Abstract
Background
Video assisted thoracoscopic (VATS) lobectomy has a demanding learning curve due to its technical complexity and risk of uncontrollable bleeding. We investigated the case number required for gaining technical proficiency by applying cumulative sum analysis on initial VATS lobectomy operations of a single surgeon.
Methods
CALGB definition was used for the definition of VATS lobectomy. The data of the initial cases evaluated and cumulative sum (CUSUM) analysis was applied to duration of the operations and length of hospital stay.
Results
Fifty-eight patients underwent VATS lobectomy. Of those 51 were malignant and 7 were benign. Fifty-five of the procedures were lobectomy, 2 were inferior bi-lobectomy and 1 was left upper lobectomy with chest wall resection. CUSUM analysis reached to proficiency at 27 cases for duration of the operations.
Conclusions
The length of learning curve depends on previous experience of the surgeon on open lobectomy and simpler VATS operations, potential number of VATS lobectomy cases and VATS capability of the surgeon. Depending on these factors, it is possible to obtain technical proficiency with an inferior number of procedures compared with existing literature (50-200).
Keywords: Videothoracoscopic lobectomy, Cumulative sum analysis, Technical proficiency
Introduction
Surgery remains the best option for cure in the treatment of non-small cell lung cancer (NSCLC), and lobectomy continues to be the gold standard in early stage NSCLC [1]. However while accessing the internal organs during the surgery some healthy tissue should be cut and sacrificed causing a surgical trauma. The cosmetic sequels and partly the morbidity are related with this surgical trauma. With the introduction of cold light source and endoscopic cameras surgeons improved the idea of decreasing surgical trauma with minimizing surgical access incisions.
The first VATS (Video Assisted Thoracoscopic Surgery) lobectomy was performed in 1991 [2,3]. After this first case the prosecution of VATS lobectomy has been rather slow. In spite of obvious advantages, the slow adoption is considered by many to be due to a demanding learning curve. The operation is considered technically demanding and has the risk of uncontrollable bleeding [3]. After 2005 VATS gained popularity and interested surgeons experienced a transition from open to VATS lobectomy. This experience was obtained with a learning curve.
The evaluation of technical proficiency in a specific operation is a difficult work [4]. Cumulative sum (CUSUM) is a graphical method of quality control which provides objective evidence on a case-by-case basis and shows changes in competence over time [5]. The analysis plots the sequential difference of a set of measured values and to define a target level for those values [4,6]. Surgeons can be objectively evaluated for a certain procedure with the establishment of the learning curve [4].
In this study we have applied the CUSUM analysis on initial VATS lobectomy operations of a single surgeon in order to find a target case number for gaining the technical proficiency.
1. Material and methods
Patient characteristics: The VATS lobectomy program was started on April 2012 and operations were performed by a single surgeon (S.G.). He had an extensive experience on open lung resections and VATS procedures before beginning VATS lobectomies and was not supervised by any other VATS lobectomy surgeon. The VATS lobectomy is accepted as a lung lobectomy with a maximum length of 8 cm for the utility incision, no use of rib-spreading, individual dissection of pulmonary vessels and bronchus, standard node dissection or sampling according to CALGB definition [7]. All patients who underwent VATS lobectomy for malignant and benign diseases included in the study. The records of the patients were evaluated for patient characteristics such as age, sex, preoperative and postoperative diagnosis, type of operations, duration of operations, duration of hospital stay, postoperative complications and mortality and stages for lung cancer patients.
Operative technique: The patients were intubated with double lumen endotracheal tubes for single lung ventilation and positioned in classical lateral decubitus position. In first cases 4 ports, later 3 and eventually -with increasing in experience-2 ports were used. One of the ports was utility incision which is 3 to 5 cm in length and just lateral to nipple or breast, generally in 5th intercostal space. Other port was 10 mm incision on anterior axillary line in 8th intercostal space for camera and stapler application. Energy devices were used for dissection. Pulmonary veins, arteries and bronchus were dissected and stapled (sometimes clipped or ligated) individually. Endoscopic staplers were used for stapling. Also incomplete fissures were divided with staplers. The specimens were removed from the thoracic cage with endoscopic bags. Lymph node dissection was performed in malignant cases. One thorax tube was settled through basal camera port.
Statistics: A CUSUM analysis was performed for duration of the operation and duration of the hospital stay. The results were presented in CUSUM charts which are basically a graphical presentation of the course of outcomes of a series of consecutive procedures performed over time. The CUSUM curve runs randomly at or above a horizontal line at an acceptable level of performance (no slope). However, the CUSUM curve slopes upward and will eventually cross a decision interval when an operation is performed at an unacceptable level. These are horizontal lines drawn across a CUSUM chart. The degree of the slope is a measure of surgeon’s progress in mastering the new skill: the greater the slope, the slower the progress. It is understood that he has mastered the new skill when the curve eventually flattens (no slope) [8]. Since the surgeon is competent from the beginning of the program, this point was accepted as the case number where proficiency was obtained.
Ethical approval: The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board or equivalent committee.
Informed consent: Informed consent has been obtained from all individuals included in this study.
Ethical approval: The research related to human use has been complied with all the relevant national regulations, institutional policies and in accordance the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board or equivalent committee.
2. Results
Fifty-eight patients were undergone VATS lobectomy between April 2012 and July 2015. Of the patients 12 were female and 46 were male with a mean age of 55 (17-78). Seven patients were operated for benign diseases and 51 were malignant. Of benign cases 5 were bronchiectasis, 1 actinomyces and 1 hamartoma. Of malignant cases 48 were non-small cell lung cancer, 2 carcinoid tumor and 1 adenoid cystic carcinoma. Fifty-five of the procedures were lobectomy, 2 were inferior bi-lobectomy (right middle and lower lobectomy together) and 1 was left upper lobectomy with chest wall resection. Four ports in 6 cases, 3 ports in 22 cases and 2 ports in 30 cases were used in operations. Mean tumor diameter was 3,6 cm (1-9 cm) in malignant cases. Mean operation time was 154 minutes (95-270 minutes) and mean hospital stay was 8,8 days (4-22 days). Thirteen patients were complicated postoperatively. Of those 10 were prolonged air leak, 2 atelectasis and 1 pneu-monia. Any operative mortality was not encountered. Postoperative pathological stages of malignant cases were differed between stage IA and IIIA. In CUSUM analysis for duration of the operations, the horizontal line was achieved in 27 cases which is the point where proficiency is obtained (Graph 1). However, the proficiency could not be achieved for length of hospital stay (Graph 2).
Graph 1.
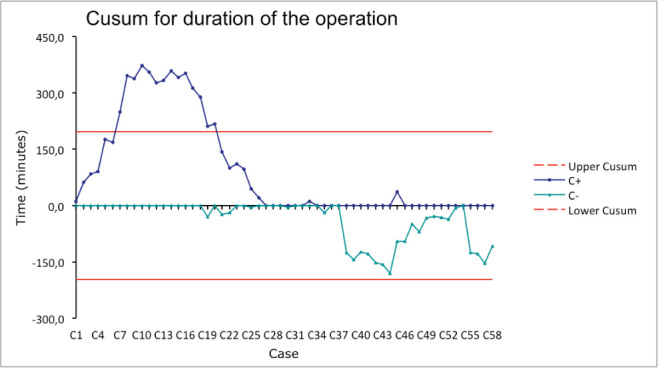
CUSUM chart for durations of the operations. Consistency (no slope) is being reached at 27 cases presenting the target number for technical proficiency of VATS lobectomy.
Graph 2.
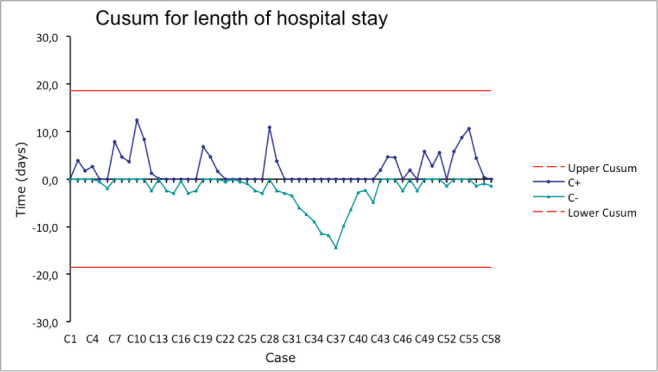
CUSUM chart for length of hospital stay. Consistency could not be reached.
3. Discussion
International VATS Lobectomy Consensus Group prepared a consensus and accepted the definition of VATS lobectomy as “no use of rib-spreading; a maximum length of 8 cm for the utility incision; individual dissection of pulmonary vessels and bronchus; standard node sampling or dissection” regarding the CALGB definition. Also 18% of the Group contributors stated that a small retractor should be acceptable when delivering a large specimen and conducting complex procedures (e.g., sleeve resection) [9].
The Consensus indicated the VATS lobectomy for tumor size ≤ 7 cm, indicated for N0/N1 disease, contrain-dicated if tumor invades rib(s), relatively contraindicated if tumor invades hilar structures. It was not a contraindication in patients who had previous thoracic surgery and/ or pleurisy. Also they contraindicated if FEV1 is < 30% and DLCO is < 30% [9].
In our surgical program we used same CALGB definition for VATS lobectomies. Also we needed a small retractor in a few cases for retrieving large specimens. However we had some differences from consensus statement in indications; 4 cases had tumor diameter >7 cm (7,5-9 cm) and 1 case had chest wall invasion. In big tumor cases we used a small retractor for retracting the specimen. In chest wall invasion case we used a hybrid technique; after classical VATS lobectomy hilar dissection through a small utility incision, we made an incision on the invaded rib and cut it on the safe areas and leaved it on the lung. So, we do not think that tumor diameter is a matter of VATS lobectomy indication. We suggest that this indication should be evaluated with the possibility of hilar dissection. Also we think that a hybrid technique -for unblock chest wall resection and lobectomy-may be thought instead of open surgery in selected cases.
CUSUM analysis is a statistical graphic that can be used to monitor the success and failure at a technical skill and examines trends over time [4,10]. It can be used to demonstrate proficiency in a newly learned technical skill. Also it can measure the quality assurance once a technical skill has been mastered such as determining whether or not a resident has achieved competency in a particular skill [4,11,12]. Lim and colleagues applied CUSUM charting to evaluate doctors’ performance of thyroidectomy, renal and breast biopsies, endoscopic retrograde pancreatography and instrumental delivery. They recommend the use of CUSUM charting as a method for evaluating the technical performance [8]. Biau and colleagues applied another form of CUSUM analyses (LC-CUSUM) for the initial 532 endoscopic retrograde cholangiopancreatographies performed by one endoscopist over 8 years, to assess the learning curve and concluded that LC-CUSUM allows quantitative monitoring of individual performance during the learning process [13]. Recently Barrie and Ammori used CUSUM analysis for the assessment of learning curve of laparoscopic distal pancreatectomy [14].
Competence is the benchmark by which physicians are permitted to perform procedures independently [15]. The proficiency is a higher degree which is the ability to perform a procedure to the established performance standard in order to demonstrate the mastery. Progressing to proficiency in a complex procedure not only necessitates substantial additional operative experience but also requires a qualitative leap in knowledge and performance [15,16]. Two measures that characterize proficiency are efficiency and consistency [15]. We studied the consistency in this paper.
International VATS Lobectomy Consensus Group stated that 50 cases are needed for VATS lobectomy technical proficiency and surgeons need to perform at least 20 cases annually to maintain VATS lobectomy operative skills [9]. McKenna indicated 50 cases for the point where surgeons feel themselves comfortable [17]. Li and colleagues evaluated the first 200 VATS lobectomy cases of 2 different senior surgeons at 2 different institutions. They assessed proficiency by evaluating efficiency and consistency. They reached that achieving proficiency in performing VATS lobectomy seems to require more than 100 cases of personal experience to develop efficiency, and attaining consistency requires 200 or more cases [15].
We reached consistency at 27 cases for duration of the operation. This is a very low number in the literature which gave 50 to 200 case numbers as mentioned above. However we could not reached consistency for length of hospital stay. The reason of this was the plenty of cases with emphysematous parenchyma which caused prolonged air leak. In most of these cases we experienced air leak a few days after the surgery in which there was no air leak at the end. We think that some tears around the stapling line were occurring with the expansion of the lung. We are planning to use stapling line reinforcing in selected cases.
Our study involves only 1 surgeon with extensive open experience, so it cannot be applied to trainees who are learning VATS lobectomy without extensive open experience. However in many countries and many centers, VATS lobectomy is still not a routine procedure and many experienced surgeons did not begin to perform VATS lobectomy. We think that our results can be applied for such centers.
Mainly the 2 factors affect the length of learning curve. First one is the previous experience of the surgeon on both open lobectomy and VATS interventions such as port placement, using camera and other instruments. If you have enough experience on lung resections you will not lose time on understanding the anatomy. The same is valid for adopting the VATS instruments. Second one is the number of VATS lobectomy cases. If you have 1 case per month, the length of the learning curve will be longer than a surgeon who has the chance of performing a few cases weekly. Also, VATS skill of the surgeon affects the learning curve as a 3rd factor.
As a conclusion, it is possible to obtain technical proficiency also with an inferior number of procedures compared with existing literature. However determining a certain case number for obtaining proficiency is not possible due to the changing factors from surgeon to surgeon and center to center.
Footnotes
Conflict of interest statement: Authors state no conflict of interest.
References
- [1].Nwogu CE, D’Cunha J, Pang H, Gu L, Wang X, Richards WG. et al. VATS Lobectomy Has Better Perioperative Outcomes Than Open Lobectomy: CALGB 31001, an Ancillary Analysis of CALGB 140202 (Alliance) Ann Thorac Surg. 2015;99:399–405. doi: 10.1016/j.athoracsur.2014.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Roviaro G, Rebuffat C, Varoli F, Vergani C, Mariani C, Maciocco M.. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc. 1992;2:244–247. [PubMed] [Google Scholar]
- [3].Petersen RH, Hansen HJ.. Learning curve associated with VATS lobectomy. Ann Cardiothorac Surg. 2012;1:47–50. doi: 10.3978/j.issn.2225-319X.2012.04.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Toker A, Tanju S, Ziyade S, Kaya S, Dilege S.. Learning curve in videothoracoscopic thymectomy: how many operations and in which situations? Eur J Cardiothorac Surg. 2008;34:155–158. doi: 10.1016/j.ejcts.2007.12.056. [DOI] [PubMed] [Google Scholar]
- [5].Weerasinghe S, Mırghanı H, Revel A, Abu-Zıdan Fm.. Cumulative sum (CUSUM) analysis in the assessment of trainee competence in fetal biometry measurement. Ultrasound Obstet Gynecol. 2006;28:199–203. doi: 10.1002/uog.2828. [DOI] [PubMed] [Google Scholar]
- [6].Goldsmith ODaP. Statistical methods in research and production. London: Longman; 1976. [Google Scholar]
- [7].Swanson SJ, Herndon JE, D’Amico TA, Demmy TL, McKenna RJ Jr, Green MR. et al. Video-assisted thoracic surgery lobectomy: report of CALGB 39802—a prospective, multi-institution feasibility study. J Clin Oncol. 2007;25:4993–4997. doi: 10.1200/JCO.2007.12.6649. [DOI] [PubMed] [Google Scholar]
- [8].Lim TO, Soraya A, Ding LM, Morad Z.. Assessing doctors’ competence: application of CUSUM technique in monitoring doctors’ performance. Int J Qual Health Care. 2002;14:251–258. doi: 10.1093/oxfordjournals.intqhc.a002616. [DOI] [PubMed] [Google Scholar]
- [9].Yan TD, Cao C, D’Amico TA, Demmy TL, He J, Hansen H. et al. Video-assisted thoracoscopic surgery lobectomy at 20 years: a consensus statement. Eur J Cardiothorac Surg. 2014;45:633–639. doi: 10.1093/ejcts/ezt463. [DOI] [PubMed] [Google Scholar]
- [10].Altman DG, Royston JP.. The hidden effect of time. Stat Med. 1988;7:629–637. doi: 10.1002/sim.4780070602. [DOI] [PubMed] [Google Scholar]
- [11].Berwick DM.. Continuous improvement as an ideal in the health care. N Engl J Med. 1989;320:53–56. doi: 10.1056/NEJM198901053200110. [DOI] [PubMed] [Google Scholar]
- [12].Williams SM, Parry RP, Schlup MMT.. Quality control: an application of the CUSUM. Br Med J. 1992;304:1359–1361. doi: 10.1136/bmj.304.6838.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Biau DJ, Williams SM, Schlup MM, Nizard RS, Porcher R.. Quantitative and individualized assessment of the learning curve using LC-CUSUM. Br J Surg. 2008;95:925–929. doi: 10.1002/bjs.6056. [DOI] [PubMed] [Google Scholar]
- [14].Barrie J, Ammori BJ.. Minimally Invasive Distal Pancreatectomy: A Single-Center Analysis of Outcome With Experience and Systematic Review of the Literature. Surg Laparosc Endosc Percutan Tech. 2015;25:297–302. doi: 10.1097/SLE.0000000000000185. [DOI] [PubMed] [Google Scholar]
- [15].Li X, Wang J, Ferguson MK.. Competence versus mastery: The time course for developing proficiency in video-assisted thoracoscopic lobectomy. J Thorac Cardiovasc Surg. 2014;147:1150–1154. doi: 10.1016/j.jtcvs.2013.11.036. [DOI] [PubMed] [Google Scholar]
- [16].Dreyfus SE, Dreyfus HL. A five-stage model of the mental activities involved in directed skill acquisition. Operations Research Center, ORC 80-2; University of California Berkeley: 1980. Feb. [Google Scholar]
- [17].McKenna RJ Jr. Complications and Learning Curves for Video-Assisted Thoracic Surgery Lobectomy. Thorac Surg Clin. 2008;18:275–280. doi: 10.1016/j.thorsurg.2008.04.004. [DOI] [PubMed] [Google Scholar]


