adult income. When relevant we report in the text the percent change in the logistic regression coefficient associated with adjusted odds ratio as covariates are added to determine whether or not the association between race and, where applicable, SES and SRH were appreciably changed with the addition of covariates (percent change = (regression coefficient before adjustment – regression coefficient after adjustment)/regression coefficient before adjustment (Rothman, 2012; Mirowsky, 2013)).
Since there is evidence of interactive effects between SES and both gender and race in the production of health disparities (Williams and Sternthal, 2010), we also explored the potential modification of each of our predictor variables by race and gender.
We evaluate whether and to what extent evidence supports a particular pathway by evaluating the observed pattern of findings. If SES pathways are prominently expressed we would expect the coefficient for childhood SES to be sizeable and significant in predicting adult self-rated health even when measures of alternative cognitive and emerging health pathways are entered as covariates. Further we would expect childhood SES to account for some part of the racial disparity in self rated health and to only be accounted for itself by indicators of adult SES such as college completion and family income.
If cognitive pathways are prominent we would expect co-efficients for child/adolescent cognition to be sizeable and significant even when variables associated with alternative socioeconomic and emerging health pathways are entered as covariates. A strong profile of results for cognitive pathways would also show that cognitive ability partially explains race and SES associations with adult self-rated health.
Finally, if emerging health itself is a prominent pathway in explaining adult disparities in self-rated health we would expect coefficients for childhood health conditions, adolescent BMI and overweight, and adolescent self-rated health to be sizeable and significant even when variables associated with alternative SES and cognition pathways are held constant. Further such child health indicators should play some role in accounting for race and SES disparities in adult self-rated health.
We used multiple imputation (20 imputations) (SAS version 9.3) to predict missing values using all independent and dependent variables from our analysis, as well as several auxiliary variables (e.g. BMI at the 5- and 9–11) National Health and Nutrition Examination Survey (2016) (Allison, 2001). Results from our multiple imputation approach (N = 476) are reported below but conform closely to results from a complete case analysis (N = 360). All analyses were conducted using SAS version 9.3 (SAS Institute Inc.).
10. Results
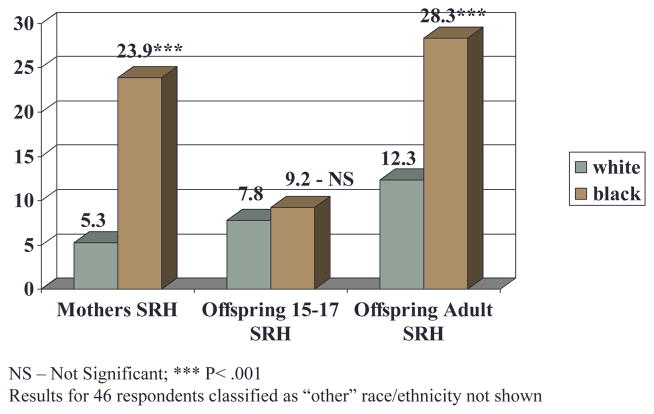
Figs. 2 and 3 show race and SES disparities in SRH that are strongly evident in mothers, not strong or significant in offspring at 15–17, but strongly present in offspring at age ~50. These patterns hold within offspring gender and are independent of maternal age.
Fig. 2.
Percent fair\poor self-rated health by race/enthnicity: Mothers when offspring are 15–17, offspring at 15–17 and offspring as adults.
Fig. 3.
Percent fair\poor self-rated health by quartiles of childhood socioeconomic status: Mothers when offspring are 15–17, offspring at 15–17 and offspring as adults.
Table 2 column 1 shows significant odds ratios for each predictor of SRH, controlling for age, gender and a dummy variable for “other” ethnicity. Concerning disparities, Black participants experience an estimated tripling (OR = 3.09, CI 1.80–5.31) of the odds of fair or poor SRH as compared to whites, and with every one standard deviation elevation in Child SES participants experience a substantial reduction in their odds of fair/poor SRH (OR = 0.56, CI 0.43 – 0.73).
Table 2.
Odd Ratios for Logistic regression: Fair/poor adult self-rated health predicted by indicators of child and adolescent health, intelligence, and socioeconomic status (N = 476).a
| Variable | Odds ratios (95% confidence intervals)
|
|||||
|---|---|---|---|---|---|---|
| Odds ratios Age and gender Adjusted |
Equation 1 | Equation 2 | Equation 3 | Equation 4 | Equation 5 | |
| Black Americians | 3.09*** (1.80, 5.31) | 2.12* (1.18, 3.82) | 1.86* (1.00, 3.45) | 1.55 (0.82, 2.94) | 2.22* (1.21, 4.10) | 1.65 (0.81, 3.37) |
| Childhood SES (standardized) | 0.56*** (0.43, 0.73) | 0.64** (0.48, 0.85) | 0.68* (0.51, 0.93) | 0.65** (0.48, 0.88) | 0.83 (0.60, 1.14) | 0.83 (0.59, 1.18) |
| Childhood cognition (standardized) | 0.57*** (0.43, 0.77) | – | 0.79 (0.56, 1.10) | – | – | 1.05 (0.71, 1.55) |
| Adolescent self-rated healthb | 2.25*** (1.48, 3.43) | – | – | 2.35*** (1.49, 3.73) | – | 2.01** (1.25, 3.23) |
| Adolescent obesity | 4.77*** (1.99, 11.4) | – | – | 3.15* (1.21, 8.18) | – | 3.52* (1.27, 9.72) |
| Adolescent overweight | 3.70*** (1.84, 7.45) | – | – | 2.84** (1.28, 6.31) | – | 2.82* (1.23, 6.43) |
| Child and adolescent health conditions | 1.57*** (1.21, 2.03) | – | – | 1.55** (1.17, 2.05) | – | 1.58** (1.17, 2.11) |
| Externalizing Behaviors (standardized) | 1.56*** (1.21, 2.01) | – | – | 1.50** (1.12, 2.01) | – | 1.35 (0.99, 1.83) |
| Graduated college | 0.17*** (0.09, 0.31) | – | – | – | 0.20*** (0.10, 0.40) | 0.31** (0.14, 0.66) |
| Adult family income (standardized) | 0.51*** (0.37, 0.70) | – | – | – | – | 0.67* (0.47, 0.94) |
p < 0.05;
p < 0.01;
p < 0.001.
All equations include controls for age, gender and the non-significant effects of a dummy variable for “other” race. One participant was missing the outcome variable self-rated health and was removed from the analysis.
Adolescent self-rated health fair 3, good 2, excellent 1.
Equation 1 shows that when race and SES are entered together, the odds ratio for race remains significant but is reduced (3.09–2.12) with the logistic regression coefficient for race declining by 33% from before to after control for childhood SES a finding that suggests that some part of the Black- White difference is attributable to the fact that Black participants were lower in socioeconomic status in childhood. Equation 2 assesses the impact of adding a measure of childhood cognition on the race and SES disparities shown in Equation 1. Whereas childhood cognition is associated with SRH before race and childhood SES are controlled its logistic regression coefficient is decreased by 58% and is no longer significant after race and childhood SES variables are added. Coefficients associated with SES and race disparities are slightly reduced (13% and 17% respectively) upon control for cognition, but each remains significantly associated with SRH.
As Equation 3 shows, adolescent SRH, obesity, overweight, externalizing mental health symptoms, and the index of child health problems are each independently and sometimes relatively strongly associated with adult SRH. Each unit of worsening adolescent SRH is associated with more than a doubling of the odds (OR 2.35, CI 1.49–3.73) of fair/poor adult SRH. Obesity (OR 3.15, CI 1.21–8.18) and overweight (OR 2.84, CI 1.28–6.31) as an adolescent are associated with substantially elevated odds of fair/poor adult SRH. A one-unit increase in child health problems and in child externalizing symptoms are associated with 1.55-fold (CI 1.17–2.05) and 1.50-fold (CI 1.12–2.01) increases in the odds of fair/poor adult SRH respectively. Adding child and adolescent health measures reduces the effect of race on adult SRH by 42% rendering it non-significant. Adolescent obesity, child health problems and externalizing behaviors each contributed to this decline (not shown). In contrast to race, the effect of childhood SES remains significant and essentially unchanged when comparing Equation 1 (OR = 0.64) to Equation 3 (OR = 0.65).
Equation 4 shows that a person who has graduated from college has 1/5 t h the odds (OR 0.20, CI 0.10 – 0.40) of experiencing fair/poor SRH as compared to a person who has not completed college. Critical to our understanding of the transmission of disparities, we find that controlling for college education attenuates the odds ratio associated with childhood SES from a significant 0.64 (Equation 1) to a non-significant 0.83 (Equation 4); a 58% decline when comparing the logistic regression coefficient before controlling college attainment to after controlling it. At the same time, despite the relatively strong protective effect of college education, we see that it plays almost no role in explaining the black-white disparity in SRH (2.12 – Equation 1; 2.22 Equation 4).
Equation 5 shows results with all predictors entered simultaneously. Child and adolescent health measures (with the exception of externalizing behaviors) remain significantly associated with adult SRH as do college education and adult family income. Cognition plays no significant role with these other variables controlled. We checked for interaction between the predictor variables in Table 2 and race and gender. Among the many comparisons we examined two that are consistent with other literature were apparent in our data as well; the benefit of college educational attainment and income for SRH were not as strong in blacks as in whites. However, in all instances the coefficients were in the same direction across race and gender groupings and in no case did the point estimate in one group fall outside of the confidence bounds of the estimate in the other group.
11. Discussion
We introduced the CHDS Disparities Study one of a relatively small set of studies that provides health-related data across the life course. It is especially unusual in its inclusion of sufficient numbers of both Black and White respondents to investigate life-course hypotheses about racial as well as SES disparities. In this paper we capitalized on an unusual opportunity to investigate the transmission of health disparities in SRH across generations and through the life course. We found that race and education disparities in SRH were substantial in the mothers of cohort members, generally absent when cohort members were adolescents, but prominent as the cohort aged into midlife. We considered three plausible life-course explanations that we conceptualized as potential causes of many causes – SES pathways, cognitive pathways and pathways involving emerging health. Any one of these pathways could have been supported by the data we collected but as we discuss below some proved more important than others. Specifically, while we found some support for each of the potential pathways we found strongest support for SES pathways, followed by child health pathways and least support for cognitive pathways. Before considering implications of our results we turn to consideration of the strengths and limitations of the study so that our conclusions can be considered in light of such strengths and limitations.
11.1. Strengths and limitations
As would be expected in a 50-year follow up study we were unable to recruit every eligible subject. Still, we found little evidence of bias either in comparisons based on archived data of recruited and non-recruited subjects or in comparisons between our sample and the nationally representative NHANES data. This first report from the CHDS Disparities Study focuses only on SRH and although this is an important health indicator subsequent investigations will examine disparities in obesity, lung function, allostatic load and other outcomes of interest. As we proceed to these other outcomes it is possible that the pattern of results found in this analysis will not be replicated, a result that would push us away from general conclusions about the importance of the three pathways to more specific and nuanced ones. An additional issue is evidence indicating that measures of self-rated health produce discrepancies concerning time trends in SRH across data sets and population groups that raise validity concerns for this otherwise simple but useful measure (Saloman et al., 2009). Finally, we focused on SES, cognition, and emerging health, across the life course and while measurement within these domains was arguably strong we have left for future research the inclusion of additional covariates such as the experience of discrimination that we measured only in adult life. The multi-generational data, the long-term follow up at age 50, the racially diverse sample and the multiple prospective assessments of childhood SES, childhood cognition (ages 9 and 15–17), child health variables are strengths of the study.
11.2. Implications for potential pathways
With respect to cognitive pathways our study is unique in its capacity to assess the role of cognition in the context of comprehensive measurement of childhood SES. While cognitive ability (assessed twice 9 and 15–17) was robustly associated with adult SRH when age, gender and race ethnicity were controlled the addition of childhood SES sharply reduced the association. The fact that cognition plays no significant role in predicting adult SRH when child SES is controlled runs counter to a meta-analysis on the role of cognition in predicting mortality (Calvin et al., 2011). This meta-analysis concluded that adjustment for childhood socioeconomic status had “almost no impact” on the relationship between cognitive ability and mortality and that childhood SES is therefore “not a confounder of the intelligence–mortality association.” But the measurement of childhood SES in these studies was not strong consisting of only a single indicator, assessed at a single time, and focused only on paternal indicators of SES circumstances. In our study childhood SES was based on multiple indicators – mother's education, father's occupation, and family income with family income and father's occupation assessed at three time points during youth. We suspect that the difference in findings between our study and the meta-analysis is due to this difference in the adequacy of the available measures of childhood SES. Beyond the issue of the role of childhood SES our study joins other studies that have assigned a relatively modest independent role for cognition in accounting for adult health status when adult SES is controlled (Calvin et al., 2011; see Davis et al., 2016 for an interesting counter point) and particularly when it is controlled comprehensively (Link et al., 2008; Clouston et al., 2015). As expected, we found a strong association between cognitive ability and adult educational attainment which is in turn associated with adult SRH, a pattern of results that suggests a possibly substantial indirect role for cognitive ability that operates through educational attainment. At the same time, the lack of an effect of cognitive ability independent SES casts doubt on explanations, like the one we offered in the introduction that portray cognitive abilities as a key active ingredient people use to construct a healthy lifestyle.
The evidence concerning child health joins many other studies that have shown substantial effects of early health on later health. In this way our results are consistent with research that suggests a “long arm” for childhood experience and supports a life-course conceptualization of health as something that builds over a life time (Hayward and Gorman, 2004; Hatch, 2005; Pearlin et al., 2005). As the first study we know of to follow Black and White individuals through the life course our finding that child health plays a role in accounting for race disparities in adult SRH is an important one. It suggests that some part of the large race disparities in health in this cohort have origins in early health circumstances. At the same time even though multiple child health indicators are related to adult SRH (sometimes quite strongly) they did not lead to a substantial attenuation of coefficients for child SES or adult education and income. Thus, unlike the situation with race disparities we are unable to conclude that child health plays a large role in producing SES-related health disparities in adult life.
With respect to pathways involving SES we found a substantial association between childhood SES and adult SRH that is only diminished to non-significance when adult attainment of a college education is controlled. Additionally, childhood SES plays a substantial but not a complete role in explaining Black/White disparities in adult SRH. Finally, adult education and income are independently associated with adult SRH with all other variables in the model held constant. These findings are particularly significant given that they remained robust even when two other pathways (cognition and child health) were multi-operationalized in a prospective design. Together, they suggest that SES pathways play a substantial role in reproducing health disparities by race and SES. When socioeconomic inequality is reproduced across generations and over the life course health inequalities are reproduced as well. Such a conclusion is consistent with explanations indicating that low SES confers adversity and stress that wears on individuals over time thereby influencing their health outcomes in adult life (Ben-Shlomo and Kuh, 2002; Hatch, 2005; Pearlin et al., 2005), with “health lifestyle” that posits strong social shaping of risk and protective factors (Cockerham, 2005) or with explanations that focus on SES-related “flexible” resources (knowledge, money, power, prestige and beneficial social connections) that either individually or collectively shape exposure to risks and influence the adoption of protective factors (Phelan et al., 2010; Freese and Lutfey, 2011). As such, the findings support the conclusion that SES and race inequalities in health are in some large part reproduced over the life course and across generations through the reproduction of SES inequalities and the differences in resources and adversity that such inequalities put in place.
Supplementary Material
Acknowledgments
This research was funded by a grant from the National Institute for Child Health and Development (NICHD) R01HD058515.
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.socscimed.2016.11.035.
References
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, Syme SL. Socioeconomic status and health: the challenge of the gradient. Am Psychol. 1994;49(1):15. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Aizer A, Currie J. The intergenerational transmission of inequality: maternal disadvantage and health at birth. Science. 2014 May 23;344(6186):856–861. doi: 10.1126/science.1251872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison PD. Missing Data. Sage; Thousand Oaks, CA: 2001. [Google Scholar]
- Basch CE. Healthier students are better learners: a missing link in school reforms to close the achievement gap. J Sch Health. 2011;81(10):593–598. doi: 10.1111/j.1746-1561.2011.00632.x. [DOI] [PubMed] [Google Scholar]
- Bauldry S, Shanahan MJ, Boardman JD, Miech RA, Macmillan R. A life course model of self-rated health through adolescence and young adulthood. Soc Sci Med. 2012;75(7):1311–1320. doi: 10.1016/j.socscimed.2012.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31(2):285–293. [PubMed] [Google Scholar]
- Brady D, Bostic A. Paradoxes of social policy welfare transfers, relative poverty, and redistribution preferences. Am Sociol Rev. 2015;80(2):268–298. [Google Scholar]
- Braveman P, Barclay C. Health disparities beginning in childhood: a life-course perspective. Pediatrics. 2009;124(Suppl 3):S163–S175. doi: 10.1542/peds.2009-1100D. [DOI] [PubMed] [Google Scholar]
- Calvin CM, Deary IJ, Fenton C, Roberts BA, Der G, Leckenby N, Batty GD. Intelligence in youth and all-cause-mortality: systematic review with meta-analysis. Int J Epidemiol. 2011 Jun 1;40(3):626–644. doi: 10.1093/ije/dyq190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [accessed 17.02.16];Child Health and Development Studies. at: http://chdstudies.org/
- Christianson RE, van den Berg B, Milkovich L, Oechsli FW. Incidence of congenital anomalies among white and black live births with long-term follow-up. Am J Public Health. 1981;71(12):1333–1341. doi: 10.2105/ajph.71.12.1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cirillo PM, Cohn BA, Krigbaum NY, Lee M, Brazil C, Factor-Litvak P. Effect of maternal coffee, smoking and drinking behavior on adult son's semen quality: prospective evidence from the Child Health and Development Studies. J Dev Orig Health Dis. 2011;2(6):375–386. doi: 10.1017/S2040174411000584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouston SA, Richards M, Cadar D, Hofer SM. Educational inequalities in health behaviors at midlife is there a role for early-life cognition? J health Soc Behav. 2015 Sep 1;56(3):323–340. doi: 10.1177/0022146515594188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cockerham WC. Health lifestyle theory and the convergence of agency and structure. J Health Soc Behav. 2005;46(1):51–67. doi: 10.1177/002214650504600105. [DOI] [PubMed] [Google Scholar]
- Cohn B, Cirillo P, Christianson R, van den Berg B, Siiteri P. Placental characteristics and reduced risk of maternal breast cancer. J Natl Cancer Inst. 2001;93(15):1133–1140. doi: 10.1093/jnci/93.15.1133. [DOI] [PubMed] [Google Scholar]
- Cohn BA, Wolff MS, Cirillo PM, Sholtz RI. DDT and breast cancer in young women: new data on the significance of age at exposure. Environ Health Perspect. 2007;115(10):1406–1414. doi: 10.1289/ehp.10260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn BA, Cirillo PM, Christianson RE. Prenatal DDT exposure and testicular cancer: a nested case-control study. Arch Environ Occup Health. 2010;65(3):127–134. doi: 10.1080/19338241003730887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis D, Cooper R, Terrera GM, Hardy R, Richards M, Kuh D. Verbal memory and search speed in early midlife are associated with mortality over 25 years' follow-up, independently of health status and early life factors: a British birth cohort study. Int J Epidemiol dyw100. 2016;45(4):1216–1225. doi: 10.1093/ije/dyw100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deary IJ, Weiss A, Batty GD. Intelligence and personality as predictors of Illness and death: how researchers in differential psychology and chronic disease epidemiology are collaborating to understand and address health inequalities. Psychol Sci Public Interest. 2010;11(2):53–79. doi: 10.1177/1529100610387081. [DOI] [PubMed] [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn LM, Dunn LM. Peabody Picture Vocabulary Test. American Guidance Service; Minnesota: 1959. [Google Scholar]
- Freese J, Lutfey K. Handbook of the Sociology of Health, Illness, and Healing. Springer; New York: 2011. Fundamental causality: challenges of an animating concept for medical sociology; pp. 67–81. [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. Am J public health. 2006 May;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottfredson LS. Intelligence: is it the epidemiologists' elusive “fundamental cause” of social class inequalities in health? J Pers Soc Psychol. 2004;86(1):174–199. doi: 10.1037/0022-3514.86.1.174. [DOI] [PubMed] [Google Scholar]
- Haas S. Trajectories of functional health: the 'long arm' of childhood health and socioeconomic factors. Soc Sci Med. 2008;66(4):849–861. doi: 10.1016/j.socscimed.2007.11.004. [DOI] [PubMed] [Google Scholar]
- Haas SA, Krueger PM, Rohlfsen L. Race/ethnic and nativity disparities in later life physical performance: the role of health and socioeconomic status over the life course. J Gerontol Ser B Psychol Sci Soc Sci. 2012;67(2):238–248. doi: 10.1093/geronb/gbr155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatch SL. Conceptualizing and identifying cumulative adversity and protective resources: implications for understanding health inequalities. J Gerontol B Psychol Sci Soc Sci. 2005;60(Spec2):S130–S134. doi: 10.1093/geronb/60.special_issue_2.s130. [DOI] [PubMed] [Google Scholar]
- Hayward MD, Gorman BK. The long arm of childhood: the influence of early-life social conditions on men's mortality. Demography. 2004;41(1):87–107. doi: 10.1353/dem.2004.0005. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- Janevic T, Kahn LG, Landsbergis P, et al. Effects of work and life stress on semen quality. Fertil Steril. 2014;102(2):530–538. doi: 10.1016/j.fertnstert.2014.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuh D, Pierce M, Adams J, et al. Cohort profile: updating the cohort profile for the MRC National Survey of Health and Development: a new clinic-based data collection for ageing research. Int J Epidemiol. 2011 Feb;40(1):e1–e9. doi: 10.1093/ije/dyq231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuh D, Cooper R, Hardy R, Richards M, Ben-Shlomo Y. A Life Course Approach to Healthy Ageing. Oxford University Press; Oxford, United Kingdom: 2014. [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav Spec No. 1995:80–94. [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of health inequalities. Handbook of Medical Sociology. 2010;6:3–17. [Google Scholar]
- Link BG, Phelan JC, Miech R, Westin EL. The resources that matter: fundamental social causes of health disparities and the challenge of intelligence. J Health Soc Behav. 2008 Mar 1;49(1):72–91. doi: 10.1177/002214650804900106. [DOI] [PubMed] [Google Scholar]
- Luo Y, Waite LJ. The impact of childhood and adult SES on physical, mental, and cognitive well- being in later life. J Gerontol B Psychol Sci Soc Sci. 2005;60(2):S93–S101. doi: 10.1093/geronb/60.2.s93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenbach JP, Kulhánová I, Bopp M, Deboosere P, Eikemo TA, Hoffmann R, et al. Variations in the relation between education and cause-specific mortality in 19 European populations: a test of the “fundamental causes” theory of social inequalities in health. Soc Sci Med. 2015;127:51–62. doi: 10.1016/j.socscimed.2014.05.021. [DOI] [PubMed] [Google Scholar]
- Mirowsky J. Handbook of the Sociology of Mental Health. Springer; Netherlands: 2013. Analyzing associations between mental health and social circumstances; pp. 143–165. [Google Scholar]
- Mirowsky J, Ross CE. Education, Social Status, and Health. Transaction Publishers; 2003. [Google Scholar]
- National Health and Nutrition Examination Survey (NHANES) [Accessed Feb. 17, 2016]; http://www.cdc.gov/nchs/nhanes.htm.
- Padyab M, Norberg M. Socioeconomic inequalities and body mass index in Vasterbotten County, Sweden: a longitudinal study of life course influences over two decades. Int J Equity Health. 2014;13:35. doi: 10.1186/1475-9276-13-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palloni A. Reproducing inequalities: luck, wallets, and the enduring effects of childhood health. Demography. 2006;43(4):587–615. doi: 10.1353/dem.2006.0036. [DOI] [PubMed] [Google Scholar]
- Pavalko EK, Caputo J. Social inequality and health across the life course. Am Behav Sci. 2013;57(8):1040–1056. 0002764213487344. [Google Scholar]
- Pearlin LI, Schieman S, Fazio EM, Meersman SC. Stress, health, and the life course: some conceptual perspectives. J Health Soc Behav. 2005;46(2):205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol. 2015 Aug 14;41:311–330. [Google Scholar]
- Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;(Suppl):S28–S40. 51. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Power C, Elliott J. Cohort profile: 1958 british birth cohort (national child development study) Int J Epidemiol. 2006;35(1):34–41. doi: 10.1093/ije/dyi183. [DOI] [PubMed] [Google Scholar]
- Rothman KJ. Epidemiology: an Introduction. Oxford University Press; 2012. [Google Scholar]
- Salomon JA, Nordhagen S, Oza S, Murray CJ. Are Americans feeling less healthy? The puzzle of trends in self-rated health. Am J Epidemiol. 2009;170(3):343–351. doi: 10.1093/aje/kwp144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salsberry PJ, Reagan PB, Fang MZ. Disparities in Women's health across a generation: a mother–daughter comparison. J Women's Health. 2013;22(7):617–624. doi: 10.1089/jwh.2012.4143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seeman TE, Crimmins E, Huang MH, Singer B, Bucur A, Gruenewald T, Berkman LF, Reuben DB. Cumulative biological risk and socioeconomic differences in mortality: MacArthur studies of successful aging. Soc Sci Med. 2004 May 31;58(10):1985–1997. doi: 10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- Sharkey P, Faber JW. Where, when, why, and for whom do residential contexts matter? Moving away from the dichotomous understanding of neighborhood effects. Annu Rev Sociol. 2014 Jul 30;40:559–579. [Google Scholar]
- Susser E, Buka S, Schaefer C, et al. The early determinants of adult health study. J Dev Orig Health Dis. 2011;2(6):311–321. doi: 10.1017/S2040174411000663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry MB, Schaefer CA, Flom JD, et al. Prenatal smoke exposure and mammographic density in mid-life. J Dev Orig Health Dis. 2011;2(6):340–352. doi: 10.1017/S2040174411000614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson D, Williams K, Thomas PA, Liu H, Thomeer MB. Race, gender, and chains of disadvantage: childhood adversity, social relationships, and health. J Health Soc Behav. 2014;55(1):20–38. doi: 10.1177/0022146514521426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Berg BJ, Christianson RE, Oechsli FW. The California child health and development studies of the school of public health, University of California at berkeley. Paediatr Perinat Epidemiol. 1988;2(3):265–282. doi: 10.1111/j.1365-3016.1988.tb00218.x. [DOI] [PubMed] [Google Scholar]
- Weber M. Economy and Society: an Outline of Interpretive Sociology. Univ of California Press; 1978. [Google Scholar]
- Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public health Rep. 2001;116(5):404. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Sternthal M. Understanding racial-ethnic disparities in health sociological contributions. J Health Soc Behav. 2010;51(1 Suppl l):S15–S27. doi: 10.1177/0022146510383838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H, Yang Y, Land KC. Variance function regression in hierarchical age-period-cohort models applications to the study of self-reported health. Am Sociol Rev. 2011;76(6):955–983. doi: 10.1177/0003122411430940. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.