Abstract
This study examines reasons why people do not seek help for alcohol or drug problems by gender and race/ethnicity using data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative survey. Multivariate models were fit for 3 barriers to seeking help (structural, attitudinal, and readiness for change) for either alcohol or drug problems, controlling for socio-demographic characteristics and problem severity. Predicted probabilities were generated to evaluate gender differences by racial/ethnic subgroups. Over three quarters of the samples endorsed attitudinal barriers related to either alcohol or drug use. Generally, women were less likely to endorse attitudinal barriers for alcohol problems. African Americans and Latina/os were less likely than Whites to endorse attitudinal barriers for alcohol problems, Latina/os were less likely than Whites to endorse readiness for change barriers for alcohol and drug problems, however, African Americans were more likely to endorse structural barriers for alcohol problems. Comparisons within racial/ethnic subgroups by gender revealed more complex findings, although across all racial/ethnic groups women endorsed attitudinal barriers for alcohol problems more than men. Study findings suggest the need to tailor interventions to increase access to help for alcohol and drug problems that take into consideration both attitudinal and structural barriers and how these vary across groups.
Keywords: gender, race/ethnicity, treatment seeking, barriers, substance use problems
Introduction
It has been widely shown that a minority of individuals who have a substance use disorder (either alcohol or drug) actually seek and receive treatment for these problems. The most recent data from the National Survey on Drug Use and Health (NSDUH) estimates that only 10.8% of individuals who met criteria for needing substance use disorder [SUD] treatment actually received treatment at a specialty addiction treatment facility in 2015 (Center for Behavioral Health Statistics and Quality, 2016). Although the rate is higher when other forms of help-seeking are included (e.g., 12-step groups, pastoral care, private physicians), most individuals with substance use problems neither seek nor receive help for these problems.
1.1. Health Belief Model and barriers to care
The Health Belief Model is a useful theoretical framework to help understand why individuals do not utilize health services. The Health Belief Model posits that service utilization is influenced by health belief factors including perceived barriers to obtaining care as well as the perceived threat of a disease, perceived efficacy of health care, and cues to action (Janz & Becker, 1984; Schempf & Strobino, 2009; Rosenstock, Strecher, & Becker 1988). In addition, the Health Belief Model recognizes that demographic characteristics, such as gender and race/ethnicity, are modifying variables that can influence service utilization directly and indirectly through the aforementioned health belief factors. Therefore, this model can be applied when assessing SUD treatment service utilization among diverse populations. Identifying the barriers to treatment and how they may vary by gender and race/ethnicity are fundamental to developing culturally appropriate services.
Using the Health Belief Model, we first consider perceived barriers to obtaining care. Overall, the literature distinguishes barriers to utilizing mental health services into two major categories: attitudinal versus structural (Crisp et al., 2000; Issakidis & Andrews, 2002; Saldivia et al., 2004; Sareen et al., 2007; Thompson, Hunt, & Issakidis, 2004; Wells et al., 1994). These two major categories may also be further subdivided to distinguish nuances among perceived barriers to obtaining care. For example, researchers have identified financial barriers separate from other logistical barriers when assessing structural barriers (Chen, Strain, Crum, & Mojtabai, 2013; Mojtabai, Chen, Kaufmann, & Crum, 2014; Schuler, Puttaiah, Mojtabai, & Crum, 2015). Similarly, perceived stigma has been identified as distinct among other attitudinal barriers, such as pessimism about treatment (Chen et al., 2013; Schuler et al., 2015). Taken as a whole, various studies using national samples have found that individuals are more apt to cite beliefs and attitudes about treatment compared to structural barriers (e.g., cost, lack of transportation, lack of information) when asked why they did not seek help for a substance use problem (Mojtabai et al., 2011; Chen et al., 2013; Schuler et al., 2015).
Another key construct in the Health Belief Model is the perceived threat of a disease. Generally, severity of substance use, psychological distress, and a greater number of perceived problems related to one’s substance use increase an individual’s perception of need for help (Grella et al., 2009). A recent study found that individuals with more severe disorders were more likely to perceive a need for help and to cite structural and attitudinal/evaluative barriers (e.g., stigma, negative experience with prior treatment, perceived ineffectiveness of treatment) as compared with those with less severe disorders (Chen, Strain, Crum & Mojtabai, 2013). Another study showed that among individuals with alcohol use disorders, those with comorbid mood or anxiety disorders were more likely to seek help, but were also more likely to perceive an unmet need for treatment and to report more barriers to obtaining care (Kaufmann, Chen, Crum, & Mojtabai, 2014). Similarly, a recent study conducted with national survey data found that individuals with unmet needs for treatment of co-occurring substance use and depressive disorders most often cited structural barriers, specifically, concerns about the cost of treatment as a barrier to receiving these services (Mojtabai, Chen, Kaufmann, & Crum, 2014).
In addition to perceived barriers to obtaining care and perceived threat of a disease, the Health Belief Model highlights the important role that demographic characteristics play in determining service utilization. Several demographic characteristics influence perceived need for treatment, with lower levels of perceived need among younger and middle-aged adults, compared with those older; males compared with females; and individuals with higher education levels compared with lower. With regard to race/ethnicity, Latina/os were more likely to report structural barriers to accessing treatment, but only among individuals with mild or moderate severity, as compared with non-Hispanic Whites (Mojtabai et al., 2014).
Thus, drawing from the Health Belief Model, it is important to understand the factors that inhibit help-seeking for substance use problems and, specifically, how these factors vary across subgroups. A better understanding of the barriers that individuals experience or perceive when seeking help for substance use problems may shed light on disparities in access to treatment among key demographic groups and suggest strategies that can be undertaken to alleviate these barriers and the resultant health disparities in treatment access. The goal of the present study is to examine differences by gender and race/ethnicity in perceived barriers to seeking help for substance use problems.
1.2. Gender differences in seeking help for substance use problems
National survey data has shown that women underutilize substance abuse treatment relative to men (Greenfield et al., 2007). A recent study found that women with alcohol dependence were less likely to receive help compared with men, although those who did receive treatment were younger at first service utilization and had a shorter interval between drinking onset and service use (Alvanzo et al., 2014). Moreover, women with substance use problems encounter unique barriers to seeking help, as compared with seeking other forms of health services use. These include factors such as greater stigma, less access to insurance coverage for addiction treatment, less family or other support for seeking treatment, concerns about jeopardizing custody of children or parental rights, and family-related demands that hinder their treatment participation (Grella, 2009; Grella & Joshi, 1999; Haller, Miles, & Dawson, 2003; Jessup, Humphreys, Brindis, & Lee, 2003).
In the past, traditional gender roles and marital relationships may have inhibited treatment participation among alcohol-dependent women. The dynamics of help-seeking may differ among women drug users, particularly if involvement in sex work or criminal behavior leads to supervision by the criminal justice or child welfare systems (Grella & Joshi, 1999), both of which may lead to diversion into drug treatment. Further, pregnant and parenting women who seek drug treatment may risk loss of child custody, or criminal prosecution (Paltrow & Flavin, 2010).
Logistical issues and access to resources, such as transportation, employment or health insurance coverage, may also facilitate or inhibit treatment use among women, (Saum, Hiller, Leigey, Inciardi, & Surratt, 2007). In addition to these, one study of women in recovery who had not participated in treatment found that they were concerned about the confrontational approaches that were pervasive in traditional substance use treatment and they held stereotyped perceptions of treatment services (e.g., the “religious” nature of 12-step groups; Copeland, 1997). However, much of the research documenting barriers to substance use treatment among women has not directly examined gender differences, nor differences within gender by race/ethnicity. Moreover, experiences of socio-economic disadvantage, exposure to community violence, criminal justice system interactions, and access to resources among women vary by race/ethnicity and influence perceptions of treatment needs and treatment access (Amaro et al., 2005, 2007).
1.3. Racial/Ethnic differences in seeking help for substance use problems
Prior research has found higher rates of unmet need for mental health treatment among African American and Latina/os relative to Whites, although findings are mixed with regard to utilization of treatment for alcohol or drug problems (Hatzenbuehler, Keyes, Narrow, Grant, & Hasin, 2008). In one study using national survey data (Wells, Klap, Koike, & Sherbourne, 2001), among those with perceived need for treatment, compared to Whites, African Americans were more likely to have no access to treatment for alcohol, drug abuse, or mental health problems (25.4% vs. 12.5%), and Latina/os were more likely to have less care than needed or delayed care (22.7% vs. 10.7%). Among those with need, Whites were more likely than Latina/os or African Americans to be receiving treatment (37.6%, 22.4%, and 25.0%, respectively).
Prior research has shown that attitudinal and perceptual factors account for some of the underutilization of mental health services among ethnic minorities; these may include perceived discriminatory practices in service provision, prior negative experiences associated with services utilization, and limited knowledge regarding available treatment/services (Alegria et al., 2002; Diala et al., 2000; Hines-Martin, Usui, Kim, & Furr, 2004; Keyes et al., 2008). Higher levels of Latino ethnic identity and Spanish language preference have also been associated with lower mental health service utilization among Latino/as, but these had no effect on service use for substance use problems, although service use was generally low (Keyes, et al., 2012). However, other research has found that Whites were less likely to report receiving help for drug use disorders than African Americans, and that there were no differences by race/ethnicity with regard to perceived barriers to drug treatment (Perron, Mowbray, et al., 2009) or time to enter treatment for alcohol or drug disorders (Alvanzo et al., 2014; Perron, Alexander-Eitzman, et al., 2009).
Further, a recent study using data from a national sample of individuals in drug treatment found that gender was a consistent moderator of receipt of treatment services across racial/ethnic groups. African American, Latina, and White women all received significantly more comprehensive services than men while in treatment, both overall and matched to their self-reported treatment needs. Moreover, among all racial/ethnic groups, women attained significantly greater reductions in substance use post-treatment compared with their male counterparts who had received the same level of service, with especially large effects in this relationship among Latina women compared with Latino men (Guerrero, Marsh, Cao, Shin, & Andrews, 2014). Hence, interactions between gender and race/ethnicity may not only shape access to treatment services, but also receipt of services while in treatment and their post-treatment effects.
1.4. Current study
The current study builds on two prior studies conducted with the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a longitudinal national probability survey. The first study identified factors that facilitated treatment seeking among individuals in the general population with alcohol and/or drug dependence; these included older age, dependence on drugs (vs. alcohol only), longer time since the onset of dependence, co-occurring mood disorder, and more problems associated with alcohol and/or drug use. Among those who perceived a need for help, there were also lower levels of accessing treatment or other services among racial/ethnic minorities compared with Whites (Grella et al., 2009). In the second study, which examined help-seeking from baseline to follow-up, women were less likely to seek help for substance dependence than men (at both the baseline and follow-up); women who did seek help were more likely to have multiple substance dependencies, comorbid mental health problems, and lower rates of employment compared with those who did not (Grella & Stein, 2013).
In this study, we further examine barriers to help-seeking for alcohol or drug-related problems with a focus on the interactions between gender and race/ethnicity in the reasons for not seeking help, among those who perceive a need for it. The study findings should further illuminate factors that may be targeted for intervention in order to improve willingness to seek help and access to it among individuals with substance use problems.
2.0 Materials and methods
2.1. NESARC study design
NESARC is an in-depth longitudinal epidemiological survey of a representative sample of the United States. The study methodology has been described in detail elsewhere (Grant et al., 2003, 2004). The target population of the NESARC was the civilian, non-institutional adult population of the United States residing in households as well as in group quarters (e.g., group homes, halfway houses). At Wave 1, face-to-face interviews were conducted with 43,093 respondents in 2001–2002 (response rate = 81%). African Americans, Latina/os, and young adults (ages 18–24 years) were over-sampled, with data adjusted for over-sampling and household- and person-level non-response. The weighted data were then adjusted to represent the U.S. civilian population based on the 2000 census.
2.2. Current study sample
All respondents were asked a series of questions regarding their use of alcohol and other drugs over their lifetime; individuals who indicated they had ever used alcohol, illegal drugs, or medicines “without a doctor’s prescription; in greater amounts, more often, or longer than prescribed; or for a reason other than a doctor said you should use them” were also asked about whether they had ever sought help for their “drinking” or “use of medicine or drugs.” Individuals who responded positively to having sought help related to their drinking or drug use, or who indicated that there was a time when they thought that they should seek help, but had not done so, were included in the current study sample. Because of the relatively small sample sizes for Asians and Native Americans that prohibited subgroup comparisons by gender, these groups were dropped from the final analysis sample.
The sample characteristics for the two groups defined by type of substance use problem (alcohol, drugs) are shown in Table 1.1 Overall, a majority of both samples is White and male, with an average age of 42.9 and 37.2 years for alcohol and drug users, respectively. About half of each group has attended college or has a college degree; similarly, about half lives in a suburban area, with the remainder living in either urban or rural areas. Approximately three quarters of each group has some form of health insurance. Over half of each group reports they are married or cohabiting with a partner (although the percentage is higher among those with alcohol problems). Only 8% of each group met diagnostic criteria for a personality disorder, although 65% and 76% of those with alcohol and drug problems, respectively, met criteria for a mood or anxiety disorder. With regard to substance use disorders, 16% and 33% met criteria for alcohol or drug abuse, respectively; 82% and 65% met criteria for alcohol or drug dependence, respectively.
Table 1.
Descriptive statistics of study participants who did not seek help for an alcohol or drug problem (weighted sample): National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), Wave 1
| Alcohol Problem (N = 1,012) Percent / Mean (SD) |
Drug Problem (N = 532) Percent / Mean (SD) |
|
|---|---|---|
| Reasons for not seeking help, % | ||
| Structural | 28.7 | 36.8 |
| Attitudinal | 82.7 | 84.4 |
| Readiness for change | 31.8 | 29.9 |
| Race/Ethnicity, % | ||
| White | 80.9 | 75.0 |
| African American | 9.7 | 14.6 |
| Latino | 9.4 | 10.4 |
| Male, % | 68.8 | 63.7 |
| Age, Mean (SE) | 42.87 (0.23) | 37.22 (0.22) |
| Urbanicity, % | ||
| Urban | 31.0 | 33.9 |
| Suburban | 48.2 | 49.5 |
| Rural | 20.8 | 16.6 |
| Insured, % | 75.6 | 74.3 |
| Education, % | ||
| Less than High School | 17.3 | 17.7 |
| High School/GED | 32.1 | 34.6 |
| Some College/College Degree | 50.6 | 47.7 |
| Household Income, % | ||
| Less than $15,000 | 15.4 | 20.8 |
| $15,000 - $39,999 | 36.2 | 32.3 |
| $40,000 - $89,999 | 37.1 | 35.2 |
| $90,000 or More | 11.3 | 11.7 |
| Marital Status, % | ||
| Unmarried | 19.8 | 26.7 |
| Married/Cohabitating | 56.0 | 51.1 |
| Widowed/Separated/Divorced | 24.2 | 22.2 |
| Mental Health Disorder, % | ||
| No Mental Health Disorder | 26.6 | 15.5 |
| Personality Disorder | 8.4 | 8.1 |
| Mood/Anxiety Disorder | 65.0 | 76.4 |
| Substance Use Disorder, % | ||
| No Substance Use Disorder | 1.8 | 2.5 |
| Substance Abuse | 16.3 | 32.6 |
| Substance Dependence | 81.9 | 64.9 |
2.3. Measures
Help seeking
Respondents were asked: Have you ever gone anywhere or seen anyone for a reason that was related in any way to your drinking/use of medicine or drugs? Responses included: Alcoholics Anonymous or any other type of 12-step meeting; family services or another social service agency; alcohol or drug detoxification program; inpatient ward of a psychiatric or general hospital or community mental health program; outpatient clinic, including outreach programs and day or partial patient programs; alcohol or drug rehabilitation program, including methadone maintenance (for drugs only); emergency room; halfway house or therapeutic community; crisis center; employee assistance program; clergyman, priest, rabbi, or any type of religious counselor; private physician, psychiatrist, psychologist, social worker, or any other professional; or any other agency or professional.
Those who indicated they had not received any help were asked: Was there ever a time when you thought you should see a doctor, counselor, or other health professional or seek any other help for your drinking/medicine or drug use? Respondents who indicated “yes” were then asked: What were your reasons for not getting help? Respondents could check all that applied from a list of 27 reasons. The reasons were coded into three categories. The first two categories were based on the literature that typically distinguished barriers to treatment by attitudinal versus structural (Crisp et al., 2000; Issakidis & Andrews, 2002; Saldivia et al., 2004; Sareen et al., 2007; Thompson, Hunt, & Issakidis, 2004; Wells et al., 1994; Schuler, Puttaiah, Mojtabai, & Crum, 2015). A third category was included to address other barriers there were qualitatively distinct from the attitudinal and structural barriers and were also endorsed by a non-trivial percentage of respondents. This third category is similar to the “readiness for change” category developed by Schuler et al. (2015) using the same dataset and will be referred to as readiness for change accordingly.
Structural barriers: health insurance didn’t cover; could not afford to pay bill; didn’t know where to go for help, didn’t have any way to get there, didn’t have time, can’t speak English very well, couldn’t arrange for childcare, had to wait too long to get into a program
Attitudinal barriers: was too embarrassed to discuss it with anyone, was afraid of what boss, friends, or family would think; was afraid they would put me into hospital, was afraid of the treatment they would give me; didn’t think anyone could help; tried to get help before, but it didn’t work; thought the problem would get better by itself, should be strong enough to handle it alone, don’t think seeking help was necessary, didn’t think problem was serious enough, didn’t want to go
Readiness for change: stopped drinking/using on my own, family or friends helped me stop drinking/using; wanted to keep drinking/using.
2.4. Statistical analyses
All analyses were conducted separately for the two groups (alcohol, drugs) in order to better understand unique patterns of help-seeking across specific substances, consistent with other research in this area (Hedden & Gfroerer, 2011). First, simple descriptive statistics were examined for the reasons for not seeking help and the sample characteristics for the two analytic groups. Next, logistic regression models were fit that modeled main effects of gender and race/ethnicity for each reason for not seeking help, including covariates that have previously been associated with help-seeking behaviors and treatment utilization (Blanco et al., 2015). These included: age, health insurance status, education status, household income, marital status, urbanicity (urban, suburban, rural), mental health disorder (none, personality disorder, mood/anxiety disorder), and substance use disorder (none, abuse, dependence). Lastly, in order to examine gender differences within racial/ethnic groups on barriers to help-seeking, a second set of logistic regression models were fit that included interaction terms between gender and race/ethnicity adjusting for the same covariates as before. We then generated predicted probabilities for each of the six gender-by-race/ethnicity groups. All analyses were weighted to be representative of the U.S. population and were performed using Stata (v13) software (StataCorp).
3. Results
3.1. Barriers to help-seeking
Overall, the most frequently cited reason for not seeking help pertained to attitudinal barriers, which were endorsed by over 80% of the samples with regard to both alcohol and drug use problems (see Table 1). Although there were similar distributions of the reasons for not seeking help, it is notable that a higher proportion of the drug-related sample compared to the alcohol-related sample endorsed structural barriers as reasons for not seeking help, 37% and 29%, respectively. Only a slightly higher proportion of the alcohol-related sample endorsed readiness for change barriers as reasons for not seeking help, 32% compared to 30% of the drug-related sample.
3.2. Main effects of gender and race/ethnicity in multivariate models
Main effects for gender and race/ethnicity were examined in multivariate logistic regression models controlling for socio-demographic covariates, presence of substance use disorders, and personality or mood/anxiety disorders (see Tables 2 and 3).
Table 2.
Associations between race/ethnicity and gender and reasons for not seeking help for alcohol problems (weighted sample): NESARC Wave 1; 2001–2002. (N = 1,012)
| Reasons for not seeking help for alcohol problems |
|||
|---|---|---|---|
| Variables | Structural | Attitudinal | Readiness for change |
| Race/Ethnicity | |||
| White (Ref.) | 1 | 1 | 1 |
| African American | 1.19** | 0.65*** | 0.92 |
| [1.05,1.34] | [0.57,0.73] | [0.81,1.04] | |
| Latino | 0.99 | 0.74* | 0.73* |
| [0.79,1.23] | [0.57,0.96] | [0.55,0.97] | |
| Gender | |||
| Female (Ref.) | 1 | 1 | 1 |
| Male | 0.98 | 0.46*** | 0.94 |
| [0.82,1.16] | [0.37,0.58] | [0.81,1.11] | |
Note: CI = confidence interval; OR = odds ratio. Models used logistic regression and adjusted for age, urbanicity, insurance status, education status, household income, marital status, mental health disorder, and substance use disorder.
p < 0.05
p < 0.01
p < 0.001
Table 3.
Associations between race/ethnicity and gender and reasons for not seeking help for drug problems (weighted sample): NESARC Wave 1; 2001–2002. (N = 532)
| Reasons for not seeking help for drug problems |
|||
|---|---|---|---|
| Variables | Structural | Attitudinal | Readiness for change |
| Race/Ethnicity | |||
| White (Ref.) | 1 | 1 | 1 |
| African American | 1.19 | 1.10 | 0.80 |
| [0.95,1.50] | [0.88,1.37] | [0.57,1.12] | |
| Latino | 0.99 | 0.74* | 0.73* |
| [0.79,1.23] | [0.57,0.96] | [0.55,0.97] | |
| Gender | |||
| Female (Ref.) | 1 | 1 | 1 |
| Male | 0.96 | 1.28 | 1.06 |
| [0.81,1.14] | [0.94,1.73] | [0.86,1.31] | |
Note: CI = confidence interval; OR = odds ratio. Models used logistic regression and adjusted for age, urbanicity, insurance status, education status, household income, marital status, mental health disorder, and substance use disorder.
p < 0.05
p < 0.01
p < 0.001
3.2.1. Structural barriers
There were no gender differences related to structural barriers for either alcohol or drugs. When examined by race/ethnicity, there were no differences among those with drug problems. However, compared with Whites, African Americans (AOR=1.19) and Latina/os (AOR=1.75) were more likely to endorse structural barriers to seeking help for alcohol problems.
3.2.2. Attitudinal barriers
Men were significantly less likely than women to endorse attitudinal barriers to seeking help for alcohol problems (AOR = O.46), but there were no differences by gender in this domain for drug problems. Similarly, Latina/os were less likely to cite attitudinal barriers as a reason for not seeking help for alcohol (AOR=0.66) and drug (AOR=0.74) problems, compared with Whites. African Americans (AOR=0.65) were also less likely to cite attitudinal barriers as a reason for not seeking help compared with Whites, but only for alcohol problems.
3.2.3. Readiness for change barriers
There were no gender differences related to readiness for change barriers for either alcohol or drugs. However, Latina/os were less likely than Whites to cite readiness for change barriers as a reason for not seeking help for alcohol (AOR= 0.76) and drug (AOR= 0.73) problems.
3.3. Interaction effects of gender by race/ethnicity
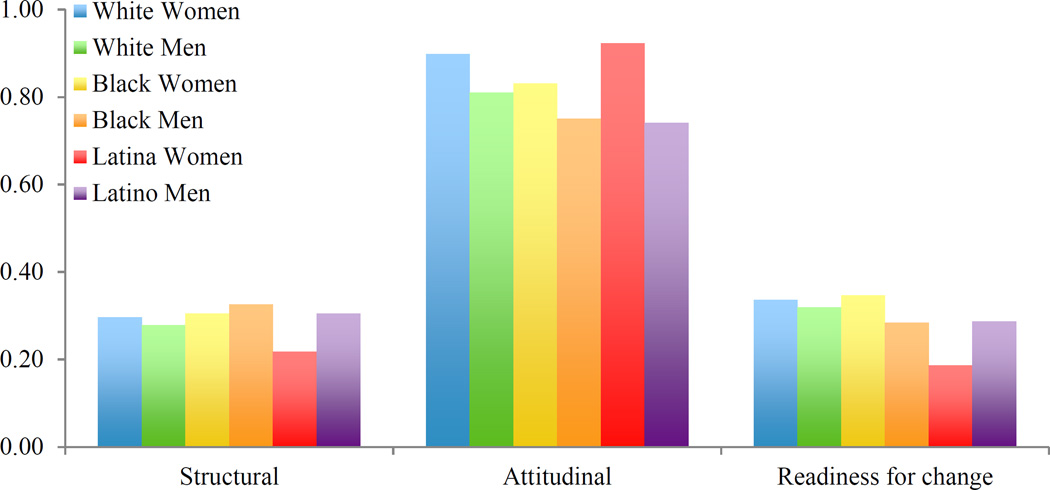
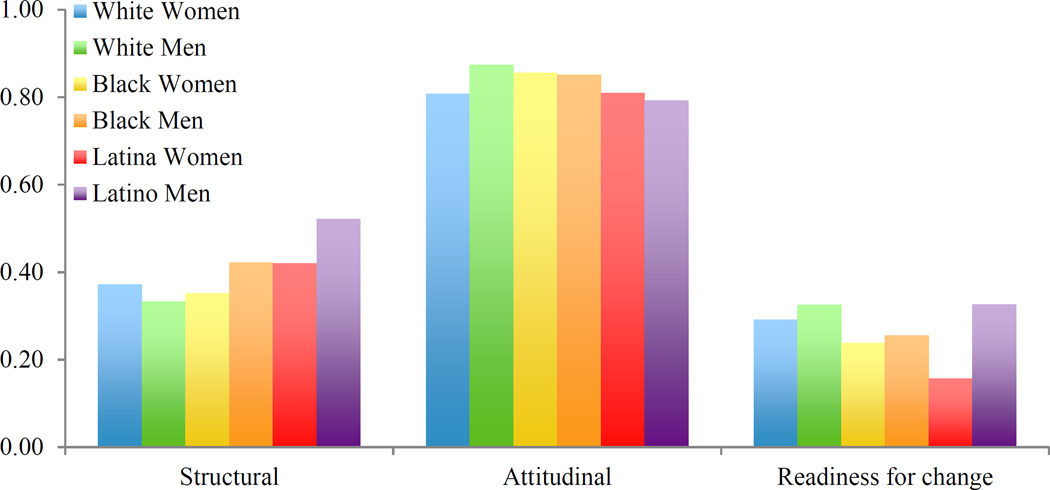
Predicted probabilities generated by interaction terms in the logistic regression models were examined to determine whether there were gender differences within racial/ethnic groups for the reasons cited for not seeking help for alcohol and drug problems (see Tables 4 and 5). These are shown graphically in Figures 1 and 2.
Table 4.
Predicted probabilities of reasons for not seeking help for alcohol problems by gender and race/ethnicity (weighted sample): NESARC, Wave 1; 2001–2002 (N = 1,012)
| Reasons for not seeking help for alcohol problems |
|||
|---|---|---|---|
| Structural | Attitudinal | Readiness for change | |
| White Women | 0.30 | 0.90 | 0.34 |
| White Men | 0.28 | 0.81 | 0.32 |
| African American Women | 0.30 | 0.83 | 0.35 |
| African American Men | 0.33 | 0.75 | 0.28 |
| Latina Women | 0.22 | 0.92 | 0.19 |
| Latino Men | 0.30 | 0.74 | 0.29 |
| Differences by gender | White*** | ||
| within race/ethnicity | African American*** | African American *** | |
| Latino* | Latino*** | Latino* | |
Models used logistic regression and adjusted for age, urbanicity, insurance status, education status, household income, marital status, mental health disorder, and substance use disorder.
p < 0.05
p < 0.01
p < 0.001
Table 5.
Predicted probabilities of reasons for not seeking help for drug problems by gender and race/ethnicity (weighted sample): NESARC, Wave 1; 2001–2002 (N=532)
| Reasons for not seeking help for drug problems |
|||
|---|---|---|---|
| Structural | Attitudinal | Readiness for change | |
| White Women | 0.37 | 0.81 | 0.29 |
| White Men | 0.33 | 0.87 | 0.33 |
| African American Women | 0.35 | 0.86 | 0.24 |
| African American Men | 0.42 | 0.85 | 0.26 |
| Latina Women | 0.42 | 0.81 | 0.16 |
| Latino Men | 0.52 | 0.79 | 0.33 |
| Differences by gender | White** | ||
| within race/ethnicity | African American * | ||
| Latino* | Latino*** | ||
Models used logistic regression and adjusted for age, urbanicity, insurance status, education status, household income, marital status, mental health disorder, and substance use disorder.
p < 0.05
p < 0.01
p < 0.001
Figure 1.
Predicted Probabilities of Reasons For Not Seeking Help for Alcohol problems by Gender and Race/Ethnicity: NESARC, Wave 1; 2001–2002.
Figure 2.
Predicted Probabilities of Reasons For Not Seeking Help for Drug Problems by Gender and Race/Ethniciti: NESARC, Wave 1; 2001–2002.
3.3.1. Structural barriers
The predicted probability of structural barriers was significantly greater for Latino men relative to Latina women for both alcohol and drug problems. In contrast, the probability of structural barriers was significantly greater for African American men, relative to women, for drug problems.
3.3.2. Attitudinal barriers
The predicted probability of attitudinal barriers related to alcohol problems was significantly greater for White, African American, and Latina women relative to men, whereas the opposite pattern was obtained related to drug problems among White men relative to women.
3.3.3. Readiness for change barriers
Latino men had a higher probability of endorsing readiness for change barriers for alcohol and drug problems relative to women. The reverse was true among African Americans for alcohol problems, as African American women had a greater probability than men of citing readiness for change barriers.
4. Discussion
Based on the Health Belief Model, the study findings help to provide a more detailed understanding of the reasons why individuals with substance use problems do not seek help, citing specific barriers to treatment, and in particular, how these perceived barriers vary by gender and race/ethnicity. Consistent with other research (Mojtabai & Crum, 2013; Chen et al., 2013), attitudinal barriers were cited most frequently; less often cited were structural barriers to seeking help for these problems.
4.1. Barriers to help-seeking by gender
The analysis of gender main effects revealed that some barriers that have been commonly cited as obstacles to seeking help for substance abuse among women (e.g., financial or structural) were pervasive among both men and women. Both men and women were equally likely to endorse structural barriers to seeking help for either alcohol or drug problems. Thus, structural impediments to seeking treatment, which may involve lack of information, time, transportation, or childcare, are pervasive among both men and women.
Interestingly, across all racial/ethnic groups, women were more likely to cite attitudinal barriers related to their alcohol use. Historians of alcohol recount that alcohol use among women in the past was usually relegated to private spheres, and thus remained relatively hidden (Lex, 1991). When women alcoholics were visible within the public sphere, they were often depicted as “sicker, less motivated and more sexually deviant than their male counterparts” (Reed, 1987, p. 153). Within the context of prevailing gender roles, studies of women alcoholics found that they often minimized the harmfulness of their drinking and emphasized that it had not impaired their ability to fulfill their roles as wives and mothers (Thom, 1986). The recognition of alcohol problems among women evolved gradually out of increasing understanding of gender differences in the initiation and patterns of alcohol use (Schmidt & Weisner, 1995), as well as distinctive patterns of help-seeking, in which women more often attributed their alcohol use to depression and anxiety and hence sought help in mental health settings (Weisner & Schmidt, 1992).
The study findings suggest that a double standard with regard to women’s use of alcohol remains pervasive, despite the increased acceptance of alcohol use among women, particularly middle class women, who have benefited from greater economic parity, which has allowed them to more freely consume alcohol (Schmidt, 2014). This study found that women who acknowledge having problems related to their alcohol use are nonetheless more likely to downplay these problems as reasons for seeking help. Motivational interventions aimed at women have usually focused on alcohol or tobacco use among pregnant women (Handmaker, Miller, & Manicke, 1999; Ondersma, Winhusen, Erickson, Stine, & Wang, 2009); the current study suggests that gender-targeted motivational interventions regarding alcohol use should be broadened to address women more generally, including the reluctance of some to acknowledge their problematic use of alcohol and need for treatment.
Although gender differences for drug use were not found, a sub analysis (data not shown) revealed that women were more likely than men to endorse negative attitudes about treatment (fear and pessimism). In some instances, drug use among women who are pregnant or have young children may lead to loss of custody or parental rights for their children, which may underlie these negative perceptions. The heightened publicity given to maternal drug use as well as examples of prosecution of pregnant women for fetal child abuse, which have disproportionately targeted low-income women of color, may contribute to these perceptions (Paltrow & Flavin, 2010, 2013). Thus interventions aimed at increasing access to drug treatment services for women should focus less on problem recognition (relative to alcohol problems), and more so on strategies to overcome barriers to treatment, including the possibility of negative ramifications for their parental status.
4.2. Barriers to help-seeking by race/ethnicity
Several patterns regarding the influence of race/ethnicity also emerged, depicting both attitudinal and structural barriers to treatment access. With regard to alcohol problems, African Americans and Latina/os were more likely than Whites to endorse structural barriers, but were less likely endorse attitudinal barriers. Latina/os were less likely than Whites to cite readiness for change barrier for alcohol problems. Similarly, with regard to drug problems, Latina/os were less likely than Whites to endorse both attitudinal and readiness for change barriers.
These findings correspond with prior research showing that racial/ethnic minorities often have high problem recognition but limited access to or prior negative experiences with mental health or substance abuse treatment, leading to under-utilization of services (Wells et al., 2001). Further, a recent study found that counties with a higher proportion of African American and uninsured residents, as well as those in rural areas, were less likely to have access to an outpatient substance abuse treatment program that accepted Medicaid, thus limiting access to treatment for individuals on public insurance (Cummings, Wen, Ko, & Druss, 2014). Therefore, disparities in access to substance use treatment operate on multiple levels, including both individual motivational and structural factors. Efforts to improve the cultural competence of substance abuse programs, particularly through workforce development, provision of language-compatible services, and outreach to local communities, can help to reduce these barriers and the resultant health disparities in treatment access (Guerrero et al., 2016).
Examination of the interaction effects of gender and race/ethnicity provides a more nuanced, and complex, understanding of how these barriers vary. With regard to treatment for alcohol problems, women were more likely than their male counterparts to endorse attitudinal barriers to treatment across all racial/ethnic groups. Latino men were more likely than Latina women to endorse structural and readiness for change barriers for alcohol problems. African American women were more likely to endorse readiness for change barriers for alcohol problems than African American men. In regards to barriers for drug problems, men were overall more likely to endorse any barriers than women across all racial/ethnic groups. Both African American and Latino men were more likely to endorse structural barriers for drug problems than their female counterparts. Whereas, White men were more likely to endorse attitudinal barriers to drug problems than White women. Lastly, Latino men were more likely to endorse readiness for change barriers to drug problems than Latina women.
It is likely that these variations in attitudinal and structural barriers reflect differences by race/ethnicity in access to resources, family and social support for treatment, and beliefs pervasive among one’s peer and social referent groups. For example, with regard to a higher endorsement of structural barriers among Latino men than Latina women, this is consistent with previous research showing that women, including Latinas, tend to receive more social services, such as transportation, that facilitate treatment access, than their male counterparts (Guerrero, Marsh, et al., 2014). Thus, the needs of Latino men may be overlooked. One significant barrier in this regard is transportation, which is a barrier to treatment access if they lack driver’s licenses or car insurance, or need to travel longer distances to access culturally and linguistically tailored treatment services (Guerrero, Kao, & Perron, 2013), or to access programs that accept public insurance (Cummings et al., 2014). Thus, strategies to minimize disparities in treatment access must address the specific needs of communities of color, which may vary by gender in addition to nativity and language preference.
4.3 Study limitations
Although the NESARC study has the advantage of a large overall sample size that is representative of the U.S. population, the sample size is still relatively small for some subgroups (e.g., Asian-Americans, Native Americans), which precluded their inclusion in this analysis. As with all national surveys, the study is limited by the use of retrospective self-report data; however, the validity of such data can be enhanced by use of standardized procedures and rigorous staff training and oversight, all of which were implemented in the NESARC study (del Boca & Noll, 2000).
Further, the data are limited to the extent that we can examine whether some perceived barriers are contingent on prior unsuccessful efforts to seek help, due to structural impediments that lead to negative perceptions about treatment. This may occur in instances where individuals were unable to access treatment due to lack of funding, long wait times or distance to travel to the program, or lack of culturally or linguistically compatible services. To explore whether these contingent relationships existed, we examined the number of barriers cited by respondents (in relation to alcohol and drug use, separately) as well as the correlations among the various barriers.
A majority of respondents cited 1 – 2 of 27 barriers: 75% for alcohol and 67% for drugs, with a modal response of one barrier. All of the correlations were in the small range (alcohol: r = 0.03 to 0.29; drugs: r = 0.01 to 0.35). Moreover, the strongest correlations were among the attitudinal barriers, such as between stigma and fear of treatment (r = 0.29) and between wanted to keeping and treatment pessimism (r = 0.26 for both alcohol and drugs). There were weak correlations between the structural and attitudinal barriers (all r < 0.25). Moreover, “wanted to keep using” was weakly correlated with structural barriers with regard to both alcohol (r = 0.20) and drugs (r = 0.13). Thus, we found little evidence to support contingent relationships between the structural and attitudinal barriers. However, a study designed expressly to explore temporal patterns in help-seeking over time would be needed to fully address this issue.
Lastly, the data were collected in early 2000’s, and thus reflect the characteristics of addiction services at that time. The recent implementation of the Affordable Care Act may increase access to substance abuse treatment, particularly through the expansion of Medicaid funding to those previously uninsured (Buck, 2011; Pating, Miller, Goplerud, Martin, & Ziedonis, 2012), although gaps still persist in access to behavioral health services (Garfield, Lave, & Donohue, 2010; Kessler, Miller, Kelly, et al., 2014). Moreover, the gap in utilization of SUD treatment among those who meet criteria for these disorders remains, as the proportion of the population in need of SUD treatment that actually receives it has remained relatively constant as measured in the NSDUH over the past decade (Center for Behavioral Health Statistics and Quality, 2016).
In sum, the study findings suggest the need to tailor interventions to increase access to help for alcohol and drug problems that take into consideration both negative perceptions, motivational readiness, and structural barriers and how these vary across both gender and race/ethnicity, in order to address the health disparities that stem from differential access and utilization of addiction services based on the Health Belief Model.
Acknowledgments
The authors acknowledge the assistance of Elizabeth Teshome and Kris Langabeer in manuscript preparation. This work was supported in part by NIDA Grant no. 5T32-DA007272.
Footnotes
Statistical comparisons between the alcohol and drug use groups with regard to background characteristics are not conducted because individuals may have endorsed a need for help for both types of problems, and hence be represented in both groups.
References
- Alegria M, Canino G, Rios R, Vera M, Calderon J, Rusch D, Ortega AN. Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatric Services. 2002;53(12):1547–1555. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- Alvanzo AA, Storr CL, Mojtabai R, Green KM, Pacek LR, La Flair LN, Crum RM. Gender and race/ethnicity differences for initiation of alcohol-related service use among persons with alcohol dependence. Drug and Alcohol Dependence. 2014;140:48–55. doi: 10.1016/j.drugalcdep.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amaro H, Dai J, Arevalo S, Acevedo A, Matsumoto A, Nieves R, Prado G. Effects of integrated trauma treatment on outcomes in a racially/ethnically diverse sample of women in urban community-based substance abuse treatment. Journal of Urban Health. 2007;84(4):508–522. doi: 10.1007/s11524-007-9160-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amaro H, Larson MJ, Gampel J, Richardson E, Savage A, Wagler D. Racial/ethnic differences in social vulnerability among women with co-occurring mental health and substance abuse disorders: Implications for treatment services. Journal of Community Psychology. 2005;33(4):495–511. [Google Scholar]
- Blanco C, Iza M, Rodriguez-Fernandez JM, Baca-Garcia E, Wang S, Olfson M. Probability and predictors of treatment-seeking for substance use disorders in the U.S. Drug and Alcohol Dependence. 2015;149:136–144. doi: 10.1016/j.drugalcdep.2015.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buck JA. The looming expansion and transformation of public substance abuse treatment under the affordable care act. Health Affairs. 2011;30(8):1402–1410. doi: 10.1377/hlthaff.2011.0480. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2016. Accessed online at: http://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf. [Google Scholar]
- Chen LY, Strain EC, Crum RM, Mojtabai R. Gender differences in substance abuse treatment and barriers to care among persons with substance use disorders with and without comorbid major depression. Journal of Addiction Medicine. 2013;7(5):325–334. doi: 10.1097/ADM.0b013e31829b7afe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copeland J. A qualitative study of barriers to formal treatment among women who self-managed change in addictive behaviours. Journal of Substance Abuse Treatment. 1997;14(2):183–190. doi: 10.1016/s0740-5472(96)00108-0. [DOI] [PubMed] [Google Scholar]
- Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. British Journal of Psychiatry. 2000;177(1):4–7. doi: 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- Cummings JR, Wen H, Ko M, Druss BG. Race/ethnicity and geographic access to Medicaid substance use disorder treatment facilities in the United States. JAMA Psychiatry. 2014;71(2):190–196. doi: 10.1001/jamapsychiatry.2013.3575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Boca FK, Noll JA. Truth or consequences: The validity of self-report data in health services research on addictions. Addiction. 2000;95:S347–S360. doi: 10.1080/09652140020004278. [DOI] [PubMed] [Google Scholar]
- Diala C, Muntaner C, Walrath C, Nickerson KJ, LaVeist TA, Leaf PJ. Racial differences in attitudes toward professional mental health care and in the use of services. American Journal of Orthopsychiatry. 2000;70(4):455–464. doi: 10.1037/h0087736. [DOI] [PubMed] [Google Scholar]
- Garfield RL, Lave JR, Donohue JM. Health reform and the scope of benefits for mental health and substance use disorder services. Psychiatric Services. 2010;61(11):1081–1086. doi: 10.1176/ps.2010.61.11.1081. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan KD, Shepard J, Moore T. Source and accuracy statement for Wave 1 of the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Brooks AJ, Gordon SM, Green CA, Kropp F, McHugh RK, Miele GM. Substance abuse treatment entry, retention, and outcome in women: A review of the literature. Drug and Alcohol Dependence. 2007;86(1):1–21. doi: 10.1016/j.drugalcdep.2006.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE. Treatment seeking and utilization among women with substance use disorders. In: Brady KT, Back SE, Greenfield SF, editors. Women and addiction: A comprehensive handbook. New York: Guilford Press; 2009. pp. 307–322. [Google Scholar]
- Grella CE, Joshi V. Gender differences in drug treatment careers among clients in the National Drug Abuse Treatment Outcome Study. American Journal of Drug and Alcohol Abuse. 1999;25(3):385–406. doi: 10.1081/ada-100101868. [DOI] [PubMed] [Google Scholar]
- Grella CE, Karno MP, Warda US, Moore AA, Niv N. Perceptions of need and help received for substance dependence in a national probability survey. Psychiatric Services. 2009;60(8):1068–1074. doi: 10.1176/appi.ps.60.8.1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grella CE, Stein JA. Remission from substance dependence: Differences between individuals in a general population longitudinal survey who do and do not seek help. Drug and Alcohol Dependence. 2013;133:146–153. doi: 10.1016/j.drugalcdep.2013.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero GE, Aarons GA, Grella CE, Garner BR, Cook B, Vega WA. Program capacity to eliminate outcome disparities in addiction health services. Administration and Policy in Mental Health and Mental Health Services Research. 2016;43(1):23–35. doi: 10.1007/s10488-014-0617-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Kao D, Perron BE. Travel distance to outpatient substance use disorder treatment facilities for Spanish-speaking clients. International Journal of Drug Policy. 2013;24:38–45. doi: 10.1016/j.drugpo.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Marsh JC, Cao D, Shin HC, Andrews C. Gender disparities in utilization and outcome of comprehensive substance abuse treatment among racial/ethnic groups. Journal of Substance Abuse Treatment. 2014;46:584–591. doi: 10.1016/j.jsat.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haller DL, Miles DR, Dawson KS. Factors influencing treatment enrollment by pregnant substance abusers. American Journal of Drug and Alcohol Abuse. 2003;29(1):117–131. doi: 10.1081/ada-120018842. [DOI] [PubMed] [Google Scholar]
- Handmaker NS, Miller WR, Manicke M. Findings of a pilot study of motivational interviewing with pregnant drinkers. Journal of Studies on Alcohol. 1999;60(2):285–287. doi: 10.15288/jsa.1999.60.285. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Keyes KM, Narrow WE, Grant BF, Hasin DS. Racial/ethnic disparities in service utilization for individuals with co-occurring mental health and substance use disorders in the general population: results from the national epidemiologic survey on alcohol and related conditions. Journal of Clinical Psychiatry. 2008;69(7):1112–1121. doi: 10.4088/jcp.v69n0711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedden SL, Gfroerer JC. Correlates of perceiving a need for treatment among adults with substance use disorders: Results from a national survey. Addictive Behaviors. 2011;36:1213–1222. doi: 10.1016/j.addbeh.2011.07.026. [DOI] [PubMed] [Google Scholar]
- Hines-Martin VP, Usui W, Kim S, Furr A. A comparison of influences on attitudes towards mental health service use in an African-American and White community. Journal of National Black Nurses’ Association. 2004;15(2):17–22. [PubMed] [Google Scholar]
- Issakidis C, Andrews G. Service utilisation for anxiety in an Australian community sample. Social Psychiatry and psychiatric epidemiology. 2002;37(4):153–163. doi: 10.1007/s001270200009. [DOI] [PubMed] [Google Scholar]
- Janz NK, Becker MH. The health belief model: A decade later. Health Education & Behavior. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Jessup MA, Humphreys JC, Brindis CD, Lee KA. Extrinsic barriers to substance abuse treatment among pregnant drug dependent women. Journal of Drug Issues. 2003;33(2):285–304. [Google Scholar]
- Kaufmann CN, Chen LY, Crum RM, Mojtabai R. Treatment seeking and barriers to treatment for alcohol use in persons with alcohol use disorders and comorbid mood or anxiety disorders. Social Psychiatry and Psychiatric Epidemiology. 2014;49(9):1489–1499. doi: 10.1007/s00127-013-0740-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R, Miller BF, Kelly M, Graham D, Kennedy A, Littenberg B, Pace WD. Mental health, substance abuse, and health behavior services in patient-centered medical homes. American Board of Family Medicine. 2014;27(5):637–644. doi: 10.3122/jabfm.2014.05.140021. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Hatzenbuehler ML, Alberti P, Narrow WE, Grant BF, Hasin DS. Service utilization differences for Axis I psychiatric and substance use disorders between white and black adults. Psychiatric Services. 2008;59(8):893–901. doi: 10.1176/appi.ps.59.8.893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keyes KM, Martins SS, Hatzenbuehler ML, Blanco C, Bates LM, Hasin DS. Mental health service utilization for psychiatric disorders among Latinos living in the United States: the role of ethnic subgroup, ethnic identity, and language/social preferences. Social Psychiatry & Psychiatric Epidemiology. 2012;47:383–394. doi: 10.1007/s00127-010-0323-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lex BW. Some gender differences in alcohol and polysubstance users. Health Psychology. 1991;10(2):121–132. doi: 10.1037//0278-6133.10.2.121. [DOI] [PubMed] [Google Scholar]
- Mojtabai R, Chen LY, Kaufmann CN, Crum RM. Comparing barriers to mental health treatment and substance use disorder treatment among individuals with comorbid major depression and substance use disorders. Journal of Substance Abuse Treatment. 2014;46(2):268–273. doi: 10.1016/j.jsat.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Crum RM. Perceived unmet need for alcohol and drug use treatments and future use of services: Results from a longitudinal study. Drug and Alcohol Dependence. 2013;127:59–64. doi: 10.1016/j.drugalcdep.2012.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R, Olfson M, Sampson NA, Jin R, Druss B, Wang PS, Kessler RC. Barriers to mental health treatment: Results from the National Comorbidity Survey Replication. Psychological Medicine. 2011;41(8):1751–1761. doi: 10.1017/S0033291710002291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ondersma SJ, Winhusen T, Erickson SJ, Stine SM, Wang Y. Motivation enhancement therapy with pregnant substance-abusing women: Does baseline motivation moderate efficacy? Drug and Alcohol. Dependence. 2009;101(1–2):74–79. doi: 10.1016/j.drugalcdep.2008.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paltrow LM, Flavin J. Punishing pregnant drug-using women: Defying law, medicine, and common sense. Journal of Addictive Diseases. 2010;29(2):231–244. doi: 10.1080/10550881003684830. [DOI] [PubMed] [Google Scholar]
- Paltrow LM, Flavin J. Arrests of and forced interventions on pregnant women in the United States, 1973–2005: Implications for women’s legal status and public health. Journal of Health Politics, Policy & Law. 2013;38(2):299–343. doi: 10.1215/03616878-1966324. [DOI] [PubMed] [Google Scholar]
- Pating DR, Miller MM, Goplerud E, Martin J, Ziedonis DM. New systems of care for substance use disorders: Treatment, finance, and technology under health care reform. Psychiatric Clinics of North America. 2012;35(2):327–356. doi: 10.1016/j.psc.2012.03.004. [DOI] [PubMed] [Google Scholar]
- Perron BE, Alexander-Eitzman B, Watkins D, Taylor RJ, Baser R, Neighbors HW, Jackson JS. Ethnic differences in delays to treatment for substance use disorders: African Americans, Black Caribbeans and non-Hispanic whites. Journal of Psychoactive Drugs. 2009;41(4):369–377. doi: 10.1080/02791072.2009.10399775. [DOI] [PubMed] [Google Scholar]
- Perron BE, Mowbray OP, Glass JE, Delva J, Vaughn MG, Howard MO. Differences in service utilization and barriers among Blacks, Hispanics, and Whites with drug use disorders. Substance Abuse Treatment, Prevention, and Policy. 2009;4:3. doi: 10.1186/1747-597X-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed BG. Developing women-sensitive drug dependence treatment services: Why so difficult? Journal of Psychoactive. Drugs. 1987;19(2):151–164. doi: 10.1080/02791072.1987.10472399. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Education & Behavior. 1988;15(2):175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Saldivia S, Vicente B, Kohn R, Rioseco P, Torres S. Use of mental health services in Chile. Psychiatric. Services. 2004;55(1):71–6. doi: 10.1176/appi.ps.55.1.71. [DOI] [PubMed] [Google Scholar]
- Sareen J, Jagdeo A, Cox BJ, Clara I, ten Have M, Belik SL, Stein MB. Perceived barriers to mental health service utilization in the United States, Ontario, and the Netherlands. Psychiatric. Services. 2007;58(3):357–364. doi: 10.1176/ps.2007.58.3.357. [DOI] [PubMed] [Google Scholar]
- Saum CA, Hiller ML, Leigey ME, Inciardi JA, Surratt HL. Predictors of substance abuse treatment entry for crime-involved, cocaine-dependent women. Drug and Alcohol Dependence. 2007;91(3):253–259. doi: 10.1016/j.drugalcdep.2007.06.005. [DOI] [PubMed] [Google Scholar]
- Schempf AH, Strobino DM. Drug use and limited prenatal care: an examination of responsible barriers. American Journal of Obstetrics and Gynecology. 2009;200(4):412–e1. doi: 10.1016/j.ajog.2008.10.055. [DOI] [PubMed] [Google Scholar]
- Schmidt L, Weisner C. The emergence of problem-drinking women as a special population in need of treatment. In: Galanter M, editor. Recent developments in alcoholism: Alcoholism and women. New York: Plenum Press; 1995. pp. 309–334. [DOI] [PubMed] [Google Scholar]
- Schmidt LA. The equal right to drink. Drug and Alcohol Review. 2014;33:581–587. doi: 10.1111/dar.12215. [DOI] [PubMed] [Google Scholar]
- Schuler MS, Puttaiah S, Mojtabai R, Crum RM. Perceived barriers to treatment for alcohol problems: A latent class analysis. Psychiatric Services. 2015;66(11):1221–1228. doi: 10.1176/appi.ps.201400160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thom B. Sex differences in help-seeking for alcohol problems: I. the barriers to help-seeking. British Journal of Addiction. 1986;81(6):777–788. doi: 10.1111/j.1360-0443.1986.tb00405.x. [DOI] [PubMed] [Google Scholar]
- Thompson A, Hunt C, Issakidis C. Why wait? Reasons for delay and prompts to seek help for mental health problems in an Australian clinical sample. Social Psychiatry and Psychiatric Epidemiology. 2004;39(10):810–817. doi: 10.1007/s00127-004-0816-7. [DOI] [PubMed] [Google Scholar]
- Weisner C, Schmidt L. Gender disparities in treatment for alcohol problems. Journal of the American Medical Association. 1992;268(14):1872–1876. [PubMed] [Google Scholar]
- Wells JE, Robins LN, Bushnell JA, Jarosz D, Oakley-Browne MA. Perceived barriers to care in St. Louis (USA) and Christchurch (NZ): Reasons for not seeking professional help for psychological distress. Social Psychiatry and Psychiatric Epidemiology. 1994;29(4):155–164. doi: 10.1007/BF00802012. [DOI] [PubMed] [Google Scholar]
- Wells K, Klap R, Koike A, Sherbourne C. Ethnic disparities in unmet need for alcoholism, drug abuse, and mental health care. American Journal of Psychiatry. 2001;158(12):2027–2032. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]