Abstract
Context
Hypotension is one of the dose limiting side effects of benzodiazepines (BZDs), in particular of diazepam (DZP) which is still widely used in the clinic. Currently, only one FDA approved antidote exists for BZD overdose and novel approaches are needed to improve management of DZP overdose, dependency and withdrawal.
Objective
Here, we hypothesized that increasing bioactive lipid mediators termed epoxy fatty acids (EpFAs) will prevent hypotension, as was shown previously in a murine model of LPS-induced hypotension. Therefore, we first characterized the time and dose dependent profile of DZP induced hypotension in mice, and then investigated the reversal of the hypotensive effect by inhibiting the soluble epoxide hydrolase (sEH), an enzyme that regulates the levels of EpFAs.
Materials and methods
Following baseline systolic BP recording using tail cuffs, mice were administered a sEH inhibitor (TPPU) before DZP and BP was monitored. Blood and brain levels of DZP and TPPU were quantified to examine distribution and metabolism. Plasma EpFAs levels were quantified to determine TPPU target engagement.
Results
In this murine model, DZP induced dose dependent hypotension which was more severe than midazolam. The temporal profile was consistent with the reported pharmacokinetics/pharmacodynamics of DZP. Treatment with TPPU reversed the hypotension resulting from high doses of DZP and decreased the sEH metabolites of EpFAs in the plasma demonstrating target engagement.
Discussion and conclusion
Overall, these findings demonstrate the similarity of a murine model of DZP induced hypotension to clinical observations in humans. Furthermore, we demonstrate that stabilization of EpFAs by inhibiting sEH is a novel approach to overcome DZP-induced hypotension and this beneficial effect can be enhanced by an omega three diet probably acting through epoxide metabolites of the fatty acids.
Keywords: Soluble epoxide hydrolase inhibitors, DZP, midazolam, hypotension, EETs, DHETs
Introduction
Benzodiazepines (BZDs) are the most frequently prescribed psychoactive agents that are used to treat a number of conditions including anxiety, insomnia, seizures and alcohol dependence [1, 2]. They are among the drugs of first choice for several epileptic conditions because of their rapid onset of activity, high efficacy and favorable risk to benefit ratio. BZDs are allosteric modulators of the GABAA chloride channel complex (gamma aminobutyric acid), which increase the affinity of this receptor channel to the neurotransmitter GABA [1]. The BZD binding site of the GABA channel is a well exploited target with a number of registered BZD drugs, which have different potencies and toxicities.
Although BZDs have been extremely useful in the treatment of major diseases, the dose limiting adverse effects such as dependence, tolerance, hypotension, and loss of consciousness leave room for improvement on the current standard of care of BZDs [3, 4]. Occasionally, BZDs are used in relatively high doses such as antidotes for pesticide or nerve gas poisoning or following overdose. Thus, an antidote for BZDs becomes necessary to prevent lethality [5, 6]. In contrast to the availability of multiple BZD drugs the only FDA approved antidote for an overdose of BZDs is flumazenil. Flumazenil competitively inhibits ligand binding at the BZD binding site inside the GABAA channel [7]. Expectedly, use of flumazenil may predispose patients to increased sensitivity to seizures or necessitate resedation [8, 9].
A rapid and significant decrease in BP is one of the most pronounced side effects of BZDs such as diazepam (DZP). The mechanism of the hypotensive effect of BZDs is largely unknown. While some studies suggest that BZDs have a vasodilatory effect, which may involve binding to GABA receptors, others suggest that BZDs affect peripheral vascular resistance through a decrease in muscle sympathetic nerve activity [10]. This hypotensive effect requires close monitoring and intervention since it could lead to fainting, decreased blood oxygen levels and reduced availability of oxygen to the brain. Because flumazenil use has limitations, an alternative approach to safely treat this overdose related toxicity could be positive modulation of BP. Agents that can be co-administered with BZDs without affecting their potency and pharmacokinetics while reducing fatal hypotension could be tremendously useful in the treatment of cases of overdose and make the BZDs safer for susceptible patient populations such as elderly people and patients with cardiovascular disease already taking anti-hypertensives. Soluble epoxide hydrolase inhibitors (sEHIs) are known to modulate BP. The sEH is a α/β hydrolase fold enzyme that metabolizes a biologically important group of endogenous lipid mediators, namely epoxy fatty acids (EpFAs). These EpFAs have numerous physiological roles such as regulation of vascular resistance and blood flow [11, 12, 13, 14], and depending on the context either raise or lower blood pressure (BP)[14, 15, 16]. In addition to BP regulating effects, the modest anticonvulsant effects of sEH inhibitors seem to depend on or be related to GABAergic signaling [17]. Systemic inhibition of sEH or intracerebroventricular (i.c.v.) administration of EpFAs, specifically those derived from arachidonic acid selectively delay the onset of GABA antagonist induced but not other types of seizures [17]. Therefore, taking advantage of these properties of the EpFAs and sEHIs we asked if DZP induced hypotension could be prevented by inhibiting sEH. We also demonstrate that this murine model is suitable to examine new agents that block hypotension induced by BZDs.
Materials and Methods
Animals and treatments
All animal protocols were approved by the University of California Davis Animal Use and Care Committee, and experiments were carried out in compliance with the National Institutes of Health Guide for the use and care of laboratory animals. Upon arrival to the vivarium, 7 week old mice (Swiss Webster mice, Charles River Laboratories, Wilmington, MA) were acclimated to their new housing environment for one week and kept under a 12 hour light/dark cycle with free access to food and water.
DZP (5 mg/mL, Hospira, Inc., Lake Forest, IL) was dissolved in 40% propylene glycol, 10 % ethanol and saline. TPPU (1-trifluoromethoxyphenyl-3-(1-propionylpiperidin-4-yl) urea) was synthesized [18], purified and characterized in-house (a kind gift of Dr Sing Lee from UC Davis) and was dissolved in PEG400 to obtain a clear solution. Mice were injected (i.p.) either with DZP alone at 1, 3 or 10 mg/kg or in combination with TPPU at 3 mg/kg i.p. one hour before administration of DZP at the doses indicated. Midazolam (Hospira, Inc., Lake Forest, IL) was administered at 1.8 and 10 mg/kg doses by intramuscular route using saline as vehicle. Animals that served as controls were given the corresponding vehicle solutions, PEG400 for TPPU or 40% propylene glycol, 10% ethanol in saline for DZP and saline for midazolam injections.
BP measurements
Systolic BP (SBP) was measured using a tail cuff volume pressure recording system (8-channel CODA, Kent Scientific, CT) with minor modifications. In our study we selected the tail cuff method instead of direct measurements for BP for several key reasons. Direct measurement methods require either surgery or sedation of the animals which could interfere with the effect of DZP and lead to misinterpretation of the data. Surgical implantation of telemetry probes often cause inflammation which may interfere with the study. Since we are interested in quantification of anti-inflammatory EpFAs, an increase in inflammatory markers such as prostaglandins would potentially affect our results after DZP administration. Moreover, we performed acute treatments and measurements which do not require long term monitoring of BP. Collection of heart rate data was initially not considered as one of the parameters mainly because DZP is known not to influence it[10].
Briefly, restrained animals were maintained on warm heating pads. During the measurements a cloth was placed on the restrainers to maintain heat and to provide a calm environment for the mice. A baseline measurement of 20 cycles was recorded for each animal before any treatment is given. After obtaining a baseline, animals were injected with either PEG400 or TPPU and SBP was measured for another 20 cycles to obtain the change in BP post-PEG400 or TPPU. One hour after administration of PEG400 or TPPU, DZP was administered and changes in BP were monitored for one hour or 120 cycles. In other experiments SBP was monitored for extended durations by placing the mice into the tail cuff and recording a 20 min period at the beginning of every hour or for the durations indicated in the figure legends.
DZP quantification in tissue and plasma
DZP was quantified in plasma and brain samples by LC/MS analysis, which was performed with a Waters Acquity UPLC (Waters, NY, USA) and TSQ Quantum Access Max mass spectrometer (MS) (Thermo Fisher Scientific™, Waltham, MA, USA). Sample preparation and LC/MS conditions are detailed in the supplementary data and Figure S1.
Quantification of EpFAs and TPPU
Bioactive lipid mediators also known as oxylipins or TPPU (see LC/MS chromatogram on Figure S2) from treated animals were extracted from plasma using solid phase extraction and quantified using the QTRAP4000 LC/MS/MS system as described previously [19] with a minor modification, which included a shorter acquisition time to focus on only the most relevant EpFAs and their diol metabolites (26 analytes).
Statistical analysis
All data are reported as mean ± standard error of the mean. To determine differences in BP among the groups repeated measures one-way ANOVA was performed, followed by pairwise comparisons using a post hoc test (i.e. Bonferroni), all of which were performed on Graph Pad Prism software. P values less than 0.05 were considered statistically significant.
Results
Characterization of the murine model of DZP induced hypotension
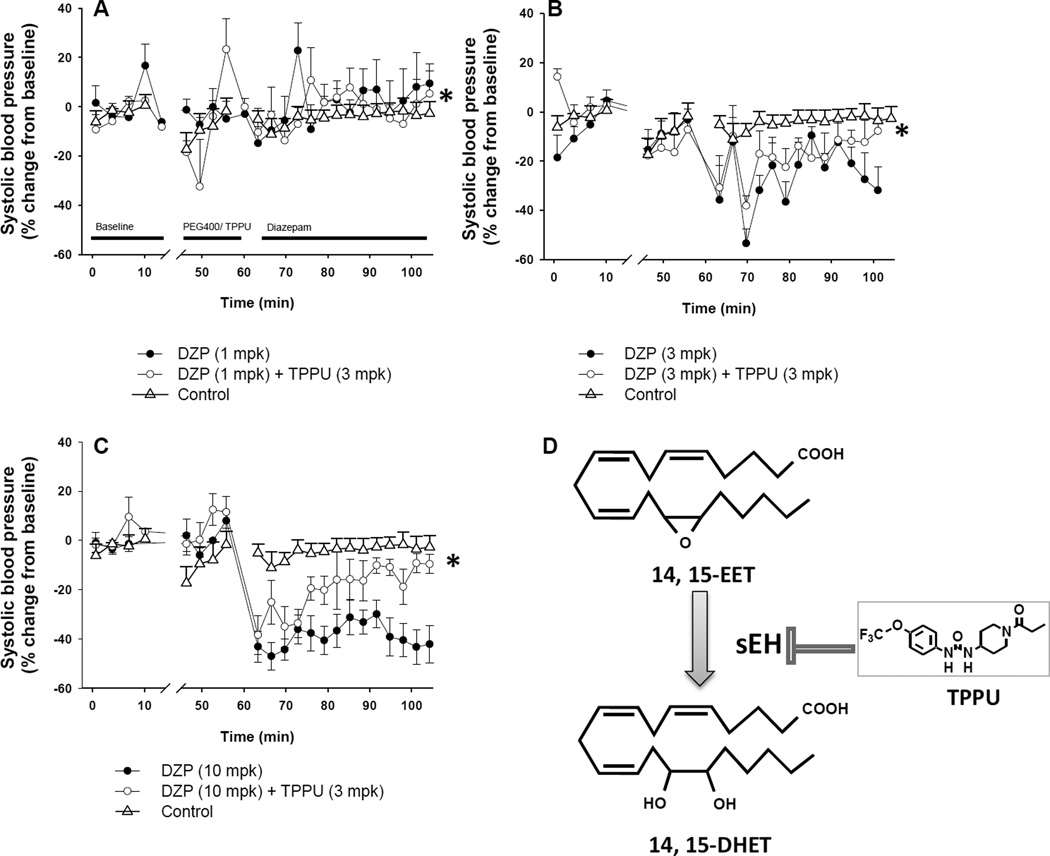
To determine if BZDs have a hypotensive effect on mice, we tested multiple doses of DZP and midazolam using NIH Swiss mice (Figs. 1–3). DZP treatment led to hypotension in mice in a dose dependent manner (Figure 1 A–C). Repeated measures one-way ANOVA revealed an overall significant blood pressure lowering effect (F = 30, P < 0.01) with significant differences among those treated with different doses of DZP (P < 0.01) except for DZP 10 mg/kg versus DZP 3 mg/kg (P > 0.05).
Figure 1.
DZP induced hypotension is dose dependent and reversible by TPPU. Dose dependent effects of DZP on blood pressure are displayed for A. 1 mg/kg, B. 3 mg/kg and C. 10 mg/kg doses. Upon obtaining baseline BP (data before the break on the x-axis), mice were administered TPPU (i.p., 3 mg/kg) or vehicle (PEG400) 1 h before injection of DZP at varying dosages. Post-PEG400 or TPPU blood pressure was recorded for 2023 cycles (between 45–60 min). Then, DZP was administered and BP was recorded following 5 min after DZP injections. Timeline of the experiment is illustrated on panel A. Data are mean ± SEM. n=6 /group. D. Lipid epoxides such as EETs are endogenous chemical mediators known to return high blood pressure to normotensive levels. EETs are rapidly converted to DHETs by soluble epoxide hydrolase (sEH). This degradation is blocked by TPPU.
Figure 3.
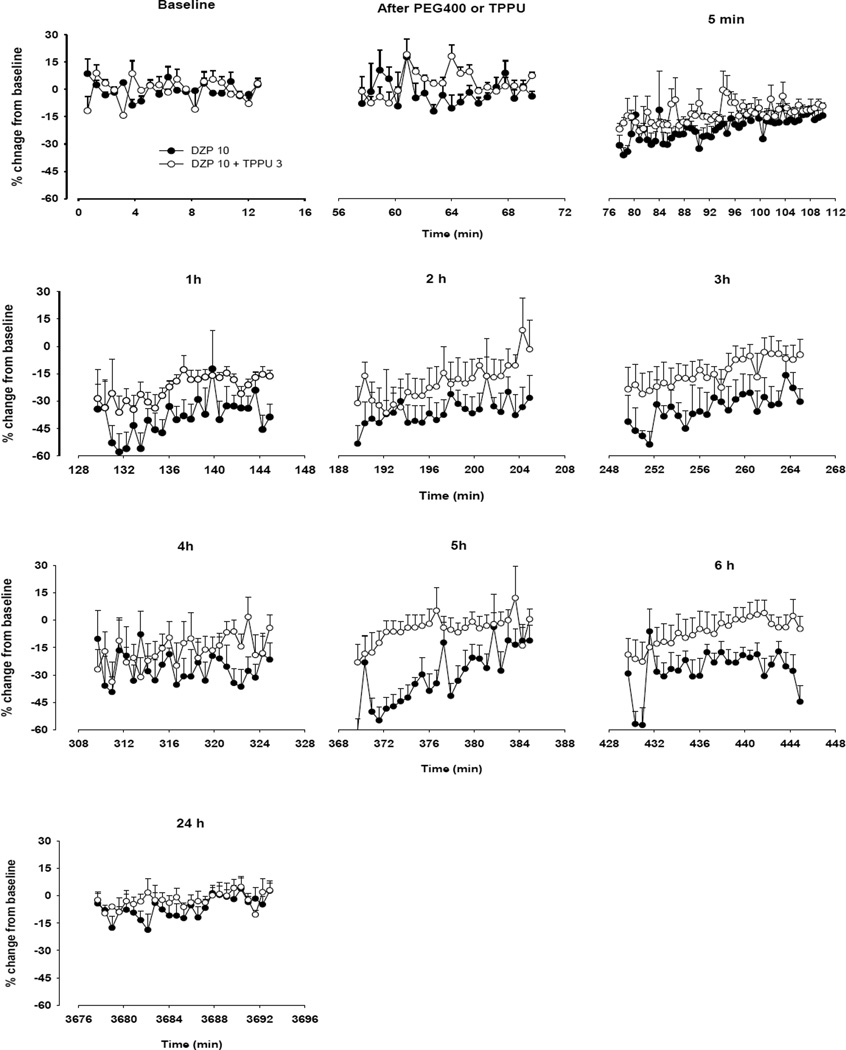
Time dependent effects of DZP at 10 mg/kg dose with or without TPPU on blood pressure (n=6 per group). Upon obtaining baseline BP, mice were administered TPPU (i.p., 3 mg/kg) 1 h before injection of DZP at varying dosages. Blood pressure was recorded at baseline, at 45 min after TPPU or PEG400 administration, at 5 min after DZP (10 mg/kg) and then at 1, 2, 3, 4, 5, 6 and 24 h. Data are mean ± SEM. n=6 /group.
Following an acclimation period, 15 min of BP recordings prior to any treatment were assigned as the baseline for each animal. The average baseline SBP was 113 ± 2 (mean ± SEM, n= 48 mice) throughout the study. In parallel to observations in patients, all doses of DZP treatment led to a decrease in BP, with the lowest dose displaying a shorter duration of effect. At the higher doses of 3 and 10 mg/kg animals experienced a more prominent and sudden drop in BP within 5 min after administration of DZP (Figure 1B and C) and the hypotensive effect lasted significantly longer. For several individual DZP treated mice the SBP was at or under the limit of detection (60 mmHg) of the tail cuff volume-pressure recording system and these were recorded as 60 mmHg and are included in the data set. At the 3 mg/kg DZP dose several periods of more intense hypotension were consistently observed, while at the 10 mg/kg dose the BP was reduced maximally and remained low throughout the rest of the 90 min recording period. Overall, hypotension induced by 3 and 10 mg/kg of DZP lowered SBP by approximately half of the baseline with a longer recovery period, while 1 mg/kg of DZP led to 10–20% decrease from baseline with a 10 min recovery time.
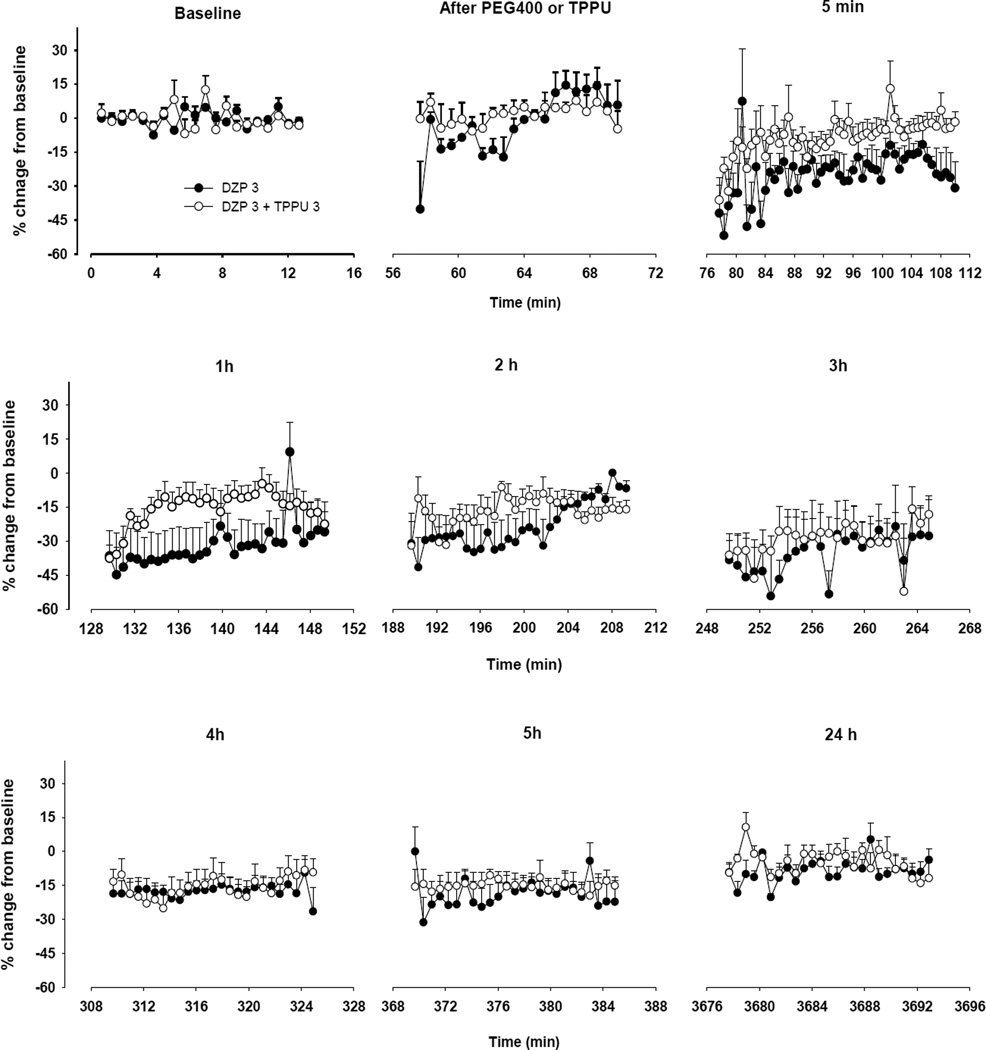
To further understand the duration of DZP induced hypotension mice treated with the 3 and 10 mg/kg DZP and were intermittently monitored over a period of 24 h (Figure 2 and 3). At 5 and 6 h post DZP, BP was still below baseline in mice treated with 3 and 10 mg/kg DZP and there was full recovery at 24 h post treatment. In addition to the first 100 min after DZP (Figure 1), we performed another repeated measures one-way ANOVA that included data collected on all time points from baseline to 24 hours. This analysis revealed a significant difference among the treatment groups (F= 140.7, P < 0.01). Pairwise comparisons showed a significant difference between DZP 10 mg/kg versus DZP 3 mg/kg and between animals treated with DZP versus DZP+TPPU within each DZP dose group (P < 0.01).
Figure 2.
DZP induced hypotension lasts for at least 6h. Time dependent effects of DZP at 3 mg/kg dose with or without TPPU on blood pressure (n=6 per group). Upon obtaining baseline BP, mice were administered TPPU (i.p., 3 mg/kg) 1 h before injection of DZP. Blood pressure was recorded at baseline, 45 min after TPPU or PEG400 administration, at 5 min after DZP (3 mg.kg) and then at 1, 2, 3, 4, 5 and 24 h. Data are mean ± SEM. n=6 /group.
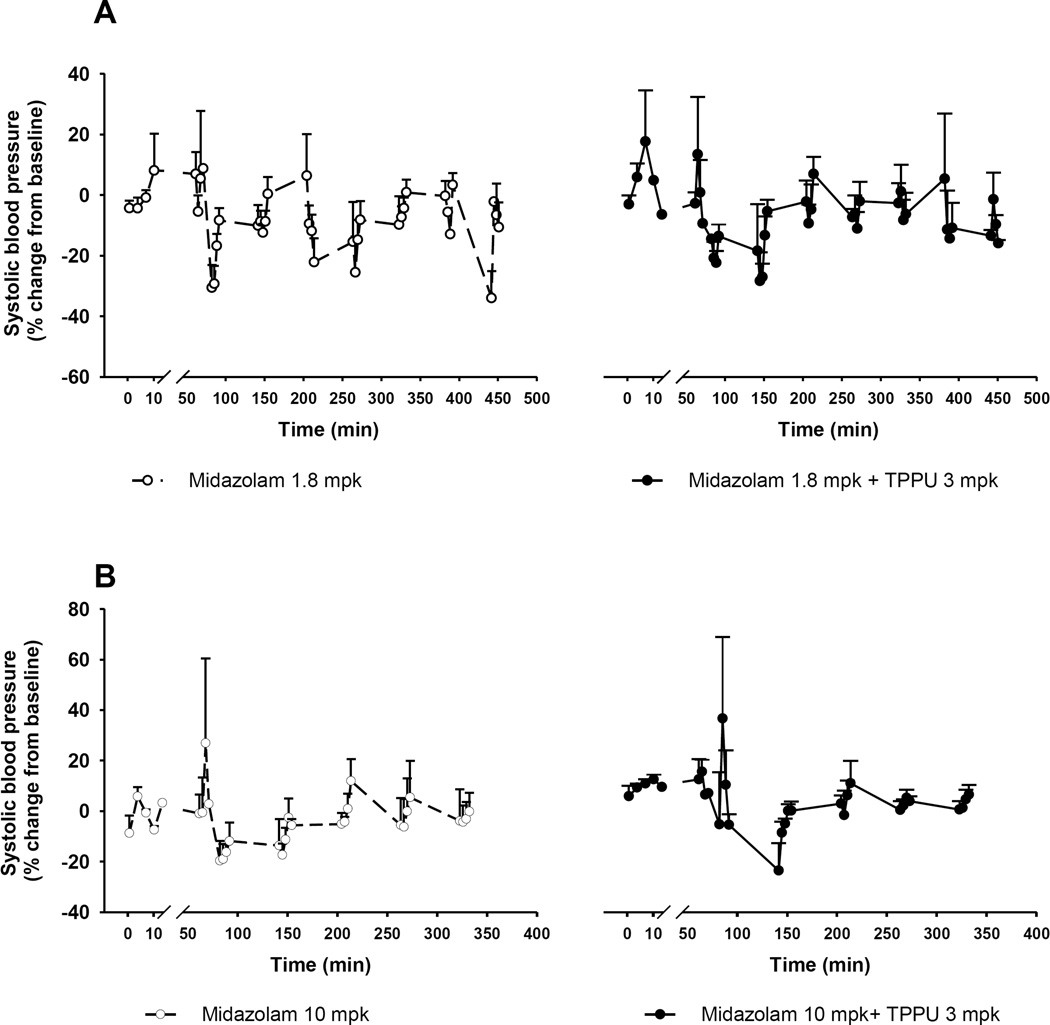
To validate the utility of the model we tested another BZD, midazolam (Figure 4). Two doses of midazolam were selected. The first dose was 1.8 mg/kg midazolam (Figure 4A) in mice which is roughly equivalent to the human dose at 1 mg/kg [20]. The second dose was 10-fold higher than the human equivalent dose (Figure 4B). Midazolam led to significant changes in BP at both doses (P < 0.01, Figure 4). The recovery from midazolam occurred between 1–2 h after midazolam was administered, suggesting a faster recovery than following DZP, which is consistent with the shorter half life of midazolam as compared to DZP.
Figure 4.
Change in blood pressure in animals treated with midazolam. Upon obtaining baseline BP, mice were administered TPPU (i.p., 3 mg/kg) 1 h before injection of midazolam at 1.8 and 10 mg/kg. Blood pressure was recorded at baseline, at 45 min after TPPU or PEG400 administration, at 5 min after midazolam and then at 1, 2, 3, 4 h. ‘ ‘ symbol indicates start of TPPU or vehicle (PEG400) treatment, ‘
‘ symbol indicates start of TPPU or vehicle (PEG400) treatment, ‘ ’ symbol indicates start of DZP or vehicle (40% propylene glycol, 10% alcohol) treatment. Data are mean ± SEM. n=6 /group.
’ symbol indicates start of DZP or vehicle (40% propylene glycol, 10% alcohol) treatment. Data are mean ± SEM. n=6 /group.
Inhibition of sEH reverses the hypotensive effect of DZP
To test if inhibition of sEH will normalize BP, we first investigated the effect of the vehicles used to formulate DZP and TPPU. These vehicle treatments by themselves did not lead to significant changes in BP (Supplementary data, Figure S3). TPPU alone or when administered together with the DZP vehicle under physiologic conditions (i.e., without DZP) did not elicit any significant changes (P =0.56, Fig, S3). These data reiterate the proposed homeostatic role of EpFAs and sEH inhibitors in the absence of an underlying pathological condition [14, 15].
A high dose of TPPU (3 mg/kg) was administered 45 min prior to all three doses of DZP treated animals and BP was recorded for an hour. At the lowest dose (1 mg/kg), DZP showed a slight hypotensive effect (Figure 1A, P = 0.3, as compared to baseline BP) and accordingly TPPU was the least effective in these mice. TPPU did not prevent the sudden drop in BP 5 min after administration of DZP at higher doses (3 and 10 mg/kg DZP). However, animals treated with TPPU recovered significantly faster from hypotension compared to those treated with DZP alone (Figure 1, P < 0.001). This reversal of SBP with TPPU treatment was maximal at about 30 min after administration of DZP. In addition, when we evaluated the area under the curve (AUC) of the BP-time course, we found that the AUC for the BP in the DZP plus TPPU treatment group was significantly higher than the AUC in the group treated with DZP alone (P < 0.05, Figure S4). These data suggest that TPPU is indeed effective in normalizing BP at higher doses of DZP.
Treatment with Midazolam also resulted in significant changes in BP in the repeated measures ANOVA analysis (F = 71.9, P < 0.01). While administration of midazolam led to significant hypotension at both doses (P < 0.05), TPPU was effective only when administered with the low dose of midazolam (P = 0.004 for midazolam 1.8 mg/kg versus midazolam 1.8 mg/kg + TPPU) (Figure 4).
Tissue and plasma levels of DZP and TPPU
Next we quantified plasma and brain levels of both compounds (Table 1). For DZP at the highest dose, an immediate and a delayed time point of 5 and 60 min were selected. For the TPPU receiving groups, these same time points corresponded to 50 and 105 min post administration of TPPU. The brain levels of DZP were significantly higher than plasma at both time points (P < 0.05) with a brain-to-plasma ratio of 3.5 ± 0.3 (mean ± SEM, n= 24), which is in line with previous reports [21, 22]. Consistent with previous reports[21], both tissue and plasma levels of DZP decreased at least 3 fold at 1 h after dosing. TPPU co-administration did not change plasma and brain levels of DZP. In addition, tissue and plasma levels of TPPU were at least 10 times higher than the IC50 for murine sEH (IC50: 2 nM [18]), suggesting a near complete inhibition of sEH. We observed three times higher levels of TPPU in the brain than in the plasma at both time points, which is consistent with effective penetration through the blood-brain barrier.
Table 1.
Tissue and plasma levels of TPPU and DZP in mice
| [TPPU] (µM) | ||
| Time after TPPU administration | Brain | Plasma |
| 50 min (5 min after DZP) | 32.8 ± 3.4 | 11.8 ± 0.6 |
| 105 min (1 h after DZP) | 27.8 ± 2 | 10 ± 0.3 |
| Time after DZP administration | [DZP] (µM) | |
| Brain | Plasma | |
| 5 min- DZP 10 mpk | 15 ± 3 | 3 ± 0.8 |
| 5 min- DZP 10 mpk+TPPU | 15 ± 3 | 7 ± 2 |
| 1 h- DZP 10 mpk | 1 ± 0.1 | 0.4 ± 0.05 |
| 1h- DZP 10 mpk + TPPU | 1 ± 0.1 | 0.4 ± 0.03 |
TTPU treatment with or without DZP modulates the plasma biomarkers of sEH inhibition
Treatment with TPPU at a 3 mg/kg dose should inhibit nearly all enzyme activity [18]. Based on previous work using i.p. or oral administration TPPU has a plasma elimination half-life of > 24 h [18, 23, 24]. Moreover, TPPU was also quantified from saline perfused mouse brain and demonstrated to have significant blood brain barrier penetration [17], in keeping with what we are finding in this study (Table 1). We therefore expected TPPU to change both plasma and brain levels of the EpFAs and as a surrogate examined plasma levels of the EpFAs and tested if DZP administration following TPPU lead to pharmacokinetic interference between these two compounds.
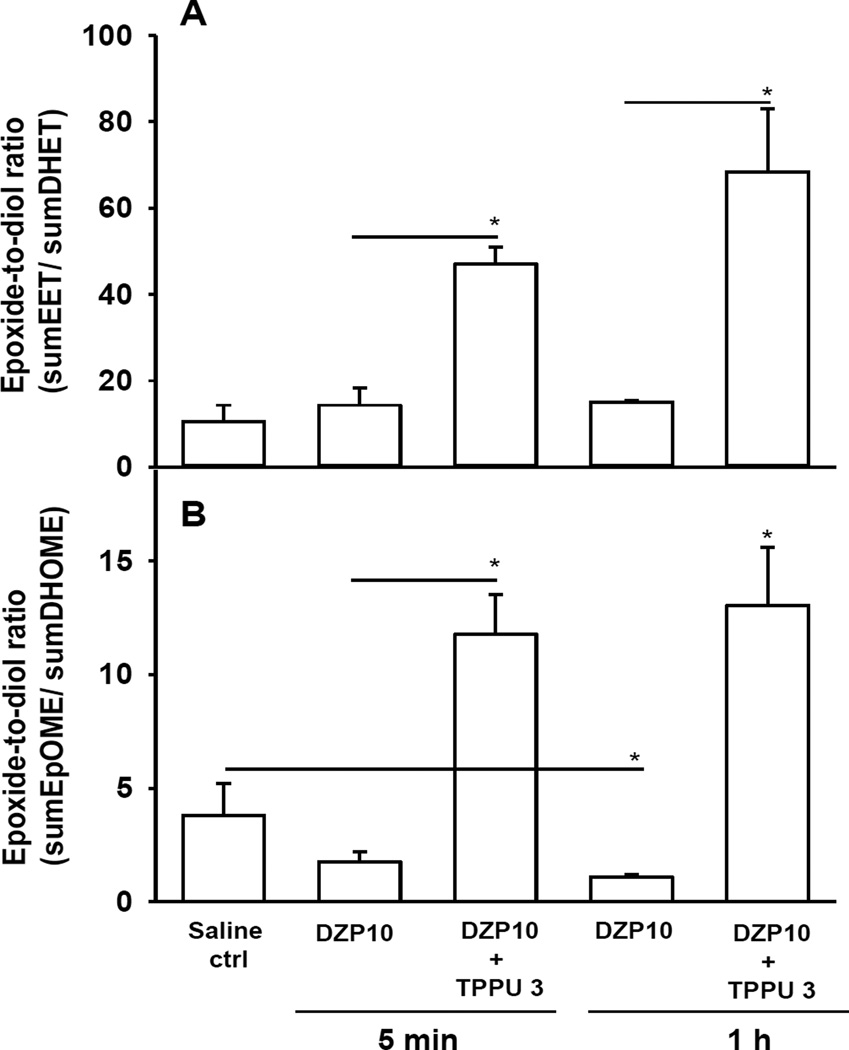
To examine target engagement by TPPU, we quantified the EETs (epoxyeicosatrienoic acid) and EpOMEs (epoxyoctadecenoic acid) from plasma. These cytochrome P450 enzyme generated bioactive lipids are highly responsive to sEH inhibition. DZP alone after 5 min did not elicit any significant changes in the levels of biomarker EpFAs, when compared to vehicle controls (P > 0.05). The EETs and EpOMEs are substrates of the sEH enzyme and are metabolized to DHETs and DiHOMEs by the sEH activity. The plasma and tissue levels of EpFAs are usually in the low nM range and in vivo their half-life is in the order of several seconds because of the sEH activity, although in vitro they are fairly stable [25, 26]. Therefore the ratio of epoxides to diols is used as biomarkers of target engagement in studies with sEH inhibitors [12, 15, 27]. In mice treated with both DZP and TPPU, both the EETs and EpOMEs increased approximately 2–3 fold with significant decreases in their corresponding degradation products the DHETs and DiHOMEs, leading to 7–10 fold higher epoxide to diol ratio at both time points (Figure 5, see Supplementary data, Table S1). In addition to P450 metabolites of arachidonic acid, we observed an increase in some of the cyclooxygenase and lipoxygenase metabolites of arachidonic acid after administration of diazepam, suggesting a trend towards increased inflammation upon DZP administration (Table S2a and S2b).
Figure 5.
Plasma and tissue epoxide-to-diol ratios in animals treated with DZP (10 mg/kg) and TPPU (3 mg/kg) or PEG400. Mice were administered with TPPU (i.p., 3 mg/kg) 1 h before injection of DZP. Samples were quantified by LC/MS/MS for the levels of ARA and LA epoxides and diols. Sum of EETs and DHETs include 8, 9-, 11, 12- and 14, 15- regioisomers (Panel A). Sum of EpOME and DiHOME include 9, 10- and 11, 12- regioisomers (Panel B). Data are mean ± SEM. n=6 /group. Asterisk indicates a statistically significant difference between PEG vs TPPU at 1 h time point.
Discussion
We established a murine model to study the hypotensive effects of DZP and midazolam and to test whether this adverse effect could be reversed by sEH inhibition. Our findings on BZD induced hypotension are consistent with reports from patients, although the murine model seems less sensitive to the hypotensive effects of DZP. However, this method provides a rapid and sufficiently stringent approach to investigate anti-hypotensive compounds. The main finding of this study is that sEH inhibition leads to a faster recovery from the hypotensive effect of DZP.
The BZD drugs have a range of potencies and toxicities based on their affinity to the GABA channel subtypes and pharmacokinetic properties including, onset and duration of action, rate of absorption and presence of active metabolites. Due to their euphoric effects, they are also drugs of abuse. The estimated number of emergency room visits in the US, involving nonmedical use of BZDs was reported to be about 270,000 in 2008 [28]. However, current options for management of BZD overdose are limited. Flumazenil is a selective BZD antagonist and therefore the drug of choice in BZD overdose [29]; however, it was reported to cause seizures, resedation and cardiac arrhythmias, in some cases within minutes of its administration [30, 31]. Additionally, it has a short half-life and requires repetitive dosings to obtain the desired effect. Therefore, its use is limited. Naloxone is also used in BZD overdose even though it is an opioid antagonist [32]. While other vasoactive substances (catecholamine, phosphodiesterase inhibitors, etc.) are available to treat hypotension in shock, cardiac arrest or calcium channel blocker toxicity [33, 34], these are not the first line of choice in the treatment of BZD overdose. Therefore, novel approaches are needed to target hypotension associated with BZDs.
Dose dependent effects of treatments with BZDs
In our study, DZP caused a dose dependent decrease in BP (Figure 1), which is consistent with previous studies[35]. Hypotension induced by both doses of DZP lasted well beyond the short plasma elimination or brain disappearance half life of DZP, which is reported to be about 8 min each following i.v. administration in mice[21]. In contrast, the two major bioactive metabolites of DZP, desmethyl DZP and oxazepam have a brain disappearance half-life of approximately 3 h following 2.85 mg/kg DZP administration, and oxazepam given alone has a brain disappearance half life of up to 5 h. Midazolam induced hypotension is rarely encountered at clinically used doses but it may elicit hypotension at high doses or when administered with opioids [36]. Data here are consistent with the characteristics of midazolam.
Effect of TPPU on BZD induced hypotension
While pretreatment with a sEH inhibitor did not cause an immediate effect on normalizing BP after DZP injection, the time to recovery from the hypotensive effect of DZP was significantly shortened. Supporting this observation, at later time points we still obtained statistically significant differences in BP between mice treated with DZP alone and mice treated with DZP and TPPU (Figure 2 and 3).
The sEH inhibitor used here is CNS permeable [17]. In line with previous findings, in this study TPPU crossed the blood brain barrier with a ~3.5 times higher concentration in the brain than in plasma. While the tissue levels of DZP and TPPU were comparable at early time points, TPPU levels remained high for a longer time. This likely contributed to the faster recovery of animals that were treated with DZP plus TPPU. Most importantly, plasma and brain levels of both DZP and TPPU from mice that received both compounds were nearly identical to those receiving individual compounds at either time point. This observation implies that there was no significant pharmacokinetic interaction between these two agents, a desired property in combinatorial treatments.
The sEH inhibitors seem to normalize BP rather than modulating it in a single direction. Anti-hypotensive and anti-hypertensive effects of sEH inhibitors are well documented in various models [12, 14]. When hypertension is induced by Angiotensin II the sEH inhibitors lower systolic BP, while in models of hypotension induced by systemic LPS elicited sepsis, they elevate BP from less than 40 mmHg (undetectable by tail cuff method) to normal range [14]. Dietary supplementation of ω-3 fatty acids or infusion of one of the EpFA regioisomers, the 19,20-EpDPE with an implanted mini-pump both enhance the efficacy of TPPU supporting the hypothesis that sEH inhibitors stabilize the levels of EpFAs which in turn regulate BP [16, 26, 37]. Reducing the hypotensive side effect of DZP should allow higher doses of BZDs like midazolam and diazepam to be used. In particular, there seems to be no negative functional interaction between GABA agonists and sEH inhibitors. Specifically the anti-convulsant effect of DZP is slightly enhanced by sEH inhibitor co-administration. In addition, sEH inhibitor may positively regulate the synthesis of an unidentified endogenous GABA agonist, possibly a neurosteroid [17]. Given the apparently large therapeutic window of sEH inhibitors and the apparent lack of negative side effects [38, 39, 40] these compounds may find use in reducing the hypertensive side effects is several drug classes. One of the other outcomes associated with the effects of sEH inhibitors on the nervous system is their anti-depressant effects. Although we have not assessed such functional outcomes in our current study, we have reported a strong and relatively quick anti-depressant effect of sEH inhibitors in different murine models of depression, where we observed remarkable increases in the tissue levels of sEH in the brain as compared to control animals [41]. The increase in the brain sEH levels also reflected itself in postmortem brain samples obtained from depressed patients. These results suggested a key role for sEH in the pathogenesis of depression. Future studies are underway to characterize sedative effects of sEH inhibitors.
Conclusions
Overall, our study demonstrates that the sEH inhibitor TPPU does not interfere with the PK of DZP but can be beneficial to treat cases of BZD induced hypotension. The observation that TPPU is most effective at the highest doses of DZP suggests the endogenous substrates, EpFAs are homeostatic molecules. Such EpFAs include P450 metabolites of omega-3 fatty acids suggesting that an omega-3 fatty acid rich diet can potentially enhance the anti-hypotensive effects of TPPU.
Supplementary Material
Acknowledgments
Sources of funding
This work was supported by the NIEHS grant R01 ES002710, NIEHS Superfund Research Program grants P42 ES004699, the CounterAct Program, National Institutes of Health Office of the Director (NIH OD), and the National Institute of Neurological Disorders and Stroke, Grant Number U54 NS079202, NIEHS grant U24 DK097154 and National Institute of Arthritis and Musculoskeletal and Skin Diseases R21AR062866.
We would like to thank Mrs. Louisa Lo for her extensive and thorough administrative assistance and help with manuscript editing.
References
- 1.Mohler H. The rise of a new GABA pharmacology. Neuropharmacology. 2011;60:1042–1049. doi: 10.1016/j.neuropharm.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 2.Greenfield LJ., Jr Molecular mechanisms of antiseizure drug activity at GABAA receptors. Seizure. 2013;22:589–600. doi: 10.1016/j.seizure.2013.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ochoa JG, Kilgo WA. The Role of Benzodiazepines in the Treatment of Epilepsy. Current treatment options in neurology. 2016;18:18. doi: 10.1007/s11940-016-0401-x. [DOI] [PubMed] [Google Scholar]
- 4.Wu W, Zhang L, Xue R. Lorazepam or diazepam for convulsive status epilepticus: A meta-analysis. Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 2016 doi: 10.1016/j.jocn.2015.10.038. [Epub Ahead of Print] [DOI] [PubMed] [Google Scholar]
- 5.Marrs TC. Diazepam in the treatment of organophosphorus ester pesticide poisoning. Toxicological reviews. 2003;22:75–81. doi: 10.2165/00139709-200322020-00002. [DOI] [PubMed] [Google Scholar]
- 6.Bailey AM, Baker SN, Baum RA, Chandler HE, Weant KA. Being prepared: emergency treatment following a nerve agent release. Advanced emergency nursing journal. 2014;36:22–33. doi: 10.1097/TME.0000000000000008. [DOI] [PubMed] [Google Scholar]
- 7.Licata SC, Rowlett JK. Abuse and dependence liability of benzodiazepine-type drugs: GABA(A) receptor modulation and beyond. Pharmacology, biochemistry, and behavior. 2008;90:74–89. doi: 10.1016/j.pbb.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seger DL. Flumazenil--treatment or toxin. Journal of toxicology Clinical toxicology. 2004;42:209–216. doi: 10.1081/clt-120030946. [DOI] [PubMed] [Google Scholar]
- 9.Bartlett D. The coma cocktail: indications, contraindications, adverse effects, proper dose, and proper route. Journal of emergency nursing: JEN : official publication of the Emergency Department Nurses Association. 2004;30:572–574. doi: 10.1016/j.jen.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 10.Kitajima T, Kanbayashi T, Saito Y, Takahashi Y, Ogawa Y, Sugiyama T, Kaneko Y, Aizawa R, Shimizu T. Diazepam reduces both arterial blood pressure and muscle sympathetic nerve activity in human. Neuroscience letters. 2004;355:77–80. doi: 10.1016/j.neulet.2003.10.054. [DOI] [PubMed] [Google Scholar]
- 11.Neckar J, Kopkan L, Huskova Z, Kolar F, Papousek F, Kramer HJ, Hwang SH, Hammock BD, Imig JD, Maly J, Netuka I, Ostadal B, Cervenka L. Inhibition of soluble epoxide hydrolase by cis-4-[4-(3-adamantan-1-ylureido)cyclohexyl-oxy]benzoic acid exhibits antihypertensive and cardioprotective actions in transgenic rats with angiotensin II-dependent hypertension. Clin Sci (Lond) 2012;122:513–525. doi: 10.1042/CS20110622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Imig JD, Zhao X, Zaharis CZ, Olearczyk JJ, Pollock DM, Newman JW, Kim IH, Watanabe T, Hammock BD. An orally active epoxide hydrolase inhibitor lowers blood pressure and provides renal protection in salt-sensitive hypertension. Hypertension. 2005;46:975–981. doi: 10.1161/01.HYP.0000176237.74820.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Loch D, Hoey A, Morisseau C, Hammock BO, Brown L. Prevention of hypertension in DOCA-salt rats by an inhibitor of soluble epoxide hydrolase. Cell Biochem Biophys. 2007;47:87–98. doi: 10.1385/cbb:47:1:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu JY, Qiu H, Morisseau C, Hwang SH, Tsai HJ, Ulu A, Chiamvimonvat N, Hammock BD. Inhibition of soluble epoxide hydrolase contributes to the anti-inflammatory effect of antimicrobial triclocarban in a murine model. Toxicol Appl Pharmacol. 2011;255:200–206. doi: 10.1016/j.taap.2011.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmelzer KR, Kubala L, Newman JW, Kim IH, Eiserich JP, Hammock BD. Soluble epoxide hydrolase is a therapeutic target for acute inflammation. Proc Natl Acad Sci U S A. 2005;102:9772–9777. doi: 10.1073/pnas.0503279102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ulu A, Harris TR, Morisseau C, Miyabe C, Inoue H, Schuster G, Dong H, Iosif AM, Liu JY, Weiss RH, Chiamvimonvat N, Imig JD, Hammock BD. Anti-inflammatory effects of omega-3 polyunsaturated fatty acids and soluble epoxide hydrolase inhibitors in angiotensin-II-dependent hypertension. J Cardiovasc Pharmacol. 2013;62:285–397. doi: 10.1097/FJC.0b013e318298e460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Inceoglu B, Zolkowska D, Yoo HJ, Wagner KM, Yang J, Hackett E, Hwang SH, Lee KS, Rogawski MA, Morisseau C, Hammock BD. Epoxy fatty acids and inhibition of the soluble epoxide hydrolase selectively modulate GABA mediated neurotransmission to delay onset of seizures. PLoS One. 2013;8(12):e80922. doi: 10.1371/journal.pone.0080922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rose TE, Morisseau C, Liu JY, Inceoglu B, Jones PD, Sanborn JR, Hammock BD. 1-Aryl-3-(1-acylpiperidin-4-yl)urea inhibitors of human and murine soluble epoxide hydrolase: structure-activity relationships, pharmacokinetics, and reduction of inflammatory pain. J Med Chem. 2010;53:7067–7075. doi: 10.1021/jm100691c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang J, Schmelzer K, Georgi K, Hammock BD. Quantitative profiling method for oxylipin metabolome by liquid chromatography electrospray ionization tandem mass spectrometry. Anal Chem. 2009;81:8085–8093. doi: 10.1021/ac901282n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reagan-Shaw S, Nihal M, Ahmad N. Dose translation from animal to human studies revisited. FASEB J. 2008;22:659–661. doi: 10.1096/fj.07-9574LSF. [DOI] [PubMed] [Google Scholar]
- 21.Kaur P, Kim K. Pharmacokinetics and brain uptake of diazepam after intravenous and intranasal administration in rats and rabbits. Int J Pharm. 2008;364:27–35. doi: 10.1016/j.ijpharm.2008.07.030. [DOI] [PubMed] [Google Scholar]
- 22.Fenyk-Melody JE, Shen X, Peng Q, Pikounis W, Colwell L, Pivnichny J, Anderson LC, Tamvakopoulos CS. Comparison of the effects of perfusion in determining brain penetration (brain-to-plasma ratios) of small molecules in rats. Comparative medicine. 2004;54:378–381. [PubMed] [Google Scholar]
- 23.Liu JY, Lin YP, Qiu H, Morisseau C, Rose TE, Hwang SH, Chiamvimonvat N, Hammock BD. Substituted phenyl groups improve the pharmacokinetic profile and anti-inflammatory effect of urea-based soluble epoxide hydrolase inhibitors in murine models. Eur J Pharm Sci. 2013;48:619–627. doi: 10.1016/j.ejps.2012.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ulu A, Appt S, Morisseau C, Hwang SH, Jones PD, Rose TE, Dong H, Lango J, Yang J, Tsai HJ, Miyabe C, Fortenbach C, Adams MR, Hammock BD. Pharmacokinetics and in vivo potency of soluble epoxide hydrolase inhibitors in cynomolgus monkeys. Br J Pharmacol. 2012;165:1401–1412. doi: 10.1111/j.1476-5381.2011.01641.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Inceoglu B, Jinks SL, Ulu A, Hegedus CM, Georgi K, Schmelzer KR, Wagner K, Jones PD, Morisseau C, Hammock BD. Soluble epoxide hydrolase and epoxyeicosatrienoic acids modulate two distinct analgesic pathways. Proc Natl Acad Sci U S A. 2008;105:18901–18906. doi: 10.1073/pnas.0809765105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ulu A, Stephen Lee KS, Miyabe C, Yang J, Hammock BG, Dong H, Hammock BD. An omega-3 epoxide of docosahexaenoic acid lowers blood pressure in angiotensin-II-dependent hypertension. J Cardiovasc Pharmacol. 2014;64:87–99. doi: 10.1097/FJC.0000000000000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ulu A, Davis BB, Tsai HJ, Kim IH, Morisseau C, Inceoglu B, Fiehn O, Hammock BD, Weiss RH. Soluble epoxide hydrolase inhibitors reduce the development of atherosclerosis in apolipoprotein e-knockout mouse model. J Cardiovasc Pharmacol. 2008;52:314–323. doi: 10.1097/FJC.0b013e318185fa3c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cai R, Crane E, Poneleit K, Paulozzi L. Emergency department visits involving nonmedical use of selected prescription drugs in the United States, 2004–2008. Journal of pain & palliative care pharmacotherapy. 2010;24:293–297. doi: 10.3109/15360288.2010.503730. [DOI] [PubMed] [Google Scholar]
- 29.Djordjevic S, Jovic-Stosic J, Kilibarda V, Segrt Z, Perkovic-Vukcevic N. Determination of flumazenil in serum by liquid chromatography-mass spectrometry: Application to kinetics study in acute diazepam overdose. Vojnosanitetski pregled. 2016;73:146–151. doi: 10.2298/vsp141222019d. [DOI] [PubMed] [Google Scholar]
- 30.Veiraiah A, Dyas J, Cooper G, Routledge PA, Thompson JP. Flumazenil use in benzodiazepine overdose in the UK: a retrospective survey of NPIS data. Emergency medicine journal : EMJ. 2012;29:565–569. doi: 10.1136/emj.2010.095075. [DOI] [PubMed] [Google Scholar]
- 31.Gerak LR, France CP. Quantitative analyses of antagonism: combinations of midazolam and either flunitrazepam or pregnanolone in rhesus monkeys discriminating midazolam. J Pharmacol Exp Ther. 2012;340:742–749. doi: 10.1124/jpet.111.188250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Galea S, Worthington N, Piper TM, Nandi VV, Curtis M, Rosenthal DM. Provision of naloxone to injection drug users as an overdose prevention strategy: early evidence from a pilot study in New York City. Addictive behaviors. 2006;31:907–912. doi: 10.1016/j.addbeh.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 33.Kanagarajan K, Marraffa JM, Bouchard NC, Krishnan P, Hoffman RS, Stork CM. The use of vasopressin in the setting of recalcitrant hypotension due to calcium channel blocker overdose. Clin Toxicol (Phila) 2007;45:56–59. doi: 10.1080/15563650600795669. [DOI] [PubMed] [Google Scholar]
- 34.Overgaard CB, Dzavik V. Inotropes and vasopressors: review of physiology and clinical use in cardiovascular disease. Circulation. 2008;118:1047–1056. doi: 10.1161/CIRCULATIONAHA.107.728840. [DOI] [PubMed] [Google Scholar]
- 35.de Morais HH, Barbalho JC, de Holanda Vasconcellos RJ, Landim FS, da Costa Araujo FA, de Souza Dias TG. Comparative study of hemodynamic changes caused by diazepam and midazolam during third molar surgery: a randomized controlled trial. Oral and maxillofacial surgery. 2015;19:267–273. doi: 10.1007/s10006-015-0488-3. [DOI] [PubMed] [Google Scholar]
- 36.Frolich MA, Arabshahi A, Katholi C, Prasain J, Barnes S. Hemodynamic characteristics of midazolam, propofol, and dexmedetomidine in healthy volunteers. Journal of clinical anesthesia. 2011;23:218–223. doi: 10.1016/j.jclinane.2010.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang G, Panigrahy D, Mahakian LM, Yang J, Liu JY, Stephen Lee KS, Wettersten HI, Ulu A, Hu X, Tam S, Hwang SH, Ingham ES, Kieran MW, Weiss RH, Ferrara KW, Hammock BD. Epoxy metabolites of docosahexaenoic acid (DHA) inhibit angiogenesis, tumor growth, and metastasis. Proc Natl Acad Sci U S A. 2013;110:6530–6535. doi: 10.1073/pnas.1304321110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Imig JD. Epoxyeicosatrienoic acids, hypertension, and kidney injury. Hypertension. 2015;65:476–482. doi: 10.1161/HYPERTENSIONAHA.114.03585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kodani SD, Hammock BD. The 2014 Bernard B. Brodie award lecture-epoxide hydrolases: drug metabolism to therapeutics for chronic pain. Drug Metab Dispos. 2015;43:788–802. doi: 10.1124/dmd.115.063339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Morisseau C, Hammock BD. Impact of soluble epoxide hydrolase and epoxyeicosanoids on human health. Annu Rev Pharmacol Toxicol. 2013;53:37–58. doi: 10.1146/annurev-pharmtox-011112-140244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ren Q, Ma M, Ishima T, Morisseau C, Yang J, Wagner KM, Zhang JC, Yang C, Yao W, Dong C, Han M, Hammock BD, Hashimoto K. Gene deficiency and pharmacological inhibition of soluble epoxide hydrolase confers resilience to repeated social defeat stress. Proc Natl Acad Sci U S A. 2016;113:E1944–E1952. doi: 10.1073/pnas.1601532113. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.