Abstract
Introduction
Eosinophilic colitis, which is a rare form of eosinophilic gastrointestinal diseases, occurs as primary and secondary allergic eosinophilic colitis of the gastrointestinal tract infection, inflammatory bowel disease, celiac disease, and vasculitis. The diagnosis is based on a significant amount of eosinophils in the inflammatory infiltrate of the colon wall.
Aim
To analyze the clinical picture taking into account comorbidities and endoscopic picture in children with eosinophilic colitis.
Material and methods
The test group consisted of 43 children, the average age – 12.1 years diagnosed with eosinophilic colitis (according to the Whitington scale) hospitalized in the Gastroenterology Unit, Department of Pediatrics of the Medical University of Silesia in Katowice. Testing for food allergies, celiac disease, inflammatory bowel disease, gastrointestinal diseases and parasitic diseases was performed in the group of children and the analysis concerned the intensity of eosinophilic infiltration of the colon mucosa with the severity of clinical symptoms, endoscopic picture, the presence of inflammatory bowel disease, and food allergy.
Results
Half of the tested children suffered from isolated eosinophilic colitis but the rest of them had eosinophilic infiltrate with inflammatory bowel disease more often, however, the Crohn’s disease. The endoscopic image was uncharacteristic, and grade III in the Whitington scale was predominant in the histopathological examination, in most cases located in the entire large intestine. The higher level of total IgE was found in less than half of the patients and it did not correlate with the severity of eosinophilic infiltration. It was shown that the severity of eosinophilic infiltration correlated with exacerbation of clinical symptoms, endoscopic image, and the presence of inflammatory bowel disease. The higher level of antibodies of ASCA and ANCA was found in approximately 20% of the children with isolated eosinophilic colitis and 63% of children with Crohn’s disease.
Conclusions
The higher concentration of total IgE in less than half of the patients with eosinophilic colitis indicates the need for improving allergy diagnosis also in terms of IgE-independent allergy. The presence of higher levels of antibodies of ASCA and ANCA in some of the patients with isolated eosinophilic colitis indicates the need for further observation for the occurrence of inflammatory bowel disease.
Keywords: eosinophilic colitis, children
Introduction
Under physiological conditions, eosinophils are commonly found in the alimentary tract, but their complex role is only being recognized [1]. Eosinophilic colitis is a rare form of eosinophilic gastrointestinal diseases (EGIDs). The first description of eosinophilic gastrointestinal diseases was made by Kaijser in 1937 [2].
In 1970, Klein et al. classified eosinophilic gastrointestinal diseases into three types: mucosal, muscular, and serosal [3]. The mucosal type is the most common, and the endoscopic image in this form of the disease is not specified: from the proper one to inflammatory changes in the form of vascularity loss, edematous mucosa, its hyperemia and softening, erosions, ulceration. In the muscular type, infiltration of the muscle membrane is associated with constriction and obstruction of the gastrointestinal tract. The least common form of eosinophilic gastrointestinal diseases is the serosal one, which is characterized by ascites, and eosinophilic infiltration in serosal and ascitic fluid. The EGID diagnosis depends on the clinical symptoms and the degree and location of eosinophilic infiltration [4]. The Whitington scale is used to assess the degree of eosinophilic infiltration of the intestinal wall [5].
Diarrhea and abdominal pain are the main clinical symptoms of eosinophilic gastrointestinal diseases [6, 7]. Atopy is a genetic predisposition to IgE-mediated reaction. Several studies support a connection between atopy and EGIDs. Atopy is common in this patient group – it concerns 75–80% of EGIDs patients [8, 9]. However it is possible that the severity of EGIDs can be dependent on following allergen-free diet [9].
The diagnosis of eosinophilic colitis among infants is the most common, and here eosinophilic colitis occurs in the form of allergic inflammation of the colon in response to cow’s milk protein or can be associated with other atopic conditions (primary form), and also among adolescents and young adults (secondary form) in the course of other diseases of the gastrointestinal tract [4, 10, 11]. Eosinophils are also a part of the inflammatory infiltrate in inflammatory bowel disease, although, they are a small part of leukocytes, both their presence and the amount is a bad prognostic rating in this disease [12].
The concentration of protein from eosinophil granules (eosinophilic cationic protein – ECP) in the gut fluid of patients with inflammatory bowel disease (IBD) is increased comparing to the healthy control group [13].
Aim
The aim of this study is a retrospective analysis of the clinical picture taking into account comorbidities and endoscopic picture in children with eosinophilic colitis.
Material and methods
The retrospective study involved 43 children diagnosed with eosinophilic colitis, hospitalized from 2004 to 2013 in the Gastroenterology Unit, Department of Pediatrics of the Medical University of Silesia in Katowice.
The diagnosis was based on histopathological examination of the samples taken from the mucosa of the colon with eosinophilic infiltration > 20 eos/HPF (the Whitington scale).
The test group consisted of 20 girls and 23 boys aged from 7 months to 18 years (average age was 12.1 years).
The test group was divided: 1) based on age: group I – 17 children aged 7 months – 12 years (average age: 6.9 years), group II – 26 children aged 13–18 years (average age: 15.5 years); 2) based on clinical diagnosis: group I – isolated eosinophilic colitis (IEC) – 23 (53.5%) patients, group II – eosinophilic colitis in the course of Crohn’s disease (EC + CD) – 11 (25.6%) patients, group III – eosinophilic colitis in the course of ulcerative colitis (EC + UC) – 7 (16.3%) patients, group IV – eosinophilic colitis accompanied by lymphocytic colitis (EC + LC) – 2 (4.6%) patients.
Abdominal pain, diarrhea (watery or bloody) and weight loss were the most common clinical symptoms in the group of children. The assessment of the body weight was based on the percentile rank of body mass index (BMI), where the body underweight was diagnosed with BMI of < 3 pcn; the normal body weight: BMI 3–97 pcn; the increased body weight: BMI > 97 pcn [14]. Colonoscopy and gastroduodenoscopy with samples taken from mucosa were performed for all the children. Macroscopic evaluation of changes was done in the mucosa of the colon, basing on the Schroeder scale [15].
Histological biopsies taken were evaluated using: the Marsh scale to evaluate changes in the duodenum [16], the Whitington scale to evaluate the degree of eosinophil infiltration of the colon mucosa [17].
The degree of the disease activity in the case of IBD was evaluated using the Pediatric Ulcerative Colitis Activity Index for patients with UC and the Pediatric Crohn’s Disease Activity Index for patients with CD [18].
Laboratory testing research in serum was performed for all patients:
tests for food allergy: total IgE and food-specific IgE on selected food products (milk protein, white and yolk of eggs, wheat flour) – using the chemiluminescence method,
tests for celiac disease: IgA tTG – using the ELISA method, IgG EmA – using IF method, when IgA deficiency was found
total IgA – using immunoturbidimetric method,
IgA and IgG ASCA, p-ANCA – using the ELISA method,
IgG Ascaris lumbricoides – using the ELISA method.
Markings were made in the laboratory in the Upper Silesian Child Health Centre in Katowice.
Statistical analysis
Statistical analysis of the results was made using: test for Spearman’s rank correlation coefficient, which verifies the importance of the relationship between a pair of ordinal variables, Mann-Whitney rank-sum test verifying the hypothesis of the differences between the results obtained in two independent groups.
Relations for which the p-value was < 0.05 were considered statistically significant.
Results
Patients’ demographic data
Most of the study group consisted of children aged > 12 years of age – 58.14%. Isolated eosinophilic colitis was observed in boys twice more often, boys also dominated in CD (54.5%), while UC was dominant among girls (71.4%).
Clinical symptoms in the children tested group
Diarrhea was the most common clinical symptom in the analyzed group of patients. It occurred in almost all patients with isolated eosinophilic colitis (36.4% – bloody diarrhea, 45.5% – watery diarrhea).
Bloody diarrhea was observed in the majority of children with UC (71.4%) and in half of the children with CD (45.5%).
Abdominal pain was the second common clinical symptom. It appeared in half of the whole study group (53.5%), regardless of the clinical group. Weight loss was reported as the third symptom among patients, but underweight was found only in 9 (20.93%) patients.
The great majority of children with isolated eosinophilic colitis were in the normal body weight range – 82.61%, only 13.04% of them were underweight.
CD was most often accompanied by body underweight (45.5%) (Table 1).
Table 1.
Clinical symptoms in the children tested group
| Clinical symptoms | N (%) | Abdominal pain | Watery diarrhea | Bloody diarrhea | BMI [pcn] | ||
|---|---|---|---|---|---|---|---|
| < 3 | 3–97 | > 97 | |||||
| IEC | 23 (53.5) | 12 (54.5%) | 10 (45.5%) | 9 (39.13%) | 3 (13%) | 19 (82.6%) | 1 (4.4%) |
| EC + CD | 11 (25.6) | 6 (54.6%) | 1 (9.1%) | 5 (45.4%) | 5 (45.4%) | 6 (54.6%) | 0 |
| EC + UC | 7 (16.3) | 3 (42.9%) | – | 5 (71.4%) | 0 | 7 (100%) | 0 |
| EC + CLM | 2 (4.6) | 2 (100%) | 1 (50%) | – | 1 (50%) | 1 (50%) | 0 |
| Sum | 43 | 23 (53.5%) | 12 (27.9%) | 19 (44.2%) | 9 (21%) | 33 (77%) | 1 (2%) |
Degree of eosinophilic infiltration by the Whitington scale
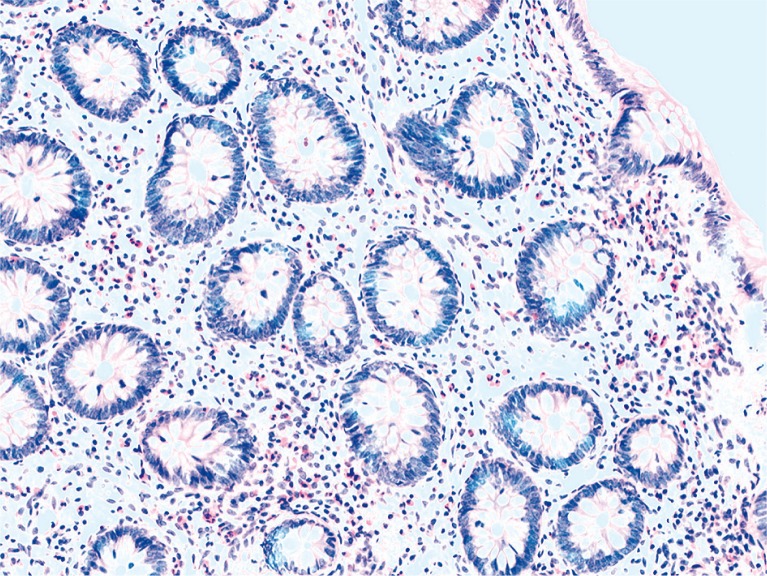
Degree II of eosinophilic infiltration was observed in 9 (20.93%) children, and in the majority it appeared in children with isolated eosinophilic colitis. Degree III was dominant in the study group and it occurred in 29 (60.46%) children, especially with CD (90.9% of them) and lymphocytic colitis (100%). Degree IV occurred in 5 (11.62%) children, in individual cases in each clinical group (Table 2, Figure 1).
Table 2.
Degree of eosinophilic infiltration of the colon mucosa in children
| Whitington scale | II degree | III degree | IV degree |
|---|---|---|---|
| IEC | 8 (34.78%) | 13 (56.52%) | 2 (8.70%) |
| EC + CD | – | 10 (90.9%) | 1 (9.09%) |
| EC + UC | 1 (14.28%) | 4 (57.14%) | 2 (28.57%) |
| EC + LC | – | 2 (100%) | – |
| Summary | 9 (20.93%) | 29 (60.46%) | 5 (11.62%) |
Figure 1.
Isolated eosinophilic colitis – III degree (Whitington scale)
Assessment of macroscopic changes in the large intestine by the Schroeder scale in the group of children
The correct image of colon mucosa in macroscopic assessment was presented by 16 (37.2%) tested patients. Mild changes in endoscopy were found in 18 (41.86%) patients. Moderate macroscopic mucosal changes were described in only 9 (20.93%) patients. 91.31% of patients with isolated eosinophilic colitis presented normal or minimally changed colon mucosa. Four (36.36%) children with CD had significant inflammatory changes in endoscopy (moderate form).
The same number of tested children with CD presented only minimal changes, whereas in 3 (27.27%) patients, the image was correct (the location in the small intestine). Almost half of the children (42.85%) with UC presented moderate intensity changes and the same number – mild changes.
No severe changes among patients were ascertained (3 points in the Schroeder scale).
Statistical analysis of clinical symptoms and endoscopic changes in the group of children, due to the eosinophilic infiltration (Table 3)
Table 3.
Statistical analysis showing relations of eosinophilic infiltration and clinical symptoms as well as macroscopic changes in colonic mucosa in the group of patients
| Whitington scale | N | R Spearman | P-value |
|---|---|---|---|
| BMI [pcn] | 43 | –0.27 | 0.0428 |
| Abd. pain + bloody diarrhea | 43 | –0.26 | 0.0488 |
| Schroeder scale | 43 | 0.32 | 0.0174 |
The severity of the clinical symptoms (abdominal pain and bloody diarrhea) and the presence of body underweight correlate with eosinophilic infiltration of the colonic mucosa among patients in the study group.
There was a statistically significant correlation between the severity of macroscopic changes in the mucosa of the colon (assessed by the Schroeder scale) and the degree of eosinophilic infiltration (Whitington scale).
Analysis of immunological tests
The higher levels of total IgE occurred in 17 (39.53%) patients, including less than half of the patients with isolated eosinophilic colitis (43.47%), and another half with CD (54.5%), and only 14.2% of patients with UC.
The positive reaction of IgE dependent on specific food allergen (food-specific IgE) was found in 5 patients (3 patients with IEC). Particular children had a higher level of food-specific IgE of two or more allergens, usually cow’s milk and egg white protein. In children with lymphocytic colitis a total IgE level was normal (Table 3).
Antibodies of ASCA (IgA or/and IgG) occurred in the higher titer in 10 (23.25%) patients, especially in children with CD. The higher concentration of antibodies in the isolated eosinophilic colitis was found in 4 (17.39%) cases. In case of antibodies of ANCA, higher levels were found in only 2 children with CD and in 1 child with isolated eosinophilic colitis (Table 4).
Table 4.
Evaluation of higher total and food-specific IgE, IgA, IgG ASCA and pANCA in children with eosinophilic colitis
| Colitis | Elevated total IgE | Food-specific IgE positive | IgA or/and IgG ASCA positive | PANCA positive |
|---|---|---|---|---|
| IEC | 10 (43.47%) | 3 (13.63%) | 4 (17.39%) | 1 (4.3%) |
| EC + CD | 6 (54.54%) | 1 (16.66%) | 6 (54.54%) | 2 (18.2%) |
| EC + UC | 1 (14.28%) | 1 (14.28%) | – | – |
| EC + LC | – | – | – | – |
| Total | 17 (39.53%) | 5 (11.62%) | 10 (23.25%) | 3 (6.97%) |
In all cases, the higher levels of antibodies (ASCA/ANCA) occurred in the patients with degree III and IV of eosinophils infiltration on the Whitington scale.
The serum level of IgA tTG was normal in all of the children.
Distribution of eosinophilic infiltration along the colon
The most pathological eosinophilic infiltration occurred along the entire colon – 55.2%. Growing eosinophilic infiltration along the colon (from the right to left colon side) was described only in 5 (17.2%) children. However, segmental density was found in 30% of the patient tested group, in an isolated eosinophilic colitis in 34.7%, in UC in 42.85%.
Disease development according to the PCDAI and PUCAI scale
In the tested group, 18 (41.8%) patients with IBD were described. Among them, the majority of children (12; 66.6%) had a moderate form of the disease, the severe form was found in one patient with UC.
Eosinophilic colitis in the course of inflammatory bowel disease
The higher degree of eosinophilic infiltration by the Whitington scale in the children with IBD (CD, UC) was shown in comparison to the children with isolated eosinophilic colitis, this correlation was statistically significant (p-value < 0.05) (Table 5).
Table 5.
Analysis of eosinophilic infiltration (by the Whitington scale) in the children with inflammatory bowel disease in the tested group
| Whitington scale | Isolated eosinophilic colitis | Inflammatory bowel disease |
|---|---|---|
| Sum of rank | 434.00 | 512.00 |
| N | 23 | 20 |
| R1–R2 | –78 | |
| m | 66.00 | |
| σ | 82.14 | |
| u | –1.75 | |
| P-value | 0.0398 | |
Discussion
Eosinophilic gastrointestinal disease is more often recognized in the Western World, however, it is still a very rare disease when relating to colon [4]. Male dominance is what draws attention in the literature [18, 19]. Similarly, in our research, boys were the vast majority of patients. If eosinophilic colitis occurs in the first year of life, prognosis is very good [7].
At after-infant age, incidence of eosinophilic colitis affects most commonly adolescents and young adults [7]. Age of the patients did not correlate with the degree of colon eosinophilic infiltration. In the research of DeBrosse et al., the average age of patients with eosinophilic colitis was 10.78 and also did not correlate with the degree of eosinophilic infiltration in the colon and in any part of the gastrointestinal tract [20].
However, the average age of the patients treated by Behjati et al. was much lower and was 6.5 years old [21]. In the study group, more than a half of children were in the age group > 12, the average age was 12.1. The older average age of the tested group is probably connected with a significant percentage of children suffering from the inflammatory bowel disease.
Abdominal pain, diarrhea, weight loss are the clinical symptoms of eosinophils colitis [7].
DeBrosse et al., drew attention to abdominal pain as the most common symptom in patients [20].
Similarly, in the analysis of children with colonic eosinophilia carried out by Pensabene, 75% of patients complained of abdominal pain, almost 60% of diarrhea, while half of them had bloody stools [8]. An 8-year-old girl described by Iwańczak experienced abdominal pain and loose stools with blood [22].
In our research, diarrhea was observed in nearly all patients of the study group, more than half of them had bloody diarrhea, and half of the patients suffered from abdominal pain. Weight loss in treated children with eosinophilic colitis was not significant in our analysis.
Children with normal weight were the vast majority, children with CD were mainly underweight. A statistically significant correlation between the degree of colon mucosa eosinophilic infiltration and the severity of clinical symptoms was found.
Similarly, Liacouras et al. claim that the degree of eosinophilic infiltration in eosinophilic gastrointestinal disease correlates with clinical symptoms and severity of the disease. Clinical symptoms are reported to be a direct consequence of tissue eosinophilic infiltration [23]. In the study of Czaja-Bulsa et al., in examined children there was a pathological infiltration in the cecum and the ascending colon with different intensity in other sections, in one patient, the arrangement was described along the entire intestine [19].
Examining 38 children, Behjati et al. observed a decrease in the eosinophilic infiltration degree from the cecum to the rectum [21]. In the research of Debrosse et al., intestine had the highest concentration of eosinophilic infiltration in the ascending colon, a lower concentration was observed in the transverse and the terminal ileum, and the smallest in the rectum [20]. Most often pathological eosinophilic infiltration of mucosa was found along the entire colon in the study group, segmental growing density was observed in 1/3 of patients. However, in the clinical study by Behjati et al., in 38 ill children, there was no correlation between density of infiltration and disease symptoms, allergy and macroscopic picture of the colon [21]. According to Lee et al., a correct macroscopic picture of eosinophilic gastrointestinal disease is not rare, so microscopic assessment of biopsies is essential [24]. Segmental nature of the inflammatory changes requires the analysis of numerous biopsies from each change, also macroscopically normal intestine [18].
In the group of examined children, in the macroscopic colonic mucosa picture assessed by the Schroeder scale, a normal picture or benign lesions appeared, whereas moderate changes occurred only in children with inflammatory bowel disease.
There was a statistically significant correlation between the degree of eosinophilic infiltration and severity of changes in endoscopy, which is probably a result of a significant proportion of children with inflammatory bowel disease.
Etiology of eosinophilic colitis is unknown, the disease may be of idiopathic characteristics or it may coexist with food allergy, infection or inflammatory bowel diseases.
It was shown that 50–75% of eosinophilic colitis coexists with allergic diseases, especially food allergy to cow’s milk protein, soy, peanuts, and the elimination diet is not usually sufficient for treatment [25]. The existence of eosinophils in the large intestine mucosa is quite common in children [8]. The significant eosinophilia in colon which is associated with the higher level of total IgE indicates that eosinophilic colitis is an allergic phenomenon [25].
Atopy was recognized in 5 of 6 patients treated by Czaja-Bulsa et al., but 2 of them suffered from allergic disease. In our research, the higher levels of total IgE was found in half of all patients with isolated eosinophilic colitis and with CD in most cases. However, only 20% had higher levels of food-specific IgE caused mainly by cow’s milk protein, eggs, wheat, and chicken. There was no statistically significant correlation between the intensity of colon eosinophilic infiltration and the higher concentration of total IgE in serum.
The concentration of IgE associated with the present allergen stimulation does not reflect the tissue concentration at the location of ongoing allergic inflammation [25]. Therefore, the question how the higher serum of IgE in children with eosinophilic colitis is associated with local inflammation in the gastrointestinal tract is still valid and remains without a clear answer. The cause of eosinophilic colitis may also be IgE-independent allergy, while according to Yan and Shaffer, most of the colon eosinophilic inflammation is associated with IgE-independent mechanism [1]. According to Inamura et al., mast cell accumulation and degranulation in colonic tissue of patients with eosinophilic colitis is related to the role of IgE in eosinophilic colitis [26]. Diagnosis of IBD should be based on history, physical and laboratory examination, esophagogastroduodenoscopy and ileocolonoscopy with histology, and evaluation of the small bowel condition especially important in suspected CD, UC with atypical presentations, and unclassified IBD [27]. Both the clinical picture of eosinophilic colitis and IBD highlight the presence of non-specific symptoms especially at the beginning of the disease, so it is important to search for minimally invasive diagnostic methods.
Bloody diarrhea is the most common symptom in UC. Crohn’s disease is rather presented by abdominal pain, diarrhea, anemia, fever, weight loss, or growth retardation.
The diagnosis of UC is based on presence of the inflammation of colon mucosa (typically continuous mucosal inflammation of the colon, starting from the rectum, without small bowel involvement, and without granulomas on biopsy or atypical variants of pediatric UC), erythema, granularity, friability, purulent exudates and ulcers in colonoscopy, and exclusion of both CD and infections [28–30]. Ulcers and cobblestoning are typical in CD [31]. Unclassified IBD (IBDU) concerns patients with definite IBD, where the inflammation is limited to the colon with features that make the differentiation between UC and CD uncertain even after a complete diagnostic process [32].
Saccharomyces cerevisiae antibodies ASCA and neutrophils cytoplasm antibodies p-ANCA have the greatest importance in serological IBD diagnosis [33].
Authors of a report of a Moroccan family in which five members developed IBD concluded that serological markers of IBD (ASCA, ASCAg, ALCA, ANCA) and genetic variants in CARD15, TLR4, NOD1, CARD18, DLG5 had no effect on the occurrence of IBD in the test group [34]. Additionally report authors expected that other environmental factors (not sanitation) are responsible for development of IBD in that family. Our earlier researches proved specificity of ASCA antibodies for CD and p-ANCA for UC. Authors observed presence of p-ANCA and ASCA in almost half of patients with allergic colitis [35]. ASCA is found more often in CD (50–70%) than in UC (10–15%) and healthy controls (< 5%) [36, 37]; these antibodies increase with age [38] and are associated with a more severe disease course in CD [39, 40]. ASCA positivity is not typically present in isolated eosinophilic colitis. pANCA is more common in UC (60–70%) than in CD (20–25%) [41]. The presence of pANCA+/ASCA– serology in patients with isolated eosinophilic colitis is not helpful for diagnosing specific phenotypes [27].
In our research, 63% of children with CD had a higher level of ASCA antibodies, whereas almost 20% suffered from isolated eosinophilic colitis, so it may indicate future development of CD in this group of patients.
In 18% of children with CD and in one child with isolated eosinophilic gastrointestinal disease, higher levels of p-ANCA were detected. In all cases there were children with degree III or IV in the Whitington scale.
The active eosinophils (extracellular degranulation of ECP) in CD, the importance of which is not clear, infiltrate tissue in relation to ulcerations only [42].
Eosinophils penetrate along the mucosal, infiltrate epithelium and pass into the lumen, where they release granularities containing proteins which are toxic to tissues [43].
It is known that the protein concentration derived from eosinophils granularity (ECP) in the intestinal fluid in patients with IBD is increased in comparison to the healthy control group [13]. Eosinophils granularity degranulation proves activation of these cells in the intestinal mucosa in patients with IBD.
It is unclear so far if the increased permeability of the gut for macro- and micro- particles occurring in patients with CD is the only factor determining the higher number of eosinophils in the intestinal mucosa of these patients.
Undoubtedly, toxic compounds released from the eosinophils granularity intensify small intestine damage. The eosinophilic infiltrates presence in CD is not yet finally determined. It is believed that eosinophilic colitis can evolve into IBD [44–46].
Pensabene et al., examining children with eosinophils in the large intestine, found that the maximum number of eosinophils per crypt was significantly higher in IBD than in other diseases of the gastrointestinal tract [7].
In our research, a correlation between the intensity of colon eosinophilic infiltration and IBD existence was found.
Two out of 7 patients were diagnosed with UC and eosinophilic colitis alongside, in the rest of patients already suffering from UC, eosinophilic colitis occurred.
Similarly, in the group of 11 children with CD, IBD and eosinophilic colitis were recognized at the same time in 2 of them, while in the rest with CD diagnosed earlier, eosinophilic inflammation was found (in everybody in degree III) in another colonoscopy. However, eosinophils in IBD do not always seem to appear to degranulate granularities, which additionally suggests their regulatory function [10, 12, 47–49]. Moreover, eosinophils in the gastrointestinal tract were described as the main source of calprotectin, the cytosolic protein with antimicrobial and antiproliferative features [50].
Still unresolved and complex function of eosinophils in IBD confirms the need for further clinical studies of this issue.
Conclusions
Higher concentrations of total IgE in half of patients with eosinophilic colitis indicates the need for diagnosis of allergy, both the IgE-mediated and non IgE-mediated allergy. Frequent coexistence of eosinophilic colitis and IBD suggests the need for immunological studies also in children with isolated eosinophilic colitis in order to estimate the risk of developing inflammatory bowel disease.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Yan B, Shaffer E. Primary eosinophilic disorders of the gastrointestinal tract. Gut. 2009;58:721–32. doi: 10.1136/gut.2008.165894. [DOI] [PubMed] [Google Scholar]
- 2.Kaijser R. Zur Kenntnis der allergischen Affektionem des Verdauungskanals vom Standpunkt des Chirurgen aus. Arch Klin Chir. 1937;188:36–64. [Google Scholar]
- 3.Klein N, Hargrove R, Sleisenger M, Jeffries G. Eosinophilic gastroenteritis. Medicine. 1970;49:299–319. doi: 10.1097/00005792-197007000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Rothenberg M. Eosinophilic gastrointestinal disorders (EGID) J Allergy Clin Immunol. 2004;113:11–28. doi: 10.1016/j.jaci.2003.10.047. [DOI] [PubMed] [Google Scholar]
- 5.Whitington P, Whitington G. Eosinophilic gastroenteropathy in childhood. J Pediat Gastroenterol Nutr. 1988;7:379–85. doi: 10.1097/00005176-198805000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Furuta G, Forbes D, Boey C, et al. EGIDs Working Group. Eosinophilic gastrointestinal diseases (EGIDs) J Pediatr Gastroenterol Nutr. 2008;47:234–8. doi: 10.1097/MPG.0b013e318181b1c3. [DOI] [PubMed] [Google Scholar]
- 7.Pensabene L, Brundler M, Bank J, di Lorenzo C. Evaluation of mucosal eosinophils in the pediatric colon. Dig Dis Sci. 2005;50:221–9. doi: 10.1007/s10620-005-1586-0. [DOI] [PubMed] [Google Scholar]
- 8.Bischoff S, Ulmer F. Eosinophils and allergic diseases of the gastrointestinal tract. Best Pract Res Clin Gastroenterol. 2008;22:455–79. doi: 10.1016/j.bpg.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 9.Spergel J, Rothenberg M, Fogg M. Eliminating eosinophilic esophagitis. Clin Immunol. 2005;115:131–2. doi: 10.1016/j.clim.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Walsh R, Gaginella T. The eosinophil in inflammatory bowel disease. Scand J Gastroenterol. 1991;26:1217–24. doi: 10.3109/00365529108998617. [DOI] [PubMed] [Google Scholar]
- 11.Alfadda A, Storr M, Shaffer E. Eosinophilic colitis: epidemiology, clinical features, and current management. Therap Adv Gastroenterol. 2011;4:301–9. doi: 10.1177/1756283X10392443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Desreumaux P, Nutten S, Colombel J. Activated eosinophils in inflammatory bowel disease: do they matter? Am J Gastroenterol. 1999;94:3396–8. doi: 10.1111/j.1572-0241.1999.01657.x. [DOI] [PubMed] [Google Scholar]
- 13.Levy A, Gleich G, Sandborn W. Increased esinophil granule proteins in gut lavage fluid from patients with IBD. Mayo Clin Proc. 1997;72:117–23. doi: 10.4065/72.2.117. [DOI] [PubMed] [Google Scholar]
- 14.Palczewska I, Niedżwiecka Z. Wskaźniki rozwoju somatycznego dzieci i młodzieży. Med Wieku Rozw. 2001;2(Suppl. 1):5. [PubMed] [Google Scholar]
- 15.Schroeder K, Tremaine W, Ilstrup D. Coated oral 5-aminosalicylic and therapy for mildly to moderately active UC. N Engl J Med. 1987;317:1625–9. doi: 10.1056/NEJM198712243172603. [DOI] [PubMed] [Google Scholar]
- 16.Oberhuber G, Vogelsang G. The histopathology of celiac disease: time for a standardized report scheme for pathologists. Eur J Gastroenterol Hepatol. 1999;11:1185–94. doi: 10.1097/00042737-199910000-00019. [DOI] [PubMed] [Google Scholar]
- 17.Whitington P, Whitington G. Eosinophilic gastroenteropathy in childhood. J Pediatr Gastroenterol Nutr. 1988;7:379–85. doi: 10.1097/00005176-198805000-00011. [DOI] [PubMed] [Google Scholar]
- 18.IBD Working Group of the European Society for Pediatric (ESPGHAN) Inflammatory bowel disease in children and adolescent: recommendations for diagnosis – the porto criteria. J Pediatr Gastroenterol Nutr. 2005;41:1–7. doi: 10.1097/01.mpg.0000163736.30261.82. [DOI] [PubMed] [Google Scholar]
- 19.Czaja-Bulsa G, Korlatowicz-Bilar A, Gębala A. Eozynofilowe zapalenie jelita grubego. Pediatr Współcz Gastroenterol Hepatol Żyw Dz. 2010;12:91–7. [Google Scholar]
- 20.DeBrosse C, Case J, Putnam P. Quantity and distribution of eosinophils in gastrointestinal tract of children. Pediatr Dev Pathol. 2006;9:210–8. doi: 10.2350/11-05-0130.1. [DOI] [PubMed] [Google Scholar]
- 21.Behjati S, Zilbauer M, Hauschkel R. Defining eosinophilic colitis in children: insights from a retrospective case series. J Pediatr Gastroenterol Nutr. 2009;49:208–15. doi: 10.1097/MPG.0b013e31818de373. [DOI] [PubMed] [Google Scholar]
- 22.Iwańczak B, Ruczka M. Eozynofilowe zapalenie jelita grubego w przebiegu nietolerancji preparatów 5-ASA u 8-letniej dziewczynki ze sferocytozą wrodzoną. Pediatr Współcz Gastroenterol Hepatol Żyw Dz. 2011;13:252–3. [Google Scholar]
- 23.Liacouras C, Bpnis P, Putnam P, et al. Summary of the First International Gastrointestinal Eosinophil Research Symposium. J Pediatr Gastroenterol Nutr. 2007;45:370–91. doi: 10.1097/MPG.0b013e318142b4f8. [DOI] [PubMed] [Google Scholar]
- 24.Lee J, Park H, Choe Y, et al. The development of eosinophilic colitis after liver transplantation in children. Pediatr Transplant. 2007;11:518–23. doi: 10.1111/j.1399-3046.2007.00693.x. [DOI] [PubMed] [Google Scholar]
- 25.Żbikowska-Gótz M, Kartuzi Z. Diagnostyka alergii pokarmowej. X Międzynarodowy Kongres Polskiego Towarzystwa Alergologicznego. 2009. [Google Scholar]
- 26.Inamura H, Kashiwase Y, Morioka J, et al. Accumulation of mast cells in the interstitium of eosinophilic colitis. Allergol Immunopathol. 2006;34:228–30. doi: 10.1157/13094031. [DOI] [PubMed] [Google Scholar]
- 27.Levine A, Koletzko S, Turner D, et al. ESPGHAN revised Porto Criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014;58:795–806. doi: 10.1097/MPG.0000000000000239. [DOI] [PubMed] [Google Scholar]
- 28.Van Limbergen J, Russell R, Drummond H, et al. Definition of phenotypic characteristics of child-hood-onset inflammatory bowel disease. Gastroenterology. 2008;135:1114–22. doi: 10.1053/j.gastro.2008.06.081. [DOI] [PubMed] [Google Scholar]
- 29.Reese G, Constantinides VA, Simillis C, et al. Diagnostic precision of anti-Saccharomyces cerevisiae antibodies and perinuclear antineurotrophil cytoplasmic antibodies in inflammatory bowel disease. Am J Gastroenterol. 2006;101:2410–22. doi: 10.1111/j.1572-0241.2006.00840.x. [DOI] [PubMed] [Google Scholar]
- 30.Stange E, Travis S, Vermiere S, et al. European evidence-based consensus on the diagnosis and management of ulcerative colitis: definitions and diagnosis. J Crohn’s Colitis. 2008;2:1–23. doi: 10.1016/j.crohns.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 31.Yantiss R, Farraye F, O`Brien M, et al. Prognostic significance of superficial fissuring ulceration in patients with severe “indeterminate” colitis. Am J Surg Pathol. 2006;30:165–70. doi: 10.1097/01.pas.0000189178.00440.bf. [DOI] [PubMed] [Google Scholar]
- 32.Melmed G, Elashoff R, Chen G, et al. Predicting a change in diagnosis from ulcerative colitis to Crohn’s disease: a nested case control study. Clin Gastroenterol Hepatol. 2007;5:602–8. doi: 10.1016/j.cgh.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 33.Bousvaros A, Antonioli D, Colletti R, et al. Differentation ulcerative colitis from Crohn’s disease in children and young adults: report of the working group of the North American Society for Pediatric, Gastroenterology, Hepatology and Nutrition and the Crohn’s and Colitis Foundation of America. J Pediatr Gastroenterol Nutr. 2007;44:653–74. doi: 10.1097/MPG.0b013e31805563f3. [DOI] [PubMed] [Google Scholar]
- 34.Joossens M, Simoens M, Vermeire S, et al. Contribution of genetic and environmental factors in the pathogenesis of Crohn’s disease in a large family with multiple cases. Inflamm Bowel Dis. 2007;13:580–4. doi: 10.1002/ibd.20086. [DOI] [PubMed] [Google Scholar]
- 35.Grzybowska-Chlebowczyk U, Woś H, Sieroń AL, et al. Serological investigations in children with inflammatory bowel disease and ford allergy. Mediators Inflamm. 2009;2009 doi: 10.1155/2009/512695. ID 512695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ruemmele F, Targan S, Levy G, et al. Diagnostic accuracy of serological assays in pediatric inflammatory bowel disease. Gastroenterol. 1998;115:822–9. doi: 10.1016/s0016-5085(98)70252-5. [DOI] [PubMed] [Google Scholar]
- 37.Hoffenberg E, Fidanza S, Sauaia A. Serologic testing for inflammatory bowel disease. J Pediatr. 1999;134:447–52. doi: 10.1016/s0022-3476(99)70202-7. [DOI] [PubMed] [Google Scholar]
- 38.Markowitz J, Kugathasan S, Dubinsky M, et al. Age of diagnosis influences serologic responses in children with Crohn’s disease: a possible clue to etiology? Inflamm Bowel Dis. 2009;15:714–9. doi: 10.1002/ibd.20831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dubinsky M, Lin Y, Dutridge D, et al. Serum immune responses predict rapid disease progression among children with Crohn’s disease: immune responses predict disease progression. Am J Gastroenterol. 2006;101:360–7. doi: 10.1111/j.1572-0241.2006.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Russell RK, Ip B, Aldhous MC, et al. Anti-Saccharomyces cerevisiae antibodies status is associated with oral involvement and disease severity in Crohn disease. J Pediatr Gastroenterol Nutr. 2009;48:161–7. doi: 10.1097/MPG.0b013e318183e112. [DOI] [PubMed] [Google Scholar]
- 41.Bartůnková J, Kolárová I, Sedivá A, et al. Antineutrophil cytoplasmic antibodies, anti-Saccharomyces cerevisiae antibodies, and specific IgE to food allergens in children with inflammatory bowel diseases. Clin Immunol. 2002;102:162–8. doi: 10.1006/clim.2001.5145. [DOI] [PubMed] [Google Scholar]
- 42.Hallgren R, Colombel J, Dahl R, et al. Neutrophil and eosinophil involvement of the small bowel in patients with celiac disease and Crohn’s disease: studies on the secretions rate and immunohistochemical localization of granulocyte granule constituemts. Am J Med. 1989;86:56–64. doi: 10.1016/0002-9343(89)90230-1. [DOI] [PubMed] [Google Scholar]
- 43.Rothenberg M, Mishra A, Brandt E, Hogan S. Gastrointestinal eosinophils. Immunol Rev. 2001;179:139–55. doi: 10.1034/j.1600-065x.2001.790114.x. [DOI] [PubMed] [Google Scholar]
- 44.Pera A, Bellando P, Caldera D, et al. Colonoscopy in inflammatory bowel disease. Diagnostic accuracy and proposal of an endoscopic score. Gastroenterology. 1987;92:181–5. [PubMed] [Google Scholar]
- 45.Moum B, Ekbom A, Vatn M, et al. Clinical course during the 1st year after diagnosis in ulcerative colitis and Crohn’s disease. Results of a large, prospective population-based study in southeastern Norway, 1990-1993. Scand J Gastroenterol. 1997;32:1005–12. doi: 10.3109/00365529709011217. [DOI] [PubMed] [Google Scholar]
- 46.Guindi R, Riddel L. Indeterminate colitis. J Clin Pathol. 2004;57:1233–44. doi: 10.1136/jcp.2003.015214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Furuta G, Akerman S, Wershil B. The role of the eosinophil in gastrointestinal diseases. Curr Opin Gastroenterol. 1995;11:541–7. [Google Scholar]
- 48.Weller P. The immunobiology of eosinophils. N Engl Med. 1991;324:1110–8. doi: 10.1056/NEJM199104183241607. [DOI] [PubMed] [Google Scholar]
- 49.Rothenberg M. Eosinophilia. N Engl J Med. 1998;338:1592–600. doi: 10.1056/NEJM199805283382206. [DOI] [PubMed] [Google Scholar]
- 50.Bjerke K, Halstensen T, Jahnsen F, et al. Distribution of macrophages and granulocytes expressing L1 protein (calprotectin) in human Peyer’s patches compared with normal ileal lamina propria and mesenteric lymph nodes. Gut. 1993;34:1357–63. doi: 10.1136/gut.34.10.1357. [DOI] [PMC free article] [PubMed] [Google Scholar]