Abstract
Objective
To evaluate the value of individual and combined measurement of human epididymis protein 4 (HE4) and cancer antigen 125 (CA-125) in the diagnosis of ovarian cancer.
Methods
A clinical case-control study was performed in which the levels of serum HE4 and CA-125 of subjects with malignant, borderline, benign ovarian tumors and healthy women were measured before surgery. An immunohistochemistry method was used to measure the expression of HE4 in different tissues. Statistical analysis was performed to determine the relationship between the level of HE4 and the pathologic type as well as the stage of the ovarian tumors.
Results
The level of HE4 in the serum was significantly elevated in the malignant ovarian cancer group compared with other groups. Women with benign ovarian tumors and non-neoplastic lesions, and healthy women were designated as references. When the level of HE4 in the serum was 58.66 pmol/L, the sensitivity and specificity of HE4 in diagnosing malignant ovarian tumors was 82.35% and 96.03%, respectively. The level of HE4 was negatively correlated with the differentiation extent of the tumors whereas positively correlated to the clinical staging. In the groups of malignant and borderline tumors, the levels of HE4 were higher than the other groups. The expression of HE4 was significant higher in the serous types of ovarian tumors than that of the mucous types (P<0.05). The level of HE4 in the serum and tissues were positively correlated with each other.
Conclusion
HE4 can be used as a novel clinical biomarker for predicting malignant ovarian tumors and its expression was closely related with the clinical pathological features of malignant ovarian tumors.
Keywords: HE4, CA125, diagnosis, ovarian tumor
1. Introduction
In the female reproductive system, ovarian cancer ranks third in incidence and 1st in mortality in gynecological malignancies [1]. Nearly 70% of patients with ovarian cancer are diagnosed at an advanced stage, and the 5 year survival rate for patients with ovarian cancer rises up to 90% through early effective treatment [2]. Hence, diagnosing at early stage is crucial to improve the prognosis of ovarian cancer. Currently, the most commonly used serum biomarkers for early diagnosis of ovarian cancer is CA125. But it could be also elevated in serum for patients with pelvic inflammatory disease, such as endometriosis peritoneal disease and injury [3]. So the application of CA125 in ovarian cancer diagnosis showed high false positive rate, and sometimes this would lead to unnecessary surgery. Human epididymis protein 4 (Human epididymis gene product 4, HE4) is considered a new biomarker for early diagnosis of ovarian cancer. In this study, we included a case-control study to determine the serum level as well as the expression of HE4 and CA125 in clinical ovarian cancer tissues. We also intended to evaluate the value of individual and/or combined measurement of HE4 and CA-125 in the diagnosis of ovarian cancer and prognosis prediction.
2. Material and method
2.1. Patients
Select the patients with a pelvic mass, who were first inpatient for gynecological surgery in the First Affiliated Hospital of Fujian Medical University, from December 2010 to October 2012. All patients had no significant syndrome that effecting tumor biomarkers, and received no preoperative chemotherapy and other treatments. According to the postoperative pathology judging results, the subjects were divided into malignant ovarian tumor group (58 cases), borderline ovarian tumor group (10 cases), benign ovarian tumors (40 cases), ovarian non-neoplastic lesions (27 cases) and other gynecologic malignancies (26 cases). Among the 58 cases of malignant ovarian tumors, there were 42 cases of epithelial ovarian tumors and 16 cases of non-epithelial ovarian tumors. In addition, the malignant ovarian tumor group included 30 cases of serous carcinomas, 12 cases of mucous carcinomas, 6 cases of ovarian endometrioid adenocarcinomas, 3 cases of clear-cell carcinomas, 4 cases of yolk sac tumors, and 3 cases of dysgerminoma. Clinical staging was classified according to the International Federation of Gynecology and Obstetrics (FIGO) criteria: 18 cases of I, 6 cases of II, 30 cases of III, and 4 cases of IV stage. There were 8 cases of highly differentiated, 18 cases of moderately differentiated and 32 cases of poorly differentiated. There were 22 patients with viscera metastasis. The borderline ovarian tumor group included 6 cases of borderline serous papillary tumors, 4 cases of borderline mucous cystadenomas. The benign ovarian tumor group included 17 cases of serous cystadenomas, 12 cases of mucous cystadenomas, 5 cases of mature teratomas, 4 cases of simple cysts, and 2 cases of fibromas. Ovarian non-neoplastic lesions included 27 cases of ovarian endometriosis cysts. Gynecological cancer group included 2 cases of uterine sarcomas, 6 cases of endometrial cancer and 18 cases of cervical cancer. All blood samples were taken from the elbow in the day before surgery, fasting venous whole blood 3 ml, placed in a test tube without anticoagulant, Specimen collection was stand at room temperature for 1 hour, centrifuged (3000 r/min) to take the clear phase, and stored in -80 degrees C freezer for testing. After reading the pathological sections of these patients, select respective paraffin blocks for section at the thickness of 4 micrometers. Meanwhile, we selected 10 cases of partial ovarian normal tissues from the surgically hysteromyoma resections followed by 4% paraformaldehyde-fixed, paraffin-embedded, and histologically confirmed by conventional HE staining. The age of malignant ovarian cancer group was from 11 to 74, with an average age of 49.43±14.69 years old. Non-ovarian cancer group was aged from 15 to 76, with an average age of 40.66±12.56. The patients were not receiving any other treatment in our hospital. Over the same period, we also tested the serum level of HE4 and CA125 in healthy women (59 cases). All the subjects of our study were in non-menstrual period, with no breast/thyroid disease, and a history of other cancers.
Ethical approval: The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board or equivalent committee.
Informed consent: Informed consent has been obtained from all individuals included in this study.
2.2. Method
The electrochemical luminescence method was used to detect the level of HE4 and CA125 in the serum. We applied the human epididymis protein 4 assay kit (Roche, Shanghai, China, 05950929190), Roche cobas e 601 and electrochemiluminescence assay.
Monoclonal mouse anti-human HE4 (ZM-0413) and CA125 (ZM-0019) antibodies were ordered from Beijing Zhongshan Golden Bridge Company. Immunohistochemical detection reagents (PV-9000) were also purchased from Beijing Zhongshan Golden Bridge Company. Take the above paraffin blocks of ovarian cancer tissues, and perform routine HE staining, and then observe the morphology of tumor cells through the microscope. Phosphate buffer was used as a negative control instead of primary antibody.
The reference value of serum HE4 is 0-140pmol/L, regarding HE4>140pmol/L as positive. The reference value of serum CAl25 is 0~35U/ml, regarding CAl25>35U/ml as positive. Serum HE4 diagnostic cutoff points was obtained through the ROC curve. Ovarian tumors were used as positive controls, with PBS instead of primary antibody as blank control. Comprehensive observing each slice, regard the brown particles appearing in cytoplasm as positive. Two pathologists read the piece randomly. The determine criteria was shown as follows: staining were divided into four levels: almost not colored for 0 point, yellow for 1 point, brown for 2 point, tan for 3 point; coloring cells in percentage: ≤ 5% as 0, 6% -25% as 1, 26-50% as 2, ≥ 51% as 3. The degree of ovarian tissue coloring, coloring percentage score: 0-1 as negative, 2-3 as +, 4-6 as ++, 6 points or more as +++.
3. Statistical analysis
Statistical analysis were performed using SPSS 13.0. The level of HE4 and CA125 were expressed as median number (M). The pathologic diagnosis was considered as the standard, the ROC curve was traced, and the sensitivity and specificity were calculated. The multigroup comparative analysis was assessed by non parameter Kruskal-Wallis test, the two comparative analysis was assessed by Mann-Whitney test. For all statistical analysis, P value of less than 0.05 was considered to be significant.
4. Results
4.1. The levels of serum HE4 and CA125
The HE4 level in the group of the malignant ovarian tumor group was significantly increased, compared with other groups, (χ2=101.129, P<0.0001). We did not observe significant difference between the other five groups (P>0.05). The CA125 level was also observed to be significantly different between the groups (χ2=61.579, P<0.0001). But in the group of the ovarian non-neoplastic lesions, the level of CA125 was significant up-regulated when compared with the ovarian benign tumor group (P<0.01) (Table 1).
Table 1.
Levels of serum HE4 and CA125
| Group | HE4(pmol/L) | CA125(IU/L) |
|---|---|---|
| malignant ovarian tumors | 93.23±58.17 | 78.95±430.90 |
| borderline ovarian tumors | 76.00±17.25 | 26.16±119.88 |
| benign ovarian tumors | 25.42±17.13 | 22.35±25.52 |
| Non-neoplastic lesions of ovarian | 34.00±15.07 | 76.79±315.40 |
| other malignant gynecologic tumors | 38.48±29.05 | 15.92±13.83 |
| healthy women | 24.00±13.55 | 20.00±17.72 |
4.2. Serum HE4 and CA125 joint evaluation
In the group of malignant ovarian cancer, including serous ovarian cancer, mucous ovarian cancer and ovarian endometrium adenoendometriocarcinoma, there was about 66.67% of those CA125 negative cases emerged as HE4 positive. In the group of non-neoplastic lesions of ovarian, there was about 88.00% of those CA125 positive cases emerged as HE4 negative.
The relationship between the serum HE4 level and the patient age, pathological type, grading and clinical staging in the malignant ovarian tumor group before operation.
The serum HE4 level in the malignant ovarian cancer group before operation was not related to the patient age (p=0.105, p>0.05, p=0.435). The median of HE4 level was 108.00±86.13pmol/L for the epithelial ovarian cancer, 62.31±69.43pmol/L for the nonepithelial ovarian cancer. There was significant difference between them (Z=-3.306, P=0.001). The median of HE4 level was 119.80±258.98pmol/L in the serous type and 75.50±58.41pmol/L in the mucous type of ovarian cancer. There was also significant difference between them (Z=-3.774, P<0.0001). The median of serum HE4 level in high, medium and low extents of differentiation were 74.61±72.75, 81.00±22.76, 117.00±121.38 (pmol/L, respectively (χ2=10.821, P=0.004). The median of HE4 level in early age(I-II) and late age (III-IV) of malignant ovarian cancer were 88.00±20.03pmol/L and 119.80±147.13pmol/L, respectively (Z=-2.855, P=0.004). Taken together, we found that the serum HE4 level was negatively correlated with the pathologic differentiation (r=-0.435, P=0.001) and positively correlated with the clinical staging (r=0.363, P=0.003) (Table 2).
Table 2.
Relationship between serum HE4 and pathological type, grading and clinical staging in group of malignant ovarian tumor
| Characteristics | HE4(M±Q) | Statistical values | P value |
|---|---|---|---|
| Pathological type | |||
| Epithelial | 108.00±86.13 | Z=-3.306 | =0.001 |
| Non-epithelial | 62.31±69.43 | ||
| Serous | 119.80±258.98 | Z=-3.774 | <0.0001 |
| Mucous | 75.50±58.41 | ||
| Pathological grade | |||
| Low | 117.00±121.38 | χ2=10.821 | 0.004 |
| Medium | 81.00±22.76 | ||
| High | 74.61±72.75 | ||
| Clinical stage | |||
| Early stage | 88.00±20.03 | Z=-2.855 | 0.004 |
| Later stage | 119.80±147.13 |
4.3. The diagnosis threshold of serum HE4 level for ovarian cancer
We regarded the population of patients who had the benign tumor of the ovarian, non-neoplastic lesions of ovarian and the healthy women as reference, and found that 58.66pmol/L was the best diagnosing point for serum HE4 level. For diagnosing malignant ovarian cancer, the ROC-AUC was 0.889 with the sensitivity of 82.35% and the specificity of 96.03%. The rate of pathological coincident diagnosis was 80.29%. For the combined detection of HE4 and CA125, the sensitivity was 92.00% and the specificity was 76.67%. The rate of pathological diagnosis coincidence was 83.64%. In the healthy group, when the serum level of HE4 was 31.08pmol/L, the ROC-AUC for diagnosing malignant ovarian cancer was 0.850, with the sensitivity of 81.91% and specificity of 50.79% (Fig 1, 2).
Figure 1.
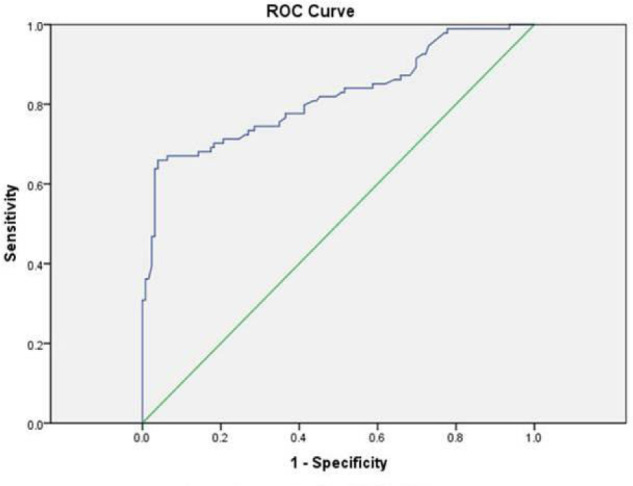
Diagnosis of HE4 boundary values with ovarian benign tumor, ovarian nonneoplastic lesions and healthy women as for reference.
Figure 2.
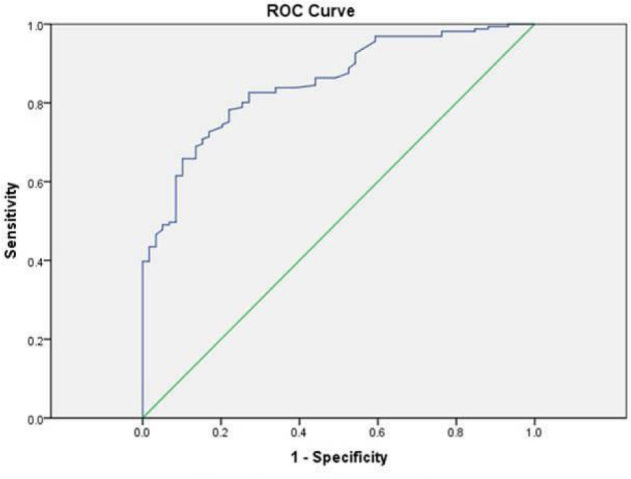
Diagnosis of HE4 boundary values with healthy women as for reference.
According to the HE4 reagent instructions, 150pmol/L was set up as the cutoff point for the diagnosis. The results showed the specificity of 100% and sensitivity of 8.70%, with the pathological diagnosis coincidence rate of 33.18%. Compared with the cutoff point of 31.08pmol/L obtained from our ROC curve, the diagnostic sensitivity and specificity exhibited statistically significance (P<0.05).
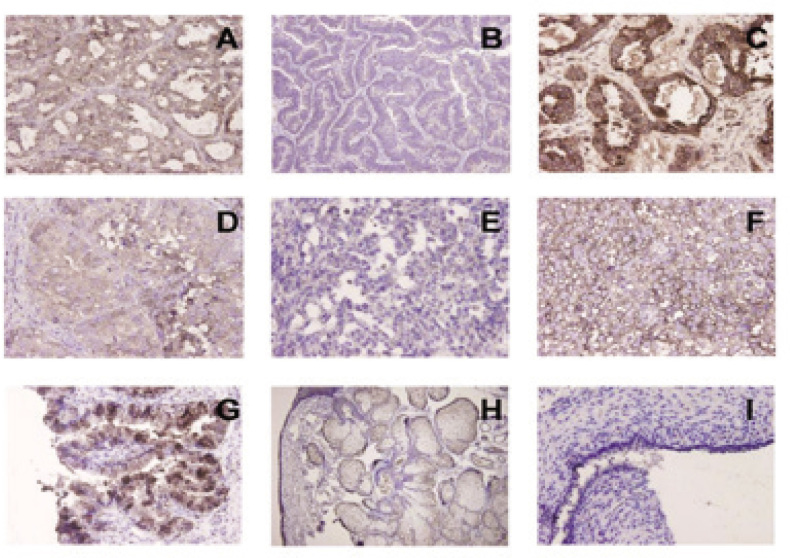
4.4. The expression of HE4 in ovarian tissues
HE4 was proved mainly expressed in the cytoplasm in the ovarian epithelial cells. HE4 was highly expressed in serous ovarian cancer tissues. The positivity expressing ratio of HE4 in mucous malignant ovarian tumors, borderline ovarian tumors, benign ovarian tumors, ovarian non-neoplastic lesions (ovarian endometriosis cyst) and the normal tissues of the ovarian was 84.48% (49/58), 70% (7/10), 17.50% (7/40), 11.11% (3/27), 0% (0/10), respectively (Fig 3A, 3B, 3C, 3D, 3E, 3F, 3G, 3H, 3I). In the group of malignant tumor and borderline tumor, the positive expression ratio of HE4 was remarkably higher than the other 3 groups (χ2=67.936, P<0.0001). There was no significant difference between the malignant tumor and borderline tumor group (χ2=1.231, P=0.267), but the expression intensity of HE4 in the malignant tumors was higher than that in the borderline tumor group. There were no significant difference between the normal ovarian group compared to the non-neoplastic lesions of ovarian (χ2=1.209, P=0.272) and ovarian benign tumor group (χ2=2.035, P=0.154); as well as the non-neoplastic lesions of ovarian compared to the ovarian benign tumor group (χ2=0.518, P=0.472).
Figure 3.
Expression of HE4 in ovarian tumor tissues Immunohistochemical staining of HE4 in serous ovarian cancer (Fig3A, ×400); mucous ovarian cancer (Fig3B, ×400); hyaline cell cancer (Fig3C, ×400); ovarian adenoendometrio carcinoma (Fig3D, ×400); corpus luteum cyst tumor (Fig3E, ×400); germ cell tumor (Fig3F, ×400); borderline ovarian tumor (Fig3G, ×400); ovarian benign tumor (Fig3H, ×400); ovarian endometriosis cyst (Fig 3I, ×400).
4.5. The relationship between HE4 expression and clinical pathological features in the malignant ovarian tumors
The positive expression rate of HE4 in the serous ovarian tumors, mucous ovarian tumors, clear-cell carcinomas, ovarian endometrioid adenocarcinomas, yolk sac tumors and dysgerminomas was 100% (30/30), 66.67% (8/12), 66.7% (2/3), 100% (6/6), 25% (1/4) and 75% (3/4), respectively. The expression of HE4 expression in serous ovarian cancer was higher than that in mucous ovarian cancer, and the variance had the statistic meaning (χ2=11.437, P=0.003). HE4 was found to be modest or highly expressed in the ovarian endometrioid adenocarcinomas, clear-cell carcinomas and dysgerminomas, and lowly expressed in the yolk sac tumors. The rate of positivity HE4 expression in the tissue of the early stage ovarian malignant tumor (I/II stage) is 66.67%, which is lower than that of the later stage (III/IV stage, 97.22%) (χ2=10.787, P=0.001). In the highly differentiated tissues, the HE4 positive expression rate was 37.50%, which was lower than that of the low differentiated tissue (92.00%, χ2=15.626, P<0.001). In the patients without metastasis, the positive expression rate was 35.57%, which was lower than that in the patient with metastasis (100%, χ2=32.318, P<0.001). Therefore, we believe that the serum level of HE4 was positively linked with the HE4 expression in the tissues (Table 3).
Table 3.
Relationship between HE4 in tissue and pathological type, grading and clinical staging in group of malignant ovarian tumor
| HE4 | ||||
|---|---|---|---|---|
| Characteristics | positive | Total | χ2 | P |
| pathological type | ||||
| serous | 30 | 30 | 11.437 | <0.05 |
| mucous | 8 | 12 | ||
| hyaline cell cance | 2 | 3 | ||
| ovarian adenoendometrio carcinoma | 6 | 6 | ||
| corpus luteum cyst tumor | 1 | 4 | ||
| germ cell tumor | 3 | 4 | ||
| Pathological grade | ||||
| Low | 32 | 32 | 15.626 | <0.05 |
| Medium | 14 | 18 | ||
| High | 3 | 8 | ||
| Clinical stage | ||||
| Early stage | 16 | 24 | 10.787 | <0.05 |
| Later stage | 33 | 34 |
5. Discussion
Human epididymis protein 4 (HE4) is considered as an important serum biomarker in early diagnosis and identification for ovarian cancer. HE4, also known as the core epitope protein 2 (WFD2), belongs to the protease inhibiting family. It is located on chromosome 20q12~q13.1, constituted of five exons and four introns, with approximately 12 kb in length [4]. Some studies [5] indicated that HE4 is an N-glycosylated protein secreted from the ovarian cancer. Its molecular weight is about 25Kda, and the molecular weight of CA125 is about 200-1000Kda, which may explain why HE4 could be more easily secreted into the blood compared with CA125 in the early stage of ovarian cancer. Bingle et al [6] reported that, HE4 protein is not only expressed in ovarian cancer, but also in the normal tissues. However, there is significant difference between the groups, suggesting that HE4 protein is not a tumor-specific protein. This also provide basis that HE4 might be served as a novel biomarker to increase the diagnostic sensitivity of ovarian cancer.
Several clinical studies [7-9] including large samples suggested that HE4 detected by ELISA could be served as a biomarker for ovarian cancer, and its sensitivity and specificity were superior to CA125, regardless if at early or late stages of the disease. In addition, HE4 level also had good sensitivity in the ovarian cancer patients when monitoring the prognosis condition postoperatively. Recently, it was reported abroad that [10], the application of electrochemiluminescence assay to determine serum HE4 level had better sensitivity and specificity than CA125. They compared the electrochemiluminescence assay with ELISA method, and proposed that the two methods had similar clinical value, but the electrochemiluminescence method possessed higher accuracy. The results of our study showed that serum HE4 levels in malignant ovarian cancer group were markedly higher than the other groups, and the differences were statistically significant. Between any other two groups, the difference was not statistically significant (P>0.05). This indicated that serum HE4 had different distribution in benign or malignant ovarian cancer and may be used as an index to screen for ovarian cancer patients. It has been reported that [11], even in the CA125 negative ovarian cancer patients, there still existed 32% of these patients that could be detected as serum HE4 positive. It indicated that HE4 and CA125 showed different distributions in ovarian cancer patients and our study confirmed the speculation. Our results showed that in the malignant ovarian cancer group, there were 66.67% of serum CA125 negative cases showed HE4 positive, and 88.0% of serum CA125 positive cases showed serum HE4 negative. So we reckoned that HE4 and CA125 had different distributions and they were complementary. Combining detection of HE4 and CA125 in serum can minimize the rate of misdiagnosis, and improve the accuracy of early diagnosis of ovarian cancer. Meanwhile, when taking healthy women, patients with ovarian non-neoplastic lesions and benign ovarian tumors as the reference population, the detection rate of HE4 in no matter early and late stages of ovarian cancer were higher than that of CA125, suggesting that HE4 could perform better diagnosis capacity of the ovarian cancer at early stage than CA125 does.
The clinical application of CA125 to identify benign and malignant ovarian cancer lacks of specificity. In patients with endometriosis peritoneal disease, the serum CA125 level usually increases and the positive rate could be up to 53% [12]. So it is easy to misdiagnose the ovarian endometriosis as ovarian cancer, making great physical and psychological burden to patients. Huhtinen’s [13] study had shown that for serum HE4 level there was no significant difference between in ovarian chocolate cyst group and in the healthy cases. While the serum CA125 levels in ovarian chocolate cyst group was more elevated than healthy cases,. All these indicated that, compared with CA125, HE4 showed better diagnosis of ovarian cancer and ovarian endometriosis. This study also showed that the level of serum HE4 between ovarian non-neoplastic lesions and benign ovarian tumor group, the difference was not statistically significant, but it was significantly higher in malignant ovarian cancer patients. Serum CA125 levels in ovarian non-neoplastic lesion group was significantly increased compared with benign ovarian tumor group (P<0.01), which was consistent with the above findings. Our results demonstrated that serum CA125 level could be increased in both ovarian cancer and ovarian endometriosis patients, which might lead to diagnosis confusion of ovarian tumors. However, the serum HE4 level would serve as a better biomarker for identification of diseases, which could further reduce misdiagnosis and avoid unnecessary surgery and overtreatment.
It has been reported [14] that in healthy people, HE4 levels positively correlated with age and was significantly up-regulated in postmenopausal women. This study showed that serum HE4 level was not correlated with age, which might be explained by our limited samples and individual differences. The serum HE4 levels were higher in epithelial ovarian cancer than non-epithelial, in serous ovarian cancer than mucous ovarian cancer, indicating that different HE4 levels had certain prediction for pathological type of ovarian cancer. And it could be induced by the decreased secretion or destruction of HE4 by non-epithelial and mucous ovarian cancer cells. Serum HE4 levels were positively correlated with pathological grade, clinical stage, and the HE4 expression in tissues. Hence in a biological view, the up-regulation of HE4 may be associated with increased cell proliferation and resistance to apoptosis in ovarian cancer. Serum HE4 concentration to some extent reflects the clinical progress and prognosis of the ovarian cancer patients. The elevated HE4 protein may be a signal for poor prognosis of ovarian cancer.
Since there is still no clear reference value of serum HE4 by the electrochemiluminescence method in the Chinese Han population, our study used ROC curve to find the best HE4 cutoff point for diagnosis of ovarian cancer. Taking benign ovarian tumors, ovarian non-neoplastic lesions and healthy women as the reference populations, we found that 58.66pmol/L was the optimal cutoff value for serum HE4. When taking healthy women as the reference population, 31.08pmol/L may be the best cutoff value for serum HE4 levels. These results illustrated that the choice of the reference population is very important for establishing the cutoff value of HE4 level in the diagnosis. The diagnostic value of HE4 is better than CA125, whereas combined detection of these two makes sensitivity of 92.00%, which is the highest diagnostic efficiency. This was consistent with the previously research results domestically and abroard. Taking 150pmol/L described in the HE4 reagent instructions as the reference value, our finding of 31.08pmol/L as the cutoff value had significant different diagnostic sensitivity and specificity (P<0.05). These two diagnostic cutoff values of difference may be due to different sample selection and individual physical characteristics. In addition, the serum samples used in this study was frozen specimens, not fresh serum, which may make the concentration of serum HE4 artificially reduced. Our study showed that large-scale clinical validations should be taken in different regions and different races to establish optimal serum HE4 interval value for diagnosis of ovarian cancer.
The study by immunohistochemistry experiments showed that, HE4 was mainly up-regulated in malignant ovarian cancer group and borderline ovarian tumor group, but its expression in normal ovarian, benign ovarian tumors, ovarian non-neoplastic lesions was low or scattered. HE4 expression in malignant ovarian tissues were positively correlated with FIGO stage and the degree of differentiation. The patient with organ metastasis showed higher HE4 expression than those without metastasis, and correlated with the type of organization. This showed that with the progression of ovarian cancer, HE4 expression was increased, suggesting that HE4 protein may be involved in tumor cell invasion and metastasis. HE4 may be a predictor of poor prognosis in ovarian cancer. Adam’s [15] study showed that, as a member of WAP gene family, HE4 is highly expressed in ovarian cancer cells and associated with poor prognosis of ovarian cancer. HE4 protein may promote the invasion and metastasis of ovarian cancer at early stage, resulting in deterioration of disease progression.
This study showed that HE4 was highly expressed in serous ovarian cancer, ovarian endometrioid adenocarcinoma, but showed low levels in mucous ovarian cancer, ovarian clear-cell carcinoma and ovarian germ-cell tumors. Drapkin’s [16] study had found that, HE4 showed absent or low levels in most non-ovarian tumor tissues, and its expression was closely related with the tissue type of ovarian cancer. Our study showed that the expression of HE4 was low-to-moderate in mucous ovarian cancer, and some of these even showed no expression. Because of the limited cases, the conclusion may be different in general, which suggesting that pathogenesis, signal transduction pathways and gene expression activation of mucous ovarian cancer might be different with those of non-mucous ovarian cancer, and these needs further study. This showed that the expression of HE4 was closely related with the pathological types of ovarian cancer, and different types of ovarian cancer can be predicted depending on the expression levels of HE4.
In order to clarify whether the level of serum HE4 could represent the expression of HE4 levels in ovarian tissue, we performed correlation analysis of serum HE4 level with its expression in tissues. The results showed a positive correlation between them, indicating that the serum HE4 levels could represent the HE4 levels in ovarian tissues. But the results also showed that not all patients with high HE4 expression in ovarian cancer tissue emerged elevated serum HE4. In malignant ovarian cancer group, 49/58 cases showed positive expression of tissue HE4, but the corresponding positive serum HE4 only had 44 cases, leaving 5 cases negative, which including two cases of mucous ovarian cancer, 3 cases of dysgerminoma. We hence speculated that secretion of HE4 by ovarian tumors into the blood might be associated with different tumor cell genetypes. Different secreted proteins reflects differences in the biological behavior of tumor cells. The study also found that there were 2 cases of ovarian mucous carcinoma, 2 cases of ovarian serous tumors and 3 cases of ovarian endometriosis showing positive serum HE4 while without HE4 expressed in the counterpart tissues, which might be associated with protein degradation or technique mistakes in operating paraffin-embedded blocks of ovarian tissues. However, some people reported [16] that t HE4 can be detected in the blood circulation. The biological function of HE4 is unclear, and further research is still needed.
The effectiveness and diagnosis value interval of serum H4 level in ovarian cancer by applying electrochemiluminescence assay in Han population is currently unclear. There are few reports about the relationship between HE4 level and tumor development, metastasis and invasion. We believe that, along with the further study in ovarian cancer, HE4 would be an important biomarker in malignant ovarian cancer early monitoring, diagnosis and prognosis of ovarian cancer.
Footnotes
Conflict of interest statement: Authors state no conflict of interest.
References
- [1].Goh J, Mohan GR, Ladwa R, Ananda S, Cohen PA, Baron-Hay S. Frontline treatment of epithelial ovarian cancer. Asia Pac J Clin Oncol. 2015;11(6):1–16. doi: 10.1111/ajco.12449. [DOI] [PubMed] [Google Scholar]
- [2].Aebi S, Castiglione M. Newly and relapsed epithelial ovarian carcinoma: ESMO clinical recommendations for diagnosis, treatment and follow-up. Annals of oncology. 2009;20(4):21–23. doi: 10.1093/annonc/mdp117. [DOI] [PubMed] [Google Scholar]
- [3].Sjovall K, Nilsson B, Einhorn N. The significance of serum CA 125 elevation in malignant and nonmalignant diseases. Gynecol Oncol. 2002;85(1):175–178. doi: 10.1006/gyno.2002.6603. [DOI] [PubMed] [Google Scholar]
- [4].Zhang P, Wang C, Cheng L. et al. Comparison of HE4, CA125, and ROMA Diagnostic Accuracy: A Prospective and Multicenter Study for Chinese Women With Epithelial Ovarian Cancer. Medicine (Abingdon) 2015;94(52):e2402. doi: 10.1097/MD.0000000000002402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kirchhoff C, Habben I, Ivell R, Krull N. A major human epididymis-specific cDNA encodes a protein with sequence homology to extracellular proteinase inhibitors. Biol Reprod. 1991;45(2):350–357. doi: 10.1095/biolreprod45.2.350. [DOI] [PubMed] [Google Scholar]
- [6].Bingle L, Singleton V, Bingle CD. The putative ovarian tumour marker gene HE4 (WFDC2), is expressed in normal tissues and undergoes complex alternative splicing to yield multiple protein isoforms. Oncogene. 2002;21(17):2768–2773. doi: 10.1038/sj.onc.1205363. [DOI] [PubMed] [Google Scholar]
- [7].Angioli R, Capriglione S, Scaletta G, The role of HE4 in endometrial cancer recurrence: how to choose the optimal follow-up program. Tumour biology: the journal of the International Society for Oncodevelopmental Biology and Medicine; 2015. [DOI] [PubMed] [Google Scholar]
- [8].Manganaro L, Anastasi E, Porpora MG. et al. Biparametric Magnetic Resonance Imaging as an Adjunct to CA125 and HE4 to Improve Characterization of Large Ovarian Masses. Anticancer Res. 2015;35(11):6341–6351. [PubMed] [Google Scholar]
- [9].Gislefoss RE, Langseth H, Bolstad N, Nustad K, Morkrid L. HE4 as an Early Detection Biomarker of Epithelial Ovarian Cancer: Investigations in Prediagnostic Specimens From the Janus Serumbank. International journal of gynecological cancer : official journal of the International Gynecological Cancer Society. 2015;25(9):1608–1615. doi: 10.1097/IGC.0000000000000532. [DOI] [PubMed] [Google Scholar]
- [10].Dikmen ZG, Colak A, Dogan P, Tuncer S, Akbiyik F. Diagnostic performances of CA125, HE4, and ROMA index in ovarian cancer. Eur J Gynaecol Oncol. 2015;36(4):457–462. [PubMed] [Google Scholar]
- [11].Wong YL, Dali AZ, Mohamed RI, Jamal R, Mokhtar NM. Potential molecular signatures in epithelial ovarian cancer by genome wide expression profiling. Asia Pac J Clin Oncol. 2014 doi: 10.1111/ajco.12182. [DOI] [PubMed] [Google Scholar]
- [12].Jacobs I, Bast RC. The CA 125 tumour-associated antigen: a review of the literature. 1. Vol. 4. Human reproduction; Oxford, England: 1989. pp. 1–12. [DOI] [PubMed] [Google Scholar]
- [13].Huhtinen K, Suvitie P, Hiissa J. et al. Serum HE4 concentration differentiates malignant ovarian tumours from ovarian endometriotic cysts. Br J Cancer. 2009;100(8):1315–1319. doi: 10.1038/sj.bjc.6605011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Lowe KA, Shah C, Wallace E. et al. Effects of personal characteristics on serum CA125, mesothelin, and HE4 levels in healthy postmenopausal women at high-risk for ovarian cancer. Cancer epidemiology, biomarkers & prevention : a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. 2008;17(9):2480–2487. doi: 10.1158/1055-9965.EPI-08-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Clauss A, Ng V, Liu J, Overexpression of elafin in ovarian carcinoma is driven by genomic gains and activation of the nuclear factor kappaB pathway and is associated with poor overall survival. 2. Vol. 12. Neoplasia; New York, N.Y: 2010. pp. 161–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Drapkin R, von HHH, Lin Y. et al. Human epididymis protein 4 (HE4) is a secreted glycoprotein that is overexpressed by serous and endometrioid ovarian carcinomas. Cancer Res. 2005;65(6):2162–2169. doi: 10.1158/0008-5472.CAN-04-3924. [DOI] [PubMed] [Google Scholar]