Abstract
Background
Childhood attention deficit hyperactivity disorder (ADHD) is reported to be more prevalent among socioeconomically disadvantaged groups in various countries. The effect of poverty on child development appears to depend on how long poverty lasts. The timing of poverty also seems to be important for childhood outcomes. Lifetime socioeconomic status may shape current health. Thus, we investigated the effects of household income changes from birth to 4 years on the occurrence of ADHD.
Methods
Data were obtained from 18,029 participants in the Korean National Health Insurance cohort who were born in 2002 and 2003. All individuals were followed until December 2013 or the occurrence of ADHD, whichever came first. Household income trajectories were estimated using the national health insurance premium and the group-based model. Cox proportional hazard models were used to compare incidence rates between different income trajectory groups after adjustment for possible confounding risk factors.
Results
Of 18,029 participants, 554 subjects (3.1%) were identified as having ADHD by age 10 or 11. Seven household income trajectories within three categories were found. Children living in decreasing, consistently low, and consistently mid-low income households had an increased risk of ADHD compared to children who consistently lived in the mid-high household income group.
Conclusions
Children who live in decreasing-income or consistently low-income households have a higher risk for ADHD. Promotion of targeted policies and priority support may help reduce ADHD in this vulnerable group.
Keywords: Socioeconomic status, Attention deficit hyperactivity disorder, Korean newborn infant, Longitudinal study
1. Introduction
Attention deficit hyperactivity disorder (ADHD) manifests in childhood with symptoms of hyperactivity, impulsivity, and/or inattention and is often accompanied by other psychiatric disorders (e.g., mood, anxiety, conduct, or oppositional defiant disorder).1–5 No single risk factor explains the development of ADHD; however, interactions between genetic, social, and environmental factors have been implicated.6 Although the risk factors are still controversial, childhood ADHD is reported to be more prevalent among socioeconomically disadvantaged groups in various regions of developed countries, including the United States, United Kingdom, and others.7–15 Studies have consistently found an association between childhood ADHD/behavioral symptoms of ADHD and socioeconomic disadvantage; ADHD symptoms and diagnosis are more common among those from low socioeconomic status (SES) backgrounds. While most research in this field has focused on concurrent associations of SES and ADHD, lifetime SES may shape current health. To this end, various models have been proposed to explain how changes in SES over time may influence childhood health.
In a life-course approach, socially patterned exposures to advantages or adversity throughout development are proposed to influence health.16,17 First, the critical period is identified as a developmental stage in which increased sensitivity to external agents may have crucial effects on later health. Second, accumulation of risk throughout the life course suggests that exposures or insults (advantages or adversity) gradually accumulate to increase (or decrease) risk of chronic disease and mortality, and that differences in cumulative lifetime exposure primarily explain observed socio-economic differences in risk of disease.18,19 Third, social mobility suggests that individuals may shift social structure categories once or more during the life course. Social mobility is also linked to downward or upward intergenerational or intragenerational mobility, which is a social phenomenon in its own right and should be considered a potential risk factor of disease.20
In particular, previous studies have found that the effect of poverty on child development appears to depend on how long poverty lasts.21,22 The timing of poverty also may be important for childhood outcomes.21,22 The association between adversity and problems in child development may occur as young as the age of 3–5 years.23,24 During early childhood, when emotional, social, and cognitive development takes place through observation, experiences, and communication with others, environmental factors play a crucial role.25 Thus, exposures to different family environments during early childhood may affect healthy (or unhealthy) development. In this context, we investigated the relationship between household income trajectory during early childhood and occurrence of childhood ADHD via national health insurance cohort data. We addressed two research questions: (a) how household income fluctuates during childhood in Korea, and (b) how changes in household income affect childhood ADHD.
2. Methods
2.1. Data collection and participants
Data were acquired from the Korean National Health Insurance Cohort Database (KNHICD) from 2002 to 2013, including information on approximately one million Korean people (eAppendix 1). The KNHICD offers nationally representative cohort data on the entire Korean population to trace characteristics over time, reveal epidemiologic causes of disease, and develop health policies. The KNHICD used a 2.5% (n = 1,025,340) stratified random sampling method, including age, sex, residence, health insurance type, household income decile (obtained through health insurance premiums), and individual total medical costs in 2002. In addition, the structure of the cohort data was semi-dynamic, such that about 9000 newborn infants were added using stratified random sampling every year (the same sampling method as with the first wave) to preserve the national representativeness of the original sample by replacing those lost due to death or emigration over time. Unique de-identified numbers for patients, age, sex, type of insurance, diagnoses according to the International Classification of Diseases (ICD-10), medical costs, and prescribed drugs were included. In addition, the unique de-identified number was linked to mortality information from the Korean National Statistical Office.
This study adhered to the tenets of the Declaration of Helsinki. The study design was reviewed and approved by the ethics board of the Graduate School of Public Health at Yonsei University (2-1040939-AB-N-01-2014-239).
We conducted a cohort study of those born in 2002/2003 to investigate the association between change in household income and ADHD. Among 1,025,340 KNHIC enrollees, we selected 9565 infants from 2002 and 9437 infants from 2003. We included participants who had complete income information to estimate the household income trajectory during early childhood (4 years after childbirth). From the pool of individuals (n = 19,002), 456 from 2002 and 517 from 2003 were lost due to emigration or death during the 4-year period after birth. Overall, we included a cohort of 18,029 infants born in 2002 (n = 9109) and 2003 (n = 8920) (eFigure 1).
2.2. Diagnosis of ADHD and follow-up
Diagnostic status was based on clinical diagnoses extracted from the KNHICD (ICD-10 codes F90.x or F98.8) (n = 556). We did not consider those who received an ADHD diagnosis before age 3 (n = 2) because diagnoses are usually made after age 3. Date of diagnosis was defined as date first recorded. All individuals were observed from birth until December 31, 2013 (10 or 11 years), or until a diagnosis of ADHD or death, whichever came first.
2.3. Socioeconomic status (household income)
We used the yearly average insurance premium as a proxy for household income. In Korea, individuals qualify for medical aid if household income is less than $600 per month. If household income is more than $600 per month, individuals qualify for national health insurance. In the dataset, individuals who qualified for national health insurance were distributed between the 1st and 100th percentile for yearly income, while those who had medical aid were classified as zero percentile. We classified household income into the following: (1) low income (medical aid/below the 30th percentile), (2) middle-low income (31st–50th percentile), (3) middle-high income (51st–80th percentile), and (4) high income (81st–100th percentile). Household income trajectory classes were observed for children at age 3 years (i.e. 0, 1, 2, and 3 years old) using a group-based model.
2.4. Covariates
Demographic factors (sex and region) and co-morbidity of ADHD (identified by reviewing medical histories) were included. Low birth weight was identified from medical records (ICD-10 codes P07.x) after birth. Conduct disorders (aggressive disorder, oppositional defiant disorder), emotional disorders (anxiety, depression), social disorders, tic disorders, autism spectrum disorders, and developmental disorders were identified based on previous literature.26 Comorbid diagnoses of conduct disorder or oppositional defiant disorder (codes F91.x), emotional disorders (codes F93.x), social disorders (codes F94.x), tick disorders (codes F95.x), autism spectrum disorders (codes F84.0, F84.1), and developmental disorders (codes F80.x, F81.x, F82.x, F83.x, F88.x, F89.x) were obtained for all cohort members from KNHICD. In addition, intellectual disability was included in this study. In South Korea, a diagnosis of intellectual disability is based on a sum score of the social maturity scale and intelligence quotient score below 70.
2.5. Statistical analysis
Distributions of general characteristics at baseline were determined. Household income trajectories were created using a group-based trajectory modeling approach within the TRAJ macro in SAS (SAS Institute, Cary, NC, USA).27,28 We fit the income trajectory model to the censored normal distribution. In addition, we used the Bayesian information criterion to determine the number of groups (eTable 1). For each child, the posterior probability of membership in each trajectory group was calculated, and children were assigned to the household income trajectory for which they had the highest probability. The mean probability of final group membership was 0.91 (range 0.88–0.95 across groups). The resulting category was then included as a predictor in Cox proportional hazard regression models to establish the occurrence of ADHD from childbirth (2002/2003) through 2013. The level of significance was set at P < 0.05. SAS version 9.4 was used for the analysis.
3. Results
Overall, 554 children (3.1%) were diagnosed with ADHD during the course of this study. Table 1 presents general characteristics of the study participants at baseline. The distributions were similar between infants born in 2002 and 2003. Of the 18,029 participants, 1117 (6.2%), 5171 (28.7%), 8576 (47.6%), and 3165 (17.6%) were included in the low, mid-low, mid-high, and high-income groups, respectively.
Table 1. General characteristics of the study participants at baseline.
| Total | 2002 | 2003 | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Total | 18,029 | 9109 | 8920 | |||
| Income | ||||||
| Quartile 1 (low) | 1117 | 6.2 | 572 | 6.3 | 545 | 6.1 |
| Quartile 2 (mid-low) | 5171 | 28.7 | 2693 | 29.6 | 2478 | 27.8 |
| Quartile 3 (mid-high) | 8576 | 47.6 | 4288 | 47.1 | 4288 | 48.1 |
| Quartile 4 (high) | 3165 | 17.6 | 1556 | 17.1 | 1609 | 18.0 |
| Income trajectory | ||||||
| Consistently low | 1026 | 5.7 | 466 | 5.1 | 560 | 6.3 |
| Consistently mid-low | 3039 | 16.9 | 1615 | 17.7 | 1424 | 16.0 |
| Mid-low to mid-high | 1632 | 9.1 | 854 | 9.4 | 778 | 8.7 |
| Consistently mid-high | 7527 | 41.7 | 3761 | 41.3 | 3766 | 42.2 |
| Decreasing | 911 | 5.1 | 470 | 5.2 | 441 | 4.9 |
| Mid-high to high | 640 | 3.5 | 328 | 3.6 | 312 | 3.5 |
| Consistently high | 3254 | 18.0 | 1615 | 17.7 | 1639 | 18.4 |
| Sex | ||||||
| Men | 9388 | 52.1 | 4755 | 52.2 | 4633 | 51.9 |
| Women | 8641 | 47.9 | 4354 | 47.8 | 4287 | 48.1 |
| Location | ||||||
| Rural | 5490 | 30.5 | 2809 | 30.8 | 2681 | 30.1 |
| Urban | 12,539 | 69.5 | 6300 | 69.2 | 6239 | 69.9 |
| Low birth weight (<2500 g) | ||||||
| No | 17,894 | 99.3 | 9050 | 99.4 | 8844 | 99.1 |
| Yes | 135 | 0.7 | 59 | 0.6 | 76 | 0.9 |
| Conduct disorders (aggressive disorder, oppositional defiant disorder) | ||||||
| No | 18,009 | 99.9 | 9098 | 99.9 | 8911 | 99.9 |
| Yes | 20 | 0.1 | 11 | 0.1 | 9 | 0.1 |
| Emotional disorders (depression, anxiety) | ||||||
| No | 17,808 | 98.8 | 8996 | 98.8 | 8812 | 98.8 |
| Yes | 221 | 1.2 | 113 | 1.2 | 108 | 1.2 |
| Social disorders | ||||||
| No | 18,000 | 99.8 | 9091 | 99.8 | 8909 | 99.9 |
| Yes | 29 | 0.2 | 18 | 0.2 | 11 | 0.1 |
| Tic disorders | ||||||
| No | 17,830 | 98.9 | 9004 | 98.8 | 8826 | 98.9 |
| Yes | 199 | 1.1 | 105 | 1.2 | 94 | 1.1 |
| Autism spectrum disorders | ||||||
| No | 18,000 | 99.8 | 9091 | 99.8 | 8909 | 99.9 |
| Yes | 29 | 0.2 | 18 | 0.2 | 11 | 0.1 |
| Developmental disorders | ||||||
| No | 17,763 | 98.5 | 8945 | 98.2 | 8818 | 98.9 |
| Yes | 266 | 1.5 | 164 | 1.8 | 102 | 1.1 |
| Intellectual disability | ||||||
| No | 17,950 | 99.6 | 9061 | 99.5 | 8889 | 99.7 |
| Yes | 79 | 0.4 | 48 | 0.5 | 31 | 0.3 |
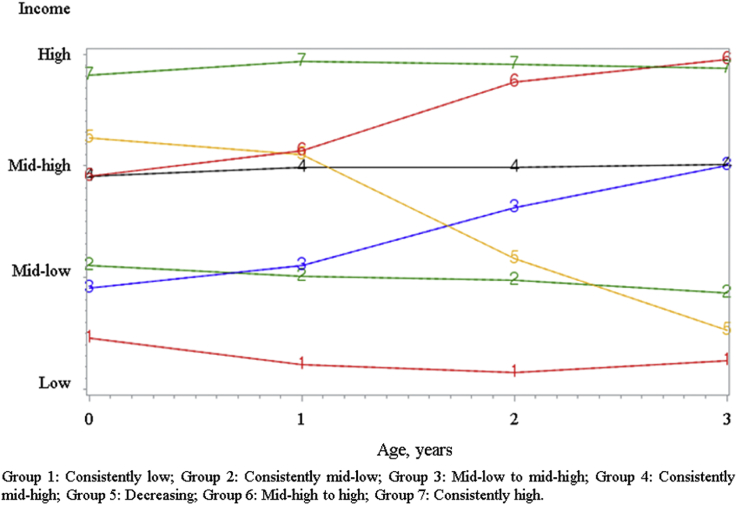
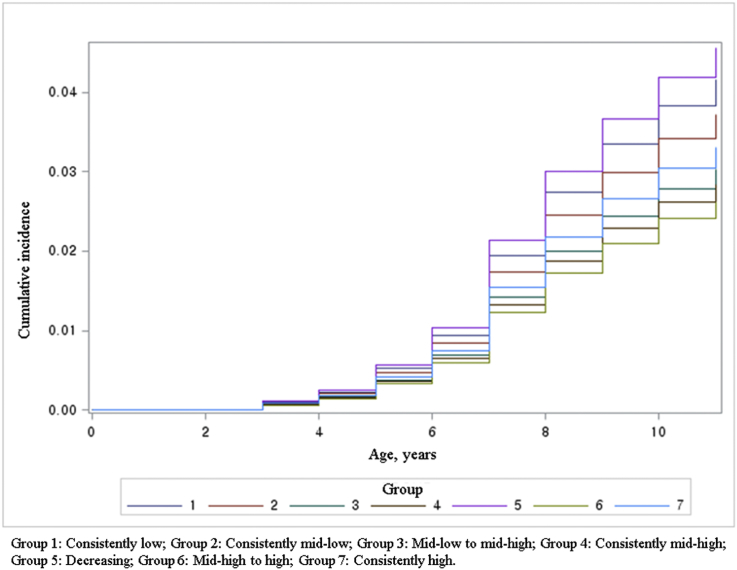
Fig. 1 displays the results of a group-based model illustrating household income trajectory patterns from birth to age 3 years. Fig. 2 displays the cumulative incidence of ADHD by household income group. The cumulative incidence of ADHD was different across household income trajectories (P = 0.035). The cumulative incidence of ADHD was, in increasing order, highest among children who lived in decreasing (group 5), consistently low (group 1), and consistently mid-low (group 2) income households.
Fig. 1. Household income quartile trajectory groups during the 4-year period after childbirth.
Fig. 2. Results of the Kaplan-Meier method for the occurrence of ADHD by household income trajectories.
Table 2 shows general characteristics according to ADHD status. Among the 554 children with ADHD, proportions were higher for boys, those who lived in urban areas, and those who had comorbid conduct, emotional, and social disorders.
Table 2. General characteristics of participants by the occurrence of ADHD.
| n | % | ADHD | Non-ADHD | |||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Total | 18,029 | 554 | 3.1 | 17,475 | 96.9 | |
| Income | ||||||
| Quartile 1 (low) | 1117 | 6.2 | 41 | 3.7 | 1076 | 96.3 |
| Quartile 2 (mid-low) | 5171 | 28.7 | 168 | 3.2 | 5003 | 96.8 |
| Quartile 3 (mid-high) | 8576 | 47.6 | 241 | 2.8 | 8335 | 97.2 |
| Quartile 4 (high) | 3165 | 17.6 | 104 | 3.3 | 3061 | 96.7 |
| Income trajectory | ||||||
| Consistently low | 1026 | 5.7 | 40 | 3.9 | 986 | 96.1 |
| Consistently mid-low | 3039 | 16.9 | 107 | 3.5 | 2932 | 96.5 |
| Mid-low to mid-high | 1632 | 9.1 | 47 | 2.9 | 1585 | 97.1 |
| Consistently mid-high | 7525 | 41.7 | 203 | 2.7 | 7322 | 97.3 |
| Decreasing | 911 | 5.1 | 39 | 4.3 | 872 | 95.7 |
| Mid-high to high | 642 | 3.6 | 16 | 2.5 | 626 | 97.5 |
| Consistently high | 3254 | 18.0 | 102 | 3.1 | 3152 | 96.9 |
| Sex | ||||||
| Men | 9388 | 52.1 | 430 | 4.6 | 8958 | 95.4 |
| Women | 8641 | 47.9 | 124 | 1.4 | 8517 | 98.6 |
| Location | ||||||
| Rural | 5490 | 30.5 | 128 | 2.3 | 5362 | 97.7 |
| Urban | 12,539 | 69.5 | 426 | 3.4 | 12,113 | 96.6 |
| Low birth weight (<2500 g) | ||||||
| No | 17,894 | 99.3 | 548 | 3.1 | 17,346 | 96.9 |
| Yes | 135 | 0.7 | 6 | 4.4 | 129 | 95.6 |
| Conduct disorders (aggressive disorder, oppositional defiant disorder) | ||||||
| No | 18,009 | 99.9 | 546 | 3.0 | 17,463 | 97.0 |
| Yes | 20 | 0.1 | 8 | 40.0 | 12 | 60.0 |
| Emotional disorders (depression, anxiety) | ||||||
| No | 17,808 | 98.8 | 512 | 2.9 | 17,296 | 97.1 |
| Yes | 221 | 1.2 | 42 | 19.0 | 179 | 81.0 |
| Social disorders | ||||||
| No | 18,003 | 99.9 | 542 | 3.0 | 17,461 | 97.0 |
| Yes | 26 | 0.1 | 12 | 46.2 | 14 | 53.8 |
| Tic disorders | ||||||
| No | 17,830 | 98.9 | 523 | 2.9 | 17,307 | 97.1 |
| Yes | 199 | 1.1 | 31 | 15.6 | 168 | 84.4 |
| Autism spectrum disorders | ||||||
| No | 18,000 | 99.8 | 541 | 3.0 | 17,459 | 97.0 |
| Yes | 29 | 0.2 | 13 | 44.8 | 16 | 55.2 |
| Developmental disorders | ||||||
| No | 17,763 | 98.5 | 500 | 2.8 | 17,263 | 97.2 |
| Yes | 266 | 1.5 | 54 | 20.3 | 212 | 79.7 |
| Intellectual disability | ||||||
| No | 17,950 | 99.6 | 537 | 3.0 | 17,413 | 97.0 |
| Yes | 79 | 0.4 | 17 | 21.5 | 62 | 78.5 |
| Year of birth | ||||||
| 2002 | 9109 | 50.5 | 309 | 3.4 | 8800 | 96.6 |
| 2003 | 8920 | 49.5 | 245 | 2.7 | 8675 | 97.3 |
ADHD, attention deficit hyperactivity disorder.
Table 3 presents the results of the Cox proportional hazards analysis, which assessed the association between household income trajectories and occurrence of ADHD. Compared to children who consistently lived in mid-high income households, children who lived in decreasing, consistently low, and consistently mid-low income households were likely to have an increased risk of ADHD. Among the children, boys and those who lived in urban areas were more likely to have ADHD. Regarding comorbidity, those who had conduct disorders, emotional disorders, social disorders, tic disorders, autism spectrum disorders, developmental disorders, and intellectual disability were more likely to have ADHD.
Table 3. Association between household income trajectories and occurrence of ADHD by 10–11 years.
| HR | 95% CI | ||
|---|---|---|---|
| Income trajectory | |||
| Consistently low | 1.476 | 1.048 | 2.079 |
| Consistently mid-low | 1.363 | 1.077 | 1.726 |
| Mid-low to mid-high | 1.062 | 0.773 | 1.459 |
| Consistently mid-high | 1.000 | ||
| Decreasing | 1.689 | 1.197 | 2.382 |
| Mid-high to high | 0.909 | 0.546 | 1.514 |
| Consistently high | 1.134 | 0.892 | 1.442 |
| Sex | |||
| Men | 2.954 | 2.414 | 3.614 |
| Women | 1.000 | ||
| Location | |||
| Rural | 1.000 | ||
| Urban | 1.497 | 1.226 | 1.828 |
| Low birth weight (<2500 g) | |||
| No | 1.000 | ||
| Yes | 1.302 | 0.580 | 2.922 |
| Conduct disorders (aggressive disorder, oppositional defiant disorder) | |||
| No | 1.000 | ||
| Yes | 6.442 | 3.133 | 13.249 |
| Emotional disorders (depression, anxiety) | |||
| No | 1.000 | ||
| Yes | 5.586 | 4.050 | 7.704 |
| Social disorders | |||
| No | 1.000 | ||
| Yes | 8.987 | 4.845 | 16.670 |
| Tic disorders | |||
| No | 1.000 | ||
| Yes | 3.525 | 2.424 | 5.126 |
| Autism spectrum disorders | |||
| No | 1.000 | ||
| Yes | 3.048 | 1.594 | 5.832 |
| Developmental disorders | |||
| No | 1.000 | ||
| Yes | 4.259 | 3.050 | 5.946 |
| Intellectual disability | |||
| No | 1.000 | ||
| Yes | 2.352 | 1.375 | 4.022 |
| Year of birth | |||
| 2002 | 1.054 | 0.887 | 1.253 |
| 2003 | 1.000 | ||
ADHD, attention deficit hyperactivity disorder; CI, confidence interval; HR, hazard ratio.
4. Discussion
This population-based cohort study examined the association between changes in household income levels and ADHD in infants born in 2002 and 2003 using data from the KNHICD. This study yielded two major findings. First, we found seven income trajectory classes from 2002/2003 to 2005/2006. During the 4-year period after birth, household income (quartiles at baseline) showed seven patterns within three categories: (1) stable groups: (a) consistently low, (b) consistently mid-low, (c) consistently mid-high, and (d) consistently high; (2) increasing groups: (a) change from mid-low to mid-high and (b) change from mid-high to high; and (3) a decreasing group. Second, our results suggested that the cumulative risk of ADHD was highest for those in the low or mid-low income groups and the decreasing income group during the 4-year period after birth.
Our main findings are consistent with previous research investigating the relationship between SES and ADHD in other populations. Based on the existing literature, the occurrence of ADHD was expected to be significantly higher in children who came from low-income families.7–10,14,15 A systematic review summarized that conflict/parent-child hostility, inappropriate treatment, or family adversity are associated with ADHD, and that severe early deprivation is a casual risk factor for ADHD.6 Another study showed that ADHD was associated with a range of indicators of social and economic disadvantages (e.g., poverty, housing tenure, income, lone parenthood, younger motherhood).29 Our results could not fully explain how low socioeconomic status affects ADHD. However, other studies have suggested that the effect of poverty on mental health in children occurs both directly (via environmental resource constraints) and indirectly (through psychological influence). Children from high-SES families benefit from an array of services, goods, parental actions, and social connections, whereas children living in low-SES families lack access, putting them at risk for developmental problems.30 Family income has been shown to indirectly affect child psychopathology via proximal risk mechanisms, such as poor parenting,31 reduced parental supervision,32 stressful events,33 family conflict, and affiliation with deviant peers,22 which are associated with childhood ADHD.
Regarding the interpretation of our results in terms of a life-course study, the increased risk of ADHD in children with consistently low, mid-low, or decreasing family income in early childhood age may have three plausible interpretations. First, the impact of early exposure on different health outcomes may provide evidence of a critical period, during which exposure to advantages or adversity has lifelong effects on subsequent health. The findings of this study are consistent with previous research showing that children born to parents with high education levels were less at risk of ADHD.10 Our results partially support those reported in relevant literature suggesting that lower family income early in life (ages 0–5 years) was associated with higher odds of a broad range of conduct problems at ages 10 and 11 compared to higher family income early in life, independent of current socioeconomic status.34 Our results should be interpreted with caution, because we could not compare the effect of SES trajectories on health outcomes with SES in other developmental periods (e.g., 5 years of age or older, during adulthood, or over the whole lifetime). In our study, the critical period was based on the existing literature. The crucial importance of early childhood experiences in development has been widely accepted by professionals and the general public.35 It has also been suggested that deprivation or an adverse environment during early childhood will permanently influence a child's future growth and behavior.35 Moreover, cumulative evidence supports the association of household poverty with developmental problems in early childhood.21,22,24,30,36 One study suggested that average family income from birth to 5 years was a much stronger predictor of completion of school than was family income measured either between ages 5 and 10 or between ages 11 and 15.37 Thus, research indicates that the level of family income during early childhood and the subsequent effect on childhood outcomes is critical compared to other periods. As a result, we proposed that exposure to disadvantaged or advantaged economic status during early childhood influences the development of ADHD.
In an attempt to understand the association between economic deprivation in early childhood and child development, two theories have been proposed: the family investment model and the family stress model. In the family investment model, household income is associated with positive child development because it enables families to purchase the materials, experiences, and services that benefit a child's development.38 On the other hand, low incomes adversely influence children by reducing the quantity and quality of investments in children, including time spent on child rearing. Although it does not address how economic circumstances may affect the quality of parenting, this economic theory provides a pathway as to how low economic status or changes in economic status may affect the level of material investments in children. Another plausible explanation can be drawn from the family stress model.39 Low income influences a child's development through its impact on parental mental health, which in turn influences parenting practices that are associated with childhood outcomes. Based on these perspectives, it has been speculated that economic deprivation directly influences children's externalizing problems. In addition, low economic circumstances may adversely affect parent's mental health, which in turn may decrease mother-child interactions or lead to poor parenting behaviors. These behaviors may then negatively influence children's development and lead to externalizing problems (inattention/hyperactivity, conduct problems) at age 3 years or older.24
Second, the risk accumulation model may offer another explanation: exposure to SES adversity (or advantage) accumulates throughout the life course and may compromise (or promote) health in later life.16 One study suggested that accumulated exposure to low economic resources causes increasing health problems.40 In the Quebec Longitudinal Study of Child Development birth cohort, children from families living in chronic poverty had more frequent and higher cumulative health problems, and children with intermittent poverty were more often perceived to be in less than very good health by their mothers. Chronic poverty affects many children and has negative consequences for preschool children's health.41 Our results showed that the decreasing-income group had a significant hazard ratio that was as high as that of the consistently low/mid-low groups. A plausible explanation is that multiple hardships existed (e.g., job loss, bankruptcy, parents' severe depression, or other adversities) within households when household income declined dramatically during short periods. Such hardships may tremendously influence households and child development compared to other income trajectories in the same periods.
Third, the adverse influence of downward household income at a young age on the development of ADHD supports social mobility models. These models suggest that those exposed to downward mobility have more accumulated risks compared to their reference groups, whereas those exposed to upward mobility are expected to benefit from status improvement throughout life. In contrast, in a birth cohort study of Brazilians, which focused on changes in family income from birth to 11 years, children whose families were always poor or who became poor between birth and 11 years had greater conduct problems at 15 years of age, but not greater emotional and attention/hyperactivity problems, compared to children whose families had consistently high income.42 Possible explanations include methodological differences in the measurement of family household income trajectories and the duration of household income trajectories. The authors in the Brazilian cohort study suggested that low prevalence of attention/hyperactivity in some family income categories may result in a lack of an observed association between income trajectories and attention/hyperactivity problems. From a methodological perspective, the Brazilian study measure nine income categories from birth to 11 years old, whereas our study measured seven income trajectories from birth to 3 years old, supporting the important periods of child development and separating exposure periods from occurrence periods.
This study expands on previous research by prospectively assessing family income throughout childhood and documenting the effects of accumulation or fluctuation in family income on ADHD. Despite cumulative evidence explaining the association between SES and ADHD, most previous research has measured income at only one time. Few studies have shown that fluctuations in family income are associated with mental health problems, including ADHD.42 Even when family income has been measured more than once, the dynamics of income during childhood have not been captured, such as the health effects of sustained exposure to low income or transitions into and out of low-income groups. Our findings reinforce the value of analyzing different measures of SES when studying the etiology of health inequalities, especially during childhood.
The strengths of this study are its population-based design and data collection from the KNHICD, which is nationally representative. Additionally, we used unique personal identity numbers of each Korean resident and linked them to national insurance and mortality data for follow-up. Despite these strengths, several limitations should be considered. First, the precise age of onset of ADHD among children in our sample was not possible to determine. Therefore, it is difficult to ascertain whether ADHD developed in these children before they had recognizable symptoms of the comorbid psychiatric disorders. Additionally, our estimations could be biased because under- and over-diagnosis may occur when using medical records. Second, the database does not include maternal information on tobacco use, alcohol consumption, dietary habits, or other behavioral factors during pregnancy. However, we attempted to consider these risk factors, given that low SES and low birth weight are associated with maternal behaviors, such as smoking or alcohol assumption. Third, we did not have sufficient data to evaluate the severity of psychiatric comorbidities. Finally, this study used household income estimated from the health insurance premium instead of actual income.
In conclusion, household income trajectory patterns should be considered when investigating SES mobility and risk of ADHD. Our results indicated that social mobility, cumulative exposure, and the critical period (based on previous research) were important in explaining ADHD. These findings suggest that understanding health disparities in Korea and other countries may be best addressed by focusing on childhood. Interventions during these early years of life may help move children onto healthier trajectories, with the hope of maximizing health throughout life.
Conflicts of interest
None declared.
Funding
This study received no external funding.
Acknowledgements
Young Choi and Jaeyong Shin (co-first authors), and Eun-Cheol Park (corresponding author) directly participated in the planning, execution, and analysis of the study. Kyung Hee Cho provided assistance for the design/analysis of the study and interpretation of results. The authors appreciate the administrative support of Yonsei University Institute of Health Services Research.
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.je.2016.09.004.
Footnotes
Peer review under responsibility of the Japan Epidemiological Association.
References
- 1.Campbell SB. Attention-deficit/hyperactivity Disorder. Handbook of Developmental Psychopathology Springer; 2000:383–401. [Google Scholar]
- 2.Angold A, Costello EJ, Erkanli A. Comorbidity. J Child Psychol Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- 3.Barkley RA. Comorbid disorders, social and family adjustment, and subtyping. Atten Deficit Hyperact Disord. 2006:184–218. [Google Scholar]
- 4.Brown TE. Developmental Complexities of Attentional Disorders. ADHD Comorbidities: Handbook of ADHD Complications in Children and Adults Arlington VA. American Psychiatric Association; 2009. [Google Scholar]
- 5.Wilens TE, Biederman J, Brown S, et al. Psychiatric comorbidity and functioning in clinically referred preschool children and school-age youths with ADHD. J Am Acad Child Adolesc Psychiatry. 2002;41:262–268. [DOI] [PubMed] [Google Scholar]
- 6.Thapar A, Cooper M, Eyre O, Langley K. Practitioner review: what have we learnt about the causes of ADHD? J Child Psychol Psychiatry. 2013;54:3–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akinbami LJ, Liu X, Pastor PN, Reuben CA. Attention Deficit Hyperactivity Disorder Among Children Aged 5-17 Years in the United States, 1998-2009. NCHS Data Brief. Number 70. Centers for Disease Control and Prevention; 2011. [PubMed] [Google Scholar]
- 8.Froehlich TE, Lanphear BP, Epstein JN, Barbaresi WJ, Katusic SK, Kahn RS. Prevalence, recognition, and treatment of attention-deficit/hyperactivity disorder in a national sample of US children. Arch Pediatr Adolesc Med. 2007;161:857–864. [DOI] [PubMed] [Google Scholar]
- 9.Pastor PN, Reuben CA. Diagnosed attention deficit hyperactivity disorder and learning disability: United States, 2004-2006. Vital Health Stat 10 Data from the National Health Survey 2008:1–14. [PubMed] [Google Scholar]
- 10.Sauver JLS, Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ. Early life risk factors for attention-deficit/hyperactivity disorder: a population-based cohort study. Mayo Clin Proc. 2004:1124–1131. Elsevier; 2004. [PubMed] [Google Scholar]
- 11.Ford T, Collishaw S, Meltzer H, Goodman R. A prospective study of childhood psychopathology: independent predictors of change over three years. Soc Psychiatry Psychiatr Epidemiol. 2007;42:953–961. [DOI] [PubMed] [Google Scholar]
- 12.Bøe T, Øverland S, Lundervold AJ, Hysing M. Socioeconomic status and children's mental health: results from the Bergen Child Study. Soc Psychiatry Psychiatr Epidemiol. 2012;47:1557–1566. [DOI] [PubMed] [Google Scholar]
- 13.Paananen R, Santalahti P, Merikukka M, Rämö A, Wahlbeck K, Gissler M. Socioeconomic and regional aspects in the use of specialized psychiatric care—a Finnish nationwide follow-up study. Eur J Public Health. 2012:cks147. [DOI] [PubMed] [Google Scholar]
- 14.Sciberras E, Ukoumunne OC, Efron D. Predictors of parent-reported attention-deficit/hyperactivity disorder in children aged 6–7 years: a national longitudinal study. J Abnorm Child Psychol. 2011;39:1025–1034. [DOI] [PubMed] [Google Scholar]
- 15.Döpfner M, Breuer D, Wille D-PN, Erhart M, Ravens-Sieberer U, Group BS. How often do children meet ICD-10/DSM-IV criteria of attention deficit-/hyperactivity disorder and hyperkinetic disorder? Parent-based prevalence rates in a national sample–results of the BELLA study. Eur Child Adolesc Psychiatry. 2008;17:59–70. [DOI] [PubMed] [Google Scholar]
- 16.Ben-Shlomo Y, Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int J Epidemiol. 2002;31:285–293. [PubMed] [Google Scholar]
- 17.Hallqvist J, Lynch J, Bartley M, Lang T, Blane D. Can we disentangle life course processes of accumulation, critical period and social mobility? An analysis of disadvantaged socio-economic positions and myocardial infarction in the Stockholm Heart Epidemiology Program. Soc Sci Med. 2004;58:1555–1562. [DOI] [PubMed] [Google Scholar]
- 18.Power C, Manor O, Matthews S. The duration and timing of exposure: effects of socioeconomic environment on adult health. Am J Public Health. 1999;89:1059–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lynch JW, Kaplan GA, Shema SJ. Cumulative impact of sustained economic hardship on physical, cognitive, psychological, and social functioning. N Eng J Med. 1997;337:1889–1895. [DOI] [PubMed] [Google Scholar]
- 20.Lynch JW, Kaplan GA, Cohen RD, et al. Childhood and adult socioeconomic status as predictors of mortality in Finland. Lancet. 1994;343:524–527. [DOI] [PubMed] [Google Scholar]
- 21.Brooks-Gunn J, Duncan GJ. The effects of poverty on children. Future Child. 1997:55–71. [PubMed] [Google Scholar]
- 22.Bradley RH, Corwyn RF. Socioeconomic status and child development. Ann Rev Psychol. 2002;53:371–399. [DOI] [PubMed] [Google Scholar]
- 23.Yeung WJ, Linver MR, Brooks-Gunn J. How money matters for young children's development: parental investment and family processes. Child Dev. 2002:1861–1879. [DOI] [PubMed] [Google Scholar]
- 24.Kiernan KE, Huerta MC. Economic deprivation, maternal depression, parenting and children's cognitive and emotional development in early childhood. Br J Sociol. 2008;59:783–806. [DOI] [PubMed] [Google Scholar]
- 25.Smith PK. In: Smith Peter K, Cowie Helen, Blades Mark, eds. Understanding Children's Development. Wiley; 2011. [Google Scholar]
- 26.Yoshimasu K, Barbaresi WJ, Colligan RC, et al. Childhood ADHD is strongly associated with a broad range of psychiatric disorders during adolescence: a population-based birth cohort study. J Child Psychol Psychiatry. 2012;53:1036–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nagin D. Group-based Modeling of Development. Harvard University Press; 2005. [Google Scholar]
- 28.Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol Methods Res. 2007;35:542–571. [Google Scholar]
- 29.Russell G, Ford T, Rosenberg R, Kelly S. The association of attention deficit hyperactivity disorder with socioeconomic disadvantage: alternative explanations and evidence. J Child Psychol Psychiatry. 2014;55:436–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duncan GJ, Brooks-Gunn J, Klebanov PK. Economic deprivation and early childhood development. Child Dev. 1994;65:296–318. [PubMed] [Google Scholar]
- 31.Rutter M. Poverty and child mental health: natural experiments and social causation. JAMA. 2003;290:2063–2064. [DOI] [PubMed] [Google Scholar]
- 32.Costello EJ, Compton SN, Keeler G, Angold A. Relationships between poverty and psychopathology: a natural experiment. JAMA. 2003;290:2023–2029. [DOI] [PubMed] [Google Scholar]
- 33.McLoyd VC. Socioeconomic disadvantage and child development. Am Psychol. 1998;53:185. [DOI] [PubMed] [Google Scholar]
- 34.Chen E, Martin AD, Matthews KA. Trajectories of socioeconomic status across children's lifetime predict health. Pediatrics. 2007;120:e297–e303. [DOI] [PubMed] [Google Scholar]
- 35.Clarke AM, Clarke ADB. Early Experience: Myth and Evidence. Open Books London; 1976. [Google Scholar]
- 36.Bor W, Najman JM, Andersen MJ, O'callaghan M, Williams GM, Behrens BC. The relationship between low family income and psychological disturbance in young children: an Australian longitudinal study. Aust N. Z J Psychiatry. 1997;31:664–675. [DOI] [PubMed] [Google Scholar]
- 37.Duncan GJ, Yeung WJ, Brooks-Gunn J, Smith JR. How much does childhood poverty affect the life chances of children? Am Sociol Rev. 1998:406–423. [Google Scholar]
- 38.Conger RD, Elder GH Jr. Families in Troubled Times: Adapting to Change in Rural America. Social Institutions and Social Change: ERIC; 1994. [Google Scholar]
- 39.Conger KJ, Rueter MA, Conger RD. The Role of Economic Pressure in the Lives of Parents and Their Adolescents: The Family Stress Model. 2000. [Google Scholar]
- 40.Aittomäki A, Martikainen P, Laaksonen M, Lahelma E, Rahkonen O. Household economic resources, labour-market advantage and health problems–A study on causal relationships using prospective register data. Soc Sci Med. 2012;75:1303–1310. [DOI] [PubMed] [Google Scholar]
- 41.Séguin L, Nikiéma B, Gauvin L, Zunzunegui M-V, Xu Q. Duration of poverty and child health in the Quebec Longitudinal Study of Child Development: longitudinal analysis of a birth cohort. Pediatrics. 2007;119:e1063–e1070. [DOI] [PubMed] [Google Scholar]
- 42.Anselmi L, Menezes AM, Hallal PC, et al. Socioeconomic changes and adolescent psychopathology in a Brazilian birth cohort study. J Adolesc Health. 2012;51:S5–S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.je.2016.09.004.