Abstract
Introduction
Access osteotomies provide direct exposure to inaccessible areas of the deep part of craniofacial skeleton for treating pathologies involving vital structures. The use of maxillary swing approach for gaining wide access to the nasopharynx, infratemporal fossa, parapharyngeal space, middle fossa of skull base. Though the maxillary swing requires transfacial incision for wide exposure but with careful handling the scar is minimum and this approach can be used in young people.
Materials and Methods
Surgical resection is carried out following preoperative embolization of the involved feeder vessels. Total 16 cases were considered for this study.
Results
This article highlights cases successfully treated in our institution, the mention of complications associated with the cases along with management.
Conclusion
Maxillary swing is a good approach for getting access to the deep pathologies like JNA.
Keywords: Angiofibroma, Vascular tumor, Maxillary swing, Embolization
Introduction
Maxillary swing approach gives wide access to Skull base, Nasopharynx, Pterygopalatine fossa and pterygomaxillary fissure. The approach was first described by Wei et al. in 1991 [1]. The incision used for this approach is Weber Fergusion with Dieffenbach extension, but other modifications can be used based on the location of the pathology. Juvenile Nasopharyngeal angiofibroma (JNA) is a benign vascular tumor that arises in the tissues in the sphenopalatine foramen. Clinical features include nasopharyngeal mass causing nasal obstruction and repeated bleeding [2].
The lesion is currently presumed to arise in the pterygopalatine fossa region and may proliferate into the surrounding anatomic area. The site of origin of the tumor is supposed to be from the superior margin of the sphenopalatine foramen. The JNA can grow into the inferior and superiororbital fissures causing erosion of the greater wing of the sphenoid bone and can extend up to the cavernous sinus [3]. Dependingon the extension of the tumor staging of JNA is done, the revised staging of JNA [4] is as shown in Table 1.
Table 1.
Revised staging of JNA as per Metin et al
| Stage | Description |
|---|---|
| I | Extension to the nose, nasopharyngeal vault, and sphenoid sinus |
| II | Extension to the maxillary sinus or the anterior cranial fossa, full occupation of the pterygo maxillary fissure, limited extension to the infratemporal fossa, or the pterygoid plates posteriorly |
| III | Deep extension into the cancellous bone at the base of the pterygoid or the body and the greater wing of the sphenoid, significant extension to the infratemporal fossa or pterygoid plates posteriorly or orbital region, and obliteration of cavernous sinus |
| IV | Intracranial extension between the pituitary gland and internal carotid artery, tumor extension posterolateral to the internal carotid artery, and extensive intracranial extension |
The surgical modality of treatment remains the gold standard; however the approach is decided by tumor size, location, extent and surgical expertise. Biopsy is generally not indicated in these cases due to risk of profuse bleeding. Complications reported with the procedure are excessive hemorrhage, trismus and prominent scar, persistent nasal crusting, facial paresthesia, lacrimal apparatus injuries and recurrence [5].
Materials and Methods
Total of 14 cases were considered for study aged between 06 and 27 years. The retrospectivestudy was carried out from 2007 to 2013 at our institution and total 14 male patients weretreated by a single surgeon. Standard surgical procedure was carried out. All cases were diagnosed cases of JNA with Type II variety in 13 cases and type III in 01 case. Right side was involved in 12 cases and left side in 2 cases. The extension of swing was decided based on the extent of involvement. All patients were subjected to histopathological examination of excised specimen confirming diagnosis of JNA. All the patients were followed for 1 year.
Surgical Procedure
Patient was planned for surgery under general anesthesia. As JNA is known to be associated with high vascularity it was decided to do pre operative embolization. The transfemoral route for embolization was selected. Digital Subtraction angiography was carried out. The mask image and contrast enhanced images were compared and the multiple feeders from the maxillary or from external carotid artery were seen. Polyvinyl alcohol beads were used to embolise the feeders. Embolization of the main artery was avoided and only feeders were embolised in most of the cases. The size used was between 200 and 400 microns. After embolising all the feeders the patient was shifted to ward. Patient was advised complete bed rest for 48 h. Patient was taken for surgery after confirming no complications due to embolization. (Figure 1). Weber Ferguson incision with subciliary extension was marked. Soft tissues were divided, including branches of the labial and angular branches of the facial artery. The skin and soft tissues under the incision were not elevated more than a few millimeters laterally over the anterior surface of maxilla. Care was taken to maintain all soft tissue attachments intact on the anterior surface of the maxilla without significant undermining. The alveolar and nasal processes of the bony maxilla were exposed, without extensive subperiosteal dissection. The subciliary incision was placed, and approximately 1-cm wide skin flap raised superficial to the orbicularis oculi muscle. The orbicularis oculi muscle was incised was then retracted cephalad to expose the bony orbital rim without opening the orbital septum, with dissection continuing laterally over the zygomatic arch. Surgical marking of osteotomy site was done predetermining the position by fixing bone plate and screw drill. Osteotomy was done in the anterior maxillary wall involving alveolar process, nasal process of maxilla and infraorbital rim, zygomatic arch and hard palate. Infraorbital nerve was transected or retracted depending on the access. Maxillary swing was achieved and was pedicled on cheek and masseter muscle (Fig. 2). Near total tumor excision was done using direct and endoscopic excision (Fig. 3). After the excision the osteotomised segments were fixed back using mini plates and screws (Fig. 4). A layered closure was done and palatal splint was positioned.
Fig. 1.
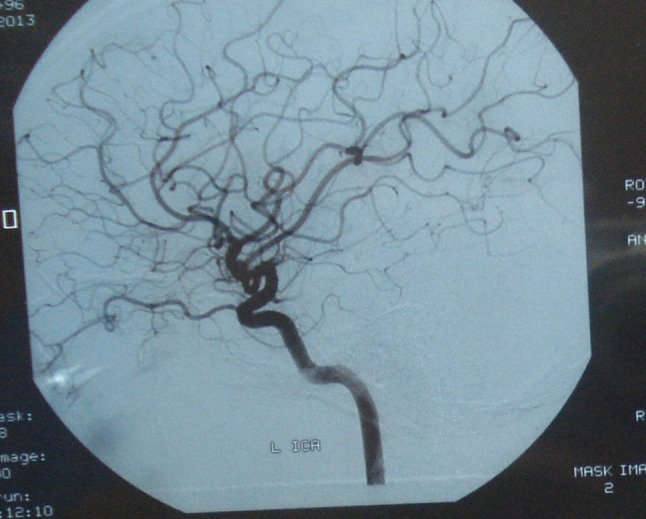
Multiple feeders in DSA
Fig. 2.
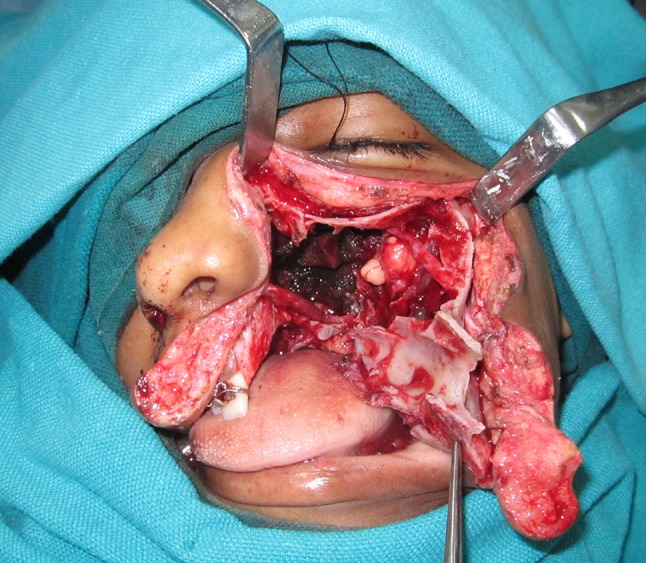
Access to tumor using maxillary swing
Fig. 3.
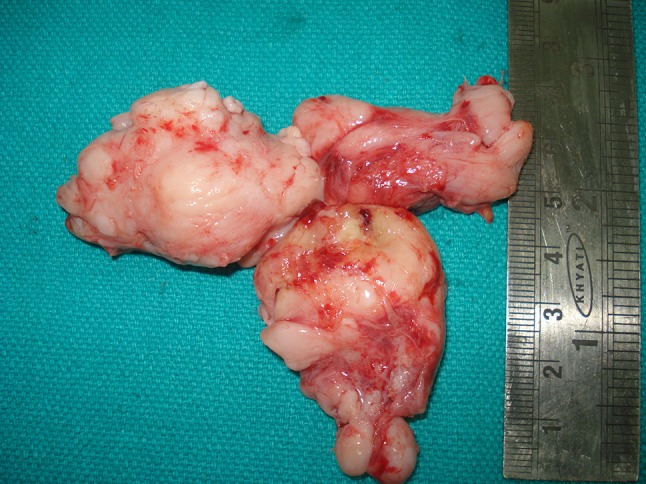
Excised tumor mass
Fig. 4.

Fixation
Results
Most of the patients had uneventful immediate postoperative period. The complications noted in the study are as mentioned in Table 2.
Table 2.
List of complication following maxillary swing for excision of JNA
| Sr no | Complication noted | Number of cases |
|---|---|---|
| 1 | Infraorbital nerve paresthesia | 14 |
| 2 | Dacrocystitis | 0 |
| 3 | Bad scar | 2 |
| 4 | Palpability of implants | 3 |
| 5 | Oronasal communication | 3 |
| 6 | Allergic rhinitis | 0 |
| 7 | Damage to tooth buds | 0 |
| 8 | Non union/mal union or unfavorable fractures | 0 |
| 9 | Hemorrhage from internal carotid artery | 0 |
| 10 | Atrophy of the soft tissue and cutaneous closure | 0 |
| 11 | Dysphagia, | 0 |
| 12 | Velopharyngeal incompetence | 0 |
| 13 | Choanal stenosis | 0 |
| 14 | Dental malocclusion | 2 |
| 15 | Osteoradionecrosis of the skull base | 0 |
| 16 | Necrosis of the maxilla | 0 |
| 17 | Recurrence | 4 |
Discussion
JNA mostly is found in adolescents males. Females are rarely affected by this condition. This suggests that there is some relation of male hormones particulary testosterone and JNA [6, 7]. Clinically patients presented with complaints like epistaxis, anosmia and facial swelling. There are various theories concerning the etiology of JNA. Chmielik et al. defined JNA as an angioma with an extended fibrous component. In the development of the lesion, the involvement of pituitary gland- gonad axis is suggested as causative factor [8]. Latest opinions suggest JNA as developmental defect which is affecting the embryonic vascular network surrounding the sphenoid bone [9].
JNA is a highly vascular tumor. In our cases blood supply in most of the tumors was from the feeders of internal maxillary artery, external carotid artery, the internal carotid artery, the common carotid artery, and ascending pharyngeal artery. JNA can cause unpredictable bleeding. So angiography for carrying out embolization is a generally indicated in JNA cases [10]. Embolization was carried out in all 14 cases 24–48 h before the surgery so as to reduce the bleeding [11]. Pre operative selective embolization of feeding vessels was done to reduce bleeding and to reduce the morbidity associated with JNA surgery [12]. Complications of embolization may range from oronasal fistula to occlusion of important arteries like central retinal artery and consequent temporary blindness, occlusion of middle cerebral artery followed by stroke, and occlusion of ophthalmic artery [13]. Also some experts believe that due to embolization surgeon may not be able to remove the complete lesion and due to that the chance of recurrence increases.
These tumors are non encapsulated tumors and spread submucosally diagnosis of JNA is a difficult task as biopsy is generally avoided. CT scan and MRI are very essential and valuable tools for diagnosis of JNA [14]. Certain characteristic CT scan findings like Antral Bowing Sign also known as Holman-Miller sign assist in diagnosis [3]. Magnetic resonance imaging due to ability to define borders of lesions remains diagnostic method of choice [15].
JNA cases are treated mainly by surgical modalities which may include endoscopic approach or open surgical approach like Weber Fergusson approach with lateral subciliary extension incision. Most commonly used approaches are Le fort I Maxillotomy, Maxillary swing and Medial maxillectomy. Endoscopic transnasal approach has advantages of no non-cosmetic sequel, less hemorrhage and no disruption in facial skeleton. Some prefer endoscopic approach for less extensive tumours due to high advantage of cosmetic results and as less morbidity is involved [16]. Still endoscopic approach has limitations as more extensive tumors cannot be removed using this approach, but combining endoscopic surgery with external approaches is increasingly being used. The combination of endoscopic and open approaches for advanced tumors allows better visualization of the lesion and facilitates total removal [17]. Maxillary swing technique allowed easy access to the deep placed tumor without damaging nearby vital structures. The subciliary incision can result in complications such as ectropion of lower eye lid, epiphora and oedema due to lymphatic obstruction. For maxillary swing incision we used Weber Ferguson incision. The block removal of maxillary bone and reinsertion approach provides maximal exposure of nasopharynx, but may affect the facial growth.
There are many complications associated with maxillary swing ranging from severe hemorrhage to trismus. The derangement of occlusion can be a chronic problem associated with the technique. In our cases the most complications reported were infraorbital nerve paresthesia in all patients, recovery and improvement was noted in ten patients after 6–8 months, while 04 cases even after 1 year paresthesia persisted. In few patients palatal fistula was a consistent finding. The management of the fistula was done by using local flap with two layered closure and with regional flap using tongue (Fig. 5). All patients with palatal fistula were successfully managed with these techniques. Also modifications as described by Ng RW and Wei WI [18] where they avoided the midline incision can be used to reduce the chances of palatal fistula formation. Embolization should only be carried out when tumour is large in size and feeding vessel evaluation by digital subtraction method reveals major vessel supplying the tumour. Many authors have proved that without embolization one can treat JNA and embolization may cause recurrence [19]. Palpability of implants due to soft tissue thinning was seen in one case, which was managed by removing the implants under local anesthesia. Bad scar was observed in 02 cases, for which scar revision surgery was done and good results were achieved. Recurrence was observed in 04 cases (28.57 %) which is significantly lower than that observed in other studies [20]. For recurrence radiation therapy was advised by the joint discussion with ENT department. Dental malocclusion was observed in 02 cases which were in the form of open bite on ipsilateral side and occlusal canting. Orthodontic treatment modalities were used to correct the problem.
Fig. 5.

Post-op Oro nasal fistula following maxillary swing
Conclusion
Even though the list of possible complications associated with Maxillary swing using Weber Ferguson is quite extensive still most of the patients in our study had acceptable results. The severe complications were avoided by careful handling of tissues and other complications were managed by secondary surgical corrections or Orthodontic treatment modalities.
Compliance with Ethical Standards
Conflict of interest
The authors declared that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Wei WI, Lam KH, Sham JS. New approach to the nasopharynx: the maxillary swing approach. Head Neck. 1991;13(3):200–207. doi: 10.1002/hed.2880130306. [DOI] [PubMed] [Google Scholar]
- 2.Gohar MS, Rashid D, Ahmed B. Common presenting symptoms diagnosis and management of angiofibroma—a study of twenty cases. Pak J Med Sci. 2004;20:377–380. [Google Scholar]
- 3.Stokes SM, Castle JT. Nasopharyngeal angiofibroma of the nasal cavity head and neck. Pathol. 2010;4:210–213. doi: 10.1007/s12105-010-0181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Metin Ö, Oguz Ö, Taskın Y. Juvenile nasopharyngeal angiofibroma: a revised staging system. Rhinology. 2006;44:39–45. [PubMed] [Google Scholar]
- 5.Wanamaker JR, Lavertu P, Levine HL. Juvenile angiofibroma. In: Kraus DH, Levine HL, editors. Nasal neoplasia. New York: Thieme; 1997. pp. 61–84. [Google Scholar]
- 6.Andrade NA, Andrade JSC, Silva PDM, Oliveira VB, Andrade BB. Nasopharyngeal angiofibroma: review of the genetic and molecular aspects. Int Arch Otorhinolaryngol (São Paulo) 2008;12:442–449. [Google Scholar]
- 7.Mendenhall WM, Werning JW, Hinerman RW, Amdur RJ, Villaret DB. Juvenile nasopharyngeal angiofibroma: review article. J HK Coll Radiol. 2003;6:15–19. [Google Scholar]
- 8.Chmielik LP, Frackiewicz M, Krajewski R, Woloszczuk-Gebicka B, Chmielik M. Perioperative problems and treatment of a teenager with a juvenile angiofibroma refusing blood transfusion. Int J Pediatr Otorhinolaryngol. 2009;73(5):689–692. doi: 10.1016/j.ijporl.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 9.Hodges JM, et al. Nasopharyngealangiofibroma: current treatment modalities and future considerations. Indian. J Otolaryngol Head Neck Surg. 2010;62(3):236–247. doi: 10.1007/s12070-010-0073-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ungkanont K, Byers RM, Weber RS, et al. Juvenile nasopharyngeal angiofibroma: an update of therapeutic management. Head Neck. 1996;18:60–66. doi: 10.1002/(SICI)1097-0347(199601/02)18:1<60::AID-HED8>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 11.Gupta G, Thakar A, Grover M. Nasomaxillary swing—a novel approach for the Bilateral Angiofibroma. Clin Rhinol Int J. 2009;2(3):33–36. doi: 10.5005/jp-journals-10013-1007. [DOI] [Google Scholar]
- 12.Mann WJ, Jecker P, Amedee RG. Juvenile angiomas: changing surgical concept over the last 20 years. Laryngoscope. 2004;114:291–293. doi: 10.1097/00005537-200402000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Andrade NA, Pinto JA, NóbregaMde O, Aguiar JE, Aguiar TF, Vinhaes ES. Exclusively endoscopic surgery for juvenile nasopharyngeal angiofibroma. Otolaryngol Head Neck Surg. 2007;137:492–496. doi: 10.1016/j.otohns.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Ahmed Z, Mutiullah S, Rahim D, Marfani MS. Juvenile nasopharyngeal angiofibroma: stage and surgical approach. Jlumhs. 2009;8:37–40. [Google Scholar]
- 15.Atalar M, Solak O, Müderris S. Juvenıle nasopharyngeal angiofibroma: radiologic evaluation and pre-operative embolization. KBB Forum. 2006;5:58–61. [Google Scholar]
- 16.Carrau RL, Snyderman CH, Kassam AB. Juvenile angiofibroma. In: Myers EN, editor. Operative otolaryngology—head and neck surgery. Philadelphia, PA: WB Saunders, Elsevier; 2008. pp. 39–49. [Google Scholar]
- 17.Nicolai P, Berlucchi M, Tomenzoli D, et al. Endoscopic surgery for juvenile angiofibroma: when and how. Laryngoscope. 2003;113:775–782. doi: 10.1097/00005537-200305000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Ng RW, Wei WI. Elimination of palatal fistula after the maxillary swing procedure. Head Neck. 2005;27(7):608–612. doi: 10.1002/hed.20220. [DOI] [PubMed] [Google Scholar]
- 19.Fonseca AS, Vinhaes E, Boaventura V, Andrade NA, Dias LA, Medeiros V, Coifman F. Surgical treatment of non-embolized patients with nasoangiofibroma. Braz J Otorhinolaryngol. 2008;74:583–587. doi: 10.1016/S1808-8694(15)30607-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCombe A, Lund VJ, Howard DJ. Recurrence in Juvenile nasopharyngeal angiofibroma. Rhinology. 1990;28:97–102. [PubMed] [Google Scholar]


