Abstract
Aim
The aim of this systematic review and meta-analysis was to compare, in the lower third molar surgery, the osteotomy techniques with rotary instruments and piezoelectric motors.
Methods
An electronic search was conducted using the following databases: Pubmed, Web of Science, and the Cochrane Oral Health Group Trials Register. Inclusion criteria were: studies in humans, randomized or nonrandomized, comparing the extraction of third molars that required osteotomy and/or odontosection with rotary instrument and osteotomy and/or odontosection with piezoelectric motor assistance. The analysis and inclusion of articles was performed by two reviewers independently. An evaluation of the quality of articles and data extraction was carried out.
Results
From a total of nine hundred seventy four (974) trials, eleven articles were included in the qualitative analysis, and seven were included in the quantitative analysis. Rotary instruments were faster than the piezoelectric surgery (95 % CI 0.34 to 1.16). The piezoelectric surgery showed better results when compared with roatry instruments when trismus was assessed in 2 (95 % CI 0.65 to 1.69), 3 (95 % CI 0.63 to 1.67) and 5 (95 % CI 0.03 to 2.26) days after surgery. Seven days after surgery, there were no differences between the techniques (95 % CI (−0.022) to (−1.49)).
Conclusion
The piezoelectric surgery was effective in reducing pain, swelling and trismus in third molar surgery, but the same requires greater surgical time than the rotary instruments.
Keywords: Third molar, Oral surgery, Piezoeletric surgery
Introduction
Due to the high frequency of partial impaction of lower third molar in the oral cavity and the potential risk of complications such as caries [1] and development of periodontal disease [2], surgical removal of these teeth is one of the most common interventions in oral surgery [3]. The extractions of third molars are usually the most complicated, due to the positioning of these teeth in the mouth. Thus, surgical removal can be considered an invasive procedure often associated with an excessive inflammatory process, which can cause pain, swelling and trismus [4]. Furthermore, it has a negative impact on the quality of life for patients [5].
Before the development of rotary instruments, dental extractions of impacted third molars were done with chisels and hammers [6]. After the development of rotary instruments, these instruments have become more accustomed to the chisels, although there are no differences between the two techniques with respect to pain, paresthesia and postoperative infection [7]. The rotary instruments used in oral surgery can use high and low speed, with no significant differences between them with respect to pain, swelling and post-operative complications [8].
Currently, the rotary instruments have been replaced by ultrasonic instruments for osteotomy and/or odontosection in various fields of maxillofacial surgery such as orthognathic surgery [9], implantology [10, 11], sinus lifting [12], bone grafts [13] and third molar surgery [14]. This type of surgery is called piezoelectric and the surgery is performed through micro vibrations of the active tip of the piezoelectric device, which promotes osteotomy or odontosection. The great advantage of this instrument is selective tissue dissection [15]. Thus, when used in surgeries such as the sagittal osteotomy of the mandible, it prevents iatrogenic injury to the inferior alveolar nerve and adjacent soft tissues, because it uses selective cutting of the mineralized tissues [9].
In addition to the selective dissection of mineralized tissues, the piezoelectric device causes less vibration and lower noise, reducing discomfort and anxiety of the patient during the procedure [14]. However, the motor for holding the piezoelectric surgery is a costly device. The aim of this study was to compare through an approach based on scientific evidence, clinical outcomes such as pain, swelling, trismus and surgical time between osteotomy techniques and/or odontosection using rotary instrument or piezoelectric instruments in third molar surgery.
Materials and Methods
This study was based on the PRISMA protocol [16].
Aim
The purpose of this systematic review was to test the null hypothesis of no difference in clinical outcomes with respect to pain, swelling, trismus and surgical time in surgical procedures for extraction of third molars, when comparing rotary instruments with the use of the technique with piezoelectric motors.
Search Strategies
An electronic search without restrictions of time or language was held on March 31, 2015 in the following databases: PubMed, Web of Science, and the Cochrane Oral Health Group Trials Register. The terms used in the electronic search were indexed terms in MeSH.
The following terms were used in the search strategy in PubMed, refining the filter “types of articles” by selecting the following terms (Clinical Trials and Comparative Study). {Subject: (third molar [Title/Abstract]) and Adjective: (surgery OR piezosurgery OR piezo-electric surgery [Title/Abstract]). The following terms were used in the search strategy in the Web of Science. {Subject: (third molar [Title] and Adjective: (Surgery OR piezosurgery OR piezo-electric surgery [Title]) The following terms were used in the search strategy in the Cochrane Oral Health Group Trials Register: third molar AND piezosurgery.
In order to find an article in press that was not indexed, a manual search of the papers related to oral and maxillofacial surgery was also performed, including Annals of Maxillofacial Surgery, British Journal of Oral and Maxillofacial Surgery, International Journal of Oral and Maxillofacial Surgery, Journal of Oral and Maxillofacial Surgery, Medicine and Pathology, Journal of Oral and Maxillofacial Surgery, Journal of Craniofacial Surgery, Journal of Cranio-Maxillofacial Surgery, Journal of Maxillofacial and Oral Surgery, Oral Surgery Oral Medicine Oral Pathology and Oral Radiology and Oral Surgery.
After completion of the search, the reference lists of included articles were checked in order to include some additional study that was not found in the electronic search. Finally, a search on some online databases that have records of clinical trials underway was carried out (http://clinicaltrials.gov; http://www.centerwatch.com/clinical-trials; http://www.clinicalconnection.com).
Inclusion and Exclusion Criteria
Inclusion criteria were: clinical trials in humans, randomized or nonrandomized, comparing the extraction of third molars that required osteotomy and/or odontosection with rotary instruments and osteotomy and/or odontosection with piezoelectric motor assistance. To be included in the studies reviewed, it should contain at least one of the variables: pain, edema, trismus or surgical time postoperative. The study exclusion criteria included case reports, technical notes, and prospective studies evaluating only one of the surgical techniques described above, animal studies, in vitro studies and review articles.
Selection of Articles
The selection of articles was performed by two independent authors (SGFM and RAM). Firstly, reading of the titles and abstracts was performed. Studies which did not fulfill inclusion criteria were excluded at this time. Articles that seemed to fill in the inclusion criteria of this review were accessed in full. The authors read the full paper independently to verify if the inclusion criteria were achieved in each paper. If there was disagreement about inclusion of papers, a third author was consulted for final decision.
Quality Assessment of the Study
Study quality was assessed using the method of verification of risk of bias in the studies recommended by Cochrane Handbook for Systematic Reviews of Interventions [17]. This tool analyzes the included studies for identification of: election bias (Random sequence generation and Allocation concealment), performance and detection bias (Blind for patient and assessor), attrition bias (Incomplete outcome data), reporting bias (Selective reporting) and other bias. For each of these cited items the studies were classified as high risk of bias, low risk of bias or unclear risk of bias, the last one when there was not enough information for the evaluation. The final classification regarding the risk of bias was performed by two independent authors. Divergences were solved by consensus (Table 1).
Table 1.
Quality assessment of the studies included
| References | Random sequence generation | Allocation concealment* | Blinding Patient | Blinding Outcome evaluators* | Incomplete outcome data | Selective outcome reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Sortino et al. [29] | Unclear | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Barone et al. [15] | Low | Unclear | Unclear | Unclear | Low | Low | Low |
| Sivolella et al. [25] | Low | Unclear | Unclear | Low | Low | Low | Low |
| Goyal et al. [23] | Unclear | Unclear | Unclear | Low | Low | Low | Low |
| Itro et al. [30] | High | High | Unclear | Unclear | Unclear | High | High |
| Bartuli et al. [26] | Unclear | Unclear | Unclear | Unclear | Low | High | High |
| Rullo et al. [24] | Low | Low | Unclear | Unclear | Unclear | Low | Low |
| Chang et al. [27] | Low | Unclear | Unclear | Unclear | Unclear | Low | Unclear |
| Mantovani et al. [14] | Low | Unclear | Unclear | Unclear | Low | Low | Low |
| Piersanti et al. [28] | Unclear | Unclear | Unclear | Unclear | Low | Low | Low |
Data Extraction and Meta-Analysis
The following data, when available, was taken from the studies evaluated and included in the final analysis: year of publication, country of origin, study design, average age, sample size, patient age, follow-up variables analyzed, (Table 2). The mean values and standard deviation and p value of the variables pain, swelling and trismus, when available, were extracted to perform the meta-analysis. In situations where absence of any data has been verified, the authors were contacted by email. In this way the data was tabulated independently in electronic forms to perform the statistical analysis.
Table 2.
Characteristics of studies included: rotary instruments versus piezosurgery for third molar surgery
| References | Country | Study design | Mean age (years) | Total no. of patients | Follow-up (days) | Pain | Swelling | Trismus | Time of surgery | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PS | RS | RS | PS | RS | PS | RS | PS | RS | PS | ||||||
| Sortino et al. [29] | Italy | RCT | 23.2 | 24.3 | 100 | 90 | ND | ND | D1 7.04±3.45 | D1 4.22±3.21 | D1 16.76±9.11 | D1 12.52±7.99 | 17.0±7.64 | 22.92±8.88 | |
| Barone et al. [15] | Italy | RCT | 31.2 | 31.2 | 26 | 7 | D1 5.3±1.5 D3 4.1±1.0 D5 3.5±1.0 D7 1.7±1.1 |
D1 5.1±1.4 D3 3.8±1.8 D5 3.8±1.1 D7 1.6±0.77 |
ND | ND | D1 20.5±3.3 D3 19.3±3.9 D5 34.0±4.1 D7 35.6±4.5 |
D1 24.8±4.5 D3 23.3±5.3 D5 36.2±3.7 D7 38.5±3.7 |
30.5±4.4 | 34.3±7.4 | |
| Sivolella et al. [25] | Italy | RCT | 15.4 | 15.4 | 26 | 30 | ND | ND | ND | ND | D7 39.4±7.7 | D7 38.9±9.9 | 11.7±6.24 | 15.77±6.56 | |
| Goyal et al. [23] | India | RCT | 29 | 29 | 40 | 15 | D1 6.45±1.19 D3 5.70±1.56 D5 4.45±1.47 D7 2.50±1.67 |
D1 0.55±1.43 D3 2.25±1.52 D5 0.95±1.28 D7 0.20±0.41 |
D1 12.30±0.89 D3 12.36±0.96 D5 12.14±0.88 D7 11.72±0.46 |
D1 11.51±0.55 D3 11.44±0.49 D5 11.35±0.51 D7 11.27±0.45 |
D1 26.7± 10.7 D3 25.4±9.3 D5 28.9±8.0 D7 34.0±8.2 |
D1 38.2±7.9 D3 3.91± 9.9 D5 42.6±8.1 D7 44.8±8.1 |
35(11) | 45(16) | |
| Itro et al. [30] | Italy | RCT | ND | ND | 70 | 7 | ND | ND | ND | ND | ND | ND | ND | ND | |
| Bartuli et al. [26] | Italy | RCT | ND | ND | 192 | 90 | ND | ND | ND | ND | ND | ND | ND | ND | |
| Rullo et al. [24] | Italy | RCT | 26.2 | 26.2 | 52 | 6 | ND | ND | ND | ND | ND | ND | 20.67±4.46 | 28.73±5.46 | |
| Chang et al. [27] | Taiwan | RCT | ND | ND | 20 | 6 | ND | ND | ND | ND | ND | ND | ND | ND | |
| Mantovani et al. [14] | Italy | RCT | 24.02 | 24.02 | 100 | 28 | D3 6.09±2.08 D5 3.14±2.11 D7 1.27±1.87 |
D3 5.97±2.14 D5 2.81±2.13 D7 0.82±1.69 |
D7 1.10±0.04 | D7 1.02±0.02 | ND | ND | 18.74±5.69 | 20.16±7.11 | |
| Piersanti et al. [28] | Italy | RCT | 22.4 | 22.4 | 10 | 7 | ND | ND | D7 3.1±0.39 | D7 2.75±0.23 | ND | ND | 30.8±6.1 | 36.8±10.6 | |
ND not declared, RCT randomized controlled trial, D1 day 1, D2 day 2, D3 day 3, D4 day 4, PS Piezosurgery, RS Rotary instrument
The software program Comprehensive Meta-Analysis Software, version 2, was used for the meta-analysis [18]. The heterogeneity of studies was performed using the I2 test [19]. A sensitivity test was conducted when heterogeneity was above 50 % [20]. When homogeneity was present (I2 = 0.00), the fixed effect model was used. When heterogeneity was present (I2 > 0), the random effects model was used for meta-analysis [19, 20]. Risk measures, 95 % confidence interval (CI) and p value were described in a forest plot, and summary measures of risk were calculated. As there were not enough studies to be grouped into a funnel plot [21, 22], publication bias was not assessed.
Results
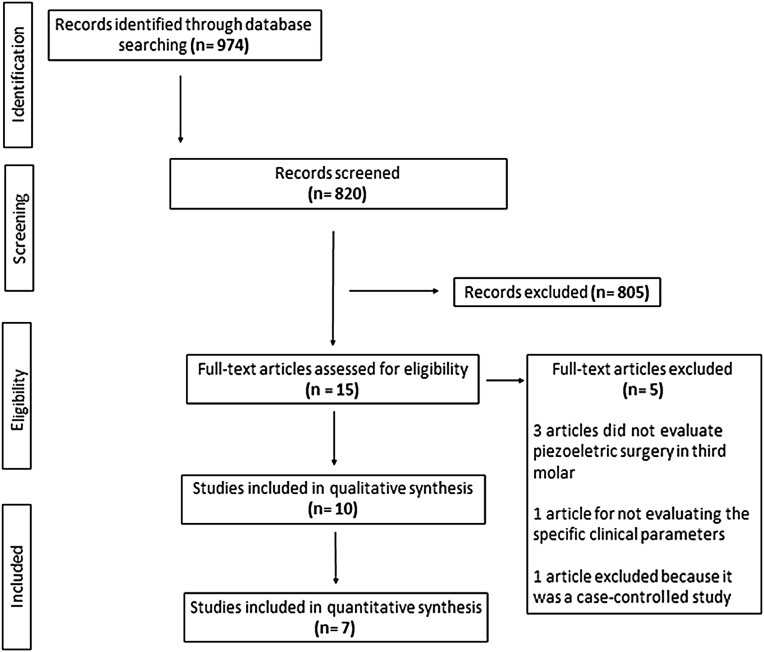
A total of nine hundred seventy-four (974) papers were identified from the databases. A study was included after searching the cross-references. One hundred fifty-four (154) studies were duplicated in the search for data, resulting in a total of eight hundred and twenty (820) studies identified in the databases. Two different evaluators read the titles and abstracts to identify articles related to the issue focus. After reading the title and abstract, eight hundred and five (805) articles were excluded and fifteen (15) were selected to read in full. From these fifteen (15) articles, a total of five articles were excluded after reading the full text. Ten (10) articles were included in the final qualitative analysis and seven (7) were included in the quantitative analysis (Fig. 1). Of the ten (10) papers included in this systematic review, five (5) showed low risk of bias for “Random sequence generation”, only one (1) showed low risk of bias for “Allocation concealment”, all papers showed unclear risk of bias for “Blinding patient”, only two (2) showed low risk of bias for “Blinding outcome for evaluators”, seven (7) showed low risk of bias for “Incomplete outcome data”, eight (8) showed low risk of bias for “Selective reporting outcome” and six (6) showed low risk of bias for “Other bias” (Table 1).
Fig. 1.
Process conducted for the selection of articles included in the review
Pain
This variable was evaluated in eight (8) of the ten (10) studies included in the systematic review. The meta-analysis showed a high heterogeneity among the studies, even after the completion of sensitivity tests, showing no consistency among the results. Among the studies that evaluated postoperative pain compared to the use of piezoelectric motor and the use of osteotomy with rotary instruments, four (4) had results favoring the use of piezoelectric motor [14, 15, 23, 24]. The other four (4) studies showed no statistically significant differences between the methods evaluated [25, 28].
Edema
It was not possible to perform a quantitative analysis for the variable edema due to differences between the methodologies used across studies, variations between the dates and methods of measurement. Of the seven (7) studies that evaluated the edema, six (6) showed favorable results for the use of the piezoelectric motor for the removal of third molars, because they have less swelling after surgery at different measurement times of 1, 2, 3, 5 and 7 days postoperative [14, 15, 23, 28–30]. In one study, there was no statistical difference between the piezoelectric motor and the rotary instruments [27].
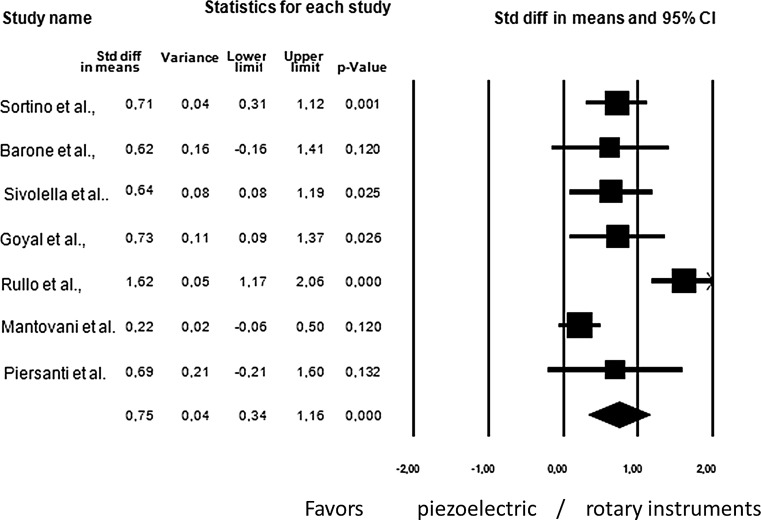
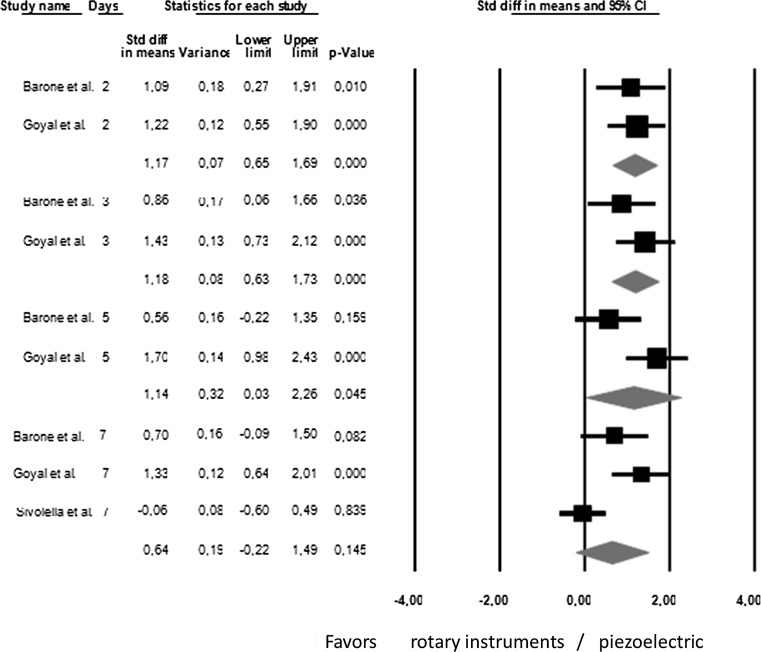
Trismus and Surgical Time
Through the meta-analysis, it was only possible to compare trismus variables [15, 23, 25] and surgical time [14, 15, 23–25, 28, 29]. A total of three hundred and sixty-four (364) subjects were enrolled in the meta-analysis for surgical time. Figure 2 shows the meta-analysis of studies comparing the use of piezoelectric versus rotary instruments in third molar surgery. The use of rotary instruments is faster than the piezoelectric third molar surgery in surgery (95 % CI 0.34–1.16). A total of ninety-two (92) subjects were enrolled in the meta-analysis for trismus. The piezoelectric surgery showed better results when compared with rotary instruments in third molar surgery when trismus was evaluated in 2 days (95 % CI 0.65 to 1.69); 3 days (95 % CI 0.63 to 1.73); 5 days (95 % CI 0.03 to 2.26) after surgery. Seven days after surgery, there were no differences between the techniques (95% CI −0.22 to 1.49) (Fig. 3).
Fig. 2.
A meta-analysis comparing the two surgical techniques regarding surgical time; I2 = 78.3, the random effect model used
Fig. 3.
Meta-analysis comparing the two surgical techniques evaluating trismus, I2 = 00:00 − 79.67, random effect model used
Discussion
Surgery for the removal of third molars through the use of piezoelectric motors seems to be a viable alternative compared to rotary instruments. Current efforts in dentoalveolar surgery endeavour to obtain less morbid results, faster healing times and less interference with the quality of life of patients who must undergo these procedures [4, 31]. Thus, the present review aimed at evaluating the variables pain, swelling, trismus and surgical time compared to rotary instruments and piezoelectric. However, the methodological quality of the selected studies was unclear in most of the papers. The “Allocation concealment” was not always reported and the “Blinding outcome” of the evaluators was unclear in most studies. The authors recognize that the blinding of the surgeon and the subjects was not possible due to the characteristics of the study. However, the postoperative valuer could be blinded for the technique used. This should have been performed and reported in the papers.
Among the studies included in this systematic review, eight (8) contemplated the variable pain [14, 15, 23–28]. Although the meta-analysis was not recommended due to the high heterogeneity among the study results, five (5) of them had results favoring the use of piezoelectric motor, when the pain was evaluated. The other three (3) studies showed no significant differences between the results. Pain is one of the worst feelings reported by the patient after surgery of third molars, directly affecting the quality of life of patients in the postoperative period. Moreover, the greater postoperative pain increases analgesic consumption, resulting in a more expensive treatment [15]. One of the justifications for the better performance of piezoelectric motors when the pain was evaluated, is due to these engines mechanism of action. The micrometer oscillations of the piezoelectric motor allows a more selective cutting of bone structures, which reduces unnecessary tissue damage, thereby reducing the episodes of pain [23, 32]. A confounding factor that may have influenced the heterogeneity between the results of these studies may have been the surgical time. In third molar surgery, surgical time and surgical difficulty are directly proportional to the postoperative pain experience [33]. Thus, the variation between the surgical procedure, the surgeon’s experience and surgical difficulty may have varied among studies, leading to heterogeneity of the results. Another confounding factor associated with the evaluation of postoperative pain is the subjectivity of pain. On the other hand, studies that evaluated pain used a standardized scale to an internationally accepted measurement; this variable is the VAS (visual analogic scale).
As well as in variable pain, it was not possible to perform meta-analysis to evaluate the edema between studies. However, in this variable, the reason was the methodological differences between the studies. The differences between the evaluation periods and how to measure the edema between studies was crucial not to perform the statistical analysis. A total of seven (7) studies evaluated the edema [14, 15, 23, 27–30]. Of these, seven showed better results for the use of the piezoelectric motor in the lower third molar surgery, than rotary instruments. Only one study showed no significant differences between the results [27]. Swelling and pain are signals indicating inflammation. Thus, the reason to better results with the use of piezoelectric motors than rotary instruments is basically the same. The selective cutting of tissue can provide fewer trauma, with less release of inflammatory chemical mediators, thereby producing less pain and swelling than rotary instruments [32]. Another study showed a low rate of facial swelling, or even a lack of facial swelling in more than 70 % of the cases analyzed with the use of piezoelectric motors when compared with rotary instruments [29]. However, the results with respect to facial swelling must be analyzed carefully. The high heterogeneity between results and employed methodological differences can give us false-positive results. Edema is a difficult variable to be measured, and measurement bias may be present, even with the calibration of the examiners, since it is a three-dimensional evaluation, with two-dimensional resources [34].
Trismus is a complication associated with extraction of third molars. Clinical trials related to the third molar extraction has evaluated a trismus variable in an attempt to minimize this postoperative complication [4]. In this meta-analysis, the trismus variable was subjected to meta-analysis, evaluating the results found in three studies [15, 23, 25]. The results of this meta-analysis were favorable to the use of the piezoelectric motor when compared to rotary instruments 2, 3 and 5 days postoperatively (Fig. 3). On the seventh postoperative day, there was no difference between the use of piezoelectric motor and the rotary instruments. This result can be explained by the increased amount of inflammatory agents in the wound area until the third day, showing regression of the inflammatory process in both cases on the seventh postoperative day, which is expected in third molar surgery. Thus, it can be seen that the amount of inflammation produced by the use of the piezoelectric motor is smaller than the rotary instruments, as trismus is directly proportional to tissue damage.
Another variable closely related to postoperative complications in third molar surgery is the operating time. The operating time is directly proportional to the amount of inflammation caused since more time is spent to remove a third molar, probably causing a greater inflammatory response. Interestingly, the present meta-analysis showed that the surgeries performed with piezoelectric motors are more time-consuming than with rotary instruments. However, they showed lower levels of inflammation with respect to swelling, pain and trismus. It is valid to emphasize that piezoelectric surgery is a relatively new technique, where the learning curve may have been instrumental in increasing the time to perform the procedure, compared to the rotary instruments.
Recently a systematic review on the subject was published [35]. Apparently, the two works were carried out at the same time as can be see in the search strategy section. Despite the similarity between the two revisions, we find that the search strategy was different between overhauls, presenting a discrepancy between the number of studies initially included. This review started with a total of nine hundred seventy-three (973) studies, while the other started with three hundred twenty-five (325) studies. In this systematic review, it included three articles that compared the rotary instrument and other techniques, but did not show as drawing the Clinical Trial Randomized Controlled. However, the authors were careful not to include these studies in the meta-analysis which could be attributed to heterogeneity in the results. Thus, these studies were analyzed descriptively, which makes the results of this review broader. There were differences between the meta-analysis of the two studies. This study used a specific tool for performing the meta-analysis, which gives greater credibility on results achieved, while in another review the program used was Stata [35], a statistical generic program. It is worth noting that the formula used by the programs is different, which can cause a difference between the results achieved. Another aspect to be highlighted is the inclusion of the assessment of heterogeneity I2 in all captions.
The results of this systematic review showed that the piezoelectric surgery was more effective than the use of rotary instruments when comparing pain, swelling and trismus, in third molar surgeries. On the other hand, more surgical time was spent to perform piezoelectric surgery. However, due to the quality of trial found, these results should be interpreted with caution.
Compliance with ethical standards
Ethical standards
As this work is a systematic review and meta-analysis, the ethical approval in an ethics committee is not necessary.
Conflicts of interest
The authors state that there are no conflicts of interest in this paper.
Informed consent
As this research did not involve human beings, informed consent was not necessary.
References
- 1.Falci SG, de Castro CR, Santos RC, de Souza Lima LD, Ramos-Jorge ML, Botelho AM, dos Santos CR. Association between the presence of partially erupted mandibular third molar and the existence of caries in the distal of the second molars. Int J Oral Maxillofac Surg. 2012;41:1270–1274. doi: 10.1016/j.ijom.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Nunn ME, Fish MD, Garcia RI, Kaye EK, Figueroa R, Gohel A, Ito M, Lee HJ, Williams DE, Miyamoto T. Retained asymptomatic third molars and risk for second molar pathology. J Dent Res. 2013;92:1095–1099. doi: 10.1177/0022034513509281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Renton T, Smeeton N, McGurk M. Factors predictive of difficulty of mandibular third molar surgery. Br Dent J. 2001;190:607–610. doi: 10.1038/sj.bdj.4801052. [DOI] [PubMed] [Google Scholar]
- 4.Alcântara CE, Falci SG, Oliveira-Ferreira F, Santos CR, Pinheiro ML. Pre-emptive effect of dexamethasone and methylprednisolone on pain, swelling, and trismus after third molar surgery: a split-mouth randomized triple-blind clinical trial. Int J Oral Maxillofac Surg. 2014;43:93–98. doi: 10.1016/j.ijom.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 5.Slade GD, Foy SP, Shugars DA, Phillips C, White RP., Jr The impact of third molar symptoms, pain, and swelling on oral health-related quality of life. J Oral Maxillofac Surg. 2004;62:1118–1124. doi: 10.1016/j.joms.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 6.Royer RQ. Use of the chisel in the removal of impacted mandibular third molars. J Oral Surg. 1969;27:26–31. [PubMed] [Google Scholar]
- 7.Absi EG, Shepherd JP. A comparison of morbidity following the removal of lower third molars by the lingual split and surgical bur methods. Int J Oral Maxillofac Surg. 1993;22:149–153. doi: 10.1016/S0901-5027(05)80240-1. [DOI] [PubMed] [Google Scholar]
- 8.Campbell JH, Murray RA. Handpiece speed and postoperative outcomes in third molar surgery. J Indiana Dent Assoc. 2004;83:4–6. [PubMed] [Google Scholar]
- 9.Monnazzi MS, Real Gabrielli MF, Passeri LA, Cabrini Gabrielli MA, Spin-Neto R, Pereira-Filho VA. Inferior alveolar nerve function after sagittal split osteotomy by reciprocating saw or piezosurgery instrument: prospective double-blinded study. J Oral Maxillofac Surg. 2014;72:1168–1172. doi: 10.1016/j.joms.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 10.Bassetti R, Bassetti M, Mericske-Stern R, Enkling N. Piezoelectric alveolar ridge-splitting technique with simultaneous implant placement: a cohort study with 2-year radiographic results. Int J Oral Maxillofac Implants. 2013;28:1570–1580. doi: 10.11607/jomi.3174. [DOI] [PubMed] [Google Scholar]
- 11.da Silva Neto UT, Joly JC, Gehrke AS. Clinical analysis of the stability of dental implants after preparation of the site by conventional drilling or piezosurgery. Br J Oral Maxillofac Surg. 2014;52:149–153. doi: 10.1016/j.bjoms.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 12.Camargo Filho GP, Corrêa L, Costa C, Pannuti CM, Schmelzeisen R, Luz JG. Comparative study of two autogenous graft techniques using piezosugery for sinus lifting. Acta Cir Bras. 2010;25:485–489. doi: 10.1590/S0102-86502010000600005. [DOI] [PubMed] [Google Scholar]
- 13.Mouraret S, Houschyar KS, Hunter DJ, Smith AA, Jew OS, Girod S, Helms JA. Cell viability after osteotomy and bone harvesting: comparison of piezoelectric surgery and conventional bur. Int J Oral Maxillofac Surg. 2014;43:966–971. doi: 10.1016/j.ijom.2013.11.018. [DOI] [PubMed] [Google Scholar]
- 14.Mantovani E, Arduino PG, Schierano G, Ferrero L, Gallesio G, Mozzati M, Russo A, Scully C, Carossa S. A split-mouth randomized clinical trial to evaluate the performance of piezosurgery compared with traditional technique in lower wisdom tooth removal. J Oral Maxillofac Surg. 2014;72:1890–1897. doi: 10.1016/j.joms.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Barone A, Marconcini S, Giacomelli L, Rispoli L, Calvo JL, Covni U. A randomized clinical evaluation of ultrasound bone surgery versus traditional rotary instruments in lower third molar extraction. J Oral Maxillofac Surg. 2010;68:330–336. doi: 10.1016/j.joms.2009.03.053. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89:873–880. [PubMed] [Google Scholar]
- 17.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. http://www.cochrane-handbook.org
- 18.Borenstein M, Hedges LV, Higgins J, Rothsten H. Comprehensive meta-analysis version 2. Englewood: Biostat; 2005. [Google Scholar]
- 19.Higgins JP, Thompson SG. Quantifying heterogeneity in meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 20.Borensterin M, Hedges LV, Higgins J, HR Rothstein. Introduction to meta-analysis. Chichester: Wiley; 2009. [Google Scholar]
- 21.Biljana M, Jelena M, Branislav J, Milorad R. Bias in meta-analysis and funnel plot asymmetry. Stud Health Technol Inform. 1999;68:323–328. [PubMed] [Google Scholar]
- 22.Egger M, Davey SG, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goyal M, Mrya K, Jhamb A, Chawala S, Sonoo PR, Singh V, Aggarwal A. Comparative evaluation of surgical outcome after removal of impacted mandibular third molars using a Piezotome or a conventional handpiece: a prospective study. Br J Oral Maxillofac Surg. 2012;50:556–561. doi: 10.1016/j.bjoms.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 24.Rullo R, Addaboo F, Papaccio G, D’Aquino R, Festa VW. Piezoelectric device vs. Conventional rotative instruments in impacted third molar surgery: relationships between surgical difficulty and postoperative pain with histological evaluations. J Craniomaxillofac Surg. 2013;41:33–38. doi: 10.1016/j.jcms.2012.07.007. [DOI] [PubMed] [Google Scholar]
- 25.Sivolella S, Berengo M, Bressan E, Di Fiore A, Stellini E. Osteotomy for lower third molar germectomy: randomized prospective crossover clinical study comparing piezosurgery and conventional rotator osteotomy. J Oral Maxillofac Surg. 2011;69:15–23. doi: 10.1016/j.joms.2010.12.036. [DOI] [PubMed] [Google Scholar]
- 26.Bartuli FN, Luciani F, Caddeo F, De Chiara L, Di Dio M, Piva P, Ottria L, Arcuri C. Piezosurgery vs High Speed Rotatory Handpiece: a comparison between the two techniques in the impacted third molar surgery. Oral Implantol (Rome) 2013;6:5–10. [PMC free article] [PubMed] [Google Scholar]
- 27.Chang HH, Lee MS, Hsu YC, Tsai SJ, Lin CP. Comparison of clinical parameters and environmental noise levels between regular surgery and piezosurgery for extraction of impacted third molars. J Formos Med Assoc. 2015;114:929–935. doi: 10.1016/j.jfma.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 28.Piersanti L, Dilorenzo M, Monaco G, Marchetti C. Piezosurgery of conventional rotator instruments for inferior third molar extractions? J Oral Maxillofac Surg. 2014;72:1647–1652. doi: 10.1016/j.joms.2014.04.032. [DOI] [PubMed] [Google Scholar]
- 29.Sortino F, Pedullà E, Masoli V. The piezoelectric and rotatory osteotomy technique in impacted third molar surgery: comparison of postoperative recovery. J Oral Maxillofac Surg. 2008;66:2444–2448. doi: 10.1016/j.joms.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 30.Itro A, Lupo G, Marra A, Carotenuto A, Cocozza E, Filipi M, D’Amato S. The piezoeletric osteotomy technique compared to the one with rotatory instruments in the surgery of included third molars. A clinical study. Minerva Stomatol. 2012;61:247–253. [PubMed] [Google Scholar]
- 31.Lopez-Lopez J, Jan-Pallí E, González-Navarro B, Jané-Salas E, Estrugo-Devesa A, Milani M. Efficacy of chlorexidine, dexpanthenol, allantoin and chitosan gel in comparison with bicarbonate oral rinse in controlling post-interventional inflamation, pain and cicatrization in subjects undergoing dental surgery. Curr Med Res Opin. 2015;15:1–16. doi: 10.1185/03007995.2015.1108909. [DOI] [PubMed] [Google Scholar]
- 32.Beziat JL, Bera JC, Lavandier B, Gleizal A. Ultrasonic osteotomy as a new technique in craniomaxillofacial surgery. Int J Oral Maxillofac Surg. 2007;36:493–500. doi: 10.1016/j.ijom.2007.01.012. [DOI] [PubMed] [Google Scholar]
- 33.Lago-Mendez L, Diniz-Freitas M, Senra-Rivera C, Gude-Sampedro F, Gándara Rey JM, García-García A. Relationship between surgical difficulty and postoperative pain in lower third molar extractions. J Oral Maxillofac Surg. 2007;65:979–983. doi: 10.1016/j.joms.2006.06.281. [DOI] [PubMed] [Google Scholar]
- 34.Grossi GB, Maiorana C, Garramone RA, Borgonovo A, Beretta M, Farronato D, Santoro F. Effect of submucosal injection of dexamethasone on postoperative discomfort after third molar surgery: a prospective study. J Oral Maxillofac Surg. 2007;65:2218–2226. doi: 10.1016/j.joms.2006.11.036. [DOI] [PubMed] [Google Scholar]
- 35.Jiang Q, Qiu Y, Yang J, Chen M, Zhang Z. Piezoeletric versus conventional rotatory techniques for impacted third molar extraction: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 2015;94:1685. doi: 10.1097/MD.0000000000001685. [DOI] [PMC free article] [PubMed] [Google Scholar]