Abstract
Background:
Creation of an ostomy leads to significant change in the body image of the patient. However, adaptation to this alteration of body image is necessary for rehabilitation following surgery. The objective of this study was to identify the factors that influence adaptation to altered body image.
Materials and Methods:
An analytical cross-sectional study was conducted among 41 ostomy patients who were treated at a single tertiary care unit. Body image disturbance questionnaire (BIDQ) was used to assess the perception of body image. Data were analyzed using independent samples t-test (unpaired), Chi-square test, and Spearman's correlation.
Results:
In our study, the mean BIDQ score was 2.22 (standard deviation ± 0.88). The body image disturbance was significantly associated with younger age (P < 0.05). The prevalence of body image disturbance was significantly higher among overweight patients (P < 0.05). Males had a higher BIDQ score than females. Those who had temporary stoma had significantly higher BIDQ score (P < 0.05). Those who felt depressed or had thoughts of self-harm soon after surgery had significantly high body image disturbance score (P < 0.05). There was a significant negative correlation with the perception of self-efficacy and body image disturbance (P < 0.01). There was no significant association between body image disturbance and the diagnosis, type of surgery, or time duration after surgery.
Conclusions:
Poor adaptation to alteration of body image was associated with younger age, overweight, and temporary stoma. Individuals at risk of poor adaptation should be identified before surgery and counseled before surgery, after surgery, and during follow-up visits.
Keywords: Body image, contributory factors, stoma
INTRODUCTION
The worldwide increase in the incidence of colorectal cancer has led to an increase in the ostomy creation surgeries.[1] Many researches have described the psychosocial and emotional problems that arise due to the creation of an ostomy and its impact on patients' lifestyle.[2] Furthermore, the quality of life of patients is also significantly affected by ostomy creation.[3]
Body image is the self-perception of one's physical well-being regarding its attractiveness and function which constantly changes during different stages in life.[4] Body image disturbance was defined as a persistent report of dissatisfaction, concern, and distress that is related to an aspect of appearance, some degree of impairment in social relations, social activities, or occupational functioning.[5] Following ostomy creation, the normal anatomy and function of the gastrointestinal system are changed, and the intestinal contents are diverted to the exterior by an abdominal opening which is created in the small or the large intestine. The contents are collected by means of collecting appliances which need to be changed regularly. Therefore, the stoma surgery creates a sense of alteration in body image and a change in awareness in both appearance and the function of an individual.[2,4]
Several studies have clearly shown that stoma patients experience a perception of negative body image.[6,7,8,9,10] Some studies have even shown that despite considerable improvement in the quality of life, the problems related to body image had only a slight improvement. This fact indicates that this problem may persist without gradually fading away with time.[11] However, the factors that contribute to maladaptation to alteration of body image have not been clearly studied. It is important to identify those factors as it will be helpful to identify those who are at a greater risk of developing maladaptation to alteration of body image. Furthermore, the modifiable contributory factors may be corrected to help the patient to cope with body image problems.
The studies done to identify possible contributory factors that may predict maladaptation to alteration of body image are very limited.[7,9,10,12] These studies have compared those with or without stoma or before and after stoma closure. Furthermore, one study has compared the alteration of body image among those who had temporary and permanent ostomies.[10]
To the authors' knowledge, there are no published studies on perception of the body image among stoma patients in the South Asian setting. Since cultural and socioeconomic factors are different in the Asian communities, it may have a different impact on the adaptation to alteration of body image compared to the Western population. Therefore, this study was aimed to describe the adaptation to alteration of body image in ostomy patients in the local setting and also to identify the contributory factors which may predict maladaptation to alteration of body image.
MATERIALS AND METHODS
This is a descriptive cross-sectional study carried out with the ethical approval obtained from the Ethics Committee of the National Hospital of Sri Lanka. All participants gave informed written consent, which included the right of withdrawing from the study at any point without compromising their clinical treatment.
The study was conducted at the National Hospital of Sri Lanka, Colombo. All patients who presented for follow-up at the Professorial Surgical Unit, National Hospital of Sri Lanka over a period of 1 year were considered for this study. All those who were aged above 18 years, who were living with an enteral ostomy and willing to participate were recruited. Those who underwent emergency surgery for ostomy creation or history of psychiatric illnesses were excluded from the study. Finally, 41 patients were enrolled into this study.
The data were collected during clinic visits while the patients were waiting for consultation. Details on demographic characteristics, details of the disease and surgery-related details were gathered. Demographic characteristics studied included, age, sex, marital status, ethnicity, educational level, body mass index, and social and psychological support. The clinical records were used to gather data on related details on ostomy, disease, and the treatment which included the type of surgery and complications of ostomy. Validated instruments were used to measure perception of body image, depression, anxiety, and self-efficacy.
Study instruments
The perception of body image was measured using a modified body image disturbance questionnaire (BIDQ).[5] This instrument was validated in a nonclinical setting, and it demonstrated good internal consistency and was free of impression-management response bias.[13] The standard seven-item BIDQ was modified so that the term “defect” was substituted with “ostomy.” This modified version of the BIDQ consisted of seven items, i.e. concerns about appearance, mental preoccupation, experiences of emotional distress, impairment in social, occupational, or other important areas of functioning, interference with social life, interference with school work, job or ability to function in one's role, and avoidance of social activities.
The Patient Health Questionnaire-9[14] and Generalized Anxiety Questionnaire-7[15] were used to assess depression and anxiety, respectively.
The level of self-efficacy on caring for stoma was measured using the Stoma Care Self-efficacy Scale, which consisted of 13 items on self-efficacy of managing a stoma. It is designed to assess a general sense of perceived self-efficacy with the aim to assess the coping with day-to-day difficulties of managing a stoma. The total score is calculated to 100, whereas <50 = low self-efficacy and more than 50 = high self-efficacy.[16]
The questionnaires were administered as an interviewer-administered questionnaire to minimize discrepancies.
Data analysis
SPSS 20.0 statistical software (SPSS Inc., Chicago, IL, USA) was used for data analysis. Continuous variables were expressed using means ± standard deviations (SDs). For inferential analysis, Spearman correlations were used to analyze the relationship between continuous variables. Independent samples t-test (unpaired) was used to analyze the relationship of continuous variables between two groups. Statistical testing was performed at <0.05 significance level.
RESULTS
Demographic factors
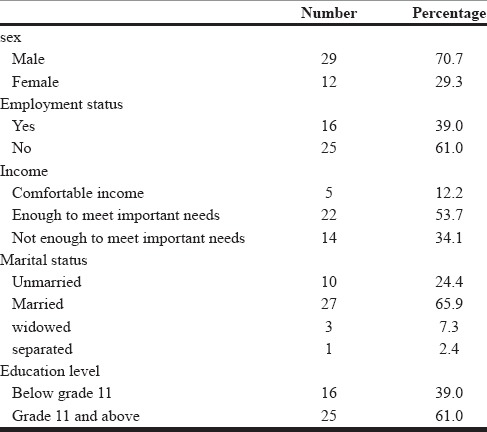
The median age of the study participants was 45 (range, 18–83) years. The median follow-up duration was 37 (range, 6–183) months. The majority of the participants were males (70.7%), unemployed (61%), and married (65.9%) [Table 1].
Table 1.
Demographic characteristics
Characteristics of ostomy
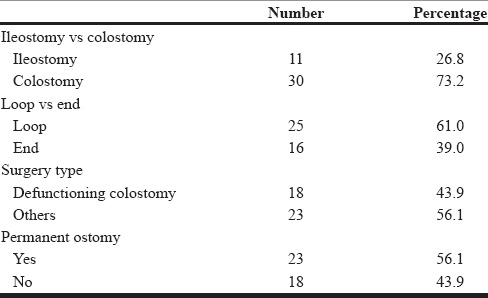
The majority of patients had a colostomy (73.2%). Around 56.1% had a permanent ostomy [Table 2].
Table 2.
Characteristics of ostomy
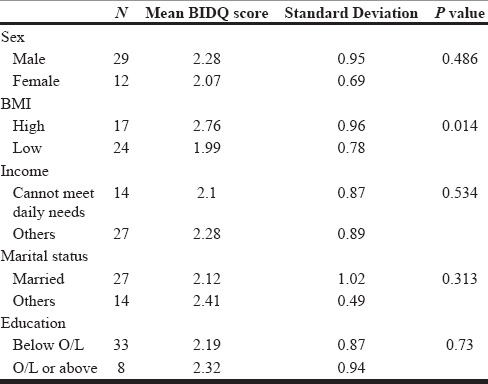
The mean BIDQ score was 2.22 (SD ± 0.88) (range, 1–5). Of the participants, 17.07% (n = 7) had mean body image disturbance higher than 3. The body image disturbance had a significant negative correlation with age (rs= −0.325, P = 0.046). A significant association with higher body image disturbance score was seen in overweight participants (P < 0.05). The cutoff used to define overweight was 23 kg/m2, which is the WHO classification for the Asian population.[17] Furthermore, males and those who cannot meet their daily needs had higher body image disturbance, but this factor was not statistically significant [P = 0.486, P = 0.534, Table 3].
Table 3.
Association with demographic parameters
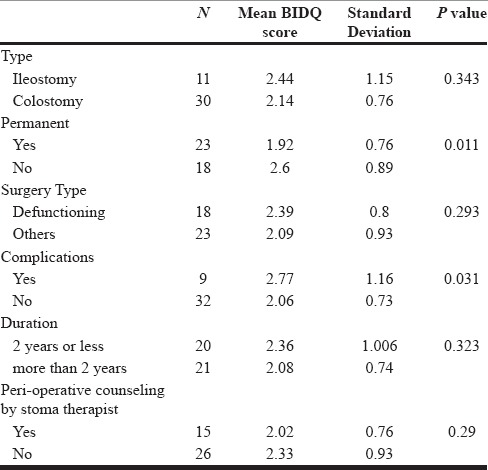
Analysis of ostomy related parameters revealed that those who had a temporary ostomy and stoma complications had significantly higher body image disturbance (P < 0.05). Those with ileostomies, duration <2 years, defunctioning ostomies and those who did not receive perioperative counseling by a specialized stoma therapist had a higher disturbance of body image which was not statistically significant [Table 4].
Table 4.
Association with ostomy related parameters
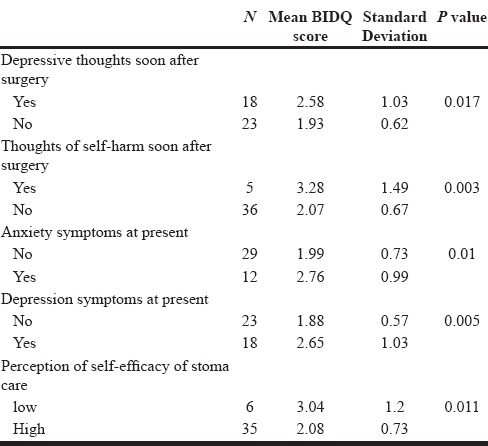
Analysis of psychological parameters revealed that those who claimed to have depressive thoughts and those who had thoughts of self-harm soon after surgery had significantly higher body image disturbance score. Similarly, those who had symptoms of depression and anxiety at the time of data collection had higher disturbance of body image, and this factor was statistically significant. Furthermore, there was a significant negative correlation with perception of self-efficacy and body image disturbance [rs= −0.655, P = 0.007, Table 5].
Table 5.
Association with psychological parameters
DISCUSSION
It has been shown that stomas tend to have a negative effect on the psychological well-being of patients.[18,19] To date, only a few studies have analyzed body image disturbance among stoma patients.[7,9,10,12] Similar studies done to assess body image in ostomates have shown that there was a considerably low perception of body image, which implies that the adaptation to the alteration of body image was poor and that the psychological rehabilitation was suboptimal.[7,10,20]
In our study, the mean body image disturbance score was 2.22 (SD ± 0.88). Of the participants, 7 (17.07%) out of 41 patients had a mean body image score of more than 3. We found several factors that were significantly associated with body image disturbance. Analysis of demographic factors showed a significant negative correlation with age (P < 0.05) which implies that younger patients have higher body image disturbance. This may be because younger individuals are more conscious of their appearance as they are more engaged in social and sexual activities compared to older individuals in our setting.
Those with high BMI had significantly higher body image disturbance score (P < 0.05). Studies have clearly shown that high BMI is associated with impaired body image even in otherwise healthy individuals.[21] Those who were overweight may have additional problems related to caring for ostomy and also have problems related to the style of clothing which could have indirectly influenced the perception of body image.
Males had higher disturbance of body image, but the association was not statistically significant. The higher disturbance may be because, in our setting, males are the usual breadwinners who need to socialize more compared to females who are generally at home. Creation of an ostomy can also have negative effects on their livelihood and also affect their productivity. Our findings are comparable to a similar study done by Hong et al.,[10] which showed that males have a significantly higher body image disturbance. In the same study, those who were married had lesser body image disturbance compared to those who were single, divorced, or separated. A descriptive cross-sectional study by Aktas and Gocman Baykara[22] showed that involving the partner in stoma care had significant positive influence on the body image of ostomates. This may be because emotional and social support by the partner had a positive impact on the perception of body image. Similarly, in our study, we noted that the body image disturbance was low in those who were married. However, the association was not statistically significant. Similar to a previous study,[10] we did not find a statistically significant association with other demographic parameters such as income or level of education.
In our study, of the ostomy-related parameters, significantly higher body image disturbance was noted among those with a temporary ostomy and those who developed complications of ostomy (P < 0.05). However, a study that compared the body image disturbance among temporary and permanent ostomies noted higher impairment among permanent ostomies which was not statistically significant.[10] The higher disturbance among temporary ostomies in our study may be due to several reasons. In our study, the follow-up duration for permanent ostomy was higher (although not statistically significant), and this may have allowed sufficient time for acceptance. Furthermore, most of the permanent ostomies were done for malignancies, and this factor may have influenced the score of the body image, as the life-threatening malignancy was removed as opposed to temporary ostomies, which were commonly done for inflammatory bowel disease and trauma in our participants. Furthermore, those with temporary ostomies were younger which may have caused a bias in our results. Those who had perioperative counseling by a specialized stoma therapist had lower body image disturbance, but it was not statistically significant. This may imply that counseling on psychological aspects such as body image needs further attention and should be made routine.
In this study, those with depressive symptoms and thoughts of self-harm soon after surgery had a significantly higher body image disturbance (P < 0.05 and P < 0.01). Furthermore, the rate of depression and anxiety in our sample was considerable as 43.9% of participants had at least mild depressive symptoms and 29.3% had at least mild anxiety symptoms at the time of data collection. Studies done among the general population of various groups on psychological well-being and body image have shown a significant association between body image and psychological parameters such as anxiety and depression.[23,24] However, only a few studies have compared body image and psychological well-being among ostomy patients.[10,25] A study conducted ostomy patients[10] assessed the self-esteem, level of depression and body image and noted a significant correlation among those parameters. Furthermore, lower level of body image and self-esteem and higher level of depression were also noted.[10]
Our study showed an association between perception of self-efficacy related to ostomy care and disturbance in body image (P < 0.01). Thus, helping the patient to adapt to this change in body image may help to improve self-efficacy in caring for one's ostomy.
Although this study is limited by its small sample size, it emphasized a few important findings, which may be helpful in the psychological rehabilitation of ostomy patients. Conducting case–control studies may be necessary to gain further insight on the risk factors of poor psychological adaptation to body image among stoma patients.
CONCLUSIONS
Poor adaptation to alteration of body image may be predicted by younger age, overweight, and temporary stoma. A significant association was noted with psychological parameters such as depression, anxiety, and also with reduced self-efficacy. We recommend that individuals at risk of poor adaptation should be identified before surgery and counseled regarding psychological adaptation before surgery, after surgery, and during follow-up visits to facilitate psychological rehabilitation. They should also be screened for depression and anxiety and may be referred to psychological interventions as needed. Furthermore, importance should be given to establish good psychological well-being to achieve a higher quality of life, in this group of patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Martinez LS, Schwartz JS, Freres D, Fraze T, Hornik RC. Patient-clinician information engagement increases treatment decision satisfaction among cancer patients through feeling of being informed. Patient Educ Couns. 2009;77:384–90. doi: 10.1016/j.pec.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atack L, Luke R, Chien E. Evaluation of patient satisfaction with tailored online patient education information. Comput Inform Nurs. 2008;26:258–64. doi: 10.1097/01.NCN.0000304838.52207.90. [DOI] [PubMed] [Google Scholar]
- 3.Smith DM, Loewenstein G, Rozin P, Sherriff RL, Ubel PA. Sensitivity to disgust, stigma, and adjustment to life with a colostomy. J Res Pers. 2007;41:787–803. doi: 10.1016/j.jrp.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McLellan A. Patient satisfaction: Public engagement with service information is key test of choice. Health Serv J. 2012;122:3. [PubMed] [Google Scholar]
- 5.Cash TF, Phillips KA, Santos MT, Hrabosky JI. Measuring “negative body image”: Validation of the body image disturbance questionnaire in a nonclinical population. Body Image. 2004;1:363–72. [Google Scholar]
- 6.Gawron CL. Body image changes in the patient requiring ostomy revision. J Enterostomal Ther. 1989;16:199–200. doi: 10.1097/00152192-198909000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Kiliç E, Taycan O, Belli AK, Ozmen M. The effect of permanent ostomy on body image, self-esteem, marital adjustment, and sexual functioning. Turk Psikiyatri Derg. 2007;18:302–10. [PubMed] [Google Scholar]
- 8.Morrall SE. The shock of the new. Altered body image after creation of a stoma. Prof Nurse. 1990;5:529–37. [PubMed] [Google Scholar]
- 9.Salter MJ. What are the differences in body image between patients with a conventional stoma compared with those who have had a conventional stoma followed by a continent pouch? J Adv Nurs. 1992;17:841–8. doi: 10.1111/j.1365-2648.1992.tb02006.x. [DOI] [PubMed] [Google Scholar]
- 10.Hong KS, Oh BY, Kim EJ, Chung SS, Kim KH, Lee RA. Psychological attitude to self-appraisal of stoma patients: Prospective observation of stoma duration effect to self-appraisal. Ann Surg Treat Res. 2014;86:152–60. doi: 10.4174/astr.2014.86.3.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gervaz P, Bucher P, Konrad B, Morel P, Beyeler S, Lataillade L, et al. A prospective longitudinal evaluation of quality of life after abdominoperineal resection. J Surg Oncol. 2008;97:14–9. doi: 10.1002/jso.20910. [DOI] [PubMed] [Google Scholar]
- 12.Jenks JM, Morin KH, Tomaselli N. The influence of ostomy surgery on body image in patients with cancer. Appl Nurs Res. 1997;10:174–80. doi: 10.1016/s0897-1897(97)80548-4. [DOI] [PubMed] [Google Scholar]
- 13.Cash TF, Grasso K. The norms and stability of new measures of the multidimensional body image construct. Body Image. 2005;2:199–203. doi: 10.1016/j.bodyim.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 14.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166:1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 16.Bekkers MJ, van Knippenberg FC, van den Borne HW, van Berge-Henegouwen GP. Prospective evaluation of psychosocial adaptation to stoma surgery: The role of self-efficacy. Psychosom Med. 1996;58:183–91. doi: 10.1097/00006842-199603000-00013. [DOI] [PubMed] [Google Scholar]
- 17.WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 18.Black PK. Psychological, sexual and cultural issues for patients with a stoma. Br J Nurs. 2004;13:692–7. doi: 10.12968/bjon.2004.13.12.13254. [DOI] [PubMed] [Google Scholar]
- 19.White CA, Hunt JC. Psychological factors in postoperative adjustment to stoma surgery. Ann R Coll Surg Engl. 1997;79:3–7. [PMC free article] [PubMed] [Google Scholar]
- 20.Cohen A. Body image in the person with a stoma. J Enterostomal Ther. 1991;18:68–71. [PubMed] [Google Scholar]
- 21.Makara-Studzinska M, Zaborska A. Obesity and body image. Psychiatr Pol. 2009;43:109–14. [PubMed] [Google Scholar]
- 22.Aktas D, Gocman Baykara Z. Body image perceptions of persons with a stoma and their partners: A descriptive, cross-sectional study. Ostomy Wound Manage. 2015;61:26–40. [PubMed] [Google Scholar]
- 23.Noles SW, Cash TF, Winstead BA. Body image, physical attractiveness, and depression. J Consult Clin Psychol. 1985;53:88–94. doi: 10.1037//0022-006x.53.1.88. [DOI] [PubMed] [Google Scholar]
- 24.Kim JS, Kang S. A study on body image, sexual quality of life, depression, and quality of life in middle-aged adults. Asian Nurs Res (Korean Soc Nurs Sci) 2015;9:96–103. doi: 10.1016/j.anr.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 25.Bullen TL, Sharpe L, Lawsin C, Patel DC, Clarke S, Bokey L. Body image as a predictor of psychopathology in surgical patients with colorectal disease. J Psychosom Res. 2012;73:459–63. doi: 10.1016/j.jpsychores.2012.08.010. [DOI] [PubMed] [Google Scholar]


