Abstract
Objective
To assess the safety, efficacy, and stone-free rate (SFR) of mini-percutaneous nephrolithotomy (mini-PCNL) and retrograde intrarenal surgery (RIRS) for the management of lower calyceal stones of ⩽2 cm, and to determine the advantages and disadvantages of each.
Patients and methods
In all, 120 patients with lower calyceal stones of ⩽2 cm were randomly divided into two equal groups: Group A were managed by mini-PCNL and Group B by RIRS using flexible ureteroscopy and laser. The mean age, sex, stone size, operating time, complications, hospital stay, and SFR were compared between the groups. The success of the procedure was defined as the absence of residual stones or small residuals of ⩽0.2 cm on computed tomography at 12 weeks postoperatively.
Results
Both groups were comparable for preoperative parameters. The mean (SD) operating time was statistically significantly longer in Group B [109.66 (20.75) min] as compared to Group A [71.66 (10.36) min]. Although the hospital stay was longer in Group A as compared to Group B this was not statistically significant (P = 0.244). The SFR for Group A was 92.72% and for Group B it was 84.31%, which was not significantly different (P = 0.060).
Conclusion
For treating lower calyceal stones of ⩽2 cm mini-PCNL and RIRS are comparable. Mini-PCNL had a better SFR than RIRS but the hospital stay was longer and there were more intraoperative complications, whilst, RIRS had a significantly longer operating time compared with mini-PCNL and a higher incidence of postoperative fever, and a lower SFR.
Keywords: RIRS, PCNL, mini-PCNL, Renal stones
Abbreviations: Ho:YAG, holmium:yttrium-aluminium-garnet; KUB, plain abdominal radiograph of the kidneys, ureters and bladder; PCNL, percutaneous nephrolithotomy; RIRS, retrograde intrarenal surgery; SFR, stone-free rate; SWL, shockwave lithotripsy
Introduction
Renal stones remain one of the most commonly encountered urological problems worldwide [1]. The optimal management of lower calyceal renal calculi of ⩽ 2 cm is still debatable. Shockwave lithotripsy (SWL) was considered for a long time to be the best method for treating lower calyceal stones. However, the stone-free rates (SFRs) for SWL in most recent studies for lower calyceal stones range between 37% and 68% [2], [3]. SWL outcomes are influenced by stone composition, the lower calyceal angle that permits the clearance of the resultant residuals, and the patient’s body habitus, which may decrease the efficacy of SWL and increase the re-treatment rate.
Other available options include percutaneous nephrolithotomy (PCNL). The main disadvantage of the traditional PCNL was the need to use a large sheath (32 F), with the resultant potential complications of bleeding, injury to adjacent organs, postoperative pain, long hospital stay, and urinary fistulae. However, the introduction of the concept of mini-PCNL and fragmenting the stones using a holmium laser without the need for a postoperative nephrostomy tube (i.e. tubeless), has dramatically decreased these complications [4].
Flexible ureteroscopy and laser lithotripsy, also referred to as retrograde intrarenal surgery (RIRS), is now considered a treatment option, as compared to SWL it has proven to have a better SFR [5]. Each technique has its advantages and disadvantages [6].
Several studies have been conducted to compare mini-PCNL and RIRS as regards the SFR and the safety for managing lower calyceal stones. The main limitations of these previous studies were the limited number of cases, the different classifications of targeted stone size, and their definition of success [7], [8], [9].
The aim of the present study was to assess the safety, efficacy, and SFR of mini-PCNL and RIRS in the management of lower calyceal stones of ⩽2 cm and to determine the advantages and disadvantages of each.
Patients and methods
This is a prospective randomised study carried out between July 2012 and December 2015. The study started with 140 patients with lower calyceal stones of ⩽2 cm, as measured by multi-slice spiral CT, who met our inclusion criteria. In all, 20 patients refused any form of surgical intervention and were excluded from the study. The remaining 120 patients were randomly divided into two groups: Group A, managed by mini-PCNL; and Group B, managed by RIRS using flexible ureteroscopy and laser [Auriga® holmium (Ho):yttrium-aluminium-garnet (YAG) laser system, StarMedTec GmbH, Germany].
The randomisation was achieved using sealed envelopes. The inclusion criteria included all adult patients with solitary lower calyceal stones of ⩽2 cm, as measured by multi-slice spiral CT. The exclusion criteria included: patients aged <18 years, multiple renal stones, renal pelvic stone, stones of >2 cm, renal stones in anomalous kidney, bilateral renal stones, patients with renal failure, patients with bleeding tendency, and pregnant women.
Study design
In all, 120 patients with lower calyceal stones of ⩽2 cm were randomly divided into two groups each included 60 patients. All patients were evaluated by history taking, laboratory investigations including kidney and liver functions, complete blood count, fasting blood sugar, bleeding profile, urine analysis and culture. Radiological investigations included abdominal ultrasonography, multi-slice spiral CT to measure the stone size and plain abdominal radiograph of the kidneys, ureters and bladder (KUB).
The 60 patients randomly assigned to Group A were managed by mini-PCNL and those in Group B were managed by RIRS.
Ethical considerations
The ethics committee approved the study and all patients were informed about the study and a signed written consent was obtained.
Procedure
All patients in both groups had a urine analysis before the procedure. All patients with UTIs received antibiotics based on urine culture and sensitivity. Urine analysis was repeated again before the procedure. All patients in both groups received a prophylactic antibiotic immediately before the procedure in the form of ceftriaxone 1 g, which was continued for the ensuing 48 h.
Group A – mini-PCNL
In all, 60 patients underwent mini-PCNL in the prone position under general anaesthesia. Localisation and proper selection of the puncture sites was aided by contrast injection through the 6-F ureteric catheter placed at the beginning of the procedure. The time needed for the insertion of the ureteric catheter, as well as that needed for patient positioning were included in the overall operating time. Calyceal puncture was performed using a 22-G needle. A 0.035-mm J-tipped guidewire was inserted through the calyceal puncture into the renal pelvis. Dilatation of the tract was performed using the first three Alkan dilators. After tract dilatation, a 16-F sheath was inserted. A rigid 10-F ureteroscope was introduced and stone fragmentation was carried out using a Ho:YAG laser (365 μm fibre; energy 0.8 J; frequency 12 Hz). At the end of the procedure a 16-F urethral catheter was left in situ for 48 h together with the ureteric catheter without placing a nephrostomy tube (i.e. tubeless).
Group B – RIRS
In all, 60 patients underwent RIRS in the dorsal lithotomy position under general anaesthesia. Thorough cystoscopy was performed with a 22-F sheath. A 0.035-mm straight guidewire was inserted through the ureteric orifice to the renal pelvis. We used a 12/14-F ureteric access sheath (Cook Medical).
A 7.5-F flexible ureteroscope (Karl Storz, Tuttlingen, Germany) was passed in a retrograde fashion to access the stone. The stones were fragmented using a Ho:YAG laser (365 μm fibre; energy 0.8 J; frequency 12 Hz). We left the resulting very small stone fragments after laser vaporisation for spontaneous passage.
At the end of the procedure a 6-F ureteric catheter together with a 16-F urethral silicone catheter was routinely placed to be removed after 48 h.
The follow-up was scheduled at 1-, 4- and 12-week intervals postoperatively. At the first visit, KUB, serum creatinine, percentage haemoglobin, and urine analysis were done. This was repeated at 4 weeks postoperatively. At 12 weeks postoperatively, a multi-slice spiral CT was carried out to assess the success of the procedure used, as well as to exclude residual stones.
The mean age, sex, stone size, operating time, complications, hospital stay, and SFR were compared between both groups. The success of the procedure was defined as the absence of residual stones or small residuals of ⩽0.2 cm on CT at 12 weeks postoperatively.
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS®), version 15 for Windows. Results are expressed as mean (SD) or rate (%). Comparison between groups was performed using the Student’s t-test. Comparison between categorical data (number/percentage) was performed using the chi-squared test. A P < 0.05 was considered to indicate statistical significance.
Sample size calculation was done based on the SFR (primary outcome). The SFR was assumed to be 94% and 73% for mini-PCNL and RIRS, respectively [10]. An uncorrected chi-squared test was chosen to perform the analysis. The Type I error probability was fixed at 0.05 and the power was entered to be 80% and the groups were assumed to be of equal size.
Results
Both groups had comparable preoperative parameters (Table 1). The mean operating time was longer in Group B (RIRS) than in Group A (mini-PCNL) (P < 0.001; Table 2).
Table 1.
The patients’ preoperative characteristics.
| Variable | Group A (mini-PCNL) | Group B (RIRS) | P |
|---|---|---|---|
| Sex, n (%) | 0.727 | ||
| Males | 38 (63.3) | 34 (56.7) | |
| Females | 22 (36.7) | 26 (43.3) | |
| Mean (SD; range): | |||
| Age, years | 37.23 (9.24; 20–56) | 37.7 (9.76; 19–57 | 0.981 |
| Stone size, cm | 1.47 (0.3; 0.8–2.0) | 1.41 (0.3; 0.8–20) | 0.392 |
| Preoperative Hb, g/dL, mean (SD; range) | 13.78 (0.797; 12.3–15.3) | 13.69 (0.755; 12.4–15.0) | 0.796 |
| Right-sided stones, n (%) | 34 (56.7) | 38 (63.3) | 0.727 |
Hb, haemoglobin.
Table 2.
The patients’ operative and postoperative characteristics.
| Variable | Group A (mini-PCNL) | Group B (RIRS) | P |
|---|---|---|---|
| Mean (SD; range): | |||
| Operating time, min | 71.66 (10.36) | 109.66 (20.75) | <0.001 |
| Postoperative Hb level, g/dL | 13.15 (0.813; 11.3–14.6) | 13.56 (0.781; 12.2–15.0) | 0.081 |
| Patients stone free at 12-week follow-up, n/N | 51/55 | 43/51 | 0.060 |
| SFR,% | 92.72 | 84.31 | |
| Complications, n (%): | |||
| Overall intraoperative | 3 (5) | 2 (3.33) | 0.187 |
| Bleeding | 2 (3.33) | 0 | |
| Minor mucosal injury | 1 (1.66) | 2 (3.33) | |
| Postoperative fever | 2 (3.33) | 3 (5) | 0.227 |
| Total complications | 5 (8.33) | 5 (8.33) | 1 |
Hb, haemoglobin.
In Group A, there were two cases (3.33%) of bleeding and a case (1.66%) of minor pelvi-ureteric injury and contrast extravasation. All three cases had an indwelling JJ stent for a month. In Group B, two patients (3.33%) had a minor ureteric injury; the procedure was completed for both patients and a JJ-stent was fixed at the end of the procedure for a month. Although intraoperative complications were recorded in three cases in Group A and two in Group B this was not statistically significant (P = 0.187; Table 2).
Stone migration was reported in two patients in Group A and three patients in Group B, and all were managed by flexible ureteroscopy giving it an advantage over the mini-PCNL.
On applying the modified Clavien–Dindo Grading system for complications, all our complications in both groups, two patients in Group A and three patients in Group B were classified as grade I, i.e. deviation from the normal postoperative course without the need for pharmacological treatment or surgical or endoscopic interventions.
For blood loss, although more in Group A vs Group B, this was not statistically significant (P = 0.081); the mean haemoglobin deficit in Group A was 0.28 g/dL as compared to 0.13 g/dL in Group B. None of the patients needed a blood transfusion and all cases of haematuria where managed conservatively by i.v. fluids, anti-bleeding measures, and bed rest (Table 1, Table 2).
Two patients (3.33%) in Group A and three patients (5%) in Group B developed postoperative fever. The fever subsided with the use of antibiotics and antipyretics after 24 h, with no statistically significant difference between the groups (P = 0.227; Table 2).
In Group A, 50 patients (83.33%) remained in hospital for 48 h postoperatively, eight (13.33%) remained for 72 h, and two left the hospital after 96 h. In Group B, 54 patients (90%) remained in hospital for 48 h postoperatively and six (10%) remained for 72 h. All those patients who remained in hospital for a longer period did so either to monitor and treat their fever or to follow-up serum haemoglobin for suspicion of a drop. When comparing Groups A and B for the hospital stay there was no statistically significant difference (P = 0.244).
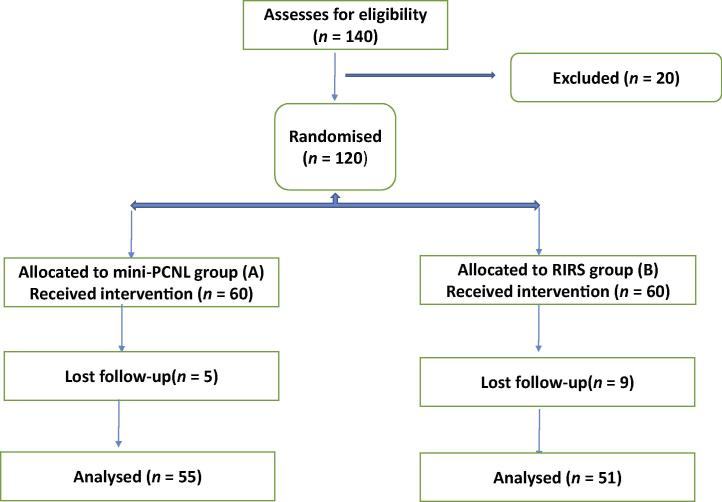
In all, 55 patients (91.66%) in Group A and 51 patients (85%) in Group B completed the study at 12 weeks postoperatively; five patients in Group A and nine patients in Group B missed the follow-up (Fig. 1, Table 2).
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) flow chart of study participants.
Despite the SFR in Group A being 92.72% vs 84.31% in Group B, according to the definition of success that was set at the beginning of the study, this was not found to be statistically significant.
Discussion
Most recent studies have compared either PCNL or RIRS to SWL to determine which is more suitable for patients with renal pelvic or lower calyceal stones of ⩽2 cm [11]. In their study, Albala et al. [2] reported a statistically significantly higher SFR for PCNL compared to SWL for lower calyceal stones of 95.8% and 40%, respectively. A similar result was also reported by Yuruk et al. [12], they compared PCNL and SWL for managing 62 patients with lower calyceal stones of <2.0 cm and documented a higher SFR for PCNL as compared to SWL of 96.7% and 56.7%, respectively. Several studies have compared RIRS to SWL for managing lower calyceal stones. Salem et al. [13] conducted their study on 60 patients with lower calyceal stones of <2.0 cm who were randomly divided into two groups and were managed with either RIRS or SWL. The SFR for RIRS was 96.7% and for SWL was 56.7%, which was statistically significant. Similar results but at 4 weeks postoperatively were also achieved by Singh et al. [14].
Lee et al. [15] conducted a study to compare mini-PCNL and RIRS for managing patients with renal stones of >1.0 cm and came to the conclusion that both techniques are safe and equally effective, with a SFR following a single session at 12 weeks follow-up of 85.7% in the mini-PCNL group and 97.0% in the RIRS group (P = 0.199). Two important differences were reported between the different studies comparing these two techniques, the first was the initial stone size studied and the second was the definition of the success. Whilst Albala et al. [2] and Carlsson and et al. [16] studied stones of ⩽3.0 cm, Pearle et al. [11] conducted their studies on stones of ⩽1.0 cm, and Kuo et al. [17] studied stones of 1.1–2.5 cm. As regards the definition of their success, Albala et al. [2] defined the success as stone free or residual fragments of ⩽0.3 cm at 12 weeks, Carlsson et al. [16] defined it as stone free or residual fragments of ⩽0.5 cm at 4 weeks and Pearle et al. [11] defined it stone free or residual fragments of ⩽0.5 cm at 12 weeks.
In the present study, we compared mini-PCNL and RIRS, after random allocation of patients, for managing lower calyceal stones in order to determine the pros and cons of each technique. Such data are important for assisting the urologist together with their patients in deciding which technique to choose.
We prospectively studied stones of ⩽2 cm and the patients were randomly divided into two groups, each of 60 patients. Our definition of success was similar to that of Albala et al. [2].
In the present study, there were no major intraoperative complications that required surgical or radiological intervention. By contrast, Ozturk et al. [10] reported a case of ureteric injury during RIRS that required surgical repair and a case of significant bleeding in their mini-PCNL group that required angio-embolisation. The most commonly encountered complication in the present study was postoperative fever reported in five cases [two in Group A (3.33%) and three in Group B (5%)] followed by minor pelvi-calyceal injury that was managed conservatively [one in Group A (1.66%) and two in Group B (3.33%)]. This is comparable to the results of Yuruk et al. [12] for PCNL. The incidence of postoperative fever in our present study was more than that reported by Hyams et al. [18] who reported fever in only 2.5%, and that reported Kumar et al. [19] of 3.3% for RIRS.
The mean operating time was statistically significantly longer in Group B (RIRS) than in Group A (mini-PCNL) (P < 0.001), which disagrees with the study of Sabnis et al. [20] who reported a shorter operating time for RIRS as compared to PCNL. However, a significantly longer operating time for RIRS than for mini-PCNL was also reported by Bozkurt et al. [21] and Kirac et al. [22].
There was no statistically significant difference between the groups for hospital stay.
When comparing the two techniques used, we found that the SFR was better in Group A (mini-PCNL) as compared to Group B (RIRS), at 92.72% and 84.31%, respectively; however, this also was not statistically significant.
The two failures in patients managed by mini-PCNL were due to stone migration to either the upper or middle calyceal areas making their access via the percutaneous route difficult. In both cases, the stones were managed by RIRS.
Our present SFR for mini-PCNL is very similar to that reported by Albala et al. [2] (95.8%), Yuruk et al. [12] (96.7%), and much better than that reported by Kuo et al. [17] (66.7%). Whilst for RIRS, our present SFR is very similar to that reported by Kumar et al. [8] (86.6%) and Singh et al. [14] (85.7%), and much better than that of Pearle et al. [11] (72%), but worse than that of Salem et al. [13] (96.7%).
A major limitation to our present study was the relatively small sample size of each study group and the lack of stratification of the groups according to stone sizes of 1.0 cm and those of 1.0–2.0 cm.
The main drawbacks of RIRS include: the need of flexible scopes, limited visualisation, reduced size of fragments removed, and the need for flexible lithotrites and baskets. Thus, cost is a major deterrent to RIRS, particularly in developing countries [23].
Conclusion
Managing renal stones of 1.0–2.0 cm remains a challenge for the urologist to attain the best SFR amongst the available techniques. For lower calyceal stones of ⩽2 cm, mini-PCNL and RIRS were comparable in SFR, complications, and hospital stay. However, mini-PCNL had statistically significant shorter operating time.
RIRS remains an available minimally invasive option with a reasonable SFR, relatively longer operating time, and higher incidence of postoperative fever. Moreover it is a reasonable option in cases of stone migration during mini-PCNL.
Conflict of interest
None.
Funding
None.
Stones/Endourology
Footnotes
Peer review under responsibility of Arab Association of Urology.
References
- 1.Türk C., Petřík A., Sarica K., Seitz C., Skolarikos A., Straub M. EAU Guidelines on Interventional Treatment for Urolithiasis. Eur Urol. 2016;69:475–482. doi: 10.1016/j.eururo.2015.07.041. [DOI] [PubMed] [Google Scholar]
- 2.Albala D.M., Assimos D.G., Clayman R.V., Denstedt J.D., Grasso M., Gutierrez-Aceves J. Lower pole I: a prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis- initial results. J Urol. 2001;166:2072–2080. doi: 10.1016/s0022-5347(05)65508-5. [DOI] [PubMed] [Google Scholar]
- 3.Obek C., Onal B., Kantay K., Kalkan M., Yalçin V., Oner A. The efficacy of extracorporeal shock wave lithotripsy for isolated lower pole calculi compared with isolated middle and upper caliceal calculi. J Urol. 2001;166:2081–2085. doi: 10.1016/s0022-5347(05)65509-7. [DOI] [PubMed] [Google Scholar]
- 4.Monga M., Oglevie S. Minipercutaneous nephorlithotomy. J Endourol. 2000;14:419–421. doi: 10.1089/end.2000.14.419. [DOI] [PubMed] [Google Scholar]
- 5.El-Nahas A.R., Ibrahim H.M., Youssef R.F., Sheir K.Z. Flexible ureterorenoscopy versus extracorporeal shock wave lithotripsy for treatment of lower pole stones of 10–20 mm. BJU Int. 2012;110:898–902. doi: 10.1111/j.1464-410X.2012.10961.x. [DOI] [PubMed] [Google Scholar]
- 6.Srisubat A., Potisat S., Lojanapiwat B., Setthawong V., Laopaiboon M. Extracorporeal shock wave lithotripsy (ESWL) versus percutaneous nephrolithotomy (PCNL) or retrograde intrarenal surgery (RIRS) for kidney stones. Cochrane Database Syst Rev. 2009;4 doi: 10.1002/14651858.CD007044.pub2. CD007044. [DOI] [PubMed] [Google Scholar]
- 7.De S., Autorino R., Kim F.J., Zargar H., Laydner H., Balsamo R. Percutaneous nephrolithotomy versus retrograde intrarenal surgery: a systematic review and meta-analysis. Eur Urol. 2015;67:125–137. doi: 10.1016/j.eururo.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Kumar A., Kumar N., Vasudeva P., Kumar Jha S., Kumar R., Singh H. A prospective, randomized comparison of shock wave lithotripsy, retrograde intrarenal surgery and miniperc for treatment of 1 to 2 cm radiolucent lower calyceal renal calculi: a single center experience. J Urol. 2015;193:160–164. doi: 10.1016/j.juro.2014.07.088. [DOI] [PubMed] [Google Scholar]
- 9.Pan J., Chen Q., Xue W., Chen Y., Xia L., Chen H. RIRS versus mPCNL for single renal stone of 2–3 cm: clinical outcome and cost-effective analysis in Chinese medical setting. Urolithiasis. 2013;41:73–78. doi: 10.1007/s00240-012-0533-8. [DOI] [PubMed] [Google Scholar]
- 10.Ozturk U., Sener N.C., Goktug H.N., Nalbant I., Gucuk A., Imamoglu M.A. Comparison of percutaneous nephrolithotomy, shock wave lithotripsy, and retrograde intrarenal surgery for lower pole renal calculi 10–20 mm. Urol Int. 2013;91:345–349. doi: 10.1159/000351136. [DOI] [PubMed] [Google Scholar]
- 11.Pearle M.S., Lingeman J.E., Leveillee R., Kuo R., Preminger G.M., Nadler R.B. Prospective randomized trial comparing shock wave lithotripsy and ureteroscopy for lower pole calyceal calculi 1 cm or less. J Urol. 2008;179:S69–S73. doi: 10.1016/j.juro.2008.03.140. [DOI] [PubMed] [Google Scholar]
- 12.Yuruk E., Binbay M., Sari E., Akman T., Altinyay E., Baykal M. A prospective, randomized trial of management for asymptomatic lower pole calculi. J Urol. 2010;183:1424–1428. doi: 10.1016/j.juro.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 13.Salem A., Saad I., Emran A., Abdelhakiem M., Abdelrazzak O., Abdelkader M. Laser lithotripsy versus ESWL for lower calyceal renal stones. J Urol. 2013;189(Suppl):e751. [Google Scholar]
- 14.Singh B.P., Prakash J., Sankhwar S.N., Dhakad U., Sankhwar P.L., Goel A. Retrograde intrarenal surgery vs extracorporeal shock wave lithotripsy for intermediate size inferior pole calculi: a prospective assessment of objective and subjective outcomes. Urology. 2014;83:1016–1022. doi: 10.1016/j.urology.2013.12.026. [DOI] [PubMed] [Google Scholar]
- 15.Lee J.W., Park J., Lee S.B., Son H., Cho S.Y., Jeong H. Mini-percutaneous nephrolithotomy vs retrograde intrarenal surgery for renal stones larger than 10 mm: a prospective randomized controlled trial. Urology. 2015;86:873–877. doi: 10.1016/j.urology.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 16.Carlsson P., Kinn A.C., Tiselius H.G., Ohlsén H., Rahmqvist M. Cost effectiveness of extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy for medium-sized kidney stones. A randomised clinical trial. Scand J Urol Nephrol. 1992;26:257–263. doi: 10.3109/00365599209180879. [DOI] [PubMed] [Google Scholar]
- 17.Kuo R.L., Lingeman J.E., Leveillee R.J., Pearle M.S., Waskins S. Lower pole II: initial results from a comparison of shock wave lithotripsy (SWL), ureteroscopy (URS), and percutaneous nephrostolithotomy (PNL) for lower pole nephrolithiasis. J Urol. 2003;169(Suppl.):486. [Google Scholar]
- 18.Hyams E.S., Munver R.I., Bird V.G., Uberoi J., Shah O. Flexible ureterorenoscopy and holmium laser lithotripsy for the management of renal stone burdens that measure 2 to 3 cm: a multi-institutional experience. J Endourol. 2010;24:1583–1588. doi: 10.1089/end.2009.0629. [DOI] [PubMed] [Google Scholar]
- 19.Kumar A., Vasudeva P., Nanda B., Kumar N., Jha S.K., Singh H. A prospective randomized comparison between shock wave lithotripsy and flexible ureterorenoscopy for lower caliceal stones >2 cm: a single-center experience. J Endourol. 2015;29:575–579. doi: 10.1089/end.2013.0473. [DOI] [PubMed] [Google Scholar]
- 20.Sabnis R.B., Ganesamoni R., Doshi A., Ganpule A.P., Jagtap J., Desai M.R. Micropercutaneous nephrolithotomy (microperc) vs retrograde intrarenal surgery for the management of small renal calculi: a randomized controlled trial. BJU Int. 2013;112:355–361. doi: 10.1111/bju.12164. [DOI] [PubMed] [Google Scholar]
- 21.Bozkurt O.F., Resorlu B., Yildiz Y., Can C.E., Unsal A. Retrograde intrarenal surgery versus percutaneous nephrolithotomy in the management of lower-pole renal stones with a diameter of 15 to 20 mm. J Endourol. 2011;25:1131–1135. doi: 10.1089/end.2010.0737. [DOI] [PubMed] [Google Scholar]
- 22.Kirac M., Bozkurt Ö.F., Tunc L., Guneri C., Unsal A., Biri H. Comparison of retrograde intrarenal surgery and mini-percutaneous nephrolithot-omy in management of lower-pole renal stones with a diameter of smaller than 15 mm. Urolithiasis. 2013;41:241–246. doi: 10.1007/s00240-013-0552-0. [DOI] [PubMed] [Google Scholar]
- 23.Landman J., Lee D.I., Lee C., Monga M. Evaluation of overall costs of concurrently available small flexible ureteroscopes. Urology. 2003;62:218–222. doi: 10.1016/s0090-4295(03)00376-5. [DOI] [PubMed] [Google Scholar]