Abstract
Adenotonsillectomy remains one of the most common surgical procedures carried out in children. Though a commonly performed procedure, it poses a great challenge to the surgeon as well as the anaesthesiologist and is associated with a substantially increased risk of morbidity and mortality. In the post-operative period, it poses threats such as post-tonsillectomy bleeding and airway obstruction if not diagnosed and treated promptly. Various recent advances in airway management and early detection of post-operative complications have been made to reduce the sequelae associated with tonsillectomy. In this article, we have reviewed the various techniques, complications and recent advances, which have evolved in the anaesthetic technique related to adenotonsillectomy.
Keywords: Anaesthesia, bleeding tonsil, recent advances, laryngospasm
INTRODUCTION
Tonsillectomy with or without adenoidectomy is a long practiced and one of the most frequently performed surgical procedures in paediatric age group worldwide. The number has declined by approximately 50% from about 1.4 million in 1959 to about 2 lakh per year till date.[1] Though a commonly performed procedure, it poses a great challenge to the surgeon as well as the anaesthesiologist and is associated with a substantially increased risk of morbidity and mortality.[1,2]
In this article, we have reviewed the available information about the techniques, complications and recent advances. We reviewed studies, research articles, guidelines and meta-analysis from PubMed, Google Scholar, etc., using the following key words: adenotonsillectomy, posttonsillectomy bleeding and recent advances.
The tonsils and adenoids are lymphoid tissues forming part of the Waldeyer's ring encircling the pharynx. It appears in the 2nd year of life and attains the largest size between 4 and 7 years of age and then regresses.[1,2]
Clinical features of adenotonsillar hypertrophy are nasal obstruction, recurrent infections, secretory otitis media, decreased hearing (secondary to Eustachian tube dysfunction) and obstructive sleep apnoea (OSA).[1]
As per the American Academy of Otolaryngology–Head and Neck Surgery, the absolute indications of the procedure are enlarged tonsils with features of upper airway obstruction, dysphagia, sleep disorders, peritonsillar abscess not adequately responding to medical management, febrile seizures due to tonsillitis and tonsillar pathology requiring biopsy for a definitive diagnosis.[3]
DEMOGRAPHY AND HISTORY
The surgical rates are age and gender specific. Tonsillectomy is usually performed in older children whereas adenoidectomy is indicated in younger age group. Adenoidectomy has more of a male preponderance and tonsillectomy has more of female preponderance for unknown reason.[4]
This procedure was first described in the Hindu literature in 1000 BC. Cornelius Celsus and Paul of Aegina invented the blunt removal using their own fingernail or a metal hook. Samuel J. Crowe popularised the use of Crowe–Davis mouth gag and sharp dissection. In the early 20th century, complete tonsillectomies came into clinical practice and have evolved to the modern day.[5]
For a long time, the tonsillectomy operations were performed without anaesthesia, and general anaesthesia for adenotonsillectomies came into vogue around 1935. Two of the popular methods were the single dose method with ethyl chloride or nitrous oxide and ether insufflations of the oropharynx. Anaesthesia for tonsillectomies has evolved greatly to the present day with operations being performed under local as well as general anaesthesia. Airway management gained importance using endotracheal tube (ETT) or laryngeal mask airway (LMA) with either spontaneous or controlled ventilation, each technique having their own pros and cons. Post-operative pain and the incidence of nausea and vomiting have been greatly reduced with improved techniques and the use of multimodal approaches.[6,7]
GOALS OF ANAESTHETIC MANAGEMENT
Anaesthesia for adenotonsillectomy is a challenge to the anaesthesiologist. A safe conduct of anaesthesia is of utmost importance to avoid the complications and associated anxiety of the patient as well as the parents. Good communication between the surgeon, anaesthesiologist and the parents of the child is a must for a successful outcome.
The goals are adequate patient preparation with premedication, providing good surgical access while 'sharing the airway', optimising perioperative analgesia, preventing post-operative nausea and vomiting (PONV), perioperative airway management and prevention and timely management of post-operative haemorrhage and other complications.
SPECIAL CONCERNS
The concerns during the pre-operative evaluation of a patient presenting for adenotonsillectomy are those associated with the patient's age (paediatric age group), the American Society of Anesthesiologists physical status, recurrent upper respiratory infection (URI) episodes, associated comorbidities and coexisting syndromes. A special emphasis must be given on the history of bleeding tendencies and easy bruising, if any.[1,2] The risk for untoward respiratory complications following surgery include young age, medical comorbidity, OSA syndrome and recurrent respiratory infections.[1] Historically, the chief indication for adenotonsillectomy was recurrent infection. However, an increasing number of children are now presenting with obstructive symptoms as well as OSA syndrome (OSAS).[7,8]
Obstructive sleep apnoea syndrome and adenotonsillectomy
Children present with a far more different symptomatology as compared with adults. Daytime drowsiness and obesity are commonly seen in adults. Children present with an inability to thrive, issues with behaviour and poor school performance.[9,10,11] Severity of disease does not coincide with the symptomatology. Polysomnography, which is more specific, is not always available in all centres. The simpler and cheaper overnight oximetry provides evidence of severity of OSAS.[12] Surgery is the answer for patients with clinical features and symptoms suggesting OSAS. The anaesthesiologist must keep in mind of the increased post-operative complications expected in this high-risk group.
Upper respiratory infection
The question which arises in the presence of URI is whether to proceed with surgery and anaesthesia or to delay? URI in children is quite common, and most children experience 6–8 episodes per year. Airway reactivity is a persistent problem in this group of patients even after several weeks. It is suggested to proceed with anaesthesia and surgery if the infection is mild. These patients are at an increased risk of post-operative respiratory problems. High-risk patients include prematurity, age <5 years, use of an ETT, reactive airway disease, paternal smoking, copious secretions, nasal congestion and a high total white blood cell (WBC) count.[11] Whenever patient has fever with high total WBC count, thick mucopurulent secretion and associated lower respiratory tract infection, it is better to postpone the surgery for a later date.
The choice of anaesthetic technique matters, especially in the presence of URI. Evidence suggests that LMA may have advantages over tracheal tube, but it has not been used frequently for adenotonsillectomy. Anaesthetic medications with lower potency of airway irritation such as propofol, sevoflurane and halothane are preferred over those which cause airway irritation such as thiopental and desflurane. There is no definitive data on the use of anticholinergic drugs to reduce airway reactivity in a patient with URI. It has been suggested for deep extubation in a child with URI, but evidence is lacking as to which method has superiority over the other in patients with URI.[13,14,15]
Pre-operative investigations required are haemoglobin and haematocrit to rule out anaemia and polycythemia (in patients with OSA), total and differential WBC count to rule out active chest infection, bleeding and clotting time, prothrombin time and International Normalised Ratio (these tests are more relevant compared to bleeding time clotting time) and electrocardiogram (ECG) in patients with OSA (to rule out right heart involvement secondary to pulmonary artery hypertension). Pre-operative room air saturation will be of great help in selected cases.
PRE-OPERATIVE ANXIETY
The factors to be taken into consideration during this procedure are the younger age of the patient, anxiety of parents and associated behavioural problems, which increases the pre-operative anxiety. In addition, surgery lasting >30 min and previous admission to the hospitals are known risk factors for increased anxiety.[16,17,18] Premedication with oral midazolam (0.5 mg/kg) has been shown to be safe and reliable, and other drugs such as clonidine may be effective. Anxiolytics/sedatives must be carefully titrated in patients with OSAS as they are more prone to airway obstruction. As per data, presence of parents during induction of anaesthesia is of no proven benefit to reduce patient anxiety.[19,20,21]
Pedicloryl (triclofos), which is commonly used for younger children, has the potential to cause airway obstruction, especially in patients with big tonsils. Intranasal midazolam, fentanyl lollipop and recently drugs such as dexmedetomidine are used with varying results.
INTRA-OPERATIVE MANAGEMENT
A meticulous pre-anaesthetic evaluation and patient preparation is the key to successful anaesthetic management of adenotonsillectomy patients. Proper preparation of the operating room (OR) including the emergency drugs and airway equipment (appropriate size-reinforced LMA, Ring, Adair and Elwyn [RAE] and conventional ETTs, oral airways, working suction apparatus and anaesthesia drugs as per protocol) should be done. Good intravenous (IV) access is essential, and IV fluids as per body weight are advocated. Eyes must be taped and protected. Basic monitors including ECG, non-invasive blood pressure, pulse oximetry, end-tidal carbon dioxide (EtCO2), precordial stethoscope, temperature probe and neuromuscular monitoring must be available. EtCO2 is a very important tool to detect the ET tube obstruction due to the gag pressing on the tube and also the displacement of the ETT. Specific drugs which can be irritant to the airway (e.g., thiopentone, desflurane) and drugs causing significant side effects such as suxamethonium (dysrhythmias, hyperkalaemia, sudden unexpected death, muscle pain, malignant hyperthermia, masseter spasm and prolonged neuromuscular blockade in face of cholinesterase deficiency) must be avoided. However, suxamethonium has a role in peripheral setup and in patients with suspected difficult airway. Drugs known to cause histamine release (atracurium) must be avoided.[13]
Propofol is the most commonly used induction agent. Furthermore, propofol maintenance decreases the incidence of PONV as compared to isoflurane. Isoflurane is the most commonly used volatile agent for maintenance followed by halothane and sevoflurane.[13,14]
The gold standard of airway management during tonsillectomy surgery remains a tracheal tube. A preformed south pole-facing tube (oral RAE) is preferable, but we have to ensure that the surgeon uses a Boyle–Davis gag [Figure 1] with a central slit. Tube placement must be confirmed by bilateral auscultation after patient is put on position and Boyle–Davis mouth gag placement. Currently, there are an increasing number of surgeries done using LMA, usually reinforced type. Use of an LMA requires adequate training and experience for safe conduct of anaesthesia and has a learning curve associated with it. Anaesthesiologists must be aware of the possibility of airway obstruction that might occur with the use of Boyle–Davis mouth gag; the airway pressure must be checked.[1,2,14] After the surgery, patients must be extubated in lateral and head low position (post-tonsillectomy position) which should be maintained in the post-operative period.[18] Achievement of haemostasis and throat free of secretions or any gauze must be confirmed before extubation. Patients must be shifted to recovery room in lateral position and must be monitored for bleeding as well as deterioration of consciousness.[1,14]
Figure 1.

Positioning with Boyle – Davis gag with a slit for RAE tube
Coroner's clot
It is an occult clot of blood left behind the nasopharynx posterior to the soft palate. It usually occurs in surgeries in the area of nasopharynx or trauma, adenotonsillectomy being one of the common causes. It has the potential to cause fatal airway obstruction following extubation. In the past, the clot was retrieved only during the postmortem and hence the name. Management includes careful suctioning of the throat and nasopharynx under vision of a direct laryngoscope, especially in high-risk patients. Flexion of the neck during laryngoscopy can be useful to bring the clot more anterior and facilitate removal by suction.
POST-OPERATIVE ANALGESIA
Multimodal analgesia is the preferred technique to provide good post-operative analgesia. A combination of opioids and mild analgesics (non-steroidal anti-inflammatory drugs [NSAIDs] or paracetamol) as per age-specific indications and institutional protocol can be administered. Use of local anaesthetic for infiltration in the tonsillar fossa has found to be particularly effective in alleviating pain. Adequate post-operative analgesia also reduces the incidence of PONV and decreases the length of hospital stay.[1,2]
Antiemetics which can be used include ondansetron at a dose of 0.1 mg/kg IV or dexamethasone at a dose of 0.15 mg/kg IV. Post-operative complications include pain and throat discomfort, restlessness, nausea and vomiting, bleeding, laryngospasm and acute pulmonary oedema. The incidence of post-operative complications is linked to the surgical technique used. Cold steel dissection has the lowest risk of post-operative haemorrhage.[22] The use of diathermy increases the risk of post-operative haemorrhage. Extensive use of diathermy is associated with an increased incidence of post-operative pain.[22,23]
SPECIAL EMPHASIS
Post-tonsillectomy bleeding
Bleeding tonsil is one of the dreaded complications in this group of patients. It is an emergency and can lead to rapid deterioration of haemodynamics if not intervened in time. Three types of haemorrhage have been defined which are primary bleeding occurring at the time of surgery, secondary bleeding occurring between 4–6 days and reactionary occurring 8–48 h postoperatively.[24]
The anaesthetic management should be apt and poses many hazards and challenges. which require proper preparation for airway management, preventing aspiration and blood volume resuscitation.
The main factors to be considered are a dehydrated, agitated, hypovolaemic child with stomach full of blood clots, in a child who has just come out of anaesthesia and muscle relaxation. Signs include increased swallowing, pallor and an unexplained tachycardia. Investigation must include a full blood count, bleeding and clotting time, blood grouping and cross-match. Resuscitation must begin even prior to the commencement of anaesthesia and must be carried out throughout perioperative period depending on the circumstances.[2]
In a child with bleeding tonsil, large bore IV access with two wide bore cannulae and working suction should be ready in the OR. The presence of an experienced anaesthesiologist and a good communication between the surgeon and the anaesthesiologist helps to tackle this life-threatening emergency. Rapid sequence induction technique should be followed with dedication.
Laryngospasm
Tonsillectomy and adenoidectomy have the highest incidence of laryngospasm (21%–26%) in the immediate post-operative period.[25] Laryngospasm can be self-limiting, but if not treated timely can have deleterious effect and life-threatening consequences. Negative pressure pulmonary oedema, pulmonary aspiration, bradycardia, oxygen desaturation and cardiac arrest are known complications of laryngospasm. Patients must be given 100% oxygen and help should be sought for. Agents which are known to decrease the incidence of laryngospasm are topical lignocaine spray (up to 4 mg/kg) or IV 2% preservative-free lignocaine (1.5 mg/kg) 3 min before extubation. Magnesium sulphate 15 mg/kg over 20 min after tracheal intubation has shown to reduce the incidence of post-adenotonsillectomy laryngospasm. Use of IV propofol 0.25–0.5 mg/kg has also been shown to have positive results.[25] If laryngospasm has occurred, the Larson's manoeuvre can be used to break the spasm. Refractory cases can be managed with succinylcholine 0.5–0.8 mg/kg IV.
USEFUL PRACTICES AND CONTROVERSIES
Day care adenotonsillectomy
Nowadays, more and more adenotonsillectomies are being performed on day care basis. This involves good communication between the surgeon, anaesthesiologist and the parents of the child. A proper review of the procedure and the probable problems which may occur must be explained to the parents. Patients suitable for day care surgery in this group are the ones with uncomplicated medical history, who have easy transport available and who can be in hospital within an hour in case of emergencies. An Operational Guide Department of Health in 2002 included adenotonsillectomy in the list of day care procedures.[26] A careful patient selection is the key to improve the scope of day care adenotonsillectomies. Patients unfavourable for day care procedure include age <3 years, significant comorbidity, OSA, living >1 h drive from the hospital or having no private transport. A major problem to be dealt with is that of primary and reactionary haemorrhage and PONV. An extended observation period of 4–6 h before discharge is usually recommended. There is an increased incidence of overnight admission with PONV, pain and poor oral intake.[1,17,18] A multimodal plan of analgesia and proper antiemetics perioperatively reduces these problems. In Indian scenario, because of the not uncommon post-operative complications such as bleeding and airway obstruction, adenotonsillectomy is rarely practiced as a day care procedure.
Spontaneous or controlled ventilation
Studies suggest that there is no difference between the intra- and post-operative complications apart from an increase in EtCO2 with spontaneous ventilation. IPPV results in less haemodynamic variations and better recovery characteristics. The incidence of PONV and agitation is slightly increased during spontaneous ventilation as compared with controlled ventilation.[15,27] Thus, spontaneous ventilation has to be discouraged in the present-day practice.
Local infiltration anaesthesia
Lesser palatine and glossopharyngeal nerve blocks combined with general anaesthesia improves the operative conditions and provides excellent post-operative analgesia. Adult patients report pain-free periods almost up to 6 h postoperatively. The extubation process is much smoother in children receiving local anaesthesia in conjunction with general anaesthesia.[7,15]
Use of non-steroidal anti-inflammatory drugs
There is ongoing controversy regarding the use of NSAIDS in post-tonsillectomy patients with regard to its antiplatelet aggregating property. Till date, there are insufficient data to conclude that NSAIDS are associated with an increased incidence of bleeding with tonsillectomy. However, the use of ketorolac has been found to have increased incidence of bleeding as evidenced in a Cochrane analysis and hence must be avoided.[1,2] Thus, paracetamol suppository is quite popular for post-operative analgesia.
Extubation - deep versus awake
There is existing controversy regarding deep versus awake extubation. At present, there are no studies which clearly state one study to be better over the other. Deep extubation in these patients with head down left lateral position is preferred by some in spite of blood or secretions in the pharynx during tonsillectomy anaesthesia. The quality of recovery is smooth and undisturbed with reduced chances of oozing from the operative site. Studies have shown no difference in complication rate whether extubated deep or awake.[15,28] Use of IV lignocaine before extubation and intraoperative use of recent drugs such as dexmedetomidine and safer long-acting antiemetic drugs make the post-extubation and recovery period pleasant and uneventful.
Superhydration to prevent nausea and vomiting
PONV is a frequent complication in children that leads to prolonged stay and increased rates of readmission. Various studies have compared the effect of intraoperative hydration with 10–30 ml/kg/h of Ringer's lactate on PONV in children aged 1–12 years undergoing tonsillectomy. The higher volume hydration protocol significantly reduced PONV, and is cost-effective in the absence of prophylactic antiemetic therapy.[25,29] To avoid the risk of volume overload leading on to pulmonary oedema, this technique should be restricted only to older children.
Laryngeal mask airway versus tracheal tube
The tracheal tube provides a definitive airway, and a 'south-facing' oral RAE [Figure 2] tube positioned in the midline provides good surgical access. The disadvantages with tracheal intubation include the need for muscle paralysis, a deeper plane of anaesthesia, possibility of endobronchial intubation or accidental extubation with hyperextension of the neck. It is considered as gold standard as it provides a definite protection against aspiration. The question of deep or awake extubation to avoid a stormy emergence and bleeding also exists. The reinforced LMA offers a good airway, avoids the use of neuromuscular blocking agents, allows smooth emergence and airway protection until fully awake. The LMA can be removed with the cuff which is still partially inflated to avoid seeping of oral contents into the trachea. Hence, considering these advantages, the use of supraglottic airway devices such as LMAs should be encouraged.
Figure 2.
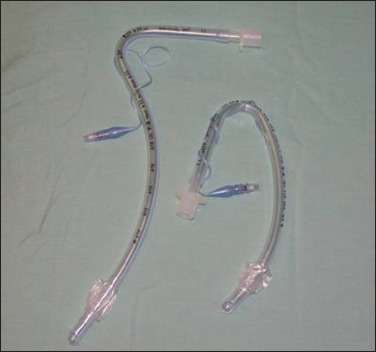
Ring Adair Elwyn tubes (south pole facing and north pole facing)
An incorrectly sized LMA or too large blade on the mouth gag can lead to obstruction and must be carefully checked.[1,2,15] LMA does not offer the definitive airway and it may restrict surgical access in younger patients. Airway patency must be re-confirmed before surgery proceeds with the use of both LMA and tracheal tube.
Nasal or oral intubation
In olden days, surgeons used to prefer nasal intubation as it provides wider surgical field, but it was associated with various disadvantages such as epistaxis, adenoid injury, nasopharyngeal tear and infection. Nowadays, with oral RAE tube, one can remove the elbow connector and anaesthetic breathing circuit from the surgical field with less trauma and infection rates. However, the oral RAE is associated with accidental bronchial intubation, cuff placement between the cords or displacement of tube.
Dexmedetomidine for the prevention of emergence agitation
Dexmedetomidine at the dose of 0.25–0.38 μg/kg has been tried to provide stable intraoperative haemodynamics and also to prevent emergence agitation produced by sevoflurane and desflurane. Thus, dexmedetomidine may have a definitive role in the prevention of emergence agitation after tonsillectomy.[30]
Adenotonsillectomy in rural settings
There is still a lingering controversy on the fate of day care adenoidectomy in rural settings. There is mixed evidence on including it as a day care procedure in rural settings given the lack of infrastructure and facilities in rural places. There are studies which show an increasing trend of day care adenotonsillectomies performed in the rural settings, provided the patient selection is appropriate.[31] Anaesthesiologists must be aware that there are higher chances of morbidity associated with this procedure, especially in the rural settings with lack of infrastructure, adequate equipment and support staff.
SUMMARY
Adenotonsillectomy, is still associated with life-threatening complications such as post-operative bleeding and airway obstruction. Hence, it should be dealt with utmost care, especially in peripheral setups with limited facilities as majority of these patients are of the paediatric age group coming from rural areas.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ravi R, Howell T. Anaesthesia for paediatric ear, nose, and throat surgery. Contin Educ Anaesth Crit Care Pain. 2007;7:33–7. [Google Scholar]
- 2.Strauss L. Anaesthetic management of paediatric adenotonsillectomy. S Afr Fam Pract. 2012;54:S17–20. [Google Scholar]
- 3.Practice Guidelines: AAO-HNS Guidelines for Tonsillectomy in Children and Adolescents - American Family Physician. [Last accessed on 2016 Aug 31]. Available from: http://www.aafp.org/afp/2011/0901/p566.html .
- 4.Glover JA. The incidence of tonsillectomy in school children: (Section of Epidemiology and State Medicine) Proc R Soc Med. 1938;31:1219–36. [PMC free article] [PubMed] [Google Scholar]
- 5.Feldmann H. 2000 year history of tonsillectomy. Images from the history of otorhinolaryngology, highlighted by instruments from the collection of the German Medical History Museum in Ingolstadt. Laryngorhinootologie. 1997;76:751–60. doi: 10.1055/s-2007-997520. [DOI] [PubMed] [Google Scholar]
- 6.Wrigley FR. The hazards and principles of anesthesia for tonsillectomy and adenoidectomy in children. Can Med Assoc J. 1958;79:459–63. [PMC free article] [PubMed] [Google Scholar]
- 7.Suvarna D, Fernandes S. Anesthesia management of adenotonsillectomy. Otorhinolaryngol Clin Int J. 2015;7:17–21. [Google Scholar]
- 8.Brown KA. What we don't know about childhood obstructive sleep apnoea. Paediatr Anaesth. 2001;11:385–9. doi: 10.1046/j.1460-9592.2001.00719.x. [DOI] [PubMed] [Google Scholar]
- 9.Warwick JP, Mason DG. Obstructive sleep apnoea syndrome in children. Anaesthesia. 1998;53:571–9. doi: 10.1046/j.1365-2044.1998.00370.x. [DOI] [PubMed] [Google Scholar]
- 10.Rosen GM, Muckle RP, Mahowald MW, Goding GS, Ullevig C. Postoperative respiratory compromise in children with obstructive sleep apnea syndrome: Can it be anticipated? Pediatrics. 1994;93:784–8. [PubMed] [Google Scholar]
- 11.Carroll JL, Loughlin GM. Diagnostic criteria for obstructive sleep apnea syndrome in children. Pediatr Pulmonol. 1992;14:71–4. doi: 10.1002/ppul.1950140202. [DOI] [PubMed] [Google Scholar]
- 12.Brouillette RT, Morielli A, Leimanis A, Waters KA, Luciano R, Ducharme FM. Nocturnal pulse oximetry as an abbreviated testing modality for pediatric obstructive sleep apnea. Pediatrics. 2000;105:405–12. doi: 10.1542/peds.105.2.405. [DOI] [PubMed] [Google Scholar]
- 13.Hatcher IS, Stack CG. Postal survey of the anaesthetic techniques used for paediatric tonsillectomy surgery. Paediatr Anaesth. 1999;9:311–5. doi: 10.1046/j.1460-9592.1999.00392.x. [DOI] [PubMed] [Google Scholar]
- 14.Barst SM, Markowitz A, Yossefy Y, Abramson A, Lebowitz P, Bienkowski RS. Propofol reduces the incidence of vomiting after tonsillectomy in children. Paediatr Anaesth. 1995;5:249–52. doi: 10.1111/j.1460-9592.1995.tb00293.x. [DOI] [PubMed] [Google Scholar]
- 15.Khan FA, Memon GA. Comparison of spontaneous with controlled mode of ventilation in tonsillectomy. Paediatr Anaesth. 2001;11:185–90. doi: 10.1046/j.1460-9592.2001.00641.x. [DOI] [PubMed] [Google Scholar]
- 16.Tait AR, Pandit UA, Voepel-Lewis T, Munro HM, Malviya S. Use of the laryngeal mask airway in children with upper respiratory tract infections: A comparison with endotracheal intubation. Anesth Analg. 1998;86:706–11. doi: 10.1097/00000539-199804000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Davidson AJ, Shrivastava PP, Jamsen K, Huang GH, Czarnecki C, Gibson MA, et al. Risk factors for anxiety at induction of anesthesia in children: A prospective cohort study. Paediatr Anaesth. 2006;16:919–27. doi: 10.1111/j.1460-9592.2006.01904.x. [DOI] [PubMed] [Google Scholar]
- 18.Cox RG. Anesthetic management of pediatric adenotonsillectomy. Can J Anaesth. 2007;54:1021–5. doi: 10.1007/BF03016639. [DOI] [PubMed] [Google Scholar]
- 19.Kain ZN, Mayes LC, Wang SM, Caramico LA, Hofstadter MB. Parental presence during induction of anesthesia versus sedative premedication: Which intervention is more effective? Anesthesiology. 1998;89:1147–56. doi: 10.1097/00000542-199811000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Kain ZN, Caldwell-Andrews AA, Mayes LC, Weinberg ME, Wang SM, MacLaren JE, et al. Family-centered preparation for surgery improves perioperative outcomes in children: A randomized controlled trial. Anesthesiology. 2007;106:65–74. doi: 10.1097/00000542-200701000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Calipel S, Lucas-Polomeni MM, Wodey E, Ecoffey C. Premedication in children: Hypnosis versus midazolam. Paediatr Anaesth. 2005;15:275–81. doi: 10.1111/j.1460-9592.2004.01514.x. [DOI] [PubMed] [Google Scholar]
- 22.Georgalas CC, Tolley NS, Narula A. Recurrent throat infections (tonsillitis) BMJ Clin Evid 2007. 2007 pii: 0503. [PubMed] [Google Scholar]
- 23.Alalami AA, Ayoub CM, Baraka AS. Laryngospasm: Review of different prevention and treatment modalities. Paediatr Anaesth. 2008;18:281–8. doi: 10.1111/j.1460-9592.2008.02448.x. [DOI] [PubMed] [Google Scholar]
- 24.Lock C, Wilson J, Steen N, Eccles M, Mason H, Carrie S, et al. North of England and Scotland Study of Tonsillectomy and Adeno-tonsillectomy in Children (NESSTAC): A pragmatic randomised controlled trial with a parallel non-randomised preference study. Health Technol Assess. 2010;14:1–164. doi: 10.3310/hta14130. iii-iv. [DOI] [PubMed] [Google Scholar]
- 25.Elgueta MF, Echevarría GC, De la Fuente N, Cabrera F, Valderrama A, Cabezón R, et al. Effect of intravenous fluid therapy on postoperative vomiting in children undergoing tonsillectomy. Br J Anaesth. 2013;110:607–14. doi: 10.1093/bja/aes453. [DOI] [PubMed] [Google Scholar]
- 26.Health Department of Day Surgery: Operational Guide. 2002. [Last cited on 2016 Dec 06]. Available from: http://www.webarchive.nationalarchives.gov.uk/content/+/
- 27.Deutsch ES. Tonsillectomy and adenoidectomy. Changing indications. Pediatr Clin North Am. 1996;43:1319–38. doi: 10.1016/s0031-3955(05)70521-6. [DOI] [PubMed] [Google Scholar]
- 28.Dillon FX. Safety considerations for otolaryngologic surgery in anaesthesia for otolaryngologic and head and neck surgery. Anaesth Clin North Am. 1993;11:637–49. [Google Scholar]
- 29.Murshed H, Islam M, Wahab M, Al-Azad M. Effect of preoperative bolus supplemental fluid on postoperative nausea and vomiting – A prospective study. [Last cited on 2016 Sep 01];J Armed Forces Med Coll Bangladesh [Internet] 2013 8:16–21. Available from: http://www.banglajol.info/index.php/JAFMC/article/view/16342 . [Google Scholar]
- 30.Kim HS, Byon HJ, Kim JE, Park YH, Lee JH, Kim JT. Appropriate dose of dexmedetomidine for the prevention of emergence agitation after desflurane anesthesia for tonsillectomy or adenoidectomy in children: Up and down sequential allocation. BMC Anesthesiol. 2015;15:79. doi: 10.1186/s12871-015-0059-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Siddiqui N, Yung MW. Day-case adenoidectomy: How popular and safe in a rural environment? J Laryngol Otol. 1997;111:444–6. doi: 10.1017/s0022215100137594. [DOI] [PubMed] [Google Scholar]


