Abstract
Background/Aim:
To compare the efficacy and tolerance of different proton pump inhibitors (PPIs) in different doses for patients with duodenal ulcers.
Materials and Methods:
An electronic database was searched to collect all randomized clinical trials (RCTs), and a pairwise and network meta-analysis were performed.
Results:
A total of 24 RCTs involving 6188 patients were included. The network meta-analysis showed that there were no significant differences for the 4-week healing rate of duodenal ulcer treated with different PPI regimens except pantoprazle 40 mg/d versus lansoprazole 15 mg/d [Relative risk (RR) = 3.57; 95% confidence interval (CI) = 1.36–10.31)] and lansoprazole 30 mg/d versus lansoprazole 15 mg/d (RR = 2.45; 95% CI = 1.01–6.14). In comparison with H2 receptor antagonists (H2 RA), pantoprazole 40 mg/d and lansoprazole 30 mg/d significantly increase the healing rate (RR = 2.96; 95% CI = 1.78–5.14 and RR = 2.04; 95% CI = 1.13–3.53, respectively). There was no significant difference for the rate of adverse events between different regimens, including H2 RA for a duration of 4-week of follow up.
Conclusion:
There was no significant difference for the efficacy and tolerance between the ordinary doses of different PPIs with the exception of lansoprazle 15 mg/d.
Key Words: Duodenal ulcer, efficacy, network meta-analysis, proton pump inhibitor
Duodenal ulcers are a very common digestive disease with a high incidence all over the world.[1,2] Current clinical treatments for duodenal ulcers primarily include H2 receptor antagonists (H2 RA) and proton pump inhibitors (PPIs). The PPIs specifically inhibit the H+/K+-ATPase of gastric parietal cells, resulting in the strong and continuous inhibition of gastric acid secretion and accelerated healing of ulcers. PPIs have become the preferred treatments in the acid-related disorders including duodenal ulcer.[3,4]
At present, there are several kinds of PPIs in the treatment of duodenal ulcer, including omeprazole (Ome), lansoprazole (Lan), raberazole (Rab), pantoprazole (Pan), esomeprazole (Esome), and the latest ilaprazole (Ila). Different PPIs and different doses may have different healing rates and different side effects,[5,6,7,8,9] in addition to different costs.[10,11] However, there are no systemic reviews to compare the relative efficacy and tolerance of various PPI regimens in the treatment of duodenal ulcer not induced by drugs such as aspirin, corticosteroids, and non-steroidal anti-inflammatory drugs (NSAIDs) until now, with only one study,[12] which compared the 4-week healing rate and tolerance of Ila 10 mg/d with other PPIs in the treatment of duodenal ulcers. Therefore, in the present study, a network meta-analysis of randomized controlled trials (RCTs) was conducted to combine the direct and indirect evidence to compare the healing rates and adverse effects of different PPIs in ordinary doses for patients with duodenal ulcer. Additional pairwise meta-analysis was also performed to obtain further evidence for the efficacy of different PPI regimens including the stratification of Helicobacter pylori (Hp).
MATERIALS AND METHODS
Search strategy
Medline, Embase, Cochrane Library, ClinicalTrails.gov, China National Knowledge Infrastructure (CNKI), and Chinese Biomedical Literature Database (CBM) were searched for “omeprazole,” “lansoprazole,” “raberazole,” “pantoprazole,” “esomeprazole,” and “ilaprazole” to collect all RCTs conducted among human participants up to May 1st, 2016. We also performed a complete manual search from the bibliographies of each peer reviewed paper selected. The language was limited to English or Chinese. Furthermore, there was no limitation regarding publication form.
Study selection criteria
The selection criteria for inclusion in the meta-analysis were: (1) RCTs comparing PPIs with other regimens including the same PPI of different doses in the treatment of duodenal ulcers in adults; (2) Duodenal ulcers must have been diagnosed by upper gastrointestinal endoscopy; (3) The patients should not have received other medical therapies before the trial, including compounds of ulcerogenic potential (aspirin corticosteroids, NSAIDs); (4) The duration of the trials should be 4 weeks; ulcer healing was also assessed by endoscopy after 4 weeks of therapy; (5) The results of the study should be based on intention-to-treat (ITT) analysis. Furthermore, we excluded trials or arms using nonstandard doses, which mainly came from dose-range studies, including Lan 7.5 mg/d, Ila 5 mg/d, and Ila 20mg/d. The decision to include or exclude any trial was made by two researchers separately.
Data extraction and quality evaluation
Data were independently abstracted from each trial by two researchers, and disagreement was resolved by consensus. Data to be extracted included (1) Author, year of publication; (2) Study design; (3) Number of patients in each treatment arm, duration of treatment, drug regimen and other baseline characteristics; (4) Outcomes: 4-week healing rate of duodenal ulcers and percentage of adverse effects. Quality of studies was assessed according to the JADAD scale: adequate method for randomization, appropriate blinding procedures, and detailed report of withdrawals.
Data analysis
The network meta-analysis was performed to compare the relative efficacy and safety of different PPIs in different doses using the Bayesian Markov Chains Monte Carlo methods with ADDIS Version 1.16.6(Decision Support Systems), and the results were summarized using relative risk (RR) and 95% confidence intervals (CIs). Then the ranking probability was estimated for each drug, that is, the most effective drug, the second best, third best, etc. The overall ranks were interpreted using the surface under the cumulative ranking (SUCRA) technique and rank probability sum to one.[13] Rank 1 is considered the preferred agent for the specific outcome. To estimate inconsistency, we calculated the difference between indirect and direct estimates, in which inconsistency was defined as disagreement between direct and indirect evidence with a 95% CI excluding 0. Furthermore, the node-splitting model was also analyzed with a P- value shown, in which a large P value indicates that no significant inconsistency was found.
The pairwise meta-analysis was conducted to compare the 4-week healing rates of different PPIs in different doses, using the random effects model with Review Manager Software (RevMan 5.3) (The Nordic Cochrane Centre). Heterogeneity was tested using the I2 test (I2 score of 50% indicates more than moderate heterogeneity). In all analysis, P < 0.05 indicated significant difference.
RESULTS
Study characteristics
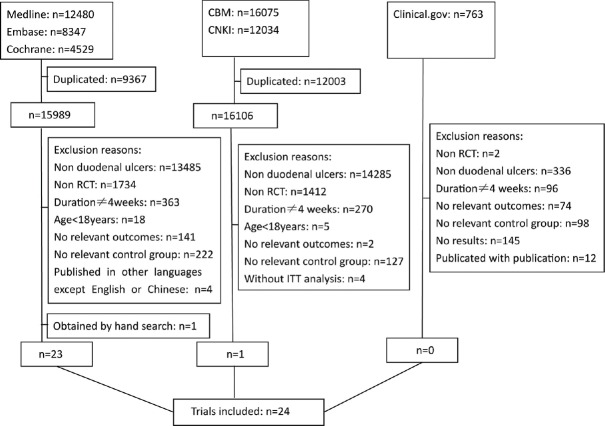
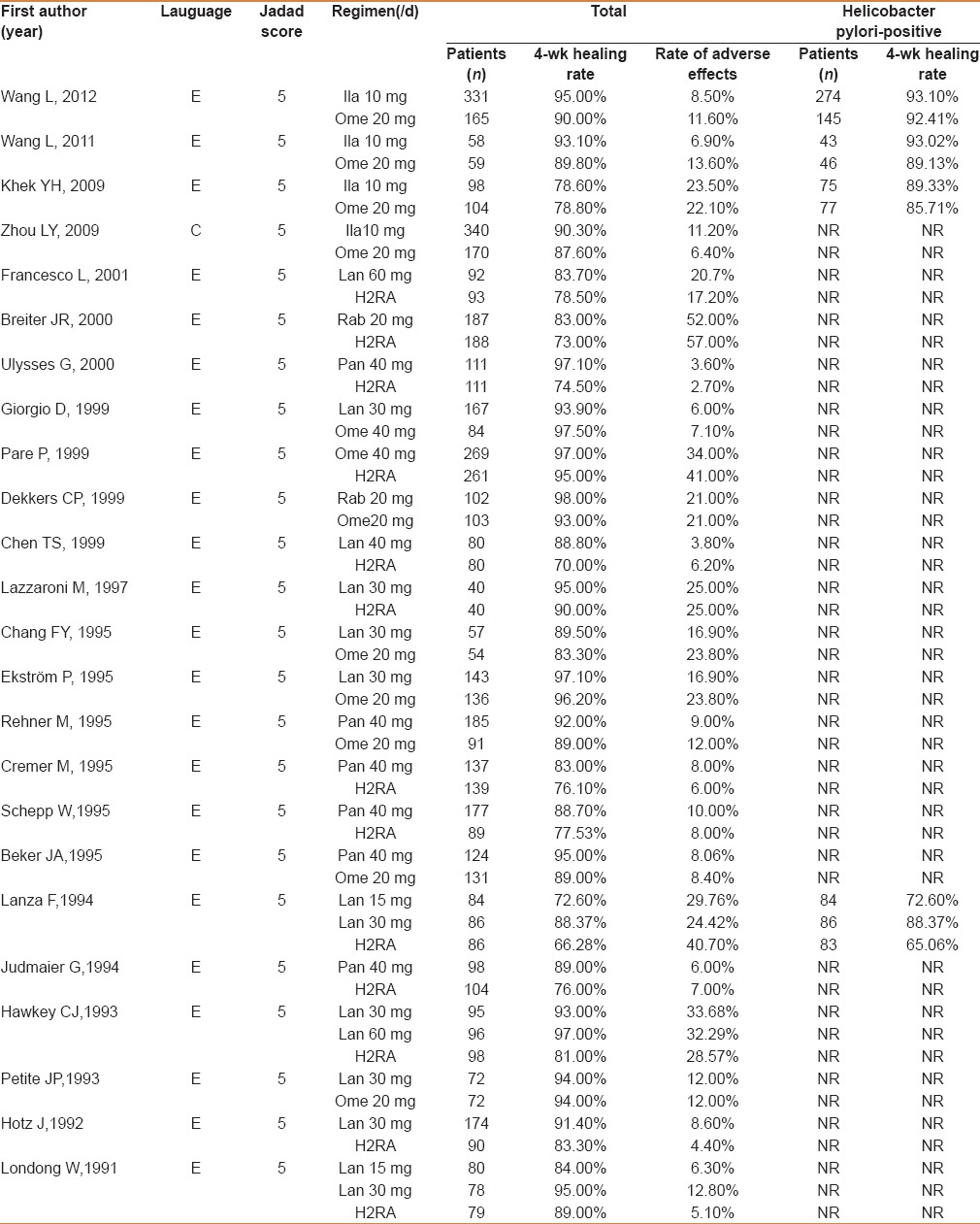
The trial flow is summarized in Figure 1. A total of 24 RCTs involving 6188 patients in the treatment of duodenal ulcer fulfilled the criteria for the meta-analysis. All the trials were published in English except one. Only 4 trials reported the healing rate of duodenal ulcer in patients infected with Hp. All the trials were of high quality, with a JADAD score of 5. The baseline characteristics and quality assessment of included trials are demonstrated in Table 1.
Figure 1.
Trials selection process
Table 1.
Baseline characteristics and quality assessment of include trials
Evidence for network meta-analysis
In the network analysis, 9 regimens were analyzed, including Ome 20 mg/d, Ome 40 mg/d, Lan 15 mg/d, Lan 30 mg/d, Lan 60 mg/d, Pan 40 mg/d, Rab 20 mg/d, Ila 10 mg/d, and H2 RA. Among the included trails, 21 were two-arm studies and 3 were three-arm studies, with 51 arms altogether [Figure 2].
Figure 2.
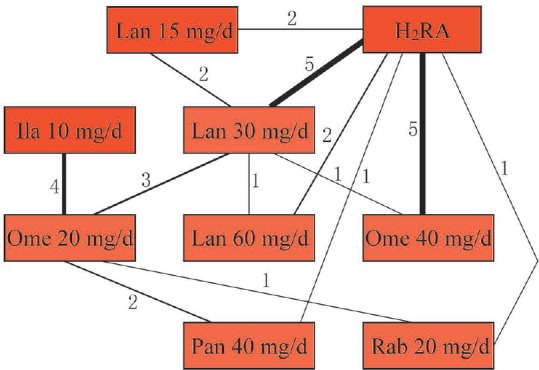
Evidence of PPIs for the 4-week healing rate of duodenal ulcer in network meta-analysis. The numbers along the link lines indicate the number of trials or pairs of trial arms. Lines connect the interventions that have been studied in head-to-head (direct) comparisons in the eligible RCTs. The width of the lines represents the cumulative number of RCTs for each comparison
Efficacy and safety of proton pump inhibitors for patients with duodenal ulcer
Figure 3 displays the geometric distribution of efficacy and safety of different PPIs in different doses for patients with duodenal ulcer. We found that Pan 40 mg/d and Lan 30 mg/d significantly increased the healing rate in comparison with H2 RA (RR = 2.96; 95% CI = 1.78–5.14 and RR = 2.04, 95% CI = 1.13–3.53, respectively). Furthermore, there were no signicant difference of the healing rate for duodenal ulcer treated with different PPIs in different doses except Pan 40 mg/d versus Lan 15 mg/d (RR = 3.57; 95% CI = 1.36–10.31) and Lan 30 mg/d versus Lan 15 mg/d (RR = 2.45, 95% CI = 1.01–6.14). Pan 40 mg/d was more effective compared with other regimens, although most of the difference was not significant and Lan 15 mg/d had a lower healing rate versus other regimens. Our analysis also indicated that there was no significant difference for the rate of adverse effects between different PPIs in different doses.
Figure 3.
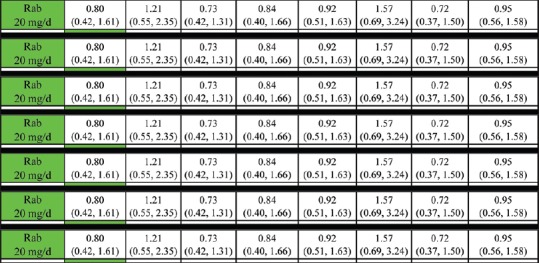
4-week healing rate (lower triangle) and rate of adverse effects (upper triangle) of all regimens according to the network meta-analysis. Comparisons between regimens should be read from left to right and the estimate is in the cell between the column-defining treatment and the row-defining treatment. For 4-week healing rate, RRs higher than 1 favor the column-defining treatment, whereas for rate of adverse effects, RRs lower than 1 favor the column-defining treatment. To obtain RRs for comparisons in the opposite direction, reciprocals should be taken (e.g., the RR of 4-week healing rate for Ila 10 mg compared with Rab 20 mg is 1/1.20 = 0.83). Significant results are in bold and underscored
The ranking of proton pump inhibitors of 4-week healing rate
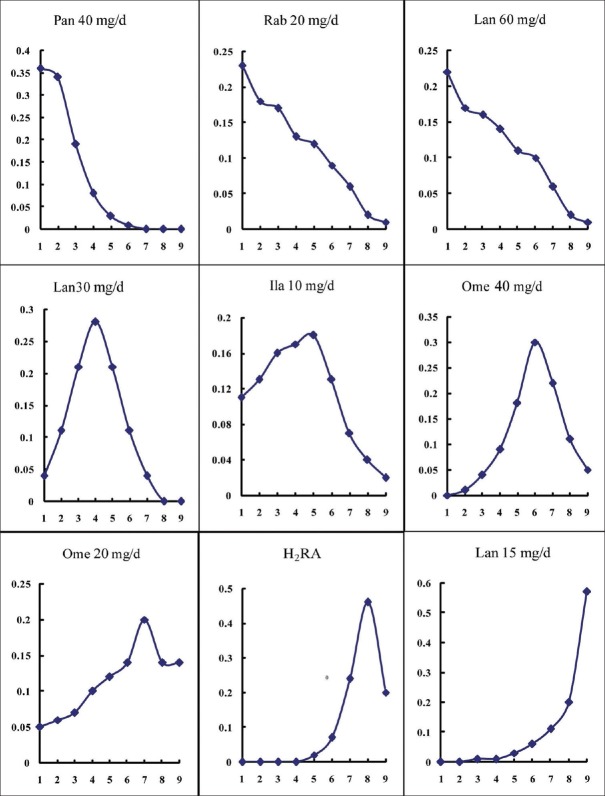
The distribution of probabilities for different PPIs being ranked at different positions for the outcome of 4-wk healing rate is shown in Figure 4. The probability ranking demonstrated that Pan 40 mg/d had a higher probability (36%) of being at the best ranking positions; Lan 15 mg/d was the treatment with the highest probability (57%) of being in the last ranking position, and the relative ranking of preferred agent for 4-week healing rate in the treatment of duodenal ulcer was: Pan 40 mg/d > Rab 20 mg/d > Lan 60 mg/d > Lan 30 mg/d > Ila 10 mg/d > Ome 40 mg/d > Ome 20 mg/d > H2 RA > Lan 15 mg/d.
Figure 4.
Ranking of treatment strategies based on the probability of their 4-week healing rate of duodenal ulcer. The x-axis indicates the ranks and the y-axis indicates ranking probability at different priority. Rank 1 on the x-axis is considered to be the preferred agent for the specific outcome, and an increasing number on the x-axis indicates a less preferred ranking
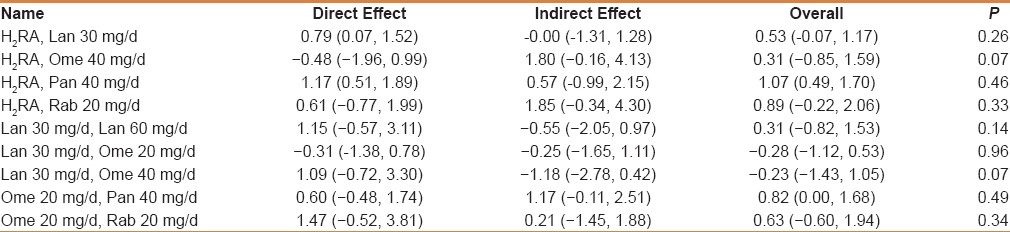
Model inconsistency
In the network meta-analysis, the disagreement between direct and indirect comparison was concerning and examined by calculating the inconsistency factors. For all comparisons in the 4-week healing rate, the 95% CI of inconsistency factors from all cycles included zero [Table 2], and the node-splitting method showed no significant inconsistency within the networks for any of these outcomes [Table 3], which suggested that the results in the network were consistent between direct and indirect evidence.
Table 2.
Inconsistency factors of all comparisons in the 4-week healing rate
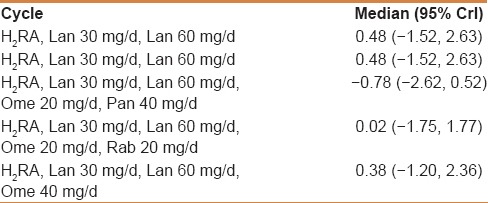
Table 3.
The node-splitting of all comparisons in the 4-week healing rate
Pairwise meta-analyses for 4-week healing rate
The RCTs of every two regimens with the direct comparisons ≥2 were included in the traditional pairwise meta-analyses for the 4-wk healing rate in the treatment of duodenal ulcer. A total of 8 comparisons [Figure 5] were conducted in the pairwise meta-analyses, including Pan 40 mg/d, Lan 60 mg/d, Lan 30 mg/d, and Lan 15 mg/d vs H2 RA, Pan 40 mg/d, Ila 10 mg/d, and Lan 30 mg/d vs Ome 20 mg/d, Lan 30 mg/d vs Lan 15 mg/d. Similarly, the results suggested that the healing rate of duodenal ulcer treated with Pan 40 mg/d and Lan 30 mg/d were significantly higher (P < 0.00001 and P = 0.04, respectively) than H2 RA. While compared to Ome 20 mg/d, there were no significant difference for all the three treatments, and Lan 30 mg/d still had a statistically significant impact on the healing rate of duodenal ulcer in comparison with Lan 15 mg/d (P = 0.003). In addition, all the I2 in the comparisons were <50%, which indicated that there was just low heterogeneity in the included trails.
Figure 5.
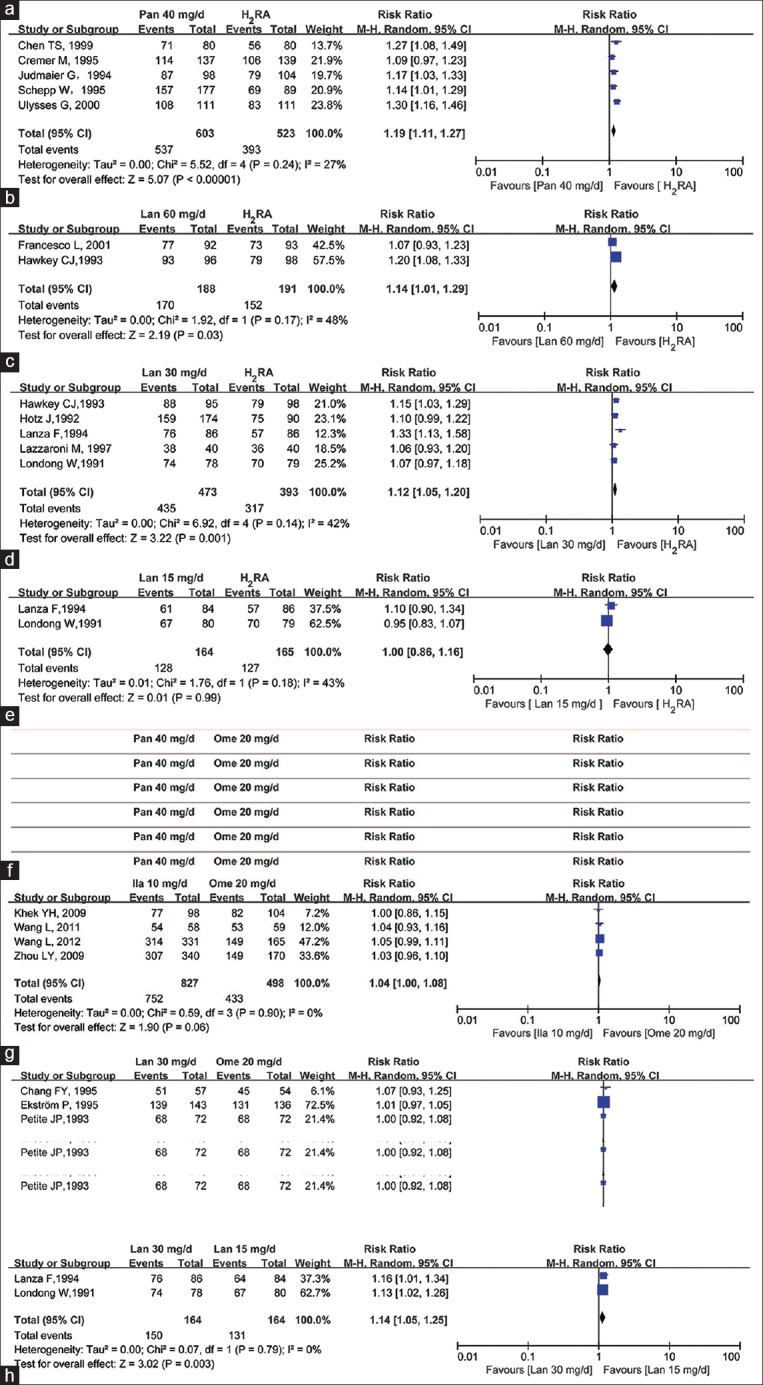
RR and 95% CI of 4-week healing rate for duodenal ulcer in pairwise meta-analyses. (a) Pan 40 mg/d versus H2 RA; (b) Lan 60 mg/d versus H2 RA; (c) Lan 30 mg/d versus H2 RA; (d) Lan 15 mg/d versus H2 RA; (e) Pan 40 mg/d versus Ome 20 mg; (f) Ila 10 mg/d versus Ome 20 mg; (g) Lan 30 mg/d versus Ome 20 mg/d; (h) Lan 30 mg/d versus Lan 15 mg/d
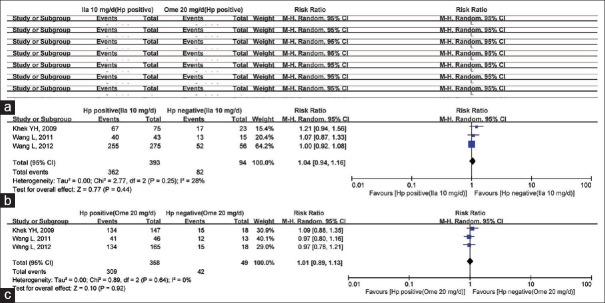
Pairwise meta-analyses for 4-week healing rate concerning the status of Helicobacter pylori
The 3 RCTs, which reported the 4-wk healing rate of Hp positive patients treated by Ila 10 mg/d or Ome 20 mg/d were included. Similar to the total 4-week healing rate of Ila 10 mg/d compared to Ome 20 mg/d [Figure 5f], the results [Figure 6] showed that the healing rate for duodenal ulcer treated with Ila 10 mg/d was slightly higher than with Ome 20 mg/d in the Hp positive patients, but without statistical significance. Furthermore, there were no significant difference between the status of Hp treated with neither Ila 10 mg/d nor Ome 20 mg/d.
Figure 6.
RR and 95% CI of 4-week healing rate for duodenal ulcer concerning the status of Helicobacter pylori (Hp). (a) Ila 10 mg/d (Hp positive) versus Ome 20 mg (Hp positive); (b) Hp positive (Ila 10 mg/d) versus Hp negative (Ila 10 mg/d); (c) Hp positive (Ome 20 mg) versus Hp negative (Ome 20 mg)
DISCUSSION
There were 24 RCTs and 6188 patients were included in the Bayesian network meta-analysis to assess the efficacy and safety of PPIs. The combined direct and indirect evidence suggested that Pan 40 mg/d may be the most effective regimen for patients with duodenal ulcers, especially compared to H2 RA and Lan 15 mg/d, and there was almost no significant difference between the two PPI regimens with the exception of Pan 40 mg/d versus Lan 7.5 mg/d and Lan 30 mg/d versus Lan 15 mg/d. The probability ranking analysis also suggested that Pan 40 mg/d was the preferred agent and Lan 15 mg/d was the most unfavorable one in the treatment of duodenal ulcer. Similarly, the head to head comparisons indicated the Pan 40 mg/d and Lan 30 mg/d were more effective in comparison with H2 RA; Lan 30 mg/d had a significantly higher healing rate versus Lan 15 mg/d. However, there were no obvious trends during each regimen for the side effects in the treatment of duodenal ulcer.
PPIs are highly effective medications widely used in the management of peptic diseases including gastric and duodenal ulcers, gastroesophageal reflux disease, and Zollinger–Ellison syndrome. Many new therapeutic drugs with similar structures and better therapeutic outcomes have been developed since Ome first entered the market, including Rab, Pan, Lan, Esome, and the new molecule Ila. However, in our study only 5 PPIs were included with yhr exception of Esome, which may be because Esome was more effective in the inhibition of gastric acid secretion[14,15] and the regimens of Esome for patients with duodenal ulcers only need 7 or 10 days.[16,17] The dose of Lan for the management of duodenal ulcer in the label was 15 mg/d, 30 mg/d, or 60 mg/d, depending on the state of illness, and the current standard dose of Ila recommended for the peptic diseases is 10 mg/d. Accordingly, the regimens of Lan in 7.5 mg/d, Ila in 5 mg/d and 20 mg/d were excluded from our analysis.
In this study, the ITT analysis was used as an inclusion criterion, which excluded 4 trials published in Chinese, which may be benefical to enhance the quality of trials, and therefore, all the RCTs included in our study were with a JADAD score as 5. Heterogeneity in the pairwise meta-analysis also suggested that there were no obvious publication bias (I2≤ 50%). In addition, model inconsistency indicated that the results in the network were consistent between direct and indirect evidence.
The healing rate of PPIs may be influenced by the status of Hp, as a result, we also compared the healing rate of different regimens in the Hp positive patients as well as of different Hp status treated with the same regimens. The results suggested that the status of Hp may have no effects on the efficacy of PPIs, however, the included RCTs and patients was too small to obtain further evidence. In addition, the genotype of CYP2C19 plays a major role in the metabolism of PPIs and it may have an impact on the clinical action of PPI regimens. Unfortunately, most of the included trials did not report the CYP2C19 genetype of patients, with the exception of the latest one;[18] therefore, the CYP2C19 genetype stratification was not analyzed in this study, which is the main limitation of this study.
However, our results may be helpful for clinicians in choosing PPIs with a higher healing rate for duodenal ulcer to some extent; Lan in a low dose (15 mg/d) may have no advantage even in comparison with H2 RA, and the relatively preferred agent may be Pan 40 mg/d. Furthermore, more RCTs to compare the efficacy and safety of different PPIs including more confounding factors are needed urgently to supply more suggestions for the clinicians.
Financial support and sponsorship
This study was financially supported by the Jiangsu Province Pharmaceutical Association, China (project number: 201414-3). The authors have no relevant affiliations or financial involvement with any other organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lau JY, Barkun A, Fan DM, Kuipers EJ, Yang YS, Chan FK. Challenges in the management of acute peptic ulcer bleeding. Lancet. 2013;381:2033–43. doi: 10.1016/S0140-6736(13)60596-6. [DOI] [PubMed] [Google Scholar]
- 2.Milosavljevic T, Kostić-Milosavljević M, Jovanović I, Jovanović I, Krstić M. Complications of peptic ulcer disease. Dig Dis. 2011;29:491–3. doi: 10.1159/000331517. [DOI] [PubMed] [Google Scholar]
- 3.Malfertheiner P, Chan FK, McColl KE. Peptic ulcer disease. Lancet. 2009;374:1449–61. doi: 10.1016/S0140-6736(09)60938-7. [DOI] [PubMed] [Google Scholar]
- 4.Chan FK. Proton-pump inhibitors in peptic ulcer disease. Lancet. 2008;372:1198–200. doi: 10.1016/S0140-6736(08)61497-X. [DOI] [PubMed] [Google Scholar]
- 5.Londong W, Barth H, Dammann HG, engels KJ, Kleinert R, Müller P, et al. Dose-related healing of duodenal ulcer with the proton pump inhibitor lansoprazole. Aliment Pharmacol Ther. 1991;5:245–54. doi: 10.1111/j.1365-2036.1991.tb00025.x. [DOI] [PubMed] [Google Scholar]
- 6.Müller P, Simon B, Khalil H, Lühmann R, Leucht U, Schneider A. Dose-range finding study with the proton pump inhibitor pantoprazole in acute duodenal ulcer patients. Z Gastroenterol. 1992;30:771–5. [PubMed] [Google Scholar]
- 7.Heidelbaugh JJ, Kim AH, Chang R, Walker PC. Overutilization of proton-pump inhibitors: What the clinician needs to know. Therap Adv Gastroenterol. 2012;5:219–32. doi: 10.1177/1756283X12437358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ramsay EN, Pratt NL, Ryan P, Roughhead EE. Proton pump inhibitors and the risk of pneumonia: A comparison of cohort and self-controlled case series designs. BMC Med Res Methodol. 2013;13:82. doi: 10.1186/1471-2288-13-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fraser LA, Leslie WD, Targownik LE, Papaioannou A, Adachi JD. CaMos Research Group. The effect of proton pump inhibitors on fracture risk: Report from the Canadian Multicenter Osteoporosis Study. Osteoporos Int. 2013;24:1161–8. doi: 10.1007/s00198-012-2112-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.MacLaren R, Campbell J. Cost-effectiveness of histamine receptor-2 antagonist versus proton pump inhibitor for stress ulcer prophylaxis in critically ill patients. Crit Care Med. 2014;42:809–15. doi: 10.1097/CCM.0000000000000032. [DOI] [PubMed] [Google Scholar]
- 11.Heidelbaugh JJ, Goldberg KL, Inadomi JM. Overutilization of proton pump inhibitors: A review of cost-effectiveness and risk [corrected] Am J Gastroenterol. 2009;104(Suppl 2):S27–32. doi: 10.1038/ajg.2009.49. [DOI] [PubMed] [Google Scholar]
- 12.Ji XQ, Du JF, Chen G, Chen G, Yu B. Efficacy of ilaprazole in the treatment of duodenal ulcers: A meta-analysis. World J Gastroenterol. 2014;20:5119–23. doi: 10.3748/wjg.v20.i17.5119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: An overview and tutorial. J Clin Epidemiol. 2011;64:163–71. doi: 10.1016/j.jclinepi.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 14.McKeage K, Blick SK, Croxtall JD, Lyseng-Williamson KA, Keating GM. Esomeprazole: A review of its use in the management of gastric acid-related diseases in adults. Drugs. 2008;68:1571–607. doi: 10.2165/00003495-200868110-00009. [DOI] [PubMed] [Google Scholar]
- 15.Beck Jean. Efficacy of esomeprazole in patients with acid-peptic disorders. Gastroenterol Nurs. 2004;27:44–9. doi: 10.1097/00001610-200403000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Subei IM, Cardona HJ, Bachelet E, Useche E, Arigbabu A, Hammour AA, et al. One week of esomeprazole triple therapy vs 1 week of omeprazole triple therapy plus 3 weeks of omeprazole for duodenal ulcer healing in Helicobacter pylori positive patients. Dig Dis Sci. 2007;52:1505–12. doi: 10.1007/s10620-006-9522-5. [DOI] [PubMed] [Google Scholar]
- 17.Boon YH, Vu C, Kaushik S, Cheng CS, Chiu TC, Chian LC. One week regimen of esomeprazole based triple therapy is sufficient for duodenal ulcer healing and Helicobacter pylori eradication in patients with duodenal ulcer disease. Eur J Gastroenterol Hepatol. 2002;14:905. doi: 10.1097/00042737-200208000-00019. [DOI] [PubMed] [Google Scholar]
- 18.Klotz U. Clinical impact of CYP2C19 polymorphism on the action of proton pump inhibitors: A review of a special problem. Int J Clin Pharmacol Ther. 2006;44:297–302. doi: 10.5414/cpp44297. [DOI] [PubMed] [Google Scholar]