Abstract
Garengeot’s hernia (GH) is defined as the presence of the appendix inside a femoral hernia. It occurs in 0.9% of femoral hernias and is usually an incidental finding during surgery. Its treatment is controversial and the aim of this article is to review the diagnostic methods and surgical considerations.
We report two cases diagnosed preoperatively by contrast-enhanced computed tomography (CT) and discuss the treatment options based on a review of the literature published in PubMed updated on 1 December, 2015.
Fifty articles reporting 64 patients (50 women, mean age 70 years) with GH were included in the analysis. Diagnosis was performed by preoperative CT in only 24 cases, including our two. The treatment of GH is emergency surgery. Several options are available laparoscopic or open approach: insertion of a mesh or simple herniorrhaphy, with or without appendectomy.
Conslusion
The preoperative diagnosis with CT can guide the choice of treatment. Appendectomy and hernioplasty should be performed via inguinotomy, if there is no perforation or abscess formation.
Keywords: Hernia, inguinal; Hernia, femoral; Amyand’s hernia; Garengeot’s hernia; Appendix; Appendicitis
1. Introduction
Garengeot’s hernia (GH) is defined as the presence of the appendix in a femoral hernia [1]. Less common is the finding of an acute appendicitis inside the femoral hernia sac. Although some cases have been diagnosed preoperatively, it is usually found incidentally during repair. We report two cases with preoperative diagnostic contrast-enhanced computed tomography (CT) and discuss the surgical considerations through a literature review.
2. Case Report 1
An 86-year-old female came to the emergency department with a 5-day history of a right-sided groin mass which had appeared after an episode of vomiting. The patient reported no change in bowel habits and no further episodes of vomiting. Her medical history included arthrosis treated with anti-inflammatory medication. On physical examination, her vital signs were stable and she was afebrile. The abdomen was soft and non-tender, with a painful right groin mass on palpation (approximately 5x3cm). There was no erythema or crepitus, nor any rebound or rigidity. Laboratory data on admission were as follows: white blood cells 6.28 x103/mm3, with 76.4% neutrophils, and C-reactive protein (CRP) 20.7 mg/L. Abdominal X- ray did not reveal any significant abnormality. A CT was performed and revealed a right femoral hernia with the vermiform appendix in the hernia sac and mural thickening. There were no signs of perforation or abscess (Figure 1).
Figure 1.
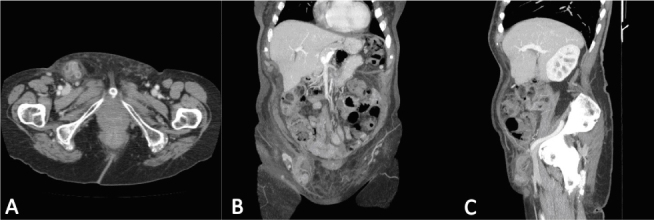
Case Report 1
Contrast-enhanced CT of the abdomen. (A) Axial view: tubular structure containing gas within the femoral hernia. (B) Coronal and (C) sagittal views: tubular structure extending from the caecal base.
An open exploration was chosen. Prior to surgery, the patient received 2g/200mg of amoxicillin/clavulanic acid i.v. and analgesia. Under general anaesthesia, the hernia sac was opened through a Gregoire incision and a phlegmonous appendix was found inside (Figure 2). An appendectomy was performed with a purse-string suture. The hernia sac was closed and the defect was repaired using a polypropylene mesh plug (Lichtenstein technique). Post-operative recovery was satisfactory, with three doses more of 1g/200mg amoxicillin/clavulanic acid i.v, and the patient was discharged on the third day. Histological examination of the appendix revealed acute appendicitis, as defined by infiltration of the appendicular muscularis propia by polymorphonuclear neutrophils. During the follow-up period of 20 months, the patient has not experienced complications or recurrence.
Figure 2.
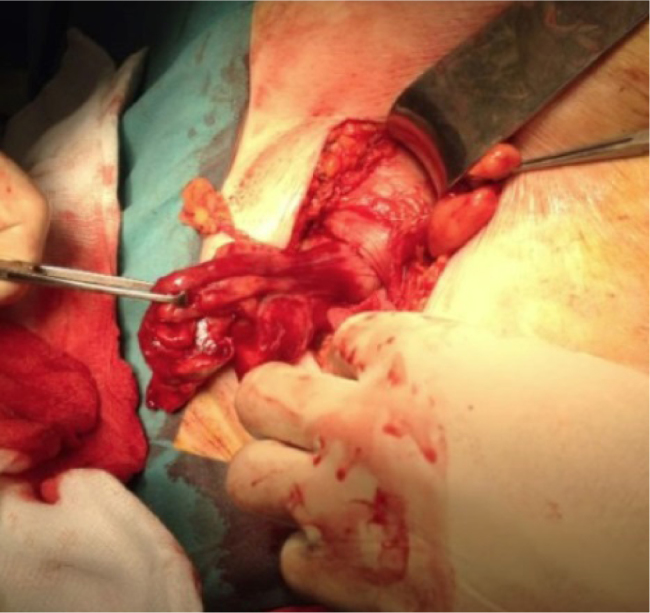
Case Report 1 Inflamed appendix inside the femoral hernia sac.
3. Case Report 2
A 77-year-old female was referred to the emergency department with diarrhea, vomiting and diffuse abdominal pain for two days. Her past medical history included hypertension, type 2 diabetes mellitus, dyslipemia, bronchial asthma, irritable bowel syndrome and hypothyroidism. On admission, the patient was haemodynamically stable and afebrile. Physical findings revealed a soft, non-distended abdomen with a tender mass in the right inguinal region measuring approximately 4x6cm. Laboratory tests showed a white blood cell count 12.30 x103/mm3, with 90.9% neutrophils, and CRP 2 mg/L. X- ray did not reveal bowel obstruction. A CT showed edematous appendix with an appendicolith inside it, in a right femoral hernia sac. The decision was taken to perform laparoscopic surgery. The patient received 2g/200mg of amoxicillin/clavulanic acid i.v. preoperatively. With general anaesthesia, an infraumbilical incision was made, and a pneumoperitoneum was obtained using Hasson’s open technique. A 5-mm abdominal port was placed suprapubically and a 12-mm port in the left iliac fossa. A 10-mm, 30-degree telescope was used to examine the abdominal cavity. A large portion of the appendix, which had undergone necrosis and perforated, was seen to pass through the femoral defect from where purulent fluid was evacuated. The mesoappendix was stapled and transected with a tissue sealing generator, and the base of the appendix with a linear cutter stapler. The femoral defect was repaired primarily with an absorbable suture. Post-operative recovery was uneventful and the patient was discharged on the sixth postoperative day. Histology showed acute ischaemic and necrotic appendicitis with perforation. During eight months of follow-up, the patient has not experienced complications.
Figure 3.
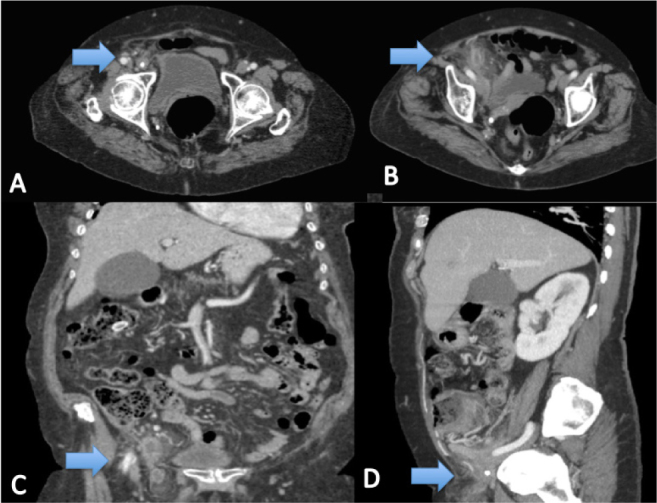
A, B, C, D Case Report 2. CT images Arrow: Appendix
4. Discussion
Garengeot’s hernia was first described in 1731 by Rene Jacques Croissant de Garengeot [1] and it accounts for 0.9% of femoral hernia repairs [2]. Moreover, acute appendicitis inside the sac is found in 0.08-0.13% of femoral hernias [3]. The first appendectomy in a GH was performed by Hevin in 1785 [4]. The difference with regard to Amyand’s hernia is that in the latter case the acute appendicitis is found in an inguinal hernia; it is named after the English surgeon Claudius Amyand, who performed the first appendectomy in an inguinal hernia sac in 1735 [4].
An unlimited literature search of the PubMed data base was performed on 1 December, 2015 with the following search criteria: ((Garengeot’s hernia) OR (Amyand’s hernia) OR (Hernia)) AND (Appendix). The search yielded 546 results. We initially identified 136 studies relevant to the subject, of which 81 were eligible for our analysis. The references of the selected studies were checked. We found 64 cases, 22 of them diagnosed on the basis of CT findings. The results of the review are listed in Table 1 [2,4,5-52].
Table 1.
Cumulative presentation of cases included.
| Author | Age | Sex | CT | Surgery | Mesh | Appendix |
|---|---|---|---|---|---|---|
| Shands AR et al (1903) [5]. | 29 | F | No | Open | No | NA |
| Gerami S et al (1970) [6]. | 71 | M | No | Open | No | perforated AA |
| Voitk AJ et al. (1974) [7]. | 59 | F | No | Open | No | Enterocutaneous fistula |
| Voitk AJ et al. (1974) [7]. | 76 | F | No | Open | No | perforated AA |
| Cutolo L et al (1978) [8]. | 78 | F | No | Open | No | gangrenous and perforated AA |
| Guirguis EM et al (1989) [9]. | 80 | F | No | NA | NA | gangrenous AA |
| Zissin L et al (2000)[10]. | 87 | F | Yes | Open | Yes | perforated AA |
| Isaacs LE et al (2002) [11]. | 76 | M | No | Open | No | NA |
| Mansari O et al (2002) [12]. | 60 | F | No | Open | No | catharral AA |
| Nguyen ET et al (2004) [13]. | 88 | M | No | Open | No | perforated AA |
| Barbaros U et al (2004) [14]. | 85 | F | No | Open | Yes | gangrenous AA |
| Fukukura Y et al (2005) [15]. | 54 | F | Yes | Open | No | phlegmonous AA |
| Priego P et al (2005) [16]. | 78 | F | No | Open | Yes | AA |
| Priego P et al (2005) [16]. | 83 | F | No | Open | No | AA |
| Priego P et al (2005) [16]. | 75 | F | No | Open | Yes | AA |
| Priego P et al (2005) [16]. | 75 | F | No | Open | No | AA |
| Priego P et al (2005) [16]. | 82 | F | No | Open | No | Normal |
| Priego P et al (2005) [16]. | 80 | F | No | Open | Yes | Normal |
| Akopian G et al (2005) [4] | 81 | F | No | Open | Yes | AA |
| D’Ambrosio N et al (2006) [17]. | 71 | F | Yes | NA | NA | perforated AA. Right hemicolectomy |
| Comman A et al (2007) [18]. | 38 | F | No | Laparoscopic | Yes | AA |
| Gillion JF et al (2007) [19]. | NA | NA | Yes | NA | NA | NA |
| Sharma H et al (2007) [20]. | NA | F | No | Open | ||
| Sharma H et al (2007) [20]. | NA | F | No | Open | 4 Yes | 1 perforated AA |
| Sharma H et al (2007) [20]. | NA | F | No | Open | 3 No | |
| Sharma H et al (2007) [20]. | NA | F | No | Open | ||
| Sharma H et al (2007) [20]. | NA | M | No | Open | ||
| Sharma H et al (2007) [20]. | NA | M | No | Open | ||
| Sharma H et al (2007) [20]. | NA | M | No | Open | ||
| Maizlin ZV et al (2007) [21]. | 83 | F | Yes | NA | NA | NA |
| Kibil W et al (2008) [22]. | NA | NA | NA | NA | NA | NA |
| Chung A et al (2009) [23]. | 83 | F | No | Open | No | necrotic AA |
| Ebisawa K et al (2009) [24]. | 90 | F | Yes | Open | Yes | AA |
| Thomas B et al (2009) [25]. | 77 | F | Yes | Both | No | AA |
| Ring A et al (2009) [26]. | 69 | F | NA | NA | NA | NA |
| Shah A et al (2010) [27]. | 46 | F | Yes | Both | No | AA |
| Caygill P et al (2011) [28]. | 78 | F | No | Open | No | AA |
| Konofaos P et al (2011) [2] | 60 | F | No | Open | Yes | gangrenous AA |
| Piperos P et al (2012) [29]. | 83 | F | No | Open | No | AA |
| Allen BC et al (2012) [30]. | 76 | F | Yes | Open | Yes | No appendectomy |
| Phillips AW et al (2012) [31]. | 73 | F | Yes | Open | No | AA |
| Salkade PR et al (2012) [32]. | 67 | F | Yes | Open | No | AA |
| Coskun K et al (2013) [33]. | 65 | F | Yes | Open | No | AA |
| Sen C et al (2013) [34]. | 58 | F | Yes | Open | No | gangrenous AA |
| Hamcan S et al (2013) [35]. | 66 | F | Yes | NA | NA | perforated AA |
| Moris D (2013) [36]. | 49 | F | No | Open | No | AA |
| Erdas E et al (2013) [37]. | 33 | F | No | Open | Yes | AA |
| Ardeleanu V et al (2013) [38]. | 76 | F | No | Open | No | AA |
| Beysens M et al (2013) [39]. | 64 | F | No | Laparoscopic | Yes | NA |
| Ramsingh J et al (2014) [40]. | 70 | F | Yes | Both | Yes | AA |
| Schäfer HM et al (2014) [41]. | 71 | F | No | Open | No | AA |
| Madiha A et al (2014) [42]. | 79 | F | No | Open | No | AA |
| Hao J et al (2014) [43]. | 81 | F | Yes | Open | Yes | Normal |
| Akbari K et al (2014) [44]. | 80 | F | No | Open | No | NA |
| Akbari K et al (2014) [44]. | 54 | F | No | Open | No | NA |
| Akbari K et al (2014) [44]. | 68 | F | Yes | Open | No | NA |
| Ahmed K et al (2014) [45]. | 71 | M | Yes | Open | No | AA perforated |
| Le H et al (2014) [46]. | 91 | F | Yes | Open | No | AA |
| Hussain A et al (2014) [47]. | 86 | F | No | Open | No | AA necrotic |
| Snoeks R et al (2014) [48]. | 76 | F | Yes | Laparoscopic | No | AA |
| Liipo TK et al (2015) [49]. | 60 | M | Yes | Open | Yes | AA |
| Talini C et al (2015) [50]. | 86 | M | No | Open | Yes | Normal |
| Pan CW et al (2015) [51]. | 50 | F | Yes | Open | Yes | gangrenous AA |
| Tancredi K et al (2015) [52]. | 85 | M | No | Open | No | AA |
| García-Amador C et al. (2015) | 86 | F | Yes | Open | Yes | phlegmonous AA |
| García-Amador C et al. (2015) | 77 | F | Yes | Laparoscopic | No | perforated AA |
NA= no available. AA=acute appendicitis.
Garengeot’s hernia is a rare occurrence. Two possible aetiologies have been proposed. According to the first theory, the appendix may be in an abnormal anatomical position owing to different degrees of intestinal rotation during embryological development, or to variations in caecal attachments. The second theory suggests that an anatomically large caecum forces the appendix into the pelvis, which therefore has a high risk of entering a hernial sac from the pelvic peritoneum [28]. The inflammatory process of the appendix is usually caused by the extraluminal obstruction of the appendix at the hernial neck, rather than by the more usual cause of intraluminal obstruction [10]. The obstruction of the neck leads to a vascular compromise which allows bacterial overgrowth [53]. Our case reports reflect the two presentations; in the first one, no obvious intraluminal obstruction was noted, and in the second an appendicolith was identified.
The female-to-male incidence ratio of GH is 5:1 with an age range from 29 to 91 years old (mean age 70). GH has been attributed to body changes during pregnancy. Other risk factors include increased intra-abdominal pressure, smoking, age and collagen disease. Most GHs occur on the right side [54]. Weakening of the transversalis fascia is also thought to play a role.
The clinical presentation usually takes the form of an incarcerated or strangulated femoral hernia and a painful groin mass. Abdominal pain, nausea, vomiting and diarrhoea are not usually reported. The narrowness and rigidity of the femoral canal usually prevents intraperitoneal spread of infection, and so there are no symptoms of peritonitis. Laboratory tests often show leucocytosis and elevated CRP [20]. X ray findings are usually nonspecific, but assist in recognizing small bowel obstruction if present.
In addition to inguinal hernia the differential diagnosis should include adnexitis, ectasia of the vena saphena magna, lymphomas, lipomas or other soft tissue tumors or a varix node [18].
Because of the rarity of the entity and the absence of the typical symptoms associated with acute appendicitis, achieving preoperative diagnosis is very difficult. Most patients are rushed to the surgical room with the inconclusive diagnosis of an incarcerated hernia. Most GH are diagnosed intraoperatively. Preoperative diagnosis by CT has been reported in only 24 cases, including the two case reports we present here. In our review, one more case was diagnosed using ultrasound [14].
In CT findings, GH should be considered when intramural air is present in an incarcerated femoral hernia sac without signs of bowel obstruction [24]. Therefore, a low-positioned caecum with a blind-ended tubular structure within the hernia sac and stranding of nearby fat on CT has been reported to have 98% sensitivity and specificity for the diagnosis of appendicitis inside a hernia sac [46].
The treatment of this disease is emergency surgery. Due to the rarity of the condition there is no standard procedure. The options available include laparoscopic or open approaches either with a mesh or simple herniorrhaphy, with or without appendectomy. In our review, most cases were performed via an open approach. Appendectomy via the hernial sac is considered appropriate; in case of perforation and abscess formation, a transabdominal access is preferred [24]. A combined approach was used in only three cases, all of which had been diagnosed preoperatively using CT. In two of them, the appendix was removed laparoscopically and the femoral hernia was repaired via a laparotomic approach [25,40]. In the other, laparoscopic drainage of the abscess and adhesiolysis were performed followed by a laparotomy for the appendectomy and herniorrhaphy [27].
Laparoscopy may be a valid technique for determining the condition of the hernia, but due to the difficulty of preoperative diagnosis it is unlikely to be the first choice for the surgical approach. In fact, in our review only three cases underwent laparoscopy [18,39,48], and only one of them had a preoperative diagnosis of GH [39].
In our two cases, the first one was treated via laparotomy and the second by laparoscopy. Both cases had been diagnosed preoperatively on the basis of the CT findings.
The appendectomy procedure is also controversial. It has been suggested that in the presence of a normal appendix appendectomy is not required. However, the surgery is not excessively complicated, and even in the absence of macroscopic inflammation the presence of microscopic inflammation from compression and ischemia within the hernia neck cannot be ruled out; for this reason, appendectomy should be performed [16]. In our review, the appendix was left in place in only one case [30].
Another controversial point is the use of a mesh, which was reported in only 55 cases in our review; in 35 a herniorrhaphy was performed. In the absence of abscess formation or perforation, the implantation of a mesh has been described as the hernia repair of choice [24]. In our first case, the surgery was performed immediately and there was no abscess formation in the hernia sac; a simultaneous appendectomy and primary hernioplasty using synthetic mesh was chosen. In the second case, as purulent fluid was evacuated, a herniorrhaphy was preferred.
The most important contributing factor to the increase in wound infection is delayed diagnosis [43]. The reported infection rates reached 29%, while severe complications such as necrotizing fasciitis and death were only rarely described [20].
5. Conclusion
GH is a rare condition which requires prompt treatment in order to avoid complications. Preoperative diagnosis with CT can indicate the correct management, that is, appendectomy via inguinotomy and hernioplasty if there is no perforation or abscess formation. More studies of procedures using the laparoscopic approach are required, especially in relation to the incidence of wound infection.
The Authors have no conflict of interest
Conflict of interest statement
Authors state no conflict of interest.
Contributor Information
Cristina Garcia-Amador, Email: cristina_ga_@hotmail.com.
Jose Ramia, Email: jose_ramia@hotmail.com.
References
- [1].De Garengeot RJC. Traite des operations de chirurgie. 2nd Ed. Paris, Huart: 1731. pp. 369–371. [Google Scholar]
- [2].Konofaos P., Spartalis E, Smirnis A., Kontzoglou K., Kouraklis G.. De Garengeot’s hernia in a 60-year-old woman: a case report. Journal of Medical Case Reports. 2011;5:258. doi: 10.1186/1752-1947-5-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Rajan S.S., Girn H.R., Ainslie W.G.. Inflamed appendix in a femoral hernia sac: de Garengeot’s hernia. Hernia. 2009;13(5):551–553. doi: 10.1007/s10029-009-0472-7. [DOI] [PubMed] [Google Scholar]
- [4].Akopian G., Alexander M.. De Garengeot Hernia. Appendicitis within a Femoral Hernia. Am Surg. 2005;71(6):526–527. [PubMed] [Google Scholar]
- [5].Shands A.R.. Inflamed Appendix in the Sac of a Femoral Hernia. Ann Surg. 1904;40(3):380–381. [PMC free article] [PubMed] [Google Scholar]
- [6].Gerami S, Easley G.W., Mendoza C.B.. Appendiceal abscess as contents of right femoral hernia. A case report. International Surgery. 1970;53(5):354–356. [PubMed] [Google Scholar]
- [7].Voitk A.J., MacFarlane J.K., Estrada R.L.. Ruptured appendicitis in femoral hernias: report of two cases and review of the literature. Ann Surg. 1974;179(1):24–26. doi: 10.1097/00000658-197401000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Cutolo L., Wasserman I., Pinck R., Mainzer R.A.. Acute suppurative appendicitis occurring within a femoral hernia: report of a case. Dis Colon Rectum. 1978;1(3):203–204. doi: 10.1007/BF02586573. [DOI] [PubMed] [Google Scholar]
- [9].Guirguis E.M., Taylor G.A., Chadwick C.D.. Femoral appendicitis: an unusual case. Can J Surg. 1989;32(5):380–381. [PubMed] [Google Scholar]
- [10].Zissin R., Brautbar O., Shapiro-Feinberg M.. CT diagnosis of acute appendicitis in a femoral hernia. Br J Radiol. 2000;73(873):1013–1014. doi: 10.1259/bjr.73.873.11064659. [DOI] [PubMed] [Google Scholar]
- [11].Isaacs L.E., Felsenstein C.H.. Acute appendicitis in a femoral hernia: an unusual presentation of a groin mass. J Emerg Med. 2002;23(1):15–18. doi: 10.1016/s0736-4679(02)00455-9. [DOI] [PubMed] [Google Scholar]
- [12].Mansari O., Sakit F., Janati M.I.. Accute apendicitis on crural hernia. Presse Med. 2002;31(24):1129–1130. [PubMed] [Google Scholar]
- [13].Nguyen E.T., Komenaka I.K.. Strangulated femoral hernia containing a perforated appendix. Can J Surg. 2004;47(1):68–69. [PMC free article] [PubMed] [Google Scholar]
- [14].Barbaros U., Asoglu O., Seven R., Kalayci M.. Appendicitis in incarcerated femoral hernia. Hernia. 2004;8(3):281–282. doi: 10.1007/s10029-004-0209-6. [DOI] [PubMed] [Google Scholar]
- [15].Fukukura Y., Chang S.D.. Acute appendicitis within a femoral hernia: multidetector CT findings. Abdom Imaging. 2005;30(5):620–622. doi: 10.1007/s00261-004-0283-3. [DOI] [PubMed] [Google Scholar]
- [16].Priego P., Lobo E., Moreno I., Sánchez-Picot S., Gil M.A., Alonso N.. et al. Acute apendicitis in an incarcerated crural hernia: analysis of our experience. Rev Esp Enferm Dig. 2005;97(10):707–715. doi: 10.4321/s1130-01082005001000004. [DOI] [PubMed] [Google Scholar]
- [17].D’Ambrosio N., Katz Z., Hines J.. Perforated appendix within a femoral hernia. AJR. 2006;186(3):906–907. doi: 10.2214/AJR.05.0080. [DOI] [PubMed] [Google Scholar]
- [18].Comman A., Gaetzschmann P., Hanner T., Behrend M.. DeGarengeot hernia: transabdominal preperitoneal hernia repair and appendectomy. JSLS. 2007;11(4):496–501. [PMC free article] [PubMed] [Google Scholar]
- [19].Gillion J.F., Bornet G., Hamrouni A., Julles M.C., Convard J.P.. Amyand and de Garengeot’hernias. Hernia. 2007;11:289–290. doi: 10.1007/s10029-007-0221-8. [DOI] [PubMed] [Google Scholar]
- [20].Sharma H., Jha P.K., Shekhawat N.S., Memon B., Memon M.A.. De Garengeot hernia: an analysis of our experience. Hernia. 2007;11(3):235–238. doi: 10.1007/s10029-007-0208-5. [DOI] [PubMed] [Google Scholar]
- [21].Maizlin Z.V., Mason A.C., Brown C., Brown J.A.. CT findings of normal and inflamed appendix in groin hernia. Emerg Radiol. 2007;14(2):97–100. doi: 10.1007/s10140-007-0601-5. [DOI] [PubMed] [Google Scholar]
- [22].Kibil W., Jedrys J., Matyja A., Legutko J., Kulig J.. Appendix incarcerated in femoral hernia-case report. Folia Med Cracov. 2008;49(1-2):45–48. [PubMed] [Google Scholar]
- [23].Chung A., Goel A.. Images in clinical medicine. De Garengeot’s hernia. N Engl J Med. 2009;361(11):18. doi: 10.1056/NEJMicm0802611. [DOI] [PubMed] [Google Scholar]
- [24].Ebisawa K., Yamazaki S., Kimura, Kashio M., Kurito K., Yasumuro S.. et al. Acute appendicitis in an incarcerated femoral hernia: a case of de Garengeot hernia. Case Rep Gastroenterol. 2009;3(3):313–317. doi: 10.1159/000250821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Thomas B., Thomas M., McVay B., Chivate J.. De Garengeot hernia. JSLS. 2009;13(3):455–457. [PMC free article] [PubMed] [Google Scholar]
- [26].Ring A., Gelis V., Klupscha C., Stenr J.. De Garengeot appendicitis-rare variant of a common medical condition. Zentralbl Chirm. 2009;134(6):564–566. doi: 10.1055/s-0029-1224564. [DOI] [PubMed] [Google Scholar]
- [27].Shah A., Janardhan H.S.. De Garengeot hernia: a case report and review of literature. Indian J Surg. 2013;75(Suppl 1):439–441. doi: 10.1007/s12262-012-0778-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Caygill P., Nair R., Sajjanshetty M., Francis D.. An unusual groin exploration: de Garengeot’s hernia. Int J Surg Case Rep. 2011;2(5):74–75. doi: 10.1016/j.ijscr.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Piperos T., Kalles V., Al Awhal Y., Konstantinou E., Skarpas G., Mariolis-Sapsakos T.. Clinical significance of de Garengeot’s hernia: a case of acute appendicitis and review of the literature. Int J Surg Case Rep. 2012;3(3):116–117. doi: 10.1016/j.ijscr.2011.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Allen B.C., Kirsch J., Szomstein S.. De Garengeot Hernia. Radiology. 2012;265(2):640–644. doi: 10.1148/radiol.12102051. [DOI] [PubMed] [Google Scholar]
- [31].Phillips A.W., Aspinall S.R.. Appendicitis and Meckel’s diverticulum in a femoral hernia: simultaneous De Garengeot and Littre’s hernia. Hernia. 2012;16(6):727–729. doi: 10.1007/s10029-011-0812-2. [DOI] [PubMed] [Google Scholar]
- [32].Salkade P.R., Chung A.Y., Law Y.M.. De Garengeot’s hernia.: an unusual right groin mass due to acute appendicitis in an incarcerated femoral hernia. Hong Kong Med J. 2012;18(5):442–445. [PubMed] [Google Scholar]
- [33].Coskun K., Kilbas Z., Yigit T., Simsek A., Harlak A.. De Garengeot’s hernia: the importance of early diagnosis and its complications. Hernia. 2012;16(6):731–733. doi: 10.1007/s10029-011-0814-0. [DOI] [PubMed] [Google Scholar]
- [34].Sen C., Tanrikulu Y., Akkapulu N.. De Garengeot’s hernia: a case of acute appendicitis in a femoral hernia sac. Ulus Travma Acil Cerrahi Derg. 2013;19(4):380–382. doi: 10.5505/tjtes.2013.37043. [DOI] [PubMed] [Google Scholar]
- [35].Hamcan S., Akgun V., Battal B., Karaman B.. Acute perforated appendicitis in femoral hernia sac: CT imaging findings. BMJ Case Rep. 2013 doi: 10.1136/bcr-2013-200050. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Moris D.. De Garengeot’s Hernia. Brief Reportd. 2013:11. [Google Scholar]
- [37].Erdas E., Sias L., Licheri S., Secci L., Aresu S., Barbarossa M.. et al. De Garengeot hernia with acute appendicitis. G Chir. 2013;34(3):86–89. [PubMed] [Google Scholar]
- [38].Ardeleanu V., Chicos S., Tutnaru D.. A rare case of acute abdomen: Garengeot hernia. Chirurgia Bucur. 2013;108(6):896–899. [PubMed] [Google Scholar]
- [39].Beysens M., Haeck L., Vindevoghel K.. Laparoscopic appendectomy combined with TEP for de Garengeot hernia: case report. Acta Chir Belg. 2013;113(6):468–470. [PubMed] [Google Scholar]
- [40].Ramsingh J., Ali A., Cameron C., Al-Ani A., Hodnett R., Chorushyj C.. De Garengeot’s hernia: diagnosis and surgical management of a rare type of femoral hernia. J Surg Case Rep. 2014 doi: 10.1093/jscr/rju008. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Schäfer H.M., von Holzen U., Nebiker C.. Swelling of the right thigh for over 30 years-The rare finding of a De Garengeot hernia. Int J Surg Case Rep. 2014;5(12):1120–1122. doi: 10.1016/j.ijscr.2014.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Madiha A., Rares H., Abdus S.. De Garengeot hernia: a forgotten rare entity? BMJ Case Rep. 2014 doi: 10.1136/bcr-2013-201413. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Hao J., Yao J., Guo D., Sun W., Liang J., Jiang X.. De Garengeot hernia: the ultrasound and computed tomographic findings in an 81-year-old woman. Am J Emerg Med. 2014;32(5):486. doi: 10.1016/j.ajem.2013.11.003. [DOI] [PubMed] [Google Scholar]
- [44].Akbari K., Wood C., Hammad A., Midletton S.. De Garengeot’s hernia: our experience of three cases and literature review. BMJ Case Rep. 2014 doi: 10.1136/bcr-2014-205031. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Ahmed K., Bashar K., McHugh T.J.. Appendicitis in De Garengeot’s Hernia Presenting as a Nontender Inguinal Mass: Case Report and Review of the Literature. Case Rep Surg. 2014 doi: 10.1155/2014/932638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Le H., Odom SR., Hsu A., Gupta A., Hauser C.J.. A combined Richter’s and de Garengeot’s hernia. Int J Surg Case Rep. 2014;5:662–664. doi: 10.1016/j.ijscr.2014.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Hussain A., Slesser A.A., Monib S., Maalo J., Soskin M., Arbuckle J.. A De Garengeot Hernia masquerading as a strangulated femoral hernia. Int J Surg Case Rep. 2014;5(10):656–658. doi: 10.1016/j.ijscr.2014.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Snoekx R., Geyskens P.. De Garengeot’s Hernia : Acute Appendicitis in a Femoral Hernia. Case Report and Literature Overview Acta Chir Belg. 2014;114:149–151. [PubMed] [Google Scholar]
- [49].Liipo T.K., Seppälä T.T., Mattila A.. De Garengeot’s hernia: 40 years after Bassini inguinal hernioplasty. BMJ Case Rep. 2015 doi: 10.1136/bcr-2014-208327. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Talini C., Oliveira L.O., Araújo A.. De Garengeot hernia: Case report and review. Int J Surg Case Rep. 2015 doi: 10.1016/j.ijscr.2014.12.042. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Pan C.W., Tsao M.J., Su C.S.. A case of De Garengeot hernia requiring early surgery. BMJ Case Rep. 2015 doi: 10.1136/bcr-2015-211102. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Tancredi A., Bellagamba R., Cotugno M., Impagnatiello E., Torre P., Masi M.. et al. De Garengeot’s Hernia: a Diagnostic Challenge. Indian J Surg. 2015 doi: 10.1007/s12262-015-1266-z. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Muffak K., Ramia J.M., Palomeque A., Segura M., Muñoz N., Garrote D., Ferron J.A.. Hernia de Aymand. Cir And. 2004;15:155–156. [Google Scholar]
- [54].Kalles V., Mekras A., Mekras D., Papapanagiotou I., Harethee W., Sotiropoulos G.. et al. De Garengeot’s hernia: a comprenhensive review. Hernia. 2013;17:177–182. doi: 10.1007/s10029-012-0993-3. [DOI] [PubMed] [Google Scholar]


