Abstract
Introduction:
Early diagnosis and management of depression is important for better therapeutic outcome. Strategies for distinguishing between unipolar and bipolar depression are yet to be defined, resulting improper management. This study aims at comparing the socio-demographic and other variables between patients with unipolar and bipolar depression, along with assessment of severity of depression.
Materials and Methods:
This cross sectional study was conducted in a tertiary care psychiatry hospital in North-East India. The study included total of 330 subjects selected through purposive sampling technique from outpatient department after obtaining due informed consent. Mini-International Neuropsychiatric Interview (M.I.N.I.) version 6.0 and Beck Depression Inventory (BDI) were applied. Statistical Package for Social Sciences (SPSS) version 16.0 was applied for analysis.
Results:
Bipolar group had onset of illness at significantly younger age with more chronicity (32.85 ± 11.084). Mean BDI score was significantly higher in the unipolar depressive group.
Conclusion:
Careful approach in eliciting symptom severity and associated socio demographic profiles in depressed patients may be helpful in early diagnosis of bipolar depression.
Keywords: Beck depression inventory, bipolar, depression, unipolar
INTRODUCTION
Depression is a common mental disorder, with an estimated global burden of 350 million.[1] Lifetime prevalence rates range from approximately 3% to 16.9%, with most countries falling somewhere between 8% and 12%.[2]
Depressive disorder is diagnosed when the patient suffers from depressed mood, loss of interest and enjoyment, and reduced energy leading to increased fatigability and diminished activity for at least 2 weeks along with other common symptoms such as reduced concentration and attention, reduced self-esteem and self-confidence, ideas of guilt and unworthiness, blank and pessimistic views of future, ideas or acts of self-harm or suicide, disturbed sleep, and diminished appetite.
If there is a history of at least one hypomanic, manic, or mixed affective episode in the past, then the depressed person is diagnosed to have bipolar depression. Psychotic symptoms may emerge in both types of depression along with relapse and remission.[3,4]
Unipolar depressive disorders were ranked fourth in 2004 and will rise to the first place by 2030 in terms of the global burden of all diseases.[1] Bipolar disorder affected an estimated 29.5 million individuals worldwide in 2004, according to the World Health Organization.[5] If the current trends for demographic and epidemiologic transition continue, it is estimated that by the year 2020, the burden of depression will increase to 5.7% of the total burden of disease and it would be the second leading cause of disability-adjusted life years.[6,7]
The distinction between unipolar and bipolar depression remains a challenging clinical problem, particularly when bipolar individuals present in the depressive phase and they may easily be mistaken for unipolar depression.[8,9,10] There are differences in the optimal management of these conditions. Patients with bipolar depression who are assumed to have unipolar depression will receive inappropriate therapy that can increase the risk of manic switch or cycle acceleration.[11,12] Measures to clinically recognize or at least to suspect the kind of disorder in the early stage can greatly improve diagnosis and management of such disorders, with more appropriate treatment selection which will help in long-term care of these groups of people.
We are yet to know the details of the biological processes involved in these clinical conditions and the different factors associated. This study was undertaken with the objective of comparing the sociodemographic variables associated with unipolar and bipolar depression groups. It also aimed at assessing the degree of depression among the unipolar and bipolar groups.
MATERIALS AND METHODS
This study is a cross-sectional study conducted in a Tertiary Care Psychiatry Hospital in North-East India. Patients with unipolar and bipolar depression from outpatient department fulfilling the inclusion criteria were selected by purposive sampling. A total of 330 depression patients, 164 unipolar and 166 bipolar cases, were included in the study.
Inclusion criteria
Patients of the age group of 18–65 years, irrespective of their genders, diagnosed with depression both unipolar and bipolar as per the International Statistical Classification of Diseases and Related Health Problem Tenth Revision (ICD-10), were included. Patients without medication for at least 1 month before the onset of the current episode who gave written informed consent were considered.
Exclusion criteria
Patients with comorbid medical illness or any other psychiatric disorder including substance dependence and personality disorders were excluded from the study.
Tools
A semi-structured pro forma was used for the assessment of the sociodemographic and clinical variables of the patients.
ICD-10 was used. Mini-International Neuropsychiatric Interview Version 6.0 was used to validate the clinical diagnosis.
The severity of depression among the depressive patients was assessed by 21-item Beck Depression Inventory (BDI).
Statistical analysis
Results were described using descriptive and analytical statistics with the help of SPSS version 23.0 (SPSS South Asia Pvt Ltd., Bangaluru, Karnataka, India).
RESULTS
The sociodemographic data, BDI score, and the severity of the depression have been summarized in Tables 1 and 2. Both groups did not differ significantly age-wise at the time of assessment.
Table 1.
Sociodemographic and illness profile of patients with unipolar and bipolar depression (for continuous variables)
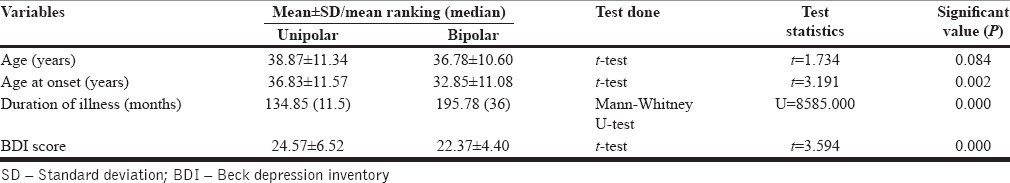
Table 2.
Sociodemographic profile of patients with unipolar and bipolar depression (for discrete variables)
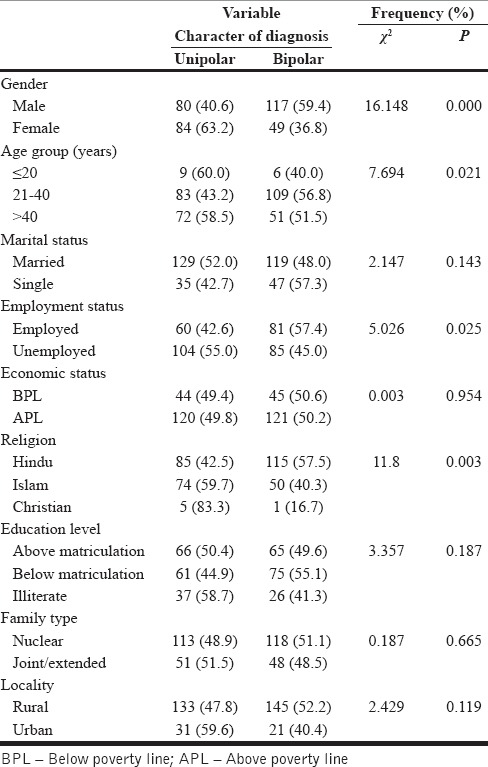
Of total 330 subjects, 197 (59.7%) were male. In the whole sample, there was over-representation of male as depressed patients. 59.4% of the male and 36.8% of the females are found to have bipolar depression and this difference was statistically significant. Thus, male-depressed persons are significantly more likely to get bipolar depression.
The mean age at onset of unipolar depression was 36.83 ± 11.57 years which is significantly higher than the mean age at onset of bipolar depression [Table 1]. Of 330 patients, 192 (58.2%) were in the age group of 21–40 years and 56.8% of them had bipolar depression. Only 15 (4.5%) of the total sample were younger than 20 years of age and had depression both in unipolar and bipolar [Table 2]. Thus, the risk of depression rises with age peaking in the middle age [Figure 1]. Table 3 shows that the age at onset of illness after 40 years is significantly associated with unipolar depression.
Figure 1.
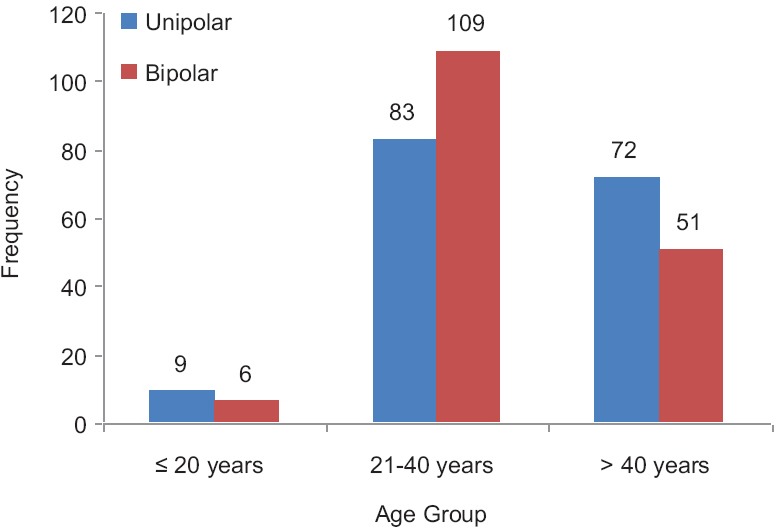
Frequency distribution based on age group
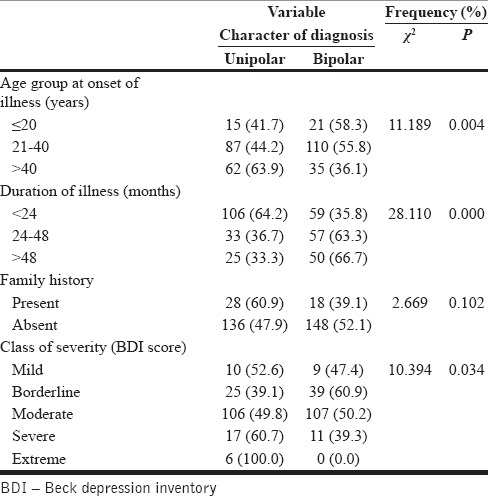
Table 3.
Illness profile of patients with unipolar and bipolar depression (for discrete variables)
Marital status, socioeconomic status, education, family type, and locality of the patient did not have any significant relationship with the type of depression [Table 2]. Interestingly, Hindu depressed patients were likely to have bipolar depression as compared to their Muslim and Christian counterparts. Of 330 patients, 141 were employed and they had more likelihood of having bipolar depression (57.4%).
Figure 2 shows that the duration of illness in both types of depression follows a similar curve with majority of them having <48 months of illness. However, the distribution is seen to be more uniformly distributed among the bipolar depression group [Figure 3]. Unipolar depression had a relatively significant lesser duration of total illness as compared to that of bipolar illness. Most patients in both groups had a moderate level of depression. The mean BDI score in unipolar depression is 24.57 ± 6.52, which is significantly higher than that of the bipolar depression group [Table 1].
Figure 2.
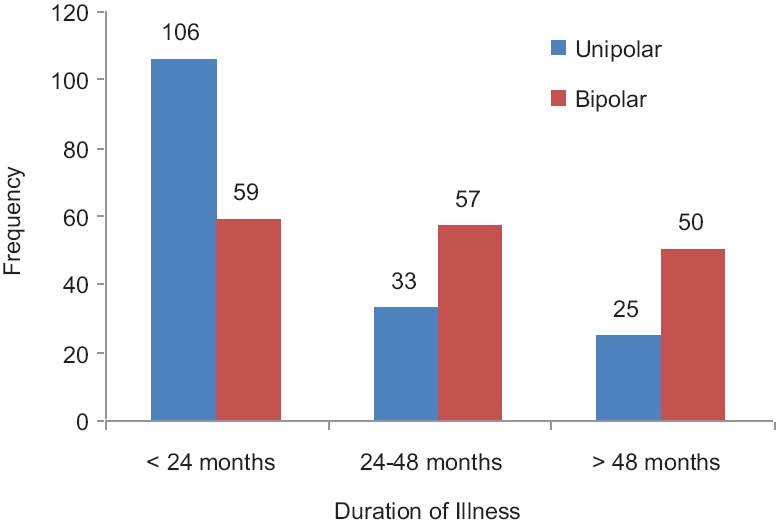
Frequency distribution based on illness duration
Figure 3.
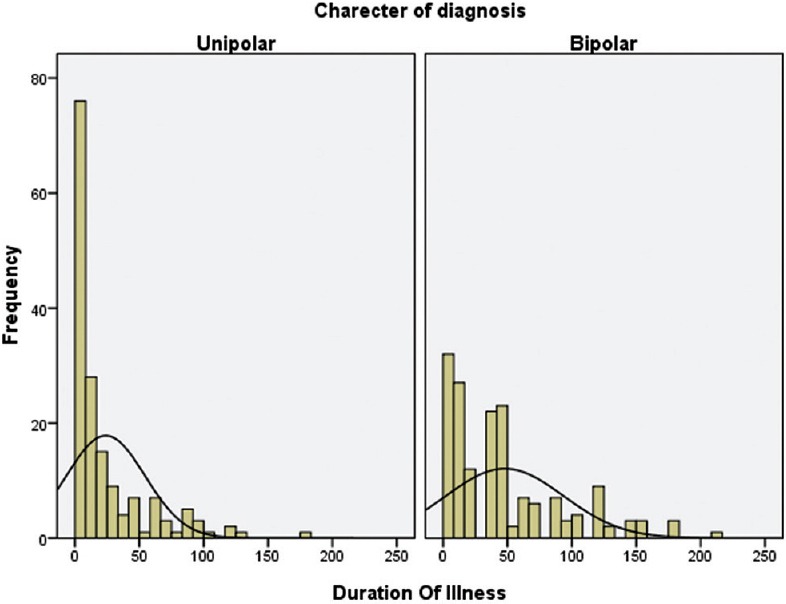
Normality curve of illness duration in unipolar and bipolar groups
DISCUSSION
The average age of the unipolar group at the time of interview was found to be higher nonsignificantly compared to the bipolar group which is consistent with the previous studies.[13,14,15,16]
Like other studies,[15,16,17,18] the mean age of illness onset and the illness onset age group is significantly earlier among the bipolar patients than among those with unipolar depression, with the median of the duration of illness more in bipolar group compared to unipolar.[13,16,17,18] Patients with unipolar depression had a shorter duration of illness. Bipolar group may have earlier onset with a more chronic course.
Although the prevalence of unipolar depression is more in female but in bipolar depression, male are found to be equally exposed. We have found male are equally exposed in unipolar group which is contrary to many other studies which were population based.[16,19,20,21,22] As the sample comprised both unipolar and bipolar depression cases and also the sampling was done on purposive method from a psychiatric hospital, we may explain over-representation of males in the sample.
Married group comprised the majority in both unipolar and bipolar groups, similar to the findings of Berlim et al., 2004.[14] In contrast to their result, we found married patients were more prone to unipolar depression compared to bipolar depression, similar to the study of Motovsky and Pecenak, 2013.[15] Employment status of the patient and depression were found to be strongly associated, most cases being unemployed, comparatively more among unipolar group. This is in consistent with the findings from the study conducted in University Hospital, Trencin, Slovakia.[15]
Economic status of the patients did not show any marked difference between unipolar and bipolar groups. However, most of them represented the economically healthy class, in contradiction to other studies where socially disadvantaged people are seen more prone to depression, either unipolar or bipolar.[20,23,24,25,26] Our finding may be explained on the basis of site of the study and the relative ability of the patients to bear travel expenses.
Hindu community comprised the majority in both unipolar and bipolar groups, with significantly more subjects in bipolar group. A deep look into religio-ethno-cultural phenomenological aspects of depression may give interesting finding.
There is no significant association observed between education level of the subjects and the character of diagnosis; however, the majority of the unipolar cases are found above matric education, but bipolar groups are found to have lower level of education as seen in other studies.[14,20,22] This may be due to the fact of preferences to services by the highly educated group.
Family type of the patients did not show any significant difference between unipolar and bipolar groups; however, majority in both were from nuclear type of family. This could be explained by the fact that emergence of nuclear family from the breakdown of joint family resulting in reduced family support.
The rural population comprised the majority as the study is based on the setting with rural majority, with no significant difference between unipolar and bipolar groups.
The severity of depression is more in unipolar group compared to bipolar group, which is in concordance with the findings of Katz et al., 1982,[28] Mitchell et al., 2004[26] and Forty et al., 2008.[13] Majority of the cases were in the moderate class of severity, with significantly higher mean BDI scores in unipolar group, as seen in the study of Kessler et al., 2005.[27]
Most of the patients had no family history of illness earlier, with nonsignificant association of family history and character of diagnosis. This finding suggests that either these ailments are associated with other nonfamilial factors or most of the cases in the earlier days might be subclinical that went unnoticed or undiagnosed. Again, recall bias could also be an important factor.
Our study is an effort, to find out the differences among the unipolar and bipolar groups of patients on the basis of certain sociodemographic variables along with clinical findings. This is believed to facilitate the proper management of the two conditions.
CONCLUSION
Male gender, employment status, Hindu religion, onset of illness before 40 years, and a long chronic course of illness are the risk factors associated with bipolar depression. As this study is a hospital-based study done using purposive sampling technique, generalizability of the findings should be done with caution.
Financial support and sponsorship
We are thankful to the financial support provided by the Department of Biotechnology, Government of India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This study is a part of the on-going project “Development/Up-gradation of Pathology, Microbiology and Biochemistry Department, under Department of Biotechnology (DBT), India”. We are thankful to DBT India, staffs of Lokopriya Gopinath Bordoloi Regional Institute of Mental Health (LGBRIMH), Tezpur, Assam, India.
REFERENCES
- 1.World Health Organization. Depression a Global Public Health Concern. 2012. [Last accessed on 2016 Feb 22]. Available from: http://www.who.int/mental_health/management/depression/who_paper_depression_wfmh_2012.pdf .
- 2.Andrade L, Caraveo-Anduaga JJ, Berglund P, Bijl RV, De Graaf R, Vollebergh W, et al. The epidemiology of major depressive episodes: Results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int J Methods Psychiatr Res. 2003;12:3–21. doi: 10.1002/mpr.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. ICD-10 International Statistical Classification of Diseases and Related Health Problem. 10th Revision. 4th ed. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 4.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders [DSM-IV]. Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 5.World Health Organization. The Global Burden of Disease: 2004 Update. Geneva: World Health Organization; 2008. [Last accessed on 2016 Apr 02]. Available from: http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004 updatefull.pdf?ua=1 . [Google Scholar]
- 6.Doris A, Ebmeier K, Shajahan P. Depressive illness. Lancet. 1999;354:1369–75. doi: 10.1016/S0140-6736(99)03121-9. [DOI] [PubMed] [Google Scholar]
- 7.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global Burden of Disease and Risk Factors. Washington, DC: The World Bank; 2006. [PubMed] [Google Scholar]
- 8.Benazzi F. Misdiagnosis of bipolar II disorder as major depressive disorder. J Clin Psychiatry. 2008;69:501–2. doi: 10.4088/jcp.v69n0324e. [DOI] [PubMed] [Google Scholar]
- 9.Ghaemi SN, Ko JY, Goodwin FK. “Cade's disease” and beyond: Misdiagnosis, antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry. 2002;47:125–34. doi: 10.1177/070674370204700202. [DOI] [PubMed] [Google Scholar]
- 10.Hirschfeld RM, Lewis L, Vornik LA. Perceptions and impact of bipolar disorder: How far have we really come. Results of the national depressive and manic-depressive association 2000 survey of individuals with bipolar disorder? J Clin Psychiatry. 2003;64:161–74. [PubMed] [Google Scholar]
- 11.Bowden CL. Strategies to reduce misdiagnosis of bipolar depression. Psychiatr Serv. 2001;52:51–5. doi: 10.1176/appi.ps.52.1.51. [DOI] [PubMed] [Google Scholar]
- 12.Ghaemi SN, Boiman EE, Goodwin FK. Diagnosing bipolar disorder and the effect of antidepressants: A naturalistic study. J Clin Psychiatry. 2000;61:804–8. doi: 10.4088/jcp.v61n1013. [DOI] [PubMed] [Google Scholar]
- 13.Forty L, Smith D, Jones L, Jones I, Caesar S, Cooper C, et al. Clinical differences between bipolar and unipolar depression. Br J Psychiatry. 2008;192:388–9. doi: 10.1192/bjp.bp.107.045294. [DOI] [PubMed] [Google Scholar]
- 14.Berlim MT, Pargendler J, Caldieraro MA, Almeida EA, Fleck MP, Joiner TE. Quality of life in unipolar and bipolar depression: Are there significant differences? J Nerv Ment Dis. 2004;192:792–5. doi: 10.1097/01.nmd.0000144700.97769.06. [DOI] [PubMed] [Google Scholar]
- 15.Motovsky B, Pecenak J. Psychopathological characteristics of bipolar and unipolar depression – Potential indicators of bipolarity. Psychiatr Danub. 2013;25:34–9. [PubMed] [Google Scholar]
- 16.Nisha A, Sathesh V, Punnoose VP, Varghese PJ. A comparative study on psycho-socio-demographic and clinical profile of patients with bipolar versus unipolar depression. Indian J Psychiatry. 2015;57:392–6. doi: 10.4103/0019-5545.171842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sadock BJ, Sadock VA. Mood Disorders. 10th ed. Philadelphia: Lippincott Williams and Wilkins; 2007. Kaplan and Sadock's Synopsis of Psychiatry – Behavioral Sciences/Clinical Psychiatry. [Google Scholar]
- 18.Perlis RH, Brown E, Baker RW, Nierenberg AA. Clinical features of bipolar depression versus major depressive disorder in large multicenter trials. Am J Psychiatry. 2006;163:225–31. doi: 10.1176/appi.ajp.163.2.225. [DOI] [PubMed] [Google Scholar]
- 19.Rao AV, Madhavan T. Depression and suicide behaviour in the aged. Indian J Psychiatry. 1983;25:251–9. [PMC free article] [PubMed] [Google Scholar]
- 20.Poongothai S, Pradeepa R, Ganesan A, Mohan V. Prevalence of depression in a large urban South Indian population – the Chennai Urban Rural Epidemiology Study (CURES-70) PLoS One. 2009;4:e7185. doi: 10.1371/journal.pone.0007185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Van de Velde S, Bracke P, Levecque K. Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Soc Sci Med. 2010;71:305–13. doi: 10.1016/j.socscimed.2010.03.035. [DOI] [PubMed] [Google Scholar]
- 22.Verma RK, Min TH, Chakravarthy S, Barua A, Kar N. Sociodemographic correlates of unipolar major depression among the Chinese elderly in Klang Valley, Malaysia: An epidemiological study. ScientificWorldJournal 2014. 2014:812712. doi: 10.1155/2014/812712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chopra HD, Bhaskaran K, Verma IP. Socio-economic status and manic depressive psychosis (a study based on hospital cases) Indian J Psychiatry. 1970;12:40–7. [Google Scholar]
- 24.Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34:119–38. doi: 10.1146/annurev-publhealth-031912-114409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Isometsä E, Aro S, Aro H. Depression in Finland: A computer assisted telephone interview study. Acta Psychiatr Scand. 1997;96:122–8. doi: 10.1111/j.1600-0447.1997.tb09916.x. [DOI] [PubMed] [Google Scholar]
- 26.Mitchell PB, Malhi GS. Bipolar depression: Phenomenological overview and clinical characteristics. Bipolar Disord. 2004;6:530–9. doi: 10.1111/j.1399-5618.2004.00137.x. [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Katz MM, Robins E, Croughan J, Secunda S, Swann A. Behavioural measurement and drug response characteristics of unipolar and bipolar depression. Psychological Medicine. 1982;12:25–36. doi: 10.1017/s0033291700043257. [DOI] [PubMed] [Google Scholar]


