Abstract
Objective
The study’s purpose was to investigate moderator, implementation, and mediator variables related to the efficacy of UV4.me, an internet intervention that decreased ultraviolet radiation (UV) exposure and increased skin protection behaviors among young adults.
Methods
Nine-hundred sixty-five 18-25 year olds at risk for skin cancer were recruited nationally online. Participants were randomized to an experimental website (UV4.me), a control website, or assessment only. Participant characteristics (moderators), engagement with and perceptions of interventions (implementation measures), and exposure and protection attitudinal variables (mediators) were assessed. Linear regression and mediation analyses were conducted.
Results
Intervention effects on skin protection were greater for participants with a family history of skin cancer (p = 0.01). Intervention effects on UV exposure were greater among recent indoor tanners (p = 0.04). Improvements in skin protection (but not UV exposure) were associated with perceiving the interventions as satisfying or helpful (ps< .01). The experimental group had better outcomes if they completed more modules (ps< .01) or set more behavioral goals (ps< .01). Knowledge and exposure decisional balance mediated intervention effects for UV exposure (ps < 0.05), and protection decisional balance, self-efficacy, and intentions mediated intervention effects for protection (ps < 0.05).
Conclusions
The experimental intervention was more efficacious for certain high risk groups. The more individuals liked and engaged with the interventions (e.g., by setting goals), the better their outcomes. Mediation results inform theory about change mechanisms and differed by behavioral outcome.
Keywords: intervention mechanisms, skin cancer prevention, young adults, online intervention
Introduction
Skin cancer is the most common cancer, with nearly five million diagnoses annually in the US, and its incidence has been increasing in recent years (Gordon, 2013; Nikolaou & Stratigos, 2014; Tuong, Cheng, & Armstrong, 2012; USDHHS, 2014). Most skin cancers are caused by ultraviolet radiation (UV) exposure from the sun and indoor tanning and are therefore preventable (Cummings, Tripp, & Herrmann, 1997). It is common for young adults (e.g., aged 18-25 years) to expose themselves to large amounts of natural and artificial UV without proper skin protection (e.g., wearing adequate sunscreen) (Buller et al., 2011; Coups, Manne, & Heckman, 2008; C. J. Heckman, Coups, & Manne, 2008; Stanton, Janda, Baade, & Anderson, 2004). For these reasons, it is important for interventions to be available that are effective in addressing skin cancer risk behaviors among young adults.
With approximately 97% of US young adults using the internet (Pew_Research_Internet_Project, 2014), and the evidence for the impact of internet interventions in improving health behaviors (Tate, Finkelstein, Khavjou, & Gustafson, 2009), the internet is an appropriate modality with which to reach young adults and explore the efficacy of a skin cancer risk reduction intervention for this population. We developed the first web-based intervention to modify skin cancer risk and protective behaviors targeted specifically for young adults (ages 18-25 years), which was informed by the Integrative Model for Behavioral Prediction (IM), which is based on other models such as the theory of reasoned action and the theory of planned behavior (Fishbein, Hennessy, Yzer, & Douglas, 2003). Constructs from the IM that can be considered in skin cancer prevention interventions because of their association with skin cancer risk and protective behaviors include demographics; past UV-related behavior; attitudes such as appearance consciousness (Arthey & Clarke, 1995; Reynolds, 2007); other individual difference variables (e.g., knowledge); UV-related beliefs (Cafri, Thompson, & Jacobsen, 2006; Danoff-Burg & Mosher, 2006; J. Hillhouse, Turrisi, Stapleton, & Robinson, 2008; J. J. Hillhouse, Turrisi, & Kastner, 2000; Mahler, Kulik, Butler, Gerrard, & Gibbons, 2008; Olson, Gaffney, Starr, & Dietrich, 2008; Thieden, Philipsen, Sandby-Moller, & Wulf, 2005); norms (Arthey & Clarke, 1995; Borland & Hill, 1990), self-efficacy (Gritz et al., 2006; Hay et al., 2006; James, Tripp, Parcel, Sweeney, & Gritz, 2002; Myers & Horswill, 2006; Stryker et al., 2004); and intentions (Myers & Horswill, 2006). For example, one meta-analysis found that viewing photo-aging information, intended to impact perceived susceptibility to photo-aging beliefs as well as UV exposure and skin protection intentions, was associated with decreased indoor tanning (Williams, Grogan, Clark-Carter, & Buckley, 2013). Thus, one module of the experimental intervention program (UV4.me) focused on photo-aging (the negative effects of UV exposure on appearance). Additionally, UV4.me was targeted to young adults, personally tailored, and included interactive, multimedia, and goal-setting components.
The experimental intervention was efficacious in significantly decreasing UV exposure and increasing skin protection behaviors among young adults at risk of skin cancer in a national randomized controlled trial conducted from March to October of 2014 (Heckman, Darlow, Ritterband, Handorf, & Manne, 2016). Relatively few studies have directly investigated moderators or mediators of successful UV exposure and skin protection intervention packages. The purpose of the current study was to investigate moderator, implementation, and mediator variables related to the intervention effects in the prior trial. Participant characteristics (moderators, Aim 1), engagement with and perceptions of the interventions (intervention implementation measures, Aim 2), and UV and protection attitudinal variables from the IM (mediators, Aim 3) were assessed. For the first aim, potential moderators that were consistent with the IM were selected that would not be likely to change during the course of the intervention but that could be associated with outcomes. These included demographic and background variables, cognitive variables, and past UV exposure behaviors. It was hypothesized that intervention effects would be moderated by variables that have been associated with skin cancer risk behaviors previously (age, sex, race/ethnicity, family history of skin cancer, skin cancer risk, appearance concern, indoor tanning, sunburn) and not moderated by variables that are not clearly associated with risk (level of education, difficulty living on income, health literacy, sensation seeking). For example, individuals with a higher score on a skin cancer risk scale would be expected to benefit more from the experimental intervention than those with lower scores who might experience a ceiling effect; whereas, we attempted to create an intervention that would be appropriate for individuals with a wide range of health literacy levels. For the second aim, it was hypothesized that implementation variables such as a higher level of participant engagement (e.g., module completion and goal setting) and satisfaction with the interventions would be associated with better behavioral outcomes. Finally, for the third aim, potential mediators included IM constructs such as knowledge, attitudes, normative beliefs, self-efficacy, and intentions, all of which were expected to be associated with changes in UV exposure and skin protection outcomes. For example, it was expected that the experimental intervention would increase knowledge, increase positive and decrease negative attitudes toward skin protection, decrease positive and increase negative attitudes toward tanning, decrease perceived norms for tanning, increase self-efficacy for UV avoidance and skin protection, and increase intentions for skin protection, which in turn would be associated with improved UV exposure and skin protection outcomes.
Methods
Participants and Procedures
Study methods and interventions have been described previously elsewhere (Heckman, Darlow, Ritterband, Handorf, & Manne, 2016)). Briefly, participants were recruited nationally online by a consumer research company, Survey Sampling International (SSI), using their US consumer opinion panel and partnerships with other panels and online communities. SSI panelists were exposed to brief web banner ads about the study from which they could click to link to the study website. Once at the study website, interested candidates were asked to complete the Brief Skin Cancer Risk Assessment Tool (BRAT),(Glanz et al., 2003) which was scored automatically. Eligible participants were 18-25 years old, had never had skin cancer, and were at moderate to high risk of developing skin cancer based on the BRAT (Glanz et al., 2003). After completing a baseline survey (n = 965), participants were randomized to one of three treatment conditions: the experimental intervention website, a control website, or assessment only. The experimental website (UV4.me) is based on the Integrative Model of Behavioral Prediction (IM) (Fishbein et al., 2003) and includes 12 main content-oriented modules and several other types of modules and activities (e.g., an avatar) targeted to young adults, personally tailored, and including interactive, multimedia, and goal-setting components. The twelve main modules were: 1. Why do people tan? 2. To tan or not to tan? 3. Indoor tanning, 4. UV & health, 5. Skin cancer, 6. UV & looks, 7. Skin damage, 8. Shade, 9. Clothes, 10. Sunscreen, 11. Sunless tanning, and 12. Skin exams. Constructs from the Integrative Model (Fishbein et al., 2003) were incorporated throughout the modules. For example, in the indoor tanning module, we provided data showing that most young adults do not indoor tan in order to attempt to influence normative beliefs about indoor tanning. The control website was the Skin Cancer Foundation website (SCF; http://www.skincancer.org). Participants completed assessments at baseline in the spring of 2014 (March-June), three weeks after baseline (April-July), and twelve weeks after baseline (June-Oct). This project was approved and monitored by a cancer center’s Institutional Review Board, and informed consent was obtained from research participants. Data were collected in 2014 and analyzed 2015-16. The trial was registered with ClinicalTrials.gov (identifier NCT02147080).
Measures
Behavioral Outcomes
These items were administered at baseline and 12-week follow-up.
Skin Protection
Participants were first asked whether they had been outdoors for more than a few minutes at a time in the past month. If answered in the affirmative, the following sun protection behaviors were assessed, using a seven-item scale adapted from Glanz and colleagues (Glanz et al., 2008): wearing sunscreen with an SPF of 15 or more on the face, wearing sunscreen with an SPF of 15 or more on other parts of the body, wearing a shirt with sleeves that cover the shoulders, wearing long pants, wearing a hat, wearing sunglasses, and staying in the shade. Participants indicated how often they engaged in these behaviors over the past month (1 = “Never”; 5 = “Always”). This measure was internally consistent in our sample (Cronbach’s alpha = 0.76).
UV Exposure
Participants were asked to indicate how often they engaged in five UV exposure behaviors [wearing clothes that expose the skin to the sun, sunbathing, getting a tan just by being outdoors (i.e., unintentional tanning), tanning indoors, and using products to get a faster or deeper tan] over the past month (1 = “Never”; 5 = “Always”), using a five-item scale adapted by Ingledew and colleagues (Ingledew, Ferguson, & Markland, 2010). This measure had acceptable internal consistency in our sample (Cronbach’s alpha = 0.74).
Moderators
Demographic and background
Age, sex (female vs. male), race/ethnicity (dichotomized as white non-Hispanic vs. not), first degree family history of skin cancer (yes vs. no), skin cancer risk (moderate vs. high risk on the 9-item BRAT (Glanz et al., 2003); education (dichotomized as at least a four-year college degree vs. not), and difficulty living on total income (dichotomized as 1,2 = not at all hard, somewhat hard and 3-5 = hard, very hard, extremely hard or impossible) were assessed at baseline. BRAT skin cancer risk items included personal skin cancer history (ineligible), hair and skin color, sensitivity to burning and tanning, number of moles and freckles, lifetime sunburn history, and climate of childhood residence.
Cognitive
Cognitive variables included appearance concern, health literacy, and sensation seeking and were assessed at baseline. Appearance concern was assessed using the eight-item body surveillance subscale of the Objectified Body Consciousness Scale (Cronbach’s alpha = .91), which includes items designed to assess concerns about and preoccupation with one’s appearance (McKinley & Hyde, 1996). Health literacy in terms of problems with understanding personal health information and confidence in filling out medical forms was assessed using three items adapted from Chew and colleagues (Chew, Bradley, & Boyko, 2004). This is a well-validated measure of health literacy (Chew et al., 2004). Cronbach’s alpha in our sample was 0.69. Sensation seeking or a tendency towards risky activities was assessed with three items from Harden and colleagues (Harden, Quinn, & Tucker-Drob, 2012) and one item from Whiteside and Lynam (Whiteside & Lynam, 2001). Cronbach’s alpha in our sample was 0.81.
Behavioral
Frequencies of indoor tanning in the past month and sunburn in the past month (both dichotomized as 0 vs. ≥1 time due to non-normality) were reported by participants at baseline.
Implementation Measures
Whether participants actually accessed their assigned intervention online or not was recorded automatically by the online system for all experimental and control participants. The following variables were available for the experimental condition only: the specific modules completed (e.g., skin cancer, indoor tanning, sunscreen), the number of modules completed (out of 12), and the number of modules at the end of which behavioral goals were set.
The following variables were assessed among both the experimental and control conditions via questionnaire at 3-week follow-up. The Internet Intervention Adherence Questionnaire assessed problems experienced with accessing and using the intervention program (Ritterband et al., 2008). Cronbach’s alpha in our sample was 0.93 (16 items). The Internet Evaluation and Perceived Utility Questionnaire assessed how useful, enjoyable, understandable, and easy to use participants perceived the intervention to be (Ritterband et al., 2008). Cronbach’s alpha in our sample was 0.69 (13 items). The Perceived Internet Impact and Effectiveness Questionnaire assessed the perceived helpfulness of the intervention (Ritterband et al., 2008). Cronbach’s alpha in our sample was 0.93 (12 items).
Mediators
Knowledge about skin cancer and its risk factors was measured using 11 items adapted from Buller and colleagues (Buller et al., 2006), Irwin and colleagues (Irwin, Mauriello, Hemminger, Pappert, & Kimball, 2007), and one investigator-created item (“Even if a sunscreen says it’s “water-resistant,” you still need to re-apply after swimming.”). Response options for each item were true, false, and not sure or strongly disagree to strongly agree, with each item scored as correct or not. Likert-type item responses were collapsed for scoring. For example, “People cannot die from skin cancer” was scored correctly if the response was disagree or strongly disagree. This produced a proportion correct ranging from 0 to 1 (split-half reliability = 0.83, range = 0.75-0.86).
Beliefs and attitudes
An exposure decisional balance scale was created by subtracting the average of the perceived cons of UV exposure from the pros of UV exposure. Pros of UV exposure was assessed using the appearance and health subscales of the tanning motivation measure by Ingledew and colleagues (Ingledew et al., 2010). Cronbach’s alpha in our sample was 0.91 (14 items). Cons of UV exposure was assessed using the 5-item photoaging subscale of the Physical Appearance Reasons for Tanning Scale by Cafri and colleagues (Cronbach’s alpha = 0.85) (Cafri et al., 2006). Cronbach’s alpha of the decisional balance scale was 0.89. A protection decisional balance scale was created by subtracting the average of the perceived cons of skin protection from the pros of protection. Pros of UV skin protection was assessed using the appearance and health subscales of the sun protection motivation measure by Ingledew and colleagues (Ingledew et al., 2010). Cronbach’s alpha in our sample was 0.92 (9 items). Cons of sun protection was assessed using eight items from Robinson and colleagues (N. G. Robinson et al., 2008) and nine items from Buller and colleagues (Buller, Buller, Beach, & Ertl, 1996). Cronbach’s alpha in our sample was 0.81. Cronbach’s alpha of the decisional balance scale was 0.84.
Norms
Perceived exposure and protection norms for significant others was measured using five items adapted from Hillhouse and colleagues (J. J. Hillhouse et al., 2000), Jackson and Aiken’s Sunbathing Norm Scales (Jackson & Aiken, 2006), and Ingledew and colleagues (Ingledew et al., 2010). Cronbach’s alpha in our sample was 0.80. Perceived societal norms for UV exposure and protection was assessed using three items adapted from Jackson and Aiken (Jackson & Aiken, 2006). Cronbach’s alpha in our sample was 0.81. The norms scores for society and significant others were averaged to create a final norms score. Higher scores indicate more perceived support for tanning and a tanned appearance.
Self-efficacy
Six items for assessing self-efficacy for using sun protection and avoiding UV exposure were adapted from a measure by Maddock and colleagues (Maddock, Redding, Rossi, & Weinstock, 2005). Cronbach’s alpha in our sample was 0.77.
Behavioral intention
Three items adapted from Mahler and colleagues (Mahler, Kulik, Gerrard, & Gibbons, 2010) were used to assess intentions to engage in sun protection behaviors such as wearing sunscreen. Two items were developed by the investigators to assess intentions for self and healthcare provider skin cancer examination. Cronbach’s alpha in our sample was 0.76.
Analyses
For exposure and protection outcomes at 12-week follow-up, moderation was tested using linear regression, with an interaction between treatment and each of the moderating variables assessed at baseline. We included 2 categorical indicators for treatment (control and experimental, with assessment being the referent group), so for each level of each potential moderator, there were 2 separate interaction terms (a simple contrast coding system). To avoid over-fitting, three models were fit for each outcome, where the model contained all pre-specified moderators within the category (demographics and background, cognitive, behavioral). Likelihood ratio tests were used to determine whether the overall interaction effect of treatment type and each moderator was statistically significant at p=0.05. Final models were then created containing only significant interaction terms.
Descriptive analyses of implementation variables were conducted. Linear regressions were conducted to assess potential associations between implementation variables and behavioral outcomes. These outcomes were measured as difference between baseline and 12-week follow-up exposure and protection behaviors. LASSO regression was used to identify specific modules that were most associated with intervention effects (Tibshirani, 1996). This procedure is a modification of ordinary least squares regression, which shrinks covariates toward zero, allowing the subset of most predictive variables to be chosen from a number of correlated variables, as is the case with the implementation variables.
Seven variables were assessed that could potentially mediate the effect of treatment on primary outcomes of exposure and protection behaviors. Briefly, to be considered a mediator, the following conditions must hold. 1) The treatment is correlated with outcome (exposure and protection at 12-weeks), 2) The treatment is associated with the mediator, 3) The mediator affects the outcome, and 4) After controlling for the mediator, the relationship between treatment and outcome is attenuated.
Each of the mediators were first tested separately to determine which variables were of interest. Statistically significant variables were then used in the main model, where all mediators were simultaneously tested using a multiple mediation models (Preacher & Hayes, 2008). This allowed us to estimate the total indirect effect, and account for correlation between the potential mediators. We used the product-of-coefficients approach to estimate effects, and a percentile bootstrap was used to determine significance of all indirect effects in both the single and multiple mediation models. As in other analyses, treatment was coded as a 3-level variable with the assessment only condition being the referent group, although the effects of the experimental condition were of primary interest.
Results
Descriptive data are presented in Table 1.
Table 1.
Descriptive Statistics for Variables of Interest
|
BEHAVIORAL OUTCOMES
(n = 594 with data at both baseline and 12-weeks) |
Possible
Range |
|
|---|---|---|
| Exposure, M (SD) | Baseline = 1.45 (0.79) 12 weeks = 1.09 (0.75) |
0-4 |
| Protection, M (SD) | Baseline = 1.88 (0.78) 12 weeks = 2.3 (0.90) |
0-4 |
|
MODERATORS
(assessed at baseline, n = 594 with data at both baseline and 12-weeks) |
||
| Demographic | ||
| Age in years, M (SD) | 21.98 (2.15) | 18-25 |
| Male sex, % (n) | 24 (145) | |
| White non Hispanic, % (n) | 82 (490) | |
| Family history of skin cancer % (n) | 36 (214) | |
| High risk of skin cancer, % (n) | 44 (262) | |
| College Degree, % (n) | 21 (125) | |
| Not hard to live on income, % (n) | 37 (218) | |
| Cognitive | ||
| Appearance Concern, M (SD) | 3.19 (0.74) | 1-5 |
| Health Literacy, M (SD) | 3.38 (0.69) | 0-4 |
| Sensation Seeking, M (SD) | 3.39 (0.86) | 1-5 |
| Behavioral | ||
| Indoor Tanned Last Month, % (n) | 9 (55) | |
| Sunburned Last Month, % (n) | 54 (319) | |
|
IMPLEMENTATION VARIABLES (n = 344 who accessed an intervention and had data at 12 weeks) |
||
| Accessed Intervention, % (n) | 78 (487) | |
| # of Modules Completed, M (SD) (UV4.me only) | 5.7 (5.0) | 0-12 |
| # of Goals Set, M (SD) (UV4.me only) | 7.3 (4.0) | 0-12 |
| Perceived Adherence (problems) | 1.27 (0.40) | 1-5 |
| Perceived Utility | 4.14 (0.69) | 1-5 |
| Perceived Impact | 4.20 (0.77) | 1-5 |
| MEDIATORS (assessed at 3-weeks, n = 519 with data at both 3 and 12 weeks) | ||
| Knowledge, M (SD) | 0.90 (0.17) | 0-1 |
| Exposure Decisional Balance, M (SD) | −1.53 (1.68) | −4-4 |
| Protection Decisional Balance, M (SD) | 0.99 (1.58) | −4-4 |
| Norms, M (SD) | 3.3 (0.69) | 1-5 |
| Self-efficacy, M (SD) | 3.44 (0.88) | 1-5 |
| Intentions, M (SD) | 4.12 (0.69) | 1-5 |
Moderator Results
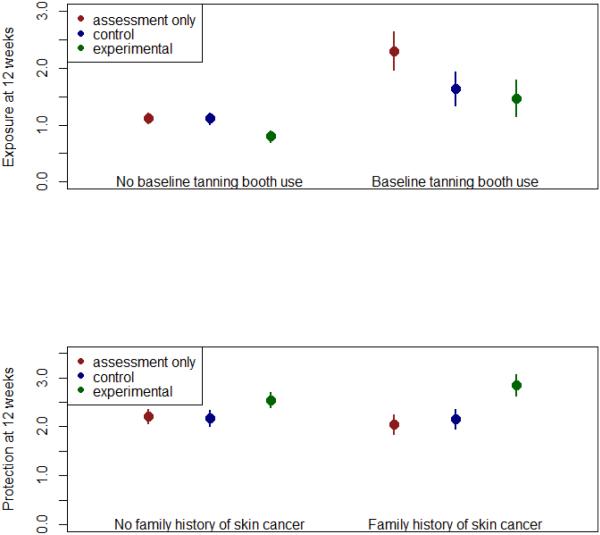
For exposure and protection outcomes at 12 weeks, 594 and 545 participants had complete data, respectively. Baseline responses were used for each moderator. Based on the regression models, in the demographics category, a family history of skin cancer was associated with greater protection at 12 weeks in the experimental arm only (interaction effect = 0.48, p=0.012). Approximately 36% of the sample reported a family history of skin cancer, and this proportion did not vary significantly by intervention condition. Family history was not associated with higher protection scores in the assessment only arm, or in the control arm. For the behavioral moderators, a significant interaction between treatment and having indoor tanned in the past month at baseline was found. In the assessment only condition, participants who reported having indoor tanned in the past month at baseline had substantially higher UV exposure scores at 12 weeks (1.18, p<0.0001) compared with those who reported no indoor tanning at baseline. However, in both the control arm and the experimental arm, this effect was attenuated (interaction effects: −0.66, −0.515, p= 0.006, 0.038, respectively). In other words, individuals who had indoor tanned in the past month at baseline reported lower UV exposure at 12 weeks in the control and experimental arms compared to the assessment only arm. See Figure 1 for a depiction of the significant moderator effects. None of the cognitive moderators demonstrated significant interaction, nor did any other demographic or behavioral moderators. However, the study may have lacked power to detect more modest effects of moderators.
Figure 1.
Moderator Results
Implementation Results
Implementation analyses included data from participants who accessed one of the interventions (i.e., not the assessment only group) and completed the 12-week follow-up questionnaire. Approximately 84% of participants randomized to the control website accessed it, and approximately 70% of experimental participants accessed the intervention materials. Participants reported spending approximately 1.5 hours on the control website and a little over 3 hours on the experimental website.
In the experimental group, approximately 32% accessed the intervention but completed no modules, and 22% completed all 12 main modules. On average, experimental participants accessed 5.8 (SD = 5.0) and completed 5.7 (SD = 5.0) out of the 12 main modules. Note that an average of only 2.7 modules was recommended to participants based on tailoring (e.g., the indoor tanning module was recommended to indoor tanners). The modules that were completed most frequently were “Why do people tan?”, “UV and health”, and “Sunless tanning” (77-90% of participants). The modules completed least often were “Skin damage”, “Shade”, and “Clothes” (45-65%).
Only approximately 6% of experimental participants set no behavioral goals (e.g., indoor tan less frequently) at the end of any module. Approximately 15% of participants set a goal at the end of all 12 modules. A greater decrease in exposure or a greater increase in protection was associated with completing more modules (t(1) = −3.96 for exposure and 2.89 for protection, ps < 0.01) and setting more goals (Wald chi-square (1) = 14.54 for exposure and 8.99 for protection, ps < 0.01).
Completion of any of nine of the twelve modules was associated with improvements in UV exposure and/or skin protection. Using LASSO selection, the modules that were most strongly associated with behavioral improvements were “Indoor tanning” and “Sunscreen” for UV exposure and “To tan or not to tan”, “Sunless tanning”, “Shade”, and “Sunscreen” for skin protection. The only modules that were not associated with behavior change were “Why do people tan?”, “Clothes”, and “Skin exams”. However, when associations between module completion and individual items rather than multi-item scales were examined, completion of the “Skin exam” module was found to be associated with greater increases in self (p = 0.003) but not provider skin examination.
Perceived intervention utility and impact were high (4.1-4.3 out of 5), and perceived intervention adherence problems were low (1.3 out of 5). Perceived intervention adherence, utility, and impact did not differ significantly between the two active intervention groups. Greater participant perception of utility or impact of both interventions was significantly associated with greater increases in skin protection (chi squares ranged from 10.57 to 20.22, ps < 0.01) but was not associated with UV exposure. Greater perceived problems with intervention adherence were associated with smaller increases in skin protection and smaller decreases in UV exposure only for experimental participants (chi square = 11.05 for exposure and 5.17 for protection, ps < 0.05).
Mediator Results
The seven potential mediators were first tested separately. For both outcomes, only the experimental treatment was significantly associated with outcome, while the control arm showed no significant differences from assessment only. Therefore, although all data was included while estimating parameters in the mediation models, all mediation effects described below are only for the experimental intervention.
For the exposure outcome, 519 participants (n = 157 in the experimental condition) had complete data on each mediator at three weeks and 12-week exposure behavior. Using independent mediation analyses, five of the six mediators met preliminary requirements to be tested in multiple mediation models: knowledge, exposure decisional balance, protection decisional balance, self-efficacy, and intentions.
In multiple mediation models (Table 3), a significant total indirect effect through these five mediators (-0.155, 95% CI: −0.256, −0.061) was found. This effect was mainly driven by two of the five mediators: knowledge and exposure decisional balance. These two variables met all criteria for mediation within the multiple mediation framework, and had statistically significant indirect effects of −0.057 (95% CI: −0.120, −0.002) and −0.076 (95% CI: −0.135, −0.027), respectively. The total effect of the experimental treatment on exposure was −0.309. Of this, −0.155 was mediated through the five variables, with a remaining direct effect of −0.154. This direct effect was still statistically significant after including the five potential mediators (p=0.031), indicating that the overall effect of the intervention was partially, but not fully, mediated by the variables described above.
Table 3.
Mediator Results (n = 519 for UV exposure and n = 478 for skin protection)
| Skin Protection | Effect | p-value |
|---|---|---|
| Total indirect effect | 0.23 | <0.001 |
| Exposure decisional balance | 0.00 | 0.958 |
| Protection decisional balance | 0.08 | 0.012 |
| Self-efficacy | 0.08 | <0.001 |
| Intentions | 0.07 | <0.001 |
| Direct effect | 0.27 | 0.004 |
| Total effect (Direct + Indirect) | 0.50 | <0.001 |
| UV Exposure | Effect | p-value |
| Total indirect effect | −0.15 | 0.004 |
| Knowledge | −0.06 | 0.044 |
| Exposure decisional balance | −0.08 | 0.004 |
| Protection decisional balance | −0.02 | 0.296 |
| Self-efficacy | −0.03 | 0.162 |
| Intentions | 0.03 | 0.072 |
| Direct effect | −0.15 | 0.031 |
| Total effect (Direct + Indirect) | −0.31 | <0.001 |
For protection, 478 participants (n = 157 in the experimental condition) had complete data on each mediator at three weeks and 12-week follow up. Using independent mediation analyses, four of the six mediators met mediation criteria: exposure decisional balance, protection decisional balance, self-efficacy, and intentions.
In multiple mediation models, a significant total indirect effect through these four mediators (0.234, 95% CI: 0.142, 0.339) was found. This effect was mainly driven by three of the four mediators: protection decisional balance, self-efficacy, and intentions. These variables met all criteria for mediation within the multiple mediation framework, and had statistically significant indirect effects of 0.080 (95% CI: 0.019, 0.161), 0.081 (95% CI: 0.031, 0.161), and 0.073 (95% CI: 0.022, 0.137), respectively. The total effect of the experimental treatment on protection was 0.505. Of this, 0.234 was mediated through the four variables, with a remaining direct effect of 0.271. This direct effect was statistically significant after including the four potential mediators (p=0.004), indicating that the overall effect of the intervention was partially, but not fully, mediated by the variables described above.
Discussion
This study’s purpose was to investigate moderator, implementation, and mediator variables associated with the efficacious UV4.me skin cancer risk reduction intervention. The national sample was at moderate to high risk for skin cancer with 54% reporting having been sunburned in the last 30 days prior to the baseline survey.
Moderators
Based on the findings from the moderator analyses for aim 1, better outcomes were reported by individuals randomized to the experimental intervention among certain high risk groups including individuals with a family history of skin cancer and those who reported indoor tanning in the last 30 days at baseline. However, this varied by behavioral outcome. Interestingly, protection was greater among individuals with a family history of skin cancer, and overall UV exposure was lower among indoor tanners. It is important to note that differences were not found for other groups such as women and men, who have less often been the focus of skin cancer prevention interventions. Similarly, though prior research has most commonly focused on college women, the current study did not find moderator effects by age, education level, difficulty living on income, or health literacy. Prior studies of moderation in skin cancer prevention interventions have focused primarily on relationship variables in dyadic interventions including patients and partners or children and parents (Hultgren, Turrisi, Mallett, Ackerman, & Robinson, 2016; Robinson, Stapleton, & Turrisi, 2008; Turrisi, Hillhouse, Robinson, Stapleton, & Adams, 2006). However, one study found that an appearance-focused workbook reduced indoor tanning specifically among low-knowledge female college indoor tanners (Stapleton, Turrisi, Hillhouse, Robinson, & Abar, 2010). In the current study, knowledge was found to be a significant mediator of intervention effects on UV exposure (see below). Another study by the same group found moderating effects of reported opiate-like reactions to tanning and dissatisfaction with natural skin tone (J. Hillhouse, Turrisi, Stapleton, & Robinson, 2010), which were not assessed in the current study.
Implementation
In terms of implementation variables included in aim 2, most participants accessed an intervention, UV4.me participants completed an average of 5.7 of the 12 available modules (which is typical for web-based health interventions (Cugelman, Thelwall, & Dawes, 2011; Kelders, Kok, Ossebaard, & Van Gemert-Pijnen, 2012) ), and most experimental participants set a behavioral goal. Completion of most of the individual modules or a greater number of modules was associated with greater improvements in exposure and/or protection outcomes.
The somewhat lower intervention access rate for the experimental intervention group overall is probably due to being required to first access instructions and items required for intervention tailoring before actually accessing the intervention materials. Within the experimental group, there are several potential reasons why participants may have completed specific modules more or less frequently than others. Each module was recommended based on responses to tailoring items. For example, if participants reported that they liked “the look of tanned skin better than untanned skin”, they were recommended to view the “Sunless tanning” module. “Why do people tan?” was recommended to all experimental participants to ensure that at least one module was recommended to everyone regardless of their responses to the tailoring items. In terms of the association of specific modules and behavior change, one of the modules that was not associated with outcomes was the “Clothes” module. A prior meta-analysis found evidence for the efficacy of behavioral interventions on sun exposure, sunburns, and sun protection in general but not for wearing protective clothing specifically (Rodrigues, Sniehotta, & Araujo-Soares, 2013). Perhaps this behavior is more difficult to modify because wearing protective clothing on hot, sunny days is unappealing. However, the “Clothes” module was also completed less often than some of the other modules, thus potentially limiting its effects on behavior.
Finally, regarding intervention implementation, participants perceived the interventions similarly favorably. Interestingly, greater participant perception of utility or impact of both interventions was significantly associated with greater improvements in skin protection but was not associated with UV exposure. Perceived problems with intervention adherence such as low motivation to use or difficulty using the website due to computer or internet problems was associated with less improvement in behavioral outcomes for the experimental group. This may have been in part because the control website had a more familiar layout and navigation scheme that is typical of an informational website, as opposed to the experimental website, which was highly interactive. The study of implementation of online interventions is especially important given the potential for cost-effective dissemination yet sometimes low observed uptake of such interventions (Cugelman et al., 2011; Kelders et al., 2012) . Few prior studies have assessed implementation of skin cancer prevention or control interventions and have found participant-perceived intervention credibility, interventionist-perceived treatment alliance, and various intervention components (e.g., viewing a video) to be associated with behavior change (C. J. Heckman et al., 2013; Lee, Weinstock, & Risica, 2008).
Mediators
For aim 3, intervention effects on UV exposure were found to be partially mediated by knowledge and exposure decisional balance; whereas, effects on protection were partially mediated by protection decisional balance, self-efficacy, and intentions. Similar to the current study, a prior study found several tanning and skin cancer related attitudes to mediate the effects of an appearance-focused workbook on indoor tanning among female college students but also identified normative beliefs as mediators (J. Hillhouse et al., 2008). It is somewhat surprising that norms were not found to be mediators in the current study given that people tan primarily for appearance enhancement and other socially-oriented reasons. Additionally, though exposure and protection are essentially “two sides of the same coin”, their mechanisms of change appear to be slightly different from one another. However, perceived pros and cons of exposure or protection were important to each. A prior study found that, although the pros of exposure or protection did not individually mediate the effects of an intervention on the protection behaviors of adolescents, their decisional balance (pros of protection minus pros of exposure) did (Adams, Norman, Hovell, Sallis, & Patrick, 2009). Self-efficacy may have emerged as a mediator of intervention effects for protection but not exposure perhaps because simply avoiding a behavior such as tanning is somewhat easier than actively engaging in a behavior such as skin protection. Additionally, the intentions scale that was used here pertained only to protection and not exposure, so it makes sense that it would mediate effects for protection only.
Study Strengths, Limitations, and Conclusions
Study strengths are that it is based on a large national RCT and assessed several different types of variables informed by theory. The limitations of the study are that it focused only on 18-25 year olds, many of whom were female. However, this is a high risk population for skin cancer risk behaviors. Additionally, the sample was recruited from a commercial research panel, though several studies have shown similar demographic representativeness and follow-up rates comparable to traditional recruitment methods (Gardner et al., 1996; West et al., 2006). Finally, self-report methods were used for outcome assessments. However, several studies have demonstrated the reliability and validity of self-report questionnaires of UV exposure and protection compared to observation and objective measures with no systematic bias identified among various populations (Glanz et al., 2010; O'Riordan et al., 2009).
In summary, the present study demonstrated better outcomes in the experimental group for high risk young adults including those with a family history of skin cancer and indoor tanners. Future studies should include more generalizable (non-commercial) samples. The study confirmed the importance of implementation variables such as engagement in (and specifically goal setting) and satisfaction with online interventions to outcomes (Crutzen et al., 2011; Cugelman et al., 2011; Kelders et al., 2012; Schubart, Stuckey, Ganeshamoorthy, & Sciamanna, 2011). The field might benefit from interventions focused on increasing the use of protective clothing (Rodrigues et al., 2013). The current study extends the prior literature on specific theoretical change mechanisms that have been investigated in RCTs related to skin cancer prevention beyond melanoma patients, parents, and female college students to young adults in general. Interventions that improve knowledge, attitudes/beliefs, and self-efficacy can improve skin cancer risk and protective behaviors.
Table 2.
Association of Module Completion with Change in Behavioral Outcomes from Baseline to 12-week Follow-up (n = 183 for UV exposure and 161 for skin protection)
| Module and Outcomes |
Participants who did not complete module |
Participants who completed module |
Difference between completers and non- completers |
p- value |
|---|---|---|---|---|
| Why do people tan? | ||||
| Change in protection | 0.45 | 0.76 | 0.31 | 0.133 |
| Change in exposure | −0.22 | −0.53 | −0.30 | 0.196 |
| UV and Health | ||||
| Change in protection | 0.25 | 0.82 | 0.57 | 0.0166 |
| Change in exposure | −0.15 | −0.56 | −0.41 | 0.0368 |
| UV and Looks | ||||
| Change in protection | 0.38 | 0.85 | 0.46 | 0.02 |
| Change in exposure | −0.21 | −0.59 | −0.38 | 0.0167 |
| Skin Cancer | ||||
| Change in protection | 0.61 | 0.80 | 0.19 | 0.2006 |
| Change in exposure | −0.30 | −0.61 | −0.31 | 0.0071 |
| Skin Damage | ||||
| Change in protection | 0.65 | 0.81 | 0.16 | 0.2293 |
| Change in exposure | −0.37 | −0.64 | −0.27 | 0.0251 |
| Indoor Tanning | ||||
| Change in protection | 0.50 | 0.87 | 0.37 | 0.0147 |
| Change in exposure | −0.22 | −0.66 | −0.43 | 0.0009 |
| To Tan or Not to Tan | ||||
| Change in protection | 0.36 | 0.86 | 0.50 | 0.006 |
| Change in exposure | −0.18 | −0.61 | −0.43 | 0.0017 |
| Sunless Tanning | ||||
| Change in protection | 0.21 | 0.84 | 0.64 | 0.0045 |
| Change in exposure | −0.28 | −0.54 | −0.26 | 0.1597 |
| Shade | ||||
| Change in protection | 0.47 | 0.91 | 0.44 | 0.0008 |
| Change in exposure | −0.31 | −0.62 | −0.32 | 0.0058 |
| Sunscreen | ||||
| Change in protection | 0.34 | 0.86 | 0.53 | 0.0054 |
| Change in exposure | −0.13 | −0.62 | −0.49 | 0.0008 |
| Clothes | ||||
| Change in protection | 0.64 | 0.80 | 0.16 | 0.2867 |
| Change in exposure | −0.37 | −0.60 | −0.23 | 0.0628 |
| Skin Exams | ||||
| Change in protection | 0.48 | 0.80 | 0.32 | 0.1179 |
| Change in exposure | −0.28 | −0.56 | −0.28 | 0.1471 |
Acknowledgements
This work was funded by R01CA154928 (CH); T32CA009035 (SD); and P30CA006927 (Cancer Center Support Grant). The study sponsor had no role in study design; collection, analysis, or interpretation of data; writing the report; or the decision to submit the report for publication. We thank Helene Conway for her assistance with manuscript preparation. LR is an equity holder of BeHealth Solutions, Inc, which developed the data management system and helped develop the intervention described in this paper. LR’s conflict of interest (COI) is being managed by a COI committee at the University of Virginia, in accordance with their respective conflict of interest policies.
References
- Adams MA, Norman GJ, Hovell MF, Sallis JF, Patrick K. Reconceptualizing decisional balance in an adolescent sun protection intervention: Mediating effects and theoretical interpretations. Health Psychology. 2009;28(2):217–225. doi: 10.1037/a0012989. doi:2009-03297-010 [pii] 10.1037/a0012989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arthey S, Clarke VA. Suntanning and sun protection: a review of the psychological literature. Social Science and Medicine. 1995;40(2):265–274. doi: 10.1016/0277-9536(94)e0063-x. doi:0277953694E0063X [pii] [DOI] [PubMed] [Google Scholar]
- Borland R, Hill DN. Being sunsmart: Changes in community awareness and reported behaviour following a primary prevention program for skin cancer control. Behaviour Change. 1990;7(3):126–135. S. [Google Scholar]
- Buller DB, Buller MK, Beach B, Ertl G. Sunny days, healthy ways: evaluation of a skin cancer prevention curriculum for elementary school-aged children. Journal of the American Academy of Dermatology. 1996;35(6):911–922. doi: 10.1016/s0190-9622(96)90115-2. [DOI] [PubMed] [Google Scholar]
- Buller DB, Cokkinides V, Hall HI, Hartman AM, Saraiya M, Miller E, Glanz K. Prevalence of sunburn, sun protection, and indoor tanning behaviors among Americans: Review from national surveys and case studies of 3 states. Journal of the American Academy of Dermatology. 2011;65(5 Suppl 1):S114–123. doi: 10.1016/j.jaad.2011.05.033. doi:S0190-9622(11)00608-6 [pii] 10.1016/j.jaad.2011.05.033. [DOI] [PubMed] [Google Scholar]
- Buller DB, Reynolds KD, Yaroch A, Cutter GR, Hines JM, Geno CR, Grandpre J. Effects of the Sunny Days, Healthy Ways curriculum on students in grades 6 to 8. American Journal of Preventive Medicine. 2006;30(1):13–22. doi: 10.1016/j.amepre.2005.08.046. doi:S0749-3797(05)00352-1 [pii] 10.1016/j.amepre.2005.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cafri G, Thompson JK, Jacobsen PB. Appearance reasons for tanning mediate the relationship between media influence and UV exposure and sun protection. Archives of Dermatology. 2006;142(8):1067–1069. doi: 10.1001/archderm.142.8.1067. doi:142/8/1067 [pii] 10.1001/archderm.142.8.1067. [DOI] [PubMed] [Google Scholar]
- Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Family Medicine. 2004;36(8):588–594. [PubMed] [Google Scholar]
- Coups EJ, Manne SL, Heckman CJ. Multiple skin cancer risk behaviors in the U.S. population. American Journal of Preventive Medicine. 2008;34(2):87–93. doi: 10.1016/j.amepre.2007.09.032. doi:S0749-3797(07)00655-1 [pii] 10.1016/j.amepre.2007.09.032. [DOI] [PubMed] [Google Scholar]
- Crutzen R, de Nooijer J, Brouwer W, Oenema A, Brug J, de Vries NK. Strategies to facilitate exposure to internet-delivered health behavior change interventions aimed at adolescents or young adults: a systematic review. Health Education and Behavior. 2011;38(1):49–62. doi: 10.1177/1090198110372878. doi:10.1177/1090198110372878. [DOI] [PubMed] [Google Scholar]
- Cugelman B, Thelwall M, Dawes P. Online interventions for social marketing health behavior change campaigns: a meta-analysis of psychological architectures and adherence factors. J Med Internet Res. 2011;13(1):e17. doi: 10.2196/jmir.1367. doi:10.2196/jmir.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings SR, Tripp MK, Herrmann NB. Approaches to the prevention and control of skin cancer. Cancer and Metastasis Reviews. 1997;16(3-4):309–327. doi: 10.1023/a:1005804328268. [DOI] [PubMed] [Google Scholar]
- Danoff-Burg S, Mosher CE. Predictors of tanning salon use: behavioral alternatives for enhancing appearance, relaxing and socializing. J Health Psychol. 2006;11(3):511–518. doi: 10.1177/1359105306063325. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Hennessy M, Yzer M, Douglas J. Can we explain why some people do and some people do not act on their intentions? Psychol Health Med. 2003;8(1):3–18. doi: 10.1080/1354850021000059223. doi:10.1080/1354850021000059223. [DOI] [PubMed] [Google Scholar]
- Gardner JS, Szpunar CA, O'Connell MJ, Facklam DP, Mariano JP, Borden EK, Leinweber FB. Cohort maintenance and comparability in a pharmacoepidemiologic study using a commercial consumer panel to recruit comparators. Pharmacoepidemiol Drug Saf. 1996;5(4):207–214. doi: 10.1002/(SICI)1099-1557(199607)5:4<207::AID-PDS190>3.0.CO;2-I. doi:10.1002/(SICI)1099-1557(199607)5:4<207::AID-PDS190>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- Glanz K, Gies P, O'Riordan DL, Elliott T, Nehl E, McCarty F, Davis E. Validity of self-reported solar UVR exposure compared with objectively measured UVR exposure. Cancer Epidemiology, Biomarkers and Prevention. 2010;19(12):3005–3012. doi: 10.1158/1055-9965.EPI-10-0709. doi:10.1158/1055-9965.EPI-10-0709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Schoenfeld E, Weinstock MA, Layi G, Kidd J, Shigaki DM. Development and reliability of a brief skin cancer risk assessment tool. Cancer Detection and Prevention. 2003;27(4):311–315. doi: 10.1016/s0361-090x(03)00094-1. doi:S0361090X03000941 [pii] [DOI] [PubMed] [Google Scholar]
- Glanz K, Yaroch AL, Dancel M, Saraiya M, Crane LA, Buller DB, Robinson JK. Measures of sun exposure and sun protection practices for behavioral and epidemiologic research. Archives of Dermatology. 2008;144(2):217–222. doi: 10.1001/archdermatol.2007.46. doi:144/2/217 [pii] 10.1001/archdermatol.2007.46. [DOI] [PubMed] [Google Scholar]
- Gordon R. Skin cancer: an overview of epidemiology and risk factors. Seminars in Oncology Nursing. 2013;29(3):160–169. doi: 10.1016/j.soncn.2013.06.002. doi:10.1016/j.soncn.2013.06.002. [DOI] [PubMed] [Google Scholar]
- Gritz ER, Tripp MK, James AS, Harrist RB, Mueller NH, Chamberlain RM, Parcel GS. Effects of a preschool staff intervention on children's sun protection: outcomes of sun protection is fun! Health Education and Behavior. 2006 doi: 10.1177/1090198105277850. [DOI] [PubMed] [Google Scholar]
- Harden KP, Quinn PD, Tucker-Drob EM. Genetically influenced change in sensation seeking drives the rise of delinquent behavior during adolescence. Dev Sci. 2012;15(1):150–163. doi: 10.1111/j.1467-7687.2011.01115.x. doi:10.1111/j.1467-7687.2011.01115.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay JL, Oliveria SA, Dusza SW, Phelan DL, Ostroff JS, Halpern AC. Psychosocial mediators of a nurse intervention to increase skin self-examination in patients at high risk for melanoma. Cancer, Epidemiology, Biomarkers and Prevention. 2006;15(6):1212–1216. doi: 10.1158/1055-9965.EPI-04-0822. [DOI] [PubMed] [Google Scholar]
- Heckman CJ, Coups EJ, Manne SL. Prevalence and correlates of indoor tanning among US adults. Journal of the American Academy of Dermatology. 2008;58(5):769–780. doi: 10.1016/j.jaad.2008.01.020. doi:S0190-9622(08)00132-1 [pii] 10.1016/j.jaad.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman CJ, Darlow S, Ritterband L, Handorf E, Manne S. Efficacy of an Intervention to Alter Skin Cancer Risk Behaviors in Young Adults. American Journal of Preventive Medicine. 2016 doi: 10.1016/j.amepre.2015.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman CJ, Zhu F, Manne SL, Kloss JD, Collins BN, Bass SB, Lessin SR. Process and outcomes of a skin protection intervention for young adults. J Health Psychol. 2013;18(4):561–573. doi: 10.1177/1359105312449193. doi:10.1177/1359105312449193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillhouse J, Turrisi R, Stapleton J, Robinson J. A randomized controlled trial of an appearance-focused intervention to prevent skin cancer. Cancer. 2008;113(11):3257–3266. doi: 10.1002/cncr.23922. doi:10.1002/cncr.23922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillhouse J, Turrisi R, Stapleton J, Robinson J. Effect of seasonal affective disorder and pathological tanning motives on efficacy of an appearance-focused intervention to prevent skin cancer. Archives of Dermatology. 2010;146(5):485–491. doi: 10.1001/archdermatol.2010.85. doi:146/5/485 [pii] 10.1001/archdermatol.2010.85. [DOI] [PubMed] [Google Scholar]
- Hillhouse JJ, Turrisi R, Kastner M. Modeling tanning salon behavioral tendencies using appearance motivation, self-monitoring and the theory of planned behavior. Health Education Research. 2000;15(4):405–414. doi: 10.1093/her/15.4.405. [DOI] [PubMed] [Google Scholar]
- Hultgren BA, Turrisi R, Mallett KA, Ackerman S, Robinson JK. Influence of Quality of Relationship Between Patient With Melanoma and Partner on Partner-Assisted Skin Examination Education: A Randomized Clinical Trial. JAMA dermatology. 2016;152(2):184–190. doi: 10.1001/jamadermatol.2015.2819. doi:10.1001/jamadermatol.2015.2819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingledew DK, Ferguson E, Markland D. Motives and sun-related behaviour. J Health Psychol. 2010;15(1):8–20. doi: 10.1177/1359105309342292. doi:15/1/8 [pii] 10.1177/1359105309342292. [DOI] [PubMed] [Google Scholar]
- Irwin B, Mauriello D, Hemminger L, Pappert A, Kimball AB. Skin sun-acne tutorial evaluation among middle- and high-school students in central New Jersey. Journal of the American Academy of Dermatology. 2007;56(3):407–412. doi: 10.1016/j.jaad.2006.11.028. doi:10.1016/j.jaad.2006.11.028. [DOI] [PubMed] [Google Scholar]
- Jackson KM, Aiken LS. Evaluation of a multicomponent appearance-based sun-protective intervention for young women: uncovering the mechanisms of program efficacy. Health Psychology. 2006;25(1):34–46. doi: 10.1037/0278-6133.25.1.34. [DOI] [PubMed] [Google Scholar]
- James AS, Tripp MK, Parcel GS, Sweeney A, Gritz ER. Psychosocial correlates of sun-protective practices of preschool staff toward their students. Health Education Research. 2002;17(3):305–314. doi: 10.1093/her/17.3.305. [DOI] [PubMed] [Google Scholar]
- Kelders SM, Kok RN, Ossebaard HC, Van Gemert-Pijnen JE. Persuasive system design does matter: a systematic review of adherence to web-based interventions. J Med Internet Res. 2012;14(6):e152. doi: 10.2196/jmir.2104. doi:10.2196/jmir.2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee KB, Weinstock MA, Risica PM. Components of a successful intervention for monthly skin self-examination for early detection of melanoma: the "Check It Out" trial. Journal of the American Academy of Dermatology. 2008;58(6):1006–1012. doi: 10.1016/j.jaad.2008.03.008. doi:S0190-9622(08)00296-X [pii] 10.1016/j.jaad.2008.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maddock JE, Redding CA, Rossi JS, Weinstock MA. Development and validation of an appearance motivation attitudes scale for sun protection. Psychology & Health. 2005;20(6):775–788. [Google Scholar]
- Mahler HI, Kulik JA, Butler HA, Gerrard M, Gibbons FX. Social norms information enhances the efficacy of an appearance-based sun protection intervention. Social Science and Medicine. 2008;67(2):321–329. doi: 10.1016/j.socscimed.2008.03.037. doi:S0277-9536(08)00181-0 [pii] 10.1016/j.socscimed.2008.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahler HI, Kulik JA, Gerrard M, Gibbons FX. Effects of upward and downward social comparison information on the efficacy of an appearance-based sun protection intervention: a randomized, controlled experiment. Journal of Behavioral Medicine. 2010;33:496–507. doi: 10.1007/s10865-010-9279-3. doi:10.1007/s10865-010-9279-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinley N, Hyde J. The objectified body consciousness scale: development and validation. Psychol. Women Q. 1996;20:181–215. [Google Scholar]
- Myers LB, Horswill MS. Social cognitive predictors of sun protection intention and behavior. Behavioral Medicine. 2006;32(2):57–63. doi: 10.3200/BMED.32.2.57-63. [DOI] [PubMed] [Google Scholar]
- Nikolaou V, Stratigos AJ. Emerging trends in the epidemiology of melanoma. British Journal of Dermatology. 2014;170(1):11–19. doi: 10.1111/bjd.12492. doi:10.1111/bjd.12492. [DOI] [PubMed] [Google Scholar]
- O'Riordan DL, Nehl E, Gies P, Bundy L, Burgess K, Davis E, Glanz K. Validity of covering-up sun-protection habits: Association of observations and self-report. Journal of the American Academy of Dermatology. 2009;60(5):739–744. doi: 10.1016/j.jaad.2008.12.015. doi:10.1016/j.jaad.2008.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson AL, Gaffney CA, Starr P, Dietrich AJ. The impact of an appearance-based educational intervention on adolescent intention to use sunscreen. Health Education Research. 2008;23(5):763–769. doi: 10.1093/her/cym005. doi:cym005 [pii] 10.1093/her/cym005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew_Research_Internet_Project Health Fact Sheet. 2014 Retrieved from http://www.pewinternet.org/fact-sheets/health-fact-sheet/ [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavioral Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Reynolds D. Literature review of theory-based empirical studies examining adolescent tanning practices. Dermatology Nursing. 2007;19(5):440–443. 447. [PubMed] [Google Scholar]
- Ritterband LM, Ardalan K, Thorndike FP, Magee JC, Saylor DK, Cox DJ, Borowitz SM. Real world use of an Internet intervention for pediatric encopresis. J Med Internet Res. 2008;10(2):e16. doi: 10.2196/jmir.1081. doi:v10i2e16 [pii] 10.2196/jmir.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson JK, Stapleton J, Turrisi R. Relationship and partner moderator variables increase self-efficacy of performing skin self-examination. Journal of the American Academy of Dermatology. 2008;58(5):755–762. doi: 10.1016/j.jaad.2007.12.027. doi:10.1016/j.jaad.2007.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson NG, White KM, Young RM, Anderson PJ, Hyde MK, Greenbank S, Baskerville D. Young people and sun safety: the role of attitudes, norms and control factors. Health Promot J Austr. 2008;19(1):45–51. doi: 10.1071/he08045. [DOI] [PubMed] [Google Scholar]
- Rodrigues A, Sniehotta FF, Araujo-Soares V. Are interventions to promote sun-protective behaviors in recreational and tourist settings effective? A systematic review with meta-analysis and moderator analysis. Annals of Behavioral Medicine. 2013;45(2):224–238. doi: 10.1007/s12160-012-9444-8. doi:10.1007/s12160-012-9444-8. [DOI] [PubMed] [Google Scholar]
- Schubart JR, Stuckey HL, Ganeshamoorthy A, Sciamanna CN. Chronic health conditions and internet behavioral interventions: a review of factors to enhance user engagement. Comput Inform Nurs. 2011;29(2 Suppl):TC9–20. doi: 10.1097/NCN.0b013e3182155274. doi:10.1097/NCN.0b013e3182155274. [DOI] [PubMed] [Google Scholar]
- Stanton WR, Janda M, Baade PD, Anderson P. Primary prevention of skin cancer: a review of sun protection in Australia and internationally. Health Promot Int. 2004;19(3):369–378. doi: 10.1093/heapro/dah310. doi:10.1093/heapro/dah310 19/3/369 [pii] [DOI] [PubMed] [Google Scholar]
- Stapleton J, Turrisi R, Hillhouse J, Robinson JK, Abar B. A comparison of the efficacy of an appearance-focused skin cancer intervention within indoor tanner subgroups identified by latent profile analysis. Journal of Behavioral Medicine. 2010;33(3):181–190. doi: 10.1007/s10865-009-9246-z. doi:10.1007/s10865-009-9246-z. [DOI] [PubMed] [Google Scholar]
- Stryker JE, Lazovich D, Forster JL, Emmons KM, Sorensen G, Demierre MF. Maternal/female caregiver influences on adolescent indoor tanning. Journal of Adolescent Health. 2004;35(6):e521–529. doi: 10.1016/j.jadohealth.2004.02.014. 528. [DOI] [PubMed] [Google Scholar]
- Tate DF, Finkelstein EA, Khavjou O, Gustafson A. Cost effectiveness of internet interventions: review and recommendations. Annals of Behavioral Medicine. 2009 doi: 10.1007/s12160-009-9131-6. doi:10.1007/s12160-009-9131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thieden E, Philipsen PA, Sandby-Moller J, Wulf HC. Sunscreen use related to UV exposure, age, sex, and occupation based on personal dosimeter readings and sun-exposure behavior diaries. Archives of Dermatology. 2005;141(8):967–973. doi: 10.1001/archderm.141.8.967. [DOI] [PubMed] [Google Scholar]
- Tibshirani R. Regression shrinkage and selection via the lasso. Journal of the Royal Statistical Society, Series B(Methodological) 1996:267–288. [Google Scholar]
- Tuong W, Cheng LS, Armstrong AW. Melanoma: epidemiology, diagnosis, treatment, and outcomes. Dermatologic Clinics. 2012;30(1):113–124. doi: 10.1016/j.det.2011.08.006. ix. doi:10.1016/j.det.2011.08.006. [DOI] [PubMed] [Google Scholar]
- Turrisi R, Hillhouse J, Robinson J, Stapleton J, Adams M. Influence of parent and child characteristics on a parent-based intervention to reduce unsafe sun practices in children 9 to 12 years old. Archives of Dermatology. 2006;142(8):1009–1014. doi: 10.1001/archderm.142.8.1009. doi:10.1001/archderm.142.8.1009. [DOI] [PubMed] [Google Scholar]
- USDHHS The Surgeon General’s Call to Action to Prevent Skin Cancer. 2014 Retrieved from Washington, DC: http://www.surgeongeneral.gov. [PubMed] [Google Scholar]
- West R, Gilsenan A, Coste F, Zhou X, Brouard R, Nonnemaker J, Sullivan SD. The ATTEMPT cohort: a multi-national longitudinal study of predictors, patterns and consequences of smoking cessation; introduction and evaluation of internet recruitment and data collection methods. Addiction. 2006;101(9):1352–1361. doi: 10.1111/j.1360-0443.2006.01534.x. doi:10.1111/j.1360-0443.2006.01534.x. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30(4):660–689. [Google Scholar]
- Williams AL, Grogan S, Clark-Carter D, Buckley E. Appearance-based interventions to reduce ultraviolet exposure and/or increase sun protection intentions and behaviours: a systematic review and meta-analyses. Br J Health Psychol. 2013;18(1):182–217. doi: 10.1111/j.2044-8287.2012.02089.x. doi:10.1111/j.2044-8287.2012.02089.x. [DOI] [PubMed] [Google Scholar]