Abstract
Background
Childcare centers are an integral part of life for many families with young children. American Indian children are at elevated health risk due to higher levels of obesity and associated health behaviors.
Objective
Assess the childcare environment and children’s physical activity (PA) and dietary intake in young children attending tribally-affiliated childcare.
Design
Cross-sectional study
Participants/setting
11 tribally-affiliated childcare centers across Oklahoma and 82 three-to-five-year-old children.
Main outcome measures
Classroom observations were conducted using the Environmental and Policy Assessment Observation to measure the PA and nutrition environments. Children wore an ActiGraph GT3X accelerometer and lunchtime plate waste was observed.
Statistical analyses
Descriptive statistics, including mean±SD and frequencies, were calculated for the children’s behaviors and environment.
Results
The total environment score was 23.9±5.2 (max 43). The nutrition score was 12.5±3.1 (max 21). The PA score was 11.7±2.2 (max 22). The participants were (mean±SD) 3.8±0.1 years old, 55% male, 67% American Indian, and 38% overweight or obese. Accelerometers were worn for 5.9±1.7 hours, excluding naptime. Children accumulated 4.3±2.2 minutes/hour of moderate-vigorous-PA, 4294±1883 steps/day, and 12.1±3.7 steps/minute. At lunch, children were served 510±241 kilocalories, and consumed 387±239 kilocalories. Lunches consisted of 47% carbohydrate, 20% protein, and 33% fat. Total number of fruit and vegetables served were 2.9±1.9 and consumed was 2.3±1.8, while whole grains served and consumed were 0.3±0.4 and 0.2±0.4, respectively, and lean proteins served and consumed were 0.3±0.4 and 0.2±0.4, respectively.
Conclusion
This study describes obesogenic aspects of the childcare environment and identifies areas for improvement. Children did not accumulate adequate PA nor excessively consume kilocalories or fat. Children consumed multiple fruits and vegetables; however, more whole grains and lean proteins could be provided. Future research might investigate how the healthfulness of the childcare environment may be improved by counseling providers on nutrition and physical activity strategies to prevent obesity.
Keywords: Early child education, American Indian, physical activity, accelerometer, dietary intake, plate waste
INTRODUCTION
In the U.S., 61% of children younger than six years of age attend childcare.1 Childcare centers provide a viable environment for early obesity prevention interventions.2,3 Given that 9% of two-to-five-year-old children were obese in 2011–2014,4 early obesity prevention is a priority. Ethnic/racial disparities in childhood obesity risk exist;5 young American Indian children suffer disproportionally higher obesity rates.6–9 One study has examined obesogenic behaviors of young American Indian children and it indicates low fruit and vegetable intake and moderate-to-vigorous PA.6
Childcare physical activity best practices include opportunities for activity indoors and outdoors, the presence of play equipment, minimized opportunities for sedentary behavior, staff physical activity behaviors and training, and policies that support an active environment.11 Only 1.5–7 minutes/hour in childcare are spent in moderate-to-vigorous physical activity (MVPA),12–15 which is insufficient. Aspects of the childcare enviroment, such as those listed above, are associated with higher levels of activity in children.15–22
Childcare nutrition benchmarks include modeling and encouraging healthy eating, assessing children’s hunger and satiety cues, serving meals family-style, and not pressuring children to eat.23 Additional recommendations include eating with children,24,25 talking about healthy foods,24 enthusiastic modelling,26,27 multiple food exposures,3,28 appropriate portion sizes,3,29 and serving nutrient-dense food first.30,31 However, children attending childcare are often served and consume foods high in fat,34,36 salt,36 sugar,36 and excessive protein.31,40 Furthermore, childcare attendees do not eat enough grains or vegetables,34–37 especially dark, nutrient-rich vegetables.33–37 Childcare centers participating in the USDA’s Child and Adults Care Food Program (CACFP) prepare lunches that are more nutrient dense41 and include more fruits and vegetables and fewer sweets and sweetened beverages,42 compared with meals provided by non-CACFP centers42 or by parents of children in care.43
The social and environmental components of childcare centers, such as access to the opportunities for activity and staff feeding and activity behaviors, have been associated with obesogenic behaviors. 13,15–19,21,22,25–28,30,31,33,44,45 Little is known about obesogenic practices in centers serving American Indian children, who are vulnerable to health inequalities.10,46–48 Understanding and improving factors related to the development of obesity by young minority children may improve health disparities. The purpose of this study was to describe the physical activity and nutrition environments at childcare centers and obesogenic behaviors in preschool children attending tribally-affiliated facilities in Oklahoma.
METHODS
Study Design, Participants, Measures Overview
This was a cross-sectional study including eleven tribally-affiliated full-day childcare centers caring for children ages three-to-five-years. These centers are supported by different tribes and predominately enroll American Indian children. There is no standardization as each center is operated by a sovereign tribe. Attempts were made to contact all 38 tribes across Oklahoma; 10 could not be contacted; 12 were not eligible (did not provide care for 3–5 year old children all day); 8 were interested but conflicts arose with scheduling; 7 tribes with 11 centers participated. Centers received a $50 gift card for participation. Legal guardians signed consents to allow personal contact by researchers. Families received a $15 gift card for participation.
All 3-to-5-year-old children (n=286) in the 11 participating centers were invited to participate. One hundred thirty-seven (48%) of the invited children’s parents provided written consent for activity and dietary measurement. A two-day environmental observation took place at each center starting at 7:30am until 5:30pm in all classrooms containing consented children. All children were observed in the classroom. For those guardians not providing written consent for activity and dietary measurement, an opt-out option was provided if they did not wish their child to be observed. The final analytical sample included 82 children with complete demographic information and at least one day (n=57 with two days) of both activity and dietary intake. The final sample was limited due to child absenteeism during scheduled observation days. All procedures were approved by University of Oklahoma Health Sciences Center and Tribal Institutional Review Boards.
Measures
Demographic Characteristics
Directors reported center characteristics including enrollment, duration of operation, teacher education requirements, and food program participation. Guardians reported children’s demographics including birthday, race, sex, and hours/day in care.
Environment and Policy Assessment and Observation Instrument (EPAO)
Trained researchers used the EPAO to observe the childcare environment for two full days regarding aspects of the nutrition and physical activity environment, foods served, opportunities for movement or sitting, and staff practices and behaviors regarding food and physical activity.49 Previous research has determined the EPAO inter-rater observations are sufficient (87.3% agreement).49 Researchers attended several hours of classroom training and at least two days of field training. Before researchers could observe independently, agreement was reached between classroom comparisons of trainees and a master observer. Some degree of subjectivity is inherent in the instrument, as some behaviors can be subtle or nuanced. For example, child satiety observation aimed to determine whether staff encouraged more eating after the child indicated they were finished, or if second helpings were provided before a child made a request. Encouraging children to try food was gentle and positive, rather than pressuring a child to eat more food or clean a plate before being excused. In this study, specific percent agreement was not utilized to determine training comprehension, rather an overall agreement and understanding of how to conduct the EPAO was used. As questions were raised, the observers discussed and reached consistency in interpreting classroom observations and subsequent scoring on the EPAO. The document review portion of the EPAO was not included to reduce burden for directors.
The EPAO includes 64 individual items and is detailed elsewhere.49 Item responses were converted from their raw responses to a 3-point score (0, 1, and 2), averaged within a given subscale, and multiplied by 10, with the average of all subscale scores representing the respective nutrition (possible range 0–21) or physical activity (possible range 0–22) scale score.49 Nutrition subscales include: fruits and vegetables served, high sugar high fat foods served, access to water and beverages, nutrition staff behaviors, nutrition environment, and nutrition training and education. Physical activity subscales include: opportunities for physical activity, opportunities for sedentary activity, sedentary environment, physical activity environment, and physical activity staff behaviors. All environment scores were collected on both days and were averaged for analyses. A higher value indicated a more healthful, i.e., less obesogenic, environment.
Observations of Children’s Physical Activities in Center Classrooms
Since not all children wore accelerometers and time in various activities were included as individual items integrated into EPAO subscales, center classroom time in activity was recorded by the researcher. Providing the actual time in activities more robustly describes these classrooms in addition to the EPAO subscales. Activity was classified as active play (child-directed play where children were substantially moving), structured physical activity (movement that was structured, such as teacher-led, video, or music), outdoor active play (active play that occurred outdoors, a subsection of active play), sedentary activities (children are seated and encouraged to stay seated), and TV viewing. The number of activity bouts lasting longer than 60 seconds were also manually recorded using digital wristwatch when 50% or more of the children in the classroom were engaged in physical activity, regardless of whether the activity was structured, outdoors, or active play. Training for determination of time in activity and the type of activity followed the EPAO training lead by instrument developers.
Objectively Measured Physical Activity
The ActiGraph GT3X accelerometer (Pensacola, FL) was used to objectively measure physical activity and sedentary behavior. ActiGraph accelerometers are valid50,51 and reliable52 and were attached to an elastic belt worn around the waist. They have been widely used with children, including three-to-five-year-old children.50–53 Activity was recorded in 5-second time intervals, which were filtered into sedentary, light, moderate and vigorous levels of intensity, using cut-points specifically developed for preschool children.53
Children wore the accelerometer from the time of arrival to departure for two days. Continuous strings of zeros lasting at least 30 minutes were considered naptime, which lasts between 2–3 hours for this age group, and removed from analyses and wear-time. Physical activity outcome variables included minutes of sedentary behavior, light activity, moderate activity, and vigorous activity, steps/day, and minutes of MVPA activity/hour. If two days of physical activity were available for a child, a computer-selected random day was used for analyses. If a single day was available, that day was used for analyses.
Observations of Children’s Dietary Intakes at Lunch
The Dietary Observation for Child Care training system54 was developed to assess food served and eaten. Each researcher observed the foods and quantities served and plate waste for no more than three children54 and each child was only observed by a single researcher. To collect dietary intake for the maximal number of children, additional researchers, if available, participated in meal observation. A maximum of four researchers observed meals as space permitted and children were eligible for observation. The process consisted of the visual estimates in tablespoons, teaspoons, quantity counts (as in the case of nuggets, for example) of foods and ounces of beverage served to each child. Quantities could vary even if food was pre-plated or served by teachers rather than children. The amount of any food or beverage that was dropped, spilled or traded, of any subsequent servings of food or beverage provided or pilfered from another plate and of each food or beverage remaining on the plate at the end of the meal was recorded.
Intake was determined by the following equation: served + subsequent servings – dropped/spilled - remaining food = intake. Efforts were made to avoid disrupting normal classroom lunch procedures. As needed, researchers took the plate or tray from the child before disposal, to allow better estimation of food. If milk was served in a carton and milk remained, the carton was removed by research staff and the remaining milk poured into a cup for the estimate of waste. Food preparation staff were interviewed after the meals for recipes, product branding, and preparation methods to accurately determine nutrients. Researchers were proficient in determining plate waste through training, a practical exam, and field training. There was high reliability between observers across foods (ICC=0.968, p<0.001).
Nutrient intakes were recorded using FoodWorks® nutrient analysis software (The Nutrition Co., Long Valley N.J.) in conjunction with the USDA food database.55 Dietary outcomes included kilocalories and macronutrients for the foods served and consumed. The number of fruits, vegetables, low-fat dairy, whole grains, high-fat meat, and high-sugar/high-fat foods were also calculated by counting foods. Justification for this approach is that the actual serving sizes of different foods vary, and the liberal approach errs in favor of the childcare center, which may try to increase exposure to fruits and vegetables in mixed dishes (i.e., tossed salad with lettuce, carrots, broccoli, and tomato), none of the ingredients of which would reach a full serving individually.56 If two days of dietary intake were available for a child, a computer-selected random day was used for analyses. If a single day was available, that day was used for analyses.
Assessment of Children’s Weight Status
Height and weight were measured by trained researchers using standard protocols using a portable SECA scale and stadiometer (Hanover, MD). Body mass index (BMI; kg/m2) and age-and sex- percentile were calculated and weight status was determined (overweight ≥85th percentile).57
Statistical Analyses
Descriptive statistics, including means, standard deviations, and frequencies, were calculated for the children’s behaviors and environment. SAS 9.3 was used for all statistical analyses.
RESULTS
Center and child characteristics are presented in detail in Table 1. There were 7.5±3.6 participants from each center, with an average total enrollment of 27.0±21.1. The total environment score was 23.9±5.2, out of possible 43. The centers’ two-day average EPAO nutrition score was 12.5±3.1, out of possible 21 and physical activity score was 11.7±2.2, out of possible 22. Respective subscale scores are shown in Figure 1. Classroom Time in activities from observation is presented in Table 2. In sum, during the day, children had an average of 3.5 bouts of activity and total active play time lasted 118.9 minutes while total minutes of sedentary time lasted 90.7 minutes.
Table 1.
Center (n=11) and Three-to-Five-Year-Old Participants (n=82) Descriptive Characteristics in Tribally-Affiliated Childcare Centers Across Oklahoma in 2012
| Center Descriptive Characteristics | Mean (SD) or Percentage | Range |
|---|---|---|
| Number children enrolled per center | 7.5 (3.6) | (3 – 14) |
| Percent American Indian enrollment | 37.3 (25.8) | (25 – 100) |
| Percent overweight/obese | 40.3 (16.0) | (14.3 – 66.7) |
| Years of center operation | 13.9 (8.2) | (6 – 28) |
| Number children allowed per center | 27.0 (21.1) | (3 – 78) |
| Director education (% of centers)a | ||
| Some college | n=5 (50%) | |
| ≥4 year college | n=5 (50%) | |
| Teacher education (% of centers)a | ||
| GED/HS + 120 hours early care (CDAb) | n=3 (30%) | |
| College degree (BA/BS) | n=1 (10%) | |
| Some with CDA and some BA/BS | n=2 (20%) | |
| No teacher education requirement | n=4 (40%) | |
| Participate in CACFPc (% of centers)a | n=10 (100%) | |
| Family style meal service (% of centers)a | n=4 (36.4%) | |
|
Participant Descriptive Characteristics | ||
| Age | 3.8 (0.8) | (3.0 – 5.0) |
| Sex (% of children) | ||
| Male | n=45 (55%) | |
| Race/Ethnicityd (% of children) | ||
| American Indian | n=55 (67%) | |
| White Non-Hispanic | n= 23 (28%) | |
| Other | n=4 (5%) | |
| Body Mass Index Percentilee | 69.8 (26.7) | (1.7 – 99.9) |
| Weight status (% of children)f | ||
| Normal weight | n=51 (62%) | |
| Overweight and obese | n=31 (38%) | |
| Hours per day at childcare | 7.6 (1.6) | (2.5 – 10.0) |
One center did not report center descriptive characteristics.
CDA = Child Development Associate. Certification requiring 120 hours of early education plus GED/High school diploma
CACFP = Child and Adult Care Food Program
Parents could select multiple of the following options for race/ethnicity: American Indian, white, black, Hispanic, Asian, Hawaiian/Pacific Islander, other (write in response). Given response rates and focus on American Indian heritage, race/ethnicity categories were combined into three mutually exclusive groups: any indication of American Indian or Alaska native, white only with no indication of any non-white race or ethnicity, and all other responses.
Body mass index percentile is adjusted for child’s age in months and sex
Overweight and obesity classification was determined ≥85th percentile for age and sex56
Figure 1. Obesogenic Environment Scores (mean across centers, range, and maximum possible score), from the Environment and Policy Assessment Observation, for 11 American Indian Child Care Centers Across Oklahoma in 2012.
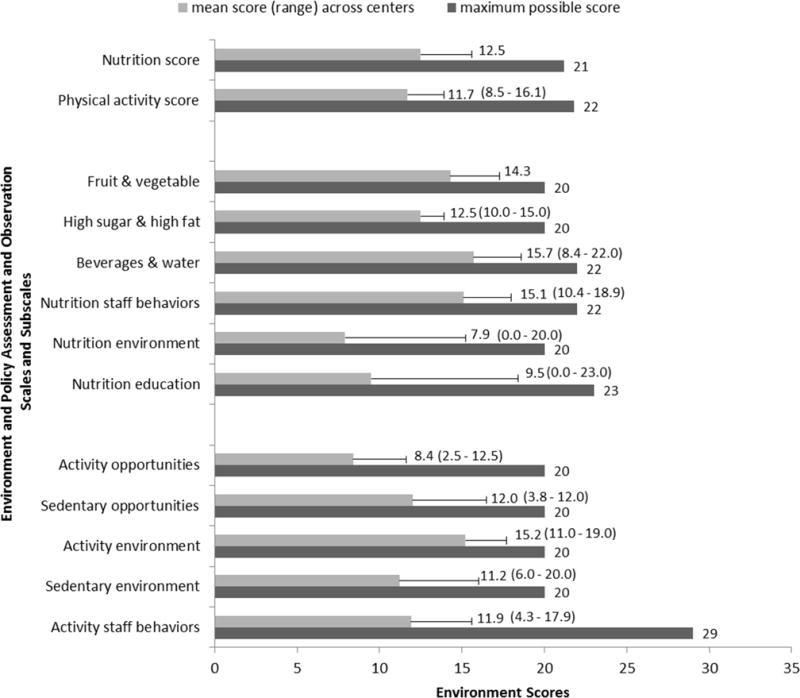
aScales and score represent the Environment and Policy Assessment Observation (EPAO) tool. As conventionally utilized and described in Ward et al.,48 observation item responses on the EPAO observation were converted from their raw responses to a 3-point scale (0, 1, and 2), averaged within a given subscale, and multiplied by 10, with the average of all subscale scores representing the respective nutrition or physical activity scale score.
Table 2.
Classroom Time Spent in Physical Activity and Sedentary Behavior in 11 Tribally-Affiliated Childcare Centers Across Oklahoma in 2012
| Variable | Mean (SD) | Range |
|---|---|---|
| Number of activity boutsa,b | 3.5 (1.9) | (1.0 – 8.0) |
| Total minutes active play timea,c | 118.9 (74.6) | (28.5 – 273.5) |
| Total minutes structure activitya,d | 8.2 (11.7) | (0.0 – 45.0) |
| Total minutes outdoor play timea,e | 99.3 (70.2) | (28.5 – 261.5) |
| Total minutes of sedentary timea,f | 90.7 (46.4) | (32.0 – 153.5) |
| Total minutes of TV viewing timea,g | 38.8 (45.4) | (0.0 – 107.5) |
Minutes of time in physical activity and sedentary behaviors were recorded by a stop watch and averaged over two days of observation per childcare center classroom.
A bout of physical activity was defined as an occasion of physical activity by at least half the class, lasting longer than one minute.
Active play time can include outdoor play time, but does not include structured activity.
Structured activity is activity lead by staff or teachers.
Outdoor play time is time spent outdoors in which the children are playing
Total sedentary time can include TV viewing time.
Total minutes of TV viewing time is the time in which the TV was present and on and at least half the class was watching TV.
Eighty-two children (55% male; 67% American Indian; 3.8±0.8 years, 69.8±26.7 BMI percentile, 38% overweight/obese) were included. Participant physical activity behaviors and dietary intake are presented in Table 3. In brief, children wore the accelerometer for 5.9 hours, excluding nap, and accumulated 4.3±2.2 minutes/hour of moderate-vigorous-PA and 12.1±3.7 steps/minute. Sedentary time lasted nearly five hours and minutes of MVPA lasted less than half an hour. At lunch, children were served 510±241 kilocalories, and consumed 387±239 kilocalories. Lunches consisted of 47% carbohydrate, 20% protein, and 33% fat and was similar between served and consumed. Total number of fruit and vegetables served were 2.9±1.9 and consumed was 2.3±1.8, while whole grains served and consumed were 0.3±0.4 and 0.2±0.4, respectively, lean proteins served and consumed were 0.3±0.4 and 0.2±0.4, and sugar sweetened beverages served and consumed were 0.1±0.3 and 0.1± 0.3, respectively.
Table 3.
Physical Activity Behaviors, and Dietary Intake of Three-to-Five-Year-Old Participants (n=82) in 11 Tribally-Affiliated Childcare Centers Across Oklahoma in 2012
| Mean (SD) | Range | |
|---|---|---|
| Physical Activitya (all values exclude nap time) | ||
| Hours wearing accelerometer | 5.9 (1.7) | 1.2–9.2 |
| Sedentary time (minutes) | 297.5 (92.0) | 56.3–585.5 |
| Light physical activity (minutes) | 33.0 (14.0) | 6.9–73.3 |
| Moderate physical activity (minutes) | 16.2 (10.2) | 1.8–41.6 |
| Vigorous physical activity (minutes) | 8.8 (7.1) | 1.1–41.6 |
| Steps/day | 4294 (1833) | 917–9025 |
| Minutes MVPAb/hour | 4.3 (2.2) | 0.6–9.8 |
| Served | Consumed | |||
|---|---|---|---|---|
| Dietary Intakec | Mean (SD) | Range | Mean (SD) | Range |
| Kilocalories | 509.7 (240.6) | 128.2–1087.0 | 387 (239.3) | 25.0–1226.0 |
| Carbohydrate (g) | 55.4 (21.8) | 15.4–106.0 | 41.5 (21.3) | 1.8–103.4 |
| Carbohydrate (%) | 45.9 (12) | 25.1–71.0 | 47.2 (15.8) | 13.1–84.0 |
| Protein (g) | 26 (12.7) | 5.1–58.7 | 19.4 (12.3) | 2.0–61.1 |
| Protein (%) | 20.9 (6.2) | 12.5–20.9 | 20.5 (8.3) | 10.0–54.1 |
| Total fat (g) | 21.1 (15.1) | 2.8–63.6 | 16.5 (15) | 0.3–78.5 |
| Total fat (%) | 33.2 (12.6) | 10.4–57.9 | 33 (14.9) | 4.1–71.4 |
| Total fruit & vegetable (number of foods) | 2.9 (1.9) | 1.0–8.0 | 2.3 (1.8) | 0.0–8.0 |
| Lean protein (number of foods) | 0.3 (0.4) | 0.0–1.0 | 0.2 (0.4) | 0.0–1.0 |
| Low fat dairy (number of foods) | 0.8 (0.4) | 0.0–1.0 | 0.8 (0.4) | 0.0–1.0 |
| Whole grains (number of foods) | 0.3 (0.4) | 0.0–1.0 | 0.2 (0.4) | 0.0–1.0 |
| Fried/pre-fried meats (number of foods) | 0.2 (0.4) | 0.0–1.0 | 0.2 (0.4) | 0.0–1.0 |
| High fat High Sugar condiments (number of foods) | 0.7 (1) | 0.0–3.0 | 0.6 (0.9) | 0.0–3.0 |
| Sugar Sweetened Beverages(number of drinks) | 0.1 (0.3) | 0.0–1.0 | 0.1 (0.3) | 0.0–1.0 |
Physical activity was measured using an ActiGraph accelerometer worn by children during the day at the waist.
MVPA = moderate-to-vigorous physical activity.
Dietary intake was assessed using observed plate waste and the Dietary Observation for Child Care instrument.
DISCUSSION
The prevalence of overweight and obesity in this sample was 38%, which is higher than the national prevalence in the same age-group (23%)58 and low-income children across Oklahoma (31%).7 However, it is lower than previous reports of overweight and obesity of preschool-aged children in Midwestern tribes (48%).6
EPAO physical activity environment score was modestly healthier than previous reports (8.315 and 10.217). The strongest aspects of the physical activity environment were a variety of fixed and portable play equipment and minimal opportunities for sedentary behavior (bouts of sitting for >30 minutes, presence and duration of TV viewing and video games). Aspects with the greatest room for improvement were staff behaviors (joining in active play, prompts to increase movement, making positive statements about activity, and physical education) and minimal minutes of active play, frequency and duration of structured activity, and frequency of access to the outdoors. Each of these areas of strength or improvement has been associated with higher volumes of physical activity in previous studies.15–22
EPAO nutrition environment scores in the present study are similar to those previously reported.60 However, a high prevalence of centers participated in family-style meal service (36% vs. 8–12%).25,36 Observations in this study are similar to self-reported practices.29,61 Given the variation between self-report and researcher observations, it is likely that providers are aware of the best-practice recommendations3,23 and may be attempting to implement family-style meal service, yet are not fully compliant. Caregiver feeding style is associated with children’s intake.45 Therefore, it is likely that the repertoire of staff feeding behaviors and discussion about healthy eating and foods affects intake during a meal, regardless of service style. Staff nutrition behaviors (encouraging, sitting with children during meals, attention to hunger and satiety cues, consuming the same foods), access to beverages and water (limited juice and sugar-sweetened beverages, easy access to water indoors and outdoors, reduced fat milk), and servings of fruit and vegetables (frequency of fruit and vegetables, with limited sugar and fat in preparation methods, served daily) were the strongest aspects of the nutrition environment. The areas requiring greatest improvement include staff talking with children about healthy foods, formally and informally, and meal service style and presence of vending machines.
Minutes of MVPA/hour (4.3) was within ranges previously published (1.5–9.0 min/hour).15,14,21,44,59 Overall MVPA accumulated at childcare was higher than previously reported in American Indian preschool children6 but substantially lower than other preschoolers in the U.S.22 Step count was lower than previous reports.16 It is interesting to note that the time spent outdoors by children in this study was three time higher than Tandon et al.;22 however, children accumulated half of the MVPA. It is possible that the centers in the Pacific Northwest22 maximize outdoor time or other variations in staff behaviors related to PA exist.
The energy and nutrients consumed were within acceptable distribution ranges for young children and similar to previous reports in the U.S.,25,39, although lower than childcare centers abroad.27 A previous report of American Indian preschoolers conducted over the full day reported the same fat consumptionbut higher carbohydrate and lower protein.6 The combined fruits and vegetables served and consumed were higher than previous reports,6,25 but this may be due to methodological differences. The previous studies examined cups of fruits and vegetables6,25 and our approach counted any fruit or vegetable served. Given the research and recommendations empahsizing a variety of foods and the need for multiple exposure,3,28 we determined presence of total fruits and vegetables was in greater agreement with this emphasis than cups. It is likely that even though children are being exposed to multiple fruits and vegetables the overall consumption was still low.
The strengths of this project include the use of validated tools and the rigorous classroom and field training completed by researchers. Understanding the centers policies could better help interpret the current study findings. Another strength is the focus on American Indians, given their increased risk for obesity-related disease. Exclusion of the document review in the current study protocol is a limitation as perhaps the center had a policies and training that were not clearly communicated and presence of physical activity policies is beneficial.16 Measurement of dietary intake by trained researchers reduced the error associated with recall and error in estimation of quantity of foods. An important note regarding the assessment of foods based on the desire to err in favor of the childcare serving a variety of fruit and vegetables28 is the potential to underestimate volume of consumption (i.e., 10 nuggets counts as one fried/pre-fried meat). Including an objective measure of physical activity strengthens the quality of the activity data, as there was no potential for misclassification and validated cut-points were used to classify intensity.53 The small sample size precludes the inclusion of experimental analyses that could examine how overall environmental scores and hypothesized constructs of interest are related to child physical activity and nutrition behaviors in this population. Future observations should be conducted on days that are randomly determined and not consecutive. This process would likely maximize the overall number of students present and thus available for participation.
CONCLUSION
This study expands previous research and describes aspects of the childcare center environment that are related to obesity and children’s health behaviors at facilities that serve predominantly American Indian children. Childcare environments assessed have room for improvement regarding physical activity and nutrition. It would be prudent for researchers and practitioners to consider other attributes of the childcare environment, other environments (i.e., families), and factors that may influence child weight and obesogenic behaviors in future studies.
Acknowledgments
We would like to thank all the Tribes and Nations, child care centers, and families for participation in this project. We would also like to acknowledge the hours invested by graduated students in the Behavioral Nutrition and Physical Activity Laboratory. Editorial review was conducted by Kathy Kyler.
Funding Statement: This study was supported by the Gretchen Swanson Center for Human Nutrition, the University of Oklahoma Health Sciences Center Stephenson Cancer Center, and the University of Oklahoma Health Sciences Center Department of Nutrition Sciences. Partial funding provided by National Institutes of Health, National Institute of General Medical Sciences, grant 1 U54GM104938. Study sponsors had no role in the study design, collection, analyses, data interpretation, manuscript writing, or submission.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial disclosures: The authors have no financial relationships relevant to this article to disclose.
Conflict of interest: No authors have any conflicts of interest to disclose.
References
- 1.Federal Interagency Forum on Child and Family Statistics. America’s Children: Key National indicators of Well-Being, 2015. 2015 http://www.childstats.gov/americaschildren/index.asp. Accessed November, 2015.
- 2.Story M, Kaphingst KM, French S. The role of child care settings in obesity prevention. Future Child. 2006;16(1):143–168. doi: 10.1353/foc.2006.0010. [DOI] [PubMed] [Google Scholar]
- 3.American Acadmy of Pediatrics, American Public Health Association, National Resource Center for Health and Safety in Child Care and Early Education. Preventing Childhood Obesity in Early Care and Education Program: Selected Standards from Caring for Our Children: National Health and Safety Performance Standards; Guidelines for Early Care and Education Programs, 3rd Edition. Second. Aurora, CO: 2012. [Google Scholar]
- 4.Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. NCHS Data Brief. 2015;(219):1–8. [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Lawman HG, et al. Trends in Obesity Prevalence Among Children and Adolescents in the United States, 1988–1994 Through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.LaRowe TL, Adams AK, Jobe JB, Cronin KA, Vannatter SM, Prince RJ. Dietary intakes and physical activity among preschool-aged children living in rural American Indian communities before a family-based healthy lifestyle intervention. J Am Diet Assoc. 2010;110(7):1049–1057. doi: 10.1016/j.jada.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weedn AE, Ang SC, C LZ, Darden PM. Obesity Prevalence in Low-Income Preschool Children in Oklahoma. Clin Pediatr. 2012 doi: 10.1177/0009922812441861. [DOI] [PubMed] [Google Scholar]
- 8.Story M, Hannan PJ, Fulkerson JA, et al. Bright Start: Description and main outcomes from a group-randomized obesity prevention trial in American Indian children. Obesity. 2012;20(11):2241–2249. doi: 10.1038/oby.2012.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schell LM, Gallo MV. Overweight and obesity among North American Indian infants, children, and youth. Am J Hum Biol. 2012;24(3):302–313. doi: 10.1002/ajhb.22257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dennison ME, Sisson SB, Lora K, Stephens LD, Copeland KC, Caudillo C. Assessment of Body Mass Index, Sugar Sweetened Beverage Intake and Time Spent in Physical Activity of American Indian Children in Oklahoma. J Community Health. 2015;40(4):808–814. doi: 10.1007/s10900-015-0004-6. [DOI] [PubMed] [Google Scholar]
- 11.McWilliams C, Ball SC, Benjamin SE, Hales D, Vaughn A, Ward DS. Best-practice guidelines for physical activity at child care. Pediatrics. 2009;124(6):1650–1659. doi: 10.1542/peds.2009-0952. [DOI] [PubMed] [Google Scholar]
- 12.Reilly JJ. Low levels of objectively measured physical activity in preschoolers in child care. Med Sci Sports Exerc. 2010;42(3):502–507. doi: 10.1249/MSS.0b013e3181cea100. [DOI] [PubMed] [Google Scholar]
- 13.Alhassan S, Sirard JR, Robinson TN. The effects of increasing outdoor play time on physical activity in Latino preschool children. Int J Pediatr Obes. 2007;2(3):153–158. doi: 10.1080/17477160701520108. [DOI] [PubMed] [Google Scholar]
- 14.Pate RR, Pfeiffer KA, Trost SG, Ziegler P, Dowda M. Physical activity among children attending preschools. Pediatrics. 2004;114(5):1258–1263. doi: 10.1542/peds.2003-1088-L. [DOI] [PubMed] [Google Scholar]
- 15.Vanderloo LM, Tucker P, Johnson AM, van Zandvoort MM, Burke SM, Irwin JD. The influence of centre-based childcare on preschoolers’ physical activity levels: a cross-sectional study. Int J Environ Res Public Health. 2014;11(2):1794–1802. doi: 10.3390/ijerph110201794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bell AC, Finch M, Wolfenden L, et al. Child physical activity levels and associations with modifiable characteristics in centre-based childcare. Aus NZ J Public Health. 2015;39(3):232–236. doi: 10.1111/1753-6405.12314. [DOI] [PubMed] [Google Scholar]
- 17.Bower JK, Hales DP, Tate DF, Rubin DA, Benjamin SE, Ward DS. The childcare environment and children’s physical activity. Am J Prev Med. 2008;34(1):23–29. doi: 10.1016/j.amepre.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 18.Brown WH, Pfeiffer KA, McIver KL, Dowda M, Addy CL, Pate RR. Social and environmental factors associated with preschoolers’ nonsedentary physical activity. Child Dev. 2009;80(1):45–58. doi: 10.1111/j.1467-8624.2008.01245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dowda M, Brown WH, McIver KL, et al. Policies and characteristics of the preschool environment and physical activity of young children. Pediatrics. 2009;123(2):e261–266. doi: 10.1542/peds.2008-2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gubbels JS, Kremers SPJ, van Kann DHH, et al. Interaction Between Physical Environment, Social Environment, and Child Characteristics in Determining Physical Activity at Child Care. Health Psychology. 2010 doi: 10.1037/a0021586. [DOI] [PubMed] [Google Scholar]
- 21.Henderson KE, Grode GM, O’Connell ML, Schwartz MB. Environmental factors associated with physical activity in childcare centers. Int J Behav Nutr Phys Act. 2015;12:43. doi: 10.1186/s12966-015-0198-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tandon PS, Saelens BE, Christakis DA. Active play opportunities at child care. Pediatrics. 2015;135(6):e1425–1431. doi: 10.1542/peds.2014-2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Benjamin Neelon SE, Briley ME. Position of the American Dietetic Association: benchmarks for nutrition in child care. J Am Diet Assoc. 2011;111(4):607–615. doi: 10.1016/j.jada.2011.02.016. [DOI] [PubMed] [Google Scholar]
- 24.Ammerman AS, Ward DS, Benjamin SE, et al. An intervention to promote healthy weight: Nutrition and Physical Activity Self-Assessment for Child Care (NAP SACC) theory and design. Prev Chronic Dis. 2007;4(3):A67. [PMC free article] [PubMed] [Google Scholar]
- 25.Kharofa RY, Kalkwarf HJ, Khoury JC, Copeland KA. Are Mealtime Best Practice Guidelines for Child Care Centers Associated with Energy, Vegetable, and Fruit Intake? Child Obesity. 2015 doi: 10.1089/chi.2015.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hendy HM. Effectiveness of teacher modeling to encourage food acceptance in preschool children. Appetite. 2000;34:61–76. doi: 10.1006/appe.1999.0286. [DOI] [PubMed] [Google Scholar]
- 27.Gubbels JS, Kremers SP, Stafleu A, Dagnelie PC, de Vries NK, Thijs C. Child-care environment and dietary intake of 2- and 3-year-old children. J Human Nutr Diet. 2010;23(1):97–101. doi: 10.1111/j.1365-277X.2009.01022.x. [DOI] [PubMed] [Google Scholar]
- 28.Addessi E, Galloway AT, Visalberghi E, Birch LL. Specific social influences on the acceptance of novel foods in 2–5-year-old children. Appetite. 2005;45:264–271. doi: 10.1016/j.appet.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 29.Sigman-Grant M, Christiansen E, Branen L, Fletcher J, Johnson SL. About feeding children: mealtimes in child-care centers in four western states. J Am Diet Assoc. 2008;108(2):340–346. doi: 10.1016/j.jada.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 30.Harnack LJ, Oakes JM, French SA, Rydell SA, Farah FM, Taylor GL. Results from an experimental trial at a Head Start center to evaluate two meal service approaches to increase fruit and vegetable intake of preschool aged children. Int J Behav Nutr Phys Act. 2012;9:51. doi: 10.1186/1479-5868-9-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwartz MB, O’Connell M, Henderson KE, Middleton AE, Scarmo S. Testing Variations on Family-Style Feeding To Increase Whole Fruit and Vegetable Consumption among Preschoolers in Child Care. Child Obesity. 2015;11(5):499–505. doi: 10.1089/chi.2015.0038. [DOI] [PubMed] [Google Scholar]
- 32.Worobey J, S WH, Adler AL. Diet, Activity and BMI in Preschool-Aged Children: Differences Across Settings. Ecol Food Nutrition. 2005;44:455–466. [Google Scholar]
- 33.Erinosho T, Dixon LB, Young C, Brotman LM, Hayman LL. Nutrition Practices and Children’s Dietary Intakes at 40 Child-Care Centers in New York City. J Am Diet Assoc. 2011;111(9):1391–1397. doi: 10.1016/j.jada.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 34.Ball SC, Benjamin SE, Ward DS. Dietary intakes in North Carolina child-care centers: are children meeting current recommendations? J Am Diet Assoc. 2008;108(4):718–721. doi: 10.1016/j.jada.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 35.Briley ME, Jastrow S, Vickers J, Roberts-Gray C. Dietary Intake at Child-Care Centers and Away: Are Parents and Care Providers Working as Partners or at Cross-Purposes? J Am Diet Assoc. 1999;99(8):950–954. doi: 10.1016/S0002-8223(99)00226-6. [DOI] [PubMed] [Google Scholar]
- 36.Benjamin Neelon SE, Vaughn A, Ball SC, McWilliams C, Ward DS. Nutrition practices and mealtime environments of North Carolina child care centers. Child Obesity. 2012;8(3):216–223. doi: 10.1089/chi.2011.0065. [DOI] [PubMed] [Google Scholar]
- 37.Padget A, Briley ME. Dietary intakes at child-care centers in central Texas fail to meet Food Guide Pyramid recommendations. J Am Diet Assoc. 2005;105(5):790–793. doi: 10.1016/j.jada.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 38.Bollella MC, Spark A, Boccia LA, Nicklas TA, Pittman BP, Williams CL. Nutrient intake of Head Start children: home vs. school. J Am Coll Nutr. 1999;18(2):108–114. doi: 10.1080/07315724.1999.10718837. [DOI] [PubMed] [Google Scholar]
- 39.Nicklas TA, Liu Y, Stuff JE, Fisher JO, Mendoza JA, O’Neil CE. Characterizing lunch meals served and consumed by pre-school children in Head Start. Public Health Nutr. 2013;16(12):2169–2177. doi: 10.1017/S1368980013001377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rasbold AH, Adamiec R, Anderson MP, et al. Macronutrient and micronutrient intakes of children in Oklahoma child-care centres, USA. Public Health Nutr. 2016;19(8):1498–1505. doi: 10.1017/S1368980015002372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bruening KS, Gilbride JA, Passannante MR, McClowry S. Dietary intake and health outcomes among young children attending 2 urban day-care centers. J Am Diet Assoc. 1999;99(12):1529–1535. doi: 10.1016/S0002-8223(99)00375-2. [DOI] [PubMed] [Google Scholar]
- 42.Ritchie LD, Boyle M, Chandran K, et al. Participation in the child and adult care food program is associated with more nutritious foods and beverages in child care. Child Obesity. 2012;8(3):224–229. doi: 10.1089/chi.2011.0061. [DOI] [PubMed] [Google Scholar]
- 43.Robson SM, Khoury JC, Kalkwarf HJ, Copeland K. Dietary intake of children attending full-time child care: What are they eating away from the child-care center? J Acad Nutr Diet. 2015;115(9):1472–1478. doi: 10.1016/j.jand.2015.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gunter KB, Rice KR, Ward DS, Trost SG. Factors associated with physical activity in children attending family child care homes. Prev Med. 2012;54(2):131–133. doi: 10.1016/j.ypmed.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 45.Hughes SO, Patrick H, Power TG, Fisher JO, Anderson CB, Nicklas TA. The impact of child care providers’ feeding on children’s food consumption. J Dev Behav Pediatr. 2007;28(2):100–107. doi: 10.1097/01.DBP.0000267561.34199.a9. [DOI] [PubMed] [Google Scholar]
- 46.Dabelea D, Mayer-Davis EJ, Saydah S, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311(17):1778–1786. doi: 10.1001/jama.2014.3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Foulds HJ, Warburton DE. The blood pressure and hypertension experience among North American Indigenous populations. J Hypertens. 2014;32(4):724–734. doi: 10.1097/HJH.0000000000000084. [DOI] [PubMed] [Google Scholar]
- 48.Wheelock KM, Sinha M, Knowler WC, Nelson RG, Fufaa GD, Hanson RL. Metabolic Risk Factors and Type 2 Diabetes Incidence in American Indian Children. J Clin Endocrin Metab. 2016;101(4):1437–1444. doi: 10.1210/jc.2015-4309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ward D, Hales D, Haverly K, et al. An instrument to assess the obesogenic environment of child care centers. Am J Health Behav. 2008;32(4):380–386. doi: 10.5555/ajhb.2008.32.4.380. [DOI] [PubMed] [Google Scholar]
- 50.Puyau MR, Adolph AL, Vohra FA, Butte NF. Validation and calibration of physical activity monitors in children. Obes Res. 2002;10(3):150–157. doi: 10.1038/oby.2002.24. [DOI] [PubMed] [Google Scholar]
- 51.Sirad JR, Riner W, McIver KL, Pate RR. Physical activity and active commuting to elementary school. Med Sci Sports Exerc. 2005;37(12):2062–2069. doi: 10.1249/01.mss.0000179102.17183.6b. [DOI] [PubMed] [Google Scholar]
- 52.Janz K, Whitt J, Mahoney L. The stability of children’s physical activity as measured by accelerometry and self-report. Med Sci Sports Exerc. 1995;27(9):1326–1332. [PubMed] [Google Scholar]
- 53.Sirard JR, Trost SG, Pfeiffer KA, Dowda M, Pate RR. Calibration and evaluation of an objective measure of physical activity in preschool children. J Phys Act Health. 2005;2(3):345–357. [Google Scholar]
- 54.Ball SC, Benjamin SE, Ward DS. Development and reliability of an observation method to assess food intake of young children in child care. J Am Diet Assoc. 2007;107(4):656–661. doi: 10.1016/j.jada.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 55.United States Department of Agriculture. USDA Food Composition Database. 2015 https://ndb.nal.usda.gov/. Accessed July, 2016.
- 56.Rasbold AH, Sisson SB, Lora KR, Mitchell CM. Television Access, Dinnertime Food Consumption and Obesity Among Young Children in Oklahoma. Advances in Pediatric Research. 2016;3(3):1–8. [Google Scholar]
- 57.Kuczmarski RJ, Flegal KM. Criteria for definition of overweight in transition: background and recommendations for the United States. Am J Clin Nutr. 2000;72(5):1074–1081. doi: 10.1093/ajcn/72.5.1074. [DOI] [PubMed] [Google Scholar]
- 58.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rice KR, Trost SG. Physical activity levels among children attending family day care. J Nutr Educ Behav. 2014;46(3):197–202. doi: 10.1016/j.jneb.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 60.Lyn R, Maalouf J, Evers S, Davis J, Griffin M. Nutrition and physical activity in child care centers: the impact of a wellness policy initiative on environment and policy assessment and observation outcomes, 2011. Prev Chronic Dis. 2013;10:E83. doi: 10.5888/pcd10.120232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sisson SB, Campbell JE, May KB, et al. Assessment of food, nutrition, and physical activity practices in Oklahoma child-care centers. J Acad Nutr Diet. 2012;112(8):1230–1240. doi: 10.1016/j.jand.2012.05.009. [DOI] [PubMed] [Google Scholar]


